|
1
|
Myint ZW, Oo TH, Thein KZ, Tun AM and
Saeed H: Copper deficiency anemia: Review article. Ann Hematol.
97:1527–1534. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Mohammadifard N, Humphries KH, Gotay C,
Mena-Sánchez G, Salas-Salvadó J, Esmaillzadeh A, Ignaszewski A and
Sarrafzadegan N: Trace minerals intake: Risks and benefits for
cardiovascular health. Crit Rev Food Sci Nutr. 59:1334–1346. 2019.
View Article : Google Scholar
|
|
3
|
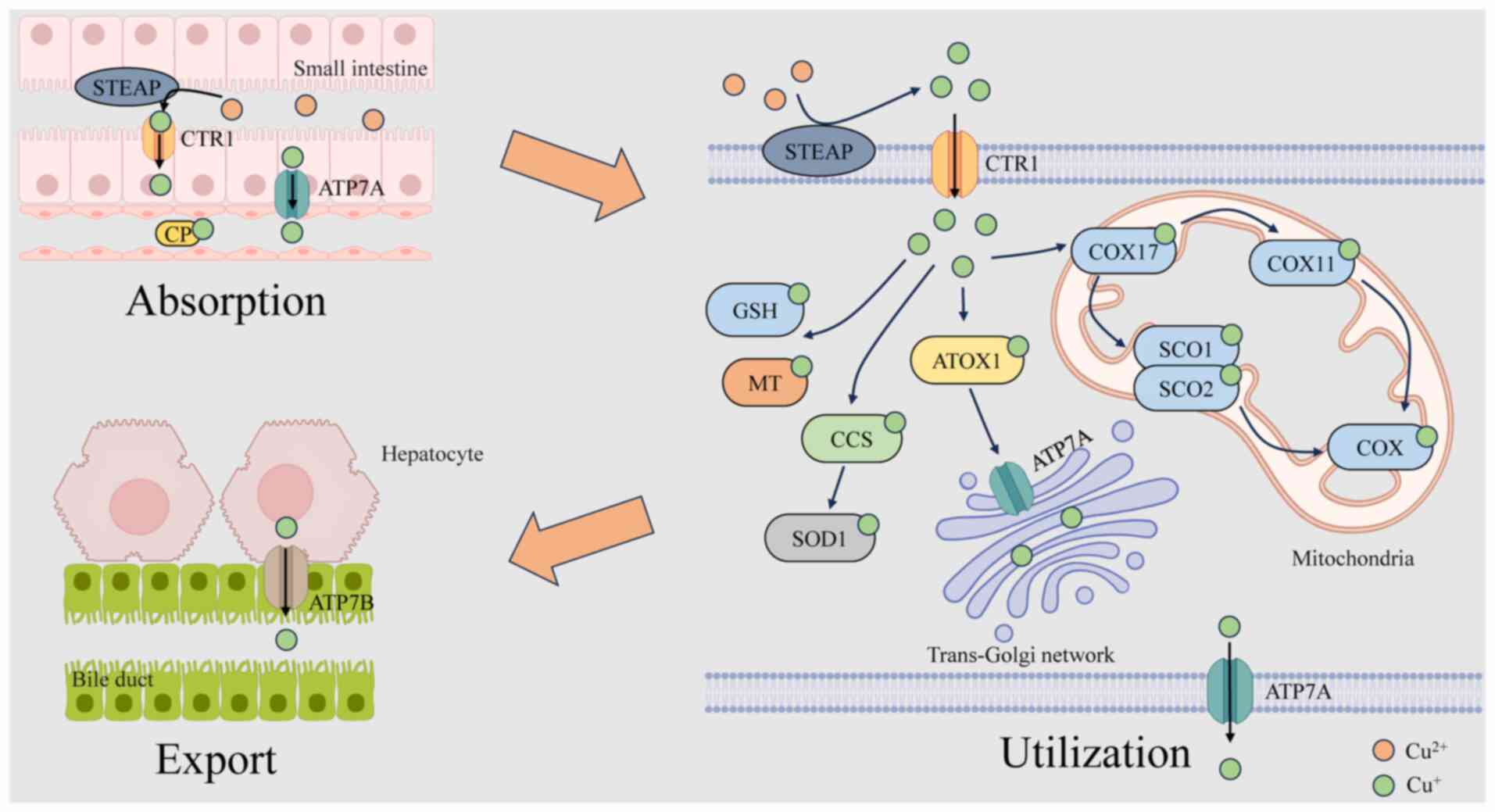
Chen X, Cai Q, Liang R, Zhang D, Liu X,
Zhang M, Xiong Y, Xu M, Liu Q, Li P, et al: Copper homeostasis and
copper-induced cell death in the pathogenesis of cardiovascular
disease and therapeutic strategies. Cell Death Dis. 14:1052023.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
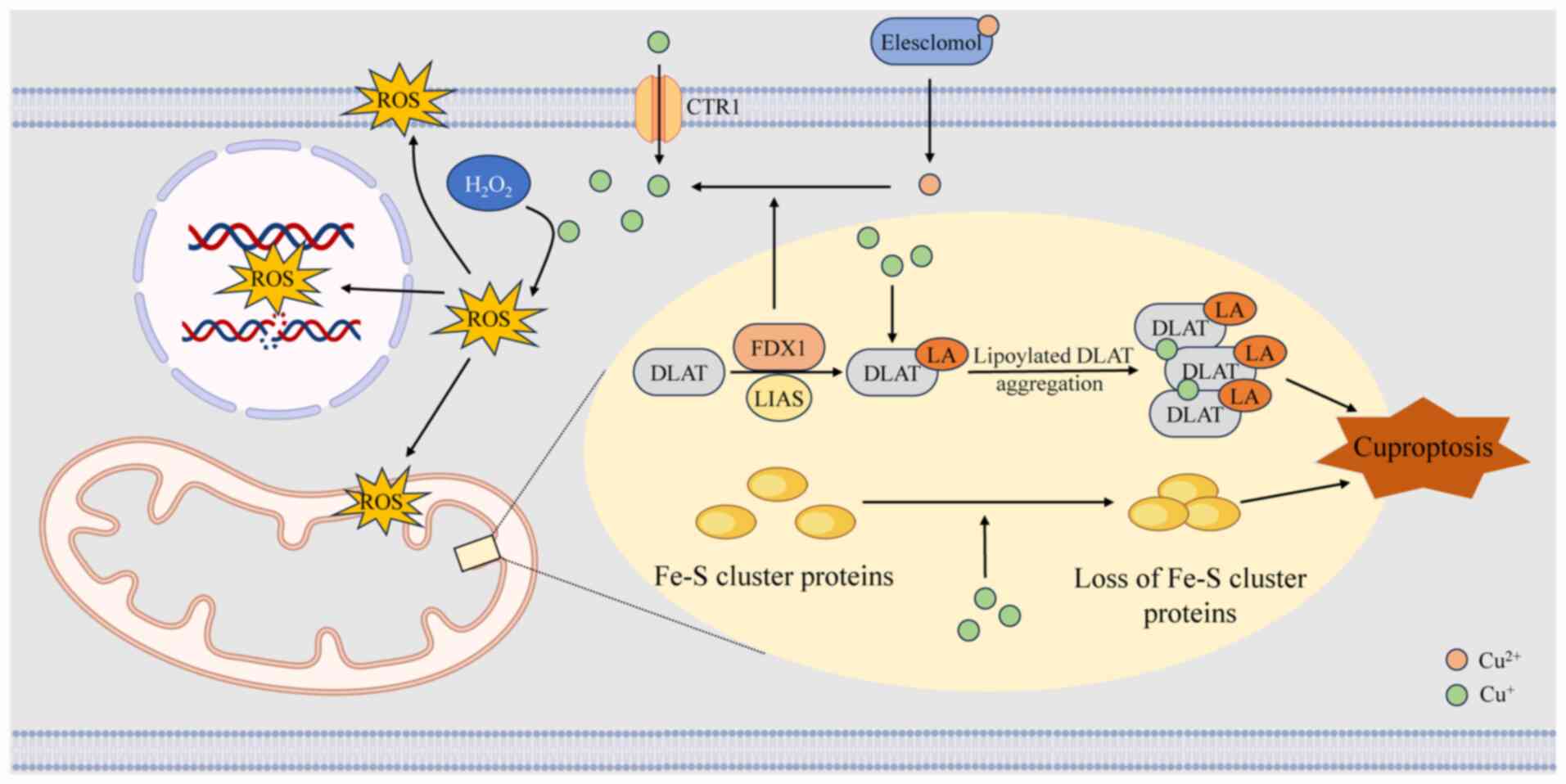
Tsvetkov P, Coy S, Petrova B, Dreishpoon
M, Verma A, Abdusamad M, Rossen J, Joesch-Cohen L, Humeidi R,
Spangler RD, et al: Copper induces cell death by targeting
lipoylated TCA cycle proteins. Science. 375:1254–1261. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Chen J, Yang X, Li W, Lin Y, Lin R, Cai X,
Yan B, Xie B and Li J: Potential molecular and cellular mechanisms
of the effects of cuproptosis-related genes in the cardiomyocytes
of patients with diabetic heart failure: A bioinformatics analysis.
Front Endocrinol (Lausanne). 15:13703872024. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Tan X, Xu S, Zeng Y, Qin Z, Yu F, Jiang H,
Xu H, Li X, Wang X, Zhang G, et al: Identification of diagnostic
signature and immune infiltration for ischemic cardiomyopathy based
on cuproptosis-related genes through bioinformatics analysis and
experimental validation. Int Immunopharmacol. 138:1125742024.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Chen YT, Xu XH, Lin L, Tian S and Wu GF:
Identification of three cuproptosis-specific expressed genes as
diagnostic biomarkers and therapeutic targets for atherosclerosis.
Int J Med Sci. 20:836–848. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Liu Y and Miao J: An emerging role of
defective copper metabolism in heart disease. Nutrients.
14:7002022. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Mason KE: A conspectus of research on
copper metabolism and requirements of man. J Nutr. 109:1979–2066.
1979. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Pierson H, Yang H and Lutsenko S: Copper
transport and disease: What can we learn from organoids? Annu Rev
Nutr. 39:75–94. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wu J, He J, Liu Z, Zhu X, Li Z, Chen A and
Lu J: Cuproptosis: Mechanism, role, and advances in urological
malignancies. Med Res Rev. 44:1662–1682. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Liu WQ, Lin WR, Yan L, Xu WH and Yang J:
Copper homeostasis and cuproptosis in cancer immunity and therapy.
