|
1
|
Romero V, Akpinar H and Assimos DG: Kidney
stones: A global picture of prevalence, incidence, and associated
risk factors. Rev Urol. 12:e86–e96. 2010.PubMed/NCBI
|
|
2
|
Morgan MS and Pearle MS: Medical
management of renal stones. BMJ. 352:i522016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Zeng G, Mai Z, Xia S, Wang Z, Zhang K,
Wang L, Long Y, Ma J, Li Y, Wan SP, et al: Prevalence of kidney
stones in China: An ultrasonography based cross-sectional study.
BJU Int. 120:109–116. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ziemba JB and Matlaga BR: Epidemiology and
economics of nephrolithiasis. Investig Clin Urol. 58:299–306. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Eisner BH and Goldfarb DS: A nomogram for
the prediction of kidney stone recurrence. J Am Soc Nephrol.
25:2685–2687. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Brikowski TH, Lotan Y and Pearle MS:
Climate-related increase in the prevalence of urolithiasis in the
United States. Proc Natl Acad Sci USA. 105:9841–9846. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Abeywickarama B, Ralapanawa U and
Chandrajith R: Geoenvironmental factors related to high incidence
of human urinary calculi (kidney stones) in Central Highlands of
Sri Lanka. Environ Geochem Health. 38:1203–1214. 2016. View Article : Google Scholar
|
|
8
|
Wang Z, Zhang JW, Zhang Y, Zhang SP, Hu QY
and Liang H: Analyses of long non-coding RNA and mRNA profiling
using RNA sequencing in calcium oxalate monohydrate-stimulated
renal tubular epithelial cells. Urolithiasis. 47:225–234. 2019.
View Article : Google Scholar
|
|
9
|
Parmar MS: Kidney stones. BMJ.
328:1420–1424. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ye Z, Zeng G, Yang H, Li J, Tang K, Wang
G, Wang S, Yu Y, Wang Y, Zhang T, et al: The status and
characteristics of urinary stone composition in China. BJU Int.
125:801–809. 2020. View Article : Google Scholar
|
|
11
|
Aggarwal KP, Narula S, Kakkar M and Tandon
C: Nephrolithiasis: Molecular mechanism of renal stone formation
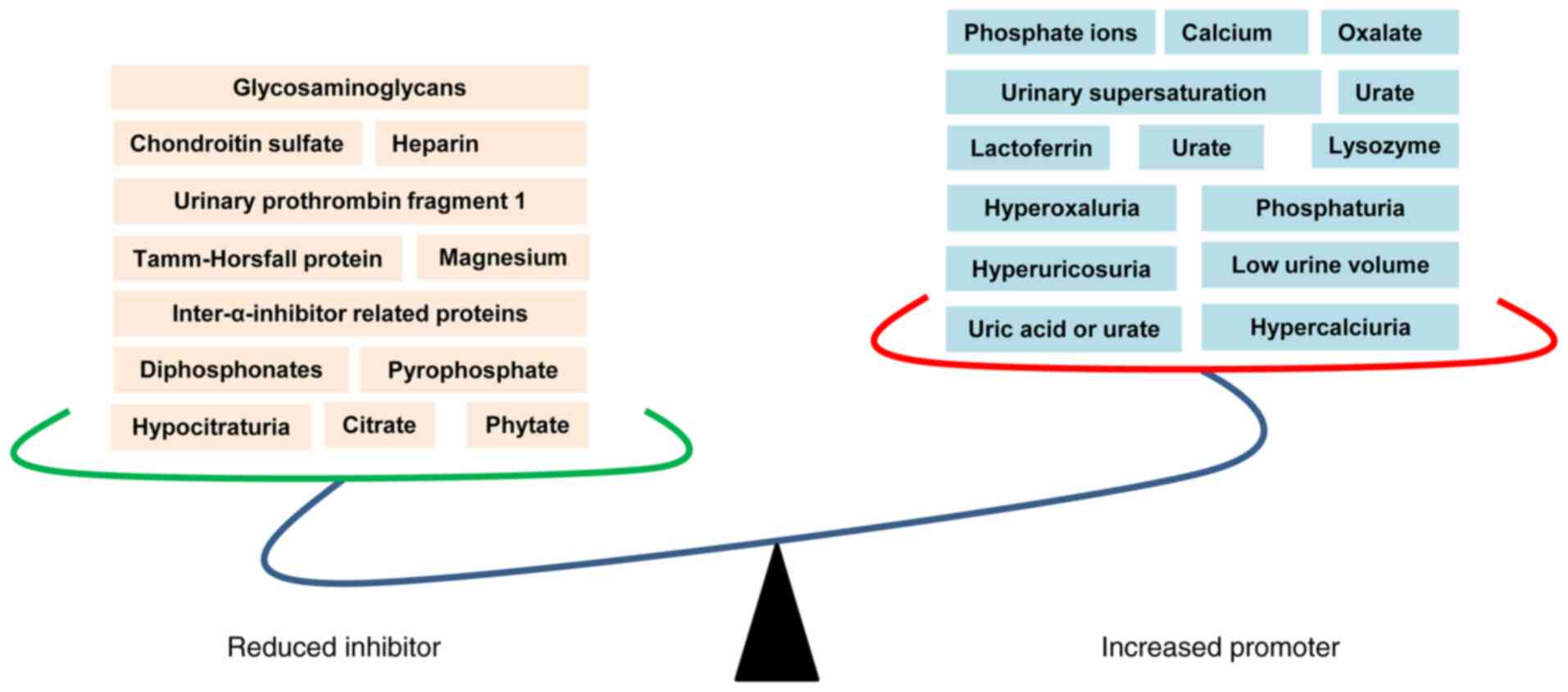
and the critical role played by modulators. Biomed Res Int.
