Introduction
Each year approximately 400,000 patients worldwide
are diagnosed with pancreatic cancer (PC). Because of its
aggressive nature, late diagnosis, rapid disease progression and
resistance to chemotherapy, PC is often fatal within 6 months
(1). The disappointing performance
of current treatments and the magnitude of the clinical problem
necessitate the development of new agents for PC.
A useful strategy in designing novel agents is the
chemical modification of known drugs in order to optimize their
pharmacological properties, primarily their efficacy (2–4).
Following this approach, we synthesized phospho-valproic acid (P-V;
MDC-1112), a novel valproic acid derivative. We have reported that
P-V is safe, based on genotoxicity and animal toxicity data, and
displays greater efficacy than valproic acid against PC in
xenograft models in mice (5). The
anticancer effect of P-V is mediated to a large extent through the
signal transducer and activator of transcription 3 (STAT3) pathway
(5). STAT3 plays a significant
role in the pathogenesis of PC, being associated with malignant
tumor initiation, transformation and progression (6–8).
Because it regulates several pathways important in tumorigenesis
(9), STAT3 is recognized as a
potential drug target for PC (10,11).
Although P-V is efficacious against PC, its
pharmacological profile limits the extent of its anticancer effect.
For this reason, we explored alternatives that would enhance P-V's
pharmacokinetic properties. Over the past decade, there has been an
increasing interest in using nanotechnology for cancer therapy, in
order to enhance drug efficacy and lower drug toxicity. Among
these, polymer-based drug delivery systems, including the
poly-L-lactic acid (PLLA) polymers, are being developed to improve
the diagnosis and treatment of various diseases, including cancer
(12). PLLA polymers are of
particular interest, since they are biodegradable, biocompatible
and FDA-approved (13). A major
breakthrough in the nanoparticle field is the use of hydrophilic
polymers, for example poly(ethylene glycol) (PEG), to efficiently
coat conventional nanoparticle surfaces (14). Amphiphilic copolymers with PEG,
such as PLLA-PEG, form a protective hydrophilic and flexible corona
around the polymeric core of the nanoparticles that repel plasma
proteins, avoid opsonization and exhibit prolonged circulation
(14).
In the present study, we assessed whether
formulating P-V in polymeric nanoparticles could improve the
pharmacokinetics of P-V and enhance its anticancer effect. We show
that P-V formulated in PLLA-PEG has potent anticancer activity
towards PC in various mouse models of PC. We also report on its
pharmacokinetic properties. Our results further support the
anticancer potential of P-V and support the use of PLLA-PEG for its
delivery.
Materials and methods
Materials
The copolymers PCL(10,000)-PEG(5,000),
PCL(5,000)-PEG(5,000) and PCL(3,600)-PEG(5,000) were obtained from
Polymer Source, Inc. (Dorval, QC, Canada). The copolymers
PS(2,000)-PEG(2,000) and PLLA(5,000)-PEG(2,000) were obtained from
PolySciTech (West Lafayette, IN, USA). Phospho-valproic acid (P-V;
MDC-1112) was a gift from Medicon Pharmaceuticals, Inc. (Stony
Brook, NY, USA). All general solvents and reagents were of hPLC
grade or the highest grade commercially available.
Preparation and characterization of
polymeric nanoparticles containing P-V
We used the single emulsification and solvent
evaporation method to prepare the polymeric nanoparticles from each
respective polymer (15). Briefly,
a dichloromethane solution of P-V and each polymer (ratio 15:100
w/w respectively) was transferred in an aqueous solution of sodium
cholate. The mixture was probe sonicated at 15W for 2 min and the
resulting oil/water emulsion was gently stirred at room temperature
in a fume hood until complete evaporation of the organic solvent.
The nanoparticles were purified by centrifugation and reconstituted
in the appropriate volume of water to achieve the desired drug
concentration.
The morphology of the nanoparticles was examined
using scanning electron microscopy. A drop of the nanoparticle
suspension was transferred onto a small metal plate. After drying,
the sample was coated with gold using an Edward 150B sputterer,
depositing 6 nm of gold, and transferred in the sample holder of a
LEO 1550 SFEG-SEM electron microscope using 2 kV accelerating
voltage and with a secondary-electron detector.
The size and ζ (zeta) potential of the nanoparticles
were determined using dynamic light scattering (DLS) and
micro-electrophoresis, respectively, 10 min after diluting the
samples in phosphate-buffered saline (PBS) and housing them at 25°C
using a ZetaPlus Brookhaven instrument (Brookhaven Instruments
Corp., Holtsville, NY, USA). Entrapped P-V was quantified with
high-performance-liquid-chromatography (HPLC) Waters Alliance 2695
equipped with a Waters 2998 photodiode array detector (220 nm)
(Waters Corp., Milford, MA, USA) and a Hypersil C18 column (150 ×
4.6 mm, particle size 3 µm; Thermo Fisher Scientific,
Waltham, MA, USA). We dissolved a small known amount of lyophilized
nanoparticle suspension into 1 ml of acetonitrile to determine the
drug loading and encapsulation efficiency for the formulation. The
mobile phase followed a gradient between buffer A (H2O,
acetonitrile, trifluoroacetic acid 94.9:5:0.1 v/v/v) and buffer B
(acetonitrile).
Cell viability assay
Human PC (Panc-1 and MIA PaCa-2) cell lines, which
carry the most common mutations for pancreatic cancer, KRAS and
TP53 mutations, as well as they present high (Panc-1) and very high
(MIA PaCa-2) constitutive STAT3 activation expression levels
(16,17), were purchased from the American
Type Culture Collection (ATCC; Manassas, VA, USA), which
characterizes them using cytogenetic analysis. We have not
authenticated these cell lines. These cells were grown at 37°C in
5% CO2 in Dulbecco's modified Eagle's medium (DMEM)
supplemented with 10% fetal calf serum (FCS), penicillin (50 U/ml)
and streptomycin (50 µg/ml). All the cell lines were
characterized for cell morphology and growth rate and passaged in
our laboratory less than 6 months after being received.
After treatment with P-V or P-V formulated in
PLLA-PEG for 24 or 48 h, cell viability was determined by the
reduction of 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium
bromide dye (MTT), following the manufacturer's protocol (Promega,
Madison, WI, USA) (4). Briefly,
MIA PaCa-2 and Panc-1 cells were plated in 96-well plates (5,000
cells/well), and the next day, cells were treated, in at least
triplicates, with varying concentrations of P-V or P-V formulated
in PLLA-PEG, and incubated for 24 or 48 h with the drugs, at 37°C
in 5% CO2. After 24 or 48 h of incubation, 10
µl/well 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium
bromide (MTT 1) (Sigma-Aldrich, St. Louis, MO, USA) was added and
incubated at 37°C for 4 h. MTT2 stop solution of 10% sodium dodecyl
sulfate (SDS) and 1M HCl at 100 µl/well was added as
solubilizing solution after incubation. Absorbance at 590 nm
(reference at 670 nm) using SpectraMax i3 plate reader (Molecular
Devices, Sunnyvale, CA, USA) was used to determine cell
viability.
Western blot analysis
Whole cell fractions were isolated from tumors as
previously described (3). Western
blots were performed as previously described (18,19).
