|
1
|
Silva PHI and Mohebbi N: Kidney metabolism
and acid-base control: Back to the basics. Pflugers Arch.
474:919–934. 2022. View Article : Google Scholar
|
|
2
|
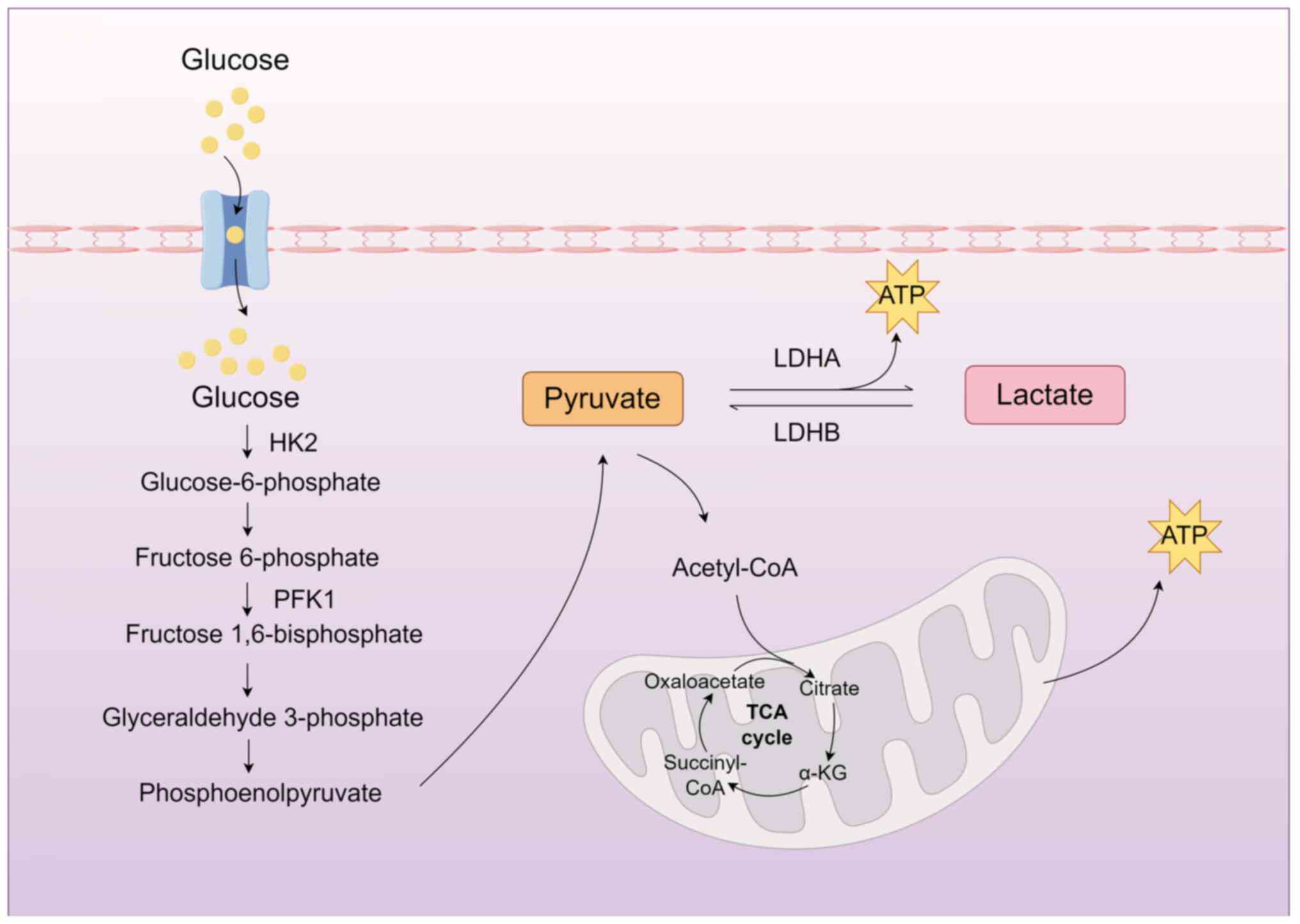
Chen Y, Fry BC and Layton AT: Modeling
glucose metabolism and lactate production in the kidney. Math
Biosci. 289:116–129. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Reddy AJ, Lam SW, Bauer SR and Guzman JA:
Lactic acidosis: Clinical implications and management strategies.
Clevel Clin J Med. 82:615–624. 2015. View Article : Google Scholar
|
|
4
|
Azushima K, Kovalik JP, Yamaji T, Ching J,
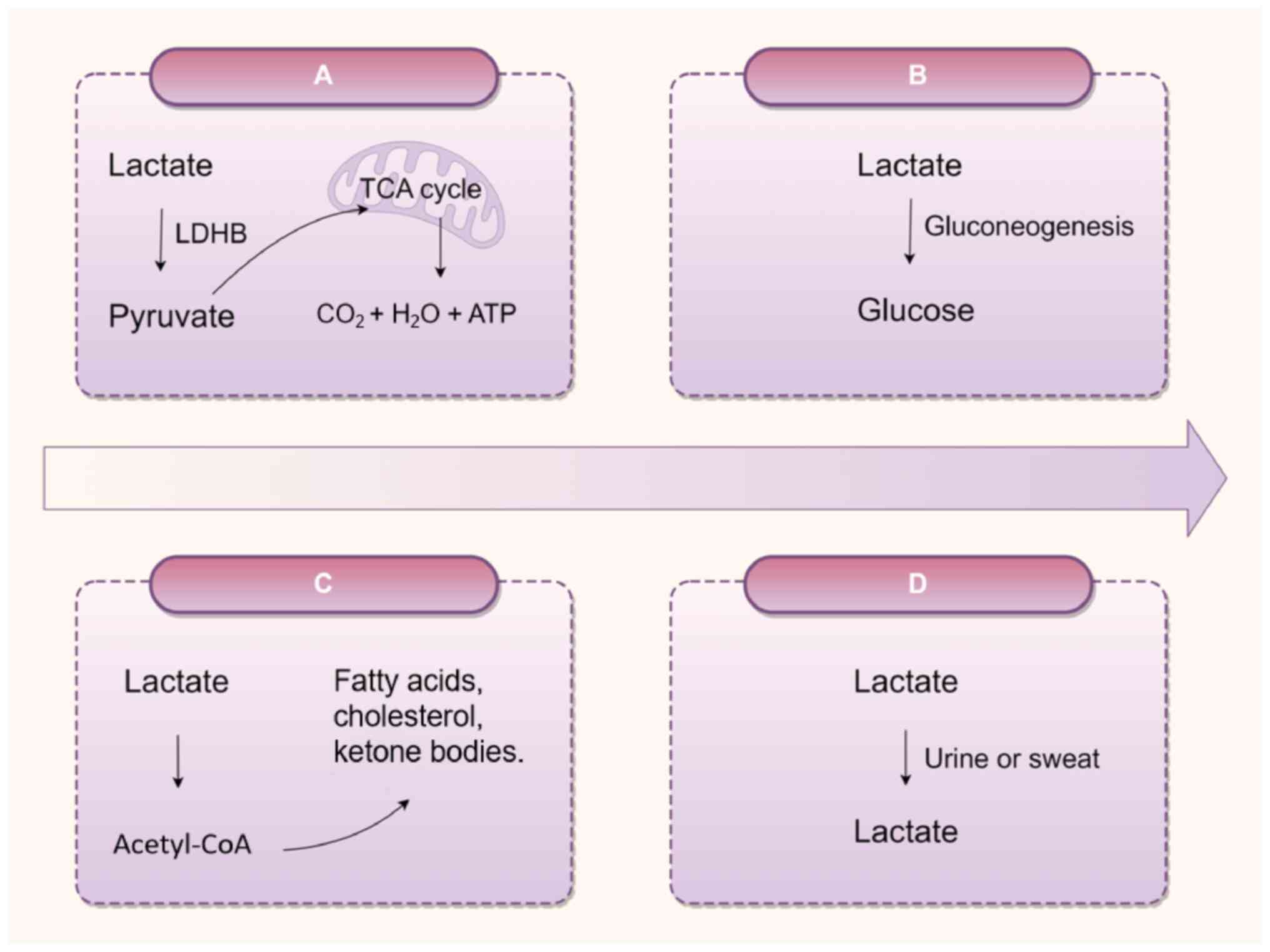
Chng TW, Guo J, Liu JJ, Nguyen M, Sakban RB, George SE, et al:
Abnormal lactate metabolism is linked to albuminuria and kidney
injury in diabetic nephropathy. Kidney Int. 104:1135–1149. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Zhang X, Chen J, Lin R, Huang Y, Wang Z,
Xu S, Wang L, Chen F, Zhang J, Pan K and Yin Z: Lactate drives
epithelial-mesenchymal transition in diabetic kidney disease via