Immunol Rev. 321:211–227. 2024. View Article : Google Scholar
|
|
13
|
Lee J, Peña MM, Nose Y and Thiele DJ:
Biochemical characterization of the human copper transporter Ctr1.
J Biol Chem. 277:4380–4387. 2002. View Article : Google Scholar
|
|
14
|
Arredondo M, Muñoz P, Mura CV and Nùñez
MT: DMT1, a physiologically relevant apical Cu1+ transporter of
intestinal cells. Am J Physiol Cell Physiol. 284:C1525–C1530. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ross MO, Xie Y, Owyang RC, Ye C, Zbihley
ONP, Lyu R, Wu T, Wang P, Karginova O, Olopade OI, et al: PTPN2
copper-sensing relays copper level fluctuations into EGFR/CREB
activation and associated CTR1 transcriptional repression. Nat
Commun. 15:69472024. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Chen L, Min J and Wang F: Copper
homeostasis and cuproptosis in health and disease. Signal Transduct
Target Ther. 7:3782022. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Li Y, Ma J, Wang R, Luo Y, Zheng S and
Wang X: Zinc transporter 1 functions in copper uptake and
cuproptosis. Cell Metab. 36:2118–2129.e6. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Krężel A and Maret W: The bioinorganic
chemistry of mammalian metallothioneins. Chem Rev. 121:14594–14648.
2021. View Article : Google Scholar
|
|
19
|
Yang D, Xiao P, Qiu B, Yu HF and Teng CB:
Copper chaperone antioxidant 1: Multiple roles and a potential
therapeutic target. J Mol Med (Berl). 101:527–542. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Perkal O, Qasem Z, Turgeman M, Schwartz R,
Gevorkyan-Airapetov L, Pavlin M, Magistrato A, Major DT and
Ruthstein S: Cu(I) controls conformational states in human Atox1
metallochaperone: An EPR and multiscale simulation study. J Phys
Chem B. 124:4399–4411. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Xue Q, Kang R, Klionsky DJ, Tang D, Liu J
and Chen X: Copper metabolism in cell death and autophagy.
Autophagy. 19:2175–2195. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Harris ED: Cellular copper transport and
metabolism. Annu Rev Nutr. 20:291–310. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Lutsenko S, Barnes NL, Bartee MY and
Dmitriev OY: Function and regulation of human copper-transporting
ATPases. Physiol Rev. 87:1011–1046. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Wong PC, Waggoner D, Subramaniam JR,
Tessarollo L, Bartnikas TB, Culotta VC, Price DL, Rothstein J and
Gitlin JD: Copper chaperone for superoxide dismutase is essential
to activate mammalian Cu/Zn superoxide dismutase. Proc Natl Acad
Sci USA. 97:2886–2891. 2000. View Article : Google Scholar
|
|
25
|
Suzuki Y, Ali M, Fischer M and Riemer J:
Human copper chaperone for superoxide dismutase 1 mediates its own
oxidation-dependent import into mitochondria. Nat Commun.
