|
1
|
Saran R, Robinson B, Abbott KC,
Bragg-Gresham J, Chen X, Gipson D, Gu H, Hirth RA, Hutton D, Jin Y,
et al: US renal data system 2019 annual data report: Epidemiology
of kidney disease in the United States. Am J Kidney Dis. 75(Suppl):
A6–A7. 2020. View Article : Google Scholar
|
|
2
|
McCullough KP, Morgenstern H, Saran R,
Herman WH and Robinson BM: Projecting ESRD incidence and prevalence
in the United States through 2030. J Am Soc Nephrol. 30:127–135.
2019. View Article : Google Scholar :
|
|
3
|
Pozzoni P, Del Vecchio L, Pontoriero G, Di
Filippo S and Locatelli F: Long-term outcome in hemodialysis:
Morbidity and mortality. J Nephrol. 17:S87–S95. 2004.PubMed/NCBI
|
|
4
|
Deb S, Wijeysundera HC, Ko DT, Tsubota H,
Hill S and Fremes SE: Coronary artery bypass graft surgery vs
percutaneous interventions in coronary revascularization: A
systematic review. JAMA. 310:2086–2095. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hori D, Yamaguchi A and Adachi H: Coronary
artery bypass surgery in end-stage renal disease patients. Ann Vasc
Dis. 10:79–87. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Pang PYK, Teow CKJ, Huang MJ, Naik MJ, Lim
SL, Chao VTT, Tan TE, Chua YL and Sin YK: Long-term prognosis in
patients with end-stage renal disease after coronary artery bypass
grafting. J Thorac Dis. 12:6722–6730. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Serafinceanu C, Neculaescu C, Cimponeriu
D, Timar R and Covic AC: Impact of gender and dialysis modality on
early mortality risk in diabetic ESRD patients: Data from a large
single center cohort. Int Urol Nephrol. 46:607–614. 2014.
View Article : Google Scholar
|
|
8
|
Tsur N, Menashe I and Haviv YS: Risk
factors before dialysis predominate as mortality predictors in
diabetic maintenance dialysis patients. Sci Rep. 9:106332019.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Schena FP: Epidemiology of end-stage renal
disease: International comparisons of renal replacement therapy.
Kidney Int. 57:S39–S45. 2000. View Article : Google Scholar
|
|
10
|
Vaios V, Georgianos PI, Liakopoulos V and
Agarwal R: Assessment and management of hypertension among patients
on peritoneal dialysis. Clin J Am Soc Nephrol. 14:297–305. 2019.
View Article : Google Scholar :
|
|
11
|
McKane W, Chandna SM, Tattersall JE,
Greenwood RN and Farrington K: Identical decline of residual renal
function in high-flux biocompatible hemodialysis and CAPD. Kidney
Int. 61:256–265. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Coentrão L, Van Biesen W, Nistor I,
Tordoir J, Gallieni M, Marti Monros A and Bolignano D: Preferred
haemodialysis vascular access for diabetic chronic kidney disease
patients: A systematic literature review. J Vasc Access.
16:259–264. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Almasri J, Alsawas M, Mainou M, Mustafa
RA, Wang Z, Woo K, Cull DL and Murad MH: Outcomes of vascular
access for hemodialysis: A systematic review and meta-analysis. J
Vasc Surg. 64:236–243. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Arhuidese IJ, Orandi BJ, Nejim B and Malas
M: Utilization, patency, and complications associated with vascular
access for hemodialysis in the United States. J Vasc Surg.