the H3K14la/KLF5 pathway. Redox Biol. 75:1032462024. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wang Y, Li H, Jiang S, Fu D, Lu X, Lu M,
Li Y, Luo D, Wu K, Xu Y, et al: The glycolytic enzyme PFKFB3 drives
kidney fibrosis through promoting histone lactylation-mediated
NF-κB family activation. Kidney Int. 106:226–240. 2024. View Article : Google Scholar : PubMed/NCBI
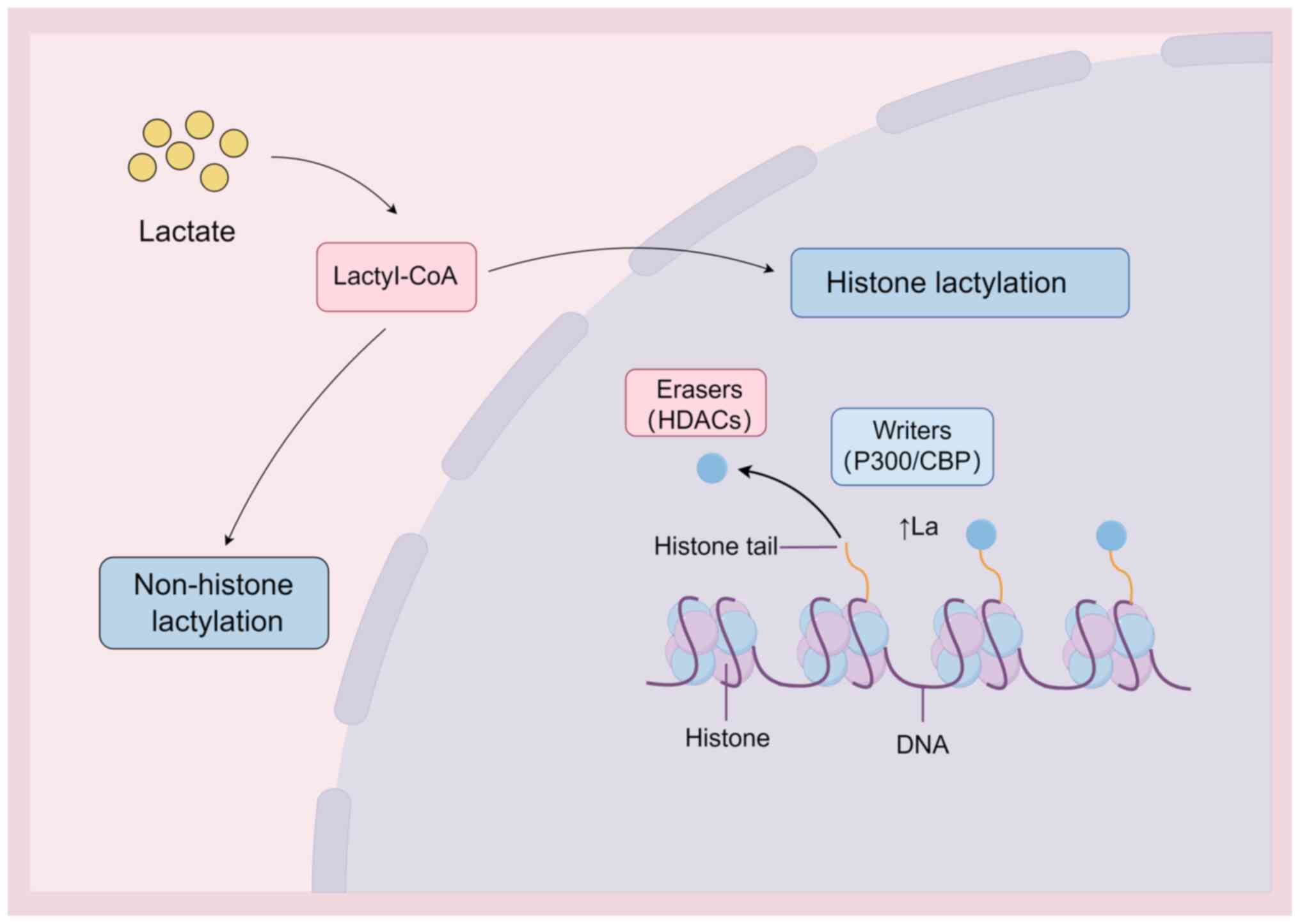
|
|
7
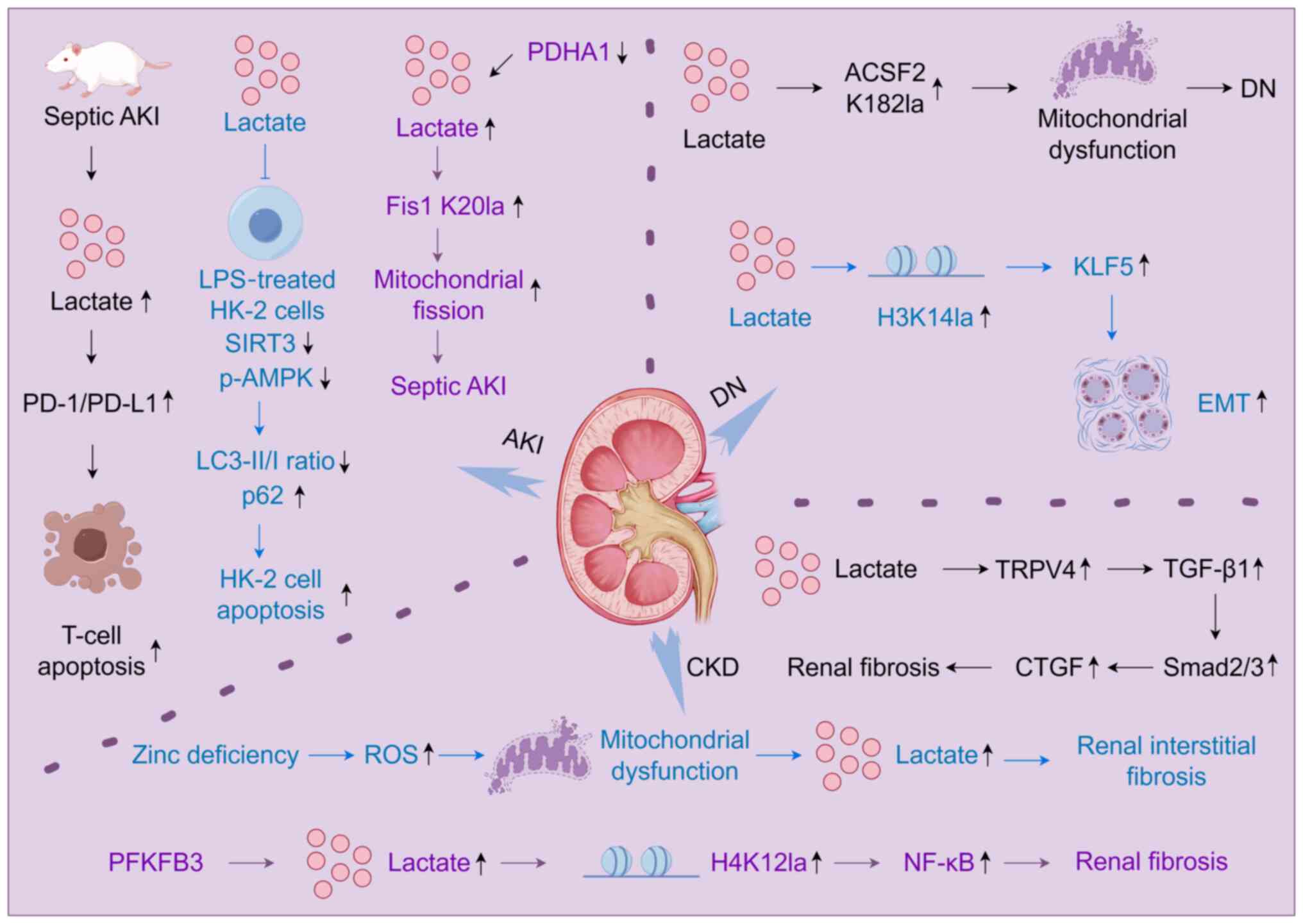
|
Verissimo T, Faivre A, Rinaldi A,
Lindenmeyer M, Delitsikou V, Veyrat-Durebex C, Heckenmeyer C,
Fernandez M, Berchtold L, Dalga D, et al: Decreased renal
gluconeogenesis is a hallmark of chronic kidney disease. J Am Soc
Nephrol. 33:810–827. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Rabinowitz JD and Enerbäck S: Lactate: The
ugly duckling of energy metabolism. Nat Metab. 2:566–571. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Merkuri F, Rothstein M and Simoes-Costa M:
Histone lactylation couples cellular metabolism with developmental
gene regulatory networks. Nat Commun. 15:902024. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Li J, Hou W, Zhao Q, Han W, Cui H, Xiao S,
Zhu L, Qu J, Liu X, Cong W, et al: Lactate regulates major zygotic
genome activation by H3K18 lactylation in mammals. Natl Sci Rev.
11:nwad2952024. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Dai W, Wu G, Liu K, Chen Q, Tao J, Liu H
and Shen M: Lactate promotes myogenesis via activating H3K9
lactylation-dependent up-regulation of Neu2 expression. J Cachexia
Sarcopenia Muscle. 14:2851–2865. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Fan W, Zeng S, Wang X, Wang G, Liao D, Li
R, He S, Li W, Huang J, Li X, et al: A feedback loop driven by H3K9
lactylation and HDAC2 in endothelial cells regulates VEGF-induced
angiogenesis. Genome Biol. 25:1652024. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Minami E, Sasa K, Yamada A, Kawai R,
Yoshida H, Nakano H, Maki K and Kamijo R: Lactate-induced histone
lactylation by p300 promotes osteoblast differentiation. PLoS One.