2013:2929532013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Khan SR, Pearle MS, Robertson WG, Gambaro
G, Canales BK, Doizi S, Traxer O and Tiselius HG: Kidney stones.
Nat Rev Dis Primers. 2:160082016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Sun X, Shen L, Cong X, Zhu H, He L and Lu
J: Infrared spectroscopic analysis of 5,248 urinary stones from
Chinese patients presenting with the first stone episode. Urol Res.
39:339–343. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
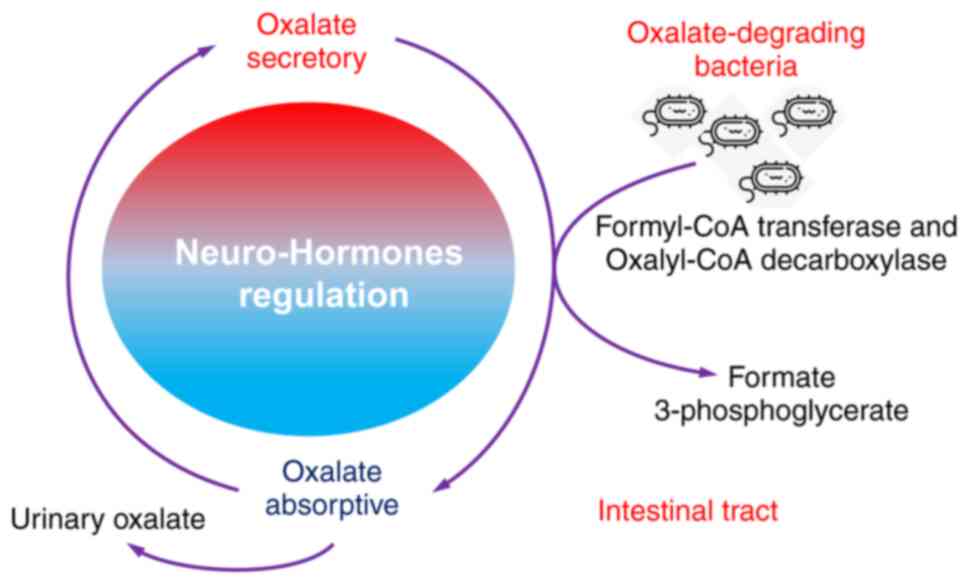
14
|
Hamamoto S, Taguchi K and Fujii Y:
Molecular mechanism of renal stone formation. Clin Calcium.
21:1481–1487. 2011.In Japanese. PubMed/NCBI
|
|
15
|
Pak CY, Sakhaee K, Moe O, Preminger GM,
Poindexter JR, Peterson RD, Pietrow P and Ekeruo W: Biochemical
profile of stone-forming patients with diabetes mellitus. Urology.
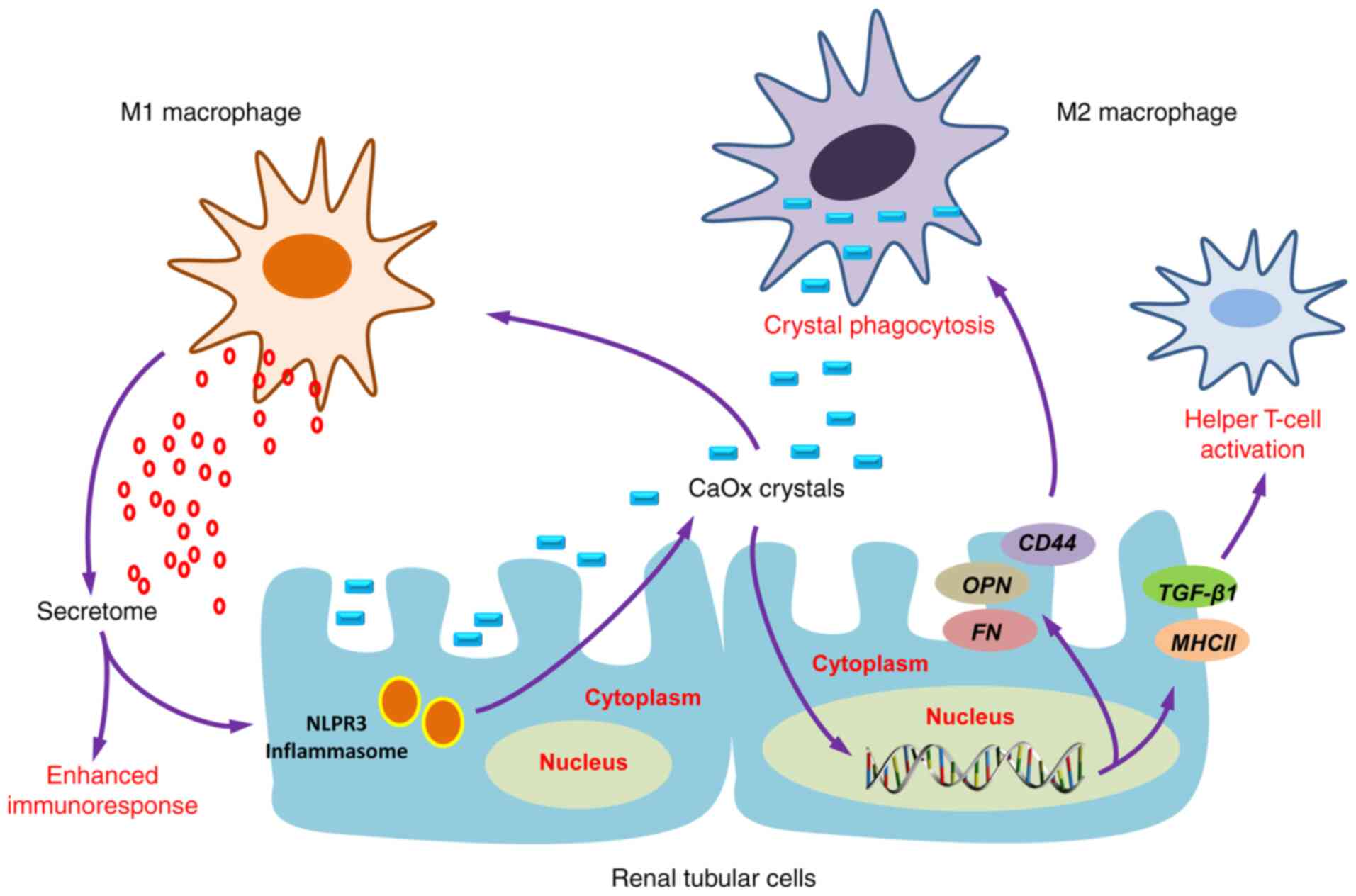
61:523–527. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Carbone A, Al Salhi Y, Tasca A, Palleschi
G, Fuschi A, De Nunzio C, Bozzini G, Mazzaferro S and Pastore AL:
Obesity and kidney stone disease: A systematic review. Minerva Urol
Nefrol. 70:393–400. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Devarajan A: Cross-talk between renal
lithogenesis and atherosclerosis: An unveiled link between kidney
stone formation and cardiovascular diseases. Clin Sci (Lond).
