Cancers of the central nervous system (CNS) affect
the brain in 95% of cases and the remaining 5% are distributed
among the meninges and spinal cord skin, cranial nerves, and spinal
cord. Initially, tumors of CNS were classified based on their
tissue and cell origin. Gliomas are of neuroectodermal origin,
derived from the supporting glial cells within the CNS (1). They demonstrate a considerable
variability in age of onset, grade of severity, histological
features, and ability to progress as well as to metastasize
(1-5).
According to the classification of CNS tumors
published by the World Health Organization (WHO) in 2016,
glioblastoma belong to the group of diffuse astrocytic and
oligodendroglial tumors with aggressive clinical behavior
corresponding to WHO grade IV comprising three subgroups: Primary
glioblastoma, secondary glioblastoma with and without presence of
isocitrate dehydrogenase (IDH) mutations, and the third one
containing not otherwise specified glioblastoma tumors (1). Glioblastoma with IDH wild type
represents 90% of the cases, which most frequently corresponds to
the clinically defined primary or de novo glioblastoma that
is predominantly found in patients aged over 55 years (6). Secondary glioblastoma with a history
of prior lower-grade diffuse glioma mainly arises in younger
patients and presents approximately 10% of the cases. The highest
incidence with ~65% is reported for individuals aged more than 65
years with the average annual age-adjusted rate of approximately 3
per 100,000 individuals per year (7). Glioblastomas are 1.58-fold more
prevalent in males than in females. With a median survival time of
14 months, the diagnosis is very poor for patients with WHO grade
IV tumors and only 5.6% of patients survive longer than five years
post diagnosis (7-10).
The Consortium to Inform Molecular and Practical
Approaches to CNS Tumor Taxonomy concluded that histologic grade II
and III IDH wild-type diffuse astrocytic gliomas that contain a
high-level of epidermal growth factor receptor (EGFR)
amplification, a combination of whole chromosome 7 gain and whole
chromosome 10 loss (+7/−10), or telomerase reverse transcriptase
(TERT) promoter mutations, correspond to WHO grade IV and should be
referred to as diffuse astrocytic glioma, IDH wild type, with
molecular features of glioblastoma, WHO grade IV (11). It was also suggested that specific
molecular signatures in subsets of IDH wild-type diffuse astrocytic
gliomas are associated with better clinical outcomes and should not
lead to a high-grade designation including those gliomas with other
genetic alterations as individual drivers (11).
In order to accomplish early diagnosis and to
develop personalized anti-cancer therapy, studies have focused on
the identification of valid tumor markers that are easily
accessible, can be simply analyzed, and provide accurate
information regarding disease and severity (12). Epigenetic dysregulation of the
ten-eleven translocation (TET) enzymes results in frequent
epigenetic alterations in human glioblastoma including DNA
hypermethylation and hypo-hydroxymethylation, as well as loss of
histone acetylation (13).
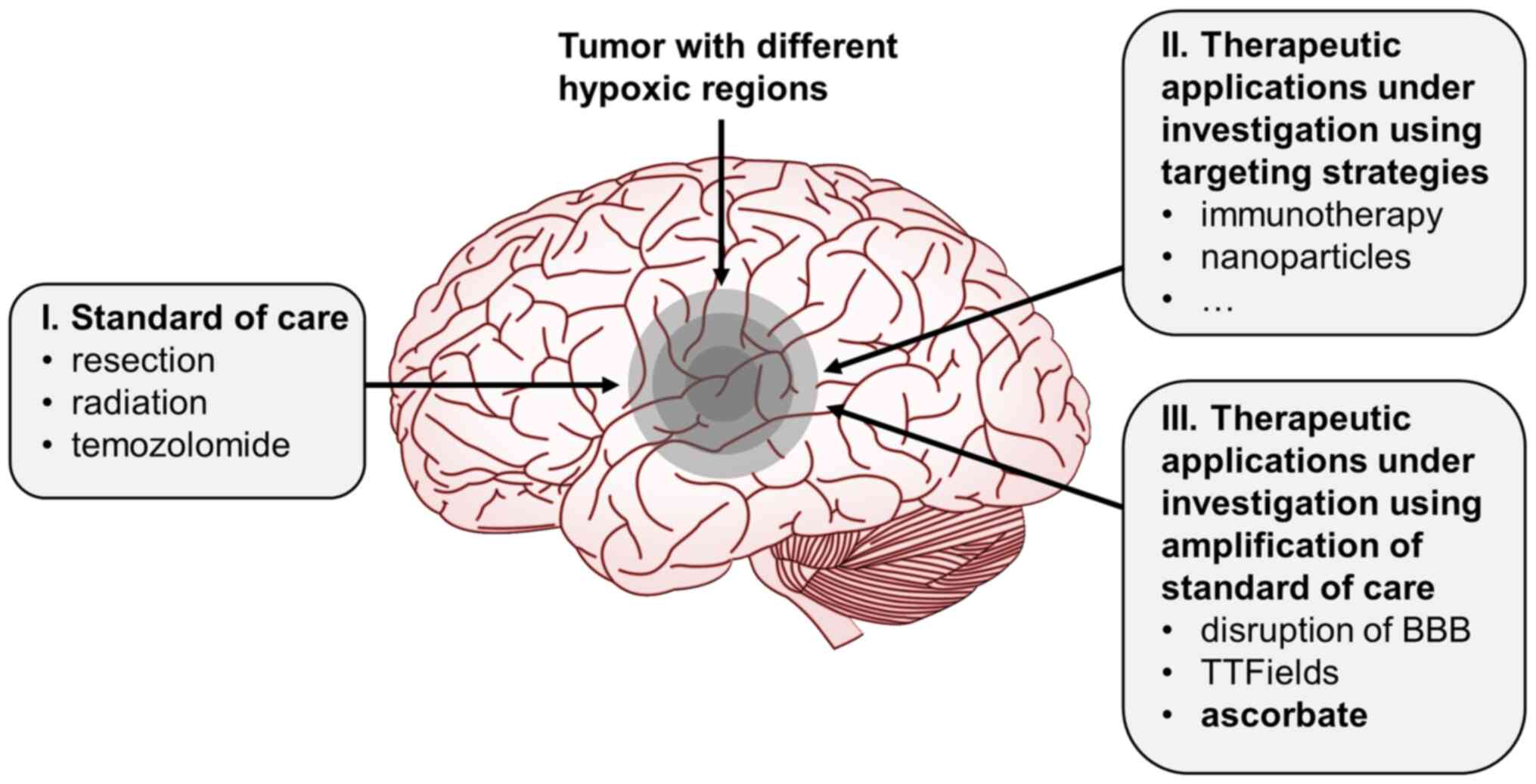
One of the current treatment options includes
surgical resection aiming to remove as much contrast-enhancing
tissue as possible without giving the patient a new functional
deficit (15-17). Since most recurrences occur in
close proximity to the primary tumor or in the tumor bed,
percutaneous fractionated radiotherapy should also be performed
(18). At present, the standard
chemotherapeutic drug for glioblastoma is temozolomide (19-22).
Despite the aggressive therapy and research efforts,
the prognosis for survival remains extremely poor and has not
improved much over the last decades. The chemotherapeutic options
are limited and restricted by poor distribution in the CNS due to
the infiltrative nature, prominent angiogenesis, and
vascularization of glioblastoma as well as acute systemic toxic
effects and long-term toxicity in the CNS and bone marrow. The
current research is dominated by checkpoint inhibitor trials,
vaccine trials, and gene therapies (23). Of note, tumor-treating fields are
electric fields that represent a non-invasive cancer treatment
option that is applied locally, displaying good results in addition
to standard of care therapy to improve the survival of newly
diagnosed patients (24).
There has also been some success via the application
of oncolytic viruses in the treatment of glioblastoma such as
H1-parvovirus (25). The effects
were caused in part by direct oncolysis but also by inducing the
antitumoral immune response (25). Dendritic cell or peptide
immunotherapy and chimeric antigen receptor (CAR) T-cell therapy
are also under consideration (26). Even though there are some
promising novel approaches, there remains a need to improve
glioblastoma treatment options.
Interestingly, high vitamin C or ascorbate
concentrations were shown to damage cancer cells by exhibiting
pro-oxidative effects. On the other hand, high-dose ascorbate seems
to be well tolerated by non-malignant cells (26-29). The aim of this review was to
examine the current findings in regard to the therapeutic potential
of pharmacological doses of vitamin C in the treatment of
glioblastoma.
For this review, the literature research was
performed using key words including 'glioblastoma', 'glioma',
'glioblastoma multiforme', 'vitamin C', 'ascorbate', 'ascorbic
acid', and 'pharmacological' 'intravenous', 'IV', and 'high-dose'
'blood brain barrier', 'brain', 'cancer', 'vitamin C or ascorbate
transporter', 'clinical trials', 'treatment', 'human' as well as
'ascorbate derivatives'. The terms were entered solely or in
combination to find original articles and reviews on the homepage
of the National Library of Medicine (PubMed.gov). The
search was not restricted to publication date or other
specifications, even though results from newly published studies
were preferred over the older ones. However, in case of
differences, both were cited in general. If results from clinical
trials were published as original research, the details from human
studies were verified using the following data sources https://clinicaltrials.gov, https://www.clinicaltrialsregister.eu/ctr-search/search,
and https://www.who.int/clinical-trials-registry-platform.
Vitamin C, also known as L-ascorbic acid (AA) or
ascorbate, is an essential micronutrient and its deficiency is
associated with several serious symptoms and ultimately death
(30). In humans and most
primates, vitamin C needs to be supplied by the diet due to the
lack of functional enzyme L-gulono-γ-lactone oxidase (GULO), which
catalyzes the last step of AA biosynthesis (31). In fluids, vitamin C occurs in two
major forms as ascorbate (90%) or in its oxidized form
dehydroascorbate (DHA). Under physiological conditions, the amount
of DHA in plasma is estimated as <1-2% relative to plasma
ascorbate levels (32). The
recommended daily dose of vitamin C varies between 75 and 100 mg
resulting in physiological plasma levels of 50-100 µmol/l
(33,34). However, there are major
discrepancies regarding recommendations for dietary vitamin C
intake depending on individual physiological and pathophysiological
conditions (35).
With ingested amounts found in foods, vitamin C
plasma concentrations usually do not exceed 100 µmol/l
(32). Even after oral
supplementation, ascorbate plasma concentrations stay below 250
µmol/l and often lower than 150 µmol/l (32,36). By contrast, after intravenous
ascorbate injection (i.v.), pharmacologic plasma ascorbate
concentrations of 26.2 +/−4.9 mmol/l are safely achieved (37). Serious side effects were only
reported for patients with pre-existing renal insufficiency or
glucose 6-phosphate dehydrogenase deficiency, both known to be
predisposed to vitamin C toxicity (38). Besides tissue accumulation and
renal reabsorption, the major determinant of plasma concentration
of orally ingested vitamin C is the saturable capacity of the gut.
Parenteral ascorbate bypasses the intestinal absorption mechanisms
that are responsible for this limitation and therefore allows the
use of ascorbate as a pharmacological agent. For vitamin C, a
linear relationship between dose and Cmax can be
observed up to 70 g/m2 in humans [approximately 112 g in
females (body surface: 1.60 m2) and 133 g in males (body
surface: 1.90 m2)] as complied from pharmacokinetic
studies, while higher doses do not translate into higher plasma
Cmax levels (39,40).
There is growing evidence that patients with cancer
have lower vitamin C plasma levels than healthy controls (41-46) and a large proportion of them
exhibit hypovitaminosis for vitamin C or manifest deficiency
(47-53). Severity of the disease also
appears to correlate with the vitamin C status and higher stages of
cancers seem to be associated with lower vitamin C levels (52,54,55). Mayland et al showed that
patients with low vitamin C plasma levels have a significantly
worse prognosis than patients with sufficient plasma levels
(48). Although it is suspected
that vitamin C blood levels are low in patients with glioblastoma,
no data according vitamin C deficiency, symptoms, and disease
progress are currently available for this tumor entity.