4:24302013. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Bertinato J and L'Abbé MR: Copper
modulates the degradation of copper chaperone for Cu,Zn superoxide
dismutase by the 26 S proteosome. J Biol Chem. 278:35071–35078.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Sturtz LA, Diekert K, Jensen LT, Lill R
and Culotta VC: A fraction of yeast Cu,Zn-superoxide dismutase and
its metallochaperone, CCS, localize to the intermembrane space of
mitochondria. A physiological role for SOD1 in guarding against
mitochondrial oxidative damage. J Biol Chem. 276:38084–38089. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Grasso M, Bond GJ, Kim YJ, Boyd S, Matson
Dzebo M, Valenzuela S, Tsang T, Schibrowsky NA, Alwan KB, Blackburn
NJ, et al: The copper chaperone CCS facilitates copper binding to
MEK1/2 to promote kinase activation. J Biol Chem. 297:1013142021.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Garza NM, Swaminathan AB, Maremanda KP,
Zulkifli M and Gohil VM: Mitochondrial copper in human genetic
disorders. Trends Endocrinol Metab. 34:21–33. 2023. View Article : Google Scholar
|
|
30
|
Maxfield AB, Heaton DN and Winge DR: Cox17
is functional when tethered to the mitochondrial inner membrane. J
Biol Chem. 279:5072–5080. 2004. View Article : Google Scholar
|
|
31
|
Sailer J, Nagel J, Akdogan B, Jauch AT,
Engler J, Knolle PA and Zischka H: Deadly excess copper. Redox
Biol. 75:1032562024. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Boyd SD, Ullrich MS, Skopp A and Winkler
DD: Copper sources for Sod1 activation. Antioxidants (Basel).
9:5002020. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Polishchuk EV, Concilli M, Iacobacci S,
Chesi G, Pastore N, Piccolo P, Paladino S, Baldantoni D, van
IJzendoorn SC, Chan J, et al: Wilson disease protein ATP7B utilizes
lysosomal exocytosis to maintain copper homeostasis. Dev Cell.
29:686–700. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Doguer C, Ha JH and Collins JF:
Intersection of iron and copper metabolism in the mammalian
intestine and liver. Compr Physiol. 8:1433–1461. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
La Fontaine S and Mercer JF: Trafficking
of the copper-ATPases, ATP7A and ATP7B: Role in copper homeostasis.
Arch Biochem Biophys. 463:149–167. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Festa RA and Thiele DJ: Copper: An
essential metal in biology. Curr Biol. 21:R877–R883. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Turnlund JR, Keyes WR, Anderson HL and
Acord LL: Copper absorption and retention in young men at three
levels of dietary copper by use of the stable isotope 65Cu. Am J
Clin Nutr. 49:870–878. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
van den Berghe PVE and Klomp LWJ:
Posttranslational regulation of copper transporters. J Biol Inorg
Chem. 15:37–46. 2010. View Article : Google Scholar
|
|
39
|
Ge EJ, Bush AI, Casini A, Cobine PA, Cross
JR, DeNicola GM, Dou QP, Franz KJ, Gohil VM, Gupta S, et al:
Connecting copper and cancer: From transition metal signalling to
metalloplasia. Nat Rev Cancer. 22:102–113. 2022. View Article : Google Scholar :
|
|
40
|
Yang L, Yang P, Lip GYH and Ren J: Copper
homeostasis and cuproptosis in cardiovascular disease therapeutics.
Trends Pharmacol Sci. 44:573–585. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Chang W and Li P: Copper and diabetes:
Current research and prospect. Mol Nutr Food Res. 67:e23004682023.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Jiayi H, Ziyuan T, Tianhua X, Mingyu Z,
Yutong M, Jingyu W, Hongli Z and Li S: Copper homeostasis in
chronic kidney disease and its crosstalk with ferroptosis.
Pharmacol Res. 202:1071392024. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Shanbhag VC, Gudekar N, Jasmer K,
Papageorgiou C, Singh K and Petris MJ: Copper metabolism as a
unique vulnerability in cancer. Biochim Biophys Acta Mol Cell Res.
1868:1188932021. View Article : Google Scholar :
|
|
44
|
Lin CH, Chin Y, Zhou M, Sobol RW, Hung MC
and Tan M: Protein lipoylation: Mitochondria, cuproptosis, and
beyond. Trends Biochem Sci. 49:729–744. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Gupte A and Mumper RJ: Elevated copper and
oxidative stress in cancer cells as a target for cancer treatment.
Cancer Treat Rev. 35:32–46. 2009. View Article : Google Scholar
|
|
46
|
Wang Y, Chen Y, Zhang J, Yang Y, Fleishman
JS, Wang Y, Wang J, Chen J, Li Y and Wang H: Cuproptosis: A novel
therapeutic target for overcoming cancer drug resistance. Drug
Resist Updat. 72:1010182024. View Article : Google Scholar
|
|
47
|
Han J, Luo J, Wang C, Kapilevich L and
Zhang XA: Roles and mechanisms of copper homeostasis and
cuproptosis in osteoarticular diseases. Biomed Pharmacother.
174:1165702024. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Chen W, Yang A, Jia J, Popov YV, Schuppan
D and You H: Lysyl oxidase (LOX) family members: Rationale and
their potential as therapeutic targets for liver fibrosis.
Hepatology. 72:729–741. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Doñate F, Juarez JC, Burnett ME, Manuia
MM, Guan X, Shaw DE, Smith EL, Timucin C, Braunstein MJ, Batuman OA
and Mazar AP: Identification of biomarkers for the antiangiogenic
and antitumour activity of the superoxide dismutase 1 (SOD1)
inhibitor tetrathiomolybdate (ATN-224). Br J Cancer. 98:776–783.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Tsui KH, Hsiao JH, Lin LT, Tsang YL, Shao
AN, Kuo CH, Chang R, Wen ZH and Li CJ: The cross-communication of
cuproptosis and regulated cell death in human pathophysiology. Int
J Biol Sci. 20:218–230. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Han X, Zhang X, Liu Z, Liu H, Wu D, He Y,
Yuan K, Lyu Y and Liu X: Copper-based nanotubes that enhance
starvation therapy through cuproptosis for synergistic cancer
treatment. Adv Sci (Weinh). 12:e041212025. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Yan C, Lv H, Feng Y, Li Y and Zhao Z:
Inhalable nanoparticles with enhanced cuproptosis and cGAS-STING
activation for synergistic lung metastasis immunotherapy. Acta
Pharm Sin B. 14:3697–3710. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Wang D, Tian Z, Zhang P, Zhen L, Meng Q,
Sun B, Xu X, Jia T and Li S: The molecular mechanisms of
cuproptosis and its relevance to cardiovascular disease. Biomed
Pharmacother. 163:1148302023. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Dreishpoon MB, Bick NR, Petrova B, Warui
DM, Cameron A, Booker SJ, Kanarek N, Golub TR and Tsvetkov P: FDX1
regulates cellular protein lipoylation through direct binding to
LIAS. J Biol Chem. 299:1050462023. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Rowland EA, Snowden CK and Cristea IM:
Protein lipoylation: An evolutionarily conserved metabolic
regulator of health and disease. Curr Opin Chem Biol. 42:76–85.
2018. View Article : Google Scholar :
|
|
56
|
Kuang J, Liu A, Xu L, Wang G, Zhang Z,
Tian C and Yu L: Electron paramagnetic resonance insights into
direct electron transfer between FDX1 and
elesclomol-Cu2+ complex in cuproptosis. Chemistry.