132:615–626. 2018. View Article : Google Scholar
|
|
18
|
Kittanamongkolchai W, Mara KC, Mehta RA,
Vaughan LE, Denic A, Knoedler JJ, Enders FT, Lieske JC and Rule AD:
Risk of hypertension among first-time symptomatic kidney stone
formers. Clin J Am Soc Nephrol. 12:476–482. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Rule AD, Bergstralh EJ, Melton LJ III, Li
X, Weaver AL and Lieske JC: Kidney stones and the risk for chronic
kidney disease. Clin J Am Soc Nephrol. 4:804–811. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Keddis MT and Rule AD: Nephrolithiasis and
loss of kidney function. Curr Opin Nephrol Hypertens. 22:390–396.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Dhondup T, Kittanamongkolchai W, Vaughan
LE, Mehta RA, Chhina JK, Enders FT, Hickson LJ, Lieske JC and Rule
AD: Risk of ESRD and mortality in kidney and bladder stone formers.
Am J Kidney Dis. 72:790–797. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Voss S, Hesse A, Zimmermann DJ, Sauerbruch
T and von Unruh GE: Intestinal oxalate absorption is higher in
idiopathic calcium oxalate stone formers than in healthy controls:
Measurements with the [(13)C2]oxalate absorption test. J Urol.
175:1711–1715. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Ha YS, Tchey DU, Kang HW, Kim YJ, Yun SJ,
Lee SC and Kim WJ: Phosphaturia as a promising predictor of
recurrent stone formation in patients with urolithiasis. Korean J
Urol. 51:54–59. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Dean C, Kanellos J, Pham H, Gomes M, Oates
A, Grover P and Ryall R: Effects of inter-alpha-inhibitor and
several of its derivatives on calcium oxalate crystallization in
vitro. Clin Sci (Lond). 98:471–480. 2000. View Article : Google Scholar
|
|
25
|
Daudon M, Frochot V, Bazin D and Jungers
P: Drug-induced kidney stones and crystalline nephropathy:
Pathophysiology, prevention and treatment. Drugs. 78:163–201. 2018.
View Article : Google Scholar
|
|
26
|
Rodgers AL: Physicochemical mechanisms of
stone formation. Urolithiasis. 45:27–32. 2017. View Article : Google Scholar
|
|
27
|
Thongboonkerd V: Proteomics of
crystal-cell interactions: A model for kidney stone research.
Cells. 8:10762019. View Article : Google Scholar
|
|
28
|
Wang Z, Li MX, Xu CZ, Zhang Y, Deng Q, Sun
R, Hu QY, Zhang SP, Zhang JW and Liang H: Comprehensive study of
altered proteomic landscape in proximal renal tubular epithelial
cells in response to calcium oxalate monohydrate crystals. BMC
Urol. 20:1362020. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Fong-Ngern K, Sueksakit K and
Thongboonkerd V: Surface heat shock protein 90 serves as a
potential receptor for calcium oxalate crystal on apical membrane
of renal tubular epithelial cells. J Biol Inorg Chem. 21:463–474.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Kumar V, Farell G, Deganello S and Lieske
JC: Annexin II is present on renal epithelial cells and binds
calcium oxalate monohydrate crystals. J Am Soc Nephrol. 14:289–297.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Anan G, Yoneyama T, Noro D, Tobisawa Y,
Hatakeyama S, Sutoh Yoneyama M, Yamamoto H, Imai A, Iwamura H,
Kohada Y, et al: The impact of glycosylation of osteopontin on
urinary stone formation. Int J Mol Sci. 21:932019. View Article : Google Scholar
|
|
32
|
Wiener SV, Ho SP and Stoller ML:
Beginnings of nephrolithiasis: Insights into the past, present and
future of Randall's plaque formation research. Curr Opin Nephrol
Hypertens. 27:236–242. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Sheng X, Ward MD and Wesson JA: Crystal
surface adhesion explains the pathological activity of calcium
oxalate hydrates in kidney stone formation. J Am Soc Nephrol.
16:1904–1908. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Ketha H, Singh RJ, Grebe SK, Bergstralh
EJ, Rule AD, Lieske JC and Kumar R: Altered calcium and vitamin D
homeostasis in first-time calcium kidney stone-formers. PLoS One.
