|
1
|
Tupchong K, Koyfman A and Foran M: Sepsis,
severe sepsis, and septic shock: A review of the literature. Afr J
Emerg Med. 5:127–135. 2015. View Article : Google Scholar
|
|
2
|
Evans L, Rhodes A, Alhazzani W, Antonelli
M, Coopersmith CM, French C, Machado FR, Mcintyre L, Ostermann M,
Prescott HC, et al: Surviving sepsis campaign: International
guidelines for management of sepsis and septic shock 2021. Crit
Care Med. 49:e1063–e1143. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Matthaeus-Kraemer CT, Thomas-Rueddel DO,
Schwarzkopf D, Rueddel H, Poidinger B, Reinhart K and Bloos F:
Crossing the handover chasm: Clinicians' perceptions of barriers to
the early detection and timely management of severe sepsis and
septic shock. J Crit Care. 36:85–91. 2016. View Article : Google Scholar : PubMed/NCBI
|
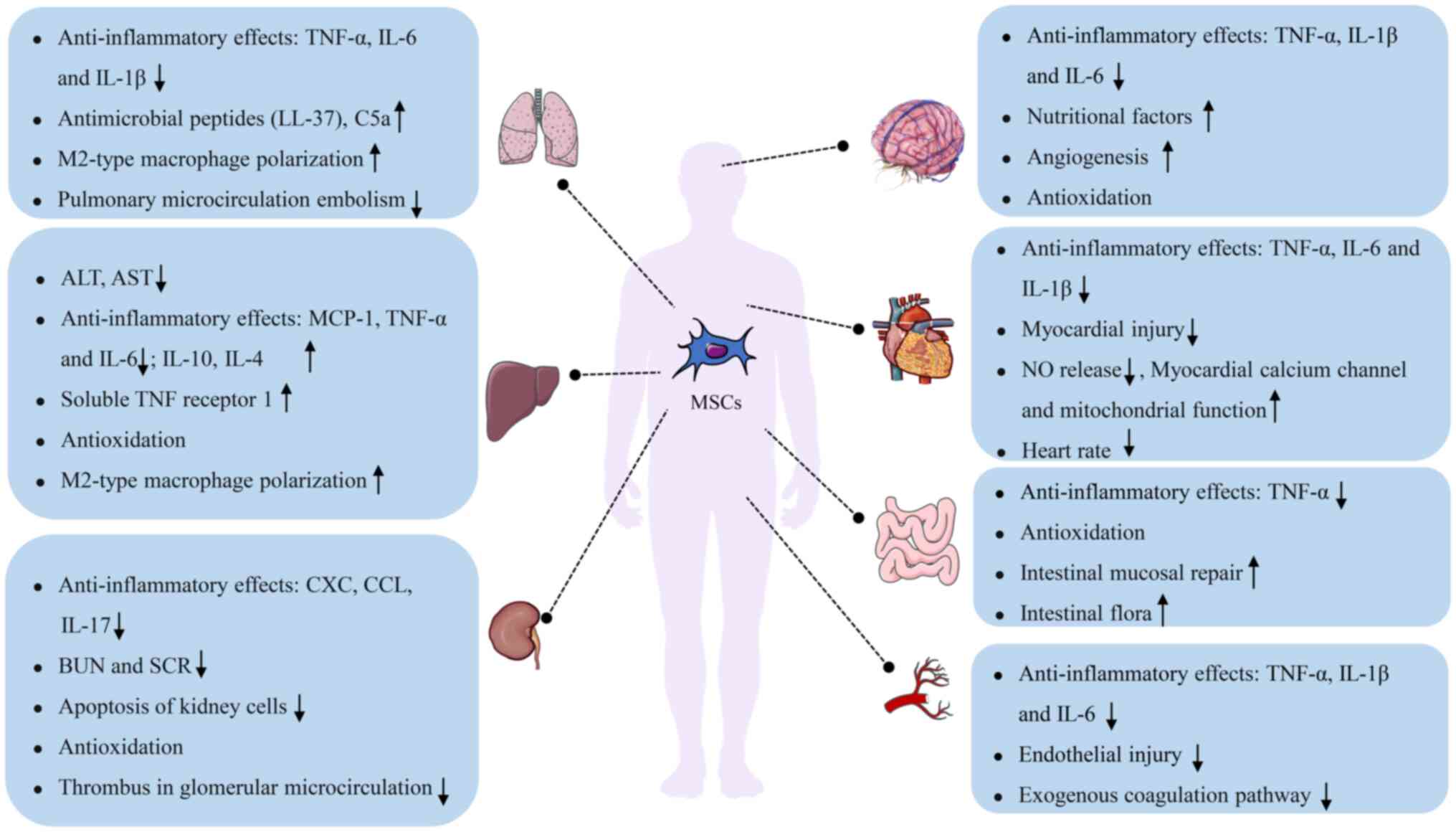
|
4
|
Liu Y, Xu L, Yang Z, Wang D, Li T, Yang F,
Li Z, Bai X and Wang Y: Gut-muscle axis and sepsis-induced
myopathy: The potential role of gut microbiota. Biomed
Pharmacother. 163:1148372023. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mankowski RT, Laitano O, Clanton TL and
Brakenridge SC: Pathophysiology and treatment strategies of acute
myopathy and muscle wasting after sepsis. J Clin Med. 10:18742021.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Callahan LA and Supinski GS:
Sepsis-induced myopathy. Crit Care Med. 37(10 Suppl): S354–S367.
2009. View Article : Google Scholar
|
|
7
|
Schefold JC, Bierbrauer J and
Weber-Carstens S: Intensive care unit-acquired weakness (ICUAW) and
muscle wasting in critically ill patients with severe sepsis and
septic shock. J Cachexia Sarcopenia Muscle. 1:147–157. 2010.
View Article : Google Scholar
|
|
8
|
Liu W, Hu C and Zhao S: Sarcopenia and
mortality risk of patients with sepsis: A meta-analysis. Int J Clin
Pract. 2022:49744102022. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Panahi A, Malekmohammad M, Soleymani F and
Hashemian SM: The prevalence and outcome of intensive care unit
acquired weakness (ICUAW). Tanaffos. 19:250–255. 2020.
|
|
10
|
Dinglas VD, Aronson Friedman L, Colantuoni
E, Mendez-Tellez PA, Shanholtz CB, Ciesla ND, Pronovost PJ and
Needham DM: Muscle weakness and 5-year survival in acute
respiratory distress syndrome survivors. Crit Care Med. 45:446–453.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Meyer-Frießem CH, Malewicz NM, Rath S,
Ebel M, Kaisler M, Tegenthoff M, Schildhauer TA, Pogatzki-Zahn EM,
Maier C and Zahn PK: Incidence, time course and influence on
quality of life of intensive care unit-acquired weakness symptoms
in long-term intensive care survivors. J Intensive Care Med.
36:1313–1322. 2021. View Article : Google Scholar
|
|
12
|
Appleton RT, Kinsella J and Quasim T: The
incidence of intensive care unit-acquired weakness syndromes: A
systematic review. J Intensive Care Soc. 16:126–136. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
de Andrade-Junior MC, de Salles ICD, de
Brito CMM, Pastore-Junior L, Righetti RF and Yamaguti WP: Skeletal
muscle wasting and function impairment in intensive care patients
with severe COVID-19. Front Physiol. 12:6409732021. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Herridge MS, Tansey CM, Matté A, Tomlinson
G, Diaz-Granados N, Cooper A, Guest CB, Mazer CD, Mehta S, Stewart
TE, et al: Functional disability 5 years after acute respiratory
distress syndrome. N Engl J Med. 364:1293–1304. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Odden AJ, Rohde JM, Bonham C, Kuhn L,
Malani PN, Chen LM, Flanders SA and Iwashyna TJ: Functional
outcomes of general medical patients with severe sepsis. BMC Infect
Dis. 13:5882013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zhang J, Huang Y, Chen Y, Shen X, Pan H
and Yu W: Impact of muscle mass on survival in patients with
sepsis: A systematic review and meta-analysis. Ann Nutr Metab.
77:330–336. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
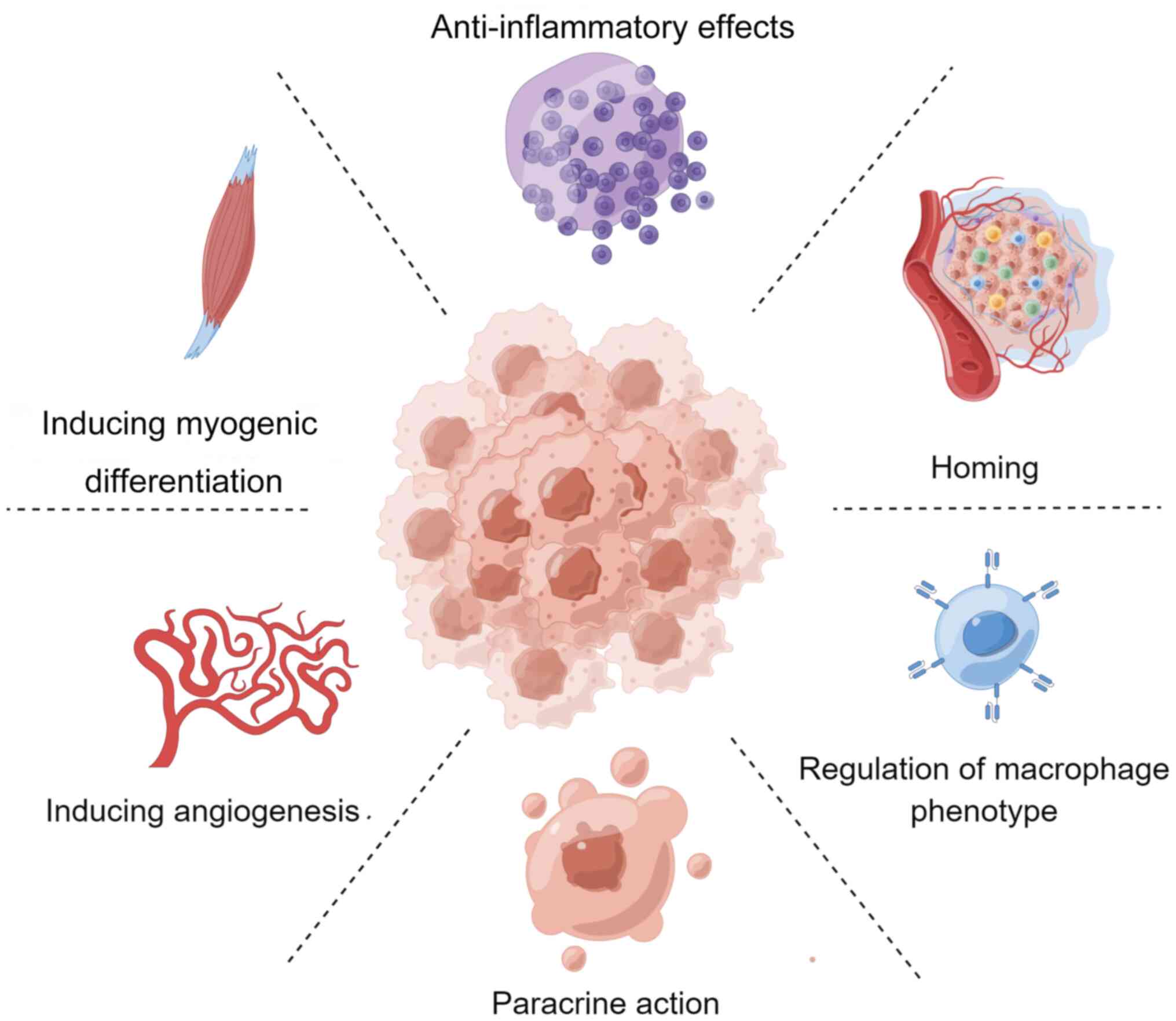
Yan W, Chen Y, Guo Y, Xia Y, Li C, Du Y,
Lin C, Xu X, Qi T, Fan M, et al: Irisin promotes cardiac homing of
intravenously delivered MSCs and protects against ischemic heart
injury. Adv Sci (Weinh). 9:e21036972022. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Gnecchi M, Danieli P and Cervio E:
Mesenchymal stem cell therapy for heart disease. Vascul Pharmacol.
57:48–55. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Tzouvelekis A, Toonkel R, Karampitsakos T,
Medapalli K, Ninou I, Aidinis V, Bouros D and Glassberg MK:
Mesenchymal stem cells for the treatment of idiopathic pulmonary
fibrosis. Front Med (Lausanne). 5:1422018. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Sinclair K, Yerkovich ST and Chambers DC:
Mesenchymal stem cells and the lung. Respirology. 18:397–411. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Ye T, Chen Z, Zhang J, Luo L, Gao R, Gong
L, Du Y, Xie Z, Zhao B, Li Q and Wang Y: Large extracellular
vesicles secreted by human iPSC-derived MSCs ameliorate
tendinopathy via regulating macrophage heterogeneity. Bioact Mater.
21:194–208. 2022.PubMed/NCBI
|
|
22
|
He X, Ai S, Guo W, Yang Y, Wang Z, Jiang D
and Xu X: Umbilical cord-derived mesenchymal stem (stromal) cells
for treatment of severe sepsis: Aphase 1 clinical trial. Transl
Res. 199:52–61. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Cribbs SK and Martin GS: Stem cells in
sepsis and acute lung injury. Am J Med Sci. 341:325–332. 2011.
View Article : Google Scholar
|
|
24
|
Walter J, Ware LB and Matthay MA:
Mesenchymal stem cells: Mechanisms of potential therapeutic benefit
in ARDS and sepsis. Lancet Respir Med. 2:1016–1026. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Khosrojerdi A, Soudi S, Hosseini AZ,
Eshghi F, Shafiee A and Hashemi SM: Immunomodulatory and
therapeutic effects of mesenchymal stem cells on organ dysfunction
in sepsis. Shock. 55:423–440. 2021. View Article : Google Scholar
|
|
26
|
Ho MSH, Mei SHJ and Stewart DJ: The
immunomodulatory and therapeutic effects of mesenchymal stromal
cells for acute lung injury and sepsis. J Cell Physiol.
230:2606–2617. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Friedenstein AJ, Petrakova KV, Kurolesova
AI and Frolova GP: Heterotopic of bone marrow. Analysis of
precursor cells for osteogenic and hematopoietic tissues.
Transplantation. 6:230–247. 1968. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Dominici M, Le Blanc K, Mueller I,
Slaper-Cortenbach I, Marini FC, Krause DS, Deans R, Keating A,
Prockop D and Horwitz E: Minimal criteria for defining multipotent
mesenchymal stromal cells. The International Society for Cellular
Therapy position statement. Cytotherapy. 8:315–317. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Bianco P: 'Mesenchymal' stem cells. Annu
Rev Cell Dev Biol. 30:677–704. 2014. View Article : Google Scholar
|
|
30
|
Rankin S: Mesenchymal stem cells. Thorax.
67:565–566. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Jiang W and Xu J: Immune modulation by
mesenchymal stem cells. Cell Prolif. 53:e127122020. View Article : Google Scholar :
|
|
32
|
Yianni V and Sharpe PT:
Perivascular-derived mesenchymal stem cells. J Dent Res.
98:1066–1072. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Zimmermann JA, Hettiaratchi MH and
McDevitt TC: Enhanced immunosuppression of T cells by sustained
presentation of bioactive interferon-γ within three-dimensional
mesenchymal stem cell constructs. Stem Cells Transl Med. 6:223–237.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Yarygin KN, Lupatov AY and Sukhikh GT:
Modulation of immune responses by mesenchymal stromal cells. Bull
Exp Biol Med. 161:561–565. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Glenn JD and Whartenby KA: Mesenchymal
stem cells: Emerging mechanisms of immunomodulation and therapy.
World J Stem Cells. 6:526–539. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Saeedi P, Halabian R and Fooladi AAI:
Antimicrobial effects of mesenchymal stem cells primed by modified
LPS on bacterial clearance in sepsis. J Cell Physiol.
234:4970–4986. 2019. View Article : Google Scholar
|
|
37
|
Spees JL, Lee RH and Gregory CA:
Mechanisms of mesenchymal stem/stromal cell function. Stem Cell Res
Ther. 7:1252016. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Le Blanc K, Tammik C, Rosendahl K,
Zetterberg E and Ringdén O: HLA expression and immunologic
properties of differentiated and undifferentiated mesenchymal stem
cells. Exp Hematol. 31:890–896. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Uccelli A, Moretta L and Pistoia V:
Mesenchymal stem cells in health and disease. Nat Rev Immunol.
8:726–736. 2008. View Article : Google Scholar
|
|
40
|
Minguell JJ, Conget P and Erices A:
Biology and clinical utilization of mesenchymal progenitor cells.
Braz J Med Biol Res. 33:881–887. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Kim WY and Hong SB: Sepsis and acute
respiratory distress syndrome: Recent update. Tuberc Respir Dis
(Seoul). 79:53–57. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Martin GS and Bernard GR: Airway and lung
in sepsis. Intensive Care Med. 27(Suppl 1): S63–S79. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Davis C: Risk factors for the development
of acute lung injury in patients with septic shock: An
observational cohort study. J Emerg Med. 36:P982009. View Article : Google Scholar
|
|
44
|
Schmidt EP, Yang Y, Janssen WJ, Gandjeva
A, Perez MJ, Barthel L, Zemans RL, Bowman JC, Koyanagi DE, Yunt ZX,
et al: The pulmonary endothelial glycocalyx regulates neutrophil
adhesion and lung injury during experimental sepsis. Nat Med.
18:1217–1223. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Lee WL and Slutsky AS: Sepsis and
endothelial permeability. N Engl J Med. 363:689–691. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Lomas-Neira J, Perl M, Venet F, Chung CS
and Ayala A: The role and source of tumor necrosis factor-α in
hemorrhage-induced priming for septic lung injury. Shock.
37:611–620. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Wang L, Taneja R, Razavi HM, Law C, Gillis
C and Mehta S: Specific role of neutrophil inducible nitric oxide
synthase in murine sepsis-induced lung injury in vivo. Shock.
37:539–547. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Grover SP and Mackman N: Tissue factor: An
essential mediator of hemostasis and trigger of thrombosis.
Arterioscler Thromb Vasc Biol. 38:709–725. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Witkowski M, Landmesser U and Rauch U:
Tissue factor as a link between inflammation and coagulation.
Trends Cardiovasc Med. 26:297–303. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Evans CE and Zhao YY: Impact of thrombosis
on pulmonary endothelial injury and repair following sepsis. Am J
Physiol Lung Cell Mol Physiol. 312:L441–L451. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Zhao Y, Yang C, Wang H, Li H, Du J, Gu W
and Jiang J: Therapeutic effects of bone marrow-derived mesenchymal
stem cells on pulmonary impact injury complicated with endotoxemia
in rats. Int Immunopharmacol. 15:246–253. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Lee FY, Chen KH, Wallace CG, Sung PH, Sheu
JJ, Chung SY, Chen YL, Lu HI, Ko SF, Sun CK, et al: Xenogeneic
human umbilical cord-derived mesenchymal stem cells reduce
mortality in rats with acute respiratory distress syndrome
complicated by sepsis. Oncotarget. 8:45626–45642. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Asami T, Ishii M, Namkoong H, Yagi K,
Tasaka S, Asakura T, Suzuki S, Kamo T, Okamori S, Kamata H, et al:
Anti-inflammatory roles of mesenchymal stromal cells during acute
Streptococcus pneumoniae pulmonary infection in mice. Cytotherapy.
20:302–313. 2017. View Article : Google Scholar
|
|
54
|
Chen HH, Chang CL, Lin KC, Sung PH, Chai
HT, Zhen YY, Chen YC, Wu YC, Leu S, Tsai TH, et al: Melatonin
augments apoptotic adipose-derived mesenchymal stem cell treatment
against sepsis-induced acute lung injury. Am J Transl Res.
6:439–458. 2014.PubMed/NCBI
|
|
55
|
Li W, Chen W, Huang S, Tang X, Yao G and
Sun L: Mesenchymal stem cells enhance pulmonary antimicrobial
immunity and prevent following bacterial infection. Stem Cells Int.
2020:31694692020. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Krasnodembskaya A, Song Y, Fang X, Gupta
N, Serikov V, Lee JW and Matthay MA: Antibacterial effect of human
mesenchymal stem cells is mediated in part from secretion of the
antimicrobial peptide LL-37. Stem Cells. 28:2229–2238. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Rabani R, Volchuk A, Jerkic M, Ormesher L,
Garces-Ramirez L, Canton J, Masterson C, Gagnon S, Tatham KC,
Marshall J, et al: Mesenchymal stem cells enhance NOX2-dependent
reactive oxygen species production and bacterial killing in
macrophages during sepsis. Eur Respir J. 51:17020212018. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Yao M, Cui B, Zhang W, Ma W, Zhao G and
Xing L: Exosomal miR-21 secreted by IL-1β-primed-mesenchymal stem
cells induces macrophage M2 polarization and ameliorates sepsis.
Life Sci. 264:1186582021. View Article : Google Scholar
|
|
59
|
Krasnodembskaya A, Samarani G, Song Y,
Zhuo H, Su X, Lee JW, Gupta N, Petrini M and Matthay MA: Human
mesenchymal stem cells reduce mortality and bacteremia in
gram-negative sepsis in mice in part by enhancing the phagocytic
activity of blood monocytes. Am J Physiol Lung Cell Mol Physiol.
302:L1003–L1013. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Tan L, Huang Y, Pan X, Quan S, Xu S, Li D,
Song L, Zhang X, Chen W and Pan J: Administration of bone marrow
stromal cells in sepsis attenuates sepsis-related coagulopathy. Ann
Med. 48:235–245. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Dos Santos CC, Amatullah H, Vaswani CM,
Maron-Gutierrez T, Kim M, Mei SHJ, Szaszi K, Monteiro APT, Varkouhi
AK, Herreroz R, et al: Mesenchymal stromal (stem) cell therapy
modulates miR-193b-5p expression to attenuate sepsis-induced acute
lung injury. Eur Respir J. 59:20042162022. View Article : Google Scholar
|
|
62
|
Younes N, Zhou L, Amatullah H, Mei SHJ,
Herrero R, Lorente JA, Stewart DJ, Marsden P, Liles WC, Hu P and
Dos Santos CC: Mesenchymal stromal/stem cells modulate response to
experimental sepsis-induced lung injury via regulation of
miR-27a-5p in recipient mice. Thorax. 75:556–567. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Bi CF, Liu J, Yang LS and Zhang JF:
Research progress on the mechanism of sepsis induced myocardial
injury. J Inflamm Res. 15:4275–4290. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Aneman A and Vieillard-Baron A: Cardiac
dysfunction in sepsis. Intensive Care Med. 42:2073–2076. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Rudiger A and Singer M: Mechanisms of
sepsis-induced cardiac dysfunction. Crit Care Med. 35:1599–1608.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Kumar A, Thota V, Dee L, Olson J, Uretz E
and Parrillo JE: Tumor necrosis factor alpha and interleukin 1beta
are responsible for in vitro myocardial cell depression induced by
human septic shock serum. Resuscitation. 32:P1661996. View Article : Google Scholar
|
|
67
|
Zhang X, Lu C, Gao M, Cao X, Ha T,
Kalbfleisch JH, Williams DL, Li C and Kao RL: Toll-like receptor 4
plays a central role in cardiac dysfunction during trauma
hemorrhage shock. Shock. 42:31–37. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Sato R and Nasu M: A review of
sepsis-induced cardiomyopathy. J Intensive Care. 3:482015.
View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Stengl M, Bartak F, Sykora R, Chvojka J,
Benes J, Krouzecky A, Novak I, Sviglerova J, Kuncova J and
Matejovic M: Reduced L-type calcium current in ventricular myocytes
from pigs with hyperdynamic septic shock. Crit Care Med.
38:579–587. 2010. View Article : Google Scholar
|
|
70
|
Kumar A, Brar R, Wang P, Dee L, Skorupa G,
Khadour F, Schulz R and Parrillo JE: Role of nitric oxide and cGMP
in human septic serum-induced depression of cardiac myocyte
contractility. Am J Physiol. 276:R265–R276. 1999.PubMed/NCBI
|
|
71
|
Lv X and Wang H: Pathophysiology of
sepsis-induced myocardial dysfunction. Mil Med Res.
3:302016.PubMed/NCBI
|
|
72
|
Wu Y, Zhou J, Bi L, Huang M, Han Y, Zhang
Q, Zhu D and Zhou S: Effects of bone marrow mesenchymal stem cells
on the cardiac function and immune system of mice with endotoxemia.
Mol Med Rep. 13:5317–5325. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Weil BR, Herrmann JL, Abarbanell AM,
Manukyan MC, Poynter JA and Meldrum DR: Intravenous infusion of
mesenchymal stem cells is associated with improved myocardial
function during endotoxemia. Shock. 36:235–241. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Wang X, Huang W, Wang Y and Fan GC:
Abstract 12290: Exosomal miR-223 contributes to mesenchymal stem
cell-elicited cardio-protection in polymicrobial sepsis.
Circulation. 1322015.
|
|
75
|
Giovannini I, Chiarla C, Giuliante F,
Vellone M, Ardito F and Nuzzo G: Sepsis-induced cholestasis.
Hepatology. 47:3612008. View Article : Google Scholar
|
|
76
|
Woźnica EA, Inglot M, Woźnica RK and
Łysenko L: Liver dysfunction in sepsis. Adv Clin Exp Med.
27:547–551. 2018. View Article : Google Scholar
|
|
77
|
Gaddam RR, Fraser R, Badiei A, Chambers S,
Cogger VC, Le Couteur DG and Bhatia M: Differential effects of
kupffer cell inactivation on inflammation and the liver sieve
following caecal-ligation and puncture-induced sepsis in mice.
Shock. 47:480–490. 2017. View Article : Google Scholar
|
|
78
|
Wang H and Liu D: Baicalin inhibits
high-mobility group box 1 release and improves survival in
experimental sepsis. Shock. 41:324–330. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Wang D, Yin Y and Yao Y: Advances in
sepsis-associated liver dysfunction. Burns Trauma. 2:97–105. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Yagi H, Soto-Gutierrez A, Kitagawa Y,
Tilles AW, Tompkins RG and Yarmush ML: Bone marrow mesenchymal
stromal cells attenuate organ injury induced by LPS and burn. Cell
Transplant. 19:823–830. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Wu KH, Wu HP, Chao WR, Lo WY, Tseng PC,
Lee CJ, Peng CT, Lee MS and Chao YH: Time-series expression of
toll-like receptor 4 signaling in septic mice treated with
mesenchymal stem cells. Shock. 45:634–640. 2016. View Article : Google Scholar
|
|
82
|
Miao CM, Jiang XW, He K, Li PZ, Liu ZJ,
Cao D, Ou ZB, Gong JP, Liu CA and Cheng Y: Bone marrow stromal
cells attenuate LPS-induced mouse acute liver injury via the
prostaglandin E 2-dependent repression of the NLRP3 inflammasome in
Kupffer cells. Immunol Lett. 179:102–113. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Yagi H, Soto-Gutierrez A, Navarro-Alvarez
N, Nahmias Y, Goldwasser Y, Kitagawa Y, Tilles AW, Tompkins RG,
Parekkadan B and Yarmush ML: Reactive bone marrow stromal cells
attenuate systemic inflammation via sTNFR1. Mol Ther. 18:1857–1864.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Liang H, Ding X, Yu Y, Zhang H, Wang L,
Kan Q, Ma S, Guan F and Sun T: Adipose-derived mesenchymal stem
cells ameliorate acute liver injury in rat model of CLP
induced-sepsis via sTNFR1. Exp Cell Res. 383:1114652019. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Umbro I, Gentile G, Tinti F, Muiesan P and
Mitterhofer AP: Recent advances in pathophysiology and biomarkers
of sepsis-induced acute kidney injury. J Infect. 72:131–142. 2016.
View Article : Google Scholar
|
|
86
|
Gómez H and Kellum JA: Sepsis-induced
acute kidney injury. Curr Opin Crit Care. 22:546–553. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Zarjou A and Agarwal A: Sepsis and acute
kidney injury. J Am Soc Nephrol. 22:999–1006. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Yoshimoto K, Komaru Y, Iwagami M and Doi
K: Acute kidney injury in sepsis: Evidence from Asia. Semin
Nephrol. 40:489–497. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Manrique-Caballero CL, Del Rio-Pertuz G
and Gomez H: Sepsis-associated acute kidney injury. Crit Care Clin.
37:279–301. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Bellomo R, Kellum JA, Ronco C, Wald R,
Martensson J, Maiden M, Bagshaw SM, Glassford NJ, Lankadeva Y,
Vaara ST and Schneider A: Acute kidney injury in sepsis. Intensive
Care Med. 43:816–828. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Luo CJ, Zhang FJ, Zhang L, Geng YQ, Li QG,
Hong Q, Fu B, Zhu F, Cui SY, Feng Z, et al: Mesenchymal stem cells
ameliorate sepsis-associated acute kidney injury in mice. Shock.
41:123–129. 2014. View Article : Google Scholar
|
|
92
|
Cóndor JM, Rodrigues CE, Sousa Moreira RD,
Canale D, Volpini RA, Shimizu MH, Camara NO, Noronha Ide L and
Andrade L: Treatment with human Wharton's Jelly-derived mesenchymal
stem cells attenuates sepsis-induced kidney injury, liver injury,
and endothelial dysfunction. Stem Cells Transl Med. 5:1048–1057.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Chen CH, Cheng BC, Chen KH, Shao PL, Sung
PH, Chiang HJ, Yang CC, Lin KC, Sun CK, Sheu JJ, et al: Combination
therapy of exendin-4 and allogenic adipose-derived mesenchymal stem
cell preserved renal function in a chronic kidney disease and
sepsis syndrome setting in rats. Oncotarget. 8:100002–100020. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Chen HH, Lin KC, Wallace CG, Chen YT, Yang
CC, Leu S, Chen YC, Sun CK, Tsai TH, Chen YL, et al: Additional
benefit of combined therapy with melatonin and apoptotic
adipose-derived mesenchymal stem cell against sepsis-induced kidney
injury. J Pineal Res. 57:16–32. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Polito A, Eischwald F, Maho AL, Polito A,
Azabou E, Annane D, Chrétien F, Stevens RD, Carlier R and Sharshar
T: Pattern of brain injury in the acute setting of human septic
shock. Crit Care. 17:R2042013. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Catarina AV, Branchini G, Bettoni L, De
Oliveira JR and Nunes FB: Sepsis-associated encephalopathy: From
pathophysiology to progress in experimental studies. Mol Neurobiol.
58:2770–2779. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Prescott HC and Angus DC: Enhancing
recovery from sepsis: A review. JAMA. 319:62–75. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Oh SH, Choi C, Chang DJ, Shin DA, Lee N,
Jeon I, Sung JH, Lee H, Hong KS, Ko JJ and Song J: Early
neuroprotective effect with lack of long-term cell replacement
effect on experimental stroke after intra-arterial transplantation
of adipose-derived mesenchymal stromal cells. Cytotherapy.
17:1090–1103. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Jiang W, Liang G, Li X, Li Z, Gao X, Feng
S, Wang X, Liu M and Liu Y: Intracarotid transplantation of
autologous adipose-derived mesenchymal stem cells significantly
improves neurological deficits in rats after MCAo. J Mater Sci
Mater Med. 25:1357–1366. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Huang P, Gebhart N, Richelson E, Brott TG,
Meschia JF and Zubair AC: Mechanism of mesenchymal stem
cell-induced neuron recovery and anti-inflammation. Cytotherapy.
16:1336–1344. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Yoo SW, Chang DY, Lee HS, Kim GH, Park JS,
Ryu BY, Joe EH, Lee YD, Kim SS and Suh-Kim H: Immune following
suppression mesenchymal stem cell transplantation in the ischemic
brain is mediated by TGF-β. Neurobiol Dis. 58:249–257. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Redondo-Castro E, Cunningham C, Miller J,
Martuscelli L, Aoulad-Ali S, Rothwell NJ, Kielty CM, Allan SM and
Pinteaux E: Interleukin-1 primes human mesenchymal stem cells
towards an anti-inflammatory and pro-trophic phenotype in vitro.
Stem Cell Res Ther. 8:792017. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Tan L, Cheng Y, Wang H, Tong J and Qin X:
Peripheral transplantation of mesenchymal stem cells at sepsis
convalescence improves cognitive function of sepsis surviving mice.
Oxid Med Cell Longev. 2022:68977652022. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Silva AYO, Amorim ÉA, Barbosa-Silva MC,
Lima MN, Oliveira HA, Granja MG, Oliveira KS, Fagundes PM, Neris
RLS, Campos RMP, et al: Mesenchymal stromal cells protect the
blood-brain barrier, reduce astrogliosis, and prevent cognitive and
behavioral alterations in surviving septic mice. Crit Care Med.
48:e290–e298. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Li X, Zheng W, Bai H, Wang J, Wei R, Wen H
and Ning H: Intravenous administration of adipose tissue-derived
stem cells enhances nerve healing and promotes BDNF expression via
the TrkB signaling in a rat stroke model. Neuropsychiatr Dis Treat.
12:1287–1293. 2016.PubMed/NCBI
|
|
106
|
Han C, Song L, Liu Y, Zou W, Jiang C and
Liu J: Rat cortex and hippocampus-derived soluble factors for the
induction of adipose-derived mesenchymal stem cells into
neuron-like cells. Cell Biol Int. 38:768–776. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Gutiérrez-Fernández M, Rodriguez-Frutos B,
Ramos-Cejudo J, Otero-Ortega L, Fuentes B, Vallejo-Cremades MT,
Sanz-Cuesta BE and Díez-Tejedor E: Comparison between xenogeneic
and allogeneic adipose mesenchymal stem cells in the treatment of
acute cerebral infarct: Proof of concept in rats. J Transl Med.
13:462015. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Ribeiro CA, Fraga JS, Grãos M, Neves NM,
Reis RL, Gimble JM, Sousa N and Salgado AJ: The secretome of stem
cells isolated from the adipose tissue and Wharton jelly acts
differently on central nervous system derived cell populations.
Stem Cell Res Ther. 3:182012. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Mahrouf-Yorgov M, Augeul L, Da Silva CC,
Jourdan M, Rigolet M, Manin S, Ferrera R, Ovize M, Henry A, Guguin
A, et al: Mesenchymal stem cells sense mitochondria released from
damaged cells as danger signals to activate their rescue
properties. Cell Death Differ. 24:1224–1238. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Liu J, Huang Y, He J, Zhuo Y, Chen W, Ge
L, Duan D, Lu M and Hu Z: Olfactory mucosa mesenchymal stem cells
ameliorate cerebral ischemic/reperfusion injury through modulation
of UBIAD1 expression. Front Cell Neurosci. 14:5802062020.
View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Cao D, Qiao H, He D, Qin X, Zhang Q and
Zhou Y: Mesenchymal stem cells inhibited the inflammation and
oxidative stress in LPS-activated microglial cells through AMPK
pathway. J Neural Transm (Vienna). 126:1589–1597. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Wang SS, Jia J and Wang Z: Mesenchymal
stem cell-derived extracellular vesicles suppresses iNOS expression
and ameliorates neural impairment in Alzheimer's disease mice. J
Alzheimers Dis. 61:1005–1013. 2018. View Article : Google Scholar
|
|
113
|
Cai G, Cai G, Zhou H, Zhuang Z, Liu K, Pei
S, Wang Y, Wang H, Wang X, Xu S, et al: Mesenchymal stem
cell-derived exosome miR-542-3p suppresses inflammation and
prevents cerebral infarction. Stem Cell Res Ther. 12:22021.
View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Fleischmann-Struzek C, Mellhammar L, Rose
N, Cassini A, Rudd KE, Schlattmann P, Allegranzi B and Reinhart K:
Incidence and mortality of hospital- and ICU-treated sepsis:
Results from an updated and expanded systematic review and
meta-analysis. Intensive Care Med. 46:1552–1562. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Aggarwal S and Pittenger MF: Human
mesenchymal stem cells modulate allogeneic immune cell responses.
Blood. 105:1815–1822. 2005. View Article : Google Scholar
|
|
116
|
Li YP, Paczesny S, Lauret E, Poirault S,
Bordigoni P, Mekhloufi F, Hequet O, Bertrand Y, Ou-Yang JP, Stoltz
JF, et al: Human mesenchymal stem cells license adult CD34+
hemopoietic progenitor cells to differentiate into regulatory
dendritic cells through activation of the Notch pathway. J Immunol.
180:1598–1608. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Chen X, Zhang Y, Wang W, Liu Z, Meng J and
Han Z: Mesenchymal stem cells modified with heme oxygenase-1 have
enhanced paracrine function and attenuate
lipopolysaccharide-induced inflammatory and oxidative damage in
pulmonary microvascular endothelial cells. Cell Physiol Biochem.
49:101–122. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Koliaraki V, Pallangyo CK, Greten FR and
Kollias G: Mesenchymal cells in colon cancer. Gastroenterology.
152:964–979. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Parikh SM, Yang Y, He L, Tang C, Zhan M
and Dong Z: Mitochondrial function and disturbances in the septic
kidney. Semin Nephrol. 35:108–119. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Zheng K, Chen S and Hu X: Peroxisome
proliferator-activated receptor gamma coactivator-1 alpha: A
double-edged sword in prostate cancer. Curr Cancer Drug Targets.
22:541–559. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Zheng D, Zhou H, Wang H, Zhu Y, Wu Y, Li
Q, Li T and Liu L: Mesenchymal stem cell-derived microvesicles
improve intestinal barrier function by restoring mitochondrial
dynamic balance in sepsis rats. Stem Cell Res Ther. 12:2992021.
View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Phinney DG, Di Giuseppe M, Njah J, Sala E,
Shiva S, St Croix CM, Stolz DB, Watkins SC, Di YP, Leikauf GD, et
al: Mesenchymal stem cells use extracellular vesicles to outsource
mitophagy and shuttle microRNAs. Nat Commun. 6:84722015. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Weber D, Hiergeist A, Weber M, Dettmer K,
Wolff D, Hahn J, Herr W, Gessner A and Holler E: Detrimental effect
of broad-spectrum antibiotics on intestinal microbiome diversity in
patients after allogeneic stem cell transplantation: Lack of
commensal sparing antibiotics. Clin Infect Dis. 68:1303–1310. 2019.
View Article : Google Scholar
|
|
124
|
Valcz G, Krenács T, Sipos F, Leiszter K,
Tóth K, Balogh Z, Csizmadia A, Muzes G, Molnár B and Tulassay Z:
The role of the bone marrow derived mesenchymal stem cells in
colonic epithelial regeneration. Pathol Oncol Res. 17:11–16. 2011.
View Article : Google Scholar
|
|
125
|
Hayashi Y, Tsuji S, Tsujii M, Nishida T,
Ishii S, Iijima H, Nakamura T, Eguchi H, Miyoshi E, Hayashi N and
Kawano S: Topical implantation of mesenchymal stem cells has
beneficial effects on healing of experimental colitis in rats. J
Pharmacol Exp Ther. 326:523–531. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Nagashima K, Sawa S, Nitta T, Tsutsumi M,
Okamura T, Penninger JM, Nakashima T and Takayanagi H:
Identification of subepithelial mesenchymal cells that induce IgA
and diversify gut microbiota. Nat Immunol. 18:675–682. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Levi M: Current understanding of
disseminated intravascular coagulation. Br J Haematol. 124:567–576.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Levi M, de Jonge E and van der Poll T:
Sepsis and disseminated intravascular coagulation. J Thromb
Thrombolysis. 16:43–47. 2003. View Article : Google Scholar
|
|
129
|
Semeraro N, Ammollo CT, Semeraro F and
Colucci M: Coagulopathy of acute sepsis. Semin Thromb Hemost.
41:650–658. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Wang B, Wu S, Wang T, Ma Z and Liu K: Bone
marrow-derived mesenchymal stem cells-mediated protection against
organ dysfunction in disseminated intravascular coagulation is
associated with peripheral immune responses. J Cell Biochem.
118:3184–3192. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Wang B, Wu SM, Wang T, Liu K, Zhang G,
Zhang XQ, Yu JH, Liu CZ and Fang CC: Pre-treatment with bone
marrow-derived mesenchymal stem cells inhibits systemic
intravascular coagulation and attenuates organ dysfunction in
lipopolysaccharide-induced disseminated intravascular coagulation
rat model. Chin Med J (Engl). 125:1753–1759. 2012.PubMed/NCBI
|
|
132
|
Baudry N, Starck J, Aussel C, Lund K,
Aletti M, Duranteau J, Banzet S, Lataillade JJ, Vicaut E and
Peltzer J: Effect of preconditioned mesenchymal stromal cells on
early microvascular disturbance in a mouse sepsis model. Stem Cells
Dev. 28:1595–1606. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Ye Q, Qiu X, Wang J, Xu B, Su Y, Zheng C,
Gui L, Yu L, Kuang H, Liu H, et al: MSCs-derived apoptotic
extracellular vesicles promote muscle regeneration by inducing
Pannexin 1 channel-dependent creatine release by myoblasts. Int J
Oral Sci. 15:72023. View Article : Google Scholar : PubMed/NCBI
|
|
134
|
Sassoli C, Zecchi-Orlandini S and Formigli
L: Trophic actions of bone marrow-derived mesenchymal stromal cells
for muscle repair/regeneration. Cells. 1:832–850. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
135
|
Gang EJ, Bosnakovski D, Simsek T, To K and
Perlingeiro RCR: Pax3 activation promotes the differentiation of
mesenchymal stem cells toward the myogenic lineage. Exp Cell Res.
314:1721–1733. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Dezawa M, Ishikawa H, Itokazu Y, Yoshihara
T, Hoshino M, Takeda SI, Ide C and Nabeshima YI: Bone marrow
stromal cells generate muscle cells and repair muscle degeneration.
Science. 309:314–317. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
137
|
Haghighipour N, Heidarian S, Shokrgozar MA
and Amirizadeh N: Differential effects of cyclic uniaxial stretch
on human mesenchymal stem cell into skeletal muscle cell. Cell Biol
Int. 36:669–675. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Ninagawa NT, Isobe E, Hirayama Y, Murakami
R, Komatsu K, Nagai M, Kobayashi M, Kawabata Y and Torihashi S:
Transplantated mesenchymal stem cells derived from embryonic stem
cells promote muscle regeneration and accelerate functional
recovery of injured skeletal muscle. Biores Open Access. 2:295–306.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
139
|
Natsu K, Ochi M, Mochizuki Y, Hachisuka H,
Yanada S and Yasunaga Y: Allogeneic bone marrow-derived mesenchymal
stromal cells promote the regeneration of injured skeletal muscle
without differentiation into myofibers. Tissue Eng. 10:1093–1112.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
140
|
Winkler T, von Roth P, Matziolis G, Mehta
M, Perka C and Duda GN: Dose-response relationship of mesenchymal
stem cell transplantation and functional regeneration after severe
skeletal muscle injury in rats. Tissue Eng Part A. 15:487–492.
2009. View Article : Google Scholar
|
|
141
|
Winkler T, von Roth P, Radojewski P,
Urbanski A, Hahn S, Preininger B, Duda GN and Perka C: Immediate
and delayed transplantation of mesenchymal stem cells improve
muscle force after skeletal muscle injury in rats. J Tissue Eng
Regen Med. 6(Suppl 3): s60–s67. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
142
|
von Roth P, Duda GN, Radojewski P,
Preininger B, Perka C and Winkler T: Mesenchymal stem cell therapy
following muscle trauma leads to improved muscular regeneration in
both male and female rats. Gend Med. 9:129–136. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
143
|
Meregalli M, Farini A, Belicchi M,
Parolini D, Cassinelli L, Razini P, Sitzia C and Torrente Y:
Perspectives of stem cell therapy in Duchenne muscular dystrophy.
FEBS J. 280:4251–4262. 2013. View Article : Google Scholar
|
|
144
|
Jiang J, Yao P, Gu Y, Xu L, Xu J and Tan
H: Adult rat mesenchymal stem cells delay denervated muscle
atrophy. Cell Mol Neurobiol. 32:1287–1298. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
145
|
Merritt EK, Cannon MV, Hammers DW, Le LN,
Gokhale R, Sarathy A, Song TJ, Tierney MT, Suggs LJ, Walters TJ and
Farrar RP: Repair of traumatic skeletal muscle injury with
bone-marrow-derived mesenchymal stem cells seeded on extracellular
matrix. Tissue Eng Part A. 16:2871–2881. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
146
|
Stana F, Vujovic M, Mayaki D, Leduc-Gaudet
JP, Leblanc P, Huck L and Hussain SNA: Differential regulation of
the autophagy and proteasome pathways in skeletal muscles in
sepsis. Crit Care Med. 45:e971–e979. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
147
|
Khalil R: Ubiquitin-proteasome pathway and
muscle atrophy. Adv Exp Med Biol. 1088:235–248. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
148
|
Peruchi BB, Petronilho F, Rojas HA,
Constantino L, Mina F, Vuolo F, Cardoso MR, Gonçalves CL, Rezin GT,
Streck EL and Dal-Pizzol F: Skeletal muscle electron transport
chain dysfunction after sepsis in rats. J Surg Res. 167:e333–e338.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
149
|
Thoma A and Lightfoot AP: NF-kB and
inflammatory cytokine signalling: Role in skeletal muscle atrophy.
Adv Exp Med Biol. 1088:267–279. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
150
|
Pelosi M, De Rossi M, Barberi L and Musarò
A: IL-6 impairs myogenic differentiation by downmodulation of
p90RSK/eEF2 and mTOR/p70S6K axes, without affecting AKT activity.
Biomed Res Int. 2014:2060262014. View Article : Google Scholar : PubMed/NCBI
|
|
151
|
Zhu S, Nagashima M, Khan MAS, Yasuhara S,
Kaneki M and Martyn JAJ: Lack of caspase-3 attenuates
immobilization-induced muscle atrophy and loss of tension
generation along with mitigation of apoptosis and inflammation.
Muscle Nerve. 47:711–721. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
152
|
Okamura LH, Cordero P, Palomino J,
Parraguez VH, Torres CG and Peralta OA: Myogenic differentiation
potential of mesenchymal stem cells derived from fetal bovine bone
marrow. Anim Biotechnol. 29:1–11. 2018. View Article : Google Scholar
|
|
153
|
Orlic D, Kajstura J, Chimenti S, Jakoniuk
I, Anderson SM, Li B, Pickel J, McKay R, Nadal-Ginard B, Bodine DM,
et al: Bone marrow cells regenerate infarcted myocardium. Nature.
410:701–705. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
154
|
Egusa H, Kobayashi M, Matsumoto T, Sasaki
J, Uraguchi S and Yatani H: Application of cyclic strain for
accelerated skeletal myogenic differentiation of mouse bone
marrow-derived mesenchymal stromal cells with cell alignment.
Tissue Eng Part A. 19:770–782. 2013. View Article : Google Scholar
|
|
155
|
Drost AC, Weng S, Feil G, Schäfer J,
Baumann S, Kanz L, Sievert KD, Stenzl A and Möhle R: In vitro
myogenic differentiation of human bone marrow-derived mesenchymal
stem cells as a potential treatment for urethral sphincter muscle
repair. Ann N Y Acad Sci. 1176:135–143. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
156
|
Maeda Y, Yonemochi Y, Nakajyo Y, Hidaka H,
Ikeda T and Ando Y: CXCL12 and osteopontin from bone marrow-derived
mesenchymal stromal cells improve muscle regeneration. Sci Rep.
7:33052017. View Article : Google Scholar : PubMed/NCBI
|
|
157
|
Wakitani S, Saito T and Caplan AI:
Myogenic cells derived from rat bone marrow mesenchymal stem cells
exposed to 5-azacytidine. Muscle Nerve. 18:1417–1426. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
158
|
Meligy FY, Shigemura K, Behnsawy HM,
Fujisawa M, Kawabata M and Shirakawa T: The efficiency of in vitro
isolation and myogenic differentiation of MSCs derived from adipose
connective tissue, bone marrow, and skeletal muscle tissue. In
Vitro Cell Dev Biol Anim. 48:203–215. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
159
|
Asakura A: Stem cells in adult skeletal
muscle. rends Cardiovasc Med. 13:123–128. 2003. View Article : Google Scholar
|
|
160
|
Dumont NA, Wang YX and Rudnicki MA:
Intrinsic and extrinsic mechanisms regulating satellite cell
function. Development. 142:1572–1581. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
161
|
Thomas K, Engler AJ and Meyer GA:
Extracellular matrix regulation in the muscle satellite cell niche.
Connect Tissue Res. 56:1–8. 2015. View Article : Google Scholar :
|
|
162
|
Tonkin J, Temmerman L, Sampson RD,
Gallego-Colon E, Barberi L, Bilbao D, Schneider MD, Musarò A and
Rosenthal N: Monocyte/macrophage-derived IGF-1 orchestrates murine
skeletal muscle regeneration and modulates autocrine polarization.
Mol Ther. 23:1189–1200. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
163
|
Karp JM and Teo GSL: Mesenchymal stem cell
homing: The devil is in the details. Cell Stem Cell. 4:206–216.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
164
|
Zhou Q, Yang C and Yang P: The promotional
effect of mesenchymal stem cell homing on bone tissue regeneration.
Curr Stem Cell Res Ther. 12:365–376. 2017. View Article : Google Scholar
|
|
165
|
Ringe J, Strassburg S, Neumann K, Endres
M, Notter M, Burmester GR, Kaps C and Sittinger M: Towards in situ
tissue repair: Human mesenchymal stem cells express chemokine
receptors CXCR1, CXCR2 and CCR2, and migrate upon stimulation with
CXCL8 but not CCL2. J Cell Biochem. 101:135–146. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
166
|
Chen L, Li Y, Chen W, Han N, Li K, Guo R,
Liu Z and Xiao Y: Enhanced recruitment and hematopoietic
reconstitution of bone marrow-derived mesenchymal stem cells in
bone marrow failure by the SDF-1/CXCR4. J Tissue Eng Regen Med.
14:1250–1260. 2020.PubMed/NCBI
|
|
167
|
Moll NM and Ransohoff RM: CXCL12 and CXCR4
in bone marrow physiology. Expert Rev Hematol. 3:315–322. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
168
|
Pozzobon T, Goldoni G, Viola A and Molon
B: CXCR4 signaling in health and disease. Immunol Lett. 177:6–15.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
169
|
Mousavi A: CXCL12/CXCR4 signal
transduction in diseases and its molecular approaches in
targeted-therapy. Immunol Lett. 217:91–115. 2020. View Article : Google Scholar
|
|
170
|
Guo J, Zhang H, Xiao J, Wu J, Ye Y, Li Z,
Zou Y and Li X: Monocyte chemotactic protein-1 promotes the
myocardial homing of mesenchymal stem cells in dilated
cardiomyopathy. Int J Mol Sci. 14:8164–8178. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
171
|
Schenk S, Mal N, Finan A, Zhang M,
Kiedrowski M, Popovic Z, McCarthy PM and Penn MS: Monocyte
chemotactic protein-3 is a myocardial mesenchymal stem cell homing
factor. Stem Cells. 25:245–251. 2007. View Article : Google Scholar
|
|
172
|
Ahn SY, Park WS, Kim YE, Sung DK, Sung SI,
Ahn JY and Chang YS: Vascular endothelial growth factor mediates
the therapeutic efficacy of mesenchymal stem cell-derived
extracellular vesicles against neonatal hyperoxic lung injury. Exp
Mol Med. 50:1–12. 2018.
|
|
173
|
Shams S, Mohsin S, Nasir GA, Khan M and
Khan SN: Mesenchymal stem cells pretreated with HGF and FGF4 can
reduce liver fibrosis in mice. Stem Cells Int. 2015:7472452015.
View Article : Google Scholar : PubMed/NCBI
|
|
174
|
Kumar S and Ponnazhagan S: Bone homing of
mesenchymal stem cells by ectopic alpha 4 integrin expression.
FASEB J. 21:3917–3927. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
175
|
Ferrari G, Cusella-De Angelis G, Coletta
M, Paolucci E, Stornaiuolo A, Cossu G and Mavilio F: Muscle
regeneration by bone marrow-derived myogenic progenitors. Science.
279:1528–1530. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
176
|
Winkler T, von Roth P, Schuman MR, Sieland
K, Stoltenburg-Didinger G, Taupitz M, Perka C, Duda GN and
Matziolis G: In vivo visualization of locally transplanted
mesenchymal stem cells in the severely injured muscle in rats.
Tissue Eng Part A. 14:1149–1160. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
177
|
Le Blanc K and Mougiakakos D: Multipotent
mesenchymal stromal cells and the innate immune system. Nat Rev
Immunol. 12:383–396. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
178
|
da Justa Pinheiro CH, de Queiroz JC,
Guimarães-Ferreira L, Vitzel KF, Nachbar RT, de Sousa LGO, de Souza
AL Jr, Nunes MT and Curi R: Local injections of adipose-derived
mesenchymal stem cells modulate inflammation and increase
angiogenesis ameliorating the dystrophic phenotype in
dystrophin-deficient skeletal muscle. Stem Cell Rev Rep. 8:363–374.
2012. View Article : Google Scholar
|
|
179
|
Németh K, Leelahavanichkul A, Yuen PS,
Mayer B, Parmelee A, Doi K, Robey PG, Leelahavanichkul K, Koller
BH, Brown JM, et al: Bone marrow stromal cells attenuate sepsis via
prostaglandin E(2)-dependent reprogramming of host macrophages to
increase their interleukin-10 production. Nat Med. 15:42–49. 2009.
View Article : Google Scholar
|
|
180
|
Chen L, Tredget EE, Wu PY and Wu Y:
Paracrine factors of mesenchymal stem cells recruit macrophages and
endothelial lineage cells and enhance wound healing. PLoS One.
3:e18862008. View Article : Google Scholar : PubMed/NCBI
|
|
181
|
Bencze M, Negroni E, Vallese D,
Yacoub-Youssef H, Chaouch S, Wolff A, Aamiri A, Di Santo JP,
Chazaud B, Butler-Browne G, et al: Proinflammatory macrophages
enhance the regenerative capacity of human myoblasts by modifying
their kinetics of proliferation and differentiation. Mol Ther.
20:2168–2179. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
182
|
Waterman RS, Tomchuck SL, Henkle SL and
Betancourt AM: A new mesenchymal stem cell (MSC) paradigm:
Polarization into a pro-inflammatory MSC1 or an Immunosuppressive
MSC2 phenotype. PLoS One. 5:e100882010. View Article : Google Scholar : PubMed/NCBI
|
|
183
|
de Couto G, Gallet R, Cambier L,
Jaghatspanyan E, Makkar N, Dawkins JF, Berman BP and Marbán E:
Exosomal MicroRNA transfer into macrophages mediates cellular
postconditioning. Circulation. 136:200–214. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
184
|
Xu R, Zhang F, Chai R, Zhou W, Hu M, Liu
B, Chen X, Liu M, Xu Q, Liu N and Liu S: Exosomes derived from
pro-inflammatory bone marrow-derived mesenchymal stem cells reduce
inflammation and myocardial injury via mediating macrophage
polarization. J Cell Mol Med. 23:7617–7631. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
185
|
Zhao J, Li X, Hu J, Chen F, Qiao S, Sun X,
Gao L, Xie J and Xu B: Mesenchymal stromal cell-derived exosomes
attenuate myocardial ischaemia-reperfusion injury through
miR-182-regulated macrophage polarization. Cardiovasc Res.
115:1205–1216. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
186
|
Simovic Markovic B, Gazdic M, Arsenijevic
A, Jovicic N, Jeremic J, Djonov V, Arsenijevic N, Lukic ML and
Volarevic V: Mesenchymal stem cells attenuate cisplatin-induced
nephrotoxicity in iNOS-dependent manner. Stem Cells Int.
2017:13153782017. View Article : Google Scholar : PubMed/NCBI
|
|
187
|
Sassoli C, Pini A, Chellini F, Mazzanti B,
Nistri S, Nosi D, Saccardi R, Quercioli F, Zecchi-Orlandini S and
Formigli L: Bone marrow mesenchymal stromal cells stimulate
skeletal myoblast proliferation through the paracrine release of
VEGF. PLoS One. 7:e375122012. View Article : Google Scholar : PubMed/NCBI
|
|
188
|
Murphy MB, Moncivais K and Caplan AI:
Mesenchymal stem cells: Environmentally responsive therapeutics for
regenerative medicine. Exp Mol Med. 45:e542013. View Article : Google Scholar : PubMed/NCBI
|
|
189
|
Sassoli C, Frati A, Tani A, Anderloni G,
Pierucci F, Matteini F, Chellini F, Zecchi Orlandini S, Formigli L
and Meacci E: Mesenchymal stromal cell secreted sphingosine
1-phosphate (S1P) exerts a stimulatory effect on skeletal myoblast
proliferation. PLoS One. 9:e1086622014. View Article : Google Scholar : PubMed/NCBI
|
|
190
|
Nakamura Y, Miyaki S, Ishitobi H,
Matsuyama S, Nakasa T, Kamei N, Akimoto T, Higashi Y and Ochi M:
Mesenchymal-stem-cell-derived exosomes accelerate skeletal muscle
regeneration. FEBS Lett. 589:1257–1265. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
191
|
Leoni G, Neumann PA, Kamaly N, Quiros M,
Nishio H, Jones HR, Sumagin R, Hilgarth RS, Alam A, Fredman G, et
al: Annexin A1-containing extracellular vesicles and polymeric
nanoparticles promote epithelial wound repair. J Clin Invest.
125:1215–1227. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
192
|
Bizzarro V, Petrella A and Parente L:
Annexin A1: Novel roles in skeletal muscle biology. J Cell Physiol.
227:3007–3015. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
193
|
Kim S, Lee MJ, Choi JY, Park DH, Kwak HB,
Moon S, Koh JW, Shin HK, Ryu JK, Park CS, et al: Roles of
exosome-like vesicles released from inflammatory C2C12 myotubes:
Regulation of myocyte differentiation and myokine expression. Cell
Physiol Biochem. 48:1829–1842. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
194
|
Choi JS, Yoon HI, Lee KS, Choi YC, Yang
SH, Kim IS and Cho YW: Exosomes from differentiating human skeletal
muscle cells trigger myogenesis of stem cells and provide
biochemical cues for skeletal muscle regeneration. J Control
Release. 222:107–115. 2016. View Article : Google Scholar
|
|
195
|
Forterre A, Jalabert A, Berger E, Baudet
M, Chikh K, Errazuriz E, De Larichaudy J, Chanon S, Weiss-Gayet M,
Hesse AM, et al: Proteomic analysis of C2C12 myoblast and myotube
exosome-like vesicles: A new paradigm for myoblast-myotube cross
talk? PLoS One. 9:e841532014. View Article : Google Scholar : PubMed/NCBI
|
|
196
|
Oswald J, Boxberger S, Jørgensen B,
Feldmann S, Ehninger G, Bornhäuser M and Werner C: Mesenchymal stem
cells can be differentiated into endothelial cells in vitro. Stem
Cells. 22:377–384. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
197
|
Wang C, Li Y, Yang M, Zou Y, Liu H, Liang
Z, Yin Y, Niu G, Yan Z and Zhang B: Efficient differentiation of
bone marrow mesenchymal stem cells into endothelial cells in vitro.
Eur J Vasc Endovasc Surg. 55:257–265. 2018. View Article : Google Scholar
|
|
198
|
Lu W, Xiu X, Zhao Y and Gui M: Improved
proliferation and differentiation of bone marrow mesenchymal stem
cells into vascular endothelial cells with sphingosine 1-phosphate.
Transplant Proc. 47:2035–2040. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
199
|
Grote K, Petri M, Liu C, Jehn P, Spalthoff
S, Kokemüller H, Luchtefeld M, Tschernig T, Krettek C, Haasper C
and Jagodzinski M: Toll-like receptor 2/6-dependent stimulation of
mesenchymal stem cells promotes angiogenesis by paracrine factors.
Eur Cell Mater. 26:66–79. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
200
|
Leroux L, Descamps B, Tojais NF, Séguy B,
Oses P, Moreau C, Daret D, Ivanovic Z, Boiron JM, Lamazière JM, et
al: Hypoxia preconditioned mesenchymal stem cells improve vascular
and skeletal muscle fiber regeneration after ischemia through a
Wnt4-dependent pathway. Mol Ther. 18:1545–1552. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
201
|
Berebichez-Fridman R and Montero-Olvera
PR: Sources and clinical applications of mesenchymal stem cells:
State-of-the-art review. Sultan Qaboos Univ Med J. 18:e264–e277.
2018. View Article : Google Scholar
|
|
202
|
Mushahary D, Spittler A, Kasper C, Weber V
and Charwat V: Isolation, cultivation, and characterization of
human mesenchymal stem cells. Cytometry A. 93:19–31. 2018.
View Article : Google Scholar
|
|
203
|
Spath L, Rotilio V, Alessandrini M,
Gambara G, De Angelis L, Mancini M, Mitsiadis TA, Vivarelli E, Naro
F, Filippini A and Papaccio G: Explant-derived human dental pulp
stem cells enhance differentiation and proliferation potentials. J
Cell Mol Med. 14:1635–1644. 2010. View Article : Google Scholar
|
|
204
|
Ueda N, Atsuta I, Ayukawa Y, Yamaza T,
Furuhashi A, Narimatsu I, Matsuura Y, Kondo R, Watanabe Y, Zhang X
and Koyano K: Novel application method for mesenchymal stem cell
therapy utilizing its attractant-responsive accumulation property.
Appl Sci. 9:49082019. View Article : Google Scholar
|
|
205
|
Castelo-Branco MTL, Soares IDO, Lopes DV,
Buongusto F, Martinusso CA, do Rosario A Jr, Souza SA, Gutfilen B,
Fonseca LM, Elia C, et al: Intraperitoneal but not intravenous
cryopreserved mesenchymal stromal cells home to the inflamed colon
and ameliorate experimental colitis. PLoS One. 7:e333602012.
View Article : Google Scholar : PubMed/NCBI
|
|
206
|
Gonçalves Fda C, Schneider N, Pinto FO,
Meyer FS, Visioli F, Pfaffenseller B, Lopez PL, Passos EP,
Cirne-Lima EO, Meurer L and Paz AH: Intravenous vs intraperitoneal
mesenchymal stem cells administration: What is the best route for
treating experimental colitis? World J Gastroenterol.
20:18228–18239. 2014. View Article : Google Scholar
|
|
207
|
Roux C, Saviane G, Pini J, Belaïd N, Dhib
G, Voha C, Ibáñez L, Boutin A, Mazure NM, Wakkach A, et al:
Immunosuppressive mesenchymal stromal cells derived from
human-induced pluripotent stem cells induce human regulatory T
cells in vitro and in vivo. Front Immunol. 8:19912018. View Article : Google Scholar : PubMed/NCBI
|
|
208
|
Braid LR, Wood CA, Wiese DM and Ford BN:
Intramuscular administration potentiates extended dwell time of
mesenchymal stromal cells compared to other routes. Cytotherapy.
20:232–244. 2018. View Article : Google Scholar
|
|
209
|
Rangarajan A, Hong SJ, Gifford A and
Weinberg RA: Erratum to species- and cell type-specific
requirements for cellular transformation [Cancer Cell 6, (2004)
171-183]. Cancer Cell. 24:394–398. 2013. View Article : Google Scholar
|
|
210
|
Wang Y, Han ZB, Song YP and Han ZC: Safety
of mesenchymal stem cells for clinical application. Stem Cells Int.
2012:6520342012. View Article : Google Scholar : PubMed/NCBI
|
|
211
|
Golpanian S, DiFede DL, Khan A, Schulman
IH, Landin AM, Tompkins BA, Heldman AW, Miki R, Goldstein BJ,
Mushtaq M, et al: Allogeneic human mesenchymal stem cell infusions
for aging frailty. J Gerontol A Biol Sci Med Sci. 72:1505–1512.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
212
|
Tompkins BA, DiFede DL, Khan A, Landin AM,
Schulman IH, Pujol MV, Heldman AW, Miki R, Goldschmidt-Clermont PJ,
Goldstein BJ, et al: Allogeneic mesenchymal stem cells ameliorate
aging frailty: A phase II randomized, double-blind,
placebo-controlled clinical trial. J Gerontol A Biol Sci Med Sci.
72:1513–1522. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
213
|
Kabat M, Bobkov I, Kumar S and Grumet M:
Trends in mesenchymal stem cell clinical trials 2004-2018: Is
efficacy optimal in a narrow dose range? Stem Cells Transl Med.
9:17–27. 2020. View Article : Google Scholar
|
|
214
|
Singer M, Deutschman CS, Seymour CW,
Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche
JD, Coopersmith CM, et al: The third international consensus
definitions for sepsis and septic shock (sepsis-3). JAMA.
315:801–810. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
215
|
Mankowski RT, Laitano O, Darden D, Kelly
L, Munley J, Loftus TJ, Mohr AM, Efron PA and Thomas RM:
Sepsis-Induced myopathy and gut microbiome dysbiosis: Mechanistic
links and therapeutic targets. Shock. 57:15–23. 2022. View Article : Google Scholar :
|
|
216
|
Liu Y, Wang D, Li T, Yang F, Li Z, Bai X
and Wang Y: The role of NLRP3 inflammasome in inflammation-related
skeletal muscle atrophy. Front Immunol. 13:10357092022. View Article : Google Scholar : PubMed/NCBI
|
|
217
|
Liu D, Huang SY, Sun JH, Zhang HC, Cai QL,
Gao C, Li L, Cao J, Xu F, Zhou Y, et al: Sepsis-induced
immunosuppression: Mechanisms, diagnosis and current treatment
options. Mil Med Res. 9:562022.PubMed/NCBI
|
|
218
|
Kramer CL: Intensive care unit-acquired
weakness. Neurol Clin. 35:723–736. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
219
|
Fu X, Liu G, Halim A, Ju Y, Luo Q and Song
AG: Mesenchymal stem cell migration and tissue repair. Cells.
8:7842019. View Article : Google Scholar : PubMed/NCBI
|
|
220
|
Song J, Liu J, Cui C, Hu H, Zang N, Yang
M, Yang J, Zou Y, Li J, Wang L, et al: Mesenchymal stromal cells
ameliorate diabetes-induced muscle atrophy through exosomes by
enhancing AMPK/ULK1-mediated autophagy. J Cachexia Sarcopenia
Muscle. 14:915–929. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
221
|
Abrigo J, Rivera JC, Aravena J, Cabrera D,
Simon F, Ezquer F, Ezquer M and Cabello-Verrugio C: High fat
diet-induced skeletal muscle wasting is decreased by mesenchymal
stem cells administration: Implications on oxidative stress,
ubiquitin proteasome pathway activation, and myonuclear apoptosis.
Oxid Med Cell Longev. 2016:90478212016. View Article : Google Scholar : PubMed/NCBI
|