Neoadjuvant chemoradiotherapy (nCRT) followed by
radical surgery has been the standard treatment modality for
patients with locally advanced rectal cancer (LARC); this treatment
modality has improved the local control rate and alleviated the
radiation-induced toxicity in patients with rectal cancer (1). However, the major challenges for
enhancing the efficacy of radiotherapy (RT) are the development of
radioresistance in the tumor and the radiation-induced
complications and toxicities. Therefore, the efficacy of RT in
rectal cancer may be improved with the identification of
radioresistance markers and predictive biomarkers of
radiosensitivity, as well as the elucidation of the mechanisms
underlying radioresistance and radiation-induced toxicity and
complications.
Radiosensitivity and radiation-induced toxicity are
predicted based on the clinical factors and irradiation doses;
however, these parameters have low predictive accuracy (2-4).
Therefore, there is a need to identify biomarkers that can predict
the response to RT in patients with LARC to optimize the radiation
doses, minimize the radiation-induced complications and select the
optimal treatment strategy. Previous studies have demonstrated that
the expression patterns of non-coding RNAs (ncRNAs) can predict the
response to RT in patients with rectal cancer (5-7).
ncRNAs can be classified as short ncRNAs and long ncRNAs (lncRNAs).
Short ncRNAs are further classified into several classes, including
piwi-associated RNAs, short-interfering RNAs and microRNAs
(miRNAs/miRs). miRNAs are short (18-25 nucleotides in length)
highly conserved RNAs that regulate gene expression at the
post-transcriptional level through the degradation and/or
translational repression of their mRNA targets (8). Currently, various miRNAs are reported
to function as master regulators of several biological processes,
including cell proliferation, apoptosis and cancer development and
progression (9). Several miRNAs
are present in the extracellular microenvironment (10,11).
Some miRNAs are stable in biological fluids (12,13).
The stability of circulating miRNAs can be attributed to their
ability to form complexes with proteins in fluids, which prevents
RNase-mediated miRNA degradation (14). Therefore, miRNAs are considered
promising biomarkers and clinical therapeutic targets for rectal
cancer.
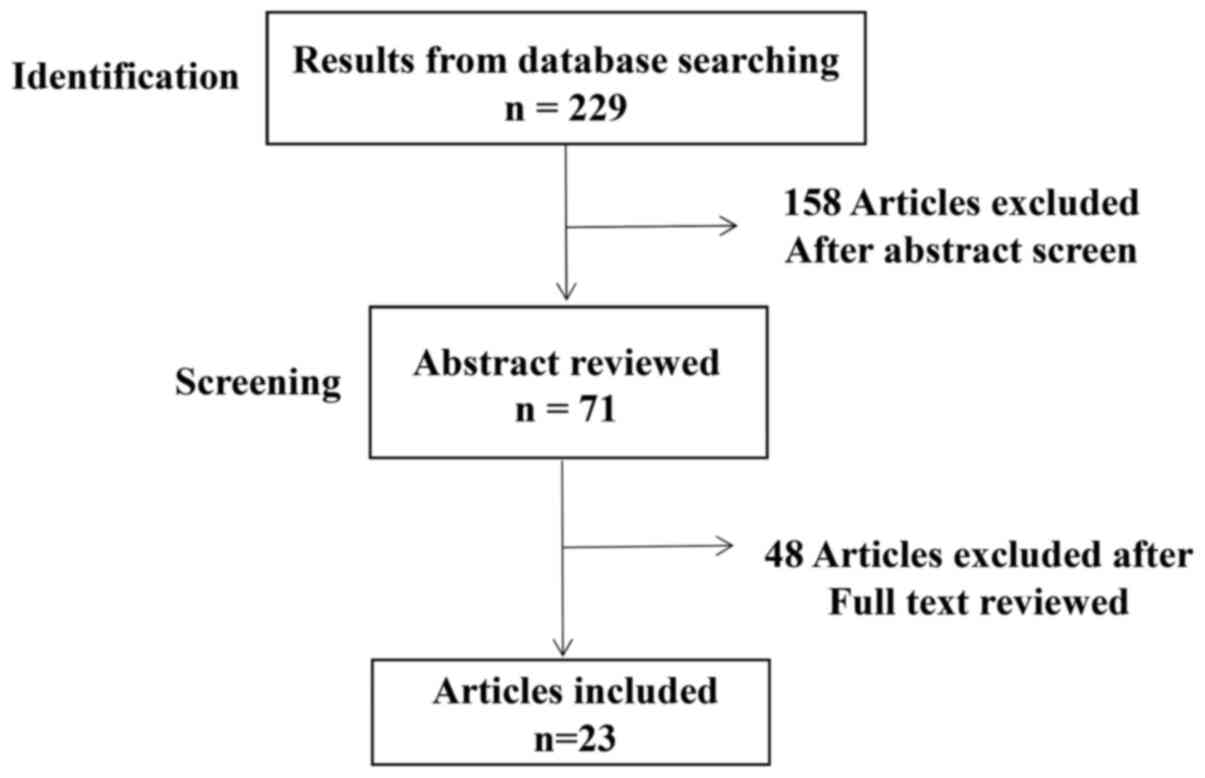
Studies on the ability of ncRNAs to predict the
response of rectal cancer to RT were searched in the following
databases: Medline through Pubmed (https://pubmed.ncbi.nlm.nih.gov/) and Cochrane
database (https://www.cochranelibrary.com/) of systemic reviews
and reference lists from the retrieved papers (January 2008-October
2020). The search terms and groups of words used were: 'Rectal
cancer', 'neoadjuvant radiotherapy', 'miRNAs in rectal cancers',
'lncRNAs' or 'non-coding RNA in rectal cancer'. The type of
articles included in the present review were systemic reviews,
meta-analyses, randomised controlled trials and clinical trials.
Published conference extracts or non-peer reviewed manuscripts were
excluded. A total of 229 related articles were identified and 23
studies were included in the final review (Fig. 1). Due to the small number of
studies yielded by the search criteria, and the heterogeneity of
outcomes, a narrative review has been performed.
Globally, colorectal cancer (CRC) is the third most
common cancer and the second most common cause of cancer-associated
mortality (23). Rectal cancer
accounts for ~30% of all CRC cases (24). Among the rectal cancer cases, ~40%
cases are LARC, which is associated with poor clinical outcomes
(25). In the United States of
America (USA), 147,950 new cases of CRC were estimated to be
diagnosed in 2020, including 104,610 cases of colon cancer and
43,340 cases of rectal cancer, with high mortality expected among
CRC cases (24).
Age and environmental and lifestyle factors
contribute to the development of CRC; hence, several studies have
demonstrated that dietary habits, sedentary lifestyles and the
increased prevalence of obesity have increased the risk of
developing CRC among younger populations (<40 years old)
compared with older populations (>40 years old) (26,27).
Previous studies have suggested that occupational exposure to
toxins may increase the risks of developing CRC (28-30).
Long-term exposure to industrial fumes and wood or metal dust and
the consumption of deep-fried and barbecued foods in young
adulthood have been markedly associated with rectal cancer
(31). Compared with individuals
residing in urban areas and involved in non-farming occupations,
individuals residing in rural areas where pesticides are not used
and involved in farming occupations were associated with a lower
risk of developing rectal cancer (32,33).
Consistently, the history of exposure to industrial toxins,
unhealthy dietary habits and sedentary lifestyle have been
positively associated with an increased incidence of rectal cancer
in young patients (26,34).
Recent advances in cancer therapeutics have
increased the therapeutic efficacy in patients with rectal cancer.
Surgery is the only curative therapy for patients with rectal
cancer, especially for those with rectal adenocarcinoma (35,36).
The development of combined modality treatment strategies, such as
the combination of RT, chemotherapy and total mesorectal excision
(TME), has improved the clinical outcomes and decreased the local
failure rates in patients with LARC (37). The development of improved staging
and surgical techniques, and the utilization of targeted
combinatorial therapies have resulted in a significant increase in
loco regional control and slightly improved overall survival in
trials (37-39).
Recent advances in the field of anatomy and
physiology have contributed to the development of advanced surgical
procedures. Heald et al (40) developed a breakthrough procedure
called TME, which is now the standard surgical procedure for
patients with LARC. TME involves the complete surgical resection of
discontinuous tumor remaining in the mesorectum, which may cause
local treatment failure, with the preservation of the pelvic nerves
using sharp instruments under direct vision (41). Subsequently, MacFarlane et
al (42) demonstrated that the
local recurrence rates in patients with rectal cancer decreased
from 30-40% without TME to <5% with TME. Another study reported
that the local recurrence rates of 1,411 patients with rectal
cancer decreased from 32-35% with conventional surgeries to 4-9%
with TME (43). These results
confirmed that TME is an optimal surgical procedure for patients
with rectal cancer, in which it markedly improves the clinical
outcome and decreases the local recurrence.
