|
1
|
Devarbhavi H, Asrani SK, Arab JP, Nartey
YA, Pose E and Kamath PS: Global burden of liver disease: 2023
Update. J Hepatol. 79:516–537. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Huang DQ, Terrault NA, Tacke F, Gluud LL,
Arrese M, Bugianesi E and Loomba R: Global epidemiology of
cirrhosis-aetiology, trends and predictions. Nat Rev Gastroenterol
Hepatol. 20:388–398. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Gilgenkrantz H, Mallat A, Moreau R and
Lotersztajn S: Targeting cell-intrinsic metabolism for antifibrotic
therapy. J Hepatol. 74:1442–1454. 2021. View Article : Google Scholar : PubMed/NCBI
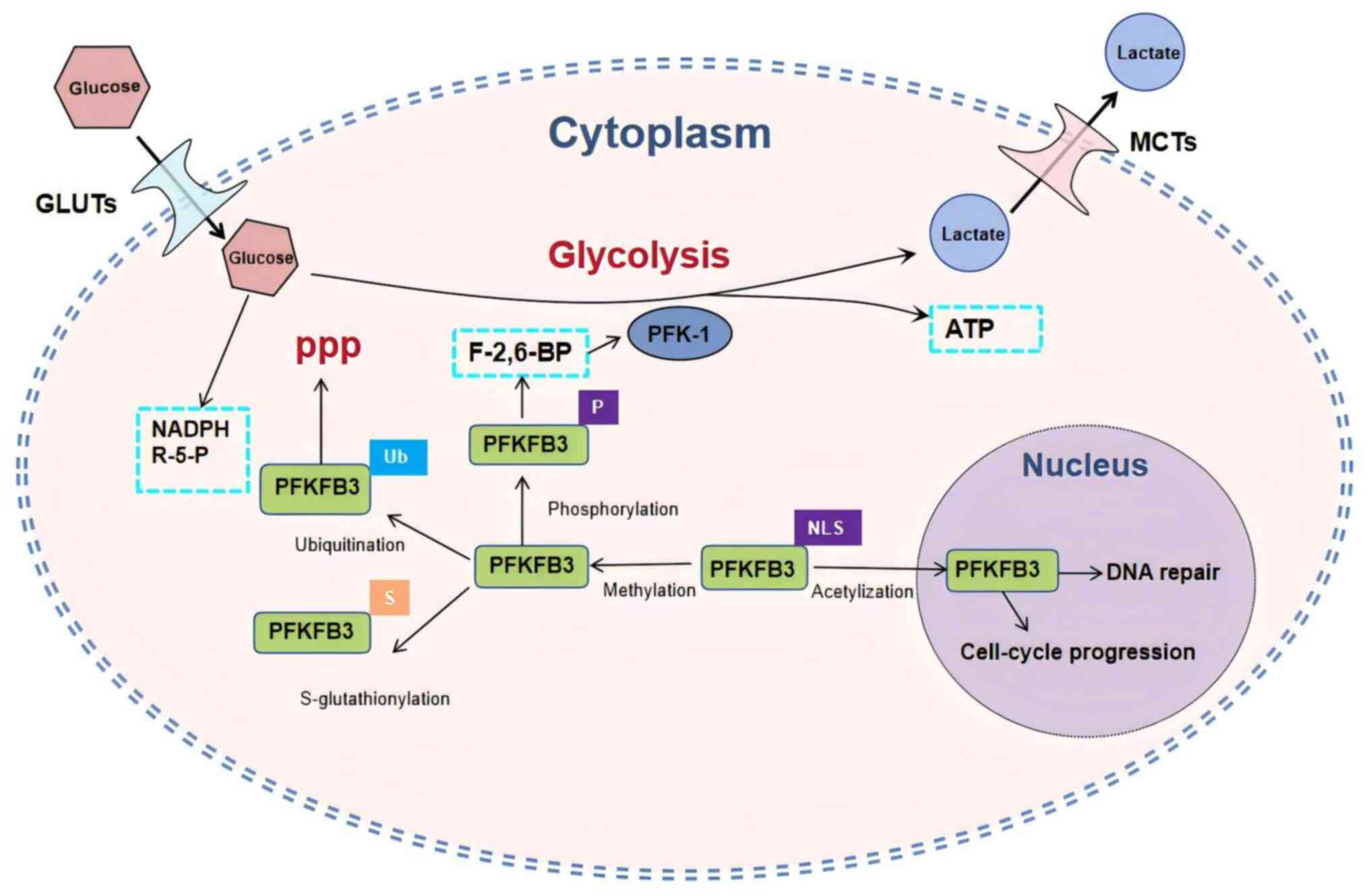
|
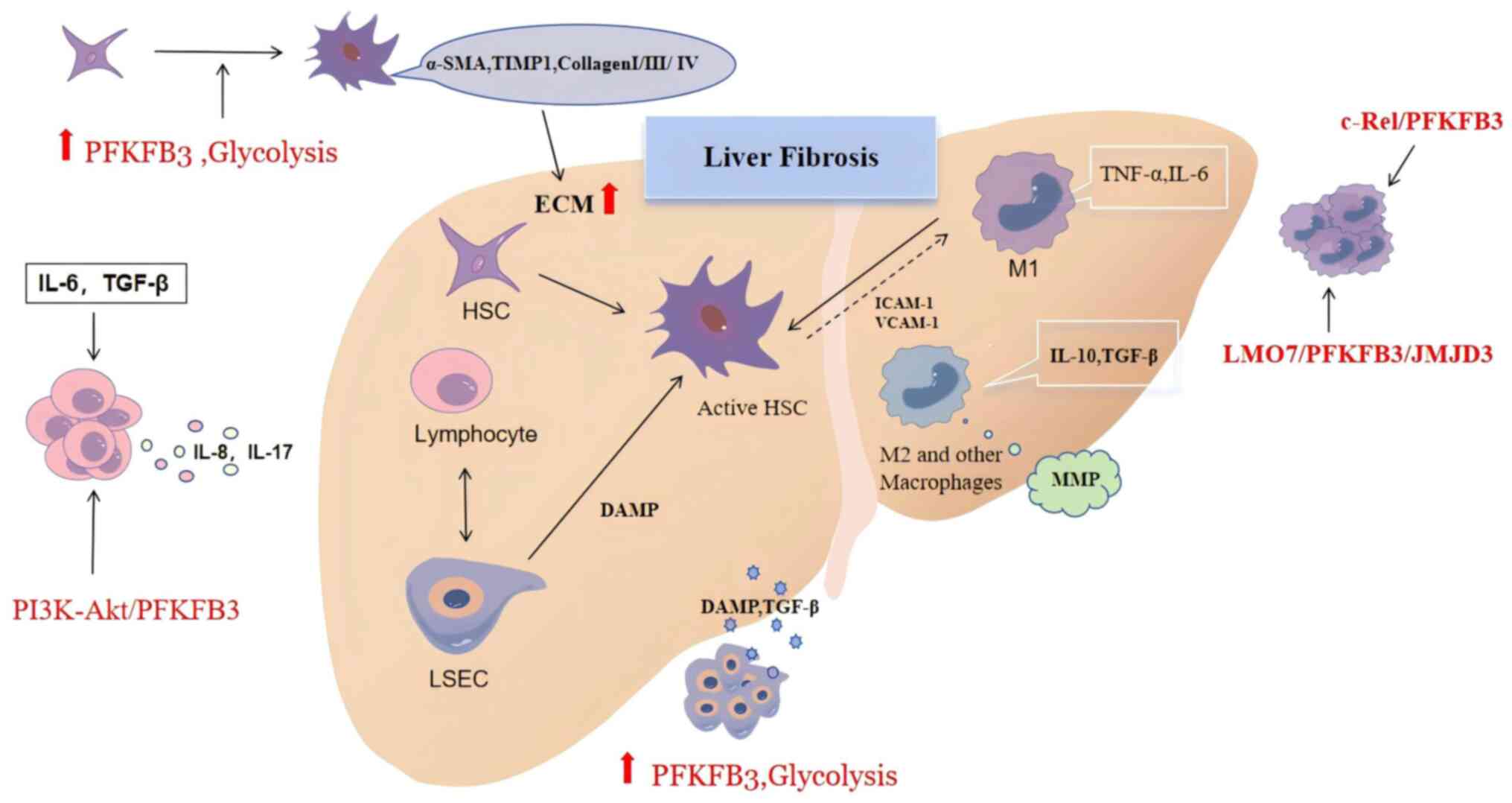
|
4
|
Parola M and Pinzani M: Liver fibrosis in
NAFLD/NASH: From pathophysiology towards diagnostic and therapeutic