31:e2025011452025. View Article : Google Scholar
|
|
57
|
Hu HT, Zhang ZY, Luo ZX, Ti HB, Wu JJ, Nie
H, Yuan ZD, Wu X, Zhang KY, Shi SW, et al: Emerging regulated cell
death mechanisms in bone remodeling: Decoding ferroptosis,
cuproptosis, disulfidptosis, and PANoptosis as therapeutic targets
for skeletal disorders. Cell Death Discov. 11:3352025. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Yang Z, Feng R and Zhao H: Cuproptosis and
Cu: A new paradigm in cellular death and their role in
non-cancerous diseases. Apoptosis. 29:1330–1360. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Huang L, Zhu J, Wu G, Xiong W, Feng J, Yan
C, Yang J, Li Z, Fan Q, Ren B, et al: A strategy of 'adding fuel to
the flames' enables a self-accelerating cycle of
ferroptosis-cuproptosis for potent antitumor therapy. Biomaterials.
311:1227012024. View Article : Google Scholar
|
|
60
|
Liu G, Tang R, Wang C, Yu D, Wang Z, Yang
H, Wei J, Zhu S, Gao F, Yuan F and Pan B: Bimetallic nanoconjugate
hijack Fe-S clusters to drive a closed-loop cuproptosis-ferroptosis
strategy for osteosarcoma inhibition. J Colloid Interface Sci.
703:1390522025.Epub ahead of print. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Zhang M, Xu H, Wu X, Chen B, Gong X and He
Y: Engineering dual-responsive nanoplatform achieves copper
metabolism disruption and glutathione consumption to provoke
cuproptosis/ferroptosis/apoptosis for cancer therapy. ACS Appl
Mater Interfaces. 17:20726–20740. 2025. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Husain N and Mahmood R: Copper(II)
generates ROS and RNS, impairs antioxidant system and damages
membrane and DNA in human blood cells. Environ Sci Pollut Res Int.
26:20654–20668. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Alqarni MH, Muharram MM, Alshahrani SM and
Labrou NE: Copper-induced oxidative cleavage of glutathione
transferase F1-1 from Zea mays. Int J Biol Macromol. 128:493–498.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Wang K, Ning X, Qin C, Wang J, Yan W, Zhou
X, Wang D, Cao J and Feng Y: Respiratory exposure to copper oxide
particles causes multiple organ injuries via oxidative stress in a
rat model. Int J Nanomedicine. 17:4481–4496. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Piret JP, Jacques D, Audinot JN, Mejia J,
Boilan E, Noël F, Fransolet M, Demazy C, Lucas S, Saout C and
Toussaint O: Copper(II) oxide nanoparticles penetrate into HepG2
cells, exert cytotoxicity via oxidative stress and induce
pro-inflammatory response. Nanoscale. 4:7168–7184. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
He H, Zou Z, Wang B, Xu G, Chen C, Qin X,
Yu C and Zhang J: Copper oxide nanoparticles induce oxidative DNA
damage and cell death via copper ion-mediated P38 MAPK activation
in vascular endothelial cells. Int J Nanomedicine. 15:3291–3302.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Martin F, Linden T, Katschinski DM, Oehme
F, Flamme I, Mukhopadhyay CK, Eckhardt K, Tröger J, Barth S,
Camenisch G and Wenger RH: Copper-dependent activation of
hypoxia-inducible factor (HIF)-1: Implications for ceruloplasmin
regulation. Blood. 105:4613–4619. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Xiao Y, Wang T, Song X, Yang D, Chu Q and
Kang YJ: Copper promotion of myocardial regeneration. Exp Biol Med
(Maywood). 245:911–921. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Martínez-González J, Varona S, Cañes L,
Galán M, Briones AM, Cachofeiro V and Rodríguez C: Emerging roles
of Lysyl oxidases in the cardiovascular system: New concepts and
therapeutic challenges. Biomolecules. 9:6102019. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Wang K, Li Y, Luo C and Chen Y: Dynamic
AFM detection of the oxidation-induced changes in size, stiffness,
and stickiness of low-density lipoprotein. J Nanobiotechnology.
18:1672020. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Widyananda MH, Grahadi R, Dinana IA,
Ansori ANM, Kharisma VD, Jakhmola V, Rebezov M, Derkho M, Burkov P,
Scherbakov P and Zainul R: Anti-atherosclerotic potential of fatty
acids in Chlorella vulgaris via inhibiting the foam cell formation:
An in silico study. Adv Life Sci. 12:296–303. 2025. View Article : Google Scholar
|
|
72
|
Widyananda MH, Kurniasari CA, Alam FM,
Rizky WC, Dings TGA, Ansori ANM and Antonius Y: Exploration of
potentially bioactive compounds from Fingerroot (Boesenbergia
rotunda L.) as inhibitor of atherosclerosis-related proteins (CETP,
ACAT1, OSC, sPLA2): An in silico study. Jordan J Pharm Sci.
16:550–564. 2023. View Article : Google Scholar
|
|
73
|
Kciuk M, Gielecińska A, Kałuzińska-Kołat
Ż, Yahya EB and Kontek R: Ferroptosis and cuproptosis:
Metal-dependent cell death pathways activated in response to
classical chemotherapy-significance for cancer treatment? Biochim
Biophys Acta Rev Cancer. 1879:1891242024. View Article : Google Scholar
|
|
74
|
Zhou D, Mao Q, Sun Y, Cheng H, Zhao J, Liu
Q, Deng M, Xu S and Zhao X: Association of blood copper with the
subclinical carotid atherosclerosis: An observational study. J Am
Heart Assoc. 13:e0334742024. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Zhu C, Wang B, Xiao L, Guo Y, Zhou Y, Cao
L, Yang S and Chen W: Mean platelet volume mediated the
relationships between heavy metals exposure and atherosclerotic
cardiovascular disease risk: A community-based study. Eur J Prev
Cardiol. 27:830–839. 2020. View Article : Google Scholar
|
|
76
|
Long P, Wang Q, Zhang Y, Zhu X, Yu K,
Jiang H, Liu X, Zhou M, Yuan Y, Liu K, et al: Profile of
copper-associated DNA methylation and its association with incident
acute coronary syndrome. Clin Epigenetics. 13:192021. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Kuzan A, Wujczyk M and Wiglusz RJ: The
study of the aorta metallomics in the context of atherosclerosis.
Biomolecules. 11:9462021. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Li H, Zhao L, Wang T and James Kang Y:
Dietary Cholesterol supplements disturb copper homeostasis in
multiple organs in rabbits: Aorta copper concentrations negatively
correlate with the severity of atherosclerotic lesions. Biol Trace
Elem Res. 200:164–171. 2022. View Article : Google Scholar
|
|
79
|
Bügel S, Harper A, Rock E, O'Connor JM,
Bonham MP and Strain JJ: Effect of copper supplementation on
indices of copper status and certain CVD risk markers in young
healthy women. Br J Nutr. 94:231–236. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Diaf M and Khaled MB: Associations between
dietary antioxidant intake and markers of atherosclerosis in
middle-aged women from north-western Algeria. Front Nutr. 5:292018.