Although TME can markedly decrease the local
recurrence rate in patients with early-stage rectal cancer
(42), the local regional
recurrence rate in patients with stage III rectal cancer is high
(~30%), with a high frequency of lymph node metastasis in lower
rectal cancer (44,45). However, extensive tumor resection
is not prescribed due to the severe side effects associated with
lateral dissection, including impaired urinary system, loss of
sexual ability and decreased 5-year survival rate (46). Therefore, additional treatment
strategies have been developed to decrease the tumor volume before
surgery. nCRT followed by TME has been developed and recommended by
the National Comprehensive Cancer Network (NCCN) guidelines
(47) as the standard therapy for
stage II/III RC treatment. It can be used to shrink the volume of
primary or metastatic tumors, resulting in decreasing the tumor
stages with reduced loco-regional recurrence and distant metastasis
rate (48). Most patients
receiving nCRT before an operation are in better physical condition
and have a better tolerance compared with those receiving CRT after
operation (38). In case of
patients with unresectable local advance RC, chemo-radiotherapy has
become the only standard therapy until the patients are available
for surgery (39). Except for
patients with contraindications, recommended radiotherapy schedules
for LARC include two radiation treatment paradigms: Short-course
(SC)- and long-course (LC)-RT. SC-RT is given as 5 daily fractions
of 5 Gy (5 Gy x 5 fractions) over 1 week or 25 Gy total followed by
immediate surgical resection within 1 week (49). LC-RT has been shown as treatment of
45-50.4 Gy in 25-28 fractions with concurrent chemotherapy followed
by delayed TME from 4 to 8 weeks after CRT (50). Both SC-RT and LC-CRT are effective
therapies and multiple trials have demonstrated the equal efficacy
and safety of SC-RT and LC-RT therapy, with no significant
differences in long-term outcome with regards to local recurrence
rate, survival and late toxicity between SC-RT and LC-CRT (51-53).
However, the choice of the optimal approach remains controversial.
In the USA, LC-RT has been used as the standard of care for
treatment of patients with LARC, while preoperative SC-RT has been
more used by radiation oncologists in Western Europe (54,55).
Radiation oncologists in the USA have emphasized that LC-RT
improves the complete response rate of patients, with lower
surgical morbidity, less incidence of positive radial resection
margins and increased tumor down-staging due to a longer delay
between irradiation and surgical resection (56). SC-RT has just been prescribed for
patients not receiving chemotherapy or having a geographic barrier
to receiving LC-CRT (54).
Conversely, supporters of SC-RT have suggested that patients
treated with SC-RT received more benefits of lower cost and less
acute radiation toxicity without different long-term outcomes
compared with LC-RT (57).
Although the positive outcomes of nCRT have been widely
demonstrated and used in Western Europe and the USA, nCRT is still
not a standard treatment in Japan (58,59).
The application of nCRT to Japanese patients with LARC has met
several obstacles. Normally, Japanese people are thinner and with
less visceral fat than individuals in Western countries and the
USA, therefore making surgery a favorable choice (60). Another reason is the lack of
radiation oncologists, RT technologists and medical physicists in
Japan, resulting in the rate of new patients with cancer who
receive RT being less than half of that in Western countries
(61,62). Evidence on the efficacy of
preoperative RT in Japan is extremely limited (61,62).
CRT before TME is currently used as the standard
therapy for patients with stage II/III rectal cancer. This strategy
is used to shrink the volume of primary or metastatic tumors, which
downgrades the tumor stage and decreases the loco-regional
recurrence and distant metastasis rates (48). Patients who undergo CRT before
surgery exhibit better physical health and therapy tolerance than
those who receive CRT after surgery (38). In patients with unresectable LARC,
CRT is the only standard therapy until the patients are eligible
for surgery (63,64).
Additionally, other treatment strategies have been
developed for special cases of rectal cancer. The 'watch and wait'
strategy has been used for patients with rectal cancer who achieved
a complete clinical response after nCRT without surgery; the
advantages of this approach include the reduction in the local
recurrence rate, which was similar to that of surgical resection,
and the preservation of organ (65). The toxicities associated with RT
and the ineligibility of some patients to undergo RT due to their
tumor location have led to the development of neoadjuvant
chemotherapy without radiation as an alternative therapeutic
strategy for patients with rectal cancer (66). However, this treatment paradigm
remains under consideration and is not yet recommended for use
according to the NCCN guidelines (47), which recommend total neoadjuvant
therapy, involving the combination of both chemotherapy and CRT
before surgery, for patients with rectal cancer. This therapeutic
strategy downgrades the tumor stage and improves the overall
survival rate (67,68). Moreover, patients who receive total
neoadjuvant therapy are eligible for the 'watch and wait'
therapeutic strategy (69). Thus,
this approach provides a viable treatment strategy for patients
with rectal cancer as per the NCCN guidelines.
The advantages of the therapeutic combination of
preoperative RT and surgery for patients with LARC have been well
documented in the last few decades. Preoperative RT markedly
improves the outcome of patients with rectal cancer (70). However, the radiation-induced
adverse effects and the development of radioresistance in the
tumors have been the major limitations for the clinical application
of this strategy (71).
Radiation-induced toxicities are classified as acute and late
toxicity based on the time of symptom onset (72). The symptoms of acute toxicities
appear during or right after treatment (73). By contrast, the symptoms of late
toxicity appear after prolonged treatment ranging from several
months to years (73). The
symptoms of acute toxicities include skin erythema, fatigue,
nausea, diarrhea and neurological pain, as well as wound healing
complications for patients undergoing surgical resection (74,75).
Gastrointestinal dysfunction, urinary dysfunction, permanent
neurological toxicities and increased risk of secondary cancers are
the major complications associated with late toxicities (76).
In a TME trial, the combination of SC-RT and TME
markedly decreased the recurrence rates of LARC from 30-50% to
<15% (78) and improved the
10-year survival rate in patients with advanced rectal cancer
compared with surgery alone (78).
However, SC-RT markedly increased the acute toxicity-associated
symptoms, such as lumbosacral plexopathy, stiff pain in the back
and legs during RT, or chronic neurological pain 75). Additionally,
a series of long-term follow-up randomized studies of Stockholm
trials (79), Swedish rectal
cancer trial (80) and Dutch TME
trial (81) indicated that the
frequency of late toxicity-associated symptoms, such as
gastrointestinal dysfunctions with impaired bowel movements and
fecal incontinence, was higher and more severe in patients who
underwent RT compared with that in patients who under-went surgery
alone (80,82). In particular, bowel dysfunction was
observed in ~62% of patients who underwent RT, but in only 38% of
patients who underwent TME alone in the Dutch TME trial (81). Daily activities were significantly
decreased and sexual activity was impaired in patients who
underwent preoperative SC-RT (83). Although the aforementioned Dutch
TME study (81) suggested the
negative effects of RT on the quality of life and sexual function,
patients who underwent RT exhibited downgraded tumor stages
compared with those who underwent only surgery. Moreover, a
follow-up study based on the Uppsala trial revealed that the risk
of secondary cancer in patients who underwent RT was two times
higher than that in patients who did not undergo RT (84). RT-associated secondary pelvic
cancers mostly appeared adjacent to other organs, such as the
colon, prostate, bladder and ureter, in patients who underwent RT
(77).
In addition to radiation-induced toxicities,
resistance to preoperative RT is a major clinical obstacle for
treating LARC. The biological complexities and heterogeneities of
tumors, and the presence of cancer stem cells or accumulated
mutations in the tumors (85,86)
render the tumors radioresistant. Radioresistance is associated
with tumor recurrence, metastasis and poor prognosis, which affect
the therapeutic outcomes (87,88).
Although a pathological complete response is obtained in numerous
cases, several cases are resistant to RT, which is the main cause
of rectal cancer-associated death (89,90).
The pathological response to preoperative RT varies markedly among
patients with LARC. Approximately 8-20% of patients with LARC
respond to preoperative RT (91,92).
However, >40% of patients have a partial response and ~20% of
patients are resistant to preoperative RT (93). These different responses to
preoperative RT are directly associated with local recurrence,
distant metastasis and overall survival of patients with rectal
cancer.
RT is an expensive and time-consuming procedure that
is associated with a high risk of perioperative morbidity. Thus,
the prediction of the response to RT has direct implications on the
clinical decisions regarding treatment strategy. Patients who are
sensitive to CRT must undergo a manual 'wait and see' procedure or
transanal local excision treatment therapy (94,95).
Conversely, patients with poor response to CRT require an
alternative therapeutic strategy. The accurate prediction of the
pathological and clinical response of patients with rectal cancer
to RT may allow clinicians to select the optimal therapeutic
strategy for each case and improve the clinical outcome of RT.
The response in patients with rectal cancer to
preoperative CRT is a critical predictor of local recurrence and
patient survival. However, there are no methods to predict the
response to RT. Previous studies have reported that ncRNAs, which
are key regulators of multiple biological signaling path-ways, are
involved in tumorigenesis and in the regulation of tumor
sensitivity to RT (5,96,97).
Aberrant ncRNA expression induces radioresistance by modulating the
signaling pathways associated with cell cycle regulation, DNA
repair, cell proliferation/apoptosis, hypoxia or self-renewal, and
differentiation of cancer stem cells (98). Since ncRNAs are not digested by
RNases, they are stable in fluids, such as blood, saliva and urine
(99). Therefore, ncRNAs can be
potential predictors of RT response in patients with cancer.
However, there are limited studies that have examined the potential
of ncRNA profiles as predictors of RT response in patients with
rectal cancer. The following section will summarize the published
studies on the ability of various ncRNAs in predicting the RT
response of patients with rectal cancer (Table I).