strategies. Mol Aspects Med. 95:1012312024. View Article : Google Scholar
|
|
5
|
Pei Q, Yi Q and Tang L: Liver fibrosis
resolution: from molecular mechanisms to therapeutic opportunities.
Int J Mol Sci. 24:96712023. View Article : Google Scholar : PubMed/NCBI
|
|
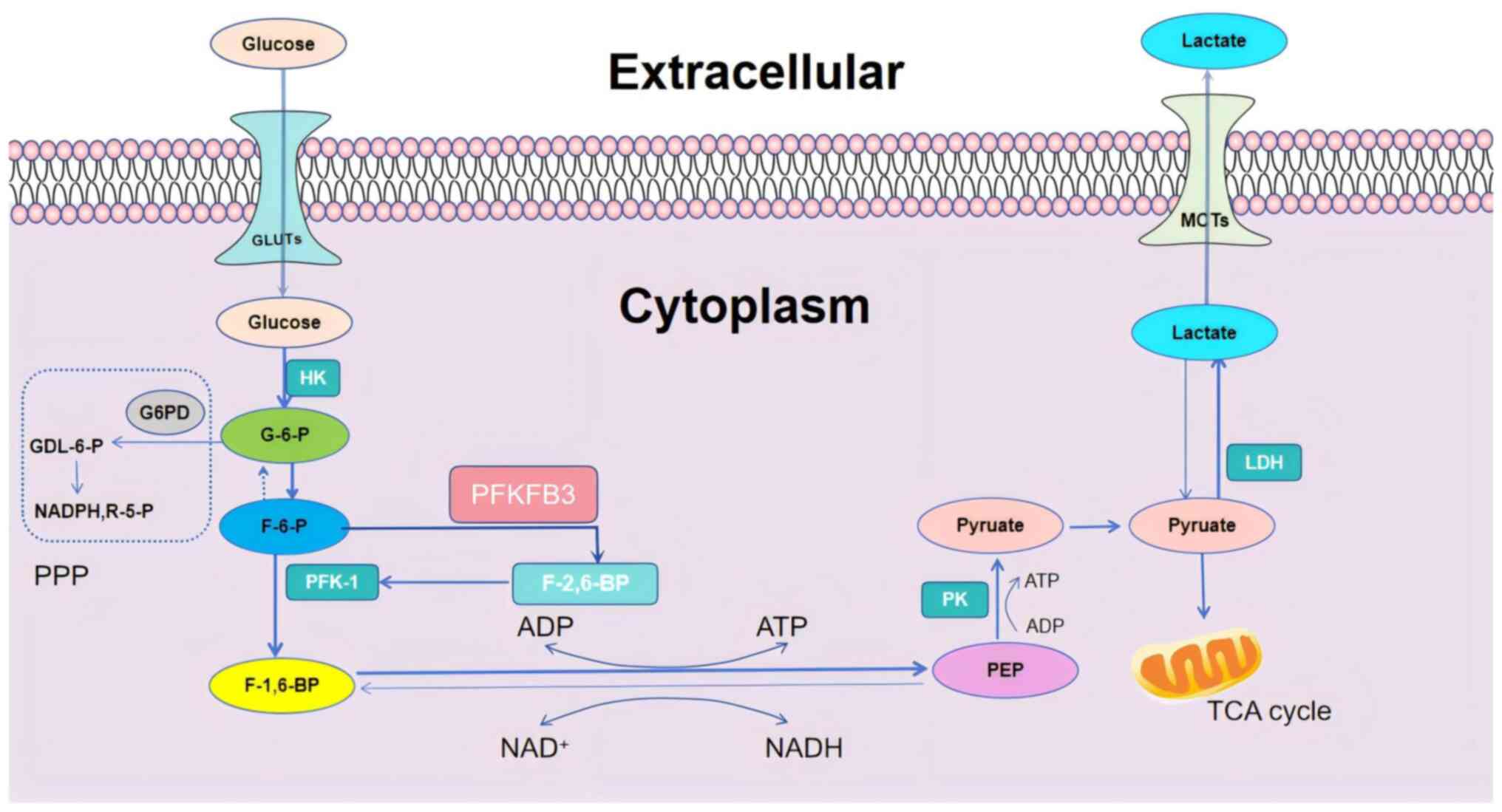
6
|
Campana L, Esser H, Huch M and Forbes S:
Liver regeneration and inflammation: From fundamental science to
clinical applications. Nat Rev Mol Cell Biol. 22:608–624. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kisseleva T and Brenner D: Molecular and
cellular mechanisms of liver fibrosis and its regression. Nat Rev
Gastroenterol Hepatol. 18:151–166. 2021. View Article : Google Scholar
|
|
8
|
Wang FD, Zhou J and Chen EQ: Molecular
mechanisms and potential new therapeutic drugs for liver fibrosis.
Front Pharmacol. 13:7877482022. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Zeng H, Pan T, Zhan M, Hailiwu R, Liu B,
Yang H and Li P: Suppression of PFKFB3-driven glycolysis restrains
endothelial-to-mesenchymal transition and fibrotic response. Signal
Transduct Target Ther. 7:3032022. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yang Q, Zong X, Zhuang L, Pan R, Tudi X,
Fan Q and Tao R: PFKFB3 inhibitor 3PO reduces cardiac remodeling
after myocardial infarction by regulating the TGF-β1/SMAD2/3
pathway. Biomolecules. 13:10722023. View Article : Google Scholar
|
|
11
|
Song C, Wang S, Fu Z, Chi K, Geng X, Liu
C, Cai G, Chen X, Wu D and Hong Q: IGFBP5 promotes diabetic kidney
disease progression by enhancing PFKFB3-mediated endothelial
glycolysis. Cell Death Dis. 13:3402022. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Jiang A, Liu J, Wang Y and Zhang C:
cGAS-STING signaling pathway promotes hypoxia-induced renal
fibrosis by regulating PFKFB3-mediated glycolysis. Free Radic Biol
Med. 208:516–529. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Hu X, Xu Q, Wan H, Hu Y, Xing S, Yang H,
Gao Y and He Z: PI3K-Akt-mTOR/PFKFB3 pathway mediated lung
fibroblast aerobic glycolysis and collagen synthesis in
lipopolysaccharide-induced pulmonary fibrosis. Lab Invest.
100:801–811. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zhao X, Kwan JYY, Yip K, Liu PP and Liu
FF: Targeting metabolic dysregulation for fibrosis therapy. Nat Rev
Drug Discov. 19:57–75. 2020. View Article : Google Scholar
|
|
15
|
Horn P and Tacke F: Metabolic
reprogramming in liver fibrosis. Cell Metab. 36:1439–1455. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Hammerich L and Tacke F: Hepatic
inflammatory responses in liver fibrosis. Nat Rev Gastroenterol
Hepatol. 20:633–646. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Cogliati B, Yashaswini CN, Wang S, Sia D
and Friedman SL: Friend or foe? The elusive role of hepatic
stellate cells in liver cancer. Nat Rev Gastroenterol Hepatol.
20:647–661. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Qu H, Liu J, Zhang D, Xie R, Wang L and
Hong J: Glycolysis in chronic liver diseases: Mechanistic insights
and therapeutic opportunities. Cells. 12:19302023. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Jones BC, Pohlmann PR, Clarke R and
Sengupta S: Treatment against glucose-dependent cancers through
metabolic PFKFB3 targeting of glycolytic flux. Cancer Metastasis
Rev. 41:447–458. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Baker SA and Rutter J: Metabolites as
signalling molecules. Nat Rev Mol Cell Biol. 24:355–374. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Shi L, Pan H, Liu Z, Xie J and Han W:
Roles of PFKFB3 in cancer. Signal Transduct Target Ther.
2:170442017. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Mejias M, Gallego J, Naranjo-Suarez S,
Ramirez M, Pell N, Manzano A, Suñer C, Bartrons R, Mendez R and
Fernandez M: CPEB4 increases expression of PFKFB3 to induce
glycolysis and activate mouse and human hepatic stellate cells,
promoting liver fibrosis. Gastroenterology. 159:273–288. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Alvarez R, Mandal D and Chittiboina P:
Canonical and non-canonical roles of PFKFB3 in brain tumors. Cells.
10:29132021. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Calderone V, Gallego J, Fernandez-Miranda
G, Garcia-Pras E, Maillo C, Berzigotti A, Mejias M, Bava FA,
Angulo-Urarte A, Graupera M, et al: Sequential functions of CPEB1
and CPEB4 regulate pathologic expression of vascular endothelial
growth factor and angiogenesis in chronic liver disease.
Gastroenterology. 150:982–997.e30. 2016. View Article : Google Scholar
|
|
25
|
Hu KF, Shu CW, Lee CH, Tseng CJ, Chou YH
and Liu PF: Comparative clinical significance and biological roles
of PFKFB family members in oral squamous cell carcinoma. Cancer
Cell Int. 23:2572023. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Zodda E, Tura-Ceide O, Mills NL,
Tarragó-Celada J, Carini M, Thomson TM and Cascante M: Autonomous
metabolic reprogramming and oxidative stress characterize
endothelial dysfunction in acute myocardial infarction. Elife.
12:e862602023. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Wang Y, Tang S, Wu Y, Wan X, Zhou M, Li H
and Zha X: Upregulation of 6-phosphofructo-2-kinase (PFKFB3) by
hyperactivated mammalian target of rapamycin complex 1 is critical
for tumor growth in tuberous sclerosis complex. IUBMB Life.
72:965–977. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Boscaro C, Carotti M, Albiero M, Trenti A,
Fadini GP, Trevisi L, Sandonà D, Cignarella A and Bolego C:
Non-genomic mechanisms in the estrogen regulation of glycolytic
protein levels in endothelial cells. FASEB J. 34:12768–12784. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Kommagani R, Szwarc MM, Kovanci E, Gibbons
WE, Putluri N, Maity S, Creighton CJ, Sreekumar A, DeMayo FJ, Lydon
JP and O'Malley BW: Acceleration of the glycolytic flux by steroid
receptor coactivator-2 is essential for endometrial
decidualization. PLoS Genet. 9:e10039002013. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Novellasdemunt L, Bultot L, Manzano A,
Ventura F, Rosa JL, Vertommen D, Rider MH, Navarro-Sabate À and
Bartrons R: PFKFB3 activation in cancer cells by the p38/MK2
pathway in response to stress stimuli. Biochem J. 452:531–543.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Watanuki S, Kobayashi H, Sugiura Y,
Yamamoto M, Karigane D, Shiroshita K, Sorimachi Y, Fujita S,
Morikawa T, Koide S, et al: Context-dependent modification of
PFKFB3 in hematopoietic stem cells promotes anaerobic glycolysis
and ensures stress hematopoiesis. Elife. 12:RP876742024. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Yi M, Ban Y, Tan Y, Xiong W, Li G and
Xiang B: 6-Phosphofructo-2-kinase/fructose-2,6-biphosphatase 3 and
4: A pair of valves for fine-tuning of glucose metabolism in human
cancer. Mol Metab. 20:1–13. 2019. View Article : Google Scholar :
|
|
33
|
Shakhpazyan N, Mikhaleva L, Bedzhanyan A,
Sadykhov N, Midiber K and Orekhov A: Commentary: PFKFB3
overexpression in monocytes of patients with colon but not rectal
cancer programs pro-tumor macrophages and is indicative for higher
risk of tumor relapse. Front Immunol. 14:12904592023. View Article : Google Scholar
|
|
34
|
Jia W, Wu Q, Shen M, Yu X, An S, Zhao L,
Huang G and Liu J: PFKFB3 regulates breast cancer tumorigenesis and
Fulvestrant sensitivity by affecting ERα stability. Cell Signal.
119:1111842024. View Article : Google Scholar
|
|
35
|
Wang Y, Wang X, Du C, Wang Z, Wang J, Zhou
N, Wang B, Tan K, Fan Y and Cao P: Glycolysis and beyond in glucose
metabolism: Exploring pulmonary fibrosis at the metabolic
crossroads. Front Endocrinol (Lausanne). 15:13795212024. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Yang Q, Huo E, Cai Y, Zhang Z, Dong C,
Asara JM, Shi H and Wei Q: Myeloid PFKFB3-mediated glycolysis
promotes kidney fibrosis. Front Immunol. 14:12594342023. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Chandel NS: Glycolysis. Cold Spring Harb
Perspect Biol. 13:a0405352021. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Paul S, Ghosh S and Kumar S: Tumor
glycolysis, an essential sweet tooth of tumor cells. Semin Cancer
Biol. 86:1216–1230. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Qiao Q, Hu S and Wang X: The regulatory
roles and clinical significance of glycolysis in tumor. Cancer
Commun (Lond). 44:761–786. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Fendt SM: 100 Years of the Warburg effect:
A cancer metabolism endeavor. Cell. 187:3824–3828. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Jaccard A, Wyss T, Maldonado-Pérez N, Rath
JA, Bevilacqua A, Peng JJ, Lepez A, Von Gunten C, Franco F, Kao KC,
et al: Reductive carboxylation epigenetically instructs T cell
differentiation. Nature. 621:849–856. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Feng J, Li J, Wu L, Yu Q, Ji J, Wu J, Dai
W and Guo C: Emerging roles and the regulation of aerobic
glycolysis in hepatocellular carcinoma. J Exp Clin Cancer Res.
39:1262020. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Ma H, Zhang J, Zhou L, Wen S, Tang HY,
Jiang B, Zhang F, Suleman M, Sun D, Chen A, et al: c-Src promotes
tumorigenesis and tumor progression by activating PFKFB3. Cell Rep.
30:4235–4249.e6. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Galindo CM, de Oliveira Ganzella FA,
Klassen G, Souza Ramos EA and Acco A: Nuances of PFKFB3 signaling
in breast cancer. Clin Breast Cancer. 22:e604–e614. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Li FL, Liu JP, Bao RX, Yan G, Feng X, Xu
YP, Sun YP, Yan W, Ling ZQ, Xiong Y, et al: Acetylation accumulates
PFKFB3 in cytoplasm to promote glycolysis and protects cells from
cisplatin-induced apoptosis. Nat Commun. 9:5082018. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Suematsu M, Nakamura T, Tokumoto Y,
Yamamoto T, Kajimura M and Kabe Y: CO-CBS-H2 S axis: From vascular
mediator to cancer regulator. Microcirculation. 23:183–190. 2016.
View Article : Google Scholar
|
|
47
|
McErlean P, Bell CG, Hewitt RJ, Busharat
Z, Ogger PP, Ghai P, Albers GJ, Calamita E, Kingston S, Molyneaux
PL, et al: DNA methylome alterations are associated with airway
macrophage differentiation and phenotype during lung fibrosis. Am J
Respir Crit Care Med. 204:954–966. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Desideri E, Vegliante R, Cardaci S,
Nepravishta R, Paci M and Ciriolo MR: MAPK14/p38α-dependent
modulation of glucose metabolism affects ROS levels and autophagy
during starvation. Autophagy. 10:1652–1665. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Yuan Y, Wang W, Zhang Y, Hong Q, Huang W,
Li L, Xie Z, Chen Y, Li X and Meng Y: Apelin-13 attenuates
lipopolysaccharide-induced inflammatory responses and acute lung
injury by regulating PFKFB3-Driven glycolysis induced by
NOX4-dependent ROS. J Inflamm Res. 15:2121–2139. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Lin S, Li Y, Wang D, Huang C, Marino D,
Bollt O, Wu C, Taylor MD, Li W, DeNicola GM, et al: Fascin promotes
lung cancer growth and metastasis by enhancing glycolysis and
PFKFB3 expression. Cancer Lett. 518:230–242. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Lin S, Taylor MD, Singh PK and Yang S: How
does fascin promote cancer metastasis? FEBS J. 288:1434–1446. 2021.
View Article : Google Scholar :
|
|
52
|
Zhang LF, Deng WQ, Huang QW, Zhang JJ,
Wang Y, Zhou TJ, Xing L and Jiang HL: Vicious cycle-breaking lipid
nanoparticles remodeling multicellular crosstalk to reverse liver
fibrosis. Adv Mater. 36:e23114742024. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Moreno-Lanceta A, Medrano-Bosch M, Fundora
Y, Perramón M, Aspas J, Parra-Robert M, Baena S, Fondevila C,
Edelman ER, Jiménez W and Melgar-Lesmes P: RNF41 orchestrates
macrophage-driven fibrosis resolution and hepatic regeneration. Sci
Transl Med. 15:eabq62252023. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Cai X, Wang J, Wang J, Zhou Q, Yang B, He
Q and Weng Q: Intercellular crosstalk of hepatic stellate cells in
liver fibrosis: New insights into therapy. Pharmacol Res.
155:1047202020. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Sinha S, Hassan N and Schwartz RE:
Organelle stress and alterations in interorganelle crosstalk during
liver fibrosis. Hepatology. 79:482–501. 2024. View Article : Google Scholar
|
|
56
|
Roehlen N, Crouchet E and Baumert TF:
Liver fibrosis: Mechanistic concepts and therapeutic perspectives.
Cells. 9:8752020. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Odagiri N, Matsubara T, Sato-Matsubara M,
Fujii H, Enomoto M and Kawada N: Anti-fibrotic treatments for
chronic liver diseases: The present and the future. Clin Mol
Hepatol. 27:413–424. 2021. View Article : Google Scholar :
|
|
58
|
An P, Wei LL, Zhao S, Sverdlov DY, Vaid
KA, Miyamoto M, Kuramitsu K, Lai M and Popov YV: Hepatocyte
mitochondria-derived danger signals directly activate hepatic
stellate cells and drive progression of liver fibrosis. Nat Commun.
11:23622020. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Geervliet E, Moreno S, Baiamonte L,
Booijink R, Boye S, Wang P, Voit B, Lederer A, Appelhans D and
Bansal R: Matrix metalloproteinase-1 decorated polymersomes, a
surface-active extracellular matrix therapeutic, potentiates
collagen degradation and attenuates early liver fibrosis. J Control
Release. 332:594–607. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Casari M, Siegl D, Deppermann C and
Schuppan D: Macrophages and platelets in liver fibrosis and
hepatocellular carcinoma. Front Immunol. 14:12778082023. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Gao J, Wei B, de Assuncao TM, Liu Z, Hu X,
Ibrahim S, Cooper SA, Cao S, Shah VH and Kostallari E: Hepatic
stellate cell autophagy inhibits extracellular vesicle release to
attenuate liver fibrosis. J Hepatol. 73:1144–1154. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Song Y, Wei J, Li R, Fu R, Han P, Wang H,
Zhang G, Li S, Chen S, Liu Z, et al: Tyrosine kinase receptor B
attenuates liver fibrosis by inhibiting TGF-β/SMAD signaling.
Hepatology. 78:1433–1447. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
de Carvalho Ribeiro M and Szabo G: Role of
the inflammasome in liver disease. Annu Rev Pathol. 17:345–365.
2022. View Article : Google Scholar
|
|
64
|
Wang F, Chen L, Kong D, Zhang X, Xia S,
Liang B, Li Y, Zhou Y, Zhang Z, Shao J, et al: Canonical Wnt
signaling promotes HSC glycolysis and liver fibrosis through an
LDH-A/HIF-1α transcriptional complex. Hepatology. 79:606–623.
2024.
|
|
65
|
Xu F, Liu C, Zhou D and Zhang L:
TGF-β/SMAD pathway and its regulation in hepatic fibrosis. J
Histochem Cytochem. 64:157–167. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Feng W, Guan Z, Ying WZ, Xing D, Ying KE
and Sanders PW: Matrix metalloproteinase-9 regulates afferent
arteriolar remodeling and function in hypertension-induced kidney
disease. Kidney Int. 104:740–753. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Yao QY, Feng YD, Han P, Yang F and Song
GQ: Hepatic microenvironment underlies fibrosis in chronic
hepatitis B patients. World J Gastroenterol. 26:3917–3928. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Giarratana AO, Prendergast CM, Salvatore
MM and Capaccione KM: TGF-β signaling: Critical nexus of
fibrogenesis and cancer. J Transl Med. 22:5942024. View Article : Google Scholar
|
|
69
|
Liu Y, Meyer C, Müller A, Herweck F, Li Q,
Müllenbach R, Mertens PR, Dooley S and Weng HL: IL-13 induces
connective tissue growth factor in rat hepatic stellate cells via
TGF-β-independent Smad signaling. J Immunol. 187:2814–2823. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Akkız H, Gieseler RK and Canbay A: Liver
fibrosis: From basic science towards clinical progress, focusing on
the central role of hepatic stellate cells. Int J Mol Sci.
25:78732024. View Article : Google Scholar
|
|
71
|
Yan M, Xie Y, Yao J and Li X: The
dual-mode transition of myofibroblasts derived from hepatic
stellate cells in liver fibrosis. Int J Mol Sci. 24:154602023.
View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Bouguéon M, Legagneux V, Hazard O, Bomo J,
Siegel A, Feret J and Théret N: A rule-based multiscale model of
hepatic stellate cell plasticity: Critical role of the inactivation
loop in fibrosis progression. PLoS Comput Biol. 20:e10118582024.
View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Lu JL, Yu CX and Song LJ: Programmed cell
death in hepatic fibrosis: Current and perspectives. Cell Death
Discov. 9:4492023. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Li R, Li Z, Feng Y, Yang H, Shi Q, Tao Z,
Cheng J and Lu X: PDGFRβ-targeted TRAIL specifically induces
apoptosis of activated hepatic stellate cells and ameliorates liver
fibrosis. Apoptosis. 25:105–119. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Noom A, Sawitzki B, Knaus P and Duda GN: A
two-way street-cellular metabolism and myofibroblast contraction.
NPJ Regen Med. 9:152024. View Article : Google Scholar
|
|
76
|
Cao Y, Wang S, Zhang M, Lai B and Liang Y:
PFKFB3-mediated glycolysis in hepatic stellate cells promotes liver
regeneration. Biochem Biophys Res Commun. 712-713:1499582024.
View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Kovacs L, Cao Y, Han W, Meadows L,
Kovacs-Kasa A, Kondrikov D, Verin AD, Barman SA, Dong Z, Huo Y and
Su Y: PFKFB3 in smooth muscle promotes vascular remodeling in
pulmonary arterial hypertension. Am J Respir Crit Care Med.
200:617–627. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Cheng D, Chai J, Wang H, Fu L, Peng S and
Ni X: Hepatic macrophages: Key players in the development and
progression of liver fibrosis. Liver Int. 41:2279–2294. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Wang Z, Du K, Jin N, Tang B and Zhang W:
Macrophage in liver fibrosis: Identities and mechanisms. Int
Immunopharmacol. 120:1103572023. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Pei L, Li R, Wang X, Xu D, Gong F, Chen W,
Zheng X, Liu W, Zhao S, Wang Q, et al: MSCs-derived extracellular
vesicles alleviate sepsis-associated liver dysfunction by
inhibiting macrophage glycolysis-mediated inflammatory response.
Int Immunopharmacol. 128:1115752024. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Liang W, Huang X and Shi J: Macrophages
serve as bidirectional regulators and potential therapeutic targets
for liver fibrosis. Cell Biochem Biophys. 81:659–671. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Strickland JD and Copple BL: Modulation of
macrophage phenotype to treat liver fibrosis-current approaches and
future possibilities. Adv Pharmacol. 91:213–228. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Liu Y, Xu R, Gu H, Zhang E, Qu J, Cao W,
Huang X, Yan H, He J and Cai Z: Metabolic reprogramming in
macrophage responses. Biomark Res. 9:12021. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Soto-Heredero G, Gómez de Las Heras MM,
Gabandé-Rodríguez E, Oller J and Mittelbrunn M: Glycolysis-a key
player in the inflammatory response. FEBS J. 287:3350–3369. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Duan S, Lou X, Chen S, Jiang H, Chen D,
Yin R, Huang X, Yan H, He J and Cai Z: Macrophage LMO7 deficiency
facilitates inflammatory injury via metabolic-epigenetic
reprogramming. Acta Pharm Sin B. 13:4785–4800. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Leslie J, Macia MG, Luli S, Worrell JC,
Reilly WJ, Paish HL, Knox A, Barksby BS, Gee LM, Zaki MYW, et al:
c-Rel orchestrates energy-dependent epithelial and macrophage
reprogramming in fibrosis. Nat Metab. 2:1350–1367. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Fuhrmann DC and Brüne B: miR-193a-3p
increases glycolysis under hypoxia by facilitating Akt
phosphorylation and PFKFB3 activation in human macrophages. Cell
Mol Life Sci. 79:892022. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Zhang J, Muri J, Fitzgerald G, Gorski T,
Gianni-Barrera R, Masschelein E, D'Hulst G, Gilardoni P, Turiel G,
Fan Z, et al: Endothelial lactate controls muscle regeneration from
ischemia by inducing M2-like macrophage polarization. Cell Metab.
31:1136–1153.e7. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Zhang M and Zhang S: T cells in fibrosis
and fibrotic diseases. Front Immunol. 11:11422020. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Koda Y, Teratani T, Chu PS, Hagihara Y,
Mikami Y, Harada Y, Tsujikawa H, Miyamoto K, Suzuki T, Taniki N, et
al: CD8+ tissue-resident memory T cells promote liver
fibrosis resolution by inducing apoptosis of hepatic stellate
cells. Nat Commun. 12:44742021. View Article : Google Scholar
|
|
91
|
Barron L and Wynn TA: Fibrosis is
regulated by Th2 and Th17 responses and by dynamic interactions
between fibroblasts and macrophages. Am J Physiol Gastrointest
Liver Physiol. 300:G723–G728. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Li N, Yamamoto G, Fuji H and Kisseleva T:
Interleukin-17 in liver disease pathogenesis. Semin Liver Dis.
41:507–515. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Savage TM, Fortson KT, de Los
Santos-Alexis K, Oliveras-Alsina A, Rouanne M, Rae SS, Gamarra JR,
Shayya H, Kornberg A, Cavero R, et al: Amphiregulin from regulatory
T cells promotes liver fibrosis and insulin resistance in
non-alcoholic steatohepatitis. Immunity. 57:303–318.e6. 2024.
View Article : Google Scholar
|
|
94
|
Hann A, Oo YH and Perera MTPR: Regulatory
T-cell therapy in liver transplantation and chronic liver disease.
Front Immune. 12:7199542021. View Article : Google Scholar
|
|
95
|
Patel AM, Liu YS, Davies SP, Brown RM,
Kelly DA, Scheel-Toellner D, Reynolds GM and Stamataki Z: The role
of B cells in adult and paediatric liver injury. Front Immunol.
12:7291432021. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Cao J, Liao S, Zeng F, Liao Q, Luo G and
Zhou Y: Effects of altered glycolysis levels on CD8+ T
cell activation and function. Cell Death Dis. 14:4072023.
View Article : Google Scholar
|
|
97
|
Madden MZ and Rathmell JC: The complex
integration of T-cell metabolism and immunotherapy. Cancer Discov.
11:1636–1643. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Icard P, Alifano M, Donnadieu E and Simula
L: Fructose-1,6-bisphosphate promotes PI3K and glycolysis in T
cells? Trends Endocrinol Metab. 32:540–543. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Simon-Molas H, Arnedo-Pac C, Fontova P,
Vidal-Alabró A, Castaño E, Rodríguez-García A, Navarro-Sabaté À,
Lloberas N, Manzano A and Bartrons R: PI3K-Akt signaling controls
PFKFB3 expression during human T-lymphocyte activation. Mol Cell
Biochem. 448:187–197. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Harshan S, Dey P and Raghunathan S:
Altered transcriptional regulation of glycolysis in circulating
CD8+ T cells of rheumatoid arthritis patients. Genes
(Basel). 13:12162022. View Article : Google Scholar
|
|
101
|
Dou Q, Grant AK, Callahan C, Coutinho de
Souza P, Mwin D, Booth AL, Nasser I, Moussa M, Ahmed M and Tsai LL:
PFKFB3-mediated pro-glycolytic shift in hepatocellular carcinoma
proliferation. Cell Mol Gastroenterol Hepatol. 15:61–75. 2023.
View Article : Google Scholar
|
|
102
|
Li Y, Zhou Y, Xia S, Chen L, Yang T, Zhao
D, Zhang Z, Shao J, Xu X, Zhang F and Zheng S: Blockade of
KLF5/LDH-A feedback loop contributes to Curcumol inhibition of
sinusoidal endothelial cell glycolysis and mitigation of liver
fibrosis. Phytomedicine. 114:1547592023. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Gracia-Sancho J, Caparros E,
Fernández-Iglesias A and Francés R: Role of liver sinusoidal
endothelial cells in liver diseases. Nat Rev Gastroenterol Hepatol.
18:411–431. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Gracia-Sancho J, Marrone G and
Fernández-Iglesias A: Hepatic microcirculation and mechanisms of
portal hypertension. Nat Rev Gastroenterol Hepatol. 16:221–234.
2019. View Article : Google Scholar
|
|
105
|
Kumar S, Duan Q, Wu R, Harris EN and Su Q:
Pathophysiological communication between hepatocytes and
non-parenchymal cells in liver injury from NAFLD to liver fibrosis.
Adv Drug Deliv Rev. 176:1138692021. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Pandey E, Nour AS and Harris EN: Prominent
receptors of liver sinusoidal endothelial cells in liver
homeostasis and disease. Front Physiol. 11:8732020. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Khan MA, Fischer J, Harrer L, Schwiering
F, Groneberg D and Friebe A: Hepatic stellate cells in zone 1
engage in capillarization rather than myofibroblast formation in
murine liver fibrosis. Sci Rep. 14:188402024. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Baiocchini A, Del Nonno F, Taibi C,
Visco-Comandini U, D'Offizi G, Piacentini M and Falasca L: Liver
sinusoidal endothelial cells (LSECs) modifications in patients with
chronic hepatitis C. Sci Rep. 9:87602019. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Lee KC, Wu PS and Lin HC: Pathogenesis and
treatment of non-alcoholic steatohepatitis and its fibrosis. Clin
Mol Hepatol. 29:77–98. 2023. View Article : Google Scholar :
|
|
110
|
Hammoutene A, Biquard L, Lasselin J,
Kheloufi M, Tanguy M, Vion AC, Mérian J, Colnot N, Loyer X, Tedgui
A, et al: A defect in endothelial autophagy occurs in patients with
non-alcoholic steatohepatitis and promotes inflammation and
fibrosis. J Hepatol. 72:528–538. 2020. View Article : Google Scholar
|
|
111
|
Maeso-Díaz R, Boyer-Diaz Z, Lozano JJ,
Ortega-Ribera M, Peralta C, Bosch J and Gracia-Sancho J: New rat
model of advanced NASH mimicking pathophysiological features and
transcriptomic signature of the human disease. Cells. 8:10622019.
View Article : Google Scholar : PubMed/NCBI
|
|
112
|
McConnell MJ, Kostallari E, Ibrahim SH and
Iwakiri Y: The evolving role of liver sinusoidal endothelial cells
in liver health and disease. Hepatology. 78:649–669. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Wei M, Zhang Y, Zhang H, Huang Z, Miao H,
Zhang T, Lu B and Ji L: HMGB1 induced endothelial to mesenchymal
transition in liver fibrosis: The key regulation of early growth
response factor 1. Biochim Biophys Acta Gen Subj. 1866:1302022022.
View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Wang L, Guo S, Cao K, Li Z, Li Z, Song M,
Wang C, Chen P, Cui Y, Dai X, et al: Glycolysis promotes
angiotensin II-induced aortic remodeling through regulating
endothelial-to-mesenchymal transition via the corepressor
C-terminal binding protein 1. Hypertension. 80:2627–2640. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Greuter T, Yaqoob U, Gan C, Jalan-Sakrikar
N, Kostallari E, Lu J, Gao J, Sun L, Liu M, Sehrawat TS, et al:
Mechanotransduction-induced glycolysis epigenetically regulates a
CXCL1-dominant angiocrine signaling program in liver sinusoidal
endothelial cells in vitro and in vivo. J Hepatol. 77:723–734.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Atherton P, Stutchbury B, Jethwa D and
Ballestrem C: Mechanosensitive components of integrin adhesions:
Role of vinculin. Exp Cell Res. 343:21–27. 2016. View Article : Google Scholar :
|
|
117
|
Lovisa S, Fletcher-Sananikone E, Sugimoto
H, Hensel J, Lahiri S, Hertig A, Taduri G, Lawson E, Dewar R,
Revuelta I, et al: Endothelial-to-mesenchymal transition
compromises vascular integrity to induce Myc-mediated metabolic
reprogramming in kidney fibrosis. Sci Signal. 13:eaaz25972020.
View Article : Google Scholar : PubMed/NCBI
|
|
118
|
DeLeve LD: Liver sinusoidal endothelial
cells in hepatic fibrosis. Hepatology. 61:1740–1746. 2015.
View Article : Google Scholar
|
|
119
|
Kim HY, Sakane S, Eguileor A, Carvalho
Gontijo Weber R, Lee W, Liu X, Lam K, Ishizuka K, Rosenthal SB,
Diggle K, et al: The origin and fate of liver myofibroblasts. Cell
Mol Gastroenterol Hepatol. 17:93–106. 2024. View Article : Google Scholar
|
|
120
|
Yang W, He H, Wang T, Su N, Zhang F, Jiang
K, Zhu J, Zhang C, Niu K, Wang L, et al: Single-cell transcriptomic
analysis reveals a hepatic stellate cell-activation roadmap and
myofibroblast origin during liver fibrosis in mice. Hepatology.
74:2774–2790. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Wang W, Zhang Y, Huang W, Yuan Y, Hong Q,
Xie Z, Li L, Chen Y, Li X and Meng Y: Alamandine/MrgD axis prevents
TGF-β1-mediated fibroblast activation via regulation of aerobic
glycolysis and mitophagy. J Transl Med. 21:242023. View Article : Google Scholar
|
|
122
|
Chen W, Zhang J, Zhong W, Liu Y, Lu Y,
Zeng Z, Huang H, Wan X, Meng X, Zou F, et al: Anlotinib inhibits
PFKFB3-driven glycolysis in myofibroblasts to reverse pulmonary
fibrosis. Front Pharmacol. 12:7448262021. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Nie Z, Wu J, Xie J and Yin W: Sinomenine
ameliorates bleomycin-induced pulmonary fibrosis by inhibiting the
differentiation of fibroblast into myofibroblast. Heliyon.
10:e333142024. View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Yang Q, Huo E, Cai Y, Zhang Z, Dong C,
Asara JM and Wei Q: PFKFB3-mediated glycolysis boosts fibroblast
activation and subsequent kidney fibrosis. Cells. 12:20812023.
View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Wang F, Yin X, Fan YM, Zhang X, Ma C, Jia
K, Zhou W, Tang Z, Qi LW and Li J: Upregulation of glycolytic
enzyme PFKFB3 by deubiquitinase OTUD4 promotes cardiac fibrosis
post myocardial infarction. J Mol Med (Berl). 101:743–756. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Dewidar B, Meyer C, Dooley S and
Meindl-Beinker AN: TGF-β in hepatic stellate cell activation and
liver fibrogenesis-updated 2019. Cells. 8:14182019. View Article : Google Scholar
|
|
127
|
Kotowski K, Rosik J, Machaj F, Supplitt S,
Wiczew D, Jabłońska K, Wiechec E, Ghavami S and Dzięgiel P: Role of
PFKFB3 and PFKFB4 in cancer: Genetic basis, impact on disease
development/progression, and potential as therapeutic targets.
Cancers (Basel). 13:9092021. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Kashyap A, Umar SM, Dev JRA, Mathur SR,
Gogia A, Batra A, Deo SVS and Prasad CP: Combination of 3PO analog
PFK15 and siPFKL efficiently suppresses the migration, colony
formation ability, and PFK-1 activity of triple-negative breast
cancers by reducing the glycolysis. J Cell Biochem. 124:1259–1272.
2023. View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Edelmann M, Fan S, De Oliveira T,
Goldhardt T, Sartorius D, Midelashvili T, Conrads K, Paul NB,
Beißbarth T, Fleischer JR, et al: Tumor vessel normalization via
PFKFB3 inhibition alleviates hypoxia and increases tumor necrosis
in rectal cancer upon radiotherapy. Cancer Res Commun. 4:2008–2024.
2024. View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Lyu ZS, Tang SQ, Xing T, Zhou Y, Lv M, Fu
HX, Wang Y, Xu LP, Zhang XH, Lee HY, et al: The glycolytic enzyme
PFKFB3 determines bone marrow endothelial progenitor cell damage
after chemotherapy and irradiation. Haematologica. 107:2365–2380.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Larionova I, Patysheva M, Iamshchikov P,
Kazakova E, Kazakova A, Rakina M, Grigoryeva E, Tarasova A,
Afanasiev S, Bezgodova N, et al: PFKFB3 overexpression in monocytes
of patients with colon but not rectal cancer programs pro-tumor
macrophages and is indicative for higher risk of tumor relapse.
Front Immunol. 13:10805012023. View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Vezza T and Víctor VM: The HIF1α-PFKFB3
pathway: A key player in diabetic retinopathy. J Clin Endocrinol
Metab. 106:e4778–e4780. 2021. View Article : Google Scholar
|
|
133
|
Min J, Zeng T, Roux M, Lazar D, Chen L and
Tudzarova S: The role of HIF1α-PFKFB3 pathway in diabetic
retinopathy. J Clin Endocrinol Metab. 106:2505–2519. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
134
|
Xiao M, Liu D, Xu Y, Mao W and Li W: Role
of PFKFB3-driven glycolysis in sepsis. Ann Med. 55:1278–1289. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
135
|
Liu D, Xiao M, Zhou J, Wang P, Peng J, Mao
W, Hu Y, Liu Y, Yin J, Ke L and Li W: PFKFB3 promotes
sepsis-induced acute lung injury by enhancing NET formation by
CXCR4hi neutrophils. Int Immunopharmacol.
123:1107372023. View Article : Google Scholar
|
|
136
|
Zhou Z, Plug LG, Patente TA, de
Jonge-Muller ESM, Elmagd AA, van der Meulen-de Jong AE, Everts B,
Barnhoorn MC and Hawinkels LJAC: Increased stromal PFKFB3-mediated
glycolysis in inflammatory bowel disease contributes to intestinal
inflammation. Front Immunol. 13:9660672022. View Article : Google Scholar : PubMed/NCBI
|
|
137
|
Zuo J, Tang J, Lu M, Zhou Z, Li Y, Tian H,
Liu E, Gao B, Liu T and Shao P: Glycolysis rate-limiting enzymes:
Novel potential regulators of rheumatoid arthritis pathogenesis.
Front Immunol. 12:7797872021. View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Wang Y, Li H, Jiang S, Fu D, Lu X, Lu M,
Li Y, Luo D, Wu K, Xu Y, et al: The glycolytic enzyme PFKFB3 drives
kidney fibrosis through promoting histone lactylation-mediated
NF-κB family activation. Kidney Int. 106:226–240. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
139
|
Tang CJ, Xu J, Ye HY and Wang XB:
Metformin prevents PFKFB3-related aerobic glycolysis from enhancing
collagen synthesis in lung fibroblasts by regulating AMPK/mTOR
pathway. Exp Ther Med. 21:5812021. View Article : Google Scholar : PubMed/NCBI
|
|
140
|
Fu J, Li N, He M, Huang D and Zhang P:
STAT3 signaling mediates peritoneal fibrosis by activating
hyperglycolysis. Am J Transl Res. 14:7552–7565. 2022.PubMed/NCBI
|
|
141
|
Wang Y, Qu C, Liu T and Wang C: PFKFB3
inhibitors as potential anticancer agents: Mechanisms of action,
current developments, and structure-activity relationships. Eur J
Med Chem. 203:1126122020. View Article : Google Scholar : PubMed/NCBI
|
|
142
|
Zlacká J, Murár M, Addová G, Moravčík R,
Boháč A and Zeman M: Synthesis of glycolysis inhibitor PFK15 and
its synergistic action with an approved multikinase antiangiogenic
drug on human endothelial cell migration and proliferation. Int J
Mol Sci. 23:142952022. View Article : Google Scholar : PubMed/NCBI
|
|
143
|
Shi WK, Zhu XD, Wang CH, Zhang YY, Cai H,
Li XL, Cao MQ, Zhang SZ, Li KS and Sun HC: PFKFB3 blockade inhibits
hepatocellular carcinoma growth by impairing DNA repair through
AKT. Cell Death Dis. 9:4282018. View Article : Google Scholar : PubMed/NCBI
|
|
144
|
Thirusangu P, Ray U, Sarkar Bhattacharya
S, Oien DB, Jin L, Staub J, Kannan N, Molina JR and Shridhar V:
PFKFB3 regulates cancer stemness through the hippo pathway in small
cell lung carcinoma. Oncogene. 41:4003–4017. 2022. View Article : Google Scholar : PubMed/NCBI
|