|
1
|
Shibanuma M, Mashimo J, Kuroki T and Nose
K: Characterization of the TGF beta 1-inducible hic-5 gene that
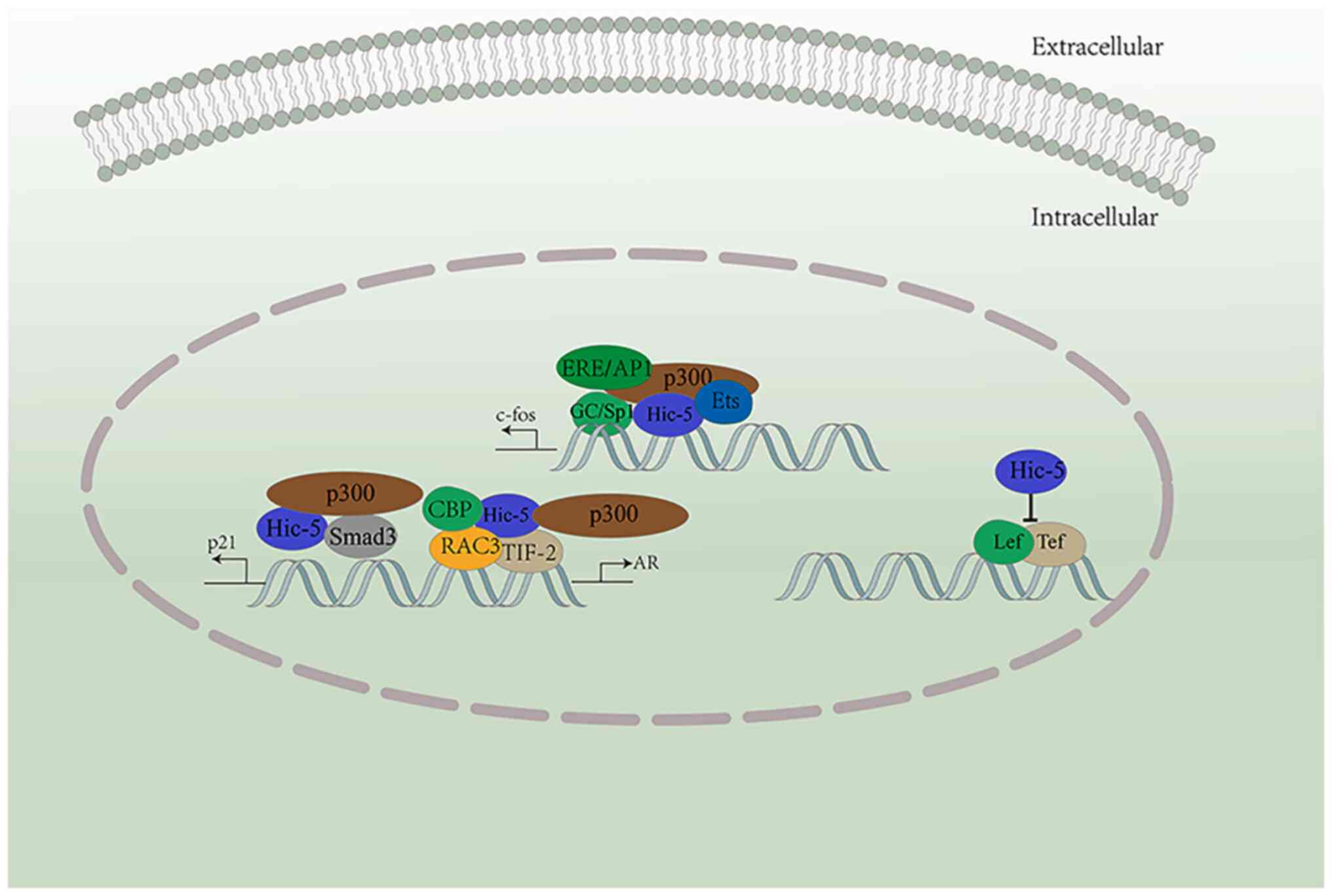
encodes a putative novel zinc finger protein and its possible
involvement in cellular senescence. J Biol Chem. 269:26767–26774.