Ascorbate is required for homeostasis and proper
functioning of the central nervous system. The brain consumes a
large portion of glucose (~25%) and oxygen (~20%), which implies
rapid metabolism with increased free radical production. Being an
organ that metabolizes oxygen with relatively weak protective
antioxidant mechanisms, the brain is particularly susceptible to
oxidative stress (56). It
therefore depends on high levels of antioxidants to maintain redox
balance. Accordingly, ascorbate is the physiologically most
abundant antioxidant present in brain tissue.
As a water soluble agent, vitamin C is absorbed from
the small intestine and then distributed from blood throughout the
extracellular space (32).
Vitamin C is accumulated in tissues against a concentration
gradient. The concentrations of vitamin C in tissues are frequently
higher (up to 4,000 µmol/l) than in fluids (up to 300
µmol/l) and may simply serve as a reservoir or have other
unknown functions (32,36,57). It should be noted that for many
human tissues accurate vitamin C concentrations are not known for
physiological nor pathophysiological conditions. The total average
concentration of vitamin C in the brain is lower in comparison to
the adrenal gland, lens, or liver. Within the brain, the highest
concentration was observed in the pituitary gland and accumulation
in neurons with 10 mmol/l was markedly higher than in the cerebral
spinal fluid or glial cells with only 1 mmol/l suggesting an
important role in the maintenance of neuronal integrity (32,58-61).
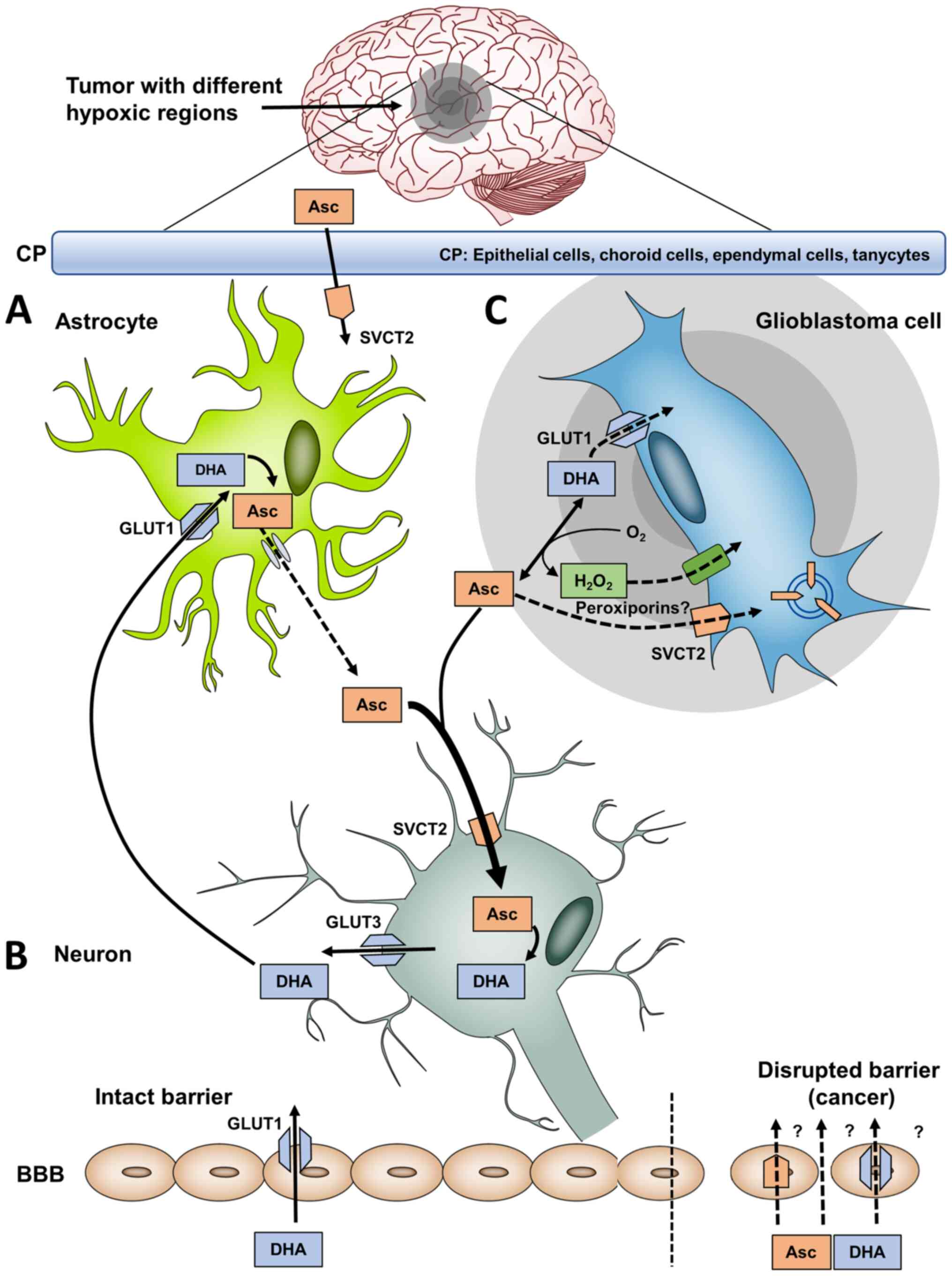
As a hydrophilic molecule, vitamin C enters the CNS
from the blood-brain-barrier (BBB) or from the blood-cerebral
spinal fluid (CSF) barrier formed by epithelial cells of the
choroid plexus (CP) (Fig. 1)
(62,63). Vitamin C initially accumulates in
CP cells and then passes through the CSF into the brain (63). This observation confirms the data
from knockout mice analysis and cell models (64-68).
The incorporation of ascorbate in the cells is
mediated via specific transporters termed sodium-dependent vitamin
C transporter (SVCT) 1 and 2 (69-72). SVCT2 is the absorptive vitamin C
transporter in the brain (69).
DHA is translocated via the solute carrier family 2, facilitated
glucose transporter, member 1 [SLC2A1 or glucose transporter 1
(GLUT1)] (73). Due to the lack
of SVCT2 in cerebrovascular endothelial cells, transport via BBB
occurs as DHA via GLUT1 (74). As
DHA concentration is low in blood, the role and influence of this
transport route into the extracellular space regarding the
maintenance of the ascorbate concentration in the brain seems to be
insignificant under physiological conditions.
Ascorbate enters CNS through SVCT2 present in
choroid plexus cells on the basal side (75,76) of the CP and also probably through
GLUT1 (69,77) and is then distributed into
ventricular space from which it penetrates across ependyma and pia
mater deeply into the brain (78). The concentration of ascorbate is
thereupon balanced between cerebrospinal fluid and the
extracellular fluid (ECF) by diffusion through ependymal cells.
SVCT2 is not expressed in astrocytes under
physiological conditions but these brain cells play an important
role in the regeneration of DHA into ascorbate. It is postulated
that astrocytes incorporate DHA through GLUT1 (79,80) and then convert DHA into ascorbate
due to the 4-fold higher intracellular glutathione levels compared
to neurons (81). After the
conversion of DHA to ascorbate within astrocytes, it is released
from astrocytes and extracellular ascorbate is capable of entering
neurons via SVCT2 again (82).
This circuit describes the bystander effect including vitamin C
recycling between astrocytes and neurons, in which neurons are the
'activated cells' inducing oxidation of ascorbate to DHA which is
subsequently absorbed by the astrocytes as 'bystander cells'
(63,83).
This ascorbate recycling as an interaction between
astrocytes and neurons is crucial for the maintenance of normal
brain ascorbate levels required for different functions inside the
CNS such as catecholamine biosynthesis (84), peptide amidation (85), myelin formation (86), enhancement of synaptic activity
(87), protection against
glutamate toxicity (88), and
modulation of precursor cell proliferation and differentiation
(63,89,90). Taken together, vitamin C is found
in higher concentrations in CSF and brain parenchyma (200-400
µmol/l) than in plasma (30-60 µmol/l) (91,92).
Since Cameron and Pauling demonstrated that
ascorbate-treated terminal cancer patients experienced a 4.2-fold
increase in the mean survival time compared to untreated controls
(93), the role of vitamin C in
tumorigenesis and anti-cancer treatment has become the object of
investigations and still not finally clarified. Twenty years later,
the pharmacokinetics of ascorbate were described by Levine et
al (36).
Ascorbate was an early unconventional and
inexpensive therapy for the treatment of cancer with an excellent
safety profile and surprising clinical efficacy (93). However, as two clinical trials
with oral ascorbate failed to reproduce these effects, ascorbate
was not used any more in the conventional oncologic therapy and
shifted to the field of complementary and alternative medicine
(94,95). Interestingly, previous studies
resulted in the re-examination of ascorbate treatment and it became
clear that only parenteral application of ascorbate yielded
millimolar plasma levels with high efficacy against tumor
progression (96-99). As the existing evidences are
preliminary, there is a number of fundamental questions around best
clinical practice, frequency of therapy, dosage, duration as well
as treatment guidelines for each tumor entity and grade (100-102).
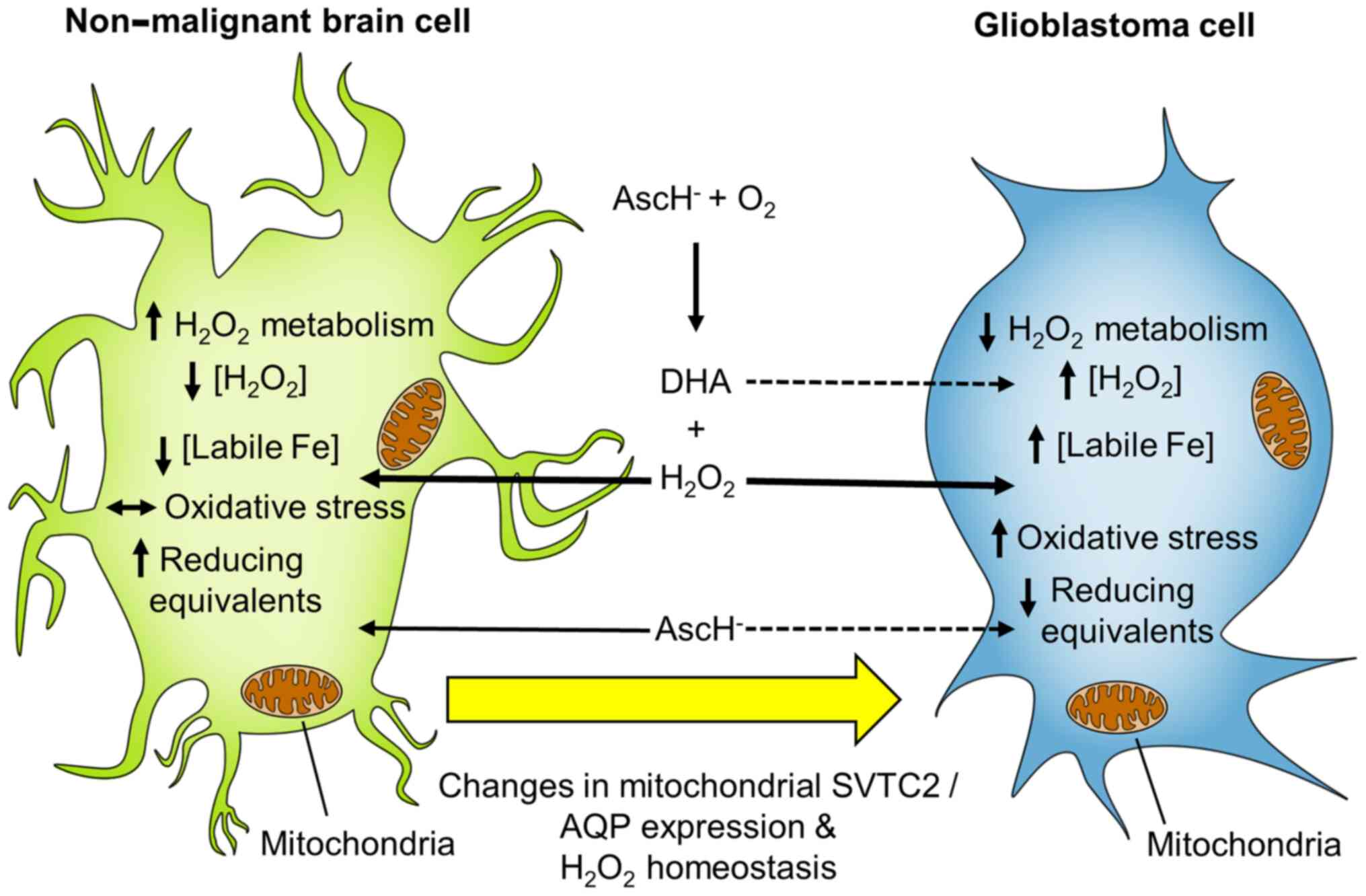
The chemistry of ascorbate defines its biological
activity in terms of its function as an anti-oxidant as well as a
pro-oxidant. It initiates selective toxicity in cancer cells
(26) but not in normal cells and
enhances cytotoxic effects in combination with radiotherapy and/or
chemotherapy (103). The prodrug
effect of pharmacological ascorbate includes its ability to form
and deliver extracellular hydrogen peroxide
(H2O2) to tissue (27). H2O2 crosses
cell membranes via peroxiporins (104-106). The selective toxicity of
ascorbate depends on an altered H2O2
metabolism in cancer compared to non-malignant cells.