18:e02936762023. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Trujillo MN, Jennings EQ, Hoffman EA,
Zhang H, Phoebe AM, Mastin GE, Kitamura N, Reisz JA, Megill E,
Kantner D, et al: Lactoylglutathione promotes inflammatory
signaling in macrophages through histone lactoylation. Mol Metab.
81:1018882024. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kierans SJ and Taylor CT: Glycolysis: A
multifaceted metabolic pathway and signaling hub. J Biol Chem.
300:1079062024. View Article : Google Scholar
|
|
16
|
Luengo A, Li Z, Gui DY, Sullivan LB,
Zagorulya M, Do BT, Ferreira R, Naamati A, Ali A, Lewis CA, et al:
Increased demand for NAD+ relative to ATP drives aerobic
glycolysis. Mol Cell. 81:691–707.e6. 2021. View Article : Google Scholar :
|
|
17
|
Wang L, Pavlou S, Du X, Bhuckory M, Xu H
and Chen M: Glucose transporter 1 critically controls microglial
activation through facilitating glycolysis. Mol Neurodegener.
14:22019. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Yin X, Choudhury M, Kang JH, Schaefbauer
KJ, Jung MY, Andrianifahanana M, Hernandez DM and Leof EB:
Hexokinase 2 couples glycolysis with the profibrotic actions of
TGF-β. Sci Signal. 12:eaax40672019. View Article : Google Scholar
|
|
19
|
Nishioku T, Anzai R, Hiramatsu S, Terazono
A, Nakao M and Moriyama M: Lactate dehydrogenase A inhibition
prevents RANKL-induced osteoclastogenesis by reducing enhanced
glycolysis. J Pharmacol Sci. 153:197–207. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kim E, Hwang Y, Kim H, Kim GU, Ryu YC,
Yoon M and Choi KY: Pyruvate Kinase M2 accelerates cutaneous wound
healing via glycolysis and Wnt/β-catenin signaling. Pharmaceutics.
15:20282023. View Article : Google Scholar
|
|
21
|
Li J, Ma P, Liu Z and Xie J: L- and
D-lactate: Unveiling their hidden functions in disease and health.
Cell Commun Signal. 23:1342025. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Heim CE, Bosch ME, Yamada KJ, Aldrich AL,
Chaudhari SS, Klinkebiel D, Gries CM, Alqarzaee AA, Li Y, Thomas
VC, et al: Lactate production by Staphylococcus aureus biofilm
inhibits HDAC11 to reprogram the host immune response during
persistent infection. Nat Microbiol. 5:1271–1284. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Monroe GR, van Eerde AM, Tessadori F,
Duran KJ, Savelberg SMC, van Alfen JC, Terhal PA, van der Crabben
SN, Lichtenbelt KD, Fuchs SA, et al: Identification of human D
lactate dehydrogenase deficiency. Nat Commun. 10:14772019.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Vernon C and LeTourneau JL: Lactic
acidosis: Recognition, kinetics, and associated prognosis. Critical
Care Clinics. 26:255–283. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Emhoff CAW and Messonnier LA: Concepts of
lactate metabolic clearance rate and lactate clamp for metabolic
inquiry: A Mini-review. Nutrients. 15:32132023. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Huang T, Liang Z, Wang K, Miao X and Zheng
L: Novel insights into athlete physical recovery concerning lactate
metabolism, lactate clearance and fatigue monitoring: A
comprehensive review. Front Physiol. 16:14597172025. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Lin Y, Wang Y and Li P: Mutual regulation
of lactate dehydrogenase and redox robustness. Front Physiol.
13:10384212022. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Adeva M, González-Lucán M, Seco M and
Donapetry C: Enzymes involved in l-lactate metabolism in humans.
Mitochondrion. 13:615–629. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Wei T, Guo Y, Huang C, Sun M, Zhou B, Gao
J and Shen W: Fibroblast-to-cardiomyocyte lactate shuttle modulates
hypertensive cardiac remodelling. Cell Biosci. 13:1512023.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Brooks GA, Curl CC, Leija RG, Osmond AD,
Duong JJ and Arevalo JA: Tracing the lactate shuttle to the
mitochondrial reticulum. Exp Mol Med. 54:1332–1347. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Zhang L, Xin C, Wang S, Zhuo S, Zhu J, Li
Z, Liu Y, Yang L and Chen Y: Lactate transported by MCT1 plays an
active role in promoting mitochondrial biogenesis and enhancing TCA
flux in skeletal muscle. Sci Adv. 10:eadn45082024. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Contreras-Baeza Y, Sandoval PY, Alarcón R,
Galaz A, Cortés-Molina F, Alegría K, Baeza-Lehnert F, Arce-Molina
R, Guequén A, Flores CA, et al: Monocarboxylate transporter 4
(MCT4) is a high affinity transporter capable of exporting lactate
in high-lactate microenvironments. J Biol Chem. 294:20135–20147.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Kobayashi M, Narumi K, Furugen A and Iseki
K: Transport function, regulation, and biology of human
monocarboxylate transporter 1 (hMCT1) and 4 (hMCT4). Pharmacol
Ther. 226:1078622021. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Yanase H, Takebe K, Nio-Kobayashi J,
Takahashi-Iwanaga H and Iwanaga T: Cellular expression of a
sodium-dependent monocarboxylate transporter (Slc5a8) and the MCT
family in the mouse kidney. Histochem Cell Biol. 130:957–966. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Becker HM, Mohebbi N, Perna A, Ganapathy
V, Capasso G and Wagner CA: Localization of members of MCT
monocarboxylate transporter family Slc16 in the kidney and
regulation during metabolic acidosis. Am J Physiol Renal Physiol.
299:F141–F154. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Osis G, Traylor AM, Black LM, Spangler D,
George JF, Zarjou A, Verlander JW and Agarwal A: Expression of
lactate dehydrogenase A and B isoforms in the mouse kidney. Am J
Physiol Renal Physiol. 320:F706–F718. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Feng Y, Sun Z, Fu J, Zhong F, Zhang W, Wei
C, Chen A, Liu BC, He JC and Lee K: Podocyte-derived soluble
RARRES1 drives kidney disease progression through direct podocyte
and proximal tubular injury. Kidney Int. 106:50–66. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Zhao Y, Fan S, Zhu H, Zhao Q, Fang Z, Xu
D, Lin W, Lin L, Hu X, Wu G, et al: Podocyte OTUD5 alleviates
diabetic kidney disease through deubiquitinating TAK1 and reducing
podocyte inflammation and injury. Nat Commun. 15:54412024.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Szrejder M, Typiak M, Pikul P, Audzeyenka
I, Rachubik P, Rogacka D, Narajczyk M and Piwkowska A: Role of
L-lactate as an energy substrate in primary rat podocytes under
physiological and glucose deprivation conditions. Eur J Cell Biol.