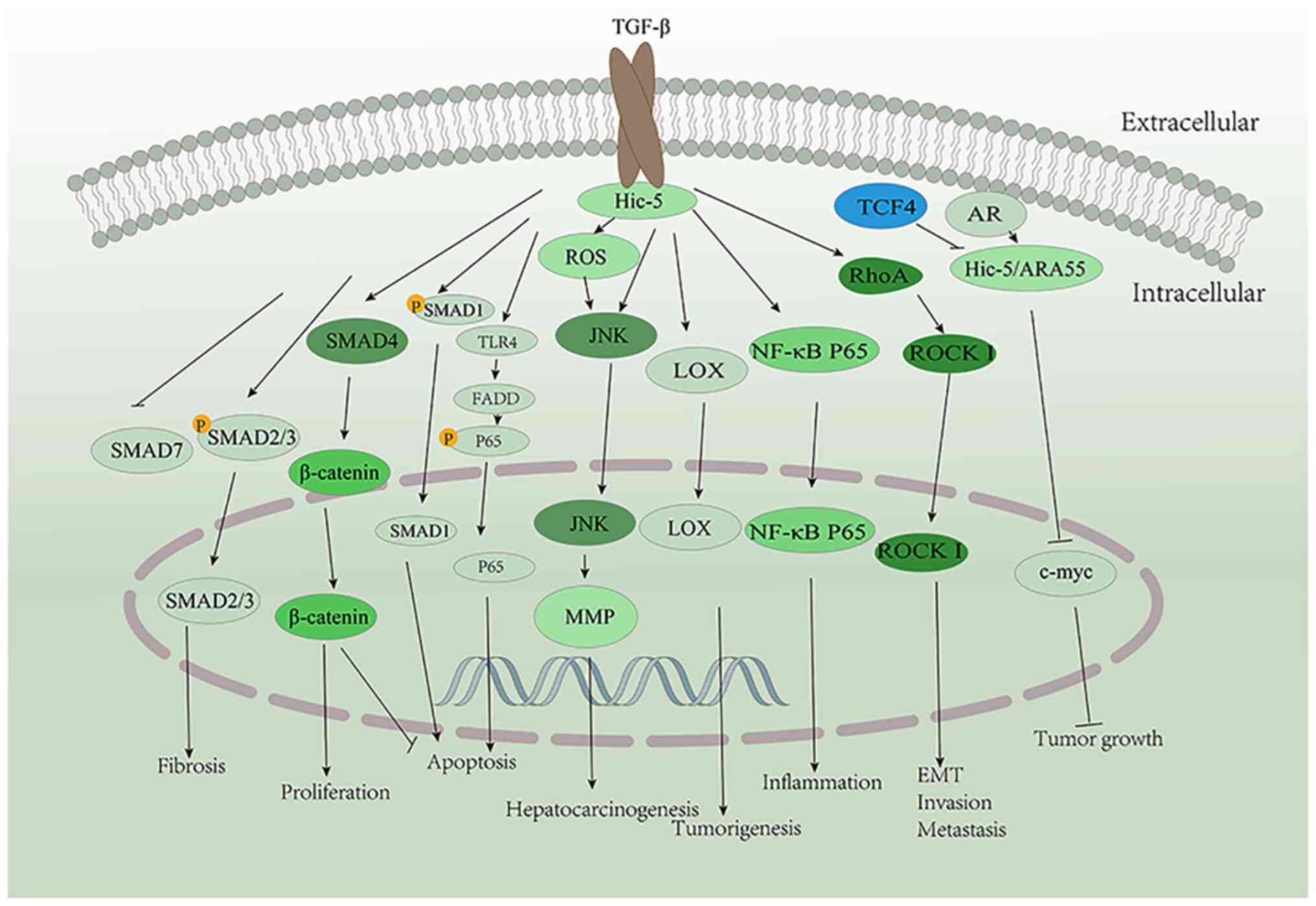
1994. View Article : Google Scholar : PubMed/NCBI
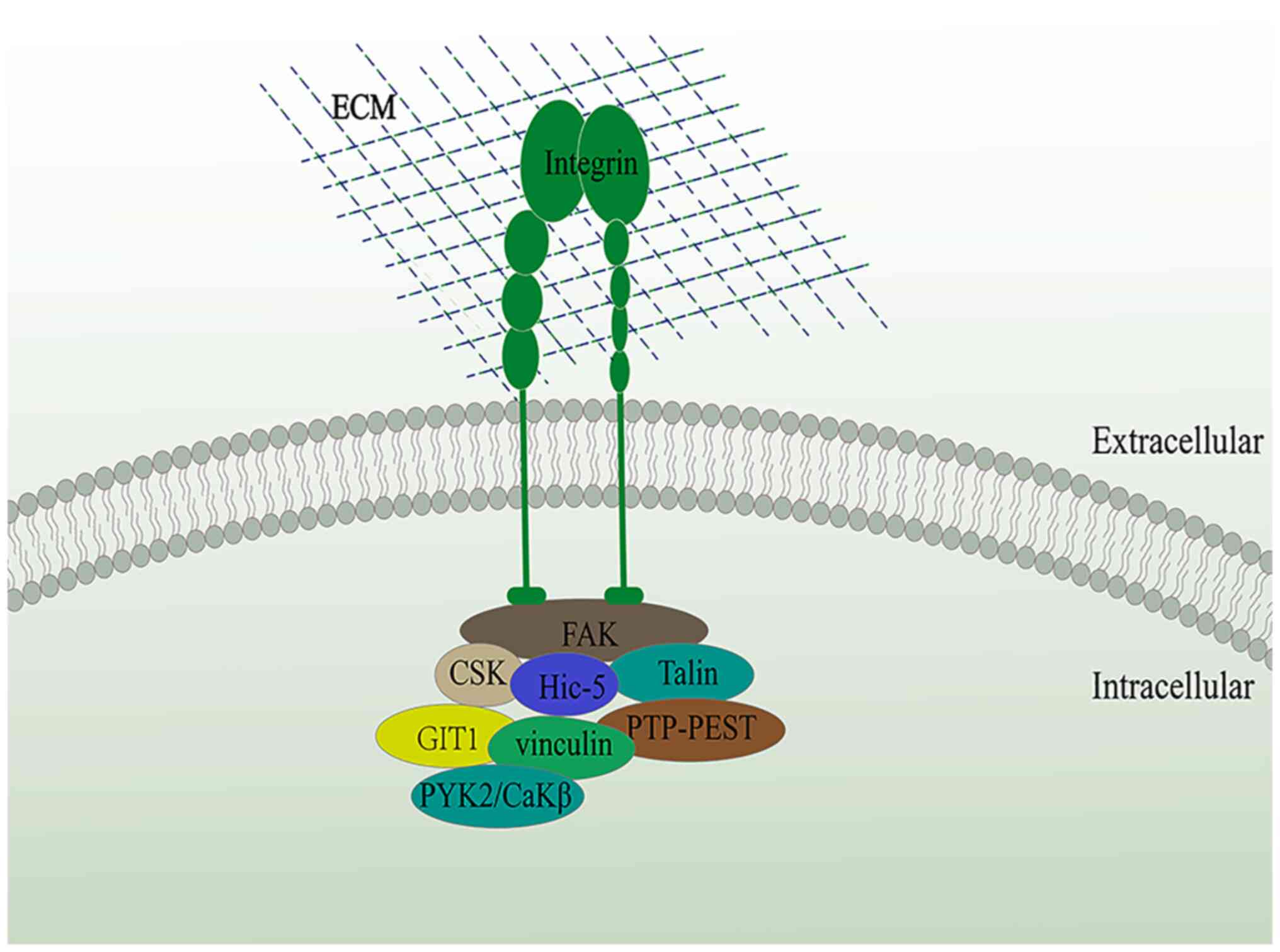
|
|
2
|
Shibanuma M, Mori K and Nose K: HIC-5: A
mobile molecular scaffold regulating the anchorage dependence of
cell growth. Int J Cell Biol. 2012:4261382012. View Article : Google Scholar
|
|
3
|
Kim-Kaneyama JR, Lei XF, Arita S, Miyauchi
A, Miyazaki T and Miyazaki A: Hydrogen peroxide-inducible clone 5
(Hic-5) as a potential therapeutic target for vascular and other
disorders. J Atheroscler Thromb. 19:601–607. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Yang L, Guerrero J, Hong H, DeFranco DB
and Stallcup MR: Interaction of the tau2 transcriptional activation
domain of glucocorticoid receptor with a novel steroid receptor
coactivator, Hic-5, which localizes to both focal adhesions and the
nuclear matrix. Mol Biol Cell. 11:2007–2018. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kim-Kaneyama JR, Shibanuma M and Nose K:
Transcriptional activation of the c-fos gene by a LIM protein,
Hic-5. Biochem Biophys Res Commun. 299:360–365. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Shibanuma M, Kim-Kaneyama JR, Sato S and
Nose K: A LIM protein, Hic-5, functions as a potential coactivator
for Sp1. J Cell Biochem. 91:633–645. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Lei XF, Fu W, Kim-Kaneyama JR, Omoto T,
Miyazaki T, Li B and Miyazaki A: Hic-5 deficiency attenuates the
activation of hepatic stellate cells and liver fibrosis through
upregulation of Smad7 in mice. J Hepatol. 64:110–117. 2016.
View Article : Google Scholar
|
|
8
|
Matsuya M, Sasaki H, Aoto H, Mitaka T,
Nagura K, Ohba T, Ishino M, Takahashi S, Suzuki R and Sasaki T:
Cell adhesion kinase beta forms a complex with a new member, Hic-5,
of proteins localized at focal adhesions. J Biol Chem.
273:1003–1014. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Nishiya N, Shirai T, Suzuki W and Nose K:
Hic-5 interacts with GIT1 with a different binding mode from
paxillin. J Biochem. 132:279–289. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Fujita H, Kamiguchi K, Cho D, Shibanuma M,
Morimoto C and Tachibana K: Interaction of Hic-5, A