View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Kärberg K, Forbes A and Lember M: Raised
dietary Zn:Cu ratio increases the risk of atherosclerosis in type 2
diabetes. Clin Nutr ESPEN. 50:218–224. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Sudhahar V, Shi Y, Kaplan JH, Ushio-Fukai
M and Fukai T: Whole-transcriptome sequencing analyses of nuclear
antixoxidant-1 in endothelial cells: Role in inflammation and
atherosclerosis. Cells. 11:29192022. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Das A, Sudhahar V, Ushio-Fukai M and Fukai
T: Novel interaction of antioxidant-1 with TRAF4: Role in
inflammatory responses in endothelial cells. Am J Physiol Cell
Physiol. 317:C1161–C1171. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Yang L, Chen X, Cheng H and Zhang L:
Dietary copper intake and risk of stroke in adults: A case-control
study based on national health and nutrition examination survey
2013-2018. Nutrients. 14:4092022. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Hu L, Bi C, Lin T, Liu L, Song Y, Wang P,
Wang B, Fang C, Ma H, Huang X, et al: Association between plasma
copper levels and first stroke: A community-based nested
case-control study. Nutr Neurosci. 25:1524–1533. 2022. View Article : Google Scholar
|
|
86
|
Lai M, Wang D, Lin Z and Zhang Y: Small
molecule copper and its relative metabolites in serum of cerebral
ischemic stroke patients. J Stroke Cerebrovasc Dis. 25:214–219.
2016. View Article : Google Scholar
|
|
87
|
Xiao Y, Yuan Y, Liu Y, Yu Y, Jia N, Zhou
L, Wang H, Huang S, Zhang Y, Yang H, et al: Circulating multiple
metals and incident stroke in Chinese adults. Stroke. 50:1661–1668.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Zhao H, Mei K, Hu Q, Wu Y, Xu Y, Qinling,
Yu P, Deng Y, Zhu W, Yan Z and Liu X: Circulating copper levels and
the risk of cardio-cerebrovascular diseases and cardiovascular and
all-cause mortality: A systematic review and meta-analysis of
longitudinal studies. Environ Pollut. 340:1227112024. View Article : Google Scholar
|
|
89
|
Zhang M, Li W, Wang Y, Wang T, Ma M and
Tian C: Association between the change of serum copper and ischemic
stroke: A systematic review and meta-analysis. J Mol Neurosci.
70:475–480. 2020. View Article : Google Scholar
|
|
90
|
Peng Y, Ren Q, Ma H, Lin C, Yu M, Li Y,
Chen J, Xu H, Zhao P, Pan S, et al: Covalent organic framework
based cytoprotective therapy after ischemic stroke. Redox Biol.
71:1031062024. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Xu J, Xu G and Fang J: Association between
serum copper and stroke risk factors in adults: Evidence from the
national health and nutrition examination survey, 2011-2016. Biol
Trace Elem Res. 200:1089–1094. 2022. View Article : Google Scholar
|
|
92
|
Yang F and Smith MJ: Metal profiling in
coronary ischemia-reperfusion injury: Implications for KEAP1/NRF2
regulated redox signaling. Free Radic Biol Med. 210:158–171. 2024.
View Article : Google Scholar
|
|
93
|
Ding C, Wang B, Zheng J, Zhang M, Li Y,
Shen HH, Guo Y, Zheng B, Tian P, Ding X and Xue W: Neutrophil
membrane-inspired nanorobots act as antioxidants ameliorate
ischemia reperfusion-induced acute kidney injury. ACS Appl Mater
Interfaces. 15:40292–40303. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Kokubo Y, Matson GB, Derugin N, Hill T,
Mancuso A, Chan PH and Weinstein PR: Transgenic mice expressing
human copper-zinc superoxide dismutase exhibit attenuated apparent
diffusion coefficient reduction during reperfusion following focal
cerebral ischemia. Brain Res. 947:1–8. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Chen Z, Oberley TD, Ho Y, Chua CC, Siu B,
Hamdy RC, Epstein CJ and Chua BH: Overexpression of CuZnSOD in
coronary vascular cells attenuates myocardial ischemia/reperfusion
injury. Free Radic Biol Med. 29:589–596. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Tanaka M, Mokhtari GK, Terry RD, Balsam
LB, Lee KH, Kofidis T, Tsao PS and Robbins RC: Overexpression of
human copper/zinc superoxide dismutase (SOD1) suppresses
ischemia-reperfusion injury and subsequent development of graft
coronary artery disease in murine cardiac grafts. Circulation.
110(11 Suppl 1): II200–II206. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Song W, Tang Q, Teng L, Zhang M, Sha S, Li
B and Zhu L: Exercise for myocardial ischemia-reperfusion injury: A
systematic review and meta-analysis based on preclinical studies.
Microvasc Res. 147:1045022023. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Kuster GM, Nietlispach F, Kiowski W,
Schindler R, Bernheim A, Schuetz P, Mueller B, Morgenthaler NG,
Rüter F, Riesen W, et al: Role of RAS inhibition in the regulation
of Cu/Zn-SOD in the cardiac and peripheral arterial beds in humans.
Clin Pharmacol Ther. 87:686–692. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Kunutsor SK, Voutilainen A, Kurl S and
Laukkanen JA: Serum copper-to-zinc ratio is associated with heart
failure and improves risk prediction in middle-aged and older
Caucasian men: A prospective study. Nutr Metab Cardiovasc Dis.
32:1924–1935. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Alexanian I, Parissis J, Farmakis D,
Athanaselis S, Pappas L, Gavrielatos G, Mihas C, Paraskevaidis I,
Sideris A, Kremastinos D, et al: Clinical and echocardiographic
correlates of serum copper and zinc in acute and chronic heart
failure. Clin Res Cardiol. 103:938–949. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Liu R, Yao J, Chen K and Peng W:
Association between biomarkers of zinc and copper status and heart
failure: A meta-analysis. ESC Heart Fail. 11:2546–2556. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Ghaemian A, Salehifar E, Jalalian R,
Ghasemi F, Azizi S, Masoumi S, Shiraj H, Mohammadpour RA and
Bagheri GA: Zinc and copper levels in severe heart failure and the
effects of atrial fibrillation on the zinc and copper status. Biol
Trace Elem Res. 143:1239–1246. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Hammadah M, Fan Y, Wu Y, Hazen SL and Tang
WH: Prognostic value of elevated serum ceruloplasmin levels in
patients with heart failure. J Card Fail. 20:946–952. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
104
|
de Andrade Freire FL, Dantas-Komatsu RCS,
de Lira NRD, Diniz RVZ, Lima SCVC, Barbosa F Jr, Pedrosa LFC and
Sena-Evangelista KCM: Biomarkers of zinc and copper status and
associated factors in outpatients with ischemic and non-ischemic
heart failure. J Am Nutr Assoc. 41:231–239. 2022.
|
|
105
|
Niu YY, Aierken A and Feng L: Unraveling
the link between dietary factors and cardiovascular metabolic
diseases: Insights from a two-sample Mendelian randomization
investigation. Heart Lung. 63:72–77. 2024. View Article : Google Scholar
|
|
106
|
Cimen YA, Taslidere B, Sarikaya U, Demirel
M, Acikgoz N and Selek S: Assessment of oxidative stress and trace
element dynamics in acute myocardial infarction and heart failure:
A focus on zinc, copper, and thiol dynamics. Clinics (Sao Paulo).
