|
1
|
Jansen M, Irving H, Gillam L, Sharwood E,
Preisz A, Basu S, Delaney C, McDougall R, Johnston C, Isaacs D and
Lister P: Ethical considerations for paediatrics during the
COVID-19 pandemic: A discussion paper from the Australian
Paediatric Clinical Ethics Collaboration. J Paediatr Child Health.
56:847–851. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
International Child Health Group; Royal
College of Paediatrics & Child Health; Royal College of
Paediatrics & Child Hea: Impact of the COVID-19 pandemic on
global child health: Joint statement of the International Child
Health Group and the Royal College of Paediatrics and Child Health.
Arch Dis Child. 106:115–116. 2021. View Article : Google Scholar
|
|
3
|
Johnston R, Sen C and Baki Y: Virtual
paediatrics: What COVID-19 has taught us about online learning.
Arch Dis Child Educ Pract Ed. 108:125–129. 2023. View Article : Google Scholar
|
|
4
|
Mammas IN, Greenough A, Theodoridou M and
Spandidos DA: The foundation of the Institute of Paediatric
Virology on the island of Euboea, Greece (Review). Exp Ther Med.
20:3022020. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mammas IN, Kramvis A, Papaevangelou V,
Doukas SG, Naya SD, Doukas PG, Melikoki V, Bouros D, Thiagarajan P,
Chrousos GP, et al: SARS-CoV-2 infection and children: Insights
from the 6th Workshop on Paediatric Virology (Review). World Acad
Sci J. 4:1–12. 2022. View Article : Google Scholar
|
|
6
|
Mammas IN, Liston M, Koletsi P, Vitoratou
DI, Koutsaftiki C, Papatheodoropoulou A, Kornarou H, Theodoridou M,
Kramvis A, Drysdale SB and Spandidos DA: Insights in paediatric
virology during the COVID-era (Review). Med Int (Lond).
2:172022.
|
|
7
|
Kramvis A, Mammas IN and Spandidos DA:
Exploring the optimal vaccination strategy against hepatitis B
virus in childhood (Review). Biomed Rep. 19:482023. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
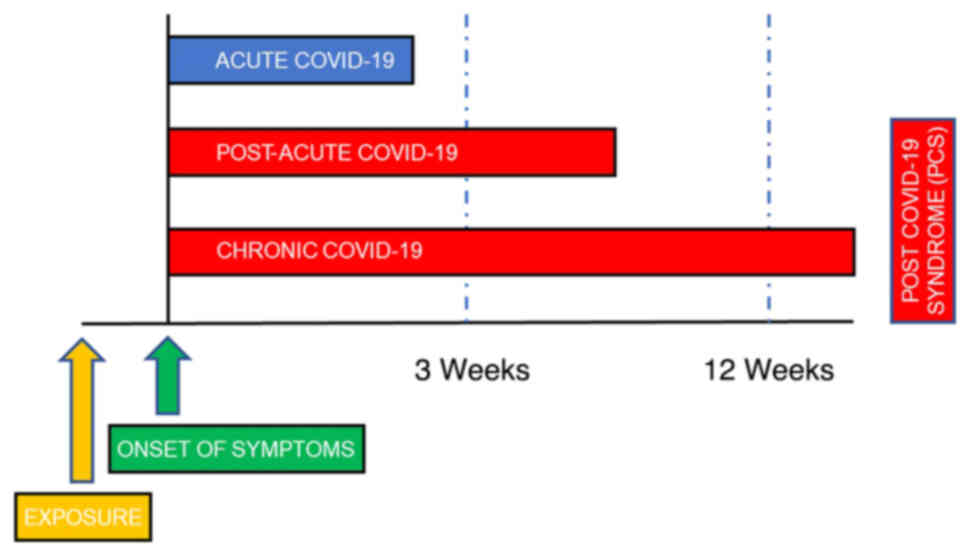
Kramvis A: The clinical implications of
hepatitis B virus genotypes and HBeAg in pediatrics. Rev Med Virol.
26:285–303. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kramvis A: Challenges for hepatitis B
virus cure in resource-limited settings in sub-Saharan Africa. Curr
Opin HIV AIDS. 15:185–192. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Maher F, Mammas IN and Spandidos DA: The
challenges and perspectives of palliative medicine: A webinar by
the Paediatric Virology Study Group. Med Int (Lond). 3:242023.
|
|
11
|
Fowler K, Mucha J, Neumann M, Lewandowski
W, Kaczanowska M, Grys M, Schmidt E, Natenshon A, Talarico C, Buck
PO and Diaz-Decaro J: A systematic literature review of the global
seroprevalence of cytomegalovirus: Possible implications for
treatment, screening, and vaccine development. BMC Public Health.