10:e01373502015. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Vezzoli G, Macrina L, Magni G and
Arcidiacono T: Calcium-sensing receptor: Evidence and hypothesis
for its role in nephrolithiasis. Urolithiasis. 47:23–33. 2019.
View Article : Google Scholar
|
|
36
|
Farell G, Huang E, Kim SY, Horstkorte R
and Lieske JC: Modulation of proliferating renal epithelial cell
affinity for calcium oxalate monohydrate crystals. J Am Soc
Nephrol. 15:3052–3062. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Gao J, Xue JF, Xu M, Gui BS, Wang FX and
Ouyang JM: Nanouric acid or nanocalcium phosphate as central nidus
to induce calcium oxalate stone formation: A high-resolution
transmission electron microscopy study on urinary nanocrystallites.
Int J Nanomedicine. 9:4399–4409. 2014.PubMed/NCBI
|
|
38
|
Ratkalkar VN and Kleinman JG: Mechanisms
of stone formation. Clin Rev Bone Miner Metab. 9:187–197. 2011.
View Article : Google Scholar
|
|
39
|
Moe OW, Abate N and Sakhaee K:
Pathophysiology of uric acid nephrolithiasis. Endocrinol Metab Clin
North Am. 31:895–914. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Shekarriz B and Stoller ML: Uric acid
nephrolithiasis: Current concepts and controversies. J Urol.
168:1307–1314. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Song L and Maalouf NM: Nephrolithiasis.
Endotext. Feingold KR, Anawalt B, Boyce A, Chrousos G, de Herder
WW, Dungan K, Grossman A, Hershman JM, Hofland HJ, Kaltsas G, et
al: MDText.com, Inc. South Dartmouth, MA: 2000
|
|
42
|
Farmanesh S, Chung J, Sosa RD, Kwak JH,
Karande P and Rimer JD: Natural promoters of calcium oxalate
monohydrate crystallization. J Am Chem Soc. 136:12648–12657. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Worcester EM: Urinary calcium oxalate
crystal growth inhibitors. J Am Soc Nephrol. 5(Suppl 1): S46–S53.
1994. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Schepers MS, van der Boom BG, Romijn JC,
Schroder FH and Verkoelen CF: Urinary crystallization inhibitors do
not prevent crystal binding. J Urol. 167:1844–1847. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Khan SR and Kok DJ: Modulators of urinary
stone formation. Front Biosci. 9:1450–1482. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Hess B, Jordi S, Zipperle L, Ettinger E
and Giovanoli R: Citrate determines calcium oxalate crystallization
kinetics and crystal morphology-studies in the presence of
Tamm-Horsfall protein of a healthy subject and a severely recurrent
calcium stone former. Nephrol Dial Transplant. 15:366–374. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Cicerello E, Ciaccia M, Cova G and Mangano
M: The impact of potassium citrate therapy in the natural course of
Medullary Sponge Kidney with associated nephrolithiasis. Arch Ital
Urol Androl. 91:102–106. 2019. View Article : Google Scholar
|
|
48
|
Siener R: Dietary treatment of metabolic
acidosis in chronic kidney disease. Nutrients. 10:5122018.
View Article : Google Scholar :
|
|
49
|
Kim D, Rimer JD and Asplin JR:
Hydroxycitrate: A potential new therapy for calcium urolithiasis.
Urolithiasis. 47:311–320. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Chung J, Granja I, Taylor MG, Mpourmpakis
G, Asplin JR and Rimer JD: Molecular modifiers reveal a mechanism
of pathological crystal growth inhibition. Nature. 536:446–450.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Ryall RL, Harnett RM and Marshall VR: The
effect of urine, pyrophosphate, citrate, magnesium and
glycosaminoglycans on the growth and aggregation of calcium oxalate
crystals in vitro. Clin Chim Acta. 112:349–356. 1981. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Riley JM, Kim H, Averch TD and Kim HJ:
Effect of magnesium on calcium and oxalate ion binding. J Endourol.
27:1487–1492. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Grases F, Rodriguez A and Costa-Bauza A:
Efficacy of mixtures of magnesium, citrate and phytate as calcium
oxalate crystallization inhibitors in urine. J Urol. 194:812–819.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Robertson WG: Do 'inhibitors of
crystallisation' play any role in the prevention of kidney stones?
A critique. Urolithiasis. 45:43–56. 2017. View Article : Google Scholar
|
|
55
|
Randall A: The origin and growth of renal
calculi. Ann Surg. 105:1009–1027. 1937. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Wiener SV, Chen L, Shimotake AR, Kang M,
Stoller ML and Ho SP: Novel insights into renal mineralization and
stone formation through advanced imaging modalities. Connect Tissue
Res. 59:S102–S110. 2018. View Article : Google Scholar
|
|
57
|
Daudon M, Bazin D and Letavernier E:
Randall's plaque as the origin of calcium oxalate kidney stones.
Urolithiasis. 43(Suppl 1): S5–S11. 2015. View Article : Google Scholar
|
|
58
|
Khan SR, Canales BK and
Dominguez-Gutierrez PR: Randall's plaque and calcium oxalate stone
formation: Role for immunity and inflammation. Nat Rev Nephrol.
17:417–433. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Chung HJ: The role of Randall plaques on
kidney stone formation. Transl Androl Urol. 3:251–254.
2014.PubMed/NCBI
|
|
60
|
Bouderlique E, Tang E, Perez J, Coudert A,
Bazin D, Verpont MC, Duranton C, Rubera I, Haymann JP, Leftheriotis
G, et al: Vitamin D and calcium supplementation accelerates
Randall's plaque formation in a murine model. Am J Pathol.