senescence-related protein, with focal adhesion kinase. J Biol
Chem. 273:26516–26521. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Hornigold N, Craven RA, Keen JN, Johnson
T, Banks RE and Mooney AF: Upregulation of Hic-5 in
glomerulosclerosis and its regulation of mesangial cell apoptosis.
Kidney Int. 77:329–338. 2010. View Article : Google Scholar
|
|
12
|
Mestayer C, Blanchère M, Jaubert F, Dufour
B and Mowszowicz I: Expression of androgen receptor coactivators in
normal and cancer prostate tissues and cultured cell lines.
Prostate. 56:192–200. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kim-Kaneyama JR, Takeda N, Sasai A,
Miyazaki A, Sata M, Hirabayashi T, Shibanuma M, Yamada G and Nose
K: Hic-5 deficiency enhances mechanosensitive apoptosis and
modulates vascular remodeling. J Mol Cell Cardiol. 50:77–86. 2011.
View Article : Google Scholar
|
|
14
|
Nishiya N, Iwabuchi Y, Shibanuma M, Côté
JF, Tremblay ML and Nose K: Hic-5, a paxillin homologue, binds to
the protein-tyrosine phosphatase PEST (PTP-PEST) through its LIM 3
domain. J Biol Chem. 274:9847–9853. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
López-Colomé AM, Lee-Rivera I,
Benavides-Hidalgo R and López E: Paxillin: A crossroad in
pathological cell migration. J Hematol Oncol. 10:502017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ma X and Hammes SR: Paxillin actions in
the nucleus. Steroids. 133:87–92. 2018. View Article : Google Scholar :
|
|
17
|
Xu W, Alpha KM, Zehrbach NM and Turner CE:
Paxillin promotes breast tumor collective cell invasion through
maintenance of adherens junction integrity. Mol Biol Cell.
33:ar142022. View Article : Google Scholar :
|
|
18
|
Tanaka N, Minemura C, Asai S, Kikkawa N,
Kinoshita T, Oshima S, Koma A, Kasamatsu A, Hanazawa T, Uzawa K and
Seki N: Identification of miR-199-5p and miR-199-3p target genes:
Paxillin facilities cancer cell aggressiveness in head and neck
squamous cell carcinoma. Genes (Basel). 12:19102021. View Article : Google Scholar
|
|
19
|
Ripamonti M, Wehrle-Haller B and de Curtis
I: Paxillin: A hub for mechano-transduction from the β3
integrin-talin-kindlin axis. Front Cell Dev Biol. 10:8520162022.