68:1166–1174. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Arhuidese IJ, Purohit A, Elemuo C,
Parkerson GR, Shames ML and Malas MB: Outcomes of autogenous
fistulas and prosthetic grafts for hemodialysis access in diabetic
and nondiabetic patients. J Vasc Surg. 72:2088–2096. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
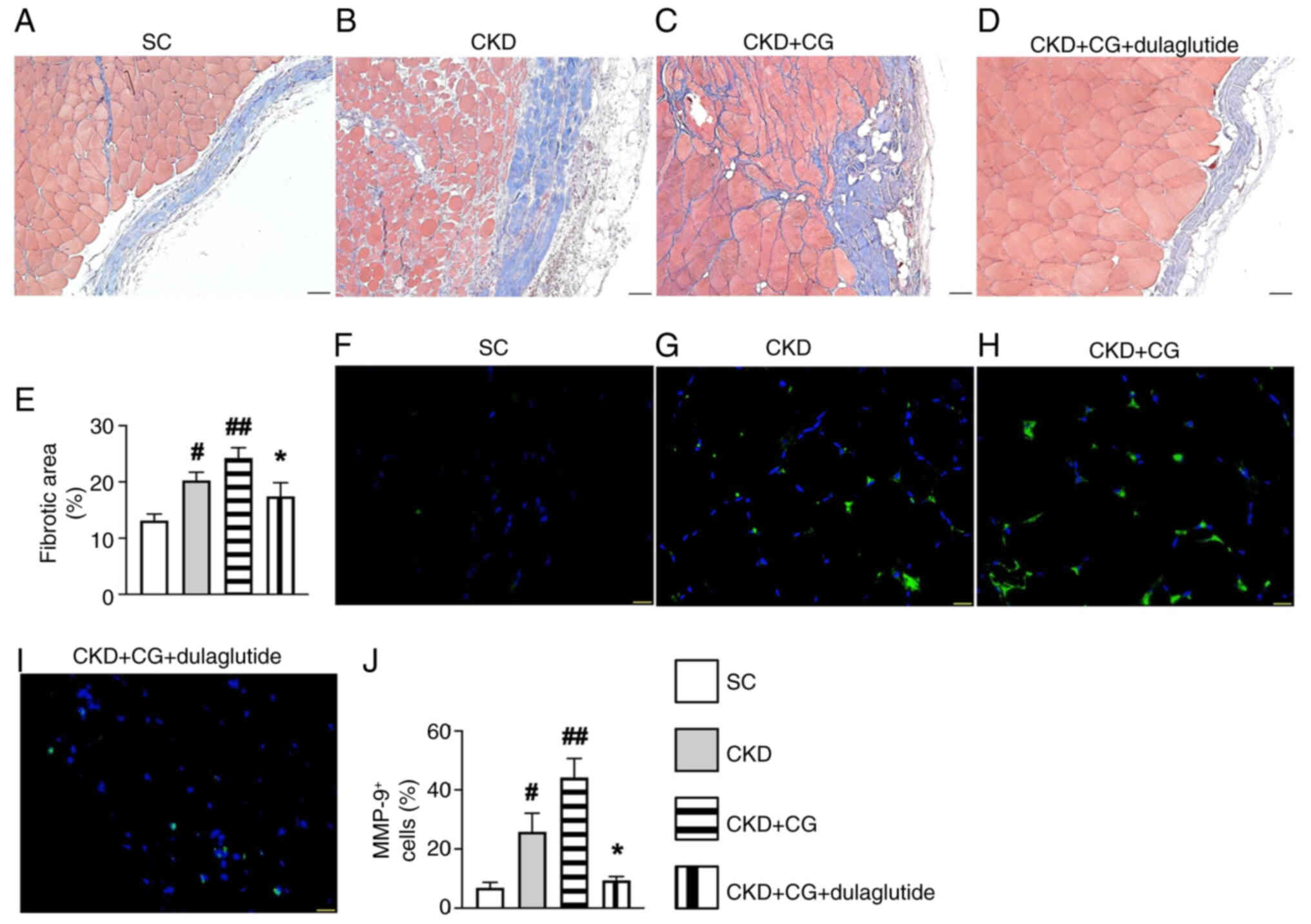
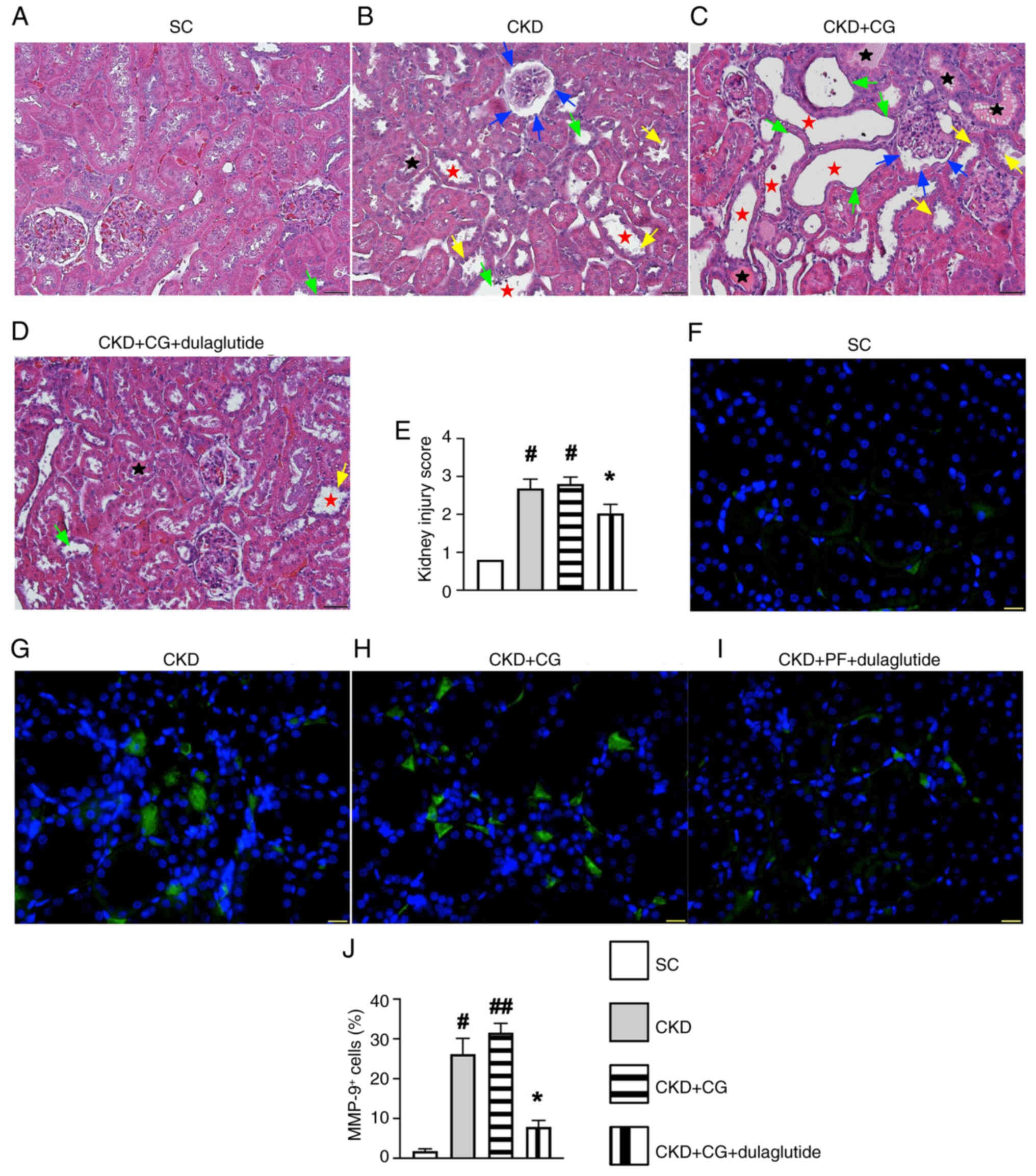
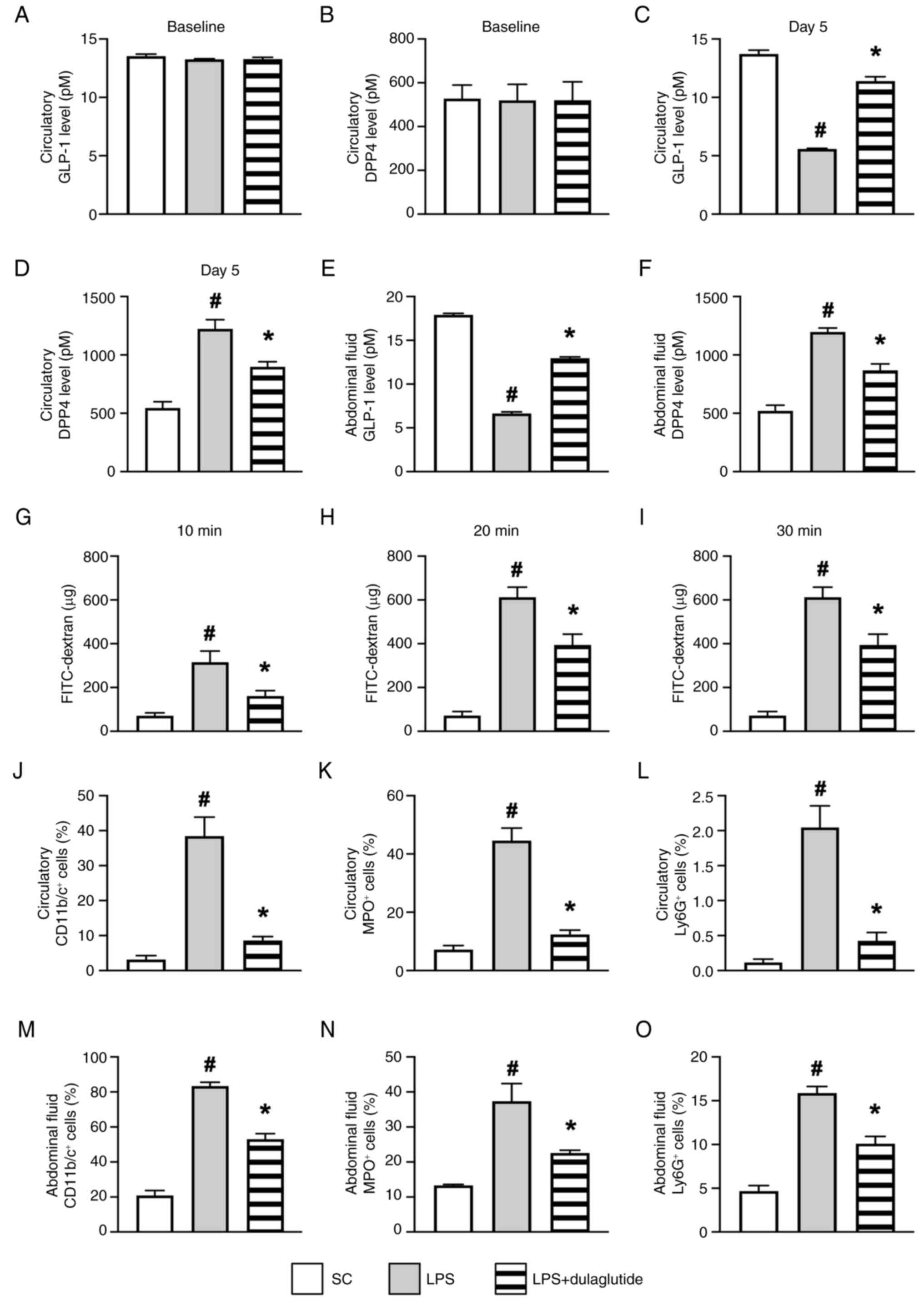
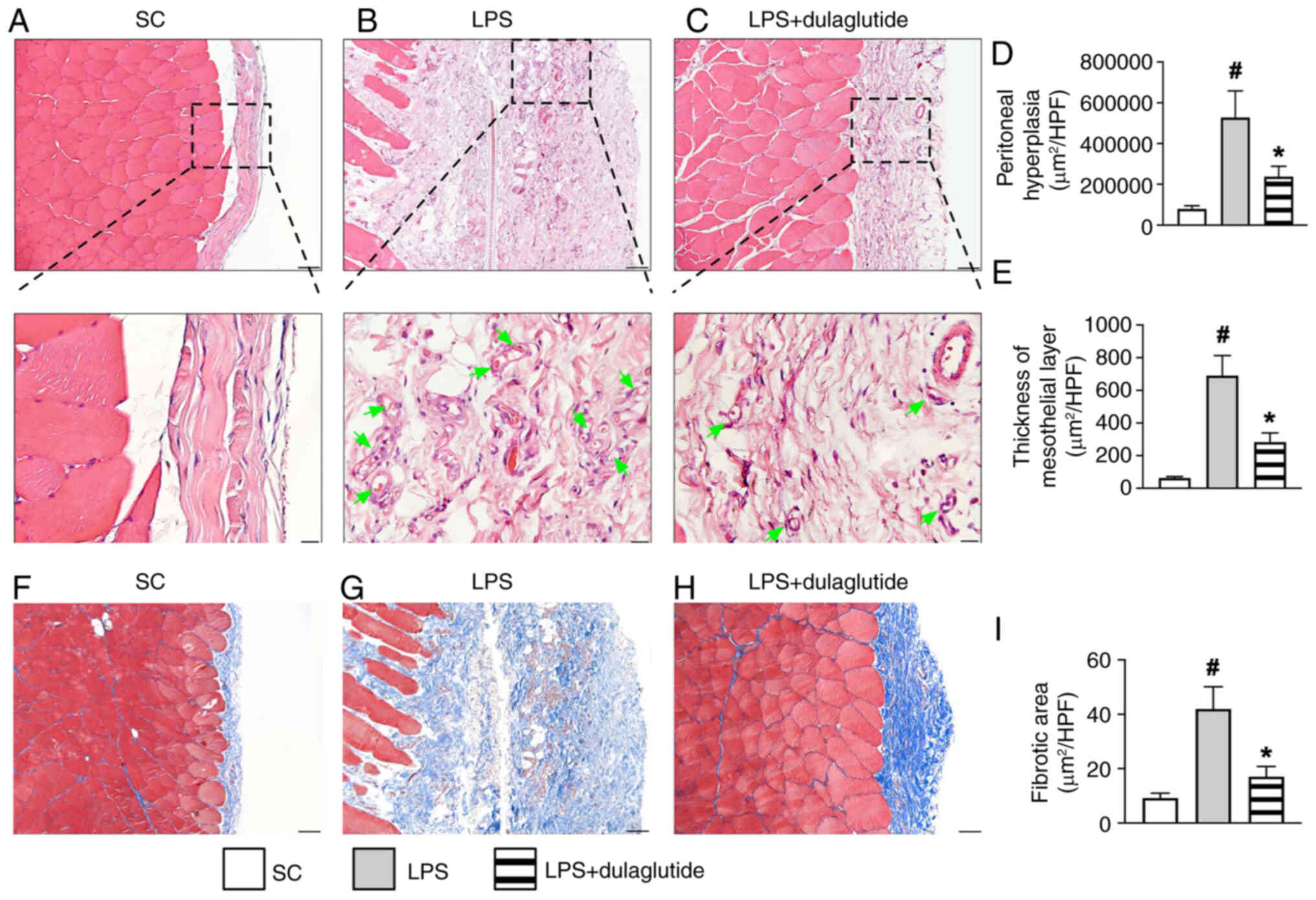
Li YC, Sung PH, Yang YH, Chiang JY, Yip HK
and Yang CC: Dipeptidyl peptidase 4 promotes peritoneal fibrosis
and its inhibitions prevent failure of peritoneal dialysis. Commun
Biol. 4:1442021. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Williams JD, Craig KJ, Topley N, Von
Ruhland C, Fallon M, Newman GR, Mackenzie RK and Williams GT:
