|
1
|
Wong WL, Su X, Li X, Cheung CM, Klein R,
Cheng CY and Wong TY: Global prevalence of age-related macular
degeneration and disease burden projection for 2020 and 2040: A
systematic review and meta-analysis. Lancet Glob Health.
2:e106–e116. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ferris FL III, Fine SL and Hyman L:
Age-related macular degeneration and blindness due to neovascular
maculopathy. Arch Ophthalmol. 102:1640–1642. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Luttrull JK, Gray G and Bhavan SV: Vision
protection therapy for prevention of neovascular age-related
macular degeneration. Sci Rep. 13:167102023. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Noël A, Jost M, Lambert V, Lecomte J and
Rakic JM: Anti-angiogenic therapy of exudative age-related macular
degeneration: Current progress and emerging concepts. Trends Mol
Med. 13:345–352. 2007. View Article : Google Scholar : PubMed/NCBI
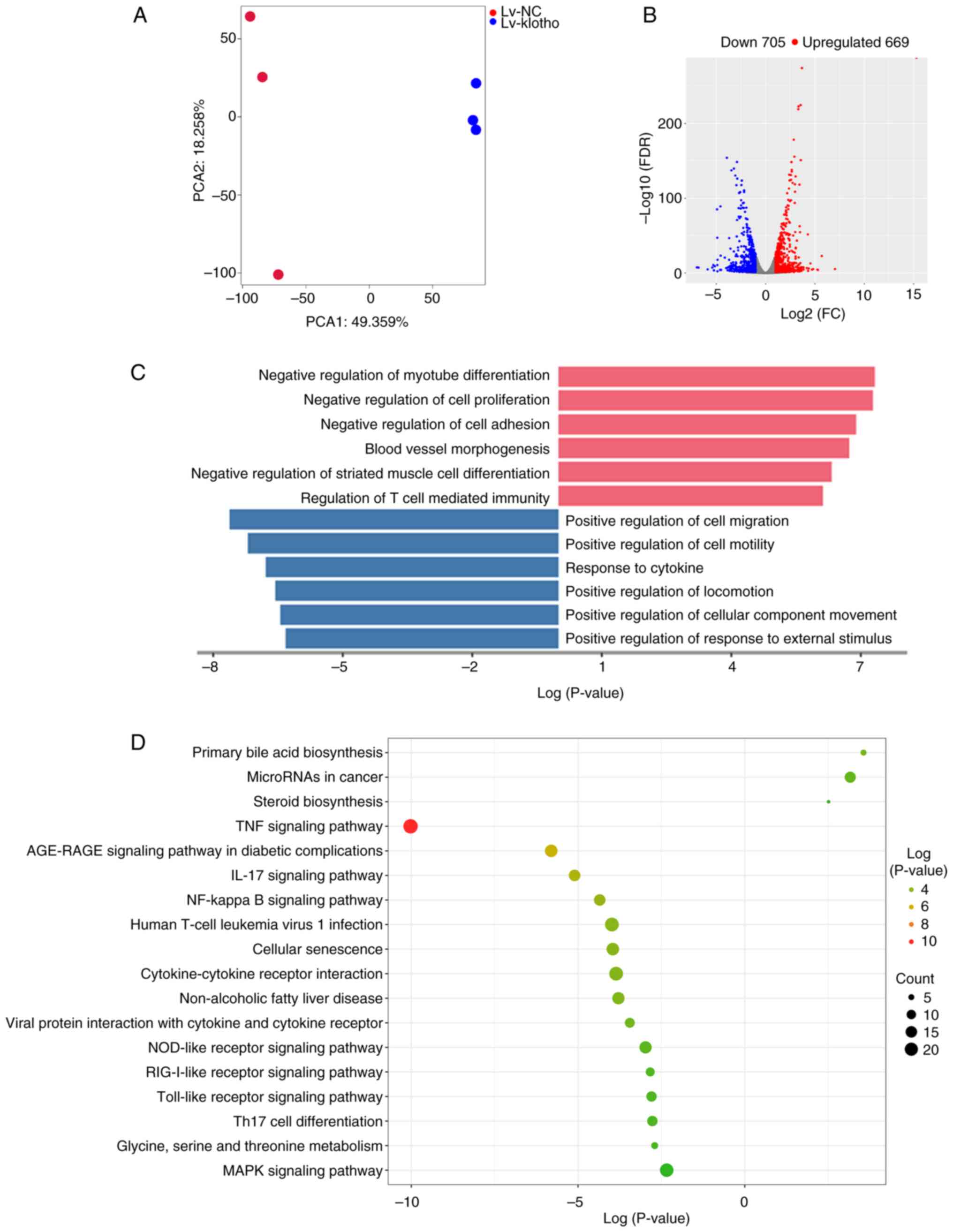
|
|
5
|
Liu D, Zhang C and Zhang J, Xu GT and
Zhang J: Molecular pathogenesis of subretinal fibrosis in
neovascular AMD focusing on epithelial-mesenchymal transformation
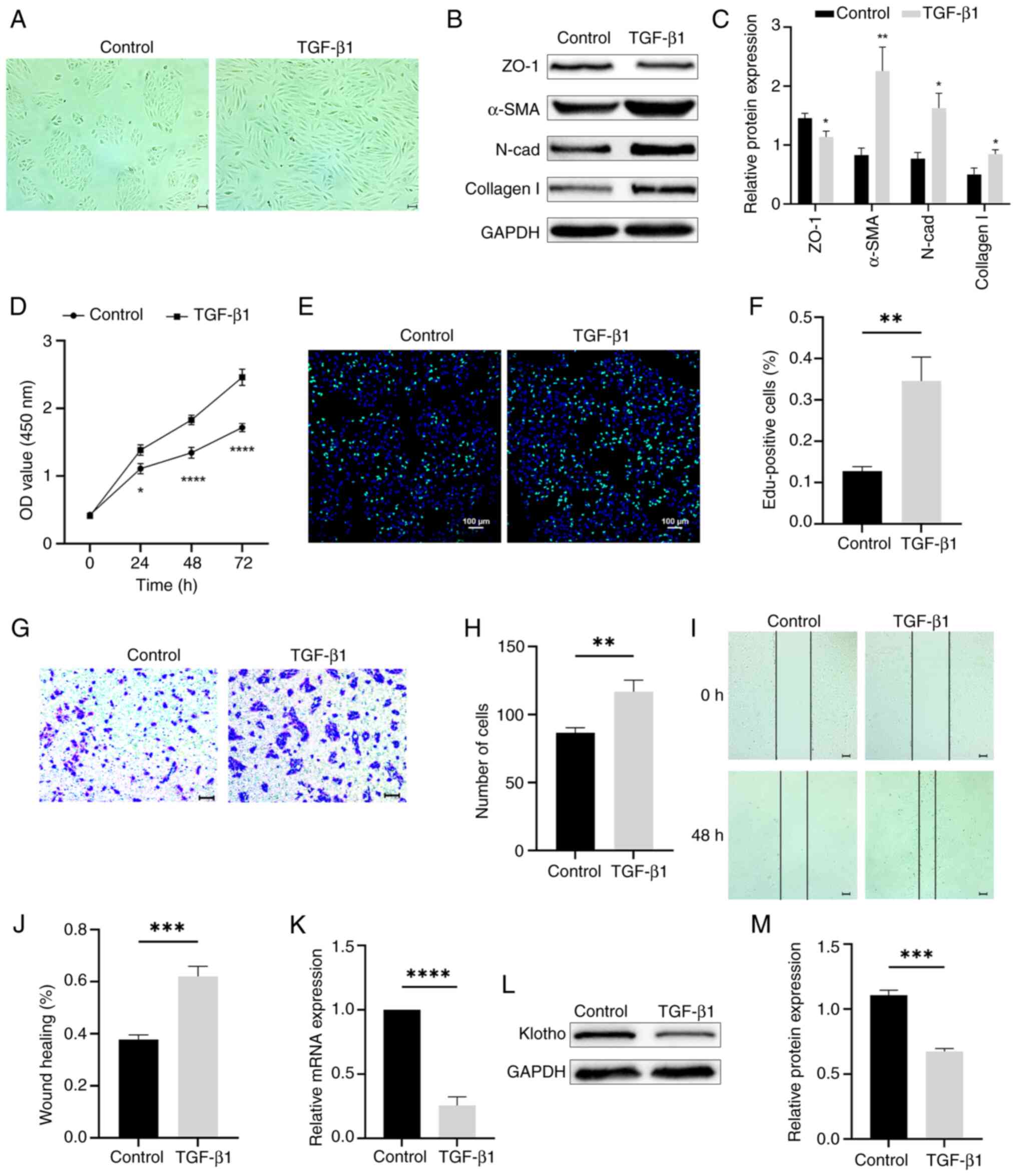
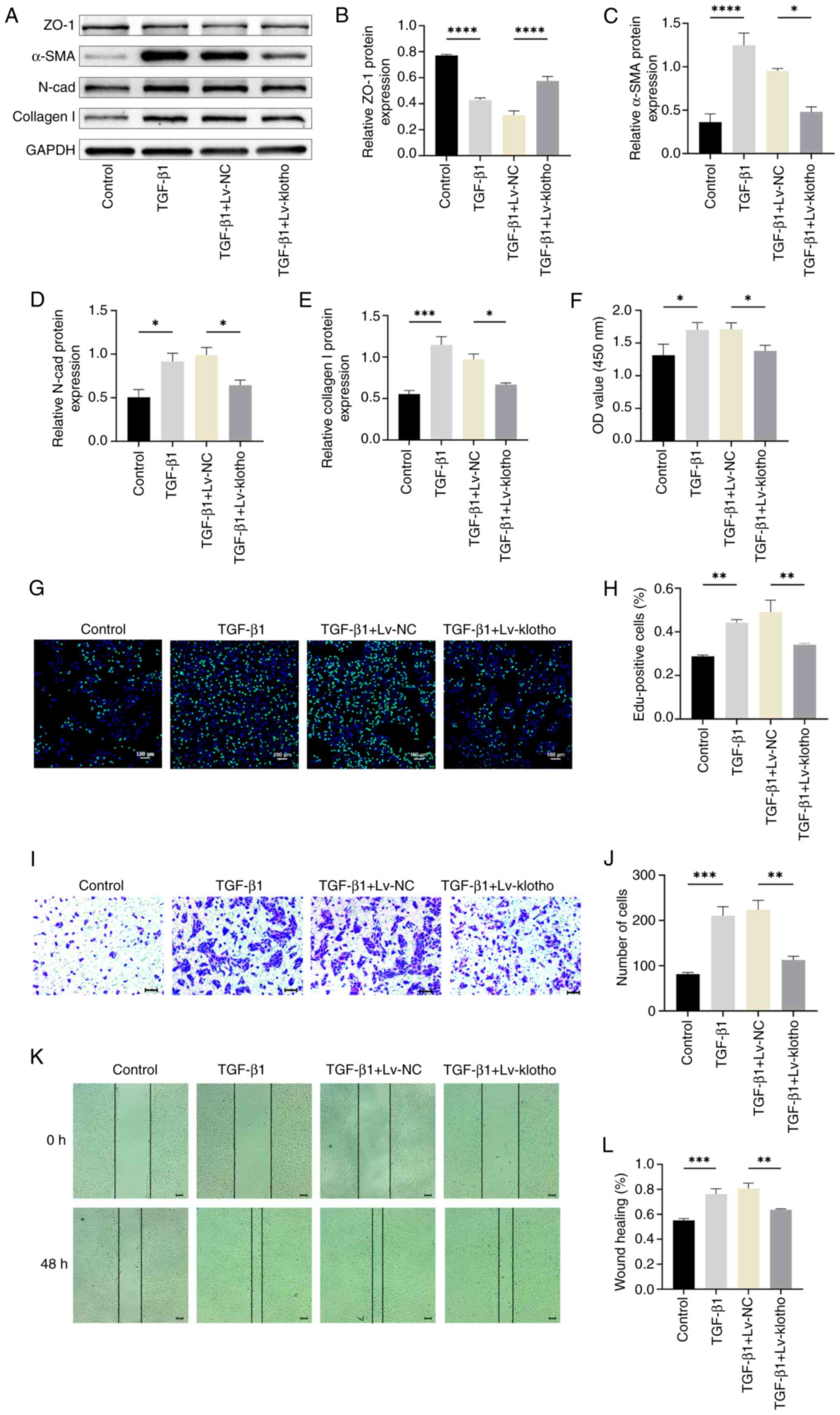
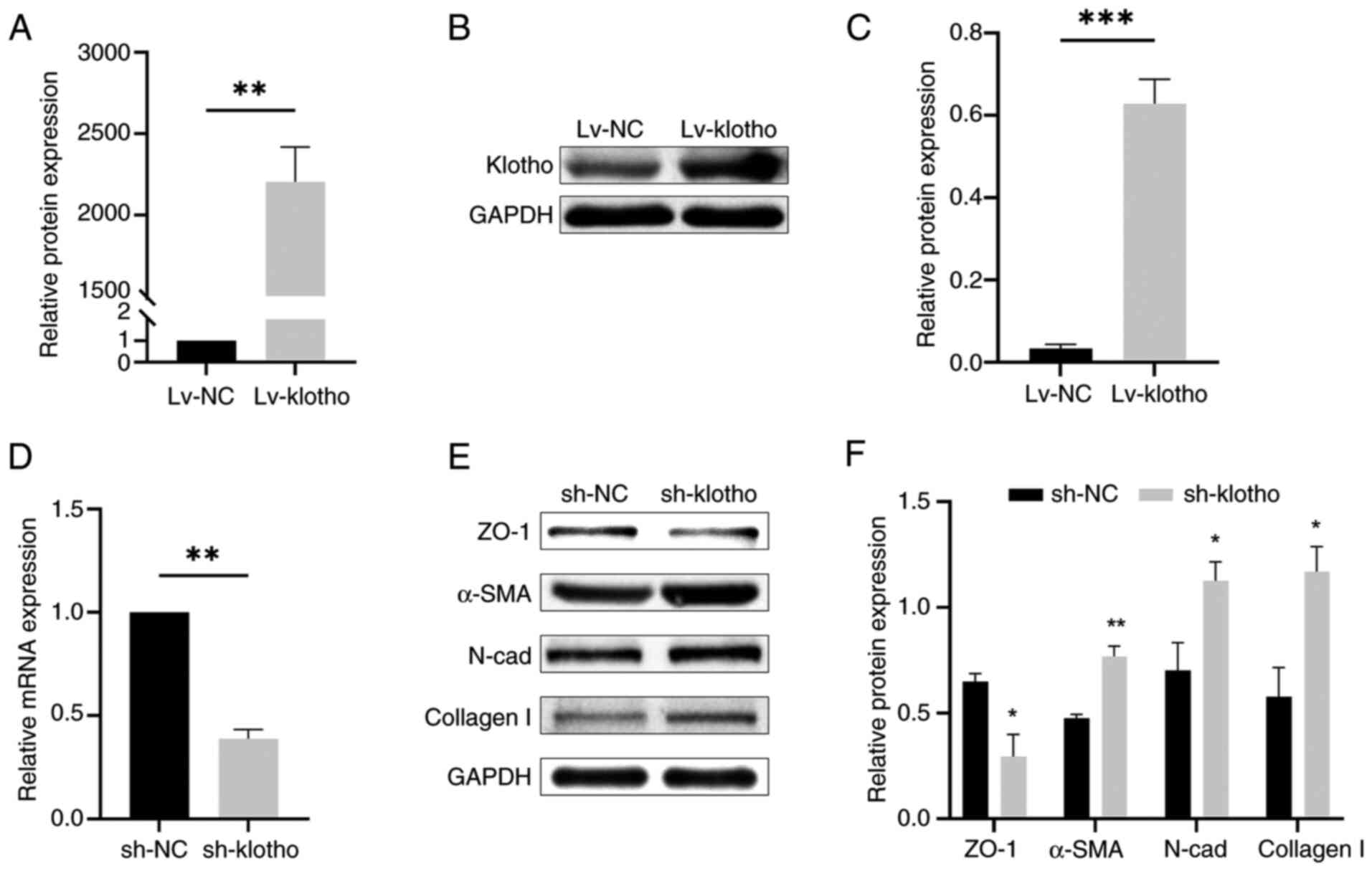
of retinal pigment epithelium. Neurobiol Dis. 185:1062502023.