80:1007552025. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Gorący I, Rębacz-Maron E, Korbecki J and
Gorący J: Concentrations of Mg, Ca, Fe, Cu, Zn, P and
anthropometric and biochemical parameters in adults with chronic
heart failure. PeerJ. 9:e122072021. View Article : Google Scholar
|
|
108
|
Zou R, Zhang M, Zou Z, Shi W, Tan S, Wang
C, Xu W, Jin J, Milton S, Chen Y, et al: Single-cell
transcriptomics reveals zinc and copper ions homeostasis in
epicardial adipose tissue of heart failure. Int J Biol Sci.
19:4036–4051. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Guo Q, Cai J, Qu Q, Cheang I, Shi J, Pang
H and Li X: Association of blood trace elements levels with
cardiovascular disease in US adults: A cross-sectional study from
the national health and nutrition examination survey 2011-2016.
Biol Trace Elem Res. 202:3037–3050. 2024. View Article : Google Scholar
|
|
110
|
Malekahmadi M, Firouzi S, Rezayi M,
Ghazizadeh H, Ranjbar G, Ferns GA and Mobarhan MG: Association of
zinc and copper status with cardiovascular diseases and their
assessment methods: A review study. Mini Rev Med Chem.
20:2067–2078. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Bomer N, Pavez-Giani MG, Grote Beverborg
N, Cleland JGF, van Veldhuisen DJ and van der Meer P: Micronutrient
deficiencies in heart failure: Mitochondrial dysfunction as a
common pathophysiological mechanism? J Intern Med. 291:713–731.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Witte KK, Nikitin NP, Parker AC, von
Haehling S, Volk HD, Anker SD, Clark AL and Cleland JG: The effect
of micronutrient supplementation on quality-of-life and left
ventricular function in elderly patients with chronic heart
failure. Eur Heart J. 26:2238–2244. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Dieterich S, Bieligk U, Beulich K,
Hasenfuss G and Prestle J: Gene expression of antioxidative enzymes
in the human heart: Increased expression of catalase in the
end-stage failing heart. Circulation. 101:33–39. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Zhang S, Liu H, Amarsingh GV, Cheung CCH,
Wu D, Narayanan U, Zhang L and Cooper GJS: Restoration of
myocellular copper-trafficking proteins and mitochondrial copper
enzymes repairs cardiac function in rats with diabetes-evoked heart
failure. Metallomics. 12:259–272. 2020. View Article : Google Scholar
|
|
115
|
Ennezat PV, Malendowicz SL, Testa M,
Colombo PC, Cohen-Solal A, Evans T and LeJemtel TH: Physical
training in patients with chronic heart failure enhances the
expression of genes encoding antioxidative enzymes. J Am Coll
Cardiol. 38:194–198. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Chen Z, Zhu Y, Chen S, Li Z, Fu G and Wang
Y: Immune patterns of cuproptosis in ischemic heart failure: A
transcriptome analysis. J Cell Mol Med. 28:e181872024. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Hao D, Meng Q, Li C, Lu S, Xiang X, Pei Q,
Jing X and Xie Z: A paclitaxel prodrug with copper depletion for
combined therapy toward triple-negative breast cancer. ACS Nano.
17:12383–12393. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Johnson TW, Holt J, Kleyman A, Zhou S,
Sammut E, Bruno VD, Gaupp C, Stanzani G, Martin J, Arina P, et al:
Development and translation of thiometallate sulfide donors using a
porcine model of coronary occlusion and reperfusion. Redox Biol.
73:1031672024. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Dyson A, Dal-Pizzol F, Sabbatini G, Lach
AB, Galfo F, Dos Santos Cardoso J, Pescador Mendonça B, Hargreaves
I, Bollen Pinto B, Bromage DI, et al: Ammonium tetrathiomolybdate
following ischemia/reperfusion injury: Chemistry, pharmacology, and
impact of a new class of sulfide donor in preclinical injury
models. PLoS Med. 14:e10023102017. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Chen YF, Qi RQ, Song JW, Wang SY, Dong ZJ,
Chen YH, Liu Y, Zhou XY, Li J, Liu XY and Zhong JC: Sirtuin 7
ameliorates cuproptosis, myocardial remodeling and heart
dysfunction in hypertension through the modulation of YAP/ATP7A
signaling. Apoptosis. 29:2161–2182. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Bogaard HJ, Mizuno S, Guignabert C, Al
Hussaini AA, Farkas D, Ruiter G, Kraskauskas D, Fadel E, Allegood
JC, Humbert M, et al: Copper dependence of angioproliferation in
pulmonary arterial hypertension in rats and humans. Am J Respir
Cell Mol Biol. 46:582–591. 2012. View Article : Google Scholar :
|
|
122
|
Wei H, Zhang WJ, McMillen TS, Leboeuf RC
and Frei B: Copper chelation by tetrathiomolybdate inhibits
vascular inflammation and atherosclerotic lesion development in
apolipoprotein E-deficient mice. Atherosclerosis. 223:306–313.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Ambi A, Stanisavljevic A, Victor TW,
Lowery AW, Davis J, Van Nostrand WE and Miller LM: Evaluation of
copper chelation therapy in a transgenic rat model of cerebral
amyloid angiopathy. ACS Chem Neurosci. 14:378–388. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Mandinov L, Moodie KL, Mandinova A, Zhuang
Z, Redican F, Baklanov D, Lindner V, Maciag T, Simons M and de
Muinck ED: Inhibition of in-stent restenosis by oral copper
chelation in porcine coronary arteries. Am J Physiol Heart Circ
Physiol. 291:H2692–H2697. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Cooper GJ, Young AA, Gamble GD, Occleshaw
CJ, Dissanayake AM, Cowan BR, Brunton DH, Baker JR, Phillips AR,
Frampton CM, et al: A copper(II)-selective chelator ameliorates
left-ventricular hypertrophy in type 2 diabetic patients: A
randomised placebo-controlled study. Diabetologia. 52:715–722.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Zhang S, Liu H, Amarsingh GV, Cheung CC,
Hogl S, Narayanan U, Zhang L, McHarg S, Xu J, Gong D, et al:
Diabetic cardiomyopathy is associated with defective myocellular
copper regulation and both defects are rectified by divalent copper
chelation. Cardiovasc Diabetol. 13:1002014. View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Zhang L, Ward ML, Phillips ARJ, Zhang S,
Kennedy J, Barry B, Cannell MB and Cooper GJS: Protection of the
heart by treatment with a divalent-copper-selective chelator
reveals a novel mechanism underlying cardiomyopathy in diabetic
rats. Cardiovasc Diabetol. 12:1232013. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Lamas GA, Anstrom KJ, Navas-Acien A,
Boineau R, Nemeth H, Huang Z, Wen J, Rosenberg Y, Stylianou M,
Jones TLZ, et al: Edetate disodium-based chelation for patients
with a previous myocardial infarction and diabetes: TACT2
randomized clinical trial. JAMA. 332:794–803. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Lamas GA, Goertz C, Boineau R, Mark DB,
Rozema T, Nahin RL, Lindblad L, Lewis EF, Drisko J and Lee KL; TACT
Investigators: Effect of disodium EDTA chelation regimen on
cardiovascular events in patients with previous myocardial
infarction: The TACT randomized trial. JAMA. 309:1241–1250. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Knudtson ML, Wyse DG, Galbraith PD, Brant
R, Hildebrand K, Paterson D, Richardson D, Burkart C and Burgess E;
Program to Assess Alternative Treatment Strategies to Achieve
Cardiac Health (PATCH) Investigators: Chelation therapy for
ischemic heart disease: A randomized controlled trial. JAMA.