189:2171–2180. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Winfree S, Weiler C, Bledsoe SB, Gardner
T, Sommer AJ, Evan AP, Lingeman JE, Krambeck AE, Worcester EM,
El-Achkar TM and Williams JC Jr: Multimodal imaging reveals a
unique autofluorescence signature of Randall's plaque.
Urolithiasis. 49:123–135. 2021. View Article : Google Scholar
|
|
62
|
Zhu Z, Huang F, Xia W, Zeng H, Gao M, Li
Y, Zeng F, He C, Chen J, Chen Z, et al: Osteogenic differentiation
of renal interstitial fibroblasts promoted by lncRNA MALAT1 may
partially contribute to Randall's plaque formation. Front Cell Dev
Biol. 8:5963632020. View Article : Google Scholar
|
|
63
|
Zhu Z, Cui Y, Huang F, Zeng H, Xia W, Zeng
F, He C, Chen J, Chen Z, Chen H and Li Y: Long non-coding RNA H9
promotes osteogenic differentiation of renal interstitial
fibroblasts through Wnt-beta-catenin pathway. Mol Cell Biochem.
470:145–155. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Liu H, Ye T, Yang X, Liu J, Jiang K, Lu H,
Xia D, Peng E, Chen Z, Sun F, et al: H19 promote calcium oxalate
nephrocalcinosis-induced renal tubular epithelial cell injury via a
ceRNA pathway. EBioMedicine. 50:366–378. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Fan J, Chandhoke PS and Grampsas SA: Role
of sex hormones in experimental calcium oxalate nephrolithiasis. J
Am Soc Nephrol. 10(Suppl 14): S376–S380. 1999.PubMed/NCBI
|
|
66
|
Li JY, Zhou T, Gao X, Xu C, Sun Y, Peng Y,
Chang Z, Zhang Y, Jiang J, Wang L and Hou J: Testosterone and
androgen receptor in human nephrolithiasis. J Urol. 184:2360–2363.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Gupta K, Gill GS and Mahajan R: Possible
role of elevated serum testosterone in pathogenesis of renal stone
formation. Int J Appl Basic Med Res. 6:241–244. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Fuster DG, Morard GA, Schneider L,
Mattmann C, Lüthi D, Vogt B and Dhayat NA: Association of urinary
sex steroid hormones with urinary calcium, oxalate and citrate
excretion in kidney stone formers. Nephrol Dial Transplant. Dec
9–2020.Epub ahead of print. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Yoshihara H, Yamaguchi S and Yachiku S:
Effect of sex hormones on oxalate-synthesizing enzymes in male and
female rat livers. J Urol. 161:668–673. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Liang L, Li L, Tian J, Lee SO, Dang Q,
Huang CK, Yeh S, Erturk E, Bushinsky D, Chang LS, et al: Androgen
receptor enhances kidney stone-CaOx crystal formation via
modulation of oxalate biosynthesis & oxidative stress. Mol
Endocrinol. 28:1291–1303. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Peng Y, Fang Z, Liu M, Wang Z, Li L, Ming
S, Lu C, Dong H, Zhang W, Wang Q, et al: Testosterone induces renal
tubular epithelial cell death through the HIF-1alpha/BNIP3 pathway.
J Transl Med. 17:622019. View Article : Google Scholar
|
|
72
|
Changtong C, Peerapen P, Khamchun S,
Fong-Ngern K, Chutipongtanate S and Thongboonkerd V: In vitro
evidence of the promoting effect of testosterone in kidney stone
disease: A proteomics approach and functional validation. J
Proteomics. 144:11–22. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Zhu W, Zhao Z, Chou F, Zuo L, Liu T, Yeh
S, Bushinsky D, Zeng G and Chang C: Loss of the androgen receptor
suppresses intrarenal calcium oxalate crystals deposition via
altering macrophage recruitment/M2 polarization with change of the
miR-185-5p/CSF-1 signals. Cell Death Dis. 10:2752019. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Sueksakit K and Thongboonkerd V:
Protective effects of finasteride against testosterone-induced
calcium oxalate crystallization and crystal-cell adhesion. J Biol
Inorg Chem. 24:973–983. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Peerapen P and Thongboonkerd V: Protective
cellular mechanism of estrogen against kidney stone formation: A
proteomics approach and functional validation. Proteomics.
19:e19000952019. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Zhu W, Zhao Z, Chou FJ, Zuo L, Liu T,
Bushinsky D, Chang C, Zeng G and Yeh S: The protective roles of
estrogen receptor β in renal calcium oxalate crystal formation via
reducing the liver oxalate biosynthesis and renal oxidative
stress-mediated cell injury. Oxid Med Cell Longev.
2019:53050142019. View Article : Google Scholar
|
|
77
|
Loughlin KR: The clinical applications of
five-alpha reductase inhibitors. Can J Urol. 28:10584–10588.
2021.PubMed/NCBI
|
|
78
|
Tian H, Chou FJ, Tian J, Zhang Y, You B,
Huang CP, Yeh S, Niu Y and Chang C: ASC-J9® suppresses
prostate cancer cell proliferation and invasion via altering the
ATF3-PTK2 signaling. J Exp Clin Cancer Res. 40:32021. View Article : Google Scholar
|
|
79
|
Hu H, Zhou H and Xu D: A review of the
effects and molecular mechanisms of dimethylcurcumin (ASC-J9) on
androgen receptor-related diseases. Chem Biol Drug Des. 97:821–835.
2021. View Article : Google Scholar
|
|
80
|
Andy G, John M, Mirna S, Rachita D,
Michael K, Maja K, Aseem S and Zeljana B: Controversies in the
treatment of androgenetic alopecia: The history of finasteride.