102:1512982023. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Audzeyenka I, Szrejder M, Rachubik P,
Grochowalska K, Kulesza T, Rogacka D, Narajczyk M and Piwkowska A:
Lactate regulates respiratory efficiency and mitochondrial dynamics
in primary rat podocytes. Free Radic Biol Med. 220:312–323. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Dalga D, Verissimo T and de Seigneux S:
Gluconeogenesis in the kidney: In health and in chronic kidney
disease. Clin Kidney J. 16:1249–1257. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Nakamura M, Satoh N, Horita S and Nangaku
M: Insulin-induced mTOR signaling and gluconeogenesis in renal
proximal tubules: A mini-review of current evidence and therapeutic
potential. Front Pharmacol. 13:10152042022. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Hatano R, Lee E, Sato H, Kiuchi M,
Hirahara K, Nakagawa Y, Shimano H, Nakayama T, Tanaka T and Miki T:
Hepatic ketone body regulation of renal gluconeogenesis. Mol Metab.
84:1019342024. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Zanza C, Facelli V, Romenskaya T,
Bottinelli M, Caputo G, Piccioni A, Franceschi F, Saviano A, Ojetti
V, Savioli G and Longhitano Y: Lactic acidosis related to
pharmacotherapy and human diseases. Pharmaceuticals (Basel).
15:14962022. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Zhang D, Tang Z, Huang H, Zhou G, Cui C,
Weng Y, Liu W, Kim S, Lee S, Perez-Neut M, et al: Metabolic
regulation of gene expression by histone lactylation. Nature.
574:575–580. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Zhou Y, Yan J, Huang H, Liu L, Ren L, Hu
J, Jiang X, Zheng Y, Xu L, Zhong F and Li X: The m6A reader IGF2BP2
regulates glycolytic metabolism and mediates histone lactylation to
enhance hepatic stellate cell activation and liver fibrosis. Cell
Death Dis. 15:1892024. View Article : Google Scholar :
|
|
47
|
Wan N, Wang N, Yu S, Zhang H, Tang S, Wang
D, Lu W, Li H, Delafield DG, Kong Y, et al: Cyclic immonium ion of
lactyllysine reveals widespread lactylation in the human proteome.
Nat Methods. 19:854–864. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
An S, Yao Y, Hu H, Wu J, Li J, Li L, Wu J,
Sun M, Deng Z, Zhang Y, et al: PDHA1 hyperacetylation-mediated
lactate overproduction promotes sepsis-induced acute kidney injury
via Fis1 lactylation. Cell Death Dis. 14:4572023. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Chen J, Feng Q, Qiao Y, Pan S, Liang L,
Liu Y, Zhang X, Liu D and Liu Z and Liu Z: ACSF2 and lysine
lactylation contribute to renal tubule injury in diabetes.
Diabetologia. 67:1429–1443. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Wang P, Xie D, Xiao T, Cheng C, Wang D,
Sun J, Wu M, Yang Y, Zhang A and Liu Q: H3K18 lactylation promotes
the progression of arsenite-related idiopathic pulmonary fibrosis
via YTHDF1/m6A/NREP. J Hazard Mater. 461:1325822024. View Article : Google Scholar
|
|
51
|
Zhang Y, Huang Z, Han W, Wu J, Li S, Qin
T, Zhang C, Shi M, Han S, Gao B, et al: Glutamine suppresses
senescence and promotes autophagy through glycolysis
inhibition-mediated AMPKα lactylation in intervertebral disc
degeneration. Commun Biol. 7:3252024. View Article : Google Scholar
|
|
52
|
Sun W, Jia M, Feng Y and Cheng X: Lactate
is a bridge linking glycolysis and autophagy through lactylation.
Autophagy. 19:3240–3241. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Wei Y, Guo H, Chen S and Tang XX:
Regulation of macrophage activation by lactylation in lung disease.
Front Immunol. 15:14277392024. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Moreno-Yruela C, Zhang D, Wei W, Bæk M,
Liu W, Gao J, Danková D, Nielsen AL, Bolding JE, Yang L, et al:
Class I histone deacetylases (HDAC1-3) are histone lysine
delactylases. Sci Adv. 8:eabi66962022. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Kikuchi M, Morita S, Wakamori M, Sato S,
Uchikubo-Kamo T, Suzuki T, Dohmae N, Shirouzu M and Umehara T:
Epigenetic mechanisms to propagate histone acetylation by p300/CBP.
Nat Commun. 14:41032023. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Dong M, Zhang Y, Chen M, Tan Y, Min J, He
X, Liu F, Gu J, Jiang H, Zheng L, et al: ASF1A-dependent
P300-mediated histone H3 lysine 18 lactylation promotes
atherosclerosis by regulating EndMT. Acta Pharm Sin B.
14:3027–3048. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Wu X and Tao WA: Uncovering ubiquitous
protein lactylation. Nat Methods. 19:793–794. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Li J, Shi X, Xu J, Wang K, Hou F, Luan X
and Chen L: Aldehyde dehydrogenase 2 lactylation aggravates
mitochondrial dysfunction by disrupting PHB2 mediated mitophagy in
acute kidney injury. Adv Sci (Weinh). 12:e24119432024. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Zhou J, Zhang J, Xu F, Gao H, Wang L, Zhao
Y and Li K: AST-120 alleviates renal ischemia-reperfusion injury by
inhibiting HK2-mediated glycolysis. Mol Med. 30:1332024. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Qiao J, Tan Y, Liu H, Yang B, Zhang Q, Liu
Q, Sun W, Li Z, Wang Q, Feng W, et al: Histone H3K18 and ezrin
lactylation promote renal dysfunction in Sepsis-associated acute
kidney injury. Adv Sci (Weinh). 11:e23072162024. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Kumar B, Navarro C, Yung PYK, Lyu J,
Salazar Mantero A, Katsori AM, Schwämmle H, Martin M and Elsässer
SJ: Multiplexed chromatin immunoprecipitation sequencing for
quantitative study of histone modifications and chromatin factors.