Briefly, after treatment with the drugs, cells were scraped on ice,
washed with ice-cold PBS and lysed in RIPA lysis buffer
(Sigma-Aldrich). Protein concentration was determined using the
Bradford method (Bio-Rad Laboratories, hercules, CA, USA). Aliquots
of total fractions containing 25–40 µg protein were
separated by reducing 10–12.5% (w/v) polyacrylamide gel
electrophoresis and electroblotted to nitrocellulose membranes. The
membranes were probed overnight with antibodies against
p-STAT3Tyr705 (cat. no. 9145; Cell Signaling Technology,
Danvers, MA, USA), p-STAT3Ser727 (cat. no. sc-135649;
Santa Cruz Biotechnology, Santa Cruz, CA, USA). β-actin (cat. no.
A1978; Sigma-Aldrich) was used as the loading control. After
incubation, for 90 min at room temperature, in the presence of the
secondary antibody (HRP-conjugated; 1:5,000 dilution), the
conjugates were visualized by chemiluminescence.
Animal studies
All animal experiments were approved by our
Institutional Animal Care and Use Committee at Stony Brook
University.
Pancreatitis-accelerated carcinogenesis
in mice with activated Kras
In a first study, 2-month-old
p48-Cre;KrasG12D mice in C57Bl/6J background (a
gift from Dr Howard Crawford) were injected intraperitoneally with
saline or cerulein (50 µg/kg hourly, six times a day, 2 days
a week, for 3 weeks; n=7/group). Cerulein-injected mice were
divided in vehicle or P-V treatment groups. P-V (150 mg/kg) was
given 5 days a week by oral gavage, starting on the day of the
first cerulein injection. On day 21, mice were euthanized and the
pancreas was excised and fixed in formalin and processed for
morphological studies.
In a second study, 10-month-old
p48-Cre;KrasG12D mice were injected
intraperitoneally with saline or cerulein (250 µg/kg, once
per day for two consecutive days). Cerulein-injected mice were
divided in vehicle or PLLA-PEG P-V treatment groups (n=5–6/group).
P-V (20 mg/kg) formulated in PLLA(5k)-PEG(2k) was given
intravenously twice a week, starting on the day of the first
cerulein injection. P-V formulated in PLLA(5k)-PEG(2k) was
administered intravenously to utilize the potential advantages of
the enhanced permeability and retention effect observed in solid
tumors. On day 21, mice were euthanized and the pancreas was
excised and fixed in formalin or snap-frozen for further
analysis.
Nude mouse xenograft studies
Female BALB/c nude mice (5–6-weeks old; Charles
River Laboratories, Wilmington, MA, USA) were subcutaneously
injected with 1.5×106 MIA PaCa-2 cells in 100 µl
PBS into the right and left flanks. When tumors reached ~200
mm3, mice (n=7/group) were randomized into groups
receiving 2-hydroxypropyl-β-cyclodextrins (vehicle control), empty
PLLA(5k)-PEG(2k) (PLLA), P-V 20 mg/kg reconstituted in
2-hydroxypropyl-β-cyclodextrins (P-V) or P-V (20 mg/kg) formulated
in PLLA(5k)-PEG(2k) given intravenously twice a week for 21 days.
Tumor volume was calculated as [length × width × (length + width/2)
× 0.56], as previously described (5). Animals were sacrificed and tumors
were removed, weighed and stored for further analysis.
Histological examination
At necropsy, pancreas was fixed in 10%
phosphate-buffered formalin for 24 h. After dehydration the sample
was embedded in paraffin blocks, and four-micrometer-thick sections
were processed routinely, stained with H&E and scored by a
pathologist blinded to sample identity. The presence and extent of
pancreatic ductal metaplasia were scored based on the degree of
epithelial stratification and nuclear atypia according to
histopathology criteria, and expressed as the percent of lesion
over the total pancreas area, as we have previously shown (20).
Immunohistochemistry
Immunohistochemical staining for PCNA (sc-15402) and
p-STAT3Ser727 (sc-135649; both from Santa Cruz
Biotechnology), α-amylase (cat. no. 3796) and
p-STAT3Tyr705 (cat. no. 9145; both from Cell Signaling
Technology) was performed as previously described (20,21).
Briefly, paraffin-embedded sections (4 µm thick) were
deparaffinized, rehydrated and microwave-heated for 10 min in 0.01
mol/l citrate buffer (pH 6.0) for antigen retrieval, and 3%
H2O2 was applied to block endogenous
peroxidase activity. After 15 min of incubation with blocking
serum, the primary antibody or control IgG (dilution 1:50) was
applied and incubated overnight at 4°C. Slides were washed three
times with PBS for 5 min each time. The biotinylated secondary
antibody and the streptavidin-biotin complex (Invitrogen, Carlsbad,
CA, USA) were applied, each for 30 min at room temperature with an
interval washing. After rinsing with PBS, the slides were immersed
for 5 min in the coloring substrate 3,3′-diaminobenzidine (DAB;
Sigma-Aldrich), then rinsed with distilled water, counterstained
with hematoxylin, dehydrated and coverslipped.
Scoring
At least 5 fields per sample (at magnification,
×200) were scored independently by one investigator blinded to the
identity of the samples. For quantification of p-STAT3 and PCNA,
cells with a blue nucleus were considered unlabeled, while those
with a brown nucleus were considered labeled. We calculated the
percentage of positive cells by dividing the number of labeled
cells by the number of cells in each field and multiplying by 100.
Quantitation of amylase positive area was performed on independent,
singly DAB stained sections using the ImageJ Immunohistochemistry
Image Analysis software (NIH, Bethesda, MD, USA).
Statistical analysis
Results are expressed as mean ± SEM. Differences
between the groups were determined by one-factor analysis of
variance followed by the Tukey's test for multiple comparisons.
P<0.05 was statistically significant.