View Article : Google Scholar : PubMed/NCBI
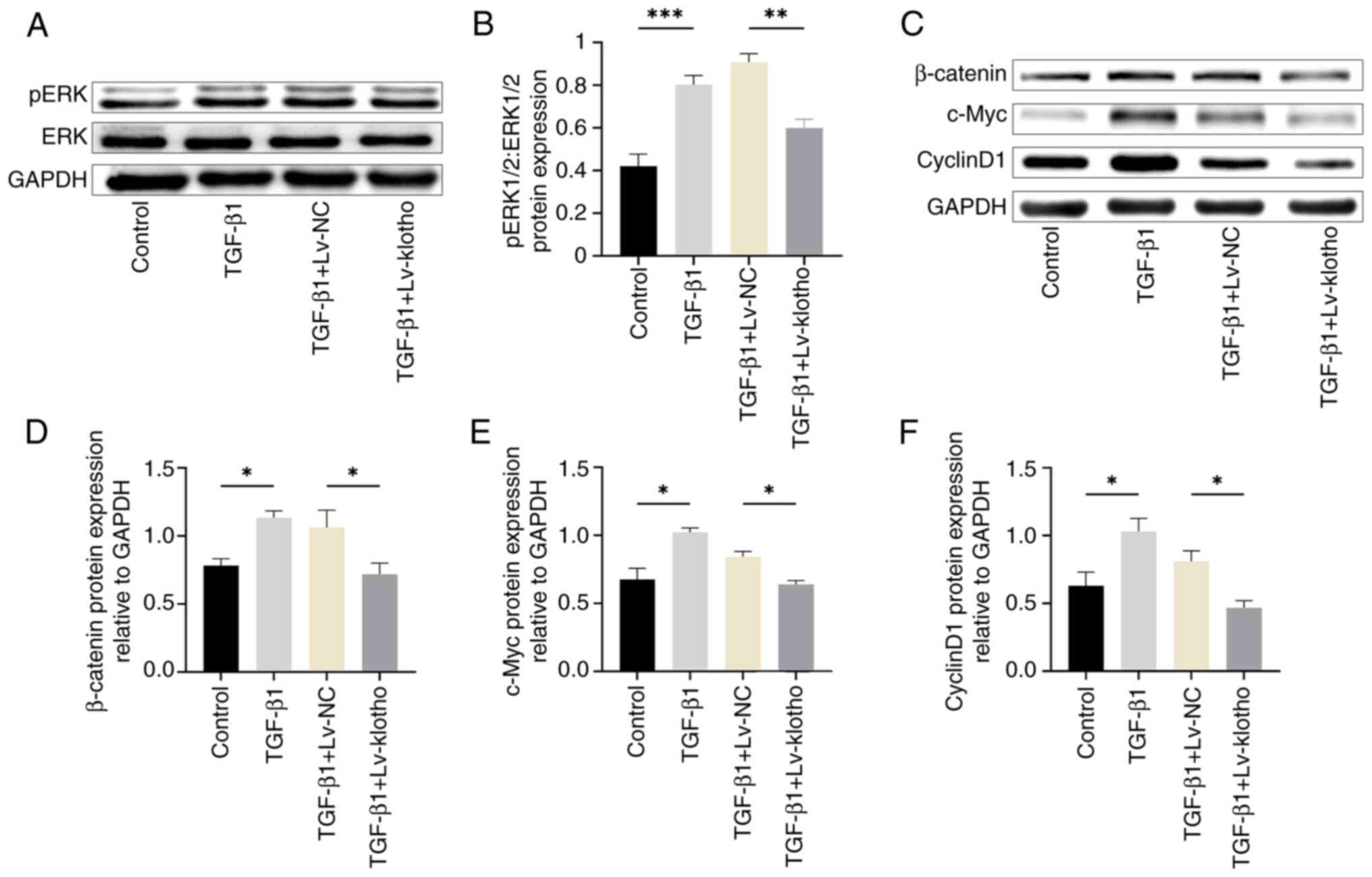
|
|
6
|
Daniel E, Pan W, Ying GS, Kim BJ, Grunwald
JE, Ferris FL III, Jaffe GJ, Toth CA, Martin DF, Fine SL, et al:
Development and course of scars in the comparison of age-related
macular degeneration treatments trials. Ophthalmology.
125:1037–1046. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ishikawa K, Kannan R and Hinton DR:
Molecular mechanisms of subretinal fibrosis in age-related macular
degeneration. Exp Eye Res. 142:19–25. 2016. View Article : Google Scholar
|
|
8
|
Little K, Llorian-Salvador M, Tang M, Du
X, Marry S, Chen M and Xu H: Macrophage to myofibroblast transition
contributes to subretinal fibrosis secondary to neovascular
age-related macular degeneration. J Neuroinflammation. 17:3552020.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Llorián-Salvador M, Byrne EM, Szczepan M,
Little K, Chen M and Xu H: Complement activation contributes to
subretinal fibrosis through the induction of
epithelial-to-mesenchymal transition (EMT) in retinal pigment
epithelial cells. J Neuroinflammation. 19:1822022. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Palko SI, Saba NJ, Bargagna-Mohan P and
Mohan R: Peptidyl arginine deiminase 4 deficiency protects against
subretinal fibrosis by inhibiting Müller glial hypercitrullination.
