|
1
|
The Lancet Diabetes Endocrinology:
Osteoporosis: Overlooked in men for too long. Lancet Diabetes
Endocrinol. 9:12021. View Article : Google Scholar
|
|
2
|
Shen Y, Huang X, Wu J, Lin X, Zhou X, Zhu
Z, Pan X, Xu J, Qiao J, Zhang T, et al: The global burden of
osteoporosis, low bone mass, and its related fracture in 204
countries and territories, 1990-2019. Front Endocrinol (Lausanne).
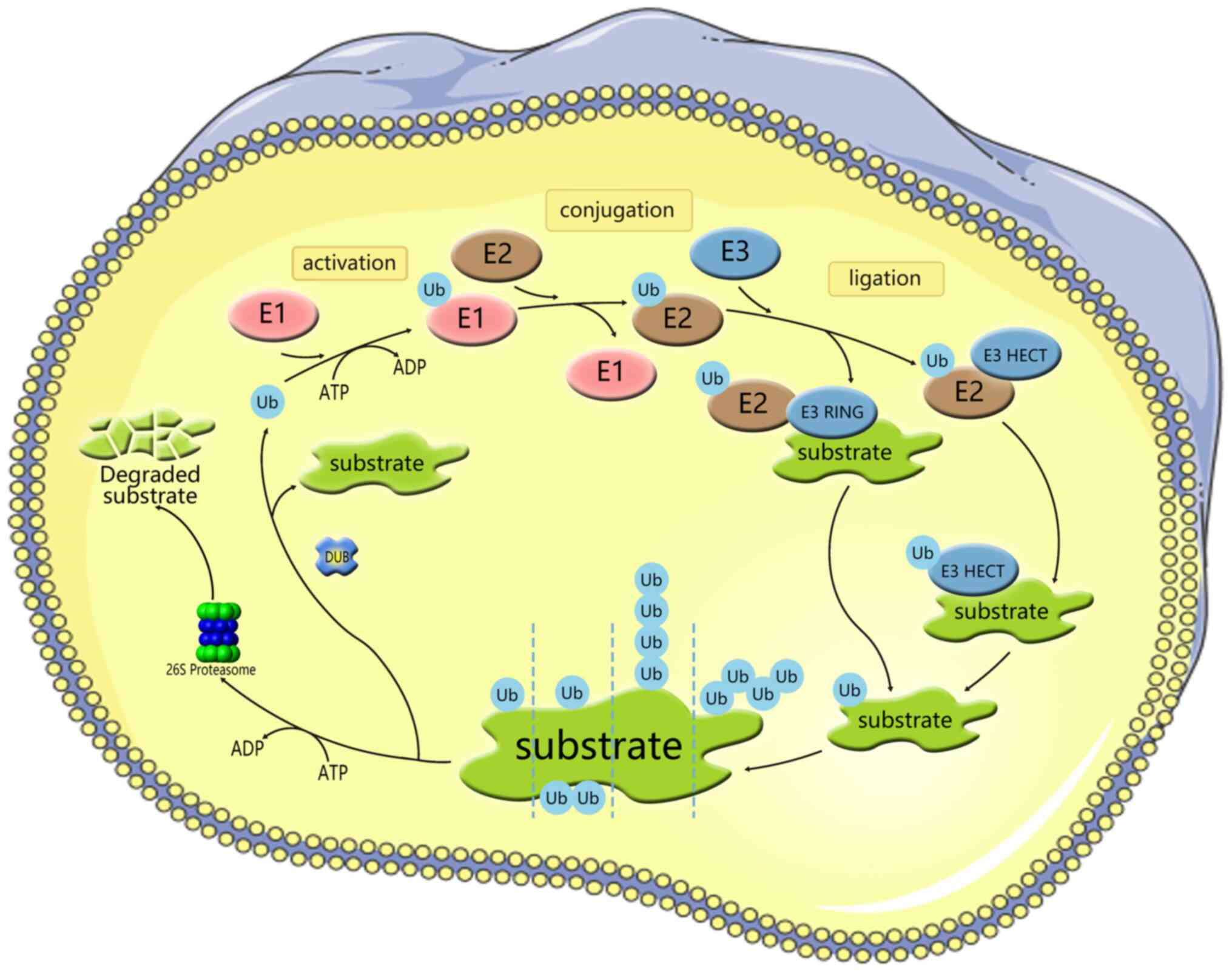
13:8822412022. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
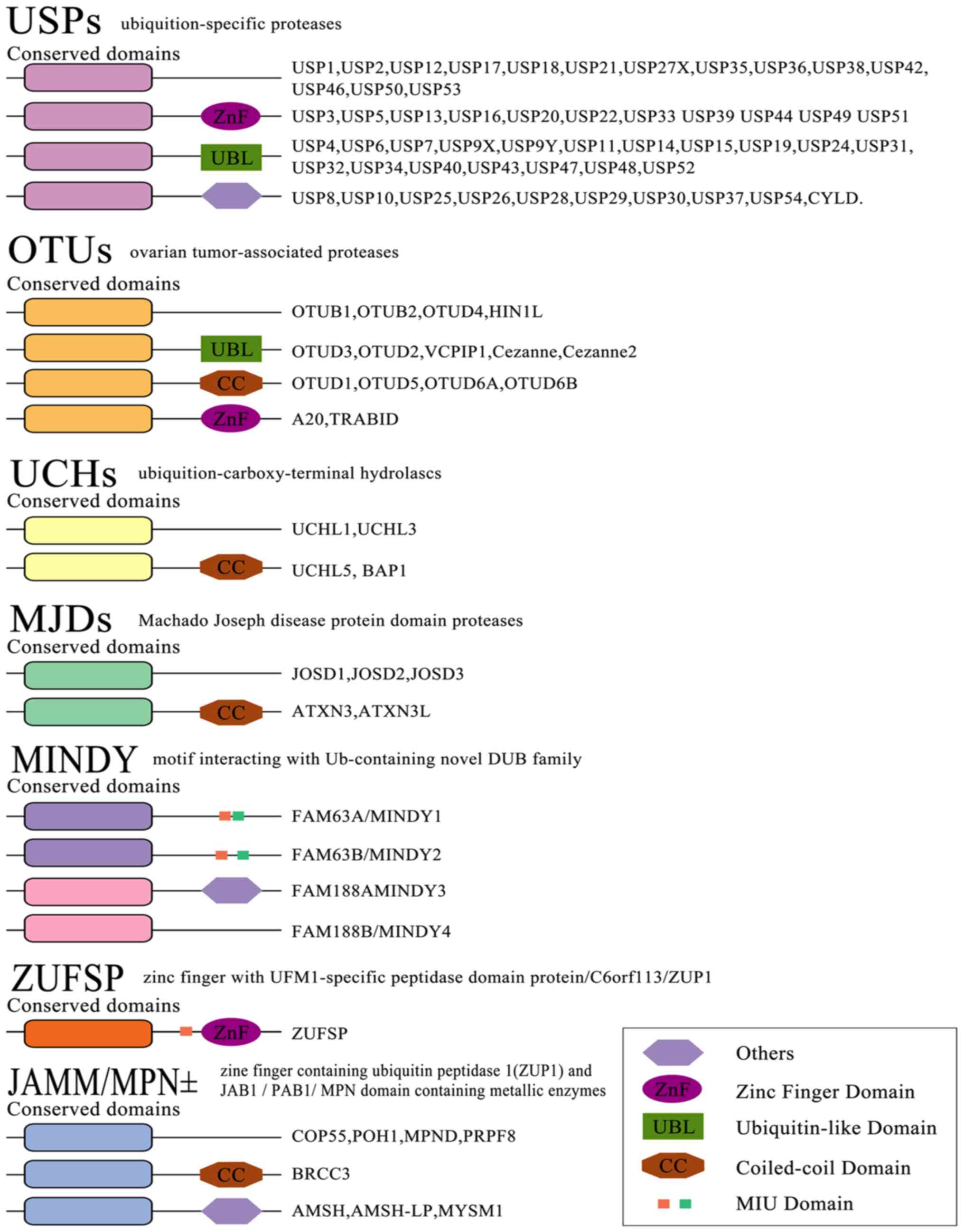
Zhu Y, Huang Z, Wang Y, Xu W, Chen H, Xu
J, Luo S, Zhang Y, Zhao D and Hu J: The efficacy and safety of
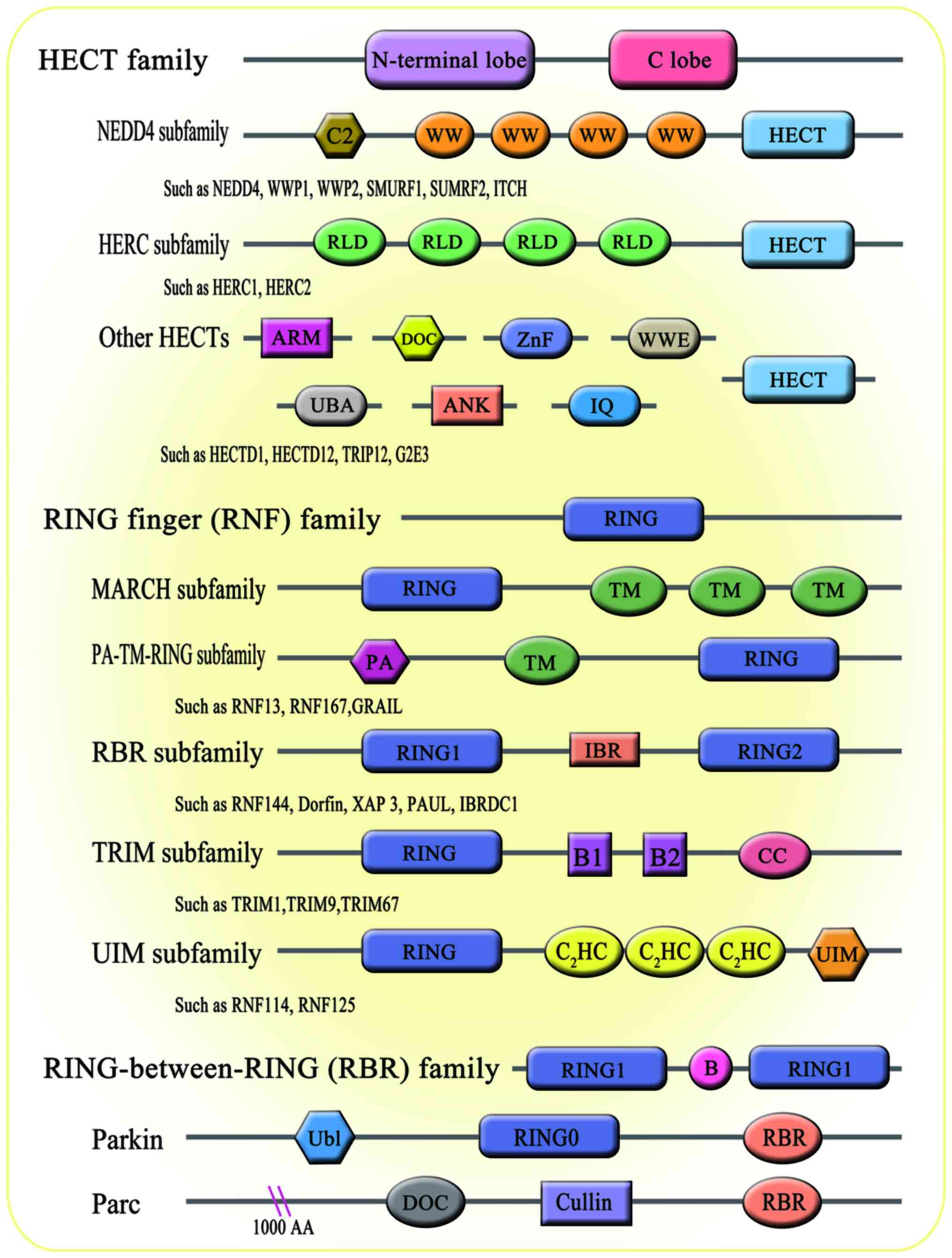
denosumab in postmenopausal women with osteoporosis previously
treated with bisphosphonates: A review. J Orthop Translat. 22:7–13.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Xu XM, Li N, Li K, Li XY, Zhang P, Xuan YJ
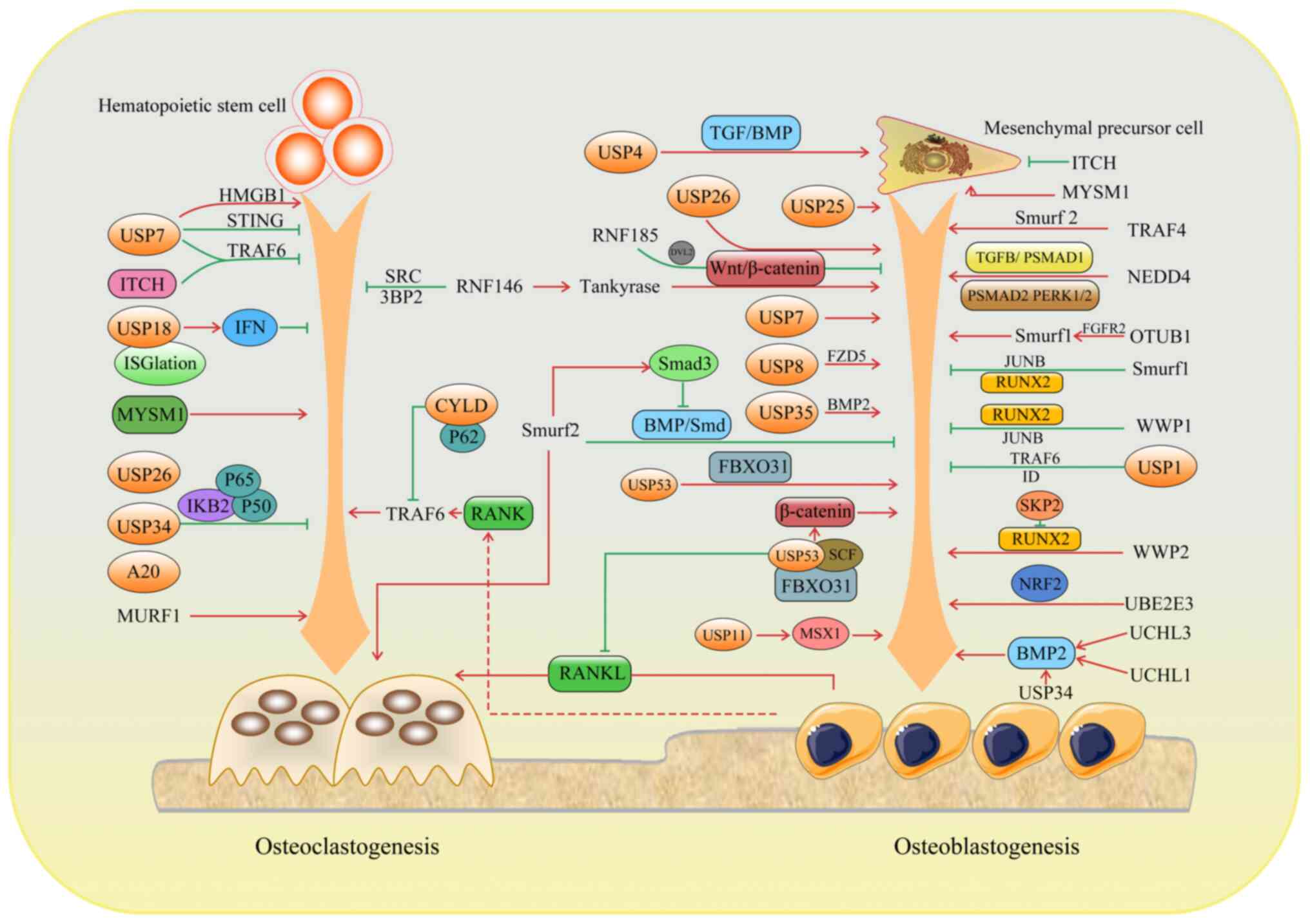
and Cheng XG: Discordance in diagnosis of osteoporosis by
quantitative computed tomography and dual-energy X-ray
absorptiometry in Chinese elderly men. J Orthop Translat. 18:59–64.
2018. View Article : Google Scholar
|
|
5
|
Zhang YW, Cao MM, Li YJ, Dai GC, Lu PP,
Zhang M, Bai LY, Chen XX, Zhang C, Shi L and Rui YF: The regulative
effect and repercussion of probiotics and prebiotics on
osteoporosis: Involvement of brain-gut-bone axis. Crit Rev Food Sci
Nutr. 63:7510–7528. 2023. View Article : Google Scholar
|
|
6
|
Intemann J, De Gorter DJJ, Naylor AJ,
Dankbar B and Wehmeyer C: Importance of osteocyte-mediated
regulation of bone remodelling in inflammatory bone disease. Swiss
Med Wkly. 150:w201872020.PubMed/NCBI
|
|
7
|
Amarasekara DS, Kim S and Rho J:
Regulation of osteoblast differentiation by cytokine networks. Int
J Mol Sci. 22:28512021. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Edwards JR and Mundy GR: Advances in
osteoclast biology: Old findings and new insights from mouse
models. Nat Rev Rheumatol. 7:235–243. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wu M, Chen G and Li YP: TGF-β and BMP
signaling in osteoblast, skeletal development, and bone formation,
homeostasis and disease. Bone Res. 4:160092016. View Article : Google Scholar
|
|
10
|
Han L, Wu J, Wang M, Zhang Z, Hua D, Lei S
and Mo X: RNA modification-related genetic variants in genomic loci
associated with bone mineral density and fracture. Genes (Basel).
13:18922022. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wang C, Chen Q and Xu H: Wnt/β-catenin
signal transduction pathway in prostate cancer and associated drug
resistance. Discov Oncol. 12:402021. View Article : Google Scholar
|
|
12
|
Hu R, Chen L, Chen X, Xie Z, Xia C and
Chen Y: Aloperine improves osteoporosis in ovariectomized mice by
inhibiting RANKL-induced NF-κB, ERK and JNK approaches. Int
Immunopharmacol. 97:1077202021. View Article : Google Scholar
|
|
13
|
Hou H, Peng Q, Wang S, Zhang Y, Cao J,
Deng Y, Wang Y, Sun WC and Wang HB: Anemonin attenuates
RANKL-induced osteoclastogenesis and ameliorates LPS-induced
inflammatory bone loss in mice via modulation of NFATc1. Front
Pharmacol. 10:16962020. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Deng L, Meng T, Chen L, Wei W and Wang P:
The role of ubiquitination in tumorigenesis and targeted drug
discovery. Signal Transduct Target Ther. 5:112020. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Cai J, Culley MK, Zhao Y and Zhao J: The
role of ubiquitination and deubiquitination in the regulation of
cell junctions. Protein Cell. 9:754–69. 2018. View Article : Google Scholar :
|
|
16
|
van Huizen M and Kikkert M: The role of
atypical ubiquitin chains in the regulation of the antiviral innate
immune response. Front Cell Dev Biol. 7:3922020. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Akutsu M, Dikic I and Bremm A: Ubiquitin
chain diversity at a glance. J Cell Sci. 129:875–880. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Gundogdu M and Walden H: Structural basis
of generic versus specific E2-RING E3 interactions in protein
ubiquitination. Protein Sci. 28:1758–1770. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Mennerich D, Kubaichuk K and Kietzmann T:
DUBs, hypoxia, and cancer. Trends Cancer. 5:632–653. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Komander D and Rape M: The ubiquitin code.
Annu Rev Biochem. 81:203–229. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Zheng N and Shabek N: Ubiquitin ligases:
Structure, function, and regulation. Annu Rev Biochem. 86:129–157.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Zhao J, Guo J, Wang Y, Ma Q, Shi Y, Cheng
F, Lu Q, Fu W, Ouyang G, Zhang J, et al: Research progress of DUB
enzyme in hepatocellular carcinoma. Front Oncol. 12:9202872022.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Clague MJ, Urbé S and Komander D: Breaking
the chains: Deubiquitylating enzyme specificity begets function.
Nat Rev Mol Cell Biol. 20:338–352. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Bello AI, Goswami R, Brown SL, Costanzo K,
Shores T, Allan S, Odah R and Mohan RD: Deubiquitinases in
neurodegeneration. Cells. 11:5562022. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Hu M, Li P, Li M, Li W, Yao T, Wu JW, Gu
W, Cohen RE and Shi Y: Crystal structure of a UBP-family
deubiquitinating enzyme in isolation and in complex with ubiquitin
aldehyde. Cell. 111:1041–1054. 2002. View Article : Google Scholar
|
|
26
|
Johnston SC, Larsen CN, Cook WJ, Wilkinson
KD and Hill CP: Crystal structure of a deubiquitinating enzyme
(human UCH-L3) at 1.8 A resolution. EMBO J. 16:3787–3796. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Li Y and Reverter D: Molecular mechanisms
of DUBs regulation in signaling and disease. Int J Mol Sci.
22:9862021. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Komander D, Clague MJ and Urbé S: Breaking
the chains: Structure and function of the deubiquitinases. Nat Rev
Mol Cell Biol. 10:550–563. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Al-Rawi R, Al-Beshri A, Mikhail FM and
McCormick K: Fragile bones secondary to SMURF1 gene duplication.
Calcif Tissue Int. 106:567–573. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Glimcher LH, Jones DC and Wein MN: Control
of postnatal bone mass by the zinc finger adapter protein
Schnurri-3. Ann N Y Acad Sci. 1116:174–181. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Liang C, Peng S, Li J, Lu J, Guan D, Jiang
F, Lu C, Li F, He X, Zhu H, et al: Inhibition of osteoblastic
Smurf1 promotes bone formation in mouse models of distinctive
age-related osteoporosis. Nat Commun. 9:34282018. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Zhao L, Huang J, Guo R, Wang Y, Chen D and
Xing L: Smurf1 inhibits mesenchymal stem cell proliferation and
differentiation into osteoblasts through JunB degradation. J Bone
Miner Res. 25:1246–1256. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Liu W, Qi M, Konermann A, Zhang L, Jin F
and Jin Y: The p53/miR-17/Smurf1 pathway mediates skeletal
deformities in an age-related model via inhibiting the function of
mesenchymal stem cells. Aging (Albany NY). 7:205–218. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Koganti P, Levy-Cohen G and Blank M:
smurfs in protein homeostasis, signaling, and cancer. Front Oncol.
8:2952018. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Xu Z, Greenblatt MB, Yan G, Feng H, Sun J,
Lotinun S, Brady N, Baron R, Glimcher LH and Zou W: SMURF2
regulates bone homeostasis by disrupting SMAD3 interaction with
vitamin D receptor in osteoblasts. Nat Commun. 8:145702017.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Bonewald LF and Mundy GR: Role of
transforming growth factor-beta in bone remodeling. Clin Orthop
Relat Res. 261–276. 1990.PubMed/NCBI
|
|
37
|
Bai Y and Ying Y: The post-translational
modifications of Smurf2 in TGF-β signaling. Front Mol Biosci.
7:1282020. View Article : Google Scholar
|
|
38
|
Kushioka J, Kaito T, Okada R, Ishiguro H,
Bal Z, Kodama J, Chijimatsu R, Pye M, Narimatsu M, Wrana JL, et al:
A novel negative regulatory mechanism of Smurf2 in BMP/Smad
signaling in bone. Bone Res. 8:412020. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Shu L, Zhang H, Boyce BF and Xing L:
Ubiquitin E3 ligase Wwp1 negatively regulates osteoblast function
by inhibiting osteoblast differentiation and migration. J Bone
Miner Res. 28:1925–1935. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Jones DC, Wein MN, Oukka M, Hofstaetter
JG, Glimcher MJ and Glimcher LH: Regulation of adult bone mass by
the zinc finger adapter protein Schnurri-3. Science. 312:1223–1227.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Zhao L, Huang J, Zhang H, Wang Y, Matesic
LE, Takahata M, Awad H, Chen D and Xing L: Tumor necrosis factor
inhibits mesenchymal stem cell differentiation into osteoblasts via
the ubiquitin E3 ligase Wwp1. Stem Cells. 29:1601–1610. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Zhu W, He X, Hua Y, Li Q, Wang J and Gan
X: The E3 ubiquitin ligase WWP2 facilitates RUNX2 protein
transactivation in a mono-ubiquitination manner during osteogenic
differentiation. J Biol Chem. 292:11178–11188. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Liu D, Kou X, Chen C, Liu S, Liu Y, Yu W,
Yu T, Yang R, Wang R, Zhou Y and Shi S: Circulating apoptotic
bodies maintain mesenchymal stem cell homeostasis and ameliorate
osteopenia via transferring multiple cellular factors. Cell Res.
28:918–933. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Matsumoto Y, Larose J, Kent OA, Lim M,
Changoor A, Zhang L, Storozhuk Y, Mao X, Grynpas MD, Cong F and
Rottapel R: RANKL coordinates multiple osteoclastogenic pathways by
regulating expression of ubiquitin ligase RNF146. J Clin Invest.
127:1303–1315. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Zhao Y and Ding S: A high-throughput siRNA
library screen identifies osteogenic suppressors in human
mesenchymal stem cells. Proc Natl Acad Sci USA. 104:9673–9678.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Zhou Y, Shang H, Zhang C, Liu Y, Zhao Y,
Shuang F, Zhong H, Tang J and Hou S: The E3 ligase RNF185
negatively regulates osteogenic differentiation by targeting Dvl2
for degradation. Biochem Biophys Res Commun. 447:431–436. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Liu J, Li X, Zhang H, Gu R, Wang Z, Gao Z
and Xing L: Ubiquitin E3 ligase Itch negatively regulates
osteoblast function by promoting proteasome degradation of
osteogenic proteins. Bone Joint Res. 6:154–161. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Zhang H and Xing L: Ubiquitin e3 ligase
itch negatively regulates osteoblast differentiation from
mesenchymal progenitor cells. Stem Cells. 31:1574–1583. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Zhang H, Wu C, Matesic LE, Li X, Wang Z,
Boyce BF and Xing L: Ubiquitin E3 ligase Itch negatively regulates
osteoclast formation by promoting deubiquitination of tumor
necrosis factor (TNF) receptor-associated factor 6. J Biol Chem.
288:22359–22368. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Zhang F, Zhao Y and Sun Y: USP2 is an SKP2
deubiquitylase that stabilizes both SKP2 and its substrates. J Biol
Chem. 297:1011092021. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Thacker G, Kumar Y, Khan MP, Shukla N,
Kapoor I, Kanaujiya JK, Lochab S, Ahmed S, Sanyal S, Chattopadhyay
N and Trivedi AK: Skp2 inhibits osteogenesis by promoting
ubiquitin-proteasome degradation of Runx2. Biochim Biophys Acta.
1863:510–519. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Eddins MJ, Marblestone JG, Suresh Kumar
KG, Leach CA, Sterner DE, Mattern MR and Nicholson B: Targeting the
ubiquitin E3 ligase MuRF1 to inhibit muscle atrophy. Cell Biochem
Biophys. 60:113–118. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Bettis T, Kim BJ and Hamrick MW: Impact of
muscle atrophy on bone metabolism and bone strength: Implications
for muscle-bone crosstalk with aging and disuse. Osteoporos Int.
29:1713–1720. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Liu Y, Cai G, Chen P, Jiang T and Xia Z:
UBE2E3 regulates cellular senescence and osteogenic differentiation
of BMSCs during aging. PeerJ. 9:e122532021. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Li J, Wang P, Xie Z, Wang S, Cen S, Li M,
Liu W, Tang S, Ye G, Zheng G, et al: TRAF4 positively regulates the
osteogenic differentiation of mesenchymal stem cells by acting as
an E3 ubiquitin ligase to degrade Smurf2. Cell Death Differ.
26:2652–2666. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
An H, Krist DT and Statsyuk AV: Crosstalk
between kinases and Nedd4 family ubiquitin ligases. Mol Biosyst.
10:1643–1657. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Wiszniak S, Harvey N and Schwarz Q: Cell
autonomous roles of Nedd4 in craniofacial bone formation. Dev Biol.
410:98–107. 2016. View Article : Google Scholar
|
|
58
|
Jeon SA, Lee JH, Kim DW and Cho JY:
E3-ubiquitin ligase NEDD4 enhances bone formation by removing
TGFβ1-induced pSMAD1 in immature osteoblast. Bone. 116:248–258.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Tang Y, Lv L, Li W, Zhang X, Jiang Y, Ge W
and Zhou Y: Protein deubiquitinase USP7 is required for osteogenic
differentiation of human adipose-derived stem cells. Stem Cell Res
Ther. 8:1862017. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Sun D, Peng Y, Ge S and Fu Q: USP1
inhibits NF-κB/NLRP3 induced pyroptosis through TRAF6 in
osteoblastic MC3T3-E1 cells. J Musculoskelet Neuronal Interact.
22:536–545. 2022.PubMed/NCBI
|
|
61
|
Williams SA, Maecker HL, French DM, Liu J,
Gregg A, Silverstein LB, Cao TC, Carano RA and Dixit VM: USP1
deubiquitinates ID proteins to preserve a mesenchymal stem cell
program in osteosarcoma. Cell. 146:918–930. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Chaugule S, Kim JM, Yang YS, Knobeloch KP,
He X and Shim JH: Deubiquitinating enzyme USP8 is essential for
skeletogenesis by regulating Wnt signaling. Int J Mol Sci.
22:102892021. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Kaushal K, Tyagi A, Karapurkar JK, Kim EJ,
Tanguturi P, Kim KS, Jung HS and Ramakrishna S: Genome-wide
CRISPR/Cas9-Based screening for deubiquitinase subfamily identifies
ubiquitin-specific protease 11 as a novel regulator of osteogenic
differentiation. Int J Mol Sci. 23:8562022. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Guo YC, Wang MY, Zhang SW, Wu YS, Zhou CC,
Zheng RX, Shao B, Wang Y, Xie L, Liu WQ, et al: Ubiquitin-specific
protease USP34 controls osteogenic differentiation and bone
formation by regulating BMP2 signaling. EMBO J. 37:e993982018.
View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Kim JY, Lee JM and Cho JY: Ubiquitin
C-terminal hydrolase-L3 regulates Smad1 ubiquitination and
osteoblast differentiation. FEBS Lett. 585:1121–1126. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Huang P, Yan R, Zhang X, Wang L, Ke X and
Qu Y: Activating Wnt/β-catenin signaling pathway for disease
therapy: Challenges and opportunities. Pharmacol Ther. 196:79–90.
2019. View Article : Google Scholar
|
|
67
|
Zhou F, Li F, Fang P, Dai T, Yang B, van
Dam H, Jia J, Zheng M and Zhang L: Ubiquitin-specific protease 4
antagonizes osteoblast differentiation through dishevelled. J Bone
Miner Res. 31:1888–8198. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Guasto A and Cormier-Daire V: Signaling
pathways in bone development and their related skeletal dysplasia.
Int J Mol Sci. 22:43212021. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Herhaus L and Sapkota GP: The emerging
roles of deubiquitylating enzymes (DUBs) in the TGFβ and BMP
pathways. Cell Signal. 26:2186–2192. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Baek D, Park KH, Lee KM, Jung S, Joung S,
Kim J and Lee JW: Ubiquitin-specific protease 53 promotes
osteogenic differentiation of human bone marrow-derived mesenchymal
stem cells. Cell Death Dis. 12:2382021. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Hariri H, Kose O, Bezdjian A, Daniel SJ
and St-Arnaud R: USP53 regulates bone homeostasis by controlling
rankl expression in osteoblasts and bone marrow adipocytes. J Bone
Miner Res. 38:578–596. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Tsuru M, Ono A, Umeyama H, Takeuchi M and
Nagata K: Ubiquitin-dependent proteolysis of CXCL7 leads to
posterior longitudinal ligament ossification. PLoS One.
13:e01962042018. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Lin L, Li S, Hu S, Yu W, Jiang B, Mao C,
Li G, Yang R, Miao X, Jin M, et al: UCHL1 impairs periodontal
ligament stem cell osteogenesis in periodontitis. J Dent Res.
102:61–71. 2023. View Article : Google Scholar
|
|
74
|
Cao Y, Zhang X, Hu M, Yang S, Li X, Han R,
Zhou J, Li D and Liu D: CYLD inhibits osteoclastogenesis to
ameliorate alveolar bone loss in mice with periodontitis. J Cell
Physiol. 238:1036–1045. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Ang E, Pavlos NJ, Rea SL, Qi M, Chai T,
Walsh JP, Ratajczak T, Zheng MH and Xu J: Proteasome inhibitors
impair RANKL-induced NF-kappaB activity in osteoclast-like cells
via disruption of p62, TRAF6, CYLD, and IkappaBalpha signaling
cascades. J Cell Physiol. 220:450–459. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Jin W, Chang M, Paul EM, Babu G, Lee AJ,
Reiley W, Wright A, Zhang M, You J and Sun SC: Deubiquitinating
enzyme CYLD negatively regulates RANK signaling and
osteoclastogenesis in mice. J Clin Invest. 118:1858–1866. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Hong JY, Bae WJ, Yi JK, Kim GT and Kim EC:
Anti-inflammatory and anti-osteoclastogenic effects of zinc finger
protein A20 overexpression in human periodontal ligament cells. J
Periodontal Res. 51:529–539. 2016. View Article : Google Scholar
|
|
78
|
Lee EG, Boone DL, Chai S, Libby SL, Chien
M, Lodolce JP and Ma A: Failure to regulate TNF-induced NF-kappaB
and cell death responses in A20-deficient mice. Science.
289:2350–2354. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Lee MJ, Lim E, Mun S, Bae S, Murata K,
Ivashkiv LB and Park-Min KH: Intravenous immunoglobulin (IVIG)
attenuates TNF-induced pathologic bone resorption and suppresses
osteoclastogenesis by inducing A20 expression. J Cell Physiol.
231:449–458. 2016. View Article : Google Scholar :
|
|
80
|
Martens A and van Loo G: A20 at the
crossroads of cell death, inflammation, and autoimmunity. Cold
Spring Harb Perspect Biol. 12:a0364182020. View Article : Google Scholar
|
|
81
|
Yan K, Wu C, Ye Y, Li L, Wang X, He W, Ren
S and Xu Y: A20 inhibits osteoclastogenesis via TRAF6-dependent
autophagy in human periodontal ligament cells under hypoxia. Cell
Prolif. 53:e127782020. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Birol M and Echalier A: Structure and
function of MPN (Mpr1/Pad1 N-terminal) domain-containing proteins.
Curr Protein Pept Sci. 15:504–517. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Fiore A, Liang Y, Lin YH, Tung J, Wang H,
Langlais D and Nijnik A: Deubiquitinase MYSM1 in the hematopoietic
system and beyond: A current review. Int J Mol Sci. 21:30072020.
View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Li P, Yang YM, Sanchez S, Cui DC, Dang RJ,
Wang XY, Lin QX, Wang Y, Wang C, Chen DF, et al: Deubiquitinase
MYSM1 Is essential for normal bone formation and mesenchymal stem
cell differentiation. Sci Rep. 6:222112016. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Haffner-Luntzer M, Kovtun A, Fischer V,
Prystaz K, Hainzl A, Kroeger CM, Krikki I, Brinker TJ, Ignatius A
and Gatzka M: Loss of p53 compensates osteopenia in murine Mysm1
deficiency. FASEB J. 32:1957–1968. 2018. View Article : Google Scholar
|
|
86
|
Lin YC, Zheng G, Liu HT, Wang P, Yuan WQ,
Zhang YH, Peng XS, Li GJ, Wu YF and Shen HY: USP7 promotes the
osteoclast differentiation of CD14+ human peripheral blood
monocytes in osteoporosis via HMGB1 deubiquitination. J Orthop
Translat. 40:80–91. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Xie Z, Wu Y, Shen Y, Guo J, Yuan P, Ma Q,
Wang S, Jie Z, Zhou H, Fan S and Chen S: USP7 inhibits
osteoclastogenesis via dual effects of attenuating TRAF6/TAK1 axis
and stimulating STING signaling. Aging Dis. 14:2267–2283. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Mustachio LM, Lu Y, Kawakami M, Roszik J,
Freemantle SJ, Liu X and Dmitrovsky E: Evidence for the
ISG15-specific deubiquitinase USP18 as an antineoplastic target.
Cancer Res. 78:587–592. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Liu X, Lu Y, Chen Z, Liu X, Hu W, Zheng L,
Chen Y, Kurie JM, Shi M, Mustachio LM, et al: The
ubiquitin-specific peptidase USP18 promotes lipolysis, fatty acid
oxidation, and lung cancer growth. Mol Cancer Res. 19:667–677.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Yim HY, Park C, Lee YD, Arimoto K, Jeon R,
Baek SH, Zhang DE, Kim HH and Kim KI: Elevated response to type I
IFN enhances RANKL-mediated osteoclastogenesis in Usp18-knockout
mice. J Immunol. 196:3887–3895. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Li Q, Wang M, Xue H, Liu W, Guo Y, Xu R,
Shao B and Yuan Q: Ubiquitin-specific protease 34 inhibits
osteoclast differentiation by regulating NF-κB signaling. J Bone
Miner Res. 35:1597–1608. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Li C, Qiu M, Chang L, Qi J, Zhang L,
Ryffel B and Deng L: The osteoprotective role of USP26 in
coordinating bone formation and resorption. Cell Death Differ.
29:1123–1136. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Zhu Q, Fu Y, Cui CP, Ding Y, Deng Z, Ning
C, Hu F, Qiu C, Yu B, Zhou X, et al: OTUB1 promotes osteoblastic
bone formation through stabilizing FGFR2. Signal Transduct Target
Ther. 8:1422023. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
LeBoff MS, Greenspan SL, Insogna KL,
Lewiecki EM, Saag KG, Singer AJ and Siris ES: The clinician's guide
to prevention and treatment of osteoporosis. Osteoporos Int.
33:2049–2102. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Eastell R, Rosen CJ, Black DM, Cheung AM,
Murad MH and Shoback D: Pharmacological management of osteoporosis
in postmenopausal women: An endocrine society* clinical
practice guideline. J Clin Endocrinol Metab. 104:1595–1622. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
96
|
McClung M, Harris ST, Miller PD, Bauer DC,
Davison KS, Dian L, Hanley DA, Kendler DL, Yuen CK and Lewiecki EM:
Bisphosphonate therapy for osteoporosis: Benefits, risks, and drug
holiday. Am J Med. 126:13–20. 2013. View Article : Google Scholar
|
|
97
|
Shane E, Burr D, Abrahamsen B, Adler RA,
Brown TD, Cheung AM, Cosman F, Curtis JR, Dell R, Dempster DW, et
al: Atypical subtrochanteric and diaphyseal femoral fractures:
Second report of a task force of the American society for bone and
mineral research. J Bone Miner Res. 29:1–23. 2014. View Article : Google Scholar
|
|
98
|
Deeks ED: Denosumab: A review in
postmenopausal osteoporosis. Drugs Aging. 35:163–173. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Morin SN, Feldman S, Funnell L,
Giangregorio L, Kim S, McDonald-Blumer H, Santesso N, Ridout R,
Ward W, Ashe MC, et al: Clinical practice guideline for management
of osteoporosis and fracture prevention in Canada: 2023 Update.
CMAJ. 195:E1333–E1348. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Lobo RA, Pickar JH, Stevenson JC, Mack WJ
and Hodis HN: Back to the future: Hormone replacement therapy as
part of a prevention strategy for women at the onset of menopause.
Atherosclerosis. 254:282–290. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Gosset A, Pouillès JM and Trémollieres F:
Menopausal hormone therapy for the management of osteoporosis. Best
Pract Res Clin Endocrinol Metab. 35:1015512021. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Rossouw JE, Anderson GL, Prentice RL,
LaCroix AZ, Kooperberg C, Stefanick ML, Jackson RD, Beresford SA,
Howard BV, Johnson KC, et al: Risks and benefits of estrogen plus
progestin in healthy postmenopausal women: Principal results from
the women's health initiative randomized controlled trial. JAMA.
288:321–333. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Prior JC, Seifert-Klauss VR, Giustini D,
Adachi JD, Kalyan S and Goshtasebi A: Estrogen-progestin therapy
causes a greater increase in spinal bone mineral density than
estrogen therapy-a systematic review and meta-analysis of
controlled trials with direct randomization. J Musculoskelet
Neuronal Interact. 17:146–154. 2017.PubMed/NCBI
|
|
104
|
de Villiers TJ, Hall JE, Pinkerton JV,
Pérez SC, Rees M, Yang C and Pierroz DD: Revised global consensus
statement on menopausal hormone therapy. Maturitas. 91:153–155.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Levin VA, Jiang X and Kagan R: Estrogen
therapy for osteoporosis in the modern era. Osteoporos Int.
29:1049–1055. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Abdi F, Mobedi H, Bayat F, Mosaffa N,
Dolatian M and Ramezani Tehrani F: The effects of transdermal
estrogen delivery on bone mineral density in postmenopausal women:
A meta-analysis. Iran J Pharm Res. 16:380–389. 2017.PubMed/NCBI
|
|
107
|
Mosca L: Rationale and overview of the
raloxifene use for the heart (RUTH) trial. Ann N Y Acad Sci.
949:181–185. 2001. View Article : Google Scholar
|
|
108
|
Ensrud K, Genazzani AR, Geiger MJ, McNabb
M, Dowsett SA, Cox DA and Barrett-Connor E: Effect of raloxifene on
cardiovascular adverse events in postmenopausal women with
osteoporosis. Am J Cardiol. 97:520–527. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Vahle JL, Long GG, Sandusky G, Westmore M,
Ma YL and Sato M: Bone neoplasms in F344 rats given teriparatide
[rhPTH(1-34)] are dependent on duration of treatment and dose.
Toxicol Pathol. 32:426–438. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Andrews EB, Gilsenan AW, Midkiff K,
Sherrill B, Wu Y, Mann BH and Masica D: The US postmarketing
surveillance study of adult osteosarcoma and teriparatide: Study
design and findings from the first 7 years. J Bone Miner Res.
27:2429–2437. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Xie J, Guo J, Kanwal Z, Wu M, Lv X,
Ibrahim NA, Li P, Buabeid MA, Arafa EA and Sun Q: Calcitonin and
bone physiology: In vitro, in vivo, and clinical investigations.
Int J Endocrinol. 2020:32368282020. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Holdsworth G, Roberts SJ and Ke HZ: Novel
actions of sclerostin on bone. J Mol Endocrinol. 62:R167–R185.
2019. View Article : Google Scholar
|
|
113
|
Weaver CM, Alexander DD, Boushey CJ,
Dawson-Hughes B, Lappe JM, LeBoff MS, Liu S, Looker AC, Wallace TC
and Wang DD: Calcium plus vitamin D supplementation and risk of
fractures: An updated meta-analysis from the national osteoporosis
foundation. Osteoporos Int. 27:367–376. 2016. View Article : Google Scholar :
|
|
114
|
Meng J, Zhang W, Wang C, Zhang W, Zhou C,
Jiang G, Hong J, Yan S and Yan W: Catalpol suppresses
osteoclastogenesis and attenuates osteoclast-derived bone
resorption by modulating PTEN activity. Biochem Pharmacol.
171:1137152020. View Article : Google Scholar
|
|
115
|
Ferlazzo N, Andolina G, Cannata A,
Costanzo MG, Rizzo V, Currò M, Ientile R and Caccamo D: Is
melatonin the cornucopia of the 21st century? Antioxidants (Basel).
9:10882020. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Lian C, Wu Z, Gao B, Peng Y, Liang A, Xu
C, Liu L, Qiu X, Huang J, Zhou H, et al: Melatonin reversed tumor
necrosis factor-alpha-inhibited osteogenesis of human mesenchymal
stem cells by stabilizing SMAD1 protein. J Pineal Res. 61:317–327.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Zheng ZG, Cheng HM, Zhou YP, Zhu ST, Thu
PM, Li HJ, Li P and Xu X: Dual targeting of SREBP2 and ERRα by
carnosic acid suppresses RANKL-mediated osteoclastogenesis and
prevents ovariectomy-induced bone loss. Cell Death Differ.
27:2048–2065. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Zheng HL, Xu WN, Zhou WS, Yang RZ, Chen
PB, Liu T, Jiang LS and Jiang SD: Beraprost ameliorates
postmenopausal osteoporosis by regulating Nedd4-induced Runx2
ubiquitination. Cell Death Dis. 12:4972021. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Zhang Y, Wang C, Cao Y, Gu Y and Zhang L:
Selective compounds enhance osteoblastic activity by targeting HECT
domain of ubiquitin ligase Smurf1. Oncotarget. 8:50521–50533. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Ye LC, Qian LF, Liang L, Jiang LJ, Che ZY
and Guo YH: Overexpression of miR-195-5p reduces osteoporosis
through activating BMP-2/SMAD/Akt/RUNX2 pathway via targeting
SMURF1. J Biol Regul Homeost Agents. 35:1201–1216. 2021.
|
|
121
|
Oyajobi BO, Garrett IR, Gupta A, Flores A,
Esparza J, Muñoz S, Zhao M and Mundy GR: Stimulation of new bone
formation by the proteasome inhibitor, bortezomib: implications for
myeloma bone disease. Br J Haematol. 139:434–438. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Uyama M, Sato MM, Kawanami M and Tamura M:
Regulation of osteoblastic differentiation by the proteasome
inhibitor bortezomib. Genes Cells. 17:548–558. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Fang Y, Liu Y, Zhao Z, Lu Y, Shen X, Zhu
T, Hou M, He F, Yang H, Zhang Y, et al: Bortezomib rescues
ovariectomy-induced bone loss via SMURF-mediated ubiquitination
pathway. Oxid Med Cell Longev. 2021:96612002021. View Article : Google Scholar
|
|
124
|
Khedgikar V, Kushwaha P, Gautam J, Verma
A, Changkija B, Kumar A, Sharma S, Nagar GK, Singh D, Trivedi PK,
et al: Withaferin A: A proteasomal inhibitor promotes healing after
injury and exerts anabolic effect on osteoporotic bone. Cell Death
Dis. 4:e7782013. View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Kabekkodu SP, Shukla V, Varghese VK, D'
Souza J, Chakrabarty S and Satyamoorthy K: Clustered miRNAs and
their role in biological functions and diseases. Biol Rev Camb
Philos Soc. 93:1955–1986. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Huang Y, Yang Y, Wang J, Yao S, Yao T, Xu
Y, Chen Z, Yuan P, Gao J, Shen S and Ma J: miR-21-5p targets SKP2
to reduce osteoclastogenesis in a mouse model of osteoporosis. J
Biol Chem. 296:1006172021. View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Liu C, Gao X, Li Y, Sun W, Xu Y, Tan Y, Du
R, Zhong G, Zhao D, Liu Z, et al: The mechanosensitive lncRNA Neat1
promotes osteoblast function through paraspeckle-dependent Smurf1
mRNA retention. Bone Res. 10:182022. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Jiang Y, Wu W, Jiao G, Chen Y and Liu H:
LncRNA SNHG1 modulates p38 MAPK pathway through Nedd4 and thus
inhibits osteogenic differentiation of bone marrow mesenchymal stem
cells. Life Sci. 228:208–214. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Liu L, Jin R, Duan J, Yang L, Cai Z, Zhu
W, Nie Y, He J, Xia C, Gong Q, et al: Bioactive iron oxide
nanoparticles suppress osteoclastogenesis and ovariectomy-induced
bone loss through regulating the TRAF6-p62-CYLD signaling complex.
Acta Biomater. 103:281–292. 2020. View Article : Google Scholar
|
|
130
|
Liu Y, Huang X, He X, Zhou Y, Jiang X,
Chen-Kiang S, Jaffrey SR and Xu G: A novel effect of thalidomide
and its analogs: Suppression of cereblon ubiquitination enhances
ubiquitin ligase function. FASEB J. 29:4829–4839. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Mishima K, Kitoh H, Ohkawara B, Okuno T,
Ito M, Masuda A, Ishiguro N and Ohno K: Lansoprazole upregulates
polyubiquitination of the TNF receptor-associated factor 6 and
facilitates Runx2-mediated osteoblastogenesis. EBioMedicine.
2:2046–2061. 2015. View Article : Google Scholar
|
|
132
|
Li X, Sun W, Li J, Wang M, Zhang H, Pei L,
Boyce BF, Wang Z and Xing L: Clomipramine causes osteoporosis by
promoting osteoclastogenesis via E3 ligase Itch, which is prevented
by zoledronic acid. Sci Rep. 7:413582017. View Article : Google Scholar : PubMed/NCBI
|