Nat Protoc. 20:779–809. 2025. View Article : Google Scholar
|
|
62
|
Zhang L, Xue G, Liu J, Li Q and Wang Y:
Revealing transcription factor and histone modification
co-localization and dynamics across cell lines by integrating
ChIP-seq and RNA-seq data. BMC Genomics. 19:9142018. View Article : Google Scholar
|
|
63
|
Miguel V, Shaw IW and Kramann R:
Metabolism at the crossroads of inflammation and fibrosis in
chronic kidney disease. Nat Rev Nephrol. 21:39–56. 2025. View Article : Google Scholar
|
|
64
|
Li Y, Min X, Zhang X, Cao X, Kong Q, Mao
Q, Cheng H, Gou L, Li Y, Li C, et al: HSPA12A promotes c-Myc
lactylation-mediated proliferation of tubular epithelial cells to
facilitate renal functional recovery from kidney
ischemia/reperfusion injury. Cell Mol Life Sci. 81:4042024.
View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Xiang T, Wang X, Huang S, Zhou K, Fei S,
Zhou B, Yue K, Li Q, Xue S, Dai Y, et al: Inhibition of PKM2 by
shikonin impedes TGF-β1 expression by repressing histone
lactylation to alleviate renal fibrosis. Phytomedicine.
136:1563242025. View Article : Google Scholar
|
|
66
|
Zheng T, Gu YP, Wang JM, Huang TT, Gou LS
and Liu YW: Lactate-triggered histone lactylation contributes to
podocyte epithelial-mesenchymal transition in diabetic nephropathy
in mice. Chem Biol Interact. 408:1114182025. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Jia L, Sheng X, Zamperetti A, Xie Y,
Corradi V, Chandel S, De Cal M, Montin DP, Caprara C and Ronco C:
Combination of biomarker with clinical risk factors for prediction
of severe acute kidney injury in critically ill patients. BMC
Nephrol. 21:5402020. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Legouis D, Ricksten S-E, Faivre A,
Verissimo T, Gariani K, Verney C, Galichon P, Berchtold L, Feraille
E, Fernandez M, et al: Altered proximal tubular cell glucose
metabolism during acute kidney injury is associated with mortality.
Nat Metab. 2:732–743. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Sklienka P, Maca J, Neiser J, Bursa F,
Sevcik P, Frelich M, Petejova N, Svagera Z, Tomaskova H and Zahorec
R: Physiologic risk factors for early acute kidney injury in
severely injured patients. Bratisl Lek Listy. 121:779–785.
2020.PubMed/NCBI
|
|
70
|
Nasu T, Ueda K, Kawashima S, Okishio Y,
Kunitatsu K, Iwasaki Y and Kato S: Prediction of early acute kidney
injury after trauma using prehospital systolic blood pressure and
lactate levels: A prospective validation study. Injury. 53:81–85.
2022. View Article : Google Scholar
|
|
71
|
Gong C, Jiang Y, Tang Y, Liu F, Shi Y,
Zhou H and Xie K: Elevated serum lactic acid level is an
independent risk factor for the incidence and mortality of
sepsis-associated acute kidney injury. Zhonghua Wei Zhong Bing Ji
Jiu Yi Xue. 34:714–720. 2022.In Chinese. PubMed/NCBI
|
|
72
|
Flores-Salinas HE, Zambada-Gamboa AJ,
Garcia-Garduño TC, Rodríguez-Zavala G, Valle Y, Chávez-Herrera JC,
Martinez-Gutierrez PE, Godinez-Flores A, Jiménez-Limón S and
Padilla-Gutiérrez JR: Association of postoperative serum lactate
levels with acute kidney injury in mexican patients undergoing
cardiac surgery. Clin Pract. 14:1100–1109. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Wang Z, Xu J, Kang Y, Liu L, Zhang L and
Wang D: Early dynamic behavior of lactate in predicting continuous
renal replacement therapy after surgery for acute type A aortic
dissection. Front Cardiovasc Med. 9:9486722022. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Kahyaoglu M, Karaduman A, Geçmen Ç, Candan
Ö, Güner A, Cakmak EO, Bayam E, Yılmaz Y, Çelik M, Izgi IA and
Kirma C: Serum lactate level may predict the development of acute
kidney injury in acute decompensated heart failure. Turk Kardiyol
Dern Ars. 48:683–689. 2020.PubMed/NCBI
|
|
75
|
Zhou X, He Y, Hu L, Zhu Q, Lin Q, Hong X,
Huang W, Shan P and Liang D: Lactate level and lactate clearance
for acute kidney injury prediction among patients admitted with
ST-segment elevation myocardial infarction: A retrospective cohort
study. Front Cardiovasc Med. 9:9302022022. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Wang R, Wang S, Zhang J, He M and Xu J:
Serum lactate level in early stage is associated with acute kidney
injury in traumatic brain injury patients. Front Surg.
8:7611662021. View Article : Google Scholar
|
|
77
|
Xu J, Ma X, Yu K, Wang R, Wang S, Liu R,
Liu H, Gao H, Yu K and Wang C: Lactate up-regulates the expression
of PD-L1 in kidney and causes immunosuppression in septic Acute
Renal Injury. J Microbiol Immunol Infect. 54:404–410. 2021.
View Article : Google Scholar
|
|
78
|
Tan C, Gu J, Li T, Chen H, Liu K, Liu M,
Zhang H and Xiao X: Inhibition of aerobic glycolysis alleviates
sepsis-induced acute kidney injury by promoting lactate/Sirtuin
3/AMPK-regulated autophagy. Int J Mol Med. 47:192021. View Article : Google Scholar :
|
|
79
|
Shen Y, Jiang L, Wen P, Ye Y, Zhang Y,
Ding H, Luo J, Xu L, Zen K, Zhou Y and Yang J: Tubule-derived
lactate is required for fibroblast activation in acute kidney
injury. Am J Physiol Renal Physiol. 318:F689–F701. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Chu X, Di C, Chang P, Li L, Feng Z, Xiao
S, Yan X, Xu X, Li H, Qi R, et al: Lactylated histone H3K18 as a
potential biomarker for the diagnosis and predicting the severity
of septic shock. Front Immunol. 12:7866662021. View Article : Google Scholar
|
|
81
|
Guo W, Song Y, Sun Y, Du H, Cai Y, You Q,
Fu H and Shao L: Systemic immune-inflammation index is associated
with diabetic kidney disease in type 2 diabetes mellitus patients:
Evidence from NHANES 2011-2018. Front Endocrinol (Lausanne).