Results
P-V prevents pancreatitis-accelerated
carcinogenesis in mice with activated Kras
We have previously shown that P-V reduces the growth
of subcutaneous and orthotopic human PC xenografts in nude mice
(5). We now investigated whether
P-V could inhibit Kras-driven pancreatic carcinogenesis in the
setting of pancreatitis induced by cerulein. For this purpose, we
treated 2-month-old p48-Cre;KrasG12D mice with
cerulein (50 µg/kg; 6-hourly injections twice per week for 3
weeks) to induce pancreatitis. Concomitant with pancreatitis
induction and continuing for the following 3 weeks, mice were
treated with P-V 150 mg/kg/days five times a week or vehicle. In
p48-Cre;KrasG12D mice, cerulein treatment
produced a significant increase in ductal metaplasia lesions in
p48-Cre;KrasG12D mice, significantly replacing
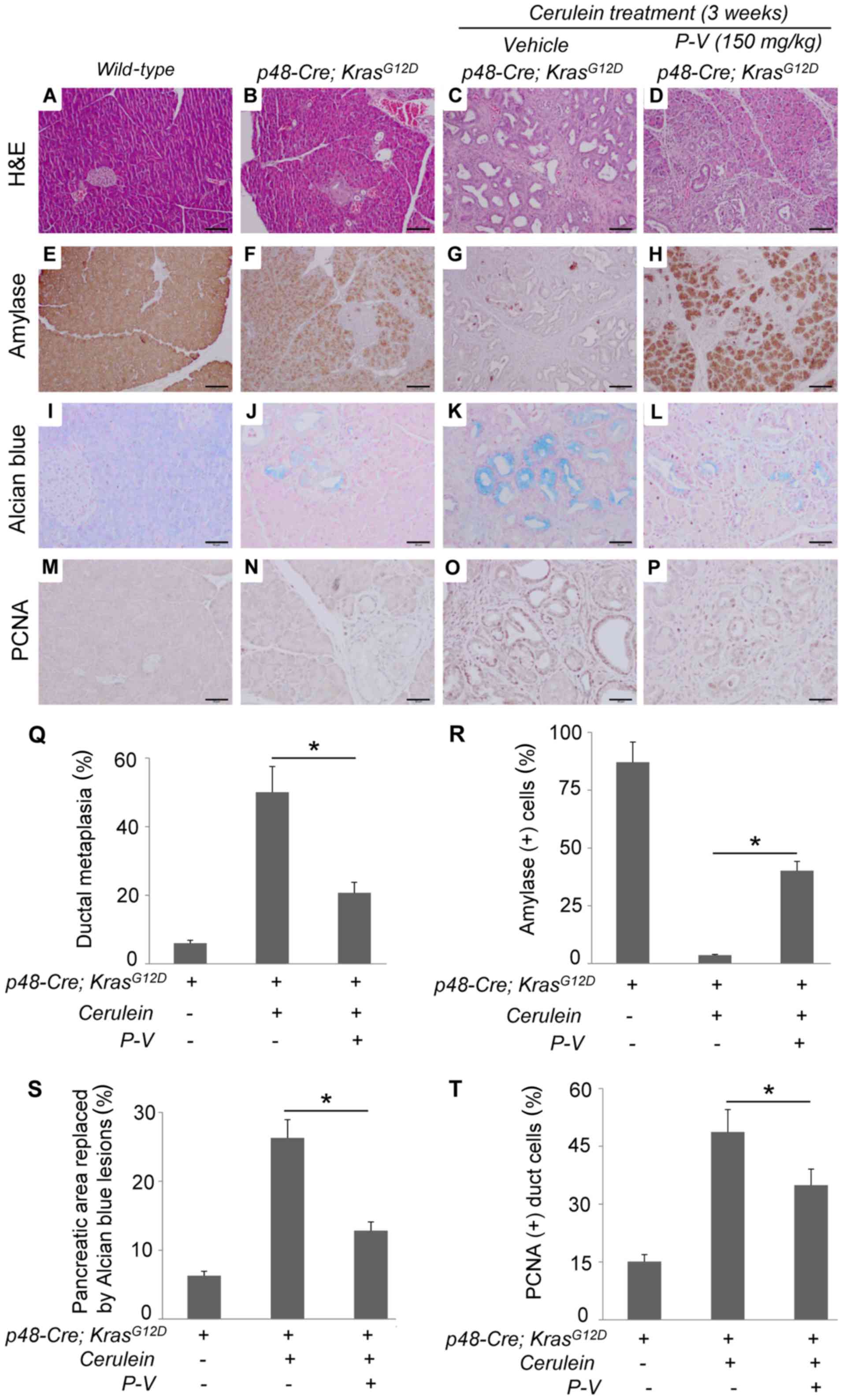
the exocrine compartment (Fig. 1).
This was accompanied by the minimal expression of amylase, an
acinar marker, and enhanced Alcian blue staining, which
characterizes PanINs (7). P-V 150
mg/kg/day prevented cerulein-induced acinar-to-ductal metaplasia by
60% (P<0.05), an effect associated with increased amylase
expression, decreased Alcian blue staining areas, and reduced
cerulein-stimulated ductal cell proliferation (P<0.01; Fig. 1). Importantly, P-V was well
tolerated by the mice, showing no body weight loss throughout the
treatment.
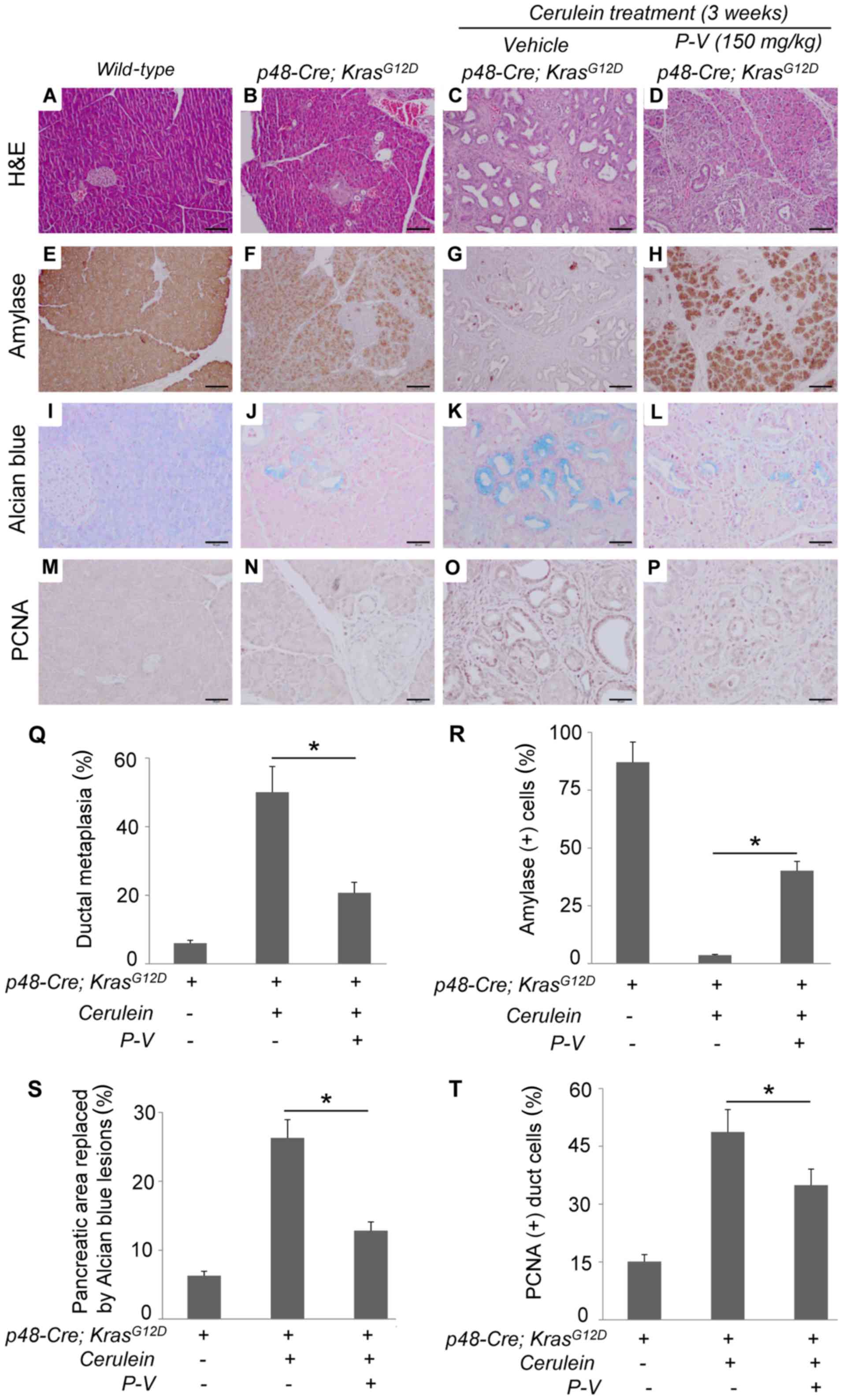 | Figure 1P-V protects against
pancreatitis-accelerated carcinogenesis in mice with activated
Kras. Two-month-old mice with activated Kras
(p48-Cre;LSL-KrasG12D) were injected with PBS (B,
F, J and N), cerulein (C, G, K and O) or cerulein + P-V (D, H, L
and P) and sacrificed 3 weeks after treatment. Wild-type mice were
used as controls (A, E, I and M). The following stains were
performed: (A–D) H&E; representative photographs are shown at
×10 magnification. (E–H) Amylase; representative photographs are
shown at ×10 magnification. (I–L) Alcian blue stain; representative
photographs are shown at ×20 magnification. (M–P) PCNA;
representative photographs are shown at ×20 magnification. (Q) The
percent of ductal metaplasia per total pancreas was quantified and
expressed as the mean ± SEM; *P<0.01. (R) Amylase
staining images were quantified and results are expressed as the
percentage of amylase positive staining per field;
*P<0.01. (S) Alcian blue positive staining in total
pancreas area was quantified and results expressed as the
percentage of pancreatic area replaced by alcian blue lesions;
*P<0.01. (T) PCNA staining images were quantified and
results expressed as the percentage of PCNA positive pancreatic
duct cells; *P<0.01. Scale bars, 100 µm for
H&E and amylase; 50 µm for Alcian blue and PCNA. |
P-V formulated in PLLA(5k)-PEG(2k)
nanoparticles increases circulating drug levels
Since the treatment of PC remains challenging, the
task of improving therapies relies on the development of additional
technologies that overcome the low accessibility of drugs to the
pancreas. P-V is rapidly hydrolyzed by carboxyesterases when
administered intravenously. We used
(2-hydroxypropyl)-β-cyclodextrin to solubilize the hydrophobic P-V
in water and after i.v. injection, the drug was not detectable even
5 min post-injection. To overcome this limitation and improve the
pharmacokinetics of P-V, we incorporated the drug in polymeric
nanoparticles of various polymers and determined its
pharmacokinetics. A panel of five different polymers composed of
poly-caprolactone (PCL) at molecular weights of 3.6, 5 and 10 kDa,
poly-styrene (PS) of 2 kDa or poly-L-lactic acid of 5 kDa, all
copolymerized with polyethylene glycol of 2 or 5 kDa, were tested
for improving the P-V pharmacokinetic profile (Table I). All formulations were prepared
by the emulsion-solvent evaporation method, and their hydrodynamic
diameter, polydispersity index and zeta potential were determined.