Some studies have examined the expression profile of
lncRNAs in patients with rectal cancer who have undergone
preoperative RT. Li et al (100) examined six patients with LARC who
had undergone preoperative CRT and demonstrated that the
lncRNA-miRNA-mRNA regulatory network was associated with the nCRT
response. This analysis revealed that 282 lncRNAs were
differentially expressed between the two groups (100). Previous studies have reported
that lncRNAs may regulate gene expression through direct
interaction with the target gene or interaction with miRNAs
(101,102). Therefore, lncRNAs and their
targets that were differentially expressed between the two groups
were identified by constructing the lncRNA-miRNA-mRNA regulatory
network with lncRNAs as key players, and the interaction pairs of
lncRNA-miRNA and miRNA-mRNA were extracted (100). Specific lncRNAs (PRDM11, RPB10
and CWC15) were positively associated with the response to nCRT
(100).
A comprehensive analysis of lncRNA profile was also
performed using lncRNA-specific microarrays (103). Among the 8,127 lncRNAs
represented in the microarrays, 11 were differentially expressed
(two-fold change in expression) between responders and
non-responders (103). Of these
11 lncRNAs, five (LINC00261, lncKIF3A-1, LINC00324, lncKLF7-1 and
LINC00511) were upregulated and six (lncWAPAL-1, lncFGF10-3,
lncMAB21L2-1, lncGALC-6, lncZNF-366-6 and lncHDAC2-2) were
downregulated in the responders (103). Additionally, these differentially
expressed lncRNAs were associated with the molecular mechanism
underlying tumor progression and resistance to therapeutics
(104-106).
Although the comprehensive analysis identified
differentially expressed lncRNAs in patients with rectal cancer,
the aforementioned studies had several limitations, such as the
small size of the study cohort and the lack of functional analyses
of lncRNA signatures. Therefore, these differentially expressed
lncRNAs must be validated and further analyzed in vitro and
in vivo to determine their ability to predict the response
to CRT in patients with LARC.
A study examining the ability of miRNAs to predict
the nCRT response in patients with rectal cancer reported that
miR-145 expression in the tumor tissues after therapy was
upregulated compared with that in the tumor tissues before therapy.
Therefore, the downregulated expression of intratumoral miRNA-145
post-treatment was positively associated with a poor response to
neoadjuvant therapy in patients with rectal cancer (107). miR-21 is one of the most
promising predictors of response to RT in different types of
cancer, such as nasopharyngeal carcinoma and non-small-cell lung
cancer (108,109). Several clinical trials have
examined the roles of miR-21 in patients with rectal cancer
undergoing CRT. Sequencing analysis of 27 rectal tumor biopsies
before CRT revealed that miR-21 was a predictive biomarker in
complete responders and that the sensitivity and specificity of
miR-21 to predict therapeutic response in responders were 78 and
86%, respectively (110). Caramés
et al (111) examined 92
patients with LARC undergoing CRT to investigate the roles of
miR-21 in clinical and molecular characteristics of the tumor,
pathological response and clinical outcome. The aforementioned
study indicated that the preoperative expression levels of miR-21
could distinguish the responders from the non-responders with 92%
positive predictive value and 42.8% negative predictive value
(111).
In addition to miR-21, there are other miRNAs that
can predict the response to therapy in patients with rectal cancer
undergoing CRT. Svoboda et al (112) observed 35 patients with LARC
undergoing CRT and identified that several miRNAs (miR-10a, miR-21,
miR-145, miR-212, miR-339 and miR-361) were differentially
expressed after RT. Among these, miR-125 and miR-137 were markedly
upregulated after the initiation of therapy in most samples
(112). The upregulated
expression levels of both miR-125 and miR-137 have been associated
with a poor response to neoadjuvant therapy (112). Additionally, serum miR-125 levels
in the non-responders are significantly upregulated compared with
those in the responders, and are associated with an excellent
discriminating power (112,113). Additionally, the upregulated
expression levels of miR-345 in both tissues and serum have been
significantly associated with a poor response to neoadjuvant CRT
(114).
A group of miRNAs can be a reliable biomarker that
can accurately predict tumor response to RT. Most studies have
included pathological staging analysis before and after
preoperative CRT as the tumor stage is associated with prognosis
and performed large-scale analysis of the expression levels of
several miRNAs (120,121). Previous miRNA expression profile
analysis has revealed the differential expression patterns of miRNA
signatures between responders and non-responders after preoperative
CRT (122,123). Della Vittoria Scarpati et
al (122) examined the
changes in the expression levels of selected miRNAs in rectal
cancer biopsies from 38 patients diagnosed with T3-4/N+ rectal
cancer who were treated with capecitabine-oxaliplatin and underwent
RT followed by surgery. Microarray was performed to analyze the
expression of 373 miRNAs in frozen biopsies obtained before
treatment (122). In total, 13
differentially expressed miRNAs were identified between good
responders and non-responders (122). Of these 13 miRNAs, 11 (miR-1183,
miR-483-5p, miR-622, miR-125a-3p, miR-1224-5p, miR-188-5p,
miR-1471, miR-671-5p, miR-1909*, miR-630 and miR-765) were
significantly upregulated in good responders, while 2 (miR-1274b
and miR-720) were downregulated (122). The specificity and sensitivity of
differentially expressed miRNAs indicated that they could predict
complete response cases, especially two miRNAs (miR-622 and
miR-630) that are involved in DNA repair mechanisms (122).
To identify the expression pattern of miRNAs to
predict the response of rectal cancer to CRT, Hotchi et al
(123) analyzed 43 patients with
rectal cancer before preoperative CRT using miRNA microarray. The
response to CRT was evaluated based on the following three
parameters: Histopathological exami-nation of surgically resected
specimens, response evaluation criteria in solid tumors (RECIST)
and downstaging (123).
Histopathological examination of surgically resected specimens
revealed that the expression levels of two miRNAs (miR-223 and
miR-142-3p) in the responders were significantly higher than those
in the non-responders (123).
Based on the RECIST parameter, nine miRNAs were identified as
predictive biomarkers of RT response (123). Compared with that in the
non-responders, the expression of one miRNA (miR-223) was
upregulated, while that of eight miRNAs (miR-20b, miR-92a,
let-7a*, miR-20a, miR-17*, miR-106a, miR-17
and miR-20a) was downregulated in the responders (123). The downstaging evaluation
revealed that the expression levels of three miRNAs (miR-223,
miR-630 and miR-126*) were associated with response to
RT (123). These results
indicated that the upregulated expression levels of these miRNA
signatures had the potential to predict the response of patients
with rectal cancer to CRT with high sensitivity and specificity
(123).
The ability of miRNA signatures to predict the
response to treatment has piqued the interest of the scientific
community. Most studies involve a small number of samples with no
validation group (123-125). The investigations involving small
cohorts are associated with a high risk of false-positive cases,
which has hindered or delayed the clinical application of
diagnostic and prognostic biomarkers (126). To overcome these limitations,
Azizian et al (127)
performed microarray analysis of a training set comprising 45
preoperative biopsies from patients with rectal cancer to identify
potential miRNAs that can predict tumor regression grade and other
clinical parameters. The selected miRNAs were then validated using
reverse transcription-quantitative PCR (RT-qPCR) with an
independent set of 147 patients with rectal cancer (127). The upregulated expression levels
of four miRNAs (miR-515-5p, miR-573, miR-579 and miR-802) were
significantly associated with overall survival and cancer-specific
survival in patients with rectal cancer (123,128). The miRNA signature comprising the
four aforementioned miRNAs may predict the treatment response
before RT in patients with rectal cancer.
miRNA signature in the plasma may also potentially
predict tumor response to CRT. Li et al (131) screened the miRNA profile of
plasma samples derived from 26 patients with rectal cancer before
and after RT. The selected miRNAs in the testing and training
groups were validated using RT-qPCR (131). A group of three miRNAs comprising
miR-374a-5p, miR-342-5p and miR-519d-3p emerged as potential
predictive markers for distinguishing the responders from the
non-responders before RT (131).
In particular, the downregulated expression levels of miR-342-5p
and miR-519d-3p in the plasma were associated with a worse
prognosis and a short 5-year survival in patients with rectal
cancer (131). These results
demonstrate the clinical importance of both tissue and blood miRNA
signatures in predicting the clinical outcomes of rectal cancer and
emphasize the necessity for validation studies in a clinical
setting.
From the aforementioned studies, it is clear that
miRNAs are becoming involved in the response to RT. They are not
only shown as a predictor of RT to select responding or
non-responding patients, but also used to predict the survival and
post-radiation toxicity. Although emerging evidence has indicated
promising roles of miRNAs as valuable clinical tools for
personalized care of rectal cancer in the future, any potential
biomarker requires multiple and large cohorts to validate its
reproducibility. Therefore, statistically rigorous independent
validation studies in different cohorts and different types of
cancer are critical to confirm the prognostic or predictive value
of these emerging findings.
Previous preliminary studies have demonstrated that
ncRNAs can be potential therapeutic targets for cancer (132,133). ncRNAs can function as oncogenes
or tumor suppressors and are involved in cancer initiation,
progression and resistance to therapeutics (134-136). Hence, various strategies have
been developed to utilize ncRNAs as therapeutic targets in cancer.