The mechanism of cytotoxicity of pharmacological
vitamin C is not only associated with high levels of extra-cellular
H2O2 (26)
but also involves labile iron pools. These catalyze the oxidation
of ascorbate to produce H2O2 thereby
generating the hydroxyl radical from H2O2 via
the Fenton reaction and causing oxidative damage to cellular
lipids, proteins, and DNA (Fig.
2) (28). This effect is well
described for neuroblastoma (107). Therefore, there are two
mechanisms, which contribute to the selective toxicity of ascorbate
in cancers: First, a reduced capacity to remove
H2O2 and second, superoxide as well as
H2O2-induced disruption of the iron
metabolism with increased levels of redox active iron (28,103,108-111). Interestingly, the addition of
extracellular catalase in vitro eliminates the antitumoral
effects of high-dose ascorbate almost completely and therefore
formation of extracellular H2O2 (112,113) seems to be a major contributor to
the antitumoral effects. The intracellular reactive oxygen species
formation appears to also affect cancer cells containing large
amounts of labile iron (28).
Furthermore, elevated iron levels identified in cancer cells
activate iron-dependent proteins that promote adaptation to hypoxia
and stimulate cell proliferation (114,115). The question whether ascorbate or
DHA is the most effective vitamin species was elucidated in cell
models (28,116,117) and showed that GLUT-mediated DHA
uptake does not play a major role in ascorbate toxicity. This is
biologically plausible, because DHA cannot form toxic
H2O2, extracellularly.
The metabolism of tumor cells differs from that of
normal cells with a shift from energy-producing pathways to those
generating macromolecules necessary for proliferation and tumor
growth, known as the Warburg effect. This is evident together with
hypoxia, a characteristic sign of solid tumors (120,121). Several mechanisms are involved
in the development of hypoxia causing significant heterogeneity in
the tissue oxygen levels in tumors (122). Adapting to an oxygen-depleted
microenvironment, tumors upregulate hypoxia inducible factors
(HIFs) and shift to an anaerobic energy production (123). Previous studies in patients with
brain cancer have already described an increase of the expression
of HIF-1 and GLUT-1 correlating to the malignancy grade (from
grades II to IV) (124-126). Previous findings on glioblastoma
cells showed a novel epigenetic mechanism underlying modulation of
HIF-1 transcriptional activity that enable cancer cells to rapidly
respond to hypoxic stress (127). A hypoxia-induced negative
feedback mechanism that maintains high activity of HIF-1 and cell
mobility in human glioblastoma cells has been suggested (112,127). Previous findings on breast
cancer tissue showed that higher vitamin C concentrations in tumor
tissue correlate with lower HIF-1 activity and increased
disease-free and disease-specific survival (128).
Importantly, ascorbate-dependent restoration seems
to play a role in cancer epigenetics. Given the fact that ectopic
overexpression of TET2 regulates neural differentiation in
glioblastoma cell lines and impairs tumor growth (13), it would be meaningful to assess
the effects of vitamin C in this process (129). Results of a recent randomized
clinical trial focusing on intravenous vitamin C, adjuvant to
decitabine, showed activation of TET2 in leukemic cells and
a significant improvement in overall survival in elderly patients
with acute myeloid leukemia (12).
Alteration in the differentiation potential of
cancer stem cells and blocking metastasis is also important
(130). Experiments with
different glioblastoma cells showed that changes of mitochondrial
oxidative and intracellular iron metabolism in combination with
pharmacological ascorbate treatment induces cancer cell selective
toxicity (28). Moreover, daily
pharmacologic ascorbate treatment significantly decreased growth
rates of gastric, ovarian, and pancreatic cancers as well as
glioblastoma established in mice (99,131-134). There are numerous studies
demonstrating the usage of pharmacological ascorbate as an adjuvant
to enhance radiation or chemotherapy responses (113,131,135-138). Millimolar concentrations of
ascorbate were able to induce pro-oxidative effects in the
interstitial fluid of the tumor cells mainly caused by
extracellular H2O2 formation resulting in DNA
damage in tumor cells and cellular adenosine triphosphate (ATP)
depletion. Furthermore, it was described that the ataxia
telangiectasia-mutated (ATM)/adenosine monophosphate-activated
protein kinase (AMPK) pathway was activated and the mammalian
target of rapamycin (mTOR) was inhibited in ovarian cancer cells
(99). The combination of
parenteral ascorbate with the conventional chemotherapeutics
carboplatin and paclitaxel synergistically inhibited the growth of
ovarian cancer in mouse models and reduced chemotherapy-associated
toxicity in patients with ovarian cancer by ascorbate treatment
(99).
Overall, it was evident that ascorbate was safe in
almost all patient populations and exhibited potential to reduce
toxicities of other cancer treatment regimens. The chemotherapeutic
potential of vitamin C requires high concentrations, which can only
be achieved intravenously. However, the IC50 values of
vitamin C against tumor cells determined in vitro vary
greatly depending on the tumor cell line employed. No conclusive
clinical data are yet available regarding the necessary
intra-venous amount. Most studies use a frequency of at least twice
weekly and doses of approximately 1 g per kg body weight (bw) with
promising results in solid tumors (96,97,141). One randomized controlled
clinical trial observed benefits with smaller amounts of 60-80
mg/kg bw in patients with acute myeloid leukemia (12). However, a small trial with doses
lower than 1 g/kg seemed to be therapeutically ineffective
(142). Considering different
cancer entities, applied chemotherapeutic agents and regimens of
radiation, the goal of most investigations was to achieve a plasma
concentration of approximately 22 mmol/l as described by Riordan
et al (49). The
therapeutic concentration and frequency in high-dose ascorbate
studies differed from 50 to 100 g and higher per day as infusion,
twice to three times weekly and the duration of treatment depended
on study design (141-145).
In addition to an overview on the clinical use of
vitamin C and its pharmacokinetics with an emphasis on
bioavailability in the CNS, this review focused also on the study
situation on high-dose intravenous ascorbate in oncology with
particular relevance to glioblastoma. Using the terms
'glioblastoma', 'glioma', and 'glioblastoma multiforme' as well as
'vitamin C', 'ascorbate', 'ascorbic acid', and 'pharmacological'
'intravenous', 'IV', and 'high-dose' in the following data sources
https://clinicaltrials.gov, https://www.clinicaltrialsregister.eu/ctr-search/search,
https://www.who.int/clinical-trials-registry-platform,
and https://www.ncbi for clinical trials, a total of
11 studies were identified (Table
I). Therefrom, intravenous ascorbate was found to be applied in
four phase I and II trials.
In the Phase I trial NCT01752491 (active, not
recruiting), the safety of high-dose ascorbate was tested in
combination with chemotherapy and temozolomide according to Stupp
et al (8) in a total of 13
study subjects. Only patients above 18 years of age were included
in that study. Thereby, dose escalation (15-125 g) was performed
for the radiation and for the adjuvant periods for each subsequent
study subject. Escalating weekly doses of ascorbate (up to 125 g)
to target a serum level of 350 mg/dl (20 mM) showed that
application of 87.5 g consistently resulted in plasma ascorbate
concentrations ≥20 mM (28,146). The absence of ascorbate-mediated
serious adverse events in neither the radiation nor adjuvant phase
enabled all subjects to maintain their performance status
throughout treatment. Overall, pharmacological ascorbate was well
tolerated and adverse events were restricted to dry mouth, fatigue,
nausea, vomiting, infection, leukopenia, and neutropenia (rendering
from grade 1-3, in total). The median overall survival was 18.3
months (146,147) compared to the historical median
of 14 months according to Stupp et al (8). Therefore, it was found that subjects
with unmethylated MGMT promoter as well as IDH wild type had longer
overall and progression-free survival compared to other study
participants. This treatment protocol for pharmacological ascorbate
was applied for one woman with glioblastoma in New Zealand
(147). She lived over four
years from glioblastoma diagnosis largely experiencing good quality
of life.
In the ongoing open-labeled, single group assigned
Phase II trial NCT02344355 (active, not recruiting), intra-venous
infusions of 87.5 g of ascorbate are administered three times
weekly during and after radiation. Additionally, ascorbate was
planned to be administered twice weekly through the end of cycle
six of temozolomide. The radiation and temozolomide treatments are
based on the previously conducted phase I study NCT01752491
(8,28,146). According to this protocol, the
overall and progression-free survival, the adverse event frequency
as well as the quality of life were to be evaluated in a cohort of
90 glioblastoma patients. In extension of the data from Schoenfeld
et al (28) and Allen
et al (146), Cushing
et al (148) established
an application using magnetic resonance imaging in humans to
visualize and measure changes in redox-active iron areas due to
pharmacological ascorbate. In a small sample-sized study, 15
subjects from NCT02344355 underwent optical imaging procedures
during application of high-dose ascorbate in addition to standard
of care treatment. Five glioblastoma patients without ascorbate
treatment were invited to participate as an active comparison group
in the study. Although without statistical significance, due to the
small number of subjects included in the study, the article
described a method that can be employed to monitor in vivo
changes in redox-active iron metabolism caused by the direct
manipulation of endogenous redox state of iron in cancer subjects,
which is in line with previous observations (28,134,148).
There are two more dose-escalation studies that
investigated intravenous ascorbate treatments in patients with
recurrent high-grade glioma (NCT02168270, NCT02833701), both
performed at the University of Nebraska. In the Phase I study, no.
NCT02833701, the role of bevacizumab and ascorbic acid was examined
in nine patients with recurrent high-grade glioma. In the Phase I
study, no. NCT02168270, temozolomide and ascorbic acid were tested
in four participants. In both trials, patients received ascorbate
intravenously over 90-120 min three times per week in addition to
bevacizumab or temozolomide, respectively. Treatment was repeated
every 28 days for up to 12 courses in the absence of disease
progression or unacceptable toxicity for each study. The primary
outcome measurements intended the determination of the
maximum-tolerated dose of intravenous ascorbate given three times
weekly in combination with temozolomide or bevacizumab and the
evaluation of adverse events. Secondly, overall and
progression-free survival, as well as quality of life were
evaluated for treated patients. According to the available data
sources, there are no dose-escalation protocols available for the
two studies (NCT02168270 and NCT02833701). Phase I study
NCT02168270 investigating the synergetic temozolomide and ascorbate
therapy procedure was terminated in 2018 due to lack of efficacy
and owing to non-completion of study protocol for all four
participants. Serious adverse events occurred in two individuals;
however, it was not specified if the serious adverse events were
ascorbate- or temozolomide-induced. For Phase I study NCT02833701,
which assessed the effects and best dose of ascorbate when given
together with bevacizumab, no results are published. Although both
clinical trials are already terminated there are no results about
detailed study outcomes publicly accessible (NCT02168270 in 2018
and NCT02833701 in 2019).
Notably, in the randomized Phase 2 clinical trial
NCT03503864, the therapeutic efficacy and toxicity of arsenic
trioxide in the treatment of patients with recurrent or refractory
stage 4 neuroblastoma was evaluated. This study is actually under
recruitment and is being conducted at Sun Yat-Sen University in
China. Owing to the study protocol patients are due to receive
chemotherapy combined with conventional induction therapy,
additionally for intravenous injection, arsenic trioxide and
simultaneously 0.5-1.0 g ascorbate in 5% glucose solution.