Table I summarizes the
results.
 | Table ICharacterization of polymeric
nanoparticles. |
Table I
Characterization of polymeric
nanoparticles.
| Formulation | Size (nm) | PDI | Z-potential
(mV) | P-V blood levels
(µM)
|
|---|
| 5 min | 1 h |
|---|
|
PCL(5k)-PEG(5k) | 81.3 | 0.181 | −6.32 | 0.6 | 0.4 |
|
PCL(3.6k)-PEG(5k) | 83 | 0.821 | 0 | 0.0 | 0.0 |
| PS(2k)-PEG(2k) | N/A | 1 | N/A | 2.3 | 0.5 |
|
PCL(10k)-PEG(5k) | 115.2 | 0.104 | −6.22 | 0.9 | 0.0 |
|
PLLA(5k)-PEG(2k) | 81.3 | 0.181 | −14.7 | 41.0 | 20.0 |
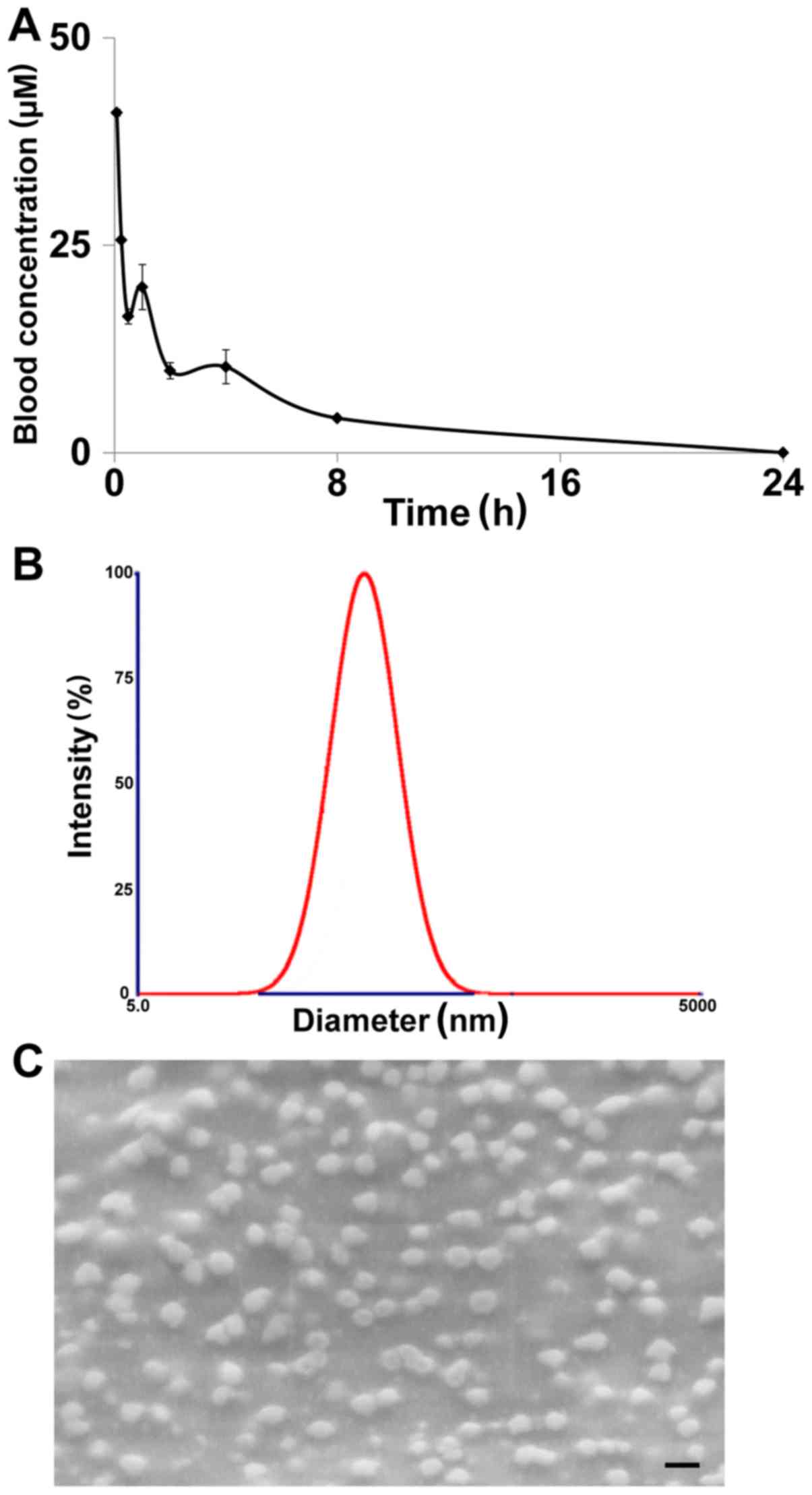
PLLA(5k)-PEG(2k) nanoparticles generated µM
blood levels of P-V (41 and 20 µM, for 5 min and 1 h,
respectively). The 24-h pharmacokinetic profile of the
PLLA(5k)-PEG(2k) nanoparticles demonstrated a prolonged and
sustained presence of the drug, which was detectable up to 8 h
after the injection (Fig. 2A). The
drug's AUC0–24 h was determined at 117.5 µM/h,
with Tmax at the first time-point of 5 min and
Cmax of 41 µM.
The basic characteristics of the PLLA(5k)-PEG(2k)
nanoparticles were: a size of 81.3 nm (Fig. 2B); a polydispersity index of 0.181
and a zeta potential of −14.7 mV. In addition, the nanoparticles
were spherical and homogeneous in size as observed under the
scanning electron microscope (Fig.