Dermatol Ther. 32:e126472019. View Article : Google Scholar
|
|
81
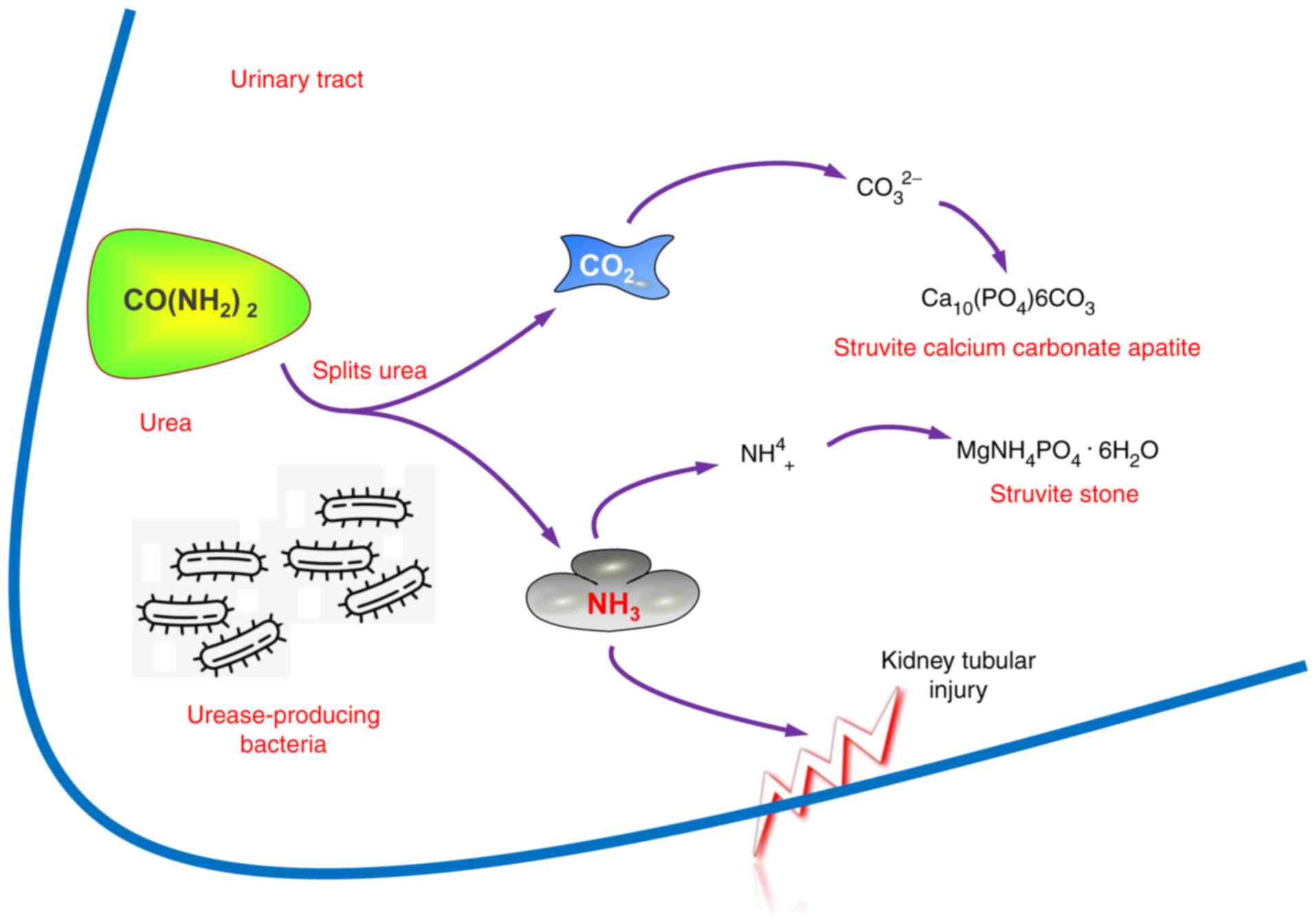
|
Whiteside SA, Razvi H, Dave S, Reid G and
Burton JP: The microbiome of the urinary tract-a role beyond
infection. Nat Rev Urol. 12:81–90. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Bichler KH, Eipper E, Naber K, Braun V,
Zimmermann R and Lahme S: Urinary infection stones. Int J
Antimicrob Agents. 19:488–498. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Espinosa-Ortiz EJ, Eisner BH, Lange D and
Gerlach R: Current insights into the mechanisms and management of
infection stones. Nat Rev Urol. 16:35–53. 2019. View Article : Google Scholar
|
|
84
|
Marien T and Miller NL: Treatment of the
Infected Stone. Urol Clin North Am. 42:459–472. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
de Cógáin MR, Lieske JC, Vrtiska TJ, Tosh
PK and Krambeck AE: Secondarily infected nonstruvite urolithiasis:
A prospective evaluation. Urology. 84:1295–1300. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Flannigan R, Choy WH, Chew B and Lange D:
Renal struvite stones-pathogenesis, microbiology, and management
strategies. Nat Rev Urol. 11:333–341. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Mehta M, Goldfarb DS and Nazzal L: The
role of the microbiome in kidney stone formation. Int J Surg.