13:10714652022. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Roointan A, Gheisari Y, Hudkins KL and
Gholaminejad A: Non-invasive metabolic biomarkers for early
diagnosis of diabetic nephropathy: Meta-analysis of profiling
metabolomics studies. Nutr Metab Cardiovasc Dis. 31:2253–2272.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Jiang C, Ma X, Chen J, Zeng Y, Guo M, Tan
X, Wang Y, Wang P, Yan P, Lei Y, et al: Development of serum
lactate Level-based nomograms for predicting diabetic kidney
disease in type 2 diabetes mellitus patients. Diabetes Metab Syndr
Obes. 17:1051–1068. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Tang L, Yang Q, Ma R, Zhou P, Peng C, Xie
C, Liang Q, Wu T, Gao W, Yu H, et al: Association between lactate
dehydrogenase and the risk of diabetic kidney disease in patients
with type 2 diabetes. Front Endocrinol (Lausanne). 15:13699682024.
View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Muiru AN, Hsu JY, Zhang X, Appel LJ, Chen
J, Cohen DL, Drawz PE, Freedman BI, Go AS, He J, et al: Risk for
chronic kidney disease progression after acute kidney injury:
Findings from the chronic renal insufficiency cohort study. Ann
Intern Med. 176:961–968. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Chesnaye NC, Ortiz A, Zoccali C, Stel VS
and Jager KJ: The impact of population ageing on the burden of
chronic kidney disease. Nat Rev Nephrol. 20:569–585. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Tanemoto M: Gap acidosis except lactic
acidosis develops and progresses during chronic kidney disease
stage G5. Clin Exp Nephrol. 23:1045–1049. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Zhao B, Xu Y, Chen Y, Cai Y, Gong Z, Li D,
Kuang H, Liu X, Zhou H, Liu G and Yin Y: Activation of TRPV4 by
lactate as a critical mediator of renal fibrosis in spontaneously
hypertensive rats after moderate- and high-intensity exercise.
Front Physiol. 13:9270782022. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Nagy A, Pethő D, Gáll T, Zavaczki E,
Nyitrai M, Posta J, Zarjou A, Agarwal A, Balla G and Balla J: Zinc
Inhibits HIF-Prolyl Hydroxylase Inhibitor-Aggravated VSMC
calcification induced by high phosphate. Front Physiol.
10:15842020. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Huang Z, Liao Y, Zheng Y, Ye S, Zhang Q,
Yu X, Liu X and Li N: Zinc deficiency causes glomerulosclerosis and
renal interstitial fibrosis through oxidative stress and increased
lactate metabolism in rats. Biol Trace Elem Res. 203:2084–2098.
2025. View Article : Google Scholar :
|
|
91
|
Li M, Jia F, Zhou H, Di J and Yang M:
Elevated aerobic glycolysis in renal tubular epithelial cells
influences the proliferation and differentiation of podocytes and
promotes renal interstitial fibrosis. Eur Rev Med Pharmacol Sci.
22:5082–5090. 2018.PubMed/NCBI
|
|
92
|
Jiang A, Liu J, Wang Y and Zhang C:
cGAS-STING signaling pathway promotes hypoxia-induced renal
fibrosis by regulating PFKFB3-mediated glycolysis. Free Radic Biol
Mede. 208:516–529. 2023. View Article : Google Scholar
|
|
93
|
Ding H, Jiang L, Xu J, Bai F, Zhou Y, Yuan
Q, Luo J, Zen K and Yang J: Inhibiting aerobic glycolysis
suppresses renal interstitial fibroblast activation and renal
fibrosis. Am J Physiol Renal Physiol. 313:F561–F575. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Li X, Ma TK, Wang M, Zhang XD, Liu TY, Liu
Y, Huang ZH, Zhu YH, Zhang S, Yin L, et al: YY1-induced
upregulation of LncRNA-ARAP1-AS2 and ARAP1 promotes diabetic kidney
fibrosis via aberrant glycolysis associated with EGFR/PKM2/HIF-1α
pathway. Front Pharmacol. 14:10693482023. View Article : Google Scholar
|
|
95
|
Wei Q, Su J, Dong G, Zhang M, Huo Y and
Dong Z: Glycolysis inhibitors suppress renal interstitial fibrosis
via divergent effects on fibroblasts and tubular cells. Am J
Physiol Renal Physiol. 316:F1162–F1172. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Md Shakhih MF, Rosslan AS, Noor AM,
Ramanathan S, Lazim AM and Wahab AA: Review-enzymatic and
Non-enzymatic electrochemical sensor for lactate detection in human
biofluids. J Electrochem Soc. 168:0675022021. View Article : Google Scholar
|
|
97
|
Henry H, Marmy Conus N, Steenhout P,
Béguin A and Boulat O: Sensitive determination of D-lactic acid and
L-lactic acid in urine by high-performance liquid
chromatography-tandem mass spectrometry. Biomed Chromatogr.
26:425–428. 2012. View Article : Google Scholar
|
|
98
|
Bollella P, Sharma S, Cass AEG and
Antiochia R: Microneedle-based biosensor for minimally-invasive
lactate detection. Biosens Bioelectron. 123:152–159. 2019.
View Article : Google Scholar
|
|
99
|
Xie Y, Li K, Liu J, Zhou Y, Zhang C, Yu Y,
Wang J, Su L and Zhang X: A smart lab on a wearable microneedle
patch with convolutional neural network-enhanced colorimetry for
early warning of syndrome of inappropriate antidiuretic hormone
secretion. Aggregate. 6:e6712025. View Article : Google Scholar
|
|
100
|
Yao S, Chai H, Tao T, Zhang L, Yang X, Li
X, Yi Z, Wang Y, An J, Wen G, et al: Role of lactate and lactate
metabolism in liver diseases (Review). Int J Mol Med. 54:592024.