Treatment is scheduled every 28 days for a maximum of nine cycles
in the absence of disease progression or unacceptable toxicity.
Therefore, the focus has been on the 3-year overall survival rate,
progression-free survival, as well as incidence of adverse events.
The study outcomes from the experimental group, treated with
arsenic trioxide combined with induction chemotherapy, should be
compared with the results from the control group which only
received conventional induction chemotherapy without arsenic
trioxide.
In addition, there is a number of studies focusing
on oral ascorbate in high-grade re-occurrent glioma, glioblastoma,
low- and high-risk neuroblastoma or brain tumors (NCT01891747,
NCT04488783, NCT01811121, and NCT01502280). Admittedly, the
ingestion of orally administered ascorbate is tightly controlled,
and intravenous administration enables bypassing of the control
mechanisms and yields up to 100-fold higher plasma levels than
those possible with maximal oral dosing. With intravenous
administration, ascorbate is turned from vitamin to drug, acting as
a pro-drug for H2O2 in the extracellular
fluid, thereby having potential in the treatment of cancer
(57,149). Therefore, the discussion of
investigations with oral ascorbate supplementation is not in the
scope of this review. The same applies for the two studies using
palmitoyl ascorbate as excipient for rapamycin in the treatment of
relapsed or refractory high-risk neuroblastoma and pineoblastoma in
multimodal molecular-targeted therapy (NCT01467986 and
NCT02596828). Overall, clinical trials employing intravenous
vitamin C in critically ill patients (150-152) and patients with cancer (40,50,96,97,140) have demonstrated a lack of
toxicity, good safety, and tolerability (141). In the current study Phase I
(NCT01752491) (146) and one
case report (147) including
glioblastoma patients, encouraging evidence was provided that
receiving chemotherapy and radiotherapy together with high-dose
ascorbate is beneficial.
Early studies on glioblastoma have been generally
focused on the tumor-specific genetics and molecular profiles.
However, tumor cells are not isolated and grow in a particular
environment by communicating with other cell types, which
influences progression, aggression, and survival of cancer. New
investigations indicate that glioma cells interact in a complex way
with their microenvironment promoting their proliferation,
invasion, and treatment resistance (153).
Surrounding brain tumor-initiating cells are
microglia, which are resident brain-specific immune cells of the
CNS and distinct from peripheral circulating monocytes as well as
other macrophages that have infiltrated from the circulation
(154-158). These cells are believed to be
initially recruited to eliminate the tumor by stimulating apoptosis
of glioma cells (159) and by
secreting inflammatory factors that prevent glioma growth and
invasiveness (160). Under the
influence of glioblastoma, microglia and macrophages are
immunosuppressed and may contribute to glioblastoma invasion.
Martins et al suggested that the local modulation of
microglia within glioblastoma can control cancer cell progression
by rendering microglial cell tumor-phagocytosis (161). Moreover, deficits of vitamin C
in the brain have been observed in different neurological
conditions and disorders, including Parkinson's and Alzheimer's
disease, in which microglia pro-inflammatory activation influences
their onset and/or progression (161).
Radiation therapy is one of the three standard of
care components for glioblastoma. Radiation can kill proliferating
tumor cells and severely impact the tumor microenvironment by
altering the extra-cellular milieu at molecular and structural
levels (162-164). Independent groups have
documented enhanced human glioma cell migration and invasion in
response to radiation (165-169). Gupta et al identified
aggressive tumor behavior, microglial activation, and metabolic
alterations with an increase of energy carriers (ATP and GTP) in
the extracellular space as well as a decline in ascorbate in mice
after radiation (170). Thus,
microglia were observed to be amoeboid with higher phagocytic
activity after radiation. In regard to the metabolic and
morphologic changes in the radiated microenvironment,
administration of ascorbate was suggested as an opportunity to
decrease radiation-associated aggressiveness of recurrent
glioblastoma and to enhance the long-term safety of brain radiation
treatment for glioblastoma (170). SVCT2-deficient mice showed
decreased ascorbate levels in the brain with a marked increase in
cognitive deficits, amyloid β accumulation, and oxidative stress
(171). Portugal et al
showed that reduced vitamin C uptake through SVCT2 triggers the
activation of primary rodent and human microglia. Thus, modulation
of SVCT2 or vitamin C supply may be an attractive strategy for
restoring microglia homeostasis and promoting neuronal viability
(172). Moreover, mitochondrial
SVCT2 was previously described in U937 cells (173) and HEK293 cells (174) and it was also observed in
various cancer-derived cell lines from different origin (175). This observation was also
correlated with cancer pathology (175) and absent in normal cells,
suggesting that mitochondrial vitamin C may be relevant for cancer
cell development or survival (176).
The BBB is a specialized non-permeable barrier in
cerebral microvessels. Tight junctions between endothelial cells in
brain capillaries are the most prominent characteristic of the BBB
and are responsible for its selectivity (177). Higher supplementation of vitamin
C in an in vivo mouse model revealed two times longer tight
junctions than in low-dose supplemented animals (178). Behind the regeneration of DHA,
derived from neuronal cells or delivered from blood, astrocytes
also control BBB tightness. When these astrocytes become malignant
as astrocytoma cells or are even turned into glioblastoma cells,
the conditions within the brain become complex (179).
Aquaporins (AQPs) have been described as crucial
controllers of the BBB integrity and play an important role in
cancer (180). Experimental
evidence depicts that some AQPs also allow the transport of
H2O2 through biological membranes. These AQPs
are termed peroxiporins (181).
Unlike normal cells, which are relatively unaffected by ascorbate,
cancer cells exhibit a wide range of susceptibility depending on
their catalase activity and plasma membrane permeability to
H2O2. Erudaitius et al demonstrated
that peroxiporin expression is an important factor for cancer cell
susceptibility to therapeutic H2O2 (106). This suggests that cell
susceptibility to ascorbate therapy is closely related to plasma
membrane permeability to H2O2 in accordance
with an elevated expression of peroxiporins. Therefore, modulation
of plasma membrane is an option to increase the permeability of
ascorbate. AQP1 and AQP4 upregulation which was observed in
gliomas, glioblastomas, and also glioblastoma stem-like cells is
believed to increase the perivascular space observed in gliomas
(182-184). As H2O2 is
known to be formed extracellularly as a byproduct of ascorbate
oxidation and then permeating into the intracellular space through
peroxiporin channeling (27,103), the efficacy of pharmacological
ascorbate therapy (185) in
glioblastoma may depend on the presence of
H2O2 and on peroxiporins to pass through the
plasma membrane, respectively.
It is possible that ascorbate delivery or uptake
into the cell is also altered due to vascular dysfunction and
disorganization (186). GLUT1
and to a lesser extent GLUT3 may be promising targets for
glioblastoma treatment. The Warburg Effect occurring in cancer
cells, is characterized by an extreme increase of glycolysis
thereby decreasing the dependence on oxidative phosphorylation.
Expression of GLUT1 and GLUT3 in glioblastoma tissue is often
markedly altered (184,187,188). Co-culture experiments in the
presence of ascorbate showed that tumor cells from CNS cells were
able to acquire vitamin C via SVCT2; however, compared with normal
cells, the capacity for ascorbate uptake was much lower in tumor
cells (189). In this regard, it
is important to emphasize that the main form of vitamin C found
after co-culture was ascorbate, meaning cancer cells are able to
efficiently reduce DHA once inside the cell (175). Additionally, the competitive
inhibition of GLUT transporters in glioblastoma cell lines did not
suppress the ascorbate-induced toxicity suggesting that DHA is not
the cancer cell-selective toxic species in this model (26,28,102,190). Reactive astrocytes generated
following brain injury, neuroinflammation, stroke, aging, or
neurodegenerative diseases, were able to induce SVCT2 expression,
probably as a neuroprotective strategy for oxidative defense
(191). On the other hand,
reactive astrocytes release cytokines, chemokines, interleukins,
nitric oxide, and other molecules, thereby promoting
neuroinflammation (192) and the
development of tumor microenvironment (155,189). Whether SVCT2 expression and
function in reactive astrocytes may be considered a potential
target for future clinical treatments remains to be further
investigated.
The mechanism by which SVCT2 is upregulated in
brain tissue is poorly understood. It has been observed that SVCT2
mRNA levels increase in neurons and astrocytes following oxidative
damage due to ischemia and reperfusion (193). These findings underscore the
importance of ascorbate as a neuroprotective agent and may have
implications for therapeutic strategies. Induction of CNS
inflammation resulted in the internalization and degradation of
SVCT2 in microglia followed by the activation of NFκB (172). In C2C12 cells, it has been
determined that the activation of NFκB and AP-1 would increase
SVCT2 expression under conditions of oxidative stress generated by
H2O2 (194). However, the whole picture of the
interactions between microglia, astrocytes from tumor-unaffected
regions, activated astrocytes, brain tumor-initiating cells,
neurons, and tumor cells requires further exploration in
glioblastoma patients and after treatment with high-dose
ascorbate.
Despite advances in surgical techniques, radiation
therapy, and chemotherapy, effective treatment of glioblastoma
remains an unresolved challenge (8) (Fig.
3). In general, oncologic patients have decreased vitamin C
levels, which are likely due to enhanced metabolic turnover as a
result of oxidative and inflammatory aspects of the disease process
(195). Nevertheless, the role
of vitamin C in cancer patients is not fully clarified (73,196,197). Enhanced oxidative stress and
pro-inflammatory biomarkers can also result from chemotherapy
(198,199) or radiation (170). At present, only a small number
of studies including glioblastoma patients and testing ascorbate as
a potential therapeutic agent are available. The combination of
pharmacological ascorbate with radiation and temozolomide provides
hope to improve the patient's treatment performance as well as to
ameliorate their life quality (47,146).
There is strong evidence that the effects of
high-dose ascorbate treatment in glioma are not only restricted to
general anti-oxidative effects that protect non-malignant and
non-brain cells from the cytotoxic effects of chemotherapy and
radiation (26,28,29,32). Additional investigations are
required to explore whether adjuvant ascorbate therapy is also
beneficial or even conflicting in combination with immunotherapy or
oncolytic virotherapy treatment approaches.
Nevertheless, adjuvant high-dose ascorbate
treatment in glioblastoma patients seems to be a promising
therapeutic option that is able to improve the survival and quality
of life of glioblastoma patients according to the available data
from in vitro and in vivo studies. As the application
of intravenous infusion is a routine standard procedure in the
hospitalized patient's treatment, administration of pharmacological
ascorbate requires no additional expertise for the staff, even more
because the intravenous solutions are notably stable at ambient
temperature (208).
Not applicable.
OR, MB, TS, and SV wrote and conceived the
manuscript. OR and MB carried out the literature and study research
and generated the figures. HM and CV revised the manuscript. All
authors read and approved the final manuscript. OR and MB confirm
the authenticity of the data.
Not applicable.
Not applicable.
OR, MB, TS, and SV declare that they have no
competing interests. CV and HM, as employees of Pascoe
Pharmazeutische Praeparate GmbH (Giessen, Germany), received the
ready designed/written manuscript for their review and were not
involved in the content-related structuring. Furthermore, CV and HM
had no influence on the content and interpretation of the
literature used.
We thank Christian Leischner and Andreas Burkard
for their excellent technical support. We further acknowledge
support by the Open Access Publishing Fund of University of
Tuebingen.
SV and MB were supported by the Else-Uebelmesser-Stiftung (grant
no. D.30.21947) and the Ministry for Rural Affairs and Consumer
Protection Baden-Wuerttemberg (grant no. 14-(34)-0802/0402 E). SV
and TS were supported by a grant from Pascoe pharmazeutische
Praeparate GmbH (grant no. D.24.01029). CV and HM are employed at
Pascoe Pharmazeutische Praeparate GmbH (Giessen, Germany).
|
1
|
Louis DN, Perry A, Reifenberger G, von
Deimling A, Figarella-Branger D, Cavenee WK, Ohgaki H, Wiestler OD,
Kleihues P and Ellison DW: The 2016 world health organization
classification of tumors of the central nervous system: A summary.
Acta Neuropathol. 131:803–820. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Silantyev AS, Falzone L, Libra M, Gurina
OI, Kardashova KS, Nikolouzakis TK, Nosyrev AE, Sutton CW, Mitsias
PD and Tsatsakis A: Current and future trends on diagnosis and
prognosis of glioblastoma: From molecular biology to proteomics.