J Neurosci Res. 101:464–479. 2023. View Article : Google Scholar
|
|
11
|
Shu DY and Lovicu FJ: Myofibroblast
transdifferentiation: The dark force in ocular wound healing and
fibrosis. Prog Retin Eye Res. 60:44–65. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Parikh BH, Liu Z, Blakeley P, Lin Q, Singh
M, Ong JY, Ho KH, Lai JW, Bogireddi H, Tran KC, et al: A
bio-functional polymer that prevents retinal scarring through
modulation of NRF2 signalling pathway. Nat Commun. 13:27962022.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wu X, Qin B, Cheng R, Zhou R, Wang X,
Zhang Z, Mao X, Xie Z, Chen M, Jiang L, et al: Angiogenic and
fibrogenic dual-effect of gremlin1 on proliferative diabetic
retinopathy. Int J Biol Sci. 20:897–915. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Corano Scheri K, Hsieh YW, Jeong E and
Fawzi AA: Limited Hyperoxia-induced proliferative retinopathy
(LHIPR) as a model of retinal fibrosis, angiogenesis, and
inflammation. Cells. 12:24682023. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ma X, Han S, Liu Y, Chen Y, Li P, Liu X,
Chang L, Chen YA, Chen F, Hou Q and Hou L: DAPL1 prevents
epithelial-mesenchymal transition in the retinal pigment epithelium
and experimental proliferative vitreoretinopathy. Cell Death Dis.
14:1582023. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Abu El-Asrar AM, De Hertogh G, Allegaert
E, Nawaz MI, Abouelasrar Salama S, Gikandi PW, Opdenakker G and
Struyf S: Macrophage-myofibroblast transition contributes to
myofibroblast formation in proliferative vitreoretinal disorders.
Int J Mol Sci. 24:135102023. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Xin Z, Ma Z, Hu W, Jiang S, Yang Z, Li T,
Chen F, Jia G and Yang Y: FOXO1/3: Potential suppressors of
fibrosis. Ageing Res Rev. 41:42–52. 2018. View Article : Google Scholar
|
|
18
|
Kuro-o M, Matsumura Y, Aizawa H, Kawaguchi
H, Suga T, Utsugi T, Ohyama Y, Kurabayashi M, Kaname T, Kume E, et
al: Mutation of the mouse klotho gene leads to a syndrome
resembling ageing. Nature. 390:45–51. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kim JH, Hwang KH, Park KS, Kong ID and Cha
SK: Biological role of anti-aging protein klotho. J Lifestyle Med.
5:1–6. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Hung Y, Chung CC, Chen YC, Kao YH, Lin WS,
Chen SA and Chen YJ: Klotho modulates pro-fibrotic activities in
human atrial fibroblasts through inhibition of phospholipase C
signaling and suppression of store-operated calcium entry.
Biomedicines. 10:15742022. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Liu Q, Zhu LJ, Waaga-Gasser AM, Ding Y,
Cao M, Jadhav SJ, Kirollos S, Shekar PS, Padera RF, Chang YC, et
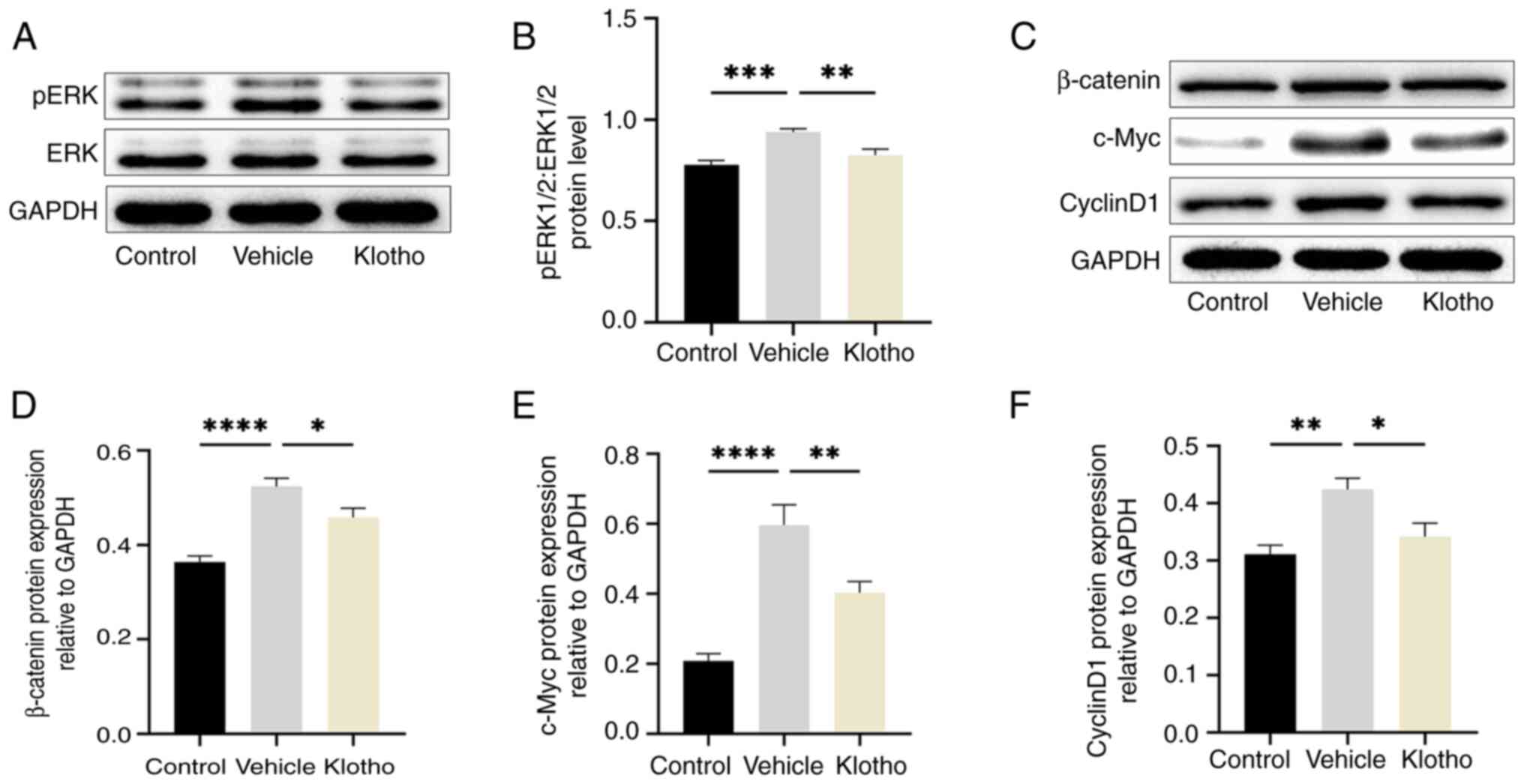
al: The axis of local cardiac endogenous klotho-TGF-β1-Wnt
signaling mediates cardiac fibrosis in human. J Mol Cell Cardiol.