Recent targeting strategies consist of the application of ncRNA
inhibitors, such as ncRNA mimics, ncRNA vectors, ncRNA sponges,
antisense oligonucleotides, ncRNA-mask oligonucleotides or
clustered regularly interspaced short palindromic repeat-Cas9
technology (137). The modulation
of ncRNA expression levels may be also achieved by transferring
ncRNAs using various delivery systems. Currently, different
strategies have been used to deliver ncRNAs, such as viral-based
vector systems (lentiviruses, retroviruses, adenoviruses or
adeno-associated viruses) and non-viral delivery systems (physical
and chemical approaches) (138,139). The advantages of non-viral
systems include decreased toxicity, low immunogenicity and the
ability to transfer large-sized passenger ncRNAs (139). The viral-based vector systems are
associated with high transfection efficiency, long half-life and
high biodegradability (140).
Therefore, designing a precise delivery system to ensure the
stability of synthetic ncRNAs in circulation, a high transfection
efficiency and tumor-specific targeting is indispensable to
translate ncRNA therapy to the clinic. The modulation of ncRNAs or
ncRNA-regulated signaling pathways can be a potential therapeutic
strategy to enhance the radiosensitivity of rectal cancer (Table II).
Several lncRNAs can modulate radiosensitivity
through multiple mechanisms in rectal cancer. The suppression of
lincRNA-ROR sensitizes rectal cancer cells by inducing cell death
after irradiation (149).
lincRNA-ROR regulates radiosensitivity by promoting the expression
levels of p53 and miR-145, and consequently modulating the
expression levels of p21 and Myc (149). lncRNA OIP5-AS1 inhibits
miR-363-3p expression and promotes DYRK1A expression (150). Ectopic expression of lncRNA
OIP5-AS1 promotes radiation-induced cell death and enhances the
radiosensitivity of rectal cancer by targeting DYRK1A (150). Additionally, lincRNA-p21 promotes
the radiosensitivity of rectal cancer by targeting the
Wnt/β-catenin signaling pathway (151), and lincRNA-p21 overexpression
enhances radiation-induced apoptosis by inducing Noxa
expression, a pro-apoptotic gene (151).
Previous studies have demonstrated that ncRNAs
mediate tumor response against radiation. Several ncRNAs may
enhance tumor radiosensitivity, while others confer resistance to
radiation by modulating the irradiation-associated signaling
pathways. Additionally, experimental studies have demonstrated that
the modulation of ncRNA expression levels may markedly enhance the
radiosensitivity of rectal cancer cells in vitro and in
vivo. These findings suggest that ncRNAs may serve as potential
therapeutic targets to improve the outcome of RT. Additionally,
ncRNAs can be targeted in combination therapy for cancer.
The ncRNA-based therapies for cancer have yielded
promising results in preclinical studies. However, the
implementation of these techniques in a clinical setting is
associated with several challenges. The expression levels of ncRNAs
vary among different types of human cancer and even among the same
tumor type in different studies. The tumor microenvironment serves
an essential role in regulating tumor biological behavior and may
hinder the quantification of ncRNA expression. Tumor progression
during RT is a dynamic process that is accompanied by dynamic
changes in ncRNA expression. To enhance the therapeutic efficacy of
ncRNA-based RT, the delivery system of ncRNAs should be modified to
increase their stability and specificity. Therefore, further
technical and scientific development and clinical investigation are
warranted to overcome these challenges.
The present review was supported by the National
Research Foundation of Korea grant funded by the Korean government
(grant no. 2020R1F1A1061122).
Not applicable.
HTHT and SH were involved in the conceptualization
of the study, and confirmed the authenticity of the data. HTHT and
HQD wrote the manuscript, and SH edited and revised it. All authors
have read and approved the final version of the manuscript.
Not applicable.
Not applicable.
The authors declare that they have no competing
interests.
Not applicable.
|
1
|
Miller KD, Siegel RL, Lin CC, Mariotto AB,
Kramer JL, Rowland JH, Stein KD, Alteri R and Jemal A: Cancer
treatment and survivorship statistics, 2016. CA Cancer J Clin.
66:271–289. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Giuliani ME, Lindsay PE, Kwan JY, Sun A,
Bezjak A, Le LW, Brade A, Cho J, Leighl NB, Shepherd FA and Hope
AJ: Correlation of dosimetric and clinical factors with the
development of esophagitis and radiation pneumonitis in patients
with limited-stage small-cell lung carcinoma. Clin Lung Cancer.
16:216–220. 2015. View Article : Google Scholar
|
|
3
|
Han S, Gu F, Lin G, Sun X, Wang Y, Wang Z,
Lin Q, Weng D, Xu Y and Mao W: Analysis of clinical and dosimetric
factors influencing radiation-induced lung injury in patients with
lung cancer. J Cancer. 6:1172–1178. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Briere TM, Krafft S, Liao Z and Martel MK:
Lung size and the risk of radiation pneumonitis. Int J Radiat Oncol
Biol Phys. 94:377–384. 2016. View Article : Google Scholar
|
|
5
|
Podralska M, Ciesielska S, Kluiver J, van
den Berg A, Dzikiewicz-Krawczyk A and Slezak-Prochazka I:
Non-coding RNAs in cancer radiosensitivity: MicroRNAs and lncRNAs
as regulators of radiation-induced signaling pathways. Cancers
(Basel). 12:16622020. View Article : Google Scholar
|
|
6
|
Dreussi E, Pucciarelli S, De Paoli A,
Polesel J, Canzonieri V, Agostini M, Friso ML, Belluco C,
Buonadonna A, Lonardi S, et al: Predictive role of microRNA-related
genetic polymorphisms in the pathological complete response to
neoadjuvant chemoradiotherapy in locally advanced rectal cancer
patients. Oncotarget. 7:19781–19793. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Fanale D, Castiglia M, Bazan V and Russo
A: Involvement of non-coding RNAs in chemo- and radioresistance of
colorectal cancer. Adv Exp Med Biol. 937:207–228. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Bartel DP: MicroRNAs: Genomics,
biogenesis, mechanism, and function. Cell. 116:281–297. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Chen CZ: MicroRNAs as oncogenes and tumor
suppressors. N Engl J Med. 353:1768–1771. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Tan S, Xia L, Yi P, Han Y, Tang L, Pan Q,
Tian Y, Rao S, Oyang L, Liang J, et al: Exosomal miRNAs in tumor
microenvironment. J Exp Clin Cancer Res. 39:672020. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Patil N, Allgayer H and Leupold JH:
MicroRNAs in the tumor microenvironment. Adv Exp Med Biol.
1277:1–31. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kosaka N, Iguchi H and Ochiya T:
Circulating microRNA in body fluid: A new potential biomarker for
cancer diagnosis and prognosis. Cancer Sci. 101:2087–2092. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Movahedpour A, Ahmadi N, Ghasemi Y,
Savardashtaki A and Shabaninejad Z: Circulating microRNAs as
potential diagnostic biomarkers and therapeutic targets in prostate
cancer: Current status and future perspectives. J Cell Biochem.
120:16316–16329. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Sohel MH: Extracellular/circulating
MicroRNAs: Release mechanisms, functions and challenges. Achiev
Life Sci. 10:175–186. 2016.
|
|
15
|
Mercer TR, Dinger ME and Mattick JS: Long
non-coding RNAs: Insights into functions. Nat Rev Genet.
10:155–159. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Fernandes JCR, Acuña SM, Aoki JI,
Floeter-Winter LM and Muxel SM: Long non-coding RNAs in the
regulation of gene expression: Physiology and disease. Noncoding
RNA. 5:172019.
|
|
17
|
Statello L, Guo CJ, Chen LL and Huarte M:
Gene regulation by long non-coding RNAs and its biological
functions. Nat Rev Mol Cell Biol. Dec 22–2020.Epub ahead of print.
PubMed/NCBI
|
|
18
|
Spizzo R, Almeida MI, Colombatti A and
Calin GA: Long non-coding RNAs and cancer: A new frontier of
translational research? Oncogene. 31:4577–4587. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Schmitt AM and Chang HY: Long noncoding
RNAs in cancer pathways. Cancer Cell. 29:452–463. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Liu K, Gao L, Ma X, Huang JJ, Chen J, Zeng
L, Ashby CR Jr, Zou C and Chen ZS: Long non-coding RNAs regulate
drug resistance in cancer. Mol Cancer. 19:542020. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Zhu Y, Zhao Y, Dong S, Liu L, Tai L and Xu
Y: Systematic identification of dysregulated lncRNAs associated
with platinum-based chemotherapy response across 11 cancer types.
Genomics. 112:1214–1222. 2020. View Article : Google Scholar
|
|
22
|
Huang L, Zeng L, Chu J, Xu P, Lv M, Xu J,
Wen J, Li W, Wang L, Wu X, et al: Chemoresistance-related long
non-coding RNA expression profiles in human breast cancer cells.
Mol Med Rep. 18:243–253. 2018.PubMed/NCBI
|
|
23
|
Arnold M, Sierra MS, Laversanne M,
Soerjomataram I, Jemal A and Bray F: Global patterns and trends in
colorectal cancer incidence and mortality. Gut. 66:683–691. 2017.