Cells. 8:8632019. View Article : Google Scholar :
|
|
3
|
Candido S, Lupo G, Pennisi M, Basile MS,
Anfuso CD, Petralia MC, Gattuso G, Vivarelli S, Spandidos DA, Libra
M and Falzone L: The analysis of miRNA expression profiling
datasets reveals inverse microRNA patterns in glioblastoma and
Alzheimer's disease. Oncol Rep. 42:911–922. 2019.PubMed/NCBI
|
|
4
|
Armento A, Ehlers J, Schötterl S and
Naumann U: Molecular mechanisms of glioma cell motility.
Glioblastoma. De Vleeschouwer S: Codon Publications; Brisbane:
2017, View Article : Google Scholar
|
|
5
|
Tabatabai G and Wakimoto H: Glioblastoma:
State of the Art and future perspectives. Cancers (Basel).
11:10912019. View Article : Google Scholar
|
|
6
|
Ohgaki H and Kleihues P: Epidemiology and
etiology of gliomas. Acta Neuropathol. 109:93–108. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ostrom QT, Gittleman H, Stetson L, Virk S
and Barnholtz-Sloan JS: Epidemiology of intracranial gliomas. Prog
Neurol Surg. 30:1–11. 2018. View Article : Google Scholar
|
|
8
|
Stupp R, Mason WP, van den Bent MJ, Weller
M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn
U, et al: Radiotherapy plus concomitant and adjuvant temozolomide
for glioblastoma. N Engl J Med. 352:987–996. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Weller M, Butowski N, Tran DD, Recht LD,
Lim M, Hirte H, Ashby L, Mechtler L, Goldlust SA, Iwamoto F, et al:
Rindopepimut with temozolomide for patients with newly diagnosed,
EGFRvIII-expressing glioblastoma (ACT IV): A randomised,
double-blind, international phase 3 trial. Lancet Oncol.
18:1373–1385. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Tian M, Ma W, Chen Y, Yu Y, Zhu D, Shi J
and Zhang Y: Impact of gender on the survival of patients with
glioblastoma. Biosci Rep. Nov 7–2018.Epub ahead of print.
View Article : Google Scholar
|
|
11
|
Brat DJ, Aldape K, Colman H, Holland EC,
Louis DN, Jenkins RB, Kleinschmidt-DeMasters BK, Perry A,
Reifenberger G, Stupp R, et al: cIMPACT-NOW update 3: Recommended
diagnostic criteria for 'Diffuse astrocytic glioma, IDH-wildtype,
with molecular features of glioblastoma, WHO grade IV'. Acta
Neuropathol. 136:805–810. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Zhao H, Zhu H, Huang J, Zhu Y, Hong M, Zhu
H, Zhang J, Li S, Yang L, Lian Y, et al: The synergy of vitamin C
with decitabine activates TET2 in leukemic cells and significantly
improves overall survival in elderly patients with acute myeloid
leukemia. Leuk Res. 66:1–7. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
García MG, Carella A, Urdinguio RG, Bayón
GF, Lopez V, Tejedor JR, Sierra MI, García-Toraño E, Santamarina P,
Perez RF, et al: Epigenetic dysregulation of TET2 in human
glioblastoma. Oncotarget. 9:25922–25934. 2018. View Article : Google Scholar :
|
|
14
|
Mansouri A, Hachem LD, Mansouri S, Nassiri
F, Laperriere NJ, Xia D, Lindeman NI, Wen PY, Chakravarti A, Mehta
MP, et al: MGMT promoter methylation status testing to guide
therapy for glioblastoma: Refining the approach based on emerging
evidence and current challenges. Neuro Oncol. 21:167–178. 2019.
View Article : Google Scholar :
|
|
15
|
Stummer W, Pichlmeier U, Meinel T,
Wiestler OD, Zanella F and Reulen HJ; ALA-Glioma Study Group:
Fluorescence-guided surgery with 5-aminolevulinic acid for
resection of malignant glioma: A randomised controlled multicentre
phase III trial. Lancet Oncol. 7:392–401. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Pichlmeier U, Bink A and Schackert G:
Resection and survival in glioblastoma multiforme: An RTOG
recursive partitioning analysis of ALA study patients. Neuro Oncol.
10:1025–1034. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Abd-El-Barr MM and Chiocca EA: How much is
enough? The question of extent of resection in glioblastoma
multiforme. World Neurosurg. 82:e109–e110. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ryken TC, Parney I, Buatti J, Kalkanis SN
and Olson JJ: The role of radiotherapy in the management of
patients with diffuse low grade glioma: A systematic review and
evidence-based clinical practice guideline. J Neurooncol.
125:551–583. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Niyazi M, Brada M, Chalmers AJ, Combs SE,
Erridge SC, Fiorentino A, Grosu AL, Lagerwaard FJ, Minniti G,
Mirimanoff RO, et al: ESTRO-ACROP guideline 'target delineation of
glioblastomas'. Radiother Oncol. 118:35–42. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Wick W, Platten M, Meisner C, Felsberg J,
Tabatabai G, Simon M, Nikkhah G, Papsdorf K, Steinbach JP, Sabel M,
et al: Temozolomide chemotherapy alone versus radiotherapy alone
for malignant astrocytoma in the elderly: The NOA-08 randomised,
phase 3 trial. Lancet Oncol. 13:707–715. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Rusthoven CG, Koshy M and Sher DJ:
Radiation plus temozolomide in patients with glioblastoma. N Engl J
Med. 376:2195–2197. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Perry JR, Laperriere N, O'Callaghan CJ,
Brandes AA, Menten J, Phillips C, Fay M, Nishikawa R, Cairncross
JG, Roa W, et al: Short-course radiation plus temozolomide in
elderly patients with glioblastoma. N Engl J Med. 376:1027–1037.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
McGranahan T, Therkelsen KE, Ahmad S and
Nagpal S: Current state of immunotherapy for treatment of
glioblastoma. Curr Treat Options Oncol. 20:242019. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Rominiyi O, Vanderlinden A, Clenton SJ,
Bridgewater C, Al-Tamimi Y and Collis SJ: Tumour treating fields
therapy for glioblastoma: Current advances and future directions.
Br J Cancer. 124:697–709. 2021. View Article : Google Scholar
|
|
25
|
Geletneky K, Hajda J, Angelova AL, Leuchs
B, Capper D, Bartsch AJ, Neumann JO, Schöning T, Hüsing J, Beelte
B, et al: Oncolytic H-1 parvovirus shows safety and signs of
immunogenic activity in a first phase I/IIa glioblastoma trial. Mol
Ther. 25:2620–2634. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Chen Q, Espey MG, Krishna MC, Mitchell JB,
Corpe CP, Buettner GR, Shacter E and Levine M: Pharmacologic
ascorbic acid concentrations selectively kill cancer cells: Action
as a prodrug to deliver hydrogen peroxide to tissues. Proc Natl
Acad Sci USA. 102:13604–13609. 2005. View Article : Google Scholar
|
|
27
|
Chen Q, Espey MG, Sun AY, Lee JH, Krishna
MC, Shacter E, Choyke PL, Pooput C, Kirk KL, Buettner GR and Levine
M: Ascorbate in pharmacologic concentrations selectively generates
ascorbate radical and hydrogen peroxide in extracellular fluid in
vivo. Proc Natl Acad Sci USA. 104:8749–8754. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Schoenfeld JD, Sibenaller ZA, Mapuskar KA,
Wagner BA, Cramer-Morales KL, Furqan M, Sandhu S, Carlisle TL,
Smith MC, Abu Hejleh T, et al: O2− and
H2O2-mediated disruption of fe metabolism
causes the differential susceptibility of NSCLC and GBM cancer
cells to pharmacological ascorbate. Cancer Cell. 32:2682017.
View Article : Google Scholar
|
|
29
|
Klingelhoeffer C, Kämmerer U, Koospal M,
Mühling B, Schneider M, Kapp M, Kübler A, Germer CT and Otto C:
Natural resistance to ascorbic acid induced oxidative stress is
mainly mediated by catalase activity in human cancer cells and
catalase-silencing sensitizes to oxidative stress. BMC Complement
Altern Med. 12:612012. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Sauberlich HE: Pharmacology of vitamin C.
Annu Rev Nutr. 14:371–391. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Nishikimi M and Yagi K: Molecular basis
for the deficiency in humans of gulonolactone oxidase, a key enzyme
for ascorbic acid biosynthesis. Am J Clin Nutr. 54(Suppl 6):
1203S–1208S. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Padayatty SJ and Levine M: Vitamin C: The
known and the unknown and goldilocks. Oral Dis. 22:463–493. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Carr A and Frei B: Does vitamin C act as a
pro-oxidant under physiological conditions? FASEB J. 13:1007–1024.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Levine M, Wang Y, Katz A, Eck P, Kwon O,
Chen S, Lee JH and Padayatty SJ: Ideal vitamin C intake.
Biofactors. 15:71–74. 2001. View Article : Google Scholar
|
|
35
|
Carr AC and Lykkesfeldt J: Discrepancies
in global vitamin C recommendations: A review of RDA criteria and
underlying health perspectives. Crit Rev Food Sci Nutr. 61:742–755.
2021. View Article : Google Scholar
|
|
36
|
Levine M, Conry-Cantilena C, Wang Y, Welch
RW, Washko PW, Dhariwal KR, Park JB, Lazarev A, Graumlich JF, King
J and Cantilena LR: Vitamin C pharmacokinetics in healthy
volunteers: Evidence for a recommended dietary allowance. Proc Natl
Acad Sci USA. 93:3704–3709. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Hoffer LJ, Levine M, Assouline S,
Melnychuk D, Padayatty SJ, Rosadiuk K, Rousseau C, Robitaille L and
Miller WH Jr: Phase I clinical trial of i.v. ascorbic acid in
advanced malignancy. Ann Oncol. 19:1969–1974. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Padayatty SJ, Sun AY, Chen Q, Espey MG,
Drisko J and Levine M: Vitamin C: Intravenous use by complementary
and alternative medicine practitioners and adverse effects. PLoS
One. 5:e114142010. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Nielsen TK, Højgaard M, Andersen JT,
Poulsen HE, Lykkesfeldt J and Mikines KJ: Elimination of ascorbic
acid after high-dose infusion in prostate cancer patients: A
pharmacokinetic evaluation. Basic Clin Pharmacol Toxicol.
116:343–348. 2015. View Article : Google Scholar
|
|
40
|
Stephenson CM, Levin RD, Spector T and Lis
CG: Phase I clinical trial to evaluate the safety, tolerability,
and pharmacokinetics of high-dose intravenous ascorbic acid in
patients with advanced cancer. Cancer Chemother Pharmacol.
72:139–146. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Torun M, Yardim S, Gönenç A, Sargin H,
Menevşe A and Símşek B: Serum beta-carotene, vitamin E, vitamin C
and malondialdehyde levels in several types of cancer. J Clin Pharm
Ther. 20:259–263. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Mahdavi R, Faramarzi E, Seyedrezazadeh E,
Mohammad-Zadeh M and Pourmoghaddam M: Evaluation of oxidative
stress, antioxidant status and serum vitamin C levels in cancer
patients. Biol Trace Elem Res. 130:1–6. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Sharma A, Tripathi M, Satyam A and Kumar
L: Study of antioxidant levels in patients with multiple myeloma.
Leuk Lymphoma. 50:809–815. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Emri S, Kilickap S, Kadilar C, Halil MG,
Akay H and Besler T: Serum levels of alpha-tocopherol, vitamin C,
beta-carotene, and retinol in malignant pleural mesothelioma. Asian
Pac J Cancer Prev. 13:3025–3029. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Mehdi WA, Zainulabdeen JA and Mehde AA:
Investigation of the antioxidant status in multiple myeloma
patients: Effects of therapy. Asian Pac J Cancer Prev.