View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Sun J, Dai W, Guo Q, Gao Y, Chen J, Chen
JL, Mao G, Sun H and Peng YK: Self-powered wearable electrochemical
sensor based on composite conductive hydrogel medium for detection
of lactate in human sweat. Biosens Bioelectron. 277:1173032025.
View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Chen Z, Zhu Z, Liang W, Luo Z, Hu J, Feng
J, Zhang Z, Luo Q, Yang H and Ding G: Reduction of anaerobic
glycolysis contributes to angiotensin II-induced podocyte injury
with foot process effacement. Kidney Int. 103:735–748. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Jiajun W, Kaifeng G and Jing Z: Urinary
PKM2, a marker predicating acute kidney injury in patients with
sepsis. Int Urol Nephrol. 56:3039–3045. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Bertelsen LB, Hansen ESS, Sadowski T, Ruf
S and Laustsen C: Hyperpolarized pyruvate to measure the influence
of PKM2 activation on glucose metabolism in the healthy kidney. NMR
Biomed. 34:e45832021. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Liu H, Takagaki Y, Kumagai A, Kanasaki K
and Koya D: The PKM2 activator TEPP-46 suppresses kidney fibrosis
via inhibition of the EMT program and aberrant glycolysis
associated with suppression of HIF-1α accumulation. J Diabetes
Investig. 12:697–709. 2021. View Article : Google Scholar
|
|
106
|
Chen Y, Bai X, Chen J, Huang M, Hong Q,
Ouyang Q, Sun X, Zhang Y, Liu J, Wang X, et al: Pyruvate kinase M2
regulates kidney fibrosis through pericyte glycolysis during the
progression from acute kidney injury to chronic kidney disease.
Cell Prolif. 57:e135482024. View Article : Google Scholar :
|
|
107
|
Wang J, Ren Y, Zheng X, Kang J, Huang Z,
Xu L and Wang Y: Anti-fibrotic effects of low toxic Microcystin-RR
on Bleomycin-induced pulmonary fibrosis: A comparison with
Microcystin-LR. Front Pharmacol. 12:6759072021. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Ren Y, Wang J, Guo W, Chen J, Wu X, Gu S,
Xu L, Wu Z and Wang Y: Renoprotection of Microcystin-RR in
unilateral ureteral Obstruction-induced renal fibrosis: Targeting
the PKM2-HIF-1α pathway. Front Pharmacol. 13:8303122022. View Article : Google Scholar
|
|
109
|
Gong M, Guo Y, Dong H, Wu F, He Q, Gong J
and Lu F: Modified Hu-lu-ba-wan protects diabetic glomerular
podocytes via promoting PKM2-mediated mitochondrial dynamic
homeostasis. Phytomedicine. 123:1552472024. View Article : Google Scholar
|
|
110
|
Qian L, Ren S, Xu Z, Zheng Y, Wu L, Yang
Y, Wang Y, Li J, Yan S and Fang Z: Qian yang yu yin granule
improves renal injury of hypertension by regulating metabolic
reprogramming mediated by HIF-1α/PKM2 positive feedback loop. Front
Pharmacol. 12:6674332021. View Article : Google Scholar
|
|
111
|
Wang M, Zeng F, Ning F, Wang Y, Zhou S, He
J, Li C, Wang C, Sun X, Zhang D, et al: Ceria nanoparticles
ameliorate renal fibrosis by modulating the balance between
oxidative phosphorylation and aerobic glycolysis. J
Nanobiotechnology. 20:32022. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Fu X, Zhang J, Huang X, Mo Z, Sang Z, Duan
W and Huang W: Curcumin antagonizes glucose fluctuation-induced
renal injury by inhibiting aerobic glycolysis via the miR-489/LDHA
pathway. Mediators Inflamm. 2021:61045292021. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Yu H, Zhu J, Chang L, Liang C, Li X and
Wang W: 3-Bromopyruvate decreased kidney fibrosis and fibroblast
activation by suppressing aerobic glycolysis in unilateral ureteral
obstruction mice model. Life Sci. 272:1192062021. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Han W, Wang C, Yang Z, Mu L, Wu M, Chen N,
Du C, Duan H and Shi Y: SRT1720 retards renal fibrosis via
inhibition of HIF1A/GLUT1 in diabetic nephropathy. J Endocrinol.
241:85–98. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Venkatesan A, Roy A, Kulandaivel S,
Natesan V and Kim SJ: p-Coumaric acid nanoparticles ameliorate
diabetic nephropathy via regulating mRNA expression of KIM-1 and
GLUT-2 in Streptozotocin-induced diabetic rats. Metabolites.
12:11662022. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Chen X, Wang H, Jiang M, Zhao J, Fan C,
Wang Y and Peng W: Huangqi (astragalus) decoction ameliorates
diabetic nephropathy via IRS1-PI3K-GLUT signaling pathway. Am J
Transl Res. 10:2491–2501. 2018.PubMed/NCBI
|
|
117
|
Ritu, Xiong Y, Sharma HP, Goyal RK, Narwal
S, Berwal A, Jain S, Priya M, Singh M, Agarwal G, et al:
Bioflavonoid combination attenuates diabetes-induced nephropathy in
rats via modulation of MMP-9/TIMP-1, TGF-β, and GLUT-4-associated
pathways. Heliyon. 10:e332172024. View Article : Google Scholar
|
|
118
|
Zhang J, Ding T, Zhang X, Tang D and Wang
J: Dapagliflozin relieves renal injury in a diabetic nephropathy
model by inducing autophagy through regulation of
miR-30e-5p/AKT/mTOR pathway. Trop J Pharm Res. 21:2115–2123. 2022.
View Article : Google Scholar
|
|
119
|
Fatouros IG, Douroudos I, Panagoutsos S,
Pasadakis P, Nikolaidis MG, Chatzinikolaou A, Sovatzidis A,
Michailidis Y, Jamurtas AZ, Mandalidis D, et al: Effects of
L-carnitine on oxidative stress responses in patients with renal
disease. Med Sci Sports Exerc. 42:1809–1818. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Sharma B and Yadav DK: L-Carnitine and
chronic kidney disease: A comprehensive review on nutrition and
health perspectives. J Pers Med. 13:2982023. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Wen YK: Impact of acute kidney injury on
metformin-associated lactic acidosis. Int Urol Nephrol. 41:967–972.
2009. View Article : Google Scholar : PubMed/NCBI
|