View Article : Google Scholar
|
|
24
|
Siegel RL, Miller KD, Goding Sauer A,
Fedewa SA, Butterly LF, Anderson JC, Cercek A, Smith RA and Jemal
A: Colorectal cancer statistics, 2020. CA Cancer J Clin.
70:145–164. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Siegel R, Desantis C and Jemal A:
Colorectal cancer statistics, 2014. CA Cancer J Clin. 64:104–117.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Lo AC, Soliman AS, Khaled HM, Aboelyazid A
and Greenson JK: Lifestyle, occupational, and reproductive factors
and risk of colorectal cancer. Dis Colon Rectum. 53:830–837. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Basen-Engquist K and Chang M: Obesity and
cancer risk: Recent review and evidence. Curr Oncol Rep. 13:71–76.
2011. View Article : Google Scholar
|
|
28
|
De Roos AJ, Ray RM, Gao DL, Fitzgibbons
ED, Ziding F, Astrakianakis G, Thomas DB and Checkoway H:
Colorectal cancer incidence among female textile workers in
Shanghai, China: A case-cohort analysis of occupational exposures.
Cancer Causes Control. 16:1177–1188. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Oddone E, Modonesi C and Gatta G:
Occupational exposures and colorectal cancers: A quantitative
overview of epidemiological evidence. World J Gastroenterol.
20:12431–12444. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Rattray NJW, Charkoftaki G, Rattray Z,
Hansen JE, Vasiliou V and Johnson CH: Environmental influences in
the etiology of colorectal cancer: The premise of metabolomics.
Curr Pharmacol Rep. 3:114–125. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Peters RK, Garabrant DH, Yu MC and Mack
TM: A case-control study of occupational and dietary factors in
colorectal cancer in young men by subsite. Cancer Res.
49:5459–5468. 1989.PubMed/NCBI
|
|
32
|
Wang Y, Lewis-Michl EL, Hwang SA,
Fitzgerald EF and Stark AD: Cancer incidence among a cohort of
female farm residents in New York State. Arch Environ Health.
57:561–567. 2002. View Article : Google Scholar
|
|
33
|
Wesseling C, Antich D, Hogstedt C,
Rodríguez AC and Ahlbom A: Geographical differences of cancer
incidence in Costa Rica in relation to environmental and
occupational pesticide exposure. Int J Epidemiol. 28:365–374. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Rushton L, Hutchings S and Brown T: The
burden of cancer at work: Estimation as the first step to
prevention. Occup Environ Med. 65:789–800. 2008. View Article : Google Scholar
|
|
35
|
Toiyama Y and Kusunoki M: Changes in
surgical therapies for rectal cancer over the past 100 years: A
review. Ann Gastroenterol Surg. 4:331–342. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Knol J and Keller DS: Total mesorectal
excision technique-past, present, and future. Clin Colon Rectal
Surg. 33:134–143. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Kapiteijn E, Marijnen CA, Nagtegaal ID,
Putter H, Steup WH, Wiggers T, Rutten HJ, Pahlman L, Glimelius B,
van Krieken JH, et al: Preoperative radiotherapy combined with
total mesorectal excision for resectable rectal cancer. N Engl J
Med. 345:638–646. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Sauer R, Becker H, Hohenberger W, Rödel C,
Wittekind C, Fietkau R, Martus P, Tschmelitsch J, Hager E, Hess CF,
et al: Preoperative versus postoperative chemoradiotherapy for
rectal cancer. N Engl J Med. 351:1731–1740. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Roeder F, Meldolesi E, Gerum S, Valentini
V and Rödel C: Recent advances in (chemo-)radiation therapy for
rectal cancer: A comprehensive review. Radiat Oncol. 15:2622020.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Heald RJ, Husband EM and Ryall RD: The
mesorectum in rectal cancer surgery-the clue to pelvic recurrence?
Br J Surg. 69:613–616. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Hermanek P, Hermanek P, Hohenberger W,
Klimpfinger M, Köckerling F and Papadopoulos T: The pathological
assessment of mesorectal excision: Implications for further
treatment and quality management. Int J Colorectal Dis. 18:335–341.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
MacFarlane JK, Ryall RD and Heald RJ:
Mesorectal excision for rectal cancer. Lancet. 341:457–460. 1993.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Havenga K, Enker WE, Norstein J, Moriya Y,
Heald RJ, van Houwelingen HC and van de Velde CJ: Improved survival
and local control after total mesorectal excision or D3
lymph-adenectomy in the treatment of primary rectal cancer: An
international analysis of 1411 patients. Eur J Surg Oncol.
25:368–374. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Randomised trial of surgery alone versus
radiotherapy followed by surgery for potentially operable locally
advanced rectal cancer. Medical research council rectal cancer
working party Lancet. 348:1605–1610. 1996.
|
|
45
|
Kim SH, Lee JM, Hong SH, Kim GH, Lee JY,
Han JK and Choi BI: Locally advanced rectal cancer: Added value of
diffusion-weighted MR imaging in the evaluation of tumor response
to neoadjuvant chemo- and radiation therapy. Radiology.
253:116–125. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Christou N, Meyer J, Toso C, Ris F and
Buchs NC: Lateral lymph node dissection for low rectal cancer: Is
it necessary? World J Gastroenterol. 25:4294–4299. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Benson AB, Venook AP, Al-Hawary MM, Arain
MA, Chen YJ, Ciombor KK, Cohen S, Cooper HS, Deming D,
Garrido-Laguna I, et al: NCCN Guidelines insights: Rectal cancer,
version 6.2020. J Natl Compr Canc Netw. 18:806–815. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Zhang S, Bai W, Tong X, Bu P, Xu J and Xi
Y: Correlation between tumor microenvironment-associated factors
and the efficacy and prognosis of neoadjuvant therapy for rectal
cancer. Oncol Lett. 17:1062–1070. 2019.PubMed/NCBI
|
|
49
|
Ma B, Gao P, Song Y, Huang X, Wang H, Xu
Q, Zhao S and Wang Z: Short-course radiotherapy in neoadjuvant
treatment for rectal cancer: A systematic review and meta-analysis.
Clin Colorectal Cancer. 17:320–330.e5. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Bujko K, Wyrwicz L, Rutkowski A,
Malinowska M, Pietrzak L, Kryński J, Michalski W, Olędzki J,
Kuśnierz J, Zając L, et al: Long-course oxaliplatin-based
preoperative chemoradiation versus 5×5 Gy and consolidation
chemotherapy for cT4 or fixed cT3 rectal cancer: Results of a
randomized phase III study. Ann Oncol. 27:834–842. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
From the American Association of
Neurological Surgeons (AANS); American Society of Neuroradiology
(ASNR); Canadian Interventional Radiology Association (CIRA);
Congress of Neurological Surgeons (CNS); European Society of
Minimally Invasive Neurological Therapy (ESMINT); European Society
of Neuroradiology (ESNR); European Stroke Organization (ESO);
Society for Cardiovascular Angiography; Interventions (SCAI);
Society of Interventional Radiology (SIR); Society of
Interventional Radiology (SIR); et al: Multisociety consensus
quality improvement revised consensus statement for endovascular
therapy of acute ischemic stroke. Int J Stroke. 13:612–632.
2018.PubMed/NCBI
|
|
52
|
Ngan SY, Burmeister B, Fisher RJ, Solomon
M, Goldstein D, Joseph D, Ackland SP, Schache D, McClure B,
McLachlan SA, et al: Randomized trial of short-course radiotherapy
versus long-course chemoradiation comparing rates of local
recurrence in patients with T3 rectal cancer: Trans-Tasman
radiation oncology group trial 01.04. J Clin Oncol. 30:3827–3833.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
McLachlan SA, Fisher RJ, Zalcberg J,
Solomon M, Burmeister B, Goldstein D, Leong T, Ackland SP,
McKendrick J, McClure B, et al: The impact on health-related
quality of life in the first 12 months: A randomised comparison of
preoperative short-course radiation versus long-course
chemoradiation for T3 rectal cancer (Trans-Tasman Radiation
Oncology Group Trial 01.04). Eur J Cancer. 55:15–26. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Mowery YM, Salama JK, Zafar SY, Moore HG,
Willett CG, Czito BG, Hopkins MB and Palta M: Neoadjuvant
long-course chemoradiation remains strongly favored over
short-course radiotherapy by radiation oncologists in the United
States. Cancer. 123:1434–1441. 2017. View Article : Google Scholar
|
|
55
|
Glynne-Jones R, Wyrwicz L, Tiret E, Brown
G, Rödel C, Cervantes A and Arnold D; ESMO Guidelines Committee:
Rectal cancer: ESMO clinical practice guidelines for diagnosis,
treatment and follow-up. Ann Oncol. 29(Suppl 4): iv2632018.
View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Sineshaw HM, Jemal A, Thomas CR Jr and
Mitin T: Changes in treatment patterns for patients with locally
advanced rectal cancer in the United States over the past decade:
An analysis from the national cancer data base. Cancer.