14:3663–3667. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Huijskens MJ, Wodzig WK, Walczak M,
Germeraad WT and Bos GM: Ascorbic acid serum levels are reduced in
patients with hematological malignancies. Results Immunol. 6:8–10.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Fain O, Mathieu E and Thomas M: Scurvy in
patients with cancer. BMJ. 316:1661–1662. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Mayland CR, Bennett MI and Allan K:
Vitamin C deficiency in cancer patients. Palliat Med. 19:17–20.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Riordan HD, Riordan NH, Jackson JA,
Casciari JJ, Hunninghake R, González MJ, Mora EM, Miranda-Massari
JR, Rosario N and Rivera A: Intravenous vitamin C as a
chemo-therapy agent: A report on clinical cases. P R Health Sci J.
23:115–118. 2004.PubMed/NCBI
|
|
50
|
Hoffer LJ, Robitaille L, Zakarian R,
Melnychuk D, Kavan P, Agulnik J, Cohen V, Small D and Miller WH Jr:
High-dose intravenous vitamin C combined with cytotoxic
chemotherapy in patients with advanced cancer: A phase I-II
clinical trial. PLoS One. 10:e01202282015. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Liu M, Ohtani H, Zhou W, Ørskov AD,
Charlet J, Zhang YW, Shen H, Baylin SB, Liang G, Grønbæk K and
Jones PA: Vitamin C increases viral mimicry induced by
5-aza-2′-deoxycytidine. Proc Natl Acad Sci USA. 113:10238–10244.
2016. View Article : Google Scholar
|
|
52
|
Shenoy N, Bhagat T, Nieves E, Stenson M,
Lawson J, Choudhary GS, Habermann T, Nowakowski G, Singh R, Wu X,
et al: Upregulation of TET activity with ascorbic acid induces
epigenetic modulation of lymphoma cells. Blood Cancer J.
7:e5872017. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Anthony HM and Schorah CJ: Severe
hypovitaminosis C in lung-cancer patients: The utilization of
vitamin C in surgical repair and lymphocyte-related host
resistance. Br J Cancer. 46:354–367. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Ramaswamy G and Krishnamoorthy L: Serum
carotene, vitamin A, and vitamin C levels in breast cancer and
cancer of the uterine cervix. Nutr Cancer. 25:173–177. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Khanzode SS, Muddeshwar MG, Khanzode SD
and Dakhale GN: Antioxidant enzymes and lipid peroxidation in
different stages of breast cancer. Free Radic Res. 38:81–85. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Popa-Wagner A, Mitran S, Sivanesan S,
Chang E and Buga AM: ROS and brain diseases: The good, the bad, and
the ugly. Oxid Med Cell Longev. 2013:9635202013. View Article : Google Scholar
|
|
57
|
Levine M, Padayatty SJ and Espey MG:
Vitamin C: A concentration-function approach yields pharmacology
and therapeutic discoveries. Adv Nutr. 2:78–88. 2011. View Article : Google Scholar :
|
|
58
|
Du J, Cullen JJ and Buettner GR: Ascorbic
acid: Chemistry, biology and the treatment of cancer. Biochim
Biophys Acta. 1826:443–457. 2012.PubMed/NCBI
|
|
59
|
Harrison FE and May JM: Vitamin C function
in the brain: Vital role of the ascorbate transporter SVCT2. Free
Radic Biol Med. 46:719–730. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Kaźmierczak-Barańska J, Boguszewska K,
Adamus-Grabicka A and Karwowski BT: Two faces of vitamin
C-antioxidative and pro-oxidative agent. Nutrients. 12:15012020.
View Article : Google Scholar
|
|
61
|
Lykkesfeldt J and Tveden-Nyborg P: The
pharmacokinetics of vitamin C. Nutrients. 11:24122019. View Article : Google Scholar :
|
|
62
|
Abbott NJ: Dynamics of CNS barriers:
Evolution, differentiation, and modulation. Cell Mol Neurobiol.
25:5–23. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Nualart F, Mack L, García A, Cisternas P,
Bongarzone ER, Heitzer M, Jara N, Martínez F, Ferrada L, Espinoza
F, et al: Vitamin C transporters, recycling and the bystander
effect in the nervous system: SVCT2 versus gluts. J Stem Cell Res
Ther. 4:2092014. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Angelow S, Haselbach M and Galla HJ:
Functional characterisation of the active ascorbic acid transport
into cerebrospinal fluid using primary cultured choroid plexus
cells. Brain Res. 988:105–113. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Haselbach M, Wegener J, Decker S,
Engelbertz C and Galla HJ: Porcine choroid plexus epithelial cells
in culture: Regulation of barrier properties and transport
processes. Microsc Res Tech. 52:137–152. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Shi LZ, Li GJ, Wang S and Zheng W: Use of
Z310 cells as an in vitro blood-cerebrospinal fluid barrier model:
Tight junction proteins and transport properties. Toxicol In Vitro.
22:190–199. 2008. View Article : Google Scholar
|
|
67
|
Strazielle N and Ghersi-Egea JF:
Demonstration of a coupled metabolism-efflux process at the choroid
plexus as a mechanism of brain protection toward xenobiotics. J
Neurosci. 19:6275–6289. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Sotiriou S, Gispert S, Cheng J, Wang Y,
Chen A, Hoogstraten-Miller S, Miller GF, Kwon O, Levine M,
Guttentag SH and Nussbaum RL: Ascorbic-acid transporter Slc23a1 is
essential for vitamin C transport into the brain and for perinatal
survival. Nat Med. 8:514–517. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Tsukaguchi H, Tokui T, Mackenzie B, Berger
UV, Chen XZ, Wang Y, Brubaker RF and Hediger MA: A family of
mammalian Na+-dependent L-ascorbic acid transporters. Nature.
399:70–75. 1999. View
Article : Google Scholar : PubMed/NCBI
|
|
70
|
Daruwala R, Song J, Koh WS, Rumsey SC and
Levine M: Cloning and functional characterization of the human
sodium-dependent vitamin C transporters hSVCT1 and hSVCT2. FEBS
Lett. 460:480–484. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Wang D, Christensen K, Chawla K, Xiao G,
Krebsbach PH and Franceschi RT: Isolation and characterization of
MC3T3-E1 preosteoblast subclones with distinct in vitro and in vivo
differentiation/mineralization potential. J Bone Miner Res.
14:893–903. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Wang Y, Mackenzie B, Tsukaguchi H,
Weremowicz S, Morton CC and Hediger MA: Human vitamin C (L-ascorbic
acid) transporter SVCT1. Biochem Biophys Res Commun. 267:488–494.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Wohlrab C, Phillips E and Dachs GU:
Vitamin C transporters in cancer: Current understanding and gaps in
knowledge. Front Oncol. 7:742017. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Agus DB, Gambhir SS, Pardridge WM,
Spielholz C, Baselga J, Vera JC and Golde DW: Vitamin C crosses the
blood-brain barrier in the oxidized form through the glucose
transporters. J Clin Invest. 100:2842–2848. 1997. View Article : Google Scholar
|
|
75
|
Ho HTB, Dahlin A and Wang J: Expression
profiling of solute carrier gene families at the blood-CSF barrier.
Front Pharmacol. 3:1542012. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Bürzle M, Suzuki Y, Ackermann D, Miyazaki
H, Maeda N, Clémençon B, Burrier R and Hediger MA: The
sodium-dependent ascorbic acid transporter family SLC23. Mol
Aspects Med. 34:436–454. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Rice ME: Ascorbate regulation and its
neuroprotective role in the brain. Trends Neurosci. 23:209–216.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Spector R, Keep RF, Robert Snodgrass S,
Smith QR and Johanson CE: A balanced view of choroid plexus
structure and function: Focus on adult humans. Exp Neurol.
267:78–86. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Mun GH, Kim MJ, Lee JH, Kim HJ, Chung YH,
Chung YB, Kang JS, Hwang YI, Oh SH, Kim JG, et al:
Immunohistochemical study of the distribution of sodium-dependent
vitamin C trans-porters in adult rat brain. J Neurosci Res.
83:919–928. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Ulloa V, García-Robles M, Martínez F,
Salazar K, Reinicke K, Pérez F, Godoy DF, Godoy AS and Nualart F:
Human choroid plexus papilloma cells efficiently transport glucose
and vitamin C. J Neurochem. 127:403–414. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Rice M and Russo-Menna I: Differential
compartmentalization of brain ascorbate and glutathione between
neurons and glia. Neuroscience. 82:1213–1223. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Castro M, Caprile T, Astuya A, Millán C,
Reinicke K, Vera JC, Vásquez O, Aguayo LG and Nualart F:
High-affinity sodium-vitamin C co-transporters (SVCT) expression in
embryonic mouse neurons. J Neurochem. 78:815–823. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Nualart FJ, Rivas CI, Montecinos VP, Godoy
AS, Guaiquil VH, Golde DW and Vera JC: Recycling of vitamin C by a
bystander effect. J Biol Chem. 278:10128–10133. 2003. View Article : Google Scholar
|
|
84
|
Kaufman S: Coenzymes and hydroxylases:
Ascorbate and dopamine-beta-hydroxylase; tetrahydropteridines and
phenyl-alanine and tyrosine hydroxylases. Pharmacol Rev. 18:61–69.
1966.PubMed/NCBI
|
|
85
|
Eipper BA, Milgram SL, Husten EJ, Yun HY
and Mains RE: Peptidylglycine alpha-amidating monooxygenase: A
multifunctional protein with catalytic, processing, and routing
domains. Protein Sci. 2:489–497. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Eldridge CF, Bunge MB, Bunge RP and Wood
PM: Differentiation of axon-related Schwann cells in vitro. I.
Ascorbic acid regulates basal lamina assembly and myelin formation.
J Cell Biol. 105:1023–1034. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Qiu S, Li L, Weeber EJ and May JM:
Ascorbate transport by primary cultured neurons and its role in
neuronal function and protection against excitotoxicity. J Neurosci
Res. 85:1046–1056. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Rebec GV and Pierce RC: A vitamin as
neuromodulator: Ascorbate release into the extracellular fluid of
the brain regulates dopaminergic and glutamatergic transmission.
Prog Neurobiol. 43:537–565. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Pastor P, Cisternas P, Salazar K,
Silva-Alvarez C, Oyarce K, Jara N, Espinoza F, Martínez AD and
Nualart F: SVCT2 vitamin C transporter expression in progenitor
cells of the post-natal neurogenic niche. Front Cell Neurosci.
7:1192013. View Article : Google Scholar
|
|
90
|
Oyarce K, Bongarzone ER and Nualart F:
Unconventional neurogenic niches and neurogenesis modulation by
vitamins. J Stem Cell Res Ther. 4:1842014.PubMed/NCBI
|
|
91
|
Davson H and Oldendorf WH: Symposium on
membrane transport. Transport in the central nervous system. Proc R
Soc Med. 60:326–329. 1967.PubMed/NCBI
|
|
92
|
Reiber H, Ruff M and Uhr M: Ascorbate
concentration in human cerebrospinal fluid (CSF) and serum.
Intrathecal accumulation and CSF flow rate. Clinica Chimica Acta.
217:163–173. 1993. View Article : Google Scholar
|
|
93
|
Cameron E and Pauling L: Supplemental
ascorbate in the supportive treatment of cancer: Prolongation of
survival times in terminal human cancer. Proc Natl Acad Sci USA.
73:3685–3689. 1976. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Creagan ET, Moertel CG, O'Fallon JR,
Schutt AJ, O'Connell MJ, Rubin J and Frytak S: Failure of high-dose
vitamin C (ascorbic acid) therapy to benefit patients with advanced
cancer. A controlled trial. N Engl J Med. 301:687–690. 1979.
View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Moertel CG, Fleming TR, Creagan ET, Rubin
J, O'Connell MJ and Ames MM: High-dose vitamin C versus placebo in
the treatment of patients with advanced cancer who have had no
prior chemotherapy. A randomized double-blind comparison. N Engl J
Med. 312:137–141. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Monti DA, Mitchell E, Bazzan AJ, Littman
S, Zabrecky G, Yeo CJ, Pillai MV, Newberg AB, Deshmukh S and Levine
M: Phase I evaluation of intravenous ascorbic acid in combination
with gemcitabine and erlotinib in patients with metastatic
pancreatic cancer. PLoS One. 7:e297942012. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Welsh JL, Wagner BA, van't Erve TJ, Zehr
PS, Berg DJ, Halfdanarson TR, Yee NS, Bodeker KL, Du J, Roberts LJ
II, et al: Pharmacological ascorbate with gemcitabine for the
control of metastatic and node-positive pancreatic cancer (PACMAN):
Results from a phase I clinical trial. Cancer Chemother Pharmacol.