Morphologic changes in the peritoneal membrane of patients with
renal disease. J Am Soc Nephrol. 13:470–479. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Williams JD, Craig KJ, von Ruhland C,
Topley N and Williams GT; Biopsy Registry Study Group: The natural
course of peritoneal membrane biology during peritoneal dialysis.
Kidney Int. (Suppl): S43–S49. 2003. View Article : Google Scholar
|
|
19
|
Mutsaers SE, Birnie K, Lansley S, Herrick
SE, Lim CB and Prêle CM: Mesothelial cells in tissue repair and
fibrosis. Front Pharmacol. 6:1132015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Di Paolo N and Sacchi G: Atlas of
peritoneal histology. Perit Dial Int. 20:S5–S96. 2000.PubMed/NCBI
|
|
21
|
Yung S and Chan TM: Pathophysiological
changes to the peritoneal membrane during PD-related peritonitis:
The role of mesothelial cells. Mediators Inflamm. 2012:4841672012.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Terri M, Trionfetti F, Montaldo C, Cordani
M, Tripodi M, Lopez-Cabrera M and Strippoli R: Mechanisms of
peritoneal fibrosis: Focus on immune cells-peritoneal stroma
interactions. Front Immunol. 12:6072042021. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Stone RC, Pastar I, Ojeh N, Chen V, Liu S,
Garzon KI and Tomic-Canic M: Epithelial-mesenchymal transition in
tissue repair and fibrosis. Cell Tissue Res. 365:495–506. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Li M, Luan F, Zhao Y, Hao H, Zhou Y, Han W
and Fu X: Epithelial-mesenchymal transition: An emerging target in
tissue fibrosis. Exp Biol Med (Maywood). 241:1–13. 2016. View Article : Google Scholar
|
|
25
|
Milan Manani S, Virzi GM, Giuliani A,
Baretta M, Corradi V, De Cal M, Biasi C, Crepaldi C and Ronco C:
Lipopolysaccharide evaluation in peritoneal dialysis patients with
peritonitis. Blood Purif. 49:434–439. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Knapp S, de Vos AF, Florquin S, Golenbock
DT and van der Poll T: Lipopolysaccharide binding protein is an
essential component of the innate immune response to escherichia
coli peritonitis in mice. Infect Immun. 71:6747–6753. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Shen WR, Kimura K, Ishida M, Sugisawa H,
Kishikawa A, Shima K, Ogawa S, Qi J and Kitaura H: The
glucagon-like peptide-1 receptor agonist exendin-4 inhibits
lipopolysaccharide-induced osteoclast formation and bone resorption
via inhibition of TNF-α expression in macrophages. J Immunol Res.