122:1996–2003. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Wang X, Zheng B, Lu X, Bai R, Feng L, Wang
Q, Zhao Y and He S: Preoperative short-course radiotherapy and
long-course radiochemotherapy for locally advanced rectal cancer:
Meta-analysis with trial sequential analysis of long-term survival
data. PLoS One. 13:e02001422018. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Otero de Pablos J and Mayol J:
Controversies in the management of lateral pelvic lymph nodes in
patients with advanced rectal cancer: East or west? Front Surg.
6:792019. View Article : Google Scholar
|
|
59
|
Watanabe T, Muro K, Ajioka Y, Hashiguchi
Y, Ito Y, Saito Y, Hamaguchi T, Ishida H, Ishiguro M, Ishihara S,
et al: Japanese society for cancer of the colon and rectum (JSCCR)
guidelines 2016 for the treatment of colorectal cancer. Int J Clin
Oncol. 23:1–34. 2018. View Article : Google Scholar :
|
|
60
|
Tokuhara K, Ueyama Y, Nakatani K, Yoshioka
K and Kon M: Outcomes of neoadjuvant chemoradiotherapy in Japanese
locally advanced rectal carcinoma patients. World J Surg Oncol.
14:1362016. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Numasaki H, Shibuya H, Nishio M, Ikeda H,
Sekiguchi K, Kamikonya N, Koizumi M, Tago M, Ando Y, Tsukamoto N,
et al: Japanese structure survey of radiation oncology in 2007 with
special reference to designated cancer care hospitals. Strahlenther
Onkol. 187:167–174. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Teshima T, Numasaki H, Shibuya H, Nishio
M, Ikeda H, Sekiguchi K, Kamikonya N, Koizumi M, Tago M, Ando Y, et
al: Japanese structure survey of radiation oncology in 2007 based
on institutional stratification of patterns of care study. Int J
Radiat Oncol Biol Phys. 78:1483–1493. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Minsky BD, Cohen AM, Enker WE, Sigurdson E
and Harrison LB: Radiation therapy for unresectable rectal cancer.
Int J Radiat Oncol Biol Phys. 21:1283–1289. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Wang G, Wang W, Jin H, Dong H, Chen W, Li
X, Li G and Li L: The effect of primary tumor radiotherapy in
patients with unresectable stage IV rectal or rectosigmoid cancer:
A propensity score matching analysis for survival. Radiat Oncol.
15:1262020. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
van der Valk MJM, Hilling DE, Bastiaannet
E, Meershoek-Klein Kranenbarg E, Beets GL, Figueiredo NL, Habr-Gama
A, Perez RO, Renehan AG and van de Velde CJH: IWWD Consortium:
Long-term outcomes of clinical complete responders after
neoadjuvant treatment for rectal cancer in the international watch
& wait database (IWWD): An international multicentre registry
study. Lancet. 391:2537–2545. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Zhao F, Wang J, Yu H, Cheng X, Li X, Zhu
X, Xu X, Lin J, Chen X and Yan S: Neoadjuvant radiotherapy improves
overall survival for T3/4N+M0 rectal cancer patients: A
population-based study of 20300 patients. Radiat Oncol. 15:492020.
View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Petrelli F, Trevisan F, Cabiddu M, Sgroi
G, Bruschieri L, Rausa E, Ghidini M and Turati L: Total neoadjuvant
therapy in rectal cancer: A systematic review and meta-analysis of
treatment outcomes. Ann Surg. 271:440–448. 2020. View Article : Google Scholar
|
|
68
|
Cercek A, Roxburgh CSD, Strombom P, Smith
JJ, Temple LKF, Nash GM, Guillem JG, Paty PB, Yaeger R, Stadler ZK,
et al: Adoption of total neoadjuvant therapy for locally advanced
rectal cancer. JAMA Oncol. 4:e1800712018. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Gilshtein H, Ghuman A, Dawoud M, Yellinek
S, Kent I, Sharp SP, Nagarajan A and Wexner SD: Total neoadjuvant
treatment for rectal cancer: Preliminary experience. Am Surg. Nov
10–2020.Epub ahead of print. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
den Dulk M, Krijnen P, Marijnen CA, Rutten
HJ, van de Poll-Franse LV, Putter H, Meershoek-Klein Kranenbarg E,
Jansen-Landheer ML, Coebergh JW and van de Velde CJ: Improved
overall survival for patients with rectal cancer since 1990: The
effects of TME surgery and pre-operative radio-therapy. Eur J
Cancer. 44:1710–1716. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Birgisson H, Påhlman L, Gunnarsson U and
Glimelius B: Late adverse effects of radiation therapy for rectal
cancer-a systematic overview. Acta Oncol. 46:504–516. 2007.
View Article : Google Scholar
|
|
72
|
Bruheim K, Guren MG, Skovlund E, Hjermstad
MJ, Dahl O, Frykholm G, Carlsen E and Tveit KM: Late side effects
and quality of life after radiotherapy for rectal cancer. Int J
Radiat Oncol Biol Phys. 76:1005–1011. 2010. View Article : Google Scholar
|
|
73
|
Joye I and Haustermans K: Early and late
toxicity of radiotherapy for rectal cancer. Recent Results Cancer
Res. 203:189–201. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Marijnen CA, Kapiteijn E, van de Velde CJ,
Martijn H, Steup WH, Wiggers T, Kranenbarg EK and Leer JW;
Cooperative Investigators of the Dutch Colorectal Cancer Group:
Acute side effects and complications after short-term preoperative
radio-therapy combined with total mesorectal excision in primary
rectal cancer: Report of a multicenter randomized trial. J Clin
Oncol. 20:817–825. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Frykholm GJ, Isacsson U, Nygård K,
Montelius A, Jung B, Påhlman L and Glimelius B: Preoperative
radiotherapy in rectal carcinoma-aspects of acute adverse effects
and radiation technique. Int J Radiat Oncol Biol Phys.
35:1039–1048. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Sipaviciute A, Sileika E, Burneckis A and
Dulskas A: Late gastrointestinal toxicity after radiotherapy for
rectal cancer: A systematic review. Int J Colorectal Dis.
35:977–983. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Swedish Rectal Cancer Trial; Cedermark B,
Dahlberg M, Glimelius B, Påhlman L, Rutqvist LE and Wilking N:
Improved survival with preoperative radiotherapy in resectable
rectal cancer. N Engl J Med. 336:980–987. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
van Gijn W, Marijnen CA, Nagtegaal ID,
Kranenbarg EM, Putter H, Wiggers T, Rutten HJ, Påhlman L, Glimelius
B and van de Velde CJ; Dutch Colorectal Cancer Group: Preoperative
radiotherapy combined with total mesorectal excision for resectable
rectal cancer: 12-year follow-up of the multicentre, randomised
controlled TME trial. Lancet Oncol. 12:575–582. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Randomized study on preoperative
radiotherapy in rectal carcinoma. Stockholm colorectal cancer study
group. Ann Surg Oncol. 3:423–430. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Birgisson H, Påhlman L, Gunnarsson U and
Glimelius B; Swedish Rectal Cancer Trial Group: Adverse effects of
preoperative radiation therapy for rectal cancer: Long-term
follow-up of the Swedish rectal cancer trial. J Clin Oncol.
23:8697–8705. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Peeters KC, van de Velde CJ, Leer JW,
Martijn H, Junggeburt JM, Kranenbarg EK, Steup WH, Wiggers T,
Rutten HJ and Marijnen CA: Late side effects of short-course
preoperative radiotherapy combined with total mesorectal excision
for rectal cancer: Increased bowel dysfunction in irradiated
patients-a Dutch colorectal cancer group study. J Clin Oncol.
23:6199–6206. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Pollack J, Holm T, Cedermark B, Altman D,
Holmström B, Glimelius B and Mellgren A: Late adverse effects of
short-course preoperative radiotherapy in rectal cancer. Br J Surg.
93:1519–1525. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Marijnen CA, van de Velde CJ, Putter H,
van den Brink M, Maas CP, Martijn H, Rutten HJ, Wiggers T,
Kranenbarg EK, Leer JW and Stiggelbout AM: Impact of short-term
preoperative radiotherapy on health-related quality of life and
sexual functioning in primary rectal cancer: Report of a
multicenter randomized trial. J Clin Oncol. 23:1847–1858. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Frykholm GJ, Glimelius B and Påhlman L:
Preoperative or postoperative irradiation in adenocarcinoma of the
rectum: Final treatment results of a randomized trial and an
evaluation of late secondary effects. Dis Colon Rectum. 36:564–572.
1993. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Shi Y, Liu N, Lai W, Yan B, Chen L, Liu S,
Liu S, Wang X, Xiao D, Liu X, et al: Nuclear EGFR-PKM2 axis induces
cancer stem cell-like characteristics in irradiation-resistant
cells. Cancer Lett. 422:81–93. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Yan B, Liu S, Shi Y, Liu N, Chen L, Wang
X, Xiao D, Liu X, Mao C, Jiang Y, et al: Activation of AhR with
nuclear IKKα regulates cancer stem-like properties in the
occurrence of radio-resistance. Cell Death Dis. 9:4902018.