71:765–775. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Herst PM, Broadley KWR, Harper JL and
McConnell MJ: Pharmacological concentrations of ascorbate
radiosensitize glio-blastoma multiforme primary cells by increasing
oxidative DNA damage and inhibiting G2/M arrest. Free Radic Biol
Med. 52:1486–1493. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Ma Y, Chapman J, Levine M, Polireddy K,
Drisko J and Chen Q: High-dose parenteral ascorbate enhanced
chemosensitivity of ovarian cancer and reduced toxicity of
chemotherapy. Sci Transl Med. 6:222ra182014. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Fritz H, Flower G, Weeks L, Cooley K,
Callachan M, McGowan J, Skidmore B, Kirchner L and Seely D:
Intravenous vitamin C and cancer: A systematic review. Integr
Cancer Ther. 13:280–300. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Carr AC and Cook J: Intravenous vitamin C
for cancer therapy-identifying the current gaps in our knowledge.
Front Physiol. 9:11822018. View Article : Google Scholar
|
|
102
|
Violet PC and Levine M: Pharmacologic
ascorbate in myeloma treatment: Doses matter. EBioMedicine.
18:9–10. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Schoenfeld JD, Alexander MS, Waldron TJ,
Sibenaller ZA, Spitz DR, Buettner GR, Allen BG and Cullen JJ:
Pharmacological ascorbate as a means of sensitizing cancer cells to
radio-chemo-therapy while protecting normal tissue. Semin Radiat
Oncol. 29:25–32. 2019. View Article : Google Scholar
|
|
104
|
Bienert GP, Schjoerring JK and Jahn TP:
Membrane transport of hydrogen peroxide. Biochim Biophys Acta.
1758:994–1003. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Bienert GP, Møller AL, Kristiansen KA,
Schulz A, Møller IM, Schjoerring JK and Jahn TP: Specific
aquaporins facilitate the diffusion of hydrogen peroxide across
membranes. J Biol Chem. 282:1183–1192. 2007. View Article : Google Scholar
|
|
106
|
Erudaitius D, Huang A, Kazmi S, Buettner
GR and Rodgers VG: Peroxiporin expression is an important factor
for cancer cell susceptibility to therapeutic
H2O2: Implications for pharmacological
ascorbate therapy. PLoS One. 12:e01704422017. View Article : Google Scholar
|
|
107
|
Deubzer B, Mayer F, Kuçi Z, Niewisch M,
Merkel G, Handgretinger R and Bruchelt G: H(2)O(2)-mediated
cytotoxicity of pharmacologic ascorbate concentrations to
neuroblastoma cells: Potential role of lactate and ferritin. Cell
Physiol Biochem. 25:767–774. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Olney KE, Du J, van 't Erve TJ, Witmer JR,
Sibenaller ZA, Wagner BA, Buettner GR and Cullen JJ: Inhibitors of
hydroperoxide metabolism enhance ascorbate-induced cytotoxicity.
Free Radic Res. 47:154–163. 2013. View Article : Google Scholar :
|
|
109
|
Du J, Martin SM, Levine M, Wagner BA,
Buettner GR, Wang S, Taghiyev AF, Du C, Knudson CM and Cullen JJ:
Mechanisms of ascorbate-induced cytotoxicity in pancreatic cancer.
Clin Cancer Res. 16:509–520. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Ibrahim WH, Habib HM, Kamal H, St Clair DK
and Chow CK: Mitochondrial superoxide mediates labile iron level:
Evidence from Mn-SOD-transgenic mice and heterozygous knockout mice
and isolated rat liver mitochondria. Free Radic Biol Med.
65:143–149. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Doskey CM, Buranasudja V, Wagner BA,
Wilkes JG, Du J, Cullen JJ and Buettner GR: Tumor cells have
decreased ability to metabolize H2O2:
Implications for pharmacological ascorbate in cancer therapy. Redox
Biol. 10:274–284. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Sinnberg T, Noor S, Venturelli S, Berger
A, Schuler P, Garbe C and Busch C: The ROS-induced cytotoxicity of
ascorbate is attenuated by hypoxia and HIF-1alpha in the NCI60
cancer cell lines. J Cell Mol Med. 18:530–541. 2014. View Article : Google Scholar :
|
|
113
|
Du J, Cieslak JA III, Welsh JL, Sibenaller
ZA, Allen BG, Wagner BA, Kalen AL, Doskey CM, Strother RK, Button
AM, et al: Pharmacological ascorbate radiosensitizes pancreatic
cancer. Cancer Res. 75:3314–3326. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Torti SV and Torti FM: Iron and cancer:
More ore to be mined. Nat Rev Cancer. 13:342–355. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Uetaki M, Tabata S, Nakasuka F, Soga T and
Tomita M: Metabolomic alterations in human cancer cells by vitamin
C-induced oxidative stress. Sci Rep. 5:138962015. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
El Banna N, Hatem E, Heneman-Masurel A,
Léger T, Baïlle D, Vernis L, Garcia C, Martineau S, Dupuy C, Vagner
S, et al: Redox modifications of cysteine-containing proteins, cell
cycle arrest and translation inhibition: Involvement in vitamin
C-induced breast cancer cell death. Redox Biol. 26:1012902019.
View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Frömberg A, Gutsch D, Schulze D,
Vollbracht C, Weiss G, Czubayko F and Aigner A: Ascorbate exerts
anti-proliferative effects through cell cycle inhibition and
sensitizes tumor cells towards cytostatic drugs. Cancer Chemother
Pharmacol. 67:1157–1166. 2011. View Article : Google Scholar :
|
|
118
|
Marklund SL, Westman NG, Lundgren E and
Roos G: Copper- and zinc-containing superoxide dismutase,
manganese-containing superoxide dismutase, catalase, and
glutathione peroxidase in normal and neoplastic human cell lines
and normal human tissues. Cancer Res. 42:1955–1961. 1982.PubMed/NCBI
|
|
119
|
Johnson RM, Ho YS, Yu DY, Kuypers FA,
Ravindranath Y and Goyette GW: The effects of disruption of genes
for peroxire-doxin-2, glutathione peroxidase-1, and catalase on
erythrocyte oxidative metabolism. Free Radic Biol Med. 48:519–525.
2010. View Article : Google Scholar
|
|
120
|
Vaupel P, Höckel M and Mayer A: Detection
and characterization of tumor hypoxia using pO2 histography.
Antioxid Redox Signal. 9:1221–1235. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Moulder JE and Rockwell S: Hypoxic
fractions of solid tumors: Experimental techniques, methods of
analysis, and a survey of existing data. Int J Radiat Oncol Biol
Phys. 10:695–712. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Vaupel P, Mayer A and Höckel M: Tumor
hypoxia and malignant progression. Methods Enzymol. 381:335–354.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Zeng W, Liu P, Pan W, Singh SR and Wei Y:
Hypoxia and hypoxia inducible factors in tumor metabolism. Cancer
Lett. 356:263–267. 2015. View Article : Google Scholar
|
|
124
|
Korkolopoulou P, Patsouris E,
Konstantinidou AE, Pavlopoulos PM, Kavantzas N, Boviatsis E,
Thymara I, Perdiki M, Thomas-Tsagli E, Angelidakis D, et al:
Hypoxia-inducible factor 1alpha/vascular endothelial growth factor
axis in astrocytomas. Associations with microvessel morphometry,
proliferation and prognosis. Neuropathol Appl Neurobiol.
30:267–278. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Mashiko R, Takano S, Ishikawa E, Yamamoto
T, Nakai K and Matsumura A: Hypoxia-inducible factor 1α expression
is a prognostic biomarker in patients with astrocytic tumors
associated with necrosis on MR image. J Neurooncol. 102:43–50.
2011. View Article : Google Scholar
|
|
126
|
Søndergaard KL, Hilton DA, Penney M,
Ollerenshaw M and Demaine AG: Expression of hypoxia-inducible
factor 1alpha in tumours of patients with glioblastoma. Neuropathol
Appl Neurobiol. 28:210–217. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Bao L, Chen Y, Lai HT, Wu SY, Wang JE,
Hatanpaa KJ, Raisanen JM, Fontenot M, Lega B, Chiang CM, et al:
Methylation of hypoxia-inducible factor (HIF)-1α by G9a/GLP
inhibits HIF-1 transcriptional activity and cell migration. Nucleic
Acids Res. 46:6576–6591. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Campbell EJ, Dachs GU, Morrin HR, Davey
VC, Robinson BA and Vissers MCM: Activation of the hypoxia pathway
in breast cancer tissue and patient survival are inversely
associated with tumor ascorbate levels. BMC Cancer. 19:3072019.
View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Camarena V and Wang G: The epigenetic role
of vitamin C in health and disease. Cell Mol Life Sci.
73:1645–1658. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Satheesh NJ, Samuel SM and Büsselberg D:
Combination therapy with vitamin c could eradicate cancer stem
cells. Biomolecules. 10:792020. View Article : Google Scholar :
|
|
131
|
O'Leary BR, Houwen FK, Johnson CL, Allen
BG, Mezhir JJ, Berg DJ, Cullen JJ and Spitz DR: Pharmacological
ascorbate as an adjuvant for enhancing radiation-chemotherapy
responses in gastric adenocarcinoma. Radiat Res. 189:456–465. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Espey MG, Chen P, Chalmers B, Drisko J,
Sun AY, Levine M and Chen Q: Pharmacologic ascorbate synergizes
with gemcitabine in preclinical models of pancreatic cancer. Free
Radic Biol Med. 50:1610–1619. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Moser JC, Rawal M, Wagner BA, Du J, Cullen
JJ and Buettner GR: Pharmacological ascorbate and ionizing
radiation (IR) increase labile iron in pancreatic cancer. Redox
Biol. 2:22–27. 2013. View Article : Google Scholar
|
|
134
|
Chen Q, Espey MG, Sun AY, Pooput C, Kirk
KL, Krishna MC, Khosh DB, Drisko J and Levine M: Pharmacologic
doses of ascorbate act as a prooxidant and decrease growth of
aggressive tumor xenografts in mice. Proc Natl Acad Sci USA.
105:11105–11109. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
135
|
Lu YX, Wu QN, Chen DL, Chen LZ, Wang ZX,
Ren C, Mo HY, Chen Y, Sheng H, Wang YN, et al: Pharmacological
ascorbate suppresses growth of gastric cancer cells with GLUT1
overexpression and enhances the efficacy of oxaliplatin through
redox modulation. Theranostics. 8:1312–1326. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Oka N, Komuro A, Amano H, Dash S, Honda M,
Ota K, Nishimura S, Ueda T, Akagi M and Okada H: Ascorbate
sensitizes human osteosarcoma cells to the cytostatic effects of
cisplatin. Pharmacol Res Perspect. 8:e006322020. View Article : Google Scholar : PubMed/NCBI
|
|
137
|
Kanter M and Akpolat M: Vitamin C protects
against ionizing radiation damage to goblet cells of the ileum in
rats. Acta Histochem. 110:481–490. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Ito Y, Kinoshita M, Yamamoto T, Sato T,
Obara T, Saitoh D, Seki S and Takahashi Y: A combination of pre-
and post-exposure ascorbic acid rescues mice from radiation-induced
lethal gastrointestinal damage. Int J Mol Sci. 14:19618–19635.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
139
|
Vollbracht C, Schneider B, Leendert V,
Weiss G, Auerbach L and Beuth J: Intravenous vitamin C
administration improves quality of life in breast cancer patients
during chemo-/radiotherapy and aftercare: Results of a
retrospective, multicentre, epidemiological cohort study in
Germany. In Vivo. 25:983–990. 2011.PubMed/NCBI
|
|
140
|
Polireddy K, Dong R, Reed G, Yu J, Chen P,
Williamson S, Violet PC, Pessetto Z, Godwin AK, Fan F, et al: High
dose parenteral ascorbate inhibited pancreatic cancer growth and
metastasis: Mechanisms and a phase I/IIa study. Sci Rep.