287:481–486. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Anderson TJ, Hubacek J, Wyse DG and
Knudtson ML: Effect of chelation therapy on endothelial function in
patients with coronary artery disease: PATCH substudy. J Am Coll
Cardiol. 41:420–425. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Escolar E, Lamas GA, Mark DB, Boineau R,
Goertz C, Rosenberg Y, Nahin RL, Ouyang P, Rozema T, Magaziner A,
et al: The effect of an EDTA-based chelation regimen on patients
with diabetes mellitus and prior myocardial infarction in the trial
to assess chelation therapy (TACT). Circ Cardiovasc Qual Outcomes.
7:15–24. 2014. View Article : Google Scholar
|
|
133
|
Kirk FT, Munk DE, Swenson ES, Quicquaro
AM, Vendelbo MH, Larsen A, Schilsky ML, Ott P and Sandahl TD:
Effects of tetrathiomolybdate on copper metabolism in healthy
volunteers and in patients with Wilson disease. J Hepatol.
80:586–595. 2024. View Article : Google Scholar
|
|
134
|
Borchard S, Raschke S, Zak KM, Eberhagen
C, Einer C, Weber E, Müller SM, Michalke B, Lichtmannegger J,
Wieser A, et al: Bis-choline tetrathiomolybdate prevents
copper-induced blood-brain barrier damage. Life Sci Alliance.
5:e2021011642021. View Article : Google Scholar : PubMed/NCBI
|
|
135
|
Wang YM, Feng LS, Xu A, Ma XH, Zhang MT
and Zhang J: Copper ions: The invisible killer of cardiovascular
disease (Review). Mol Med Rep. 30:2102024. View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Juarez JC, Betancourt O Jr, Pirie-Shepherd
SR, Guan X, Price ML, Shaw DE, Mazar AP and Doñate F: Copper
binding by tetrathiomolybdate attenuates angiogenesis and tumor
cell proliferation through the inhibition of superoxide dismutase
1. Clin Cancer Res. 12:4974–4982. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
137
|
Yang D, Wang T, Liu J, Wang H and Kang YJ:
Reverse regulation of hepatic ceruloplasmin production in rat model
of myocardial ischemia. J Trace Elem Med Biol. 64:1266862021.
View Article : Google Scholar
|
|
138
|
Villarruz-Sulit MV, Forster R, Dans AL,
Tan FN and Sulit DV: Chelation therapy for atherosclerotic
cardiovascular disease. Cochrane Database Syst Rev.
5:Cd0027852020.PubMed/NCBI
|
|
139
|
Steinbrueck A, Sedgwick AC, Brewster JT
II, Yan KC, Shang Y, Knoll DM, Vargas-Zúñiga GI, He XP, Tian H and
Sessler JL: Transition metal chelators, pro-chelators, and
ionophores as small molecule cancer chemotherapeutic agents. Chem
Soc Rev. 49:3726–3747. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
140
|
Ranucci G, Polishchuck R and Iorio R:
Wilson's disease: Prospective developments towards new therapies.
World J Gastroenterol. 23:5451–5456. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
141
|
Zhang C, Huang T and Li L: Targeting
cuproptosis for cancer therapy: Mechanistic insights and clinical
perspectives. J Hematol Oncol. 17:682024. View Article : Google Scholar : PubMed/NCBI
|
|
142
|
Zheng P, Zhou C, Lu L, Liu B and Ding Y:
Elesclomol: A copper ionophore targeting mitochondrial metabolism
for cancer therapy. J Exp Clin Cancer Res. 41:2712022. View Article : Google Scholar : PubMed/NCBI
|
|
143
|
Li Y, Chen F, Chen J, Chan S, He Y, Liu W
and Zhang G: Disulfiram/copper induces antitumor activity against
both nasopharyngeal cancer cells and cancer-associated fibroblasts
through ROS/MAPK and ferroptosis pathways. Cancers (Basel).
12:1382020. View Article : Google Scholar : PubMed/NCBI
|
|
144
|
He P, Li H, Liu C, Liu M, Zhang Z, Zhang
Y, Zhou C, Li Q, Ye Z, Wu Q, et al: U-shaped association between
dietary copper intake and new-onset hypertension. Clin Nutr.
41:536–542. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
145
|
Li R, Bourcy K, Wang T, Sun M and Kang YJ:
The involvement of vimentin in copper-induced regression of
cardiomyocyte hypertrophy. Metallomics. 7:1331–1337. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
146
|
Liu Y, Tan L, Kuang Y, Zhang Y, Wang P,
Liu C and Ma Q: A national cross-sectional analysis of dietary
copper intake and abdominal aortic calcification in the US adults:
NHANES 2013-2014. Nutr Metab Cardiovasc Dis. 33:1941–1950. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
147
|
Hu S, Wei B and Zhang A: Association of
multiple dietary metal intake with cardiovascular-kidney-metabolic
syndrome: A cross-sectional study based on NHANES 2003-2018. Front
Nutr. 12:16124582025. View Article : Google Scholar : PubMed/NCBI
|
|
148
|
Xu H, Liu Z, Yao B and Xu Z: The impact of
dietary copper intake on cardiovascular morbidity and mortality
among hypertensive patients: A longitudinal analysis from NHANES
(2001-2018). BMC Public Health. 25:9362025. View Article : Google Scholar : PubMed/NCBI
|
|
149
|
Li X, Dehghan M, Tse LA, Lang X,
Rangarajan S, Liu W, Hu B, Yusuf S, Wang C and Li W: Associations
of dietary copper intake with cardiovascular disease and mortality:
Findings from the Chinese Perspective Urban and Rural epidemiology
(PURE-China) study. BMC Public Health. 23:25252023. View Article : Google Scholar : PubMed/NCBI
|
|
150
|
Cai L, Tan Y, Holland B and Wintergerst K:
Diabetic cardiomyopathy and cell death: Focus on metal-mediated
cell death. Cardiovasc Toxicol. 24:71–84. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
151
|
Kong B, Zheng X, Hu Y, Zhao Y, Hai J, Ti Y
and Bu P: Sirtuin3 attenuates pressure overload-induced
pathological myocardial remodeling by inhibiting cardiomyocyte
cuproptosis. Pharmacol Res. 216:1077392025. View Article : Google Scholar : PubMed/NCBI
|
|
152
|
Mo N, Tai C, Yang Y, Ling C, Zhang B, Wei
L, Yao C, Wang H and Chen C: MT2A promotes angiogenesis in
chronically ischemic brains through a copper-mitochondria
regulatory mechanism. J Transl Med. 23:1622025. View Article : Google Scholar : PubMed/NCBI
|
|
153
|
Huang XP, Shi ZH, Ming GF, Xu DM and Cheng
SQ: S-Allyl-L-cysteine (SAC) inhibits copper-induced apoptosis and
cuproptosis to alleviate cardiomyocyte injury. Biochem Biophys Res
Commun. 730:1503412024. View Article : Google Scholar : PubMed/NCBI
|
|
154
|
Huo S, Wang Q, Shi W, Peng L, Jiang Y, Zhu
M, Guo J, Peng D, Wang M, Men L, et al: ATF3/SPI1/SLC31A1 signaling
promotes cuproptosis induced by advanced glycosylation end products
in diabetic myocardial injury. Int J Mol Sci. 24:16672023.