136:113–124. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Yang YL, Xue M, Jia YJ, Hu F, Zheng ZJ,
Wang L, Si ZK and Xue YM: Long noncoding RNA NEAT1 is involved in
the protective effect of klotho on renal tubular epithelial cells
in diabetic kidney disease through the ERK1/2 signaling pathway.
Exp Mol Med. 52:266–280. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Kadoya H, Satoh M, Nishi Y, Kondo M, Wada
Y, Sogawa Y, Kidokoro K, Nagasu H, Sasaki T and Kashihara N: Klotho
is a novel therapeutic target in peritoneal fibrosis via Wnt
signaling inhibition. Nephrol Dial Transplant. 35:773–781. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Barnes JW, Duncan D, Helton S, Hutcheson
S, Kurundkar D, Logsdon NJ, Locy M, Garth J, Denson R, Farver C, et
al: Role of fibroblast growth factor 23 and klotho cross talk in
idiopathic pulmonary fibrosis. Am J Physiol Lung Cell Mol Physiol.
317:L141–L154. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Reish NJ, Maltare A, McKeown AS, Laszczyk
AM, Kraft TW, Gross AK and King GD: The age-regulating protein
klotho is vital to sustain retinal function. Invest Ophthalmol Vis
Sci. 54:6675–6685. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Kokkinaki M, Abu-Asab M, Gunawardena N,
Ahern G, Javidnia M, Young J and Golestaneh N: Klotho regulates
retinal pigment epithelial functions and protects against oxidative
stress. J Neurosci. 33:16346–16359. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Wen X, Li S, Zhang Y, Zhu L, Xi X, Zhang S
and Li Y: Recombinant human klotho protects against hydrogen
peroxide-mediated injury in human retinal pigment epithelial cells
via the PI3K/Akt-Nrf2/HO-1 signaling pathway. Bioengineered.
13:11767–11781. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Jang HY, Kim SJ, Park KS and Kim JH:
Klotho prevents transforming growth factor-β2-induced
senescent-like morphological changes in the retinal pigment
epithelium. Cell Death Dis. 14:3342023. View Article : Google Scholar
|
|
29
|
Xie L, Wang Y, Li Q, Ji X, Tu Y, Du S, Lou
H, Zeng X, Zhu L, Zhang J and Zhu M: The
HIF-1α/p53/miRNA-34a/klotho axis in retinal pigment epithelial
cells promotes subretinal fibrosis and exacerbates choroidal
neovascularization. J Cell Mol Med. 25:1700–1711. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Xu L, Li S, Shabala S, Jian T and Zhang W:
Plants grown in parafilm-wrapped petri dishes are stressed and
possess altered gene expression profile. Front Plant Sci.
10:6372019. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Bakhtiarizadeh MR, Salehi A, Alamouti AA,
Abdollahi-Arpanahi R and Salami SA: Deep transcriptome analysis
using RNA-Seq suggests novel insights into molecular aspects of
fat-tail metabolism in sheep. Sci Rep. 9:92032019. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Yu G, Wang LG, Han Y and He QY:
clusterProfiler: An R package for comparing biological themes among
gene clusters. OMICS. 16:284–287. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Kanehisa M and Goto S: KEGG: Kyoto
encyclopedia of genes and genomes. Nucleic Acids Res. 28:27–30.
2000. View Article : Google Scholar
|
|
34
|
Kinoshita S, Noda K, Tagawa Y, Inafuku S,
Dong Y, Fukuhara J, Dong Z, Ando R, Kanda A and Ishida S: Genistein
attenuates choroidal neovascularization. J Nutr Biochem.