View Article : Google Scholar
|
|
87
|
Rycaj K and Tang DG: Cancer stem cells and
radioresistance. Int J Radiat Biol. 90:615–621. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Li F, Zhou K, Gao L, Zhang B, Li W, Yan W,
Song X, Yu H, Wang S, Yu N and Jiang Q: Radiation induces the
generation of cancer stem cells: A novel mechanism for cancer
radioresistance. Oncol Lett. 12:3059–3065. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Hartley A, Ho KF, McConkey C and Geh JI:
Pathological complete response following pre-operative
chemoradiotherapy in rectal cancer: Analysis of phase II/III
trials. Br J Radiol. 78:934–938. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Sinukumar S, Patil P, Engineer R, Desouza
A and Saklani A: Clinical outcome of patients with complete
pathological response to neoadjuvant chemoradiotherapy for locally
advanced rectal cancers: The Indian scenario. Gastroenterol Res
Pract. 2014:8678412014. View Article : Google Scholar
|
|
91
|
Valentini V, Aristei C, Glimelius B,
Minsky BD, Beets-Tan R, Borras JM, Haustermans K, Maingon P,
Overgaard J, Pahlman L, et al: Multidisciplinary rectal cancer
management: 2nd European rectal cancer consensus conference
(EURECA-CC2). Radiother Oncol. 92:148–163. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Gérard JP, Conroy T, Bonnetain F, Bouché
O, Chapet O, Closon-Dejardin MT, Untereiner M, Leduc B, Francois E,
Maurel J, et al: Preoperative radiotherapy with or without
concurrent fluorouracil and leucovorin in T3-4 rectal cancers:
Results of FFCD 9203. J Clin Oncol. 24:4620–4625. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Yoon WH, Kim HJ, Kim CH, Joo JK, Kim YJ
and Kim HR: Oncologic impact of pathologic response on clinical
outcome after preoperative chemoradiotherapy in locally advanced
rectal cancer. Ann Surg Treat Res. 88:15–20. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Pozo ME and Fang SH: Watch and wait
approach to rectal cancer: A review. World J Gastrointest Surg.
7:306–312. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Renehan AG, Malcomson L, Emsley R, Gollins
S, Maw A, Myint AS, Rooney PS, Susnerwala S, Blower A, Saunders MP,
et al: Watch-and-wait approach versus surgical resection after
chemoradiotherapy for patients with rectal cancer (the OnCoRe
project): A propensity-score matched cohort analysis. Lancet Oncol.
17:174–183. 2016. View Article : Google Scholar
|
|
96
|
Chan N, Milosevic M and Bristow RG: Tumor
hypoxia, DNA repair and prostate cancer progression: New targets
and new therapies. Future Oncol. 3:329–341. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Anastasiadou E, Jacob LS and Slack FJ:
Non-coding RNA networks in cancer. Nat Rev Cancer. 18:5–18. 2018.
View Article : Google Scholar
|
|
98
|
Zhu J, Chen S, Yang B, Mao W, Yang X and
Cai J: Molecular mechanisms of lncRNAs in regulating cancer cell
radiosensitivity. Biosci Rep. 39:BSR201905902019. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Sole C, Arnaiz E, Manterola L, Otaegui D
and Lawrie CH: The circulating transcriptome as a source of cancer
liquid biopsy biomarkers. Semin Cancer Biol. 58:100–108. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Li N, Yu J, Luo A, Tang Y, Liu W, Wang S,
Liu Y, Song Y, Fang H, Chen B, et al: LncRNA and mRNA signatures
associated with neoadjuvant chemoradiotherapy downstaging effects
in rectal cancer. J Cell Biochem. 120:5207–5217. 2019. View Article : Google Scholar
|
|
101
|
Liz J and Esteller M: lncRNAs and
microRNAs with a role in cancer development. Biochim Biophys Acta.
1859:169–176. 2016. View Article : Google Scholar
|
|
102
|
Cao MX, Jiang YP, Tang YL and Liang XH:
The crosstalk between lncRNA and microRNA in cancer metastasis:
Orchestrating the epithelial-mesenchymal plasticity. Oncotarget.
8:12472–12483. 2017. View Article : Google Scholar :
|
|
103
|
Ferrando L, Cirmena G, Garuti A, Scabini
S, Grillo F, Mastracci L, Isnaldi E, Marrone C, Gonella R, Murialdo
R, et al: Development of a long non-coding RNA signature for
prediction of response to neoadjuvant chemoradiotherapy in locally
advanced rectal adenocarcinoma. PLoS One. 15:e02265952020.
View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Wang ZK, Yang L, Wu LL, Mao H, Zhou YH,
Zhang PF and Dai GH: Long non-coding RNA LINC00261 sensitizes human
colon cancer cells to cisplatin therapy. Braz J Med Biol Res.
51:e67932017. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Liao J and Dong LP: Linc00261 suppresses
growth and metastasis of non-small cell lung cancer via repressing
epithelial-mesenchymal transition. Eur Rev Med Pharmacol Sci.
23:3829–3837. 2019.PubMed/NCBI
|
|
106
|
Fang Q, Sang L and Du S: Long noncoding
RNA LINC00261 regulates endometrial carcinoma progression by
modulating miRNA/FOXO1 expression. Cell Biochem Funct. 36:323–330.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Drebber U, Lay M, Wedemeyer I, Vallböhmer
D, Bollschweiler E, Brabender J, Mönig SP, Hölscher AH, Dienes HP
and Odenthal M: Altered levels of the onco-microRNA 21 and the
tumor-supressor microRNAs 143 and 145 in advanced rectal cancer
indicate successful neoadjuvant chemoradiotherapy. Int J Oncol.
39:409–415. 2011.PubMed/NCBI
|
|
108
|
Zhu H, Zhu X, Cheng G, Zhou M and Lou W:
Downregulation of microRNA-21 enhances radiosensitivity in
nasopharyngeal carcinoma. Exp Ther Med. 9:2185–2189. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Huang Q: Predictive relevance of ncRNAs in
non-small-cell lung cancer patients with radiotherapy: A review of
the published data. Biomark Med. 12:1149–1159. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Lopes-Ramos CM, Habr-Gama A, Quevedo Bde
S, Felício NM, Bettoni F, Koyama FC, Asprino PF, Galante PA,
Gama-Rodrigues J, Camargo AA, et al: Overexpression of miR-21-5p as
a predictive marker for complete tumor regression to neoadjuvant
chemoradiotherapy in rectal cancer patients. BMC Med Genomics.
7:682014. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Caramés C, Cristóbal I, Moreno V, del
Puerto L, Moreno I, Rodriguez M, Marín JP, Correa AV, Hernández R,
Zenzola V, et al: MicroRNA-21 predicts response to preoperative
chemoradiotherapy in locally advanced rectal cancer. Int J
Colorectal Dis. 30:899–906. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Svoboda M, Izakovicova Holla L, Sefr R,
Vrtkova I, Kocakova I, Tichy B and Dvorak J: Micro-RNAs miR125b and
miR137 are frequently upregulated in response to capecitabine
chemoradiotherapy of rectal cancer. Int J Oncol. 33:541–547.
2008.PubMed/NCBI
|
|
113
|
D'Angelo E, Fassan M, Maretto I,
Pucciarelli S, Zanon C, Digito M, Rugge M, Nitti D and Agostini M:
Serum miR-125b is a non-invasive predictive biomarker of the
pre-operative chemoradiotherapy responsiveness in patients with
rectal adenocarcinoma. Oncotarget. 7:28647–28657. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Yu J, Li N, Wang X, Ren H, Wang W, Wang S,
Song Y, Liu Y, Li Y, Zhou X, et al: Circulating serum microRNA-345
correlates with unfavorable pathological response to preoperative
chemo-radiotherapy in locally advanced rectal cancer. Oncotarget.
7:64233–64243. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Caramés C, Cristobal I, Moreno V, Marín
JP, González-Alonso P, Torrejón B, Minguez P, Leon A, Martín JI,
Hernández R, et al: MicroRNA-31 emerges as a predictive biomarker
of pathological response and outcome in locally advanced rectal
cancer. Int J Mol Sci. 17:8782016. View Article : Google Scholar :
|
|
116
|
Chiang Y, Song Y, Wang Z, Liu Z, Gao P,
Liang J, Zhu J, Xing C and Xu H: microRNA-192, -194 and -215 are
frequently down-regulated in colorectal cancer. Exp Ther Med.
3:560–566. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Wang B, Shen ZL, Gao ZD, Zhao G, Wang CY,
Yang Y, Zhang JZ, Yan YC, Shen C, Jiang KW, et al: MiR-194,
commonly repressed in colorectal cancer, suppresses tumor growth by
regulating the MAP4K4/c-Jun/MDM2 signaling pathway. Cell Cycle.