7:171882017. View Article : Google Scholar : PubMed/NCBI
|
|
141
|
Nauman G, Gray JC, Parkinson R, Levine M
and Paller CJ: Systematic review of intravenous ascorbate in cancer
clinical trials. Antioxidants (Basel). 7:892018. View Article : Google Scholar
|
|
142
|
Nielsen TK, Højgaard M, Andersen JT,
Jørgensen NR, Zerahn B, Kristensen B, Henriksen T, Lykkesfeldt J,
Mikines KJ and Poulsen HE: Weekly ascorbic acid infusion in
castration-resistant prostate cancer patients: A single-arm phase
II trial. Transl Androl Urol. 6:517–528. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
143
|
Wang F, He MM, Wang ZX, Li S, Jin Y, Ren
C, Shi SM, Bi BT, Chen SZ, Lv ZD, et al: Phase I study of high-dose
ascorbic acid with mFOLFOX6 or FOLFIRI in patients with metastatic
colorectal cancer or gastric cancer. BMC Cancer. 19:4602019.
View Article : Google Scholar : PubMed/NCBI
|
|
144
|
Alexander MS, Wilkes JG, Schroeder SR,
Buettner GR, Wagner BA, Du J, Gibson-Corley K, O'Leary BR, Spitz
DR, Buatti JM, et al: Pharmacologic ascorbate reduces
radiation-induced normal tissue toxicity and enhances tumor
radiosensitization in pancreatic cancer. Cancer Res. 78:6838–6851.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
145
|
Ou J, Zhu X, Chen P, Du Y, Lu Y, Peng X,
Bao S, Wang J, Zhang X, Zhang T and Pang CLK: A randomized phase II
trial of best supportive care with or without hyperthermia and
vitamin C for heavily pretreated, advanced, refractory
non-small-cell lung cancer. J Adv Res. 24:175–182. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
146
|
Allen BG, Bodeker KL, Smith MC, Monga V,
Sandhu S, Hohl R, Carlisle T, Brown H, Hollenbeck N, Vollstedt S,
et al: First-in-human phase I clinical trial of pharmacologic
ascorbate combined with radiation and temozolomide for newly
diagnosed glioblastoma. Clin Cancer Res. 25:6590–6597. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
147
|
Baillie N, Carr AC and Peng S: The use of
intravenous vitamin C as a supportive therapy for a patient with
glioblastoma multiforme. Antioxidants (Basel). 7:1152018.
View Article : Google Scholar
|
|
148
|
Cushing CM, Petronek MS, Bodeker KL,
Vollstedt S, Brown HA, Opat E, Hollenbeck NJ, Shanks T, Berg DJ,
Smith BJ, et al: Magnetic resonance imaging (MRI) of
pharmacological ascorbate-induced iron redox state as a biomarker
in subjects undergoing radio-chemotherapy. Redox Biol.
38:1018042021. View Article : Google Scholar
|
|
149
|
Padayatty SJ, Sun H, Wang Y, Riordan HD,
Hewitt SM, Katz A, Wesley RA and Levine M: Vitamin C
pharmacokinetics: Implications for oral and intravenous use. Ann
Intern Med. 140:533–537. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
150
|
Fowler AA III, Syed AA, Knowlson S,
Sculthorpe R, Farthing D, DeWilde C, Farthing CA, Larus TL, Martin
E, Brophy DF, et al: Phase I safety trial of intravenous ascorbic
acid in patients with severe sepsis. J Transl Med. 12:322014.
View Article : Google Scholar : PubMed/NCBI
|
|
151
|
Zabet MH, Mohammadi M, Ramezani M and
Khalili H: Effect of high-dose ascorbic acid on vasopressor's
requirement in septic shock. J Res Pharm Pract. 5:94–100. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
152
|
Tanaka H, Matsuda T, Miyagantani Y,
Yukioka T, Matsuda H and Shimazaki S: Reduction of resuscitation
fluid volumes in severely burned patients using ascorbic acid
administration: A randomized, prospective study. Arch Surg.
135:326–331. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
153
|
Li G, Qin Z, Chen Z, Xie L, Wang R and
Zhao H: Tumor microenvironment in treatment of glioma. Open Med
(Wars). 12:247–251. 2017. View Article : Google Scholar
|
|
154
|
Ginhoux F, Greter M, Leboeuf M, Nandi S,
See P, Gokhan S, Mehler MF, Conway SJ, Ng LG, Stanley ER, et al:
Fate mapping analysis reveals that adult microglia derive from
primitive macrophages. Science. 330:841–845. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
155
|
Charles NA, Holland EC, Gilbertson R,
Glass R and Kettenmann H: The brain tumor microenvironment. Glia.
60:502–514. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
156
|
Poon CC, Sarkar S, Yong VW and Kelly JJP:
Glioblastoma-associated microglia and macrophages: Targets for
therapies to improve prognosis. Brain. 140:1548–1560. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
157
|
Poon CC, Gordon PMK, Liu K, Yang R, Sarkar
S, Mirzaei R, Ahmad ST, Hughes ML, Yong VW and Kelly JJP:
Differential microglia and macrophage profiles in human IDH-mutant
and -wild type glioblastoma. Oncotarget. 10:3129–3143. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
158
|
Tomaszewski W, Sanchez-Perez L, Gajewski
TF and Sampson JH: Brain tumor microenvironment and host state:
Implications for immunotherapy. Clin Cancer Res. 25:4202–4210.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
159
|
Hwang SY, Yoo BC, Jung J, Oh ES, Hwang JS,
Shin JA, Kim SY, Cha SH and Han IO: Induction of glioma apoptosis
by microglia-secreted molecules: The role of nitric oxide and
cathepsin B. Biochim Biophys Acta. 1793:1656–1668. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
160
|
Chicoine MR, Zahner M, Won EK, Kalra RR,
Kitamura T, Perry A and Higashikubo R: The in vivo antitumoral
effects of lipopolysaccharide against glioblastoma multiforme are
mediated in part by Toll-like receptor 4. Neurosurgery. 60:372–381.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
161
|
Martins TA, Schmassmann P, Shekarian T,
Boulay JL, Ritz MF, Zanganeh S, vom Berg J and Hutter G:
Microglia-centered combinatorial strategies against glioblastoma.
Front Immunol. 11:5719512020. View Article : Google Scholar : PubMed/NCBI
|
|
162
|
Gupta K and Burns TC: Radiation-induced
alterations in the recurrent glioblastoma microenvironment:
Therapeutic implications. Front Oncol. 8:5032018. View Article : Google Scholar : PubMed/NCBI
|
|
163
|
Yoshimura M, Itasaka S, Harada H and
Hiraoka M: Micro-environment and radiation therapy. Biomed Res Int.
2013:6853082013. View Article : Google Scholar
|
|
164
|
Bellail AC, Hunter SB, Brat DJ, Tan C and
van Meir EG: Microregional extracellular matrix heterogeneity in
brain modulates glioma cell invasion. Int J Biochem Cell Biol.
36:1046–1069. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
165
|
Wild-Bode C, Weller M, Rimner A, Dichgans
J and Wick W: Sublethal irradiation promotes migration and
invasiveness of glioma cells: Implications for radiotherapy of
human glioblastoma. Cancer Res. 61:2744–2750. 2001.PubMed/NCBI
|
|
166
|
Shankar A, Kumar S, Iskander AS, Varma NR,
Janic B, deCarvalho A, Mikkelsen T, Frank JA, Ali MM, Knight RA, et
al: Subcurative radiation significantly increases cell
proliferation, invasion, and migration of primary glioblastoma
multiforme in vivo. Chin J Cancer. 33:148–158. 2014. View Article : Google Scholar :
|
|
167
|
Wank M, Schilling D, Reindl J, Meyer B,
Gempt J, Motov S, Alexander F, Wilkens JJ, Schlegel J, Schmid TE
and Combs SE: Evaluation of radiation-related invasion in primary
patient-derived glioma cells and validation with established cell
lines: Impact of different radiation qualities with differing LET.
J Neurooncol. 139:583–590. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
168
|
Wank M, Schilling D, Schmid TE, Meyer B,
Gempt J, Barz M, Schlegel J, Liesche F, Kessel KA, Wiestler B, et
al: Human glioma migration and infiltration properties as a target
for personalized radiation medicine. Cancers (Basel). 10:4562018.
View Article : Google Scholar
|
|
169
|
Zhang X, Wang X, Xu R, Ji J, Xu Y, Han M,
Wei Y, Huang B, Chen A, Zhang Q, et al: YM155 decreases
radiation-induced invasion and reverses epithelial-mesenchymal
transition by targeting STAT3 in glioblastoma. J Transl Med.
16:792018. View Article : Google Scholar : PubMed/NCBI
|
|
170
|
Gupta K, Vuckovic I, Zhang S, Xiong Y,
Carlson BL, Jacobs J, Olson I, Petterson XM, Macura SI, Sarkaria J
and Burns TC: Radiation induced metabolic alterations associate
with tumor aggressiveness and poor outcome in glioblastoma. Front
Oncol. 10:5352020. View Article : Google Scholar : PubMed/NCBI
|
|
171
|
Dixit S, Bernardo A, Walker JM, Kennard
JA, Kim GY, Kessler ES and Harrison FE: Vitamin C deficiency in the
brain impairs cognition, increases amyloid accumulation and
deposition, and oxidative stress in APP/PSEN1 and normally aging
mice. ACS Chem Neurosci. 6:570–581. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
172
|
Portugal CC, Socodato R and Relvas JB: The
ascorbate transporter SVCT2 to target microglia-dependent
inflammation. Oncotarget. 8:99217–99218. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
173
|
Azzolini C, Fiorani M, Cerioni L,
Guidarelli A and Cantoni O: Sodium-dependent transport of ascorbic
acid in U937 cell mitochondria. IUBMB Life. 65:149–153. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
174
|
Muñoz-Montesino C, Roa FJ, Peña E,
González M, Sotomayor K, Inostroza E, Muñoz CA, González I,
Maldonado M, Soliz C, et al: Mitochondrial ascorbic acid transport
is mediated by a low-affinity form of the sodium-coupled ascorbic
acid transporter-2. Free Radic Biol Med. 70:241–254. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
175
|
Peña E, Roa FJ, Inostroza E, Sotomayor K,
González M, Gutierrez-Castro FA, Maurin M, Sweet K, Labrousse C,
Gatica M, et al: Increased expression of mitochondrial
sodium-coupled ascorbic acid transporter-2 (mitSVCT2) as a central
feature in breast cancer. Free Radic Biol Med. 135:283–292. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
176
|
Roa FJ, Peña E, Gatica M, Escobar-Acuña K,
Saavedra P, Maldonado M, Cuevas ME, Moraga-Cid G, Rivas CI and
Muñoz-Montesino C: Therapeutic use of vitamin C in cancer:
Physiological considerations. Front Pharmacol. 11:2112020.
View Article : Google Scholar : PubMed/NCBI
|
|
177
|
McCaffrey G, Staatz WD, Quigley CA, Nametz
N, Seelbach MJ, Campos CR, Brooks TA, Egleton RD and Davis TP:
Tight junctions contain oligomeric protein assembly critical for
maintaining blood-brain barrier integrity in vivo. J Neurochem.
103:2540–2555. 2007.PubMed/NCBI
|
|
178
|
Kook SY, Lee KM, Kim Y, Cha MY, Kang S,
Baik SH, Lee H, Park R and Mook-Jung I: High-dose of vitamin C
supplementation reduces amyloid plaque burden and ameliorates
pathological changes in the brain of 5XFAD mice. Cell Death Dis.
5:e10832014. View Article : Google Scholar : PubMed/NCBI
|
|
179
|
Dubois LG, Campanati L, Righy C,
D'Andrea-Meira I, Spohr TC, Porto-Carreiro I, Pereira CM,
Balça-Silva J, Kahn SA, DosSantos MF, et al: Gliomas and the
vascular fragility of the blood brain barrier. Front Cell Neurosci.
8:4182014. View Article : Google Scholar
|
|
180
|
Prata C, Hrelia S and Fiorentini D:
Peroxiporins in cancer. Int J Mol Sci. 20:13712019. View Article : Google Scholar :
|
|
181
|
Henzler T and Steudle E: Transport and
metabolic degradation of hydrogen peroxide in Chara corallina:
Model calculations and measurements with the pressure probe suggest
transport of H(2)O(2) across water channels. J Exp Bot.
51:2053–2066. 2000. View Article : Google Scholar
|
|