View Article : Google Scholar : PubMed/NCBI
|
|
155
|
Lin Y, Chen K, Guo J, Chen P, Qian ZR and
Zhang T: Identification of cuproptosis-related genes and immune
infiltration in dilated cardiomyopathy. Int J Cardiol.
399:1317022024. View Article : Google Scholar : PubMed/NCBI
|
|
156
|
Zhou S, Wang L, Huang X, Wang T, Tang Y,
Liu Y and Xu M: Comprehensive bioinformatics analytics and in vivo
validation reveal SLC31A1 as an emerging diagnostic biomarker for
acute myocardial infarction. Aging (Albany NY). 16:8361–8377.
2024.PubMed/NCBI
|
|
157
|
Wang B, Zhou J and An N: Investigating
molecular markers linked to acute myocardial infarction and
cuproptosis: Bioinformatics analysis and validation in the AMI mice
model. PeerJ. 12:e172802024. View Article : Google Scholar : PubMed/NCBI
|
|
158
|
Fang C, Sun S, Chen W, Huang D, Wang F,
Wei W and Wang W: Bioinformatics analysis of the role of
cuproptosis gene in acute myocardial infarction. Minerva Cardiol
Angiol. 72:595–606. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
159
|
Zhang J, Yue Z, Zhu N and Zhao N:
Identification of potential biomarkers associated with cuproptosis
and immune microenvironment analysis in acute myocardial
infarction: A diagnostic accuracy study. Medicine (Baltimore).
104:e408172025. View Article : Google Scholar : PubMed/NCBI
|
|
160
|
Wang M, Xu X, Li J, Gao Z, Ding Y, Chen X,
Xiang Q and Shen L: Integrated bioinformatics and experiment
revealed that cuproptosis is the potential common pathogenesis of
three kinds of primary cardiomyopathy. Aging (Albany NY).
15:14210–14241. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
161
|
Wang Y, Wang Q, Liu P, Jin L, Qin X and
Zheng Q: Construction and validation of a cuproptosis-related
diagnostic gene signature for atrial fibrillation based on ensemble
learning. Hereditas. 160:342023. View Article : Google Scholar : PubMed/NCBI
|
|
162
|
Zhang B and He M: Identification of
potential biomarkers for coronary artery disease based on
cuproptosis. Cardiovasc Ther. 2023:59961442023. View Article : Google Scholar : PubMed/NCBI
|
|
163
|
Tu B, Song K, Zhou ZY, Lin LC, Liu ZY, Sun
H, Zhou Y, Sha JM, Shi Y, Yang JJ, et al: SLC31A1 loss depletes
mitochondrial copper and promotes cardiac fibrosis. Eur Heart J.
46:2458–2474. 2025. View Article : Google Scholar : PubMed/NCBI
|
|
164
|
Lv X, Zhao L, Song Y, Chen W and Tuo Q:
Deciphering the role of copper homeostasis in atherosclerosis: From
molecular mechanisms to therapeutic targets. Int J Mol Sci.
25:114622024. View Article : Google Scholar : PubMed/NCBI
|
|
165
|
Shen Z, Liu Z, Cai S, Fu H, Gan Y, Li X,
Wang X, Liu C, Ma W, Chen J and Li N: Copper homeostasis and
cuproptosis in myocardial infarction: Molecular mechanisms,
treatment strategies and potential therapeutic targets. Front
Pharmacol. 16:15255852025. View Article : Google Scholar : PubMed/NCBI
|
|
166
|
Chen G, Wei M, Zhao CY, Zhang AY, Su JB,
Ni ZR, Cai WW, Hou B, Du B, Liu MH, et al: Phillygenin ameliorates
myocardial ischemia-reperfusion injury by inhibiting cuproptosis
via the autophagy-lysosome degradation of CTR1. Free Radic Biol
Med. 237:542–557. 2025. View Article : Google Scholar : PubMed/NCBI
|
|
167
|
Lutsenko S, Roy S and Tsvetkov P:
Mammalian copper homeostasis: Physiological roles and molecular
mechanisms. Physiol Rev. 105:441–491. 2025. View Article : Google Scholar :
|
|
168
|
Goutman SA, Hardiman O, Al-Chalabi A, Chió
A, Savelieff MG, Kiernan MC and Feldman EL: Emerging insights into
the complex genetics and pathophysiology of amyotrophic lateral
sclerosis. Lancet Neurol. 21:465–479. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
169
|
Meng K, Jia H, Hou X, Zhu Z, Lu Y, Feng Y,
Feng J, Xia Y, Tan R, Cui F and Yuan J: Mitochondrial dysfunction
in neurodegenerative diseases: Mechanisms and corresponding
therapeutic strategies. Biomedicines. 13:3272025. View Article : Google Scholar : PubMed/NCBI
|
|
170
|
Suwara J and Hartman ML: Balancing between
cuproplasia and copper-dependent cell death: Molecular basis and
clinical implications of ATOX1 in cancer. J Exp Clin Cancer Res.
44:2222025. View Article : Google Scholar : PubMed/NCBI
|
|
171
|
Chen J, Jiang Y, Shi H, Peng Y, Fan X and
Li C: The molecular mechanisms of copper metabolism and its roles
in human diseases. Pflugers Arch. 472:1415–1429. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
172
|
Ding C, Min J, Tan Y, Zheng L, Ma R, Zhao
R, Zhao H, Ding Q, Chen H and Huo D: Combating atherosclerosis with
chirality/phase dual-engineered nanozyme featuring
microenvironment-programmed senolytic and senomorphic actions. Adv
Mater. 36:e24013612024. View Article : Google Scholar : PubMed/NCBI
|
|
173
|
Lu Y, Fan X, Pan Q, He B and Pu Y: A
mitochondria-targeted anticancer copper dithiocarbamate amplifies
immunogenic cuproptosis and macrophage polarization. J Mater Chem
B. 12:2006–2014. 2024. View Article : Google Scholar : PubMed/NCBI
|