14:1046–1058. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Zhao Y, Li F, Zhang X, Liu A, Qi J, Cui H
and Zhao P: MicroRNA-194 acts as a prognostic marker and inhibits
proliferation in hepatocellular carcinoma by targeting MAP4K4. Int
J Clin Exp Pathol. 8:12446–12454. 2015.
|
|
119
|
D'Angelo E, Zanon C, Sensi F, Digito M,
Rugge M, Fassan M, Scarpa M, Pucciarelli S, Nitti D and Agostini M:
miR-194 as predictive biomarker of responsiveness to neoadjuvant
chemoradiotherapy in patients with locally advanced rectal
adenocarcinoma. J Clin Pathol. 71:344–350. 2018. View Article : Google Scholar
|
|
120
|
Slotta-Huspenina J, Drecoll E, Feith M,
Habermehl D, Combs S, Weichert W, Bettstetter M, Becker K and
Langer R: MicroRNA expression profiling for the prediction of
resistance to neoadjuvant radiochemotherapy in squamous cell
carcinoma of the esophagus. J Transl Med. 16:1092018. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Du B, Wang X, Wu D, Wang T, Yang X, Wang
J, Shi X, Chen L and Zhang W: MicroRNA expression profiles identify
biomarkers for predicting the response to chemoradiotherapy in
rectal cancer. Mol Med Rep. 18:1909–1916. 2018.PubMed/NCBI
|
|
122
|
Della Vittoria Scarpati G, Falcetta F,
Carlomagno C, Ubezio P, Marchini S, De Stefano A, Singh VK,
D'Incalci M, De Placido S and Pepe S: A specific miRNA signature
correlates with complete pathological response to neoadjuvant
chemoradiotherapy in locally advanced rectal cancer. Int J Radiat
Oncol Biol Phys. 83:1113–1119. 2012. View Article : Google Scholar
|
|
123
|
Hotchi M, Shimada M, Kurita N, Iwata T,
Sato H, Morimoto S, Yoshikawa K, Higashijima J and Miyatani T:
microRNA expression is able to predict response to
chemoradiotherapy in rectal cancer. Mol Clin Oncol. 1:137–142.
2013.PubMed/NCBI
|
|
124
|
Kheirelseid EA, Miller N, Chang KH, Curran
C, Hennessey E, Sheehan M, Newell J, Lemetre C, Balls G and Kerin
MJ: miRNA expressions in rectal cancer as predictors of response to
neoadjuvant chemoradiation therapy. Int J Colorectal Dis.
28:247–260. 2013. View Article : Google Scholar
|
|
125
|
Svoboda M, Sana J, Fabian P, Kocakova I,
Gombosova J, Nekvindova J, Radova L, Vyzula R and Slaby O: MicroRNA
expression profile associated with response to neoadjuvant
chemoradiotherapy in locally advanced rectal cancer patients.
Radiat Oncol. 7:1952012. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Calanzani N, Druce PE, Snudden C, Milley
KM, Boscott R, Behiyat D, Saji S, Martinez-Gutierrez J, Oberoi J,
Funston G, et al: Identifying novel biomarkers ready for evaluation
in low-prevalence populations for the early detection of upper
gastrointestinal cancers: A systematic review. Adv Ther. Dec
11–2020.Epub ahead of print. View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Azizian A, Epping I, Kramer F, Jo P,
Bernhardt M, Kitz J, Salinas G, Wolff HA, Grade M, Beißbarth T, et
al: Prognostic value of MicroRNAs in preoperative treated rectal
cancer. Int J Mol Sci. 17:5682016. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Toyota M, Suzuki H, Sasaki Y, Maruyama R,
Imai K, Shinomura Y and Tokino T: Epigenetic silencing of
microRNA-34b/c and B-cell translocation gene 4 is associated with
CpG island methylation in colorectal cancer. Cancer Res.
68:4123–4132. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Campayo M, Navarro A, Benítez JC,
Santasusagna S, Ferrer C, Monzó M and Cirera L: miR-21, miR-99b and
miR-375 combination as predictive response signature for
preoperative chemoradiotherapy in rectal cancer. PLoS One.
13:e02065422018. View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Machackova T, Trachtova K, Prochazka V,
Grolich T, Farkasova M, Fiala L, Sefr R, Kiss I, Skrovina M,
Dosoudil M, et al: Tumor microRNAs identified by small RNA
sequencing as potential response predictors in locally advanced
rectal cancer patients treated with neoadjuvant chemoradiotherapy.
Cancer Genomics Proteomics. 17:249–257. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Li AL, Chung TS, Chan YN, Chen CL, Lin SC,
Chiang YR, Lin CH, Chen CC and Ma N: microRNA expression pattern as
an ancillary prognostic signature for radiotherapy. J Transl Med.
16:3412018. View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Rupaimoole R and Slack FJ: MicroRNA
therapeutics: Towards a new era for the management of cancer and
other diseases. Nat Rev Drug Discov. 16:203–222. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Renganathan A and Felley-Bosco E: Long
noncoding RNAs in cancer and therapeutic potential. Adv Exp Med
Biol. 1008:199–222. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
134
|
Guzel E, Okyay TM, Yalcinkaya B,
Karacaoglu S, Gocmen M and Akcakuyu MH: Tumor suppressor and
oncogenic role of long non-coding RNAs in cancer. North Clin
Istanb. 7:81–86. 2019.
|
|
135
|
Zhang H, Chen Z, Wang X, Huang Z, He Z and
Chen Y: Long non-coding RNA: A new player in cancer. J Hematol
Oncol. 6:372013. View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Rasool M, Malik A, Zahid S, Basit Ashraf
MA, Qazi MH, Asif M, Zaheer A, Arshad M, Raza A and Jamal MS:
Non-coding RNAs in cancer diagnosis and therapy. Noncoding RNA Res.
1:69–76. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
137
|
Dizaji BF: Strategies to target long
non-coding RNAs in cancer treatment: Progress and challenges. Egypt
J Med Hum Genet. 21:412020. View Article : Google Scholar
|
|
138
|
Yang N: An overview of viral and nonviral
delivery systems for microRNA. Int J Pharm Investig. 5:179–181.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
139
|
Labatut AE and Mattheolabakis G: Non-viral
based miR delivery and recent developments. Eur J Pharm Biopharm.
128:82–90. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
140
|
Zhang Y, Wang Z and Gemeinhart RA:
Progress in microRNA delivery. J Control Release. 172:962–974.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
141
|
Meng WJ, Yan H, Zhou B, Zhang W, Kong XH,
Wang R, Zhan L, Li Y, Zhou ZG and Sun XF: Correlation of SATB1
overexpression with the progression of human rectal cancer. Int J
Colorectal Dis. 27:143–150. 2012. View Article : Google Scholar
|
|
142
|
Zhang P, Wang L, Rodriguez-Aguayo C, Yuan
Y, Debeb BG, Chen D, Sun Y, You MJ, Liu Y, Dean DC, et al: miR-205
acts as a tumour radiosensitizer by targeting ZEB1 and Ubc13. Nat
Commun. 5:56712014. View Article : Google Scholar : PubMed/NCBI
|
|
143
|
Huang X, Taeb S, Jahangiri S, Emmenegger
U, Tran E, Bruce J, Mesci A, Korpela E, Vesprini D, Wong CS, et al:
miRNA-95 mediates radioresistance in tumors by targeting the
sphingolipid phosphatase SGPP1. Cancer Res. 73:6972–6986. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
144
|
Ha Thi HT, Kim HY, Kim YM and Hong S:
MicroRNA-130a modulates a radiosensitivity of rectal cancer by
targeting SOX4. Neoplasia. 21:882–892. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
145
|
Kelley KA, Ruhl RA, Rana SR, Dewey E,
Espinosa C, Thomas CR Jr, Martindale RG, Anand S and Tsikitis VL:
Understanding and resetting radiation sensitivity in rectal cancer.
Ann Surg. 266:610–616. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
146
|
Ruhl R, Rana S, Kelley K, Espinosa-Diez C,
Hudson C, Lanciault C, Thomas CR Jr, Liana Tsikitis V and Anand S:
microRNA-451a regulates colorectal cancer proliferation in response
to radiation. BMC Cancer. 18:5172018. View Article : Google Scholar : PubMed/NCBI
|
|
147
|
Luo J, Liu L, Zhou N, Shen J, Sun Q, Zhu Y
and Chen M: miR-519b-3p promotes responsiveness to preoperative
chemo-radiotherapy in rectal cancer patients by targeting ARID4B.
Gene. 655:84–90. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
148
|
Winter SF, Lukes L, Walker RC, Welch DR
and Hunter KW: Allelic variation and differential expression of the
mSIN3A histone deacetylase complex gene Arid4b promote mammary
tumor growth and metastasis. PLoS Genet. 8:e10027352012. View Article : Google Scholar : PubMed/NCBI
|
|
149
|
Yang P, Yang Y, An W, Xu J, Zhang G, Jie J
and Zhang Q: The long noncoding RNA-ROR promotes the resistance of
radiotherapy for human colorectal cancer cells by targeting the
p53/miR-145 pathway. J Gastroenterol Hepatol. 32:837–845. 2017.
View Article : Google Scholar
|
|
150
|
Zou Y, Yao S, Chen X, Liu D, Wang J, Yuan
X, Rao J, Xiong H, Yu S, Yuan X, et al: LncRNA OIP5-AS1 regulates
radioresistance by targeting DYRK1A through miR-369-3p in
colorectal cancer cells. Eur J Cell Biol. 97:369–378. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
151
|
Wang G, Li Z, Zhao Q, Zhu Y, Zhao C, Li X,
Ma Z, Li X and Zhang Y: LincRNA-p21 enhances the sensitivity of
radiotherapy for human colorectal cancer by targeting the
Wnt/β-catenin signaling pathway. Oncol Rep. 31:1839–1845. 2014.
View Article : Google Scholar : PubMed/NCBI
|