22:16592022. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hiskey L, Madigan T, Ristagno EH,
Razonable RR and Ferdjallah A: Prevention and management of human
cytomegalovirus in pediatric HSCT recipients: A review. Front
Pediatr. 10:10399382022. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Pesch MH, Kuboushek K, McKee MM, Thorne MC
and Weinberg JB: Congenital cytomegalovirus infection. BMJ.
373:n12122021. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Faure-Bardon V, Fourgeaud J, Stirnemann J,
Leruez-Ville M and Ville Y: Secondary prevention of congenital
cytomegalovirus infection with valacyclovir following maternal
primary infection in early pregnancy. Ultrasound Obstet Gynecol.
58:576–581. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Chen SJ, Wang SC and Chen YC: Challenges,
recent advances and perspectives in the treatment of human
cytomegalovirus infections. Trop Med Infect Dis. 7:4392022.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Acosta E, Bowlin T, Brooks J, Chiang L,
Hussein I, Kimberlin D, Kauvar LM, Leavitt R, Prichard M and
Whitley R: Advances in the development of therapeutics for
cytomegalovirus infections. J Infect Dis. 221(Suppl 1): S32–S44.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Li L, Freed DC, Liu Y, Li F, Barrett DF,
Xiong W, Ye X, Adler SP, Rupp RE, Wang D, et al: A conditionally
replication-defective cytomegalovirus vaccine elicits potent and
diverse functional monoclonal antibodies in a phase I clinical
trial. NPJ Vaccines. 6:792021. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Das R, Blazquez-Gamero D, Bernstein DI,
Gantt S, Bautista O, Beck K, BSN RN, Conlon A, Rosenbloom D, Wang
D, et al: 1048. Double-blind, randomized, placebo-controlled phase
2b multicenter trial of V160, a replication-defective human
cytomegalovirus (CMV) vaccine. Open Forum Infect Dis. 8(Suppl 1):
S615–S616. 2021. View Article : Google Scholar
|
|
19
|
Mustonen J, Huttunen NP,
Brummer-Korvenkontio M and Vaheri A: Clinical picture of
nephropathia epidemica in children. Acta Paediatr. 83:526–529.
1994. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Peters CJ: Viral Hemorrhagic Fevers. Viral
Pathogenesis. Lippincott-Raven Publishers; New York, NY: pp.
779–794. 1997
|
|
21
|
Peters CJ, Simpson GL and Levy H: Spectrum
of hantavirus infection: Hemorrhagic fever with renal Syndrome and
hantavirus pulmonary Syndrome. Annu Rev Med. 50:531–545. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Linderholm M and Elgh F: Clinical
characteristics of hantavirus infections on the Eurasian continent.
Curr Top Microbiol Immunol. 256:135–151. 2001.PubMed/NCBI
|
|
23
|
Koskela S, Mäkelä S, Strandin T, Vaheri A,
Outinen T, Joutsi-Korhonen L, Pörsti I, Mustonen J and Laine O:
Coagulopathy in acute puumala hantavirus infection. Viruses.
13:15532021. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Latus J, Schwab M, Tacconelli E, Pieper
FM, Wegener D, Rettenmaier B, Schwab A, Hoffmann L, Dippon J,
Müller S, et al: Acute kidney injury and tools for
risk-stratification in 456 patients with hantavirus-induced
nephropathia epidemica. Nephrol Dial Transplant. 30:245–251. 2015.
View Article : Google Scholar
|
|
25
|
Latus J, Kitterer D, Segerer S, Artunc F,
Alscher MD and Braun N: Severe thrombocytopenia in
hantavirus-induced nephropathia epidemica. Infection. 43:83–87.
2015. View Article : Google Scholar
|
|
26
|
Antoniades A, Grekas D, Rossi CA and LeDuc
JW: Isolation of a hantavirus from a severely ill patient with
hemorrhagic fever with renal syndrome in Greece. J Infect Dis.
156:1010–1013. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Ferres M and Vial P: Hantavirus infection
in children. Curr Opin Pediatr. 16:70–75. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Dusek J, Pejcoch M, Kolsky A, Seeman T,
Nemec V, Stejskal J, Vondrak K and Janda J: Mild course of Puumala
nephropathy in children in an area with sporadic occurrence
Hantavirus infection. Pediatr Nephrol. 21:1889–1892. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
van der Werff ten Bosch J, Heyman P,
Potters D, Peeters S, Cochez C and Piérard D: Hantavirus Puumala
infection as a cause of fever of unknown origin in a child. Acta
Paediatr. 93:1120–1122. 2004. View Article : Google Scholar
|
|
30
|
Eboriadou M, Kalevrosoglou I, Varlamis G,
Mitsiakos G, Papa A and Antoniadis A: Hantavirus nephropathy in a
child. Nephrol Dial Transplant. 14:1040–1041. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Papadopoulos NG, Moustaki M, Tsolia M,
Bossios A, Astra E, Prezerakou A, Gourgiotis D and Kafetzis D:
Association of rhinovirus infection with increased disease severity
in acute bronchiolitis. Am J Respir Crit Care Med. 165:1285–1289.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Asner SA, Petrich A, Hamid JS, Mertz D,
Richardson SE and Smieja M: Clinical severity of
rhinovirus/enterovirus compared to other respiratory viruses in
children. Influenza Other Respir Viruses. 8:436–442. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Smith ME and Wilson PT: Human
rhinovirus/enterovirus in pediatric acute respiratory distress
Syndrome. J Pediatr Intensive Care. 9:81–86. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Miller EK, Williams JV, Gebretsadik T,
Carroll KN, Dupont WD, Mohamed YA, Morin LL, Heil L, Minton PA,
Woodward K, et al: Host and viral factors associated with severity
of human rhinovirus-associated infant respiratory tract illness. J
Allergy Clin Immunol. 127:883–891. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Costa LF, Queiróz DA, Lopes da Silveira H,
Bernardino Neto M, de Paula NT, Oliveira TF, Tolardo AL and
Yokosawa J: Human rhinovirus and disease severity in children.
Pediatrics. 133:e312–e321. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Miller EK, Bugna J, Libster R, Shepherd
BE, Scalzo PM, Acosta PL, Hijano D, Reynoso N, Batalle JP, Coviello
S, et al: Human rhinoviruses in severe respiratory disease in very
low birth weight infants. Pediatrics. 129:e60–e67. 2012. View Article : Google Scholar :
|
|
37
|
Brand HK, de Groot R, Galama JM, Brouwer
ML, Teuwen K, Hermans PW, Melchers WJ and Warris A: Infection with
multiple viruses is not associated with increased disease severity
in children with bronchiolitis. Pediatr Pulmonol. 47:393–400. 2012.
View Article : Google Scholar
|
|
38
|
Spaeder MC, Custer JW, Miles AH, Ngo L,
Morin NP, Scafidi S, Bembea MM and Song X: A multicenter outcomes
analysis of children with severe rhino/enteroviral respiratory
infection. Pediatr Crit Care Med. 16:119–123. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Louie JK, Roy-Burman A, Guardia-Labar L,
Boston EJ, Kiang D, Padilla T, Yagi S, Messenger S, Petru AM,
Glaser CA and Schnurr DP: Rhinovirus associated with severe lower
respiratory tract infections in children. Pediatr Infect Dis J.
28:337–339. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Renwick N, Schweiger B, Kapoor V, Liu Z,
Villari J, Bullmann R, Miething R, Briese T and Lipkin WI: A
recently identified rhinovirus genotype is associated with severe
respiratory-tract infection in children in Germany. J Infect Dis.
196:1754–1760. 2007. View
Article : Google Scholar
|
|
41
|
Lee WM, Kiesner C, Pappas T, Lee I,
Grindle K, Jartti T, Jakiela B, Lemanske RF Jr, Shult PA and Gern
JE: A diverse group of previously unrecognized human rhinoviruses
are common causes of respiratory illnesses in infants. PLoS One.
2:e9662007. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
To KK, Lau SK, Chan KH, Mok KY, Luk HK,
Yip CC, Ma YK, Sinn LH, Lam SH, Ngai CW, et al: Pulmonary and
extrapulmonary complications of human rhinovirus infection in
critically ill patients. J Clin Virol. 77:85–91. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Liu J, Zhao H, Feng Z, Liu Y, Feng Q, Qian
S, Xu L, Gao H and Xie Z: A severe case of human rhinovirus A45
with central nervous system involvement and viral sepsis. Virol J.
19:722022. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Li CX, Burrell R, Dale RC, Kesson A, Blyth
CC, Clark JE, Crawford N, Jones CA, Britton PN and Holmes EC:
Diagnosis and analysis of unexplained cases of childhood
encephalitis in Australia using metatranscriptomic sequencing. J
Gen Virol. 1032022.
|
|
45
|
Hazama K, Shiihara T, Tsukagoshi H,
Matsushige T, Dowa Y and Watanabe M: Rhinovirus-associated acute
encephalitis/encephalopathy and cerebellitis. Brain Dev.
41:551–554. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Triantafilou K, Vakakis E, Richer EA,
Evans GL, Villiers JP and Triantafilou M: Human rhinovirus
recognition in non-immune cells is mediated by Toll-like receptors
and MDA-5, which trigger a synergetic pro-inflammatory immune
response. Virulence. 2:22–29. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Centers for Disease Control and Prevention
(CDC): Adenoviruses. CDC. Atlanta, GA: 2022, https://www.cdc.gov/adenovirus/hcp/index.html.
|
|
48
|
Edmond K, Scott S, Korczak V, Ward C,
Sanderson C, Theodoratou E, Clark A, Griffiths U, Rudan I and
Campbell H: Long term sequelae from childhood pneumonia; systematic
review and meta-analysis. PLoS One. 7:e312392012. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Birenbaum E, Linder N, Varsano N, Azar R,
Kuint J, Spierer A and Reichman B: Adenovirus type 8 conjunctivitis
outbreak in a neonatal intensive care unit. Arch Dis Child. 68(5
Spec No): 610–611. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Bowles NE, Ni J, Kearney DL, Pauschinger
M, Schultheiss HP, McCarthy R, Hare J, Bricker JT, Bowles KR and
Towbin JA: Detection of viruses in myocardial tissues by polymerase
chain reaction. Evidence of adenovirus as a common cause of
myocarditis in children and adults. J Am Coll Cardiol. 42:466–472.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
World Health Organization (WHO): Severe
acute hepatitis of unknown aetiology in children-Multi-country.
WHO; Geneva: 2022, https://www.who.int/emergen-cies/disease-outbreak-news/item/2022-DON400.
Accessed October 20, 2022
|
|
52
|
Cates J, Baker JM, Almendares O,
Kambhampati AK, Burke RM, Balachandran N, Burnett E, Potts CC,
Reagan-Steiner S, Kirking HL, et al: Interim analysis of acute
hepatitis of unknown etiology in children aged >10 years-United
States, October 2021-June 2022. MMWR Morb Mortal Wkly Rep.
71:852–858. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Morfopoulou S, Buddle S, Torres Montaguth
OE, Atkinson L, Guerra-Assunção JA, Storey N, Roy S, Lennon A, Lee
JCD, Williams R, et al: Genomic investigations of acute hepatitis
of unknown aetiology in children. View Article : Google Scholar : https://media.gosh.nhs.uk/documents/MEDRXIV-2022-277963v1-Breuer.pdf.
Accessed October 20, 2022
|
|
54
|
Schwartz KL, Richardson SE, MacGregor D,
Mahant S, Raghuram K and Bitnun A: Adenovirus-Associated central
nervous system disease in children. J Pediatr. 205:130–137. 2019.
View Article : Google Scholar
|
|
55
|
Huang YC, Huang SL, Chen SP, Huang YL,
Huang CG, Tsao KC and Lin TY: Adenovirus infection associated with
central nervous system dysfunction in children. J Clin Virol.
57:300–304. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Otto WR, Behrens EM, Teachey DT, Lamson
DM, Barrett DM, Bassiri H, Lambert MP, Mount S, Petrosa WL, Romberg
N, et al: Human adenovirus 7-associated hemophagocytic
lymphohistiocytosis-like Illness: Clinical and virological
characteristics in a cluster of five pediatric cases. Clin Infect
Dis. 73:e1532–e1538. 2021. View Article : Google Scholar :
|
|
57
|
Censoplano N, Gorga S, Waldeck K,
Stillwell T, Rabah-Hammad R and Flori H: Neonatal adenovirus
infection complicated by hemophagocytic lymphohistiocytosis
Syndrome. Pediatrics. 141(Suppl 5): S475–S480. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Munoz FM, Piedra PA and Demmler GJ:
Disseminated adenovirus disease in immunocompromised and
immunocompetent children. Clin Infect Dis. 27:1194–1200. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Alcamo AM, Wolf MS, Alessi LJ, Chong HJ,
Green M, Williams JV and Simon DW: Successful use of cidofovir in
an immunocompetent child with severe adenoviral sepsis. Pediatrics.
145:e201916322020. View Article : Google Scholar
|
|
60
|
Ljungman P, Ribaud P, Eyrich M,
Matthes-Martin S, Einsele H, Bleakley M, Machaczka M, Bierings M,
Bosi A, Gratecos N, et al: Cidofovir for adenovirus infections
after allogeneic hematopoietic stem cell transplantation: A survey
by the Infectious Diseases Working Party of the European Group for
Blood and Marrow Transplantation. Bone Marrow Transplant.
31:481–486. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Sofer A, Arger N and Vest M: Successful
Treatment of Adenovirus-Induced ARDS With Cidofovir and IVIG. Chest
Infect. 144:229A2013. View Article : Google Scholar
|
|
62
|
Leen AM, Bollard CM, Mendizabal AM, Shpall
EJ, Szabolcs P, Antin JH, Kapoor N, Pai SY, Rowley SD, Kebriaei P,
et al: Multicenter study of banked third-party virus-specific T
cells to treat severe viral infections after hematopoietic stem
cell transplantation. Blood. 121:5113–5123. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Callard F and Perego E: How and why
patients made long COVID. Soc Sci Med. 268:1134262021. View Article : Google Scholar
|
|
64
|
Soriano JB, Murthy S, Marshall JC, Relan P
and Diaz JV; WHO Clinical Case Definition Working Group on
Post-COVID-19 condition: A clinical case definition of
post-COVID-19 condition by a Delphi consensus. Lancet Infect Dis.
22:e102–e107. 2022. View Article : Google Scholar
|
|
65
|
Munblit D, Simpson F, Mabbitt J,
Dunn-Galvin A, Semple CO and Warner J: Legacy of COVID-19 infection
in children: Long-COVID will have a lifelong health/economic
impact. Arch Dis Child. 107:e22022. View Article : Google Scholar
|
|
66
|
Lopez-Leon S, Wegman-Ostrosky T, Ayuzo del
Valle NC, Perelman C, Sepulveda R, Rebolledo PA, Cuapio A and
Villapol S: Long COVID in children and adolescents: A systematic
review and meta-analyses. Sci Rep. 12:99502022. View Article : Google Scholar
|
|
67
|
Thallapureddy K, Thallapureddy K, Zerda E,
Suresh N, Kamat D, Rajasekaran K and Moreira A: Long-Term
complications of COVID-19 infection in adolescents and children.
Curr Pediatr Rep. 10:11–17. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Fainardi V, Meoli A, Chiopris G, Motta M,
Skenderaj K, Grandinetti R, Bergomi A, Antodaro F, Zona S and
Esposito S: Long COVID in children and adolescents. Life (Basel).
12:2852022.PubMed/NCBI
|
|
69
|
Borch L, Holm M, Knudsen M,
Ellermann-Eriksen S and Hagstroem S: Long COVID symptoms and
duration in SARS-CoV-2 positive children-a nationwide cohort study.
Eur J Pediatr. 181:1597–1607. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Kompaniyets L, Bull-Otterson L, Boehmer
TK, Baca S, Alvarez P, Hong K, Hsu J, Harris AM, Gundlapalli AV and
Saydah S: Post-COVID-19 symptoms and conditions among children and
adolescents-United States. March 1, 2020-January 31, 2022. MMWR
Morb Mortal Wkly Rep. 71:993–999. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Zimmermann P, Pittet LF and Curtis N: How
common is Long COVID in children and adolescents? Pediatr Infect
Dis J. 40:e482–e487. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Nittas V, Gao M, West EA, Ballouz T,
Menges D, Wulf Hanson S and Puhan MA: Long COVID through a public
health lens: An umbrella review. Public Health Rev. 43:16045012022.
View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Pavli A, Theodoridou M and Maltezou H:
Post-COVID Syndrome: Incidence, clinical spectrum and challenges
for Primary Healthcare Professionals. Arch Med Res. 52:575–581.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Osmanov IM, Spiridonova E, Bobkova P,
Gamirova A, Shikhaleva A, Andreeva M, Blyuss O, El-Taravi Y,
DunnGalvin A, Comberiati P, et al: Risk factors for post-COVID-19
condition in previously hospitalized children using the ISARIC
Global follow-up protocol: A prospective cohort study. Eur Respir
J. 59:2101342022. View Article : Google Scholar
|
|
75
|
Zimmermann P, Pittet LF and Curtis N: Long
covid in children and adolescents. BMJ. 376:o1432022. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Zimmermann P, Pittet LF and Curtis N: The
challenge of studying Long COVID: An updated review. Pediatr Infect
Dis J. 41:424–426. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Greenhalgh T, Sivan M, Delaney B, Evans R
and Milne R: Long covid-an update for primary care. BMJ.
378:e0721172022. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Esposito S, Principi N, Azzari C,
Cardinale F, Di Mauro G, Galli L, Gattinara GC, Fainardi V, Guarino
A, Lancella L, et al: Italian intersociety consensus on management
of long covid in children. Ital J Pediatr. 48:422022. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Goldman RD: Long COVID in children. Can
Fam Physician. 68:263–265. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Cozzi G, Marchetti F and Barbi E:
Clinicians need to be careful that they do not confuse mental
health issues and long COVID in children and adolescents. Acta
Paediatr. 112:180–183. 2023. View Article : Google Scholar
|
|
81
|
Morrow AK, Malone LA, Kokorelis C,
Petracek LS, Eastin EF, Lobner KL, Neuendorff L and Rowe PC:
Long-term COVID 19 sequelae in adolescents: The overlap with
orthostatic intolerance and ME/CFS. Curr Pediatr Rep. 10:31–44.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Salomon LJ and Garel C: Magnetic resonance
imaging examination of the fetal brain. Ultrasound Obstet Gynecol.
30:1019–1032. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Neuberger I, Garcia J, Meyers ML, Feygin
T, Bulas DI and Mirsky DM: Imaging of congenital central nervous
system infections. Pediatr Radiol. 48:513–523. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Rossi AC and Prefumo F: Additional value
of fetal magnetic resonance imaging in the prenatal diagnosis of
central nervous system anomalies: A systematic review of the
literature. Ultrasound Obstet Gynecol. 44:388–393. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Lo CP and Chen CY: Neuroimaging of viral
infections in infants and young children. Neuroimaging Clin N Am.
18:119–132. viii2008. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Griffiths PD, Mooney C, Bradburn M and
Jarvis D: Should we perform in utero MRI on a fetus at increased
risk of a brain abnormality if ultrasonography is normal or shows
non-specific findings? Clin Radiol. 73:123–134. 2018. View Article : Google Scholar
|
|
87
|
Verstraelen H, Vanzieleghem B, Defoort P,
Vanhaesebrouck P and Temmerman M: Prenatal ultrasound and magnetic
imaging in fetal varicella syndrome: Correlation with pathology
findings. Prenat Diagn. 23:705–709. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Sanchez TR, Datlow MD and Nidecker AE:
Diffuse periventricular calcification and brain atrophy: A case of
neonatal central nervous system cytomegalovirus infection.
Neuroradiol J. 29:314–316. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Mammas IN, Drysdale SB, Theodoridou M and
Spandidos DA: Exploring medical terminology inexpediencies:
Tripledemic vs. triple epidemic. Exp Ther Med. 26:3342023.
View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Centers for Disease Control and Prevention
(CDC): Post-COVID Conditions: Information for Healthcare Providers.
CDC; Atlanta, GA2022, https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/post-covid-conditions.html.
Accessed October 20, 2022
|
|
91
|
The National Institute for Health and Care
Excellence (NICE): COVID-19 rapid guideline: managing the long-term
effects of COVID-19. https://www.nice.org.uk/guidance/NG. pp. 188Accessed
October 20, 2022
|
|
92
|
National Institute for Health and Care
Research (NIHR): Living with Covid-19-Second Review. https://evidence.nihr.ac.uk/theme-dreview/living-with-covid19-second-review.
Accessed October 20, 2022
|
|
93
|
Stephenson T, Allin B, Nugawela MD, Rojas
N, Dalrymple E, Pinto Pereira S, Soni M, Knight M, Cheung EY,
Heyman I, et al: Long COVID (post-COVID-19 condition) in children:
A modified Delphi process. Arch Dis Child. 107:674–680. 2022.
View Article : Google Scholar : PubMed/NCBI
|