25:1177–1182. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
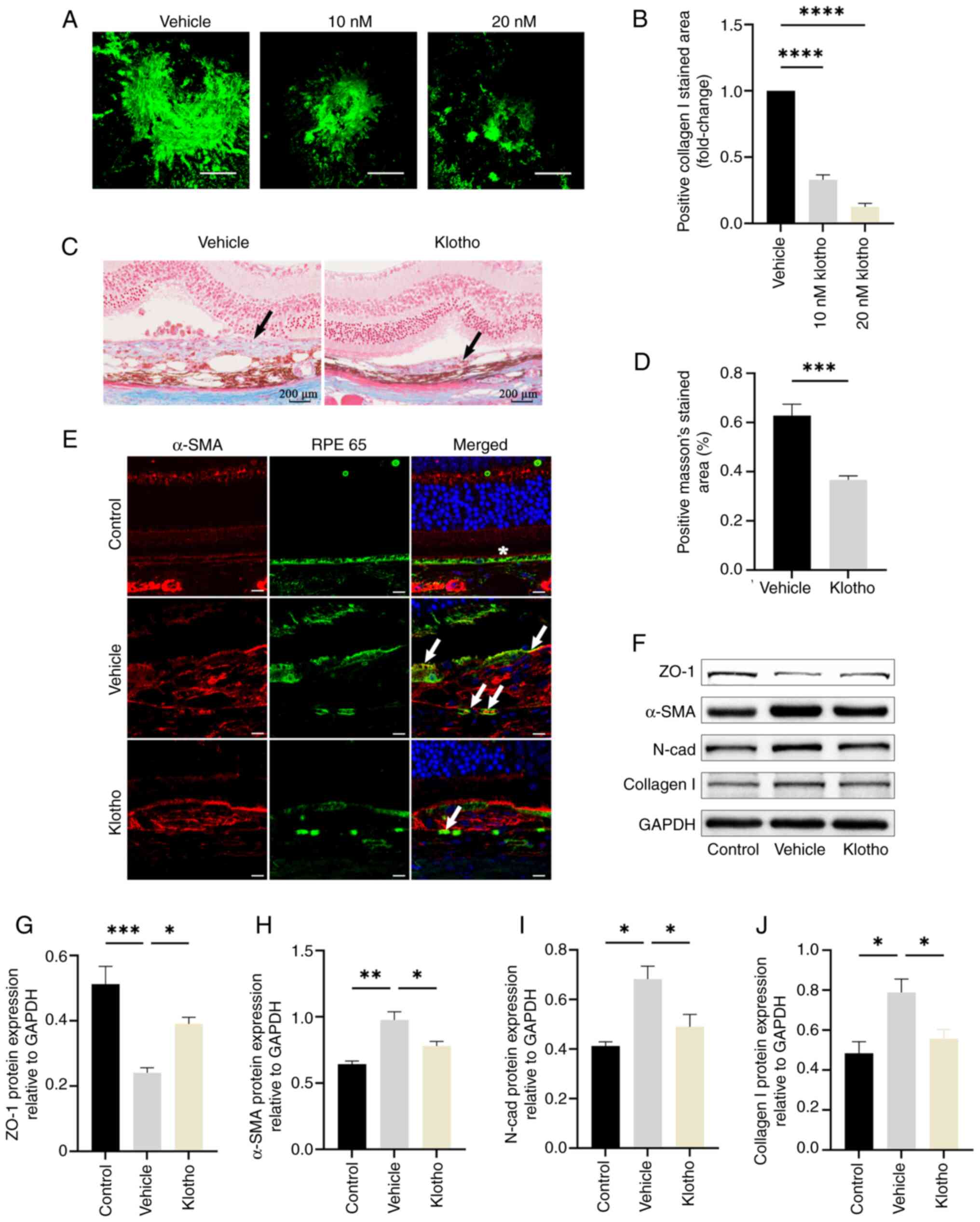
Ma X, Takahashi Y, Wu W, Chen J, Dehdarani
M, Liang W, Shin YH, Benyajati S and Ma JX: Soluble very
low-density lipoprotein receptor (sVLDLR) inhibits fibrosis in
neovascular age-related macular degeneration. FASEB J.
35:e220582021. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar
|
|
37
|
Ren LL, Miao H, Wang YN, Liu F, Li P and
Zhao YY: TGF-β as A master regulator of aging-associated tissue
fibrosis. Aging Dis. 14:1633–1650. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Liu D, Du J, Xie H, Tian H, Lu L, Zhang C,
Xu GT and Zhang J: Wnt5a/β-catenin-mediated epithelial-mesenchymal
transition: A key driver of subretinal fibrosis in neovascular
age-related macular degeneration. J Neuroinflammation. 21:752024.
View Article : Google Scholar
|
|
39
|
Ilg MM, Bustin SA, Ralph DJ and Cellek S:
TGF-β1 induces formation of TSG-6-enriched extracellular vesicles
in fibroblasts which can prevent myofibroblast transformation by
modulating Erk1/2 phosphorylation. Sci Rep. 14:123892024.
View Article : Google Scholar
|
|
40
|
Chang B, Kim J, Jeong D, Jeong Y, Jeon S,
Jung SI, Yang Y, Kim KI, Lim JS, Kim C and Lee MS: Klotho inhibits
the capacity of cell migration and invasion in cervical cancer.
Oncol Rep. 28:1022–1028. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Barikian A, Mahfoud Z, Abdulaal M, Safar A
and Bashshur ZF: Induction with intravitreal bevacizumab every two
weeks in the management of neovascular age-related macular
degeneration. Am J Ophthalmol. 159:131–137. 2015. View Article : Google Scholar
|
|
42
|
Wolff B, Macioce V, Vasseur V, Castelnovo
L, Michel G, Nguyen V, Daien V, Mauget-Faÿsse M and Gillies M:
Ten-year outcomes of anti-vascular endothelial growth factor
treatment for neovascular age-related macular disease: A
single-centre French study. Clin Exp Ophthalmol. 48:636–643. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Daley R, Maddipatla V, Ghosh S, Chowdhury
O, Hose S, Zigler JS Jr, Sinha D and Liu H: Aberrant Akt2 signaling
in the RPE may contribute to retinal fibrosis process in diabetic
retinopathy. Cell Death Discov. 9:2432023. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Zhang C, Zhang Y, Hu X, Zhao Z, Chen Z,
Wang X, Zhang Z, Jin H and Zhang J: Luteolin inhibits subretinal
fibrosis and epithelial-mesenchymal transition in laser-induced
mouse model via suppression of Smad2/3 and YAP signaling.