36:607–612. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Martel J, Peng HH, Young D, Wu CY and
Young JD: Of nanobacteria, nanoparticles, biofilms and their role
in health and disease: Facts, fancy and future. Nanomedicine
(Lond). 9:483–499. 2014. View Article : Google Scholar
|
|
89
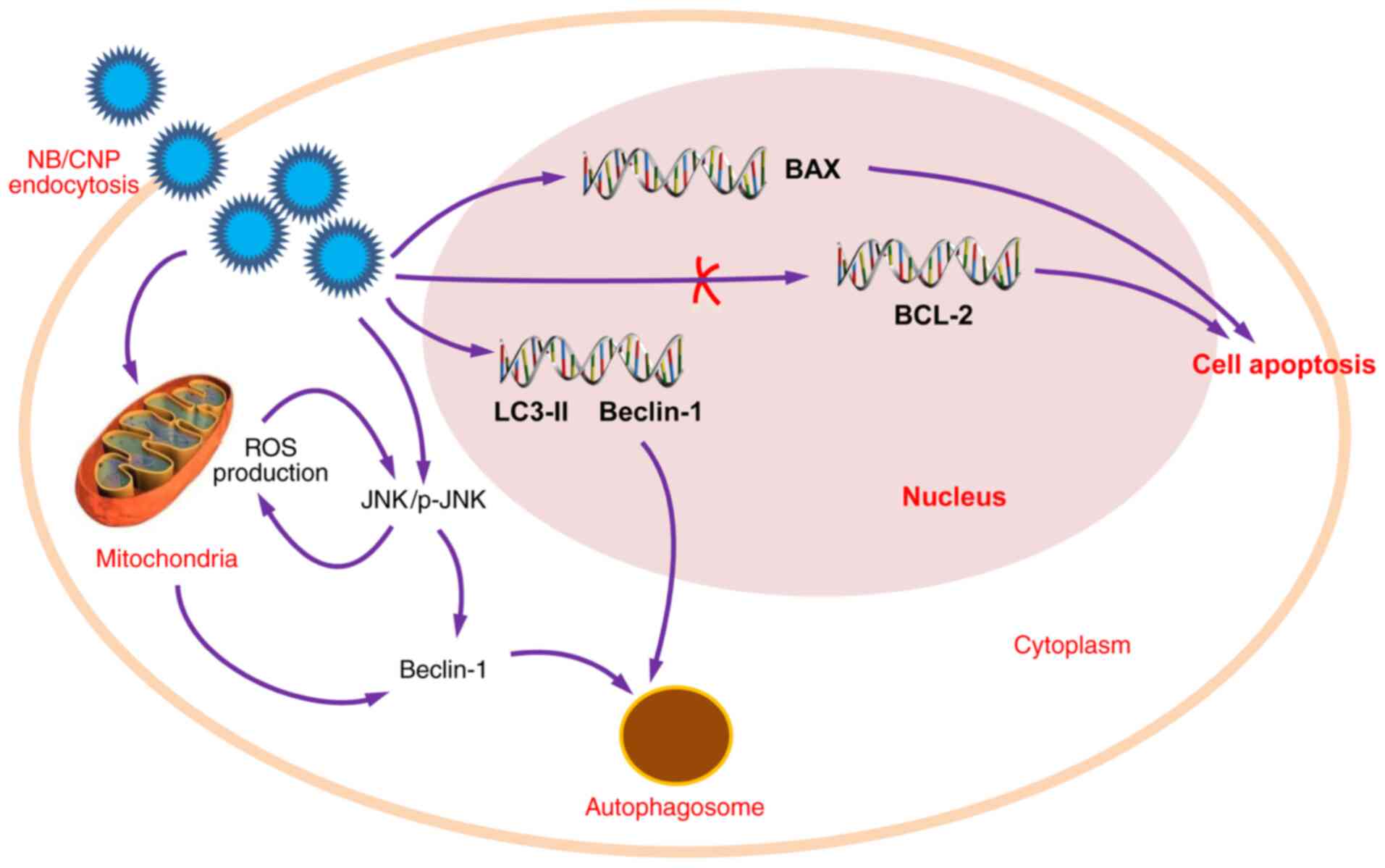
|
Wu J, Tao Z, Deng Y, Liu Q, Liu Y, Guan X
and Wang X: Calcifying nanoparticles induce cytotoxicity mediated
by ROS-JNK signaling pathways. Urolithiasis. 47:125–135. 2019.
View Article : Google Scholar
|
|
90
|
Ansari H, Akhavan Sepahi A and Akhavan
Sepahi M: Different approaches to detect 'Nanobacteria' in patients
with kidney stones: An infectious cause or a subset of life? Urol
J. 14:5001–5007. 2017.PubMed/NCBI
|
|
91
|
Kajander EO, Ciftcioglu N, Aho K and
Garcia-Cuerpo E: Characteristics of nanobacteria and their possible
role in stone formation. Urol Res. 31:47–54. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Ciftçioglu N, Björklund M, Kuorikoski K,
Bergström K and Kajander EO: Nanobacteria: An infectious cause for
kidney stone formation. Kidney Int. 56:1893–1898. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Khullar M, Sharma SK, Singh SK, Bajwa P,
Shiekh FA, Relan V and Sharma M: Morphological and immunological
characteristics of nanobacteria from human renal stones of a north
Indian population. Urol Res. 32:190–195. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Shiekh FA, Khullar M and Singh SK:
Lithogenesis: Induction of renal calcifications by nanobacteria.
Urol Res. 34:53–57. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Kajander EO and Ciftçioglu N:
Nanobacteria: An alternative mechanism for pathogenic intra- and
extracellular calcification and stone formation. Proc Natl Acad Sci
USA. 95:8274–8279. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Abrol N, Panda A, Kekre NS and Devasia A:
Nanobacteria in the pathogenesis of urolithiasis: Myth or reality?
Indian J Urol. 31:3–7. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Hong X, Wang X, Wang T, Yu C and Li H:
Role of nanobacteria in the pathogenesis of kidney stone formation.