2C). The drug loading for these nanoparticles was 5% and the
encapsulation efficiency was 13.4%.
In contrast, the other tested formulations led to
significantly less P-V levels in the blood at 5 min and 1 h post
intravenous injection, without exceeding the concentration of 3
µM in any case (Table I).
To note, we were unable to determine the size and zeta potential
for the formulation prepared with PCL(3.6k)-PEG(5k) and
PS(2k)-PEG(2k). It is conceivable that these polymers resulted in
the formation of micelles that their respective size was below the
detection limit of our equipment.
Overall, PLLA(5k)-PEG(2k) nanoparticles provided a
significantly improved pharmacokinetic profile for P-V compared to
the other tested formulations. In addition, PLLA-PEG co-polymers
are considered biocompatible and biodegradable, and appear safe
based on previous toxicity studies (15). Thus, we chose PLLA(5k)-PEG(2k)
nanoparticles as the formulation of choice for P-V and we used this
formulation in the studies described below.
P-V formulated in PLLA(5k)-PEG(2k)
nanoparticles reduces PC growth in vitro and in vivo
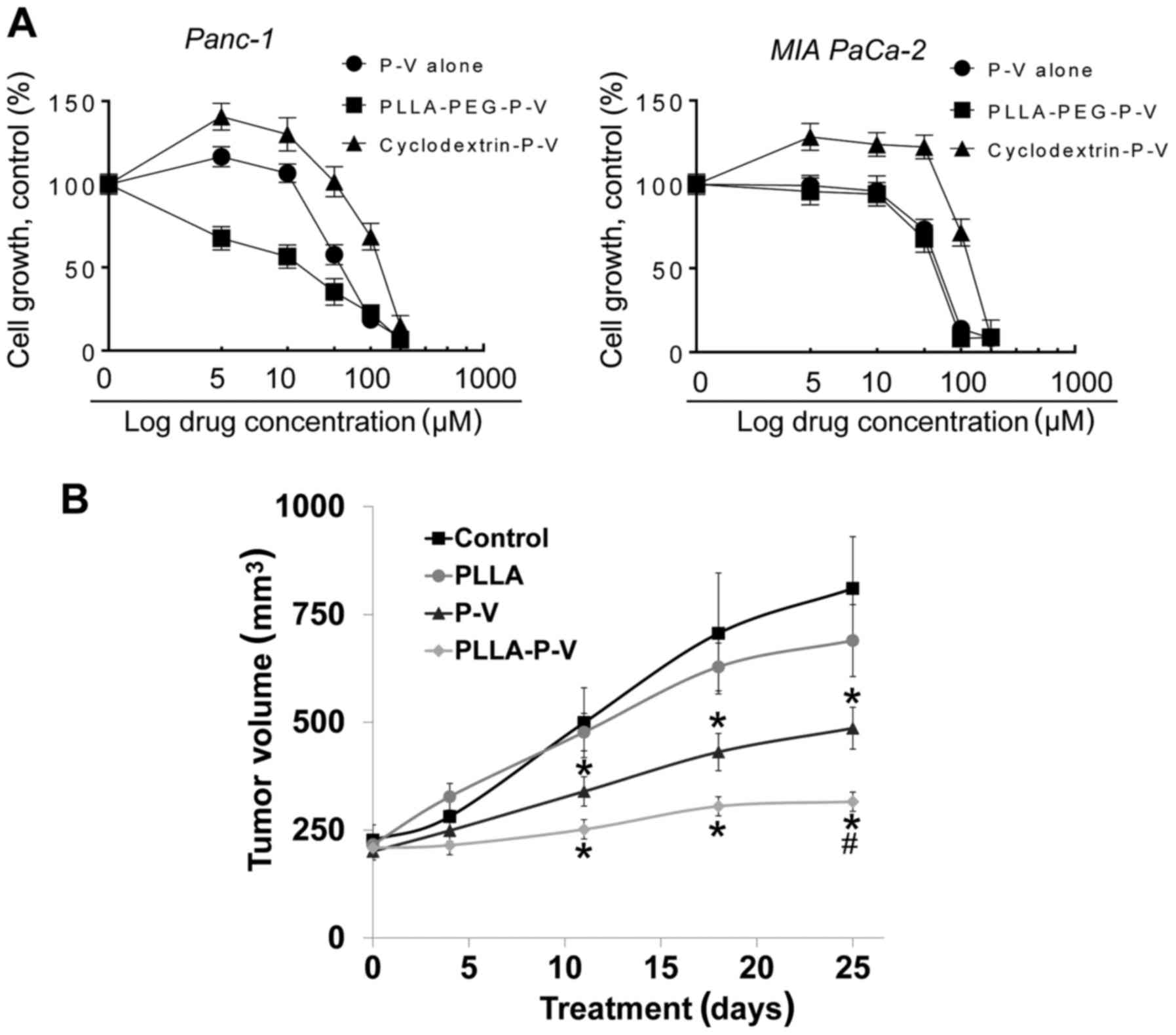
Initially, we evaluated the cytotoxicity of P-V
incorporated in PLLA(5k)-PEG(2k) (PLLA-P-V) in two human PC cell
lines, MIA PaCa-2 and Panc-1 and compared the effect of P-V alone.
The values of 24 h IC50 were as follows: MIA PaCa-2
cells: P-V=73.2 µM and PLLA-P-V=67.5 µM; Panc-1
cells: P-V=57.7 µM and PLLA-P-V=35.3 µM (Fig. 3A). On the other hand, P-V
formulated in cyclodextrins led to higher IC50 values in
both cell lines. PLLA(5k)-PEG(2k) by itself had no effect on cell
growth (data not shown).
We then investigated the effect of PLLA-P-V in MIA
PaCa-2 subcutaneous xenografts in nude mice and compared it to that
of P-V. When compared to Panc-1 xenografts, MIA PaCa-2 xenografts
present some advantages as they are better grafted and they grow at
a higher speed (22–24), better mimicking the aggressiveness
of PC. Thus, we explored the efficacy of PLLA-P-V in MIA PaCa-2
xenografts. When tumors reached a volume ~200 mm3, mice
were randomly divided into four groups: vehicle control, empty
PLLA-PEG, P-V dissolved in 2-hydroxypropyl-β-cyclodextrins (P-V)
and PLLA-P-V-treated groups. Mice in the PLLA-P-V group received
P-V (20 mg/kg) formulated in PLLA(5k)-PEG(2k) given intravenously
twice a week for 25 days. When compared to controls, the inhibitory
effect of PLLA-P-V became statistically significant starting 11
days after the start of the treatment (P<0.01). Compared to
vehicle-treated controls, PLLA-P-V reduced tumor growth by 81%
(P<0.01), whereas P-V dissolved in
2-hydroxypropyl-β-cyclodextrins, given at an equi-dose, reduced it
by 51%, indicating a 1.58-fold reduction in the rate of tumor
growth for PLLA-P-V when compared to plain P-V (Fig. 3B). Compared to controls, both
effects are statistically significant (P<0.01), as is the
difference between the effects of PLLA-P-V and P-V groups
(P<0.05). PLLA-P-V was well tolerated by the mice, which showed
no weight loss or other signs of toxicity. Throughout the study the
body weight of mice receiving PLLA-P-V, was comparable to that of
the control group.
P-V formulated in PLLA(5k)-PEG(2k)
nanoparticles reduces pancreatic ductal metaplasia incidence
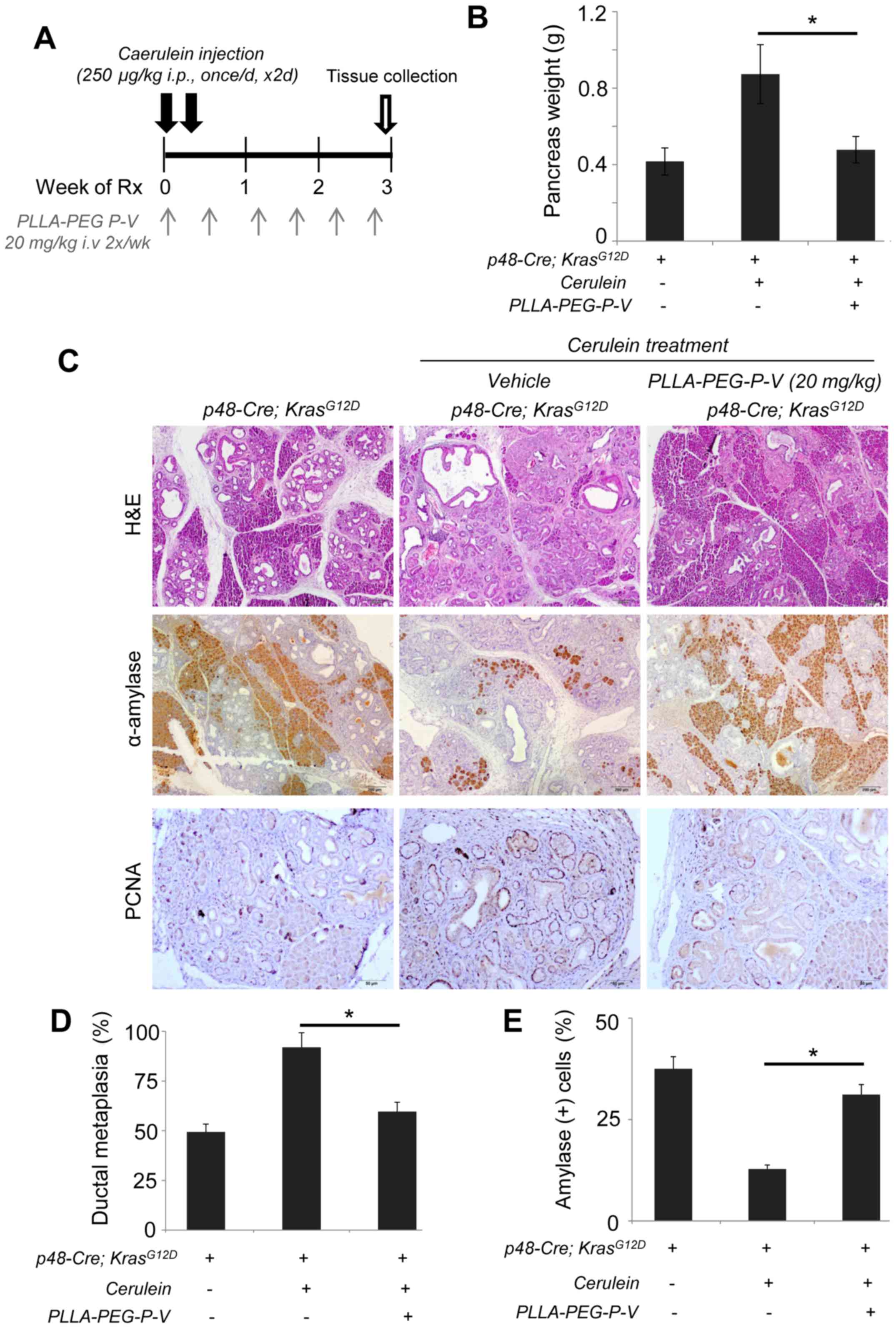
To gain additional information on P-V formulated in
PLLA(5k)-PEG(2k) as a therapeutic agent for PC, we evaluated the
efficacy of PLLA-P-V in Kras-driven pancreatic carcinogenesis in
the setting of pancreatitis (Fig.
4A). Ten-month-old p48-Cre;KrasG12D mice
already presented with 100% penetrance of PanIN lesions, with mice
replaced their exocrine compartment by 50%. Treatment with cerulein
(250 µg/kg), once a day for 2 consecutive days, led to an
acceleration of ductal metaplasia incidence in the 10-month-old
p48-Cre;KrasG12D mice. This effect was
accompanied by enhanced PCNA staining and minimal expression of
amylase. PLLA-P-V treatment at 20 mg/kg twice a week for 3 weeks
reduced ductal metaplasia incidence by 87% (P<0.05) in
transgenic mice, compared to cerulein-treated controls (Fig. 4B). This effect was associated with
reduced ductal cell proliferation and increased amylase expression
(P<0.01; Fig. 4C–E).
P-V formulated in PLLA(5k)-PEG(2k)
nanoparticles inhibits STAT3 signaling in PC
In PC cells in culture and xenografts, P-V inhibits
STAT3 activation (5) a signaling
molecule overexpressed in PC and considered a promising therapeutic
target (11). In the present
study, we tested whether P-V could inhibit STAT3 activation during
Kras-driven metaplasia induced by pancreatitis, evaluating by
immunohistochemistry the activation of STAT3 by phosphorylation at
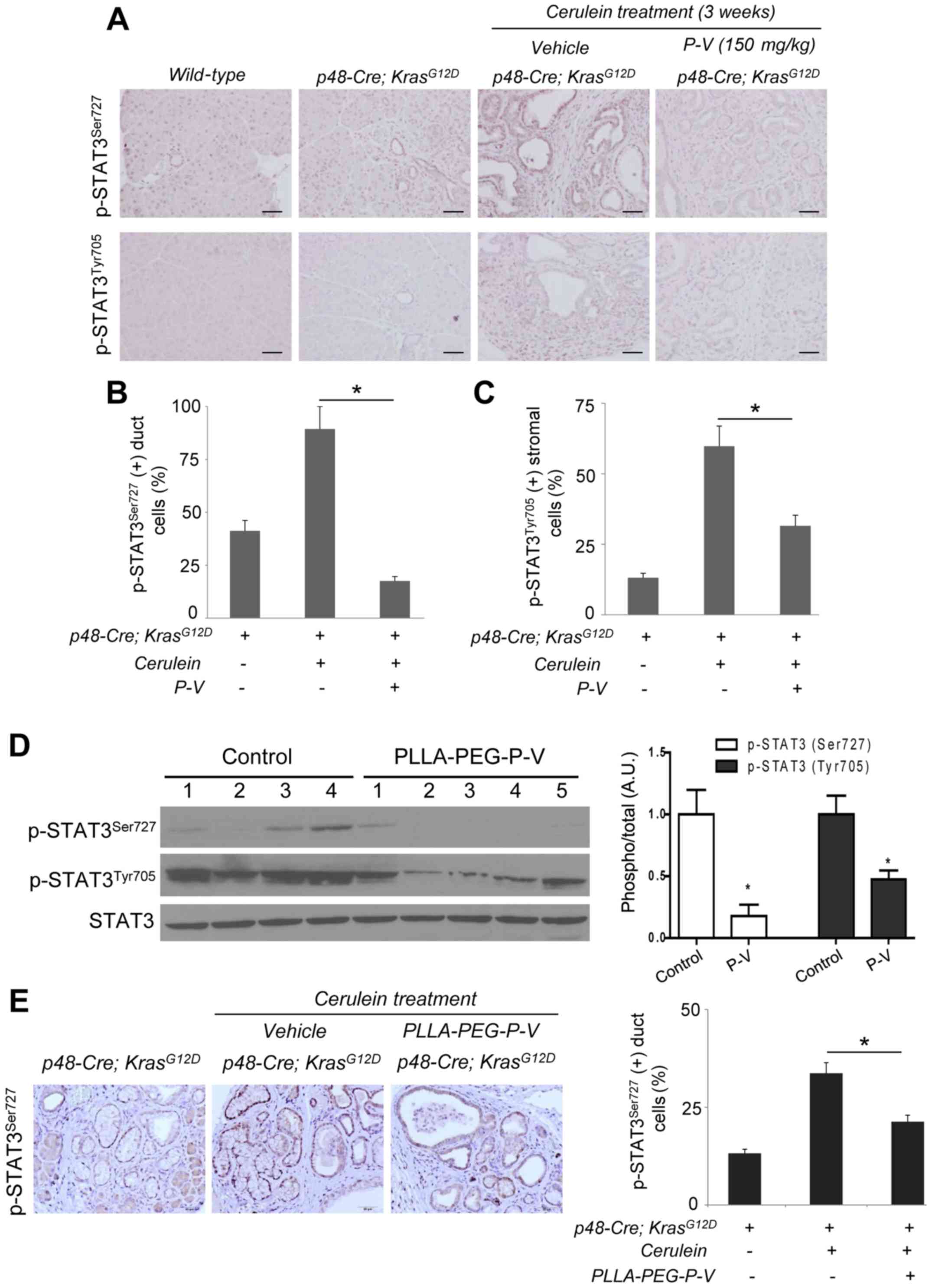
two critical sites: Ser727 and Tyr705 (Fig. 5A–C). Cerulein-treated mice had
significantly more p-STAT3Ser727 positive duct cells
than Kras control mice, while P-V completely blocked it (Fig. 5B). Moreover, there were
significantly more p-STAT3Tyr705 positive stromal cells
after cerulein treatment; P-V-treatment decreased this by half
(P<0.01; Fig. 5C).
We next evaluated whether P-V formulated in
PLLA(5k)-PEG(2k) also inhibited STAT3 phosphorylation. As shown in
Fig. 5D, PLLA-P-V reduced
p-STAT3Ser727 and p-STAT3Tyr705 levels in MIA
PaCa-2 xenografts, compared to control. A reduction in
STAT3Ser727 phosphorylation levels was also observed by
immunohistochemistry. While cerulein-treated mice had significantly
more p-STAT3Ser727 positive duct cells than Kras control
mice, treatment with PLLA-P-V significantly (P<0.05) reduced
p-STAT3Ser727 levels by 60.4% (Fig. 5E).
Discussion
PC is an almost universally fatal disease, with
unsatisfactory treatment options (25). Clearly, this unmet medical need
requires developing new agents and novel strategies for PC
treatment. We have previously shown that the novel compound P-V is
a strong inhibitor of PC in xenograft models in mice (5). In the present study, we have extended
our work and show that P-V is also effective in transgenic
Kras-driven models of PC and that the formulation of P-V in
PLLA(5k)-PEG(2k) nanoparticles, which improves the P-V
pharmacological profile, results in an attractive alternative for
future drug design. The anticancer efficacy of P-V and its apparent
lack of toxicity make it a promising candidate drug for the
treatment of PC.
Cancer-associated inflammation is a molecular key
feature in PC. In response to acute pancreatitis induced by
cerulein, acini transiently de-differentiate into duct-like
structures that express embryonic factors characteristic of
pancreatic embryonic progenitors. However, the presence of mutant
Kras compromises the ability of acinar cells to regenerate
following acute pancreatitis and locks damaged cells in a
persistently de-differentiated, ductal state that can rapidly give
rise to PanINs (26). This model
of pancreatitis-accelerated carcinogenesis in Kras-mutant mice is
an established model to study the potential chemopreventive effect
of novel agents. As shown by our findings using this model, P-V
reduces the incidence of PC by 60%. This effect is similar to the
effect we observed for P-V in human xenograft models (5).
To enhance the P-V bioavailability and efficacy, we
tested various potential copolymers to formulate nanoparticles.
PLLA(5k)-PEG(2k) nanoparticles proved to be ideal for P-V, leading
to a significantly improved pharmacokinetic profile with increased
levels of intact drug in the blood, when compared to the other
tested copolymers and to the drug alone. PLLA(5k)-PEG(2k)
nanoparticles have been successfully used to entrap anticancer
drugs, achieving improved water solubility, bioavailability and
antitumor efficacy via the enhanced permeability and retention
effect (27). For instance,
PLLA(5k)-PEG(2k) co-polymers loaded with doxorubicin and
paclitaxel, accumulated in tumors, released the drug slowly
(28), which resulted in tumor
regression in mice (29). P-V
formulated in PLLA(5k)-PEG(2k) exhibited a protection from
esterases, leading to longer circulation time of P-V. This can be
explained by the steric hindrance produced by the hydrophilic
corona formed by the flexible PEG chains being exposed out and away
from the solid hydrophobic polymeric core. It is of interest that
the other tested polymers, though copolymers containing PEG, were
unable to produce such a favorable result for P-V. We suspect that
PLLA created the appropriate hydrophobic environment in the solid
polymeric core for P-V to remain entrapped. Furthermore, based on
our findings in two different PC mouse models, in which the
efficacy was ≥80%, formulating P-V in PLLA(5k)-PEG(2k)
nanoparticles appears an ideal approach to protect P-V and enhance
its efficacy.
STAT3 plays an essential role in the initiation and
progression of PC (7,8) and in the induction of resistance to
apoptosis (11). STAT3 has been
shown to cooperate with other inflammatory-related transcription
factors, such as NFATc1, in pancreatic development (30), and STAT3 activation by IL-6
transignaling promotes progression of PanIN and development of PC
(8). Indeed, STAT3 may serve as a
mediator of inflammation-associated processes, such as
pancreatitis-driven PanIN development. P-V alone and formulated in
PLLA(5k)-PEG(2k) nanoparticles inhibited STAT3 phosphorylation at
the Ser727 and Tyr705 residues in both the xenografts as well as in
the Kras/pancreatitis-associated PC models.
In summary, the novel compound P-V is an effective
anticancer agent in preclinical models of PC, acting primarily
through STAT3 inhibition. Furthermore, its formulation in
PLLA(5k)-PEG(2k) nanoparticles increases its circulation time and
enhances its efficacy. Our data further indicate P-V as a promising
candidate drug for PC and suggest its formulation in
PLLA(5k)-PEG(2k) nanoparticles for its administration.
Acknowledgments
The present study was funded in part by grants from
NIHCA175699, NIHCA181727 to G.G.M and the Knapp Foundation to
B.R.
References
|
1
|
Siegel RL, Miller KD and Jemal A V1:
Cancer statistics, 2016. CA Cancer J Clin. 66:7–30. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Huang L, Mackenzie GG, Sun Y, Ouyang N,
Xie G, Vrankova K, Komninou D and Rigas B: Chemotherapeutic
properties of phospho-nonsteroidal anti-inflammatory drugs, a new
class of anticancer compounds. Cancer Res. 71:7617–7627. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Mackenzie GG, Bartels LE, Xie G,
Papayannis I, Alston N, Vrankova K, Ouyang N and Rigas B: A novel
Ras inhibitor (MDC-1016) reduces human pancreatic tumor growth in
mice. Neoplasia. 15:1184–1195. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Mackenzie GG, Sun Y, Huang L, Xie G,
Ouyang N, Gupta RC, Johnson F, Komninou D, Kopelovich L and Rigas
B: Phospho-sulindac (OxT-328), a novel sulindac derivative, is safe
and effective in colon cancer prevention in mice. Gastroenterology.
139:1320–1332. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mackenzie GG, Huang L, Alston N, Ouyang N,
Vrankova K, Mattheolabakis G, Constantinides PP and Rigas B:
Targeting mitochondrial STAT3 with the novel phospho-valproic acid
(MDC-1112) inhibits pancreatic cancer growth in mice. PLoS One.
8:e615322013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Corcoran RB, Contino G, Deshpande V,
Tzatsos A, Conrad C, Benes CH, Levy DE, Settleman J, Engelman JA
and Bardeesy N: STAT3 plays a critical role in KRAS-induced
pancreatic tumorigenesis. Cancer Res. 71:5020–5029. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Fukuda A, Wang SC, Morris JP IV, Folias
AE, Liou A, Kim GE, Akira S, Boucher KM, Firpo MA, Mulvihill SJ, et
al: Stat3 and MMP7 contribute to pancreatic ductal adenocarcinoma
initiation and progression. Cancer Cell. 19:441–455. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Lesina M, Kurkowski MU, Ludes K, Rose-John
S, Treiber M, Klöppel G, Yoshimura A, Reindl W, Sipos B, Akira S,
et al: Stat3/Socs3 activation by IL-6 transsignaling promotes
progression of pancreatic intraepithelial neoplasia and development
of pancreatic cancer. Cancer Cell. 19:456–469. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Scholz A, Heinze S, Detjen KM, Peters M,
Welzel M, Hauff P, Schirner M, Wiedenmann B and Rosewicz S:
Activated signal transducer and activator of transcription 3
(STAT3) supports the malignant phenotype of human pancreatic
cancer. Gastroenterology. 125:891–905. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Buettner R, Mora LB and Jove R: Activated
STAT signaling in human tumors provides novel molecular targets for
therapeutic intervention. Clin Cancer Res. 8:945–954.
2002.PubMed/NCBI
|
|
11
|
Sahu RP and Srivastava SK: The role of
STAT-3 in the induction of apoptosis in pancreatic cancer cells by
benzyl isothiocyanate. J Natl Cancer Inst. 101:176–193. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Mattheolabakis G, Rigas B and
Constantinides PP: Nanodelivery strategies in cancer chemotherapy:
Biological rationale and pharmaceutical perspectives. Nanomedicine
(Lond). 7:1577–1590. 2012. View Article : Google Scholar
|
|
13
|
Soppimath KS, Aminabhavi TM, Kulkarni AR
and Rudzinski WE: Biodegradable polymeric nanoparticles as drug
delivery devices. J Control Release. 70:1–20. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Brigger I, Dubernet C and Couvreur P:
Nanoparticles in cancer therapy and diagnosis. Adv Drug Deliv Rev.
54:631–651. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Mattheolabakis G, Taoufik E, Haralambous
S, Roberts ML and Avgoustakis K: In vivo investigation of tolerance
and antitumor activity of cisplatin-loaded PLGA-mPEG nanoparticles.
Eur J Pharm Biopharm. 71:190–195. 2009. View Article : Google Scholar
|
|
16
|
Wei D, Le X, Zheng L, Wang L, Frey JA, Gao
AC, Peng Z, Huang S, Xiong HQ, Abbruzzese JL, et al: Stat3
activation regulates the expression of vascular endothelial growth
factor and human pancreatic cancer angiogenesis and metastasis.
Oncogene. 22:319–329. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Deer EL, González-Hernández J, Coursen JD,
Shea JE, Ngatia J, Scaife CL, Firpo MA and Mulvihill SJ: Phenotype
and genotype of pancreatic cancer cell lines. Pancreas. 39:425–435.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Sun Y and Rigas B: The thioredoxin system
mediates redox-induced cell death in human colon cancer cells:
Implications for the mechanism of action of anticancer agents.
Cancer Res. 68:8269–8277. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Mackenzie GG, Queisser N, Wolfson ML,
Fraga CG, Adamo AM and Oteiza PI: Curcumin induces cell-arrest and
apoptosis in association with the inhibition of constitutively
active NF-kappaB and STAT3 pathways in Hodgkin's lymphoma cells.
Int J Cancer. 123:56–65. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Mattheolabakis G, Papayannis I, Yang J,
Vaeth BM, Wang R, Bandovic J, Ouyang N, Rigas B and Mackenzie GG:
Phospho-aspirin (MDC-22) prevents pancreatic carcinogenesis in
mice. Cancer Prev Res. 9:624–634. 2016. View Article : Google Scholar
|
|
21
|
Mackenzie GG, Ouyang N, Xie G, Vrankova K,
Huang L, Sun Y, Komninou D, Kopelovich L and Rigas B:
Phospho-sulindac (OxT-328) combined with difluoromethylornithine
prevents colon cancer in mice. Cancer Prev Res (Phila).
4:1052–1060. 2011. View Article : Google Scholar
|
|
22
|
Fogar P, Greco E, Basso D, Habeler W,
Navaglia F, Zambon CF, Tormen D, Gallo N, Cecchetto A, Plebani M,
et al: Suicide gene therapy with HSV-TK in pancreatic cancer has no
effect in vivo in a mouse model. Eur J Surg Oncol. 29:721–730.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Freeman JW, Mattingly CA and Strodel WE:
Increased tumorigenicity in the human pancreatic cell line MIA
PaCa-2 is associated with an aberrant regulation of an IGF-1
autocrine loop and lack of expression of the TGF-beta type RII
receptor. J Cell Physiol. 165:155–163. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Mattheolabakis G, Papayannis I, Yang J,
Vaeth BM, Wang R, Bandovic J, Ouyang N, Rigas B and Mackenzie GG:
Phospho-aspirin (MDC-22) prevents pancreatic carcinogenesis in
mice. Cancer Prev Res (Phila). 9:624–634. 2016. View Article : Google Scholar
|
|
25
|
Li J and Saif MW: Advancements in the
management of pancreatic cancer. JOP. 10:109–117. 2009.PubMed/NCBI
|
|
26
|
Morris JP IV, Wang SC and Hebrok M: KRAS,
Hedgehog, Wnt and the twisted developmental biology of pancreatic
ductal adenocarcinoma. Nat Rev Cancer. 10:683–695. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Zhan C, Gu B, Xie C, Li J, Liu Y and Lu W:
Cyclic RGD conjugated poly(ethylene glycol)-co-poly(lactic acid)
micelle enhances paclitaxel anti-glioblastoma effect. J Control
Release. 143:136–142. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Ahmed F, Pakunlu RI, Srinivas G, Brannan
A, Bates F, Klein ML, Minko T and Discher DE: Shrinkage of a
rapidly growing tumor by drug-loaded polymersomes: pH-triggered
release through copolymer degradation. Mol Pharm. 3:340–350. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Kim SC, Kim DW, Shim YH, Bang JS, Oh HS,
Wan Kim S and Seo MH: In vivo evaluation of polymeric micellar
paclitaxel formulation: toxicity and efficacy. J Control Release.
72:191–202. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Baumgart S, Chen NM, Siveke JT, König A,
Zhang JS, Singh SK, Wolf E, Bartkuhn M, Esposito I, Heßmann E, et
al: Inflammation-induced NFATc1-STAT3 transcription complex
promotes pancreatic cancer initiation by KrasG12D.
Cancer Discov. 4:688–701. 2014. View Article : Google Scholar : PubMed/NCBI
|