2018:57836392018. View Article : Google Scholar
|
|
28
|
Mehdi SF, Pusapati S, Anwar MS, Lohana D,
Kumar P, Nandula SA, Nawaz FK, Tracey K, Yang H, LeRoith D, et al:
Glucagon-like peptide-1: A multi-faceted anti-inflammatory agent.
Front Immunol. 14:11482092023. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Zheng Z, Zong Y, Ma Y, Tian Y, Pang Y,
Zhang C and Gao J: Glucagon-like peptide-1 receptor: Mechanisms and
advances in therapy. Signal Transduct Target Ther. 9:2342024.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Chen YT, Tsai TH, Yang CC, Sun CK, Chang
LT, Chen HH, Chang CL, Sung PH, Zhen YY, Leu S, et al: Exendin-4
and sitagliptin protect kidney from ischemia-reperfusion injury
through suppressing oxidative stress and inflammatory reaction. J
Transl Med. 11:2702013. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Yip HK, Yang CC, Chen KH, Huang TH, Chen
YL, Zhen YY, Sung PH, Chiang HJ, Sheu JJ, Chang CL, et al: Combined
melatonin and exendin-4 therapy preserves renal ultrastructural
integrity after ischemia-reperfusion injury in the male rat. J
Pineal Res. 59:434–447. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Chang YC, Hsu SY, Yang CC, Sung PH, Chen
YL, Huang TH, Kao GS, Chen SY, Chen KH, Chiang HJ, et al: Enhanced
protection against renal ischemia-reperfusion injury with combined
melatonin and exendin-4 in a rodent model. Exp Biol Med (Maywood).
241:1588–1602. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Zhen YY, Yang CC, Hung CC, Lee CC, Lee CC,
Wu CH, Chen YT, Chen WY, Chen KH, Yip HK and Ko SF: Extendin-4
protects kidney from acute ischemia-reperfusion injury through
upregulation of NRF2 signaling. Am J Transl Res. 9:4756–4771.
2017.PubMed/NCBI
|
|
34
|
Sung PH, Chiang HJ, Wallace CG, Yang CC,
Chen YT, Chen KH, Chen CH, Shao PL, Chen YL, Chua S, et al:
Exendin-4-assisted adipose derived mesenchymal stem cell therapy
protects renal function against co-existing acute kidney
ischemia-reperfusion injury and severe sepsis syndrome in rat. Am J
Transl Res. 9:3167–3183. 2017.PubMed/NCBI
|
|
35
|
Yang CC, Chen YT, Wallace CG, Chen KH,
Cheng BC, Sung PH, Li YC, Ko SF, Chang HW and Yip HK: Early
administration of empagliflozin preserved heart function in
cardiorenal syndrome in rat. Biomed Pharmacother. 109:658–670.