Am J Transl Res. 8:3227–3234. 2016.PubMed/NCBI
|
|
98
|
Sadaf H, Raza SI and Hassan SW: Role of
gut microbiota against calcium oxalate. Microb Pathog. 109:287–291.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Ticinesi A, Nouvenne A, Chiussi G,
Castaldo G, Guerra A and Meschi T: Calcium oxalate nephrolithiasis
and gut microbiota: Not just a gut-kidney axis. A nutritional
perspective. Nutrients. 12:5482020. View Article : Google Scholar :
|
|
100
|
Ticinesi A, Milani C, Guerra A, Allegri F,
Lauretani F, Nouvenne A, Mancabelli L, Lugli GA, Turroni F, Duranti
S, et al: Understanding the gut-kidney axis in nephrolithiasis: An
analysis of the gut microbiota composition and functionality of
stone formers. Gut. 67:2097–2106. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Stern JM, Moazami S, Qiu Y, Kurland I,
Chen Z, Agalliu I, Burk R and Davies KP: Evidence for a distinct
gut microbiome in kidney stone formers compared to non-stone
formers. Urolithiasis. 44:399–407. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Falony G: Beyond Oxalobacter: The gut
microbiota and kidney stone formation. Gut. 67:2078–2079. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Miller AW and Dearing D: The metabolic and
ecological interactions of oxalate-degrading bacteria in the
Mammalian gut. Pathogens. 2:636–652. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Worcester EM, Fellner SK, Nakagawa Y and
Coe FL: Effect of renal transplantation on serum oxalate and
urinary oxalate excretion. Nephron. 67:414–418. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Hatch M, Freel RW and Vaziri ND:
Mechanisms of oxalate absorption and secretion across the rabbit
distal colon. Pflugers Arch. 426:101–109. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Peck AB, Canales BK and Nguyen CQ:
Oxalate-degrading microorganisms or oxalate-degrading enzymes:
Which is the future therapy for enzymatic dissolution of
calcium-oxalate uroliths in recurrent stone disease? Urolithiasis.
44:45–50. 2016. View Article : Google Scholar
|
|
107
|
Knight J, Deora R, Assimos DG and Holmes
RP: The genetic composition of Oxalobacter formigenes and its
relationship to colonization and calcium oxalate stone disease.
Urolithiasis. 41:187–196. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Batagello CA, Monga M and Miller AW:
Calcium oxalate urolithiasis: A case of missing microbes? J
Endourol. 32:995–1005. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Cornelius JG and Peck AB: Colonization of
the neonatal rat intestinal tract from environmental exposure to
the anaerobic bacterium Oxalobacter formigenes. J Med Microbiol.
53:249–254. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Nikolic-Paterson DJ, Wang S and Lan HY:
Macrophages promote renal fibrosis through direct and indirect
mechanisms. Kidney Int Suppl (2011). 4:34–38. 2014. View Article : Google Scholar
|
|
111
|
Okada A, Yasui T, Fujii Y, Niimi K,
Hamamoto S, Hirose M, Kojima Y, Itoh Y, Tozawa K, Hayashi Y and
Kohri K: Renal macrophage migration and crystal phagocytosis via
inflammatory-related gene expression during kidney stone formation
and elimination in mice: Detection by association analysis of
stone-related gene expression and microstructural observation. J
Bone Miner Res. 25:2701–2711. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Singhto N, Kanlaya R, Nilnumkhum A and
Thongboonkerd V: Roles of macrophage exosomes in immune response to
calcium oxalate monohydrate crystals. Front Immunol. 9:3162018.
View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Singhto N and Thongboonkerd V: Exosomes
derived from calcium oxalate-exposed macrophages enhance IL-8
production from renal cells, neutrophil migration and crystal
invasion through extracellular matrix. J Proteomics. 185:64–76.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Tamura M, Aizawa R, Hori M and Ozaki H:
Progressive renal dysfunction and macrophage infiltration in
interstitial fibrosis in an adenine-induced tubulointerstitial
nephritis mouse model. Histochem Cell Biol. 131:483–490. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Kusmartsev S, Dominguez-Gutierrez PR,
Canales BK, Bird VG, Vieweg J and Khan SR: Calcium oxalate stone
fragment and crystal phagocytosis by human macrophages. J Urol.
195:1143–1151. 2016. View Article : Google Scholar :
|
|
116
|
Sintiprungrat K, Singhto N and
Thongboonkerd V: Characterization of calcium oxalate
crystal-induced changes in the secretome of U937 human monocytes.
Mol Biosyst. 12:879–889. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Histiocytosis syndromes in children.
Writing Group of the Histiocyte Society. Lancet. 1:208–209.
1987.PubMed/NCBI
|
|
118
|
Okada A, Yasui T, Hamamoto S, Hirose M,
Kubota Y, Itoh Y, Tozawa K, Hayashi Y and Kohri K: Genome-wide
analysis of genes related to kidney stone formation and elimination
in the calcium oxalate nephrolithiasis model mouse: Detection of
stone-preventive factors and involvement of macrophage activity. J
Bone Miner Res. 24:908–924. 2009. View Article : Google Scholar
|
|
119
|
Vervaet BA, Verhulst A, Dauwe SE, De Broe
ME and D'Haese PC: An active renal crystal clearance mechanism in
rat and man. Kidney Int. 75:41–51. 2009. View Article : Google Scholar
|
|
120
|
Dominguez-Gutierrez PR, Kusmartsev S,
Canales BK and Khan SR: Calcium oxalate differentiates human
monocytes into inflammatory M1 macrophages. Front Immunol.
9:18632018. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Taguchi K, Okada A, Hamamoto S, Unno R,
Moritoki Y, Ando R, Mizuno K, Tozawa K, Kohri K and Yasui T:
M1/M2-macrophage phenotypes regulate renal calcium oxalate crystal
development. Sci Rep. 6:351672016. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Dominguez-Gutierrez PR, Kwenda EP, Khan SR
and Canales BK: Immunotherapy for stone disease. Curr Opin Urol.
30:183–189. 2020. View Article : Google Scholar : PubMed/NCBI
|