View Article : Google Scholar
|
|
20
|
Hagel M, George EL, Kim A, Tamimi R, Opitz
SL, Turner CE, Imamoto A and Thomas SM: The adaptor protein
paxillin is essential for normal development in the mouse and is a
critical transducer of fibronectin signaling. Mol Cell Biol.
22:901–915. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kim-Kaneyama JR, Suzuki W, Ichikawa K,
Ohki T, Kohno Y, Sata M, Nose K and Shibanuma M: Uni-axial
stretching regulates intracellular localization of Hic-5 expressed
in smooth-muscle cells in vivo. J Cell Sci. 118:937–949. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Mashimo J, Shibanuma M, Satoh H, Chida K
and Nose K: Genomic structure and chromosomal mapping of the mouse
hic-5 gene that encodes a focal adhesion protein. Gene. 249:99–103.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Panetti TS, Hannah DF, Avraamides C,
Gaughan JP, Marcinkiewicz C, Huttenlocher A and Mosher DF:
Extracellular matrix molecules regulate endothelial cell migration
stimulated by lysophosphatidic acid. J Thromb Haemost. 2:1645–1656.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Hetey SE, Lalonde DP and Turner CE:
Tyrosine-phosphorylated Hic-5 inhibits epidermal growth
factor-induced lamellipodia formation. Exp Cell Res. 311:147–156.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Tumbarello DA, Brown MC and Turner CE: The
paxillin LD motifs. FEBS Lett. 513:114–118. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Brown MC and Turner CE: Paxillin: Adapting
to change. Physiol Rev. 84:1315–1339. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Nishiya N, Tachibana K, Shibanuma M,
Mashimo JI and Nose K: Hic-5-reduced cell spreading on fibronectin:
Competitive effects between paxillin and Hic-5 through interaction
with focal adhesion kinase. Mol Cell Biol. 21:5332–5345. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Shibanuma M, Kim-Kaneyama JR, Ishino K,
Sakamoto N, Hishiki T, Yamaguchi K, Mori K, Mashimo J and Nose K:
Hic-5 communicates between focal adhesions and the nucleus through
oxidant-sensitive nuclear export signal. Mol Biol Cell.
14:1158–1171. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Heitzer MD and DeFranco DB: Hic-5, an
adaptor-like nuclear receptor coactivator. Nucl Recept Signal.
4:e0192006. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Chodankar R, Wu DY, Schiller BJ, Yamamoto
KR and Stallcup MR: Hic-5 is a transcription coregulator that acts
before and/or after glucocorticoid receptor genome occupancy in a
gene-selective manner. Proc Natl Acad Sci USA. 111:4007–4012. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Heitzer MD and DeFranco DB: Hic-5/ARA55, a
LIM domain-containing nuclear receptor coactivator expressed in
prostate stromal cells. Cancer Res. 66:7326–7333. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Ghogomu SM, van Venrooy S, Ritthaler M,
Wedlich D and Gradl D: HIC-5 is a novel repressor of lymphoid
enhancer factor/T-cell factor-driven transcription. J Biol Chem.
281:1755–1764. 2006. View Article : Google Scholar
|
|
33
|
Drori S, Girnun GD, Tou L, Szwaya JD,
Mueller E, Xia K, Shivdasani RA and Spiegelman BM: Hic-5 regulates
an epithelial program mediated by PPARgamma. Genes Dev. 19:362–375.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Heitzer MD and DeFranco DB: Mechanism of
action of Hic-5/androgen receptor activator 55, a LIM
domain-containing nuclear receptor coactivator. Mol Endocrinol.
20:56–64. 2006. View Article : Google Scholar
|
|
35
|
Deakin NO and Turner CE: Distinct roles
for paxillin and Hic-5 in regulating breast cancer cell morphology,
invasion, and metastasis. Mol Biol Cell. 22:327–341. 2011.
View Article : Google Scholar :
|
|
36
|
Vohnoutka RB, Gulvady AC, Goreczny G,
Alpha K, Handelman SK, Sexton JZ and Turner CE: The focal adhesion
scaffold protein Hic-5 regulates vimentin organization in
fibroblasts. Mol Biol Cell. 30:3037–3056. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Paul J, Singh AK, Kathania M, Elviche TL,
Zeng M, Basrur V, Theiss AL and Venuprasad K: IL-17-driven
intestinal fibrosis is inhibited by Itch-mediated ubiquitination of
HIC-5. Mucosal Immunol. 11:427–436. 2018. View Article : Google Scholar
|
|
38
|
Lei XF, Kim-Kaneyama JR, Arita-Okubo S,
Offermanns S, Itabe H, Miyazaki T and Miyazaki A: Identification of
Hic-5 as a novel scaffold for the MKK4/p54 JNK pathway in the
development of abdominal aortic aneurysms. J Am Heart Assoc.
3:e0007472014. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Frangogiannis N: Transforming growth
factor-β in tissue fibrosis. J Exp Med. 217:e201901032020.
View Article : Google Scholar
|
|
40
|
Peng D, Fu M, Wang M, Wei Y and Wei X:
Targeting TGF-β signal transduction for fibrosis and cancer
therapy. Mol Cancer. 21:1042022. View Article : Google Scholar
|
|
41
|
Gao L, Lei XF, Miyauchi A, Noguchi M,
Omoto T, Haraguchi S, Miyazaki T, Miyazaki A and Kim-Kaneyama JR:
Hic-5 is required for activation of pancreatic stellate cells and
development of pancreatic fibrosis in chronic pancreatitis. Sci
Rep. 10:191052020. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Shola DT, Wang H, Wahdan-Alaswad R and
Danielpour D: Hic-5 controls BMP4 responses in prostate cancer
cells through inter-acting with Smads 1,5 and 8. Oncogene.
31:2480–2490. 2012. View Article : Google Scholar
|
|
43
|
Sha L, Ma D and Chen C: Exosome-mediated
Hic-5 regulates proliferation and apoptosis of osteosarcoma via
Wnt/β-catenin signal pathway. Aging (Albany NY). 12:23598–23608.
2020. View Article : Google Scholar
|
|
44
|
Chen H, Tan P, Qian B, Du Y, Wang A, Shi
H, Huang Z, Huang S, Liang T and Fu W: Hic-5 deficiency protects
cerulein-induced chronic pancreatitis via down-regulation of the
NF-κB (p65)/IL-6 signalling pathway. J Cell Mol Med. 24:1488–1503.
2020. View Article : Google Scholar
|
|
45
|
Gao L, Qian B, Chen H, Wang A, Li Q, Li J,
Tan P, Xia X, Du Y and Fu W: Hic-5 deficiency attenuates hepatic
ischemia reperfusion injury through TLR4/NF-κB signaling pathways.
Life Sci. 249:1175172020. View Article : Google Scholar
|
|
46
|
Wu JR, Hu CT, You RI, Pan SM, Cheng CC,
Lee MC, Wu CC, Chang YJ, Lin SC, Chen CS, et al: Hydrogen peroxide
inducible clone-5 mediates reactive oxygen species signaling for
hepatocellular carcinoma progression. Oncotarget. 6:32526–32544.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Tumbarello DA and Turner CE: Hic-5
contributes to epithelial-mesenchymal transformation through a
RhoA/ROCK-dependent pathway. J Cell Physiol. 211:736–747. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Sheta R, Wang ZQ, Bachvarova M, Plante M,
Gregoire J, Renaud MC, Sebastianelli A, Gobeil S, Morin C,
Macdonald E, et al: Hic-5 regulates epithelial to mesenchymal
transition in ovarian cancer cells in a TGFβ1-independent manner.
Oncotarget. 8:82506–82530. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Yuminamochi T, Yatomi Y, Osada M, Ohmori
T, Ishii Y, Nakazawa K, Hosogaya S and Ozaki Y: Expression of the
LIM proteins paxillin and Hic-5 in human tissues. J Histochem
Cytochem. 51:513–521. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Komorowsky C, Samarin J, Rehm M, Guidolin
D and Goppelt-Struebe M: Hic-5 as a regulator of endothelial cell
morphology and connective tissue growth factor gene expression. J
Mol Med (Berl). 88:623–631. 2010. View Article : Google Scholar
|
|
51
|
Dave JM, Abbey CA, Duran CL, Seo H,
Johnson GA and Bayless KJ: Hic-5 mediates the initiation of
endothelial sprouting by regulating a key surface
metalloproteinase. J Cell Sci. 129:743–756. 2016.PubMed/NCBI
|
|
52
|
Kim-Kaneyama JR, Miyauchi A, Lei XF, Arita
S, Mino T, Takeda N, Kou K, Eto K, Yoshida T, Miyazaki T, et al:
Identification of Hic-5 as a novel regulatory factor for integrin
αIIbβ3 activation and platelet aggregation in mice. J Thromb
Haemost. 10:1867–1874. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Popp M, Thielmann I, Nieswandt B and
Stegner D: Normal platelet integrin function in mice lacking
hydrogen peroxide-induced clone-5 (Hic-5). PLoS One.
10:e01334292015. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Gao J, Huang M, Lai J, Mao K, Sun P, Cao
Z, Hu Y, Zhang Y, Schulte ML, Jin C, et al: Kindlin supports
platelet integrin αIIbβ3 activation by interacting with paxillin. J
Cell Sci. 130:3764–3775. 2017.PubMed/NCBI
|
|
55
|
Kim-Kaneyama JR, Wachi N, Sata M, Enomoto
S, Fukabori K, Koh K, Shibanuma M and Nose K: Hic-5, an adaptor
protein expressed in vascular smooth muscle cells, modulates the
arterial response to injury in vivo. Biochem Biophys Res Commun.
376:682–687. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Vergallo R and Crea F: Atherosclerotic
plaque healing. N Engl J Med. 383:846–857. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Almeida SO and Budoff M: Effect of statins
on atherosclerotic plaque. Trends Cardiovasc Med. 29:451–455. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Arita-Okubo S, Kim-Kaneyama JR, Lei XF, Fu
WG, Ohnishi K, Takeya M, Miyauchi A, Honda H, Itabe H, Miyazaki T
and Miyazaki A: Role of Hic-5 in the formation of microvilli-like
structures and the monocyte-endothelial interaction that
accelerates atherosclerosis. Cardiovasc Res. 105:361–371. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Yund EE, Hill JA and Keller RS: Hic-5 is
required for fetal gene expression and cytoskeletal organization of
neonatal cardiac myocytes. J Mol Cell Cardiol. 47:520–527. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Ji J, Yu F, Ji Q, Li Z, Wang K, Zhang J,
Lu J, Chen L, E Q, Zeng Y and Ji Y: Comparative proteomic analysis
of rat hepatic stellate cell activation: A comprehensive view and
suppressed immune response. Hepatology. 56:332–349. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Vege SS and Chari ST: Chronic
pancreatitis. N Engl J Med. 386:869–878. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Jamba A, Kondo S, Urushihara M, Nagai T,
Kim-Kaneyama JR, Miyazaki A and Kagami S: Hydrogen
peroxide-inducible clone-5 regulates mesangial cell proliferation
in proliferative glomerulonephritis in mice. PLoS One.
10:e01227732015. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Hornigold N and Mooney A: Extracellular
matrix-induced Hic-5 expression in glomerular mesangial cells leads
to a prosclerotic phenotype independent of TGF-β. FASEB J.
29:4956–4967. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Li X, Martinez-Ferrer M, Botta V,
Uwamariya C, Banerjee J and Bhowmick NA: Epithelial Hic-5/ARA55
expression contributes to prostate tumorigenesis and castrate
responsiveness. Oncogene. 30:167–177. 2011. View Article : Google Scholar :
|
|
65
|
Cárdenas S, Colombero C, Panelo L,
Dakarapu R, Falck JR, Costas MA and Nowicki S: GPR75 receptor
mediates 20-HETE-signaling and metastatic features of
androgen-insensitive prostate cancer cells. Biochim Biophys Acta
Mol Cell Biol Lipids. 1865:1585732020. View Article : Google Scholar :
|
|
66
|
Lee BH and Stallcup MR: Different
chromatin and DNA sequence characteristics define glucocorticoid
receptor binding sites that are blocked or not blocked by
coregulator Hic-5. PLoS One. 13:e01969652018. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Leach DA, Need EF, Trotta AP, Grubisha MJ,
DeFranco DB and Buchanan G: Hic-5 influences genomic and
non-genomic actions of the androgen receptor in prostate
myofibroblasts. Mol Cell Endocrinol. 384:185–199. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Li P, Yu X, Ge K, Melamed J, Roeder RG and
Wang Z: Heterogeneous expression and functions of androgen receptor
co-factors in primary prostate cancer. Am J Pathol. 161:1467–1474.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Solomon JD, Heitzer MD, Liu TT, Beumer JH,
Parise RA, Normolle DP, Leach DA, Buchanan G and DeFranco DB: VDR
activity is differentially affected by Hic-5 in prostate cancer and
stromal cells. Mol Cancer Res. 12:1166–1180. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Mao X, Xu J, Wang W, Liang C, Hua J, Liu
J, Zhang B, Meng C, Yu X and Shi S: Crosstalk between
cancer-associated fibroblasts and immune cells in the tumor
microenvironment: New findings and future perspectives. Mol Cancer.
20:1312021. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Gulvady AC, Dubois F, Deakin NO, Goreczny
GJ and Turner CE: Hic-5 expression is a major indicator of cancer
cell morphology, migration, and plasticity in three-dimensional
matrices. Mol Biol Cell. 29:1704–1717. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Shen T and Guo Q: Role of Pyk2 in human
cancers. Med Sci Monit. 24:8172–8182. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Sun CK, Ng KT, Lim ZX, Cheng Q, Lo CM,
Poon RT, Man K, Wong N and Fan ST: Proline-rich tyrosine kinase 2
(Pyk2) promotes cell motility of hepatocellular carcinoma through
induction of epithelial to mesenchymal transition. PLoS One.
6:e188782011. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Qian B, Wei L, Yang Z, He Q, Chen H, Wang
A, Yang D, Li Q, Li J, Zheng S and Fu W: Hic-5 in pancreatic
stellate cells affects proliferation, apoptosis, migration,
invasion of pancreatic cancer cells and postoperative survival time
of pancreatic cancer. Biomed Pharmacother. 121:1093552020.
View Article : Google Scholar
|
|
75
|
Hanahan D: Hallmarks of cancer: New
dimensions. Cancer Discov. 12:31–46. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Biffi G and Tuveson DA: Diversity and
biology of cancer-associated fibroblasts. Physiol Rev. 101:147–176.
2021. View Article : Google Scholar :
|
|
77
|
Sun X, He X, Zhang Y, Hosaka K, Andersson
P, Wu J, Wu J, Jing X, Du Q, Hui X, et al: Inflammatory
cell-derived CXCL3 promotes pancreatic cancer metastasis through a
novel myofibroblast-hijacked cancer escape mechanism. Gut.
71:129–147. 2022. View Article : Google Scholar
|
|
78
|
Zhang M, Liu ZZ, Aoshima K, Cai WL, Sun H,
Xu T, Zhang Y, An Y, Chen JF, Chan LH, et al: CECR2 drives breast
cancer metastasis by promoting NF-κB signaling and
macrophage-mediated immune suppression. Sci Transl Med.
14:eabf54732022. View Article : Google Scholar
|
|
79
|
Du X, Xu Q, Pan D, Xu D, Niu B, Hong W,
Zhang R, Li X and Chen S: HIC-5 in cancer-associated fibroblasts
contributes to esophageal squamous cell carcinoma progression. Cell
Death Dis. 10:8732019. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Hernandez-Quiles M, Broekema MF and
Kalkhoven E: PPARgamma in metabolism, immunity, and cancer: Unified
and diverse mechanisms of action. Front Endocrinol (Lausanne).
12:6241122021. View Article : Google Scholar
|
|
81
|
Omoto T, Kim-Kaneyama JR, Lei XF, Orimo A,
Ohnishi K, Yoshihara K, Miyauchi A, Li S, Gao L, Umemoto T, et al:
The impact of stromal Hic-5 on the tumorigenesis of colorectal
cancer through lysyl oxidase induction and stromal remodeling.
Oncogene. 37:1205–1219. 2018. View Article : Google Scholar
|
|
82
|
Goreczny GJ, Ouderkirk-Pecone JL, Olson
EC, Krendel M and Turner CE: Hic-5 remodeling of the stromal matrix
promotes breast tumor progression. Oncogene. 36:2693–2703. 2017.
View Article : Google Scholar :
|
|
83
|
Goreczny GJ, Forsythe IJ and Turner CE:
Hic-5 regulates fibrillar adhesion formation to control tumor
extracellular matrix remodeling through interaction with tensin1.
Oncogene. 37:1699–1713. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Noguchi F, Inui S, Nakajima T and Itami S:
Hic-5 affects proliferation, migration and invasion of B16 murine
melanoma cells. Pigment Cell Melanoma Res. 25:773–782. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Caltagarone J, Hamilton RL, Murdoch G,
Jing Z, DeFranco DB and Bowser R: Paxillin and hydrogen
peroxide-inducible clone 5 expression and distribution in control
and Alzheimer disease hippocampi. J Neuropathol Exp Neurol.
69:356–371. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Miyauchi A, Kim-Kaneyama JR, Lei XF, Chang
SH, Saito T, Haraguchi S, Miyazaki T and Miyazaki A: Alleviation of
murine osteoarthritis by deletion of the focal adhesion
mechanosensitive adapter, Hic-5. Sci Rep. 9:157702019. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Inui S, Fukuzato Y, Nakajima T, Kurata S
and Itami S: Androgen receptor co-activator Hic-5/ARA55 as a
molecular regulator of androgen sensitivity in dermal papilla cells
of human hair follicles. J Invest Dermatol. 127:2302–2306. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Dabiri G, Tumbarello DA, Turner CE and Van
de Water L: Hic-5 promotes the hypertrophic scar myofibroblast
phenotype by regulating the TGF-beta1 autocrine loop. J Invest
Dermatol. 128:2518–2525. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Inui S, Shono F, Noguchi F, Nakajima T,
Hosokawa K and Itami S: In vitro and in vivo evidence of pathogenic
roles of Hic-5/ARA55 in keloids through Smad pathway and
profibrotic transcription. J Dermatol Sci. 58:152–154. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Piera-Velazquez S, Fertala J,
Huaman-Vargas G, Louneva N and Jiménez SA: Increased expression of
the transforming growth factor β-inducible gene HIC-5 in systemic
sclerosis skin and fibroblasts: A novel antifibrotic therapeutic
target. Rheumatology (Oxford). 59:3092–3098. 2020. View Article : Google Scholar
|
|
91
|
Reina-Torres E, De Ieso ML, Pasquale LR,
Madekurozwa M, van Batenburg-Sherwood J, Overby DR and Stamer WD:
The vital role for nitric oxide in intraocular pressure
homeostasis. Prog Retin Eye Res. 83:1009222021. View Article : Google Scholar :
|
|
92
|
Nair KS, Srivastava C, Brown RV, Koli S,
Choquet H, Kang HS, Kuo YM, Grimm SA, Sutherland C, Badea A, et al:
GLIS1 regulates trabecular meshwork function and intraocular
pressure and is associated with glaucoma in humans. Nat Commun.
12:48772021. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Pattabiraman PP and Rao PV: Hic-5
regulates actin cytoskeletal reorganization and expression of
fibrogenic markers and myocilin in trabecular meshwork cells.
Invest Ophthalmol Vis Sci. 56:5656–5669. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
You Q, Duan L, Wang F, Du X and Xiao M:
Characterization of the inhibition of vein graft intimal
hyperplasia by a biodegradable vascular stent. Cell Biochem
Biophys. 59:99–107. 2011. View Article : Google Scholar
|
|
95
|
Low EL, Baker AH and Bradshaw AC: TGFβ,
smooth muscle cells and coronary artery disease: A review. Cell
Signal. 53:90–101. 2019. View Article : Google Scholar :
|
|
96
|
Bai H, Lee JS, Hu H, Wang T, Isaji T, Liu
S, Guo J, Liu H, Wolf K, Ono S, et al: Transforming growth
factor-β1 inhibits pseudoaneurysm formation after aortic patch
angioplasty. Arterioscler Thromb Vasc Biol. 38:195–205. 2018.
View Article : Google Scholar
|
|
97
|
Goumans MJ and Ten Dijke P: TGF-β
signaling in control of cardiovascular function. Cold Spring Harb
Perspect Biol. 10:a0222102018. View Article : Google Scholar
|
|
98
|
Boers W, Aarrass S, Linthorst C, Pinzani
M, Elferink RO and Bosma P: Transcriptional profiling reveals novel
markers of liver fibrogenesis: Gremlin and insulin-like growth
factor-binding proteins. J Biol Chem. 281:16289–16295. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Gough NR, Xiang X and Mishra L: TGF-β
signaling in liver, pancreas, and gastrointestinal diseases and
cancer. Gastroenterology. 161:434–452.e15. 2021. View Article : Google Scholar
|
|
100
|
Nogueira MA, Coelho AM, Sampietre SN,
Patzina RA, Pinheiro da Silva F, D'Albuquerque LA and Machado MC:
Beneficial effects of adenosine triphosphate-sensitive K+ channel
opener on liver ischemia/reperfusion injury. World J Gastroenterol.
20:15319–15326. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Ma C, Kesarwala AH, Eggert T,
Medina-Echeverz J, Kleiner DE, Jin P, Stroncek DF, Terabe M, Kapoor
V, ElGindi M, et al: NAFLD causes selective CD4(+) T lymphocyte
loss and promotes hepatocarcinogenesis. Nature. 531:253–257. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Shen Y, Wei Y, Wang Z, Jing Y, He H, Yuan
J, Li R, Zhao Q, Wei L, Yang T and Lu J: TGF-β regulates
hepatocellular carcinoma progression by inducing Treg cell
polarization. Cell Physiol Biochem. 35:1623–1632. 2015. View Article : Google Scholar
|
|
103
|
Caja L, Dituri F, Mancarella S,
Caballero-Diaz D, Moustakas A, Giannelli G and Fabregat I: TGF-β
and the tissue microenvironment: Relevance in fibrosis and cancer.
Int J Mol Sci. 19:12942018. View Article : Google Scholar
|
|
104
|
Bansod S, Doijad N and Godugu C: Berberine
attenuates severity of chronic pancreatitis and fibrosis via
AMPK-mediated inhibition of TGF-β1/Smad signaling and M2
polarization. Toxicol Appl Pharmacol. 403:1151622020. View Article : Google Scholar
|
|
105
|
Gore J, Imasuen-Williams IE, Conteh AM,
Craven KE, Cheng M and Korc M: Combined targeting of TGF-β, EGFR
and HER2 suppresses lymphangiogenesis and metastasis in a
pancreatic cancer model. Cancer Lett. 379:143–153. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Song W, Dai WJ, Zhang MH, Wang H and Yang
XZ: Comprehensive analysis of the expression of TGF-β signaling
regulators and prognosis in human esophageal cancer. Comput Math
Methods Med. 2021:18122272021. View Article : Google Scholar
|
|
107
|
Calon A, Lonardo E, Berenguer-Llergo A,
Espinet E, Hernando-Momblona X, Iglesias M, Sevillano M,
Palomo-Ponce S, Tauriello DV, Byrom D, et al: Stromal gene
expression defines poor-prognosis subtypes in colorectal cancer.
Nat Genet. 47:320–329. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Tauriello DVF, Palomo-Ponce S, Stork D,
Berenguer-Llergo A, Badia-Ramentol J, Iglesias M, Sevillano M,
Ibiza S, Cañellas A, Hernando-Momblona X, et al: TGFβ drives immune
evasion in genetically reconstituted colon cancer metastasis.
Nature. 554:538–543. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Meng XM: Inflammatory mediators and renal
fibrosis. Adv Exp Med Biol. 1165:381–406. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Gu YY, Liu XS, Huang XR, Yu XQ and Lan HY:
Diverse role of TGF-β in kidney disease. Front Cell Dev Biol.
8:1232020. View Article : Google Scholar
|
|
111
|
Wang H, Song K, Krebs TL, Yang J and
Danielpour D: Smad7 is inactivated through a direct physical
interaction with the LIM protein Hic-5/ARA55. Oncogene.
27:6791–6805. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Thompson-Elliott B, Johnson R and Khan SA:
Alterations in TGFβ signaling during prostate cancer progression.
Am J Clin Exp Urol. 9:318–328. 2021.
|
|
113
|
Mirzaei S, Paskeh MDA, Saghari Y, Zarrabi
A, Hamblin MR, Entezari M, Hashemi M, Aref AR, Hushmandi K, Kumar
AP, et al: Transforming growth factor-beta (TGF-β) in prostate
cancer: A dual function mediator? Int J Biol Macromol. 206:435–452.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Huang M, Fu M, Wang J, Xia C, Zhang H,
Xiong Y, He J, Liu J, Liu B, Pan S and Liu F: TGF-β1-activated
cancer-associated fibroblasts promote breast cancer invasion,
metastasis and epithelial-mesenchymal transition by autophagy or
overexpression of FAP-α. Biochem Pharmacol. 188:1145272021.
View Article : Google Scholar
|
|
115
|
Roane BM, Arend RC and Birrer MJ: Review:
Targeting the transforming growth factor-beta pathway in ovarian
cancer. Cancers (Basel). 11:6682019. View Article : Google Scholar
|
|
116
|
Lamora A, Talbot J, Bougras G, Amiaud J,
Leduc M, Chesneau J, Taurelle J, Stresing V, Le Deley MC, Heymann
MF, et al: Overexpression of smad7 blocks primary tumor growth and
lung metastasis development in osteosarcoma. Clin Cancer Res.
20:5097–5112. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Xu S, Yang S, Sun G, Huang W and Zhang Y:
Transforming growth factor-beta polymorphisms and serum level in
the development of osteosarcoma. DNA Cell Biol. 33:802–806. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Bu MT, Chandrasekhar P, Ding L and Hugo W:
The roles of TGF-β and VEGF pathways in the suppression of
antitumor immunity in melanoma and other solid tumors. Pharmacol
Ther. 240:1082112022.Epub ahead of print. View Article : Google Scholar
|
|
119
|
Zheng C, Zhou XW and Wang JZ: The dual
roles of cytokines in Alzheimer's disease: Update on interleukins,
TNF-α, TGF-β and IFN-γ. Transl Neurodegener. 5:72016. View Article : Google Scholar
|
|
120
|
Park JK, Lee KJ, Kim JY and Kim H: The
association of blood-based inflammatory factors IL-1β, TGF-β and
CRP with cognitive function in Alzheimer's disease and mild
cognitive impairment. Psychiatry Investig. 18:11–18. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
121
|
van der Kraan PM: The changing role of
TGFβ in healthy, ageing and osteoarthritic joints. Nat Rev
Rheumatol. 13:155–163. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Kuźnik-Trocha K, Winsz-Szczotka K,
Komosińska-Vassev K, Jura-Półtorak A, Kotulska-Kucharz A, Kucharz
EJ, Kotyla P and Olczyk K: Plasma glycosaminoglycan profiles in
systemic sclerosis: Associations with MMP-3, MMP-10, TIMP-1,
TIMP-2, and TGF-beta. Biomed Res Int. 2020:64165142020. View Article : Google Scholar
|
|
123
|
Wu WS, Ling CH, Lee MC, Cheng CC, Chen RF,
Lin CF, You RI and Chen YC: Targeting Src-Hic-5 signal cascade for
preventing migration of cholangiocarcinoma cell HuCCT1.
Biomedicines. 10:10222022. View Article : Google Scholar : PubMed/NCBI
|