2019. View Article : Google Scholar
|
|
36
|
Yin TC, Sung PH, Chen KH, Li YC, Luo CW,
Huang CR, Sheu JJ, Chiang JY, Lee MS and Yip HK: Extracorporeal
shock wave-assisted adipose-derived fresh stromal vascular fraction
restores the blood flow of critical limb ischemia in rat. Vascul
Pharmacol. 113:57–69. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
National Research Council (US) Committee
for the Update of the Guide for the Care and Use of Laboratory
Animals: Guide for the care and use of laboratory animals: Eighth
edition. The National Academies Press; Washington, DC: 2011
|
|
38
|
Huang TH, Chen YT, Sung PH, Chiang HJ,
Chen YL, Chai HT, Chung SY, Tsai TH, Yang CC, Chen CH, et al:
Peripheral blood-derived endothelial progenitor cell therapy
prevented deterioration of chronic kidney disease in rats. Am J
Transl Res. 7:804–824. 2015.PubMed/NCBI
|
|
39
|
Chang CL, Sung PH, Sun CK, Chen CH, Chiang
HJ, Huang TH, Chen YL, Zhen YY, Chai HT, Chung SY, et al:
Protective effect of melatonin-supported adipose-derived
mesenchymal stem cells against small bowel ischemia-reperfusion
injury in rat. J Pineal Res. 59:206–220. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Yue Y, Yeh JN, Chiang JY, Sung PH, Chen
YL, Liu F and Yip HK: Intrarenal arterial administration of human
umbilical cord-derived mesenchymal stem cells effectively preserved
the residual renal function of diabetic kidney disease in rat. Stem
Cell Res Ther. 13:1862022. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Lin KC, Yeh JN, Shao PL, Chiang JY, Sung
PH, Huang CR, Chen YL, Yip HK and Guo J: Jagged/Notch proteins
promote endothelial-mesenchymal transition-mediated pulmonary
arterial hypertension via upregulation of the expression of GATAs.
J Cell Mol Med. 27:1110–1130. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Sung PH, Cheng BC, Hsu TW, Chiang JY,
Chiang HJ, Chen YL, Yang CC and Yip HK: Oxidized-LDL deteriorated
the renal residual function and parenchyma in CKD rat through
upregulating epithelial mesenchymal transition and extracellular
matrix-mediated tubulointerstitial fibrosis-pharmacomodulation of
rosuvastatin. Antioxidants (Basel). 11:24652022. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Sung PH, Sun CK, Ko SF, Chang LT, Sheu JJ,
Lee FY, Wu CJ, Chua S and Yip HK: Impact of hyperglycemic control
on left ventricular myocardium. A molecular and cellular basic
study in a diabetic rat model. Int Heart J. 50:191–206. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Sheu JJ, Yang CC, Wallace CG, Chen KH,
Shao PL, Sung PH, Li YC, Chu YC, Guo J and Yip HK: Uremic toxic
substances are essential elements for enhancing carotid artery
stenosis after balloon-induced endothelial denudation: Worsening
role of the adventitial layer. Am J Transl Res. 12:7144–7159.
2020.PubMed/NCBI
|
|
45
|
Yip HK, Lee MS, Li YC, Shao PL, Chiang JY,
Sung PH, Yang CH and Chen KH: Dipeptidyl peptidase-4 deficiency
effectively protects the brain and neurological function in rodent
after acute hemorrhagic stroke. Int J Biol Sci. 16:3116–3132. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Ko SF, Chen KH, Wallace CG, Yang CC, Sung
PH, Shao PL, Li YC, Chen YT and Yip HK: Protective effect of
combined therapy with hyperbaric oxygen and autologous
adipose-derived mesenchymal stem cells on renal function in rodent
after acute ischemia-reperfusion injury. Am J Transl Res.
12:3272–3287. 2020.PubMed/NCBI
|
|
47
|
Vanholder R, Pletinck A, Schepers E and
Glorieux G: Biochemical and clinical impact of organic uremic
retention solutes: A comprehensive update. Toxins (Basel).
10:332018. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Chen YT, Wallace CG, Yang CC, Chen CH,
Chen KH, Sung PH, Chen YL, Chai HT, Chung SY, Chua S, et al: DPP-4
enzyme deficiency protects kidney from acute ischemia-reperfusion
injury: Role for remote intermittent bowel ischemia-reperfusion
preconditioning. Oncotarget. 8:54821–54837. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Chang MW, Chen CH, Chen YC, Wu YC, Zhen
YY, Leu S, Tsai TH, Ko SF, Sung PH, Yang CC, et al: Sitagliptin
protects rat kidneys from acute ischemia-reperfusion injury via
upregulation of GLP-1 and GLP-1 receptors. Acta Pharmacol Sin.
36:119–130. 2015. View Article : Google Scholar :
|