Phytomedicine. 116:1548652023. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Lee H, Han JH, Kang YJ, Hwangbo H, Yoon A,
Kim HS, Lee D, Lee SY, Choi BH, Kim JJ, et al: CD82 attenuates
TGF-β1-mediated epithelial-mesenchymal transition by blocking
smad-dependent signaling in ARPE-19 cells. Front Pharmacol.
13:9910562022. View Article : Google Scholar
|
|
46
|
Fuchs HR, Meister R, Lotke R and Framme C:
The microRNAs miR-302d and miR-93 inhibit TGFB-mediated EMT and
VEGFA secretion from ARPE-19 cells. Exp Eye Res. 201:1082582020.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Wang X, Ma W, Han S, Meng Z, Zhao L, Yin
Y, Wang Y and Li J: TGF-β participates choroid neovascularization
through Smad2/3-VEGF/TNF-α signaling in mice with laser-induced wet
age-related macular degeneration. Sci Rep. 7:96722017. View Article : Google Scholar
|
|
48
|
Tosi GM, Caldi E, Neri G, Nuti E,
Marigliani D, Baiocchi S, Traversi C, Cevenini G, Tarantello A,
Fusco F, et al: HTRA1 and TGF-β1 concentrations in the aqueous
humor of patients with neovascular age-related macular
degeneration. Invest Ophthalmol Vis Sci. 58:162–167. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Amin R, Puklin JE and Frank RN: Growth
factor localization in choroidal neovascular membranes of
age-related macular degeneration. Invest Ophthalmol Vis Sci.
35:3178–3188. 1994.PubMed/NCBI
|
|
50
|
Bracken CP and Goodall GJ: The many
regulators of epithelial-mesenchymal transition. Nat Rev Mol Cell
Biol. 23:89–90. 2022. View Article : Google Scholar
|
|
51
|
Fan Y, Cui C, Rosen CJ, Sato T, Xu R, Li
P, Wei X, Bi R, Yuan Q and Zhou C: Klotho in
Osx+-mesenchymal progenitors exerts pro-osteogenic and
anti-inflammatory effects during mandibular alveolar bone formation
and repair. Signal Transduct Target Ther. 7:1552022. View Article : Google Scholar
|
|
52
|
Abraham CR and Li A: Aging-suppressor
klotho: Prospects in diagnostics and therapeutics. Ageing Res Rev.
82:1017662022. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Valiño-Rivas L, Cuarental L, Ceballos MI,
Pintor-Chocano A, Perez-Gomez MV, Sanz AB, Ortiz A and Sanchez-Niño
MD: Growth differentiation factor-15 preserves klotho expression in
acute kidney injury and kidney fibrosis. Kidney Int. 101:1200–1215.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Xu Y and Sun Z: Molecular basis of klotho:
From gene to function in aging. Endocr Rev. 36:174–193. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Xue M, Yang F, Le Y, Yang Y, Wang B, Jia
Y, Zheng Z and Xue Y: Klotho protects against diabetic kidney
disease via AMPK- and ERK-mediated autophagy. Acta Diabetol.
58:1413–1423. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Shi M, Flores B, Gillings N, Bian A, Cho
HJ, Yan S, Liu Y, Levine B, Moe OW and Hu MC: αKlotho mitigates
progression of AKI to CKD through activation of autophagy. J Am Soc
Nephrol. 27:2331–2345. 2016. View Article : Google Scholar
|
|
57
|
Liu Y, Bi X, Xiong J, Han W, Xiao T, Xu X,
Yang K, Liu C, Jiang W, He T, et al: MicroRNA-34a promotes renal
fibrosis by downregulation of klotho in tubular epithelial cells.
Mol Ther. 27:1051–1065. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Liu QF, Ye JM, Yu LX, Dong XH, Feng JH,
Xiong Y, Gu XX and Li SS: Klotho mitigates cyclosporine A
(CsA)-induced epithelial-mesenchymal transition (EMT) and renal
fibrosis in rats. Int Urol Nephrol. 49:345–352. 2017. View Article : Google Scholar
|
|
59
|
Ma Z, Liu J, Li J, Jiang H and Kong J:
Klotho levels are decreased and associated with enhanced oxidative
stress and inflammation in the aqueous humor in patients with
exudative age-related macular degeneration. Ocul Immunol Inflamm.
30:630–637. 2022. View Article : Google Scholar
|
|
60
|
Zhou S, Hum J, Taskintuna K, Olaya S,
Steinman J, Ma J and Golestaneh N: The anti-aging hormone klotho
promotes retinal pigment epithelium cell viability and metabolism
by activating the AMPK/PGC-1α pathway. Antioxidants (Basel).
12:3852023. View Article : Google Scholar
|
|
61
|
Wu D, Kanda A, Liu Y, Kase S, Noda K and
Ishida S: Galectin-1 promotes choroidal neovascularization and
subretinal fibrosis mediated via epithelial-mesenchymal transition.
FASEB J. 33:2498–2513. 2019. View Article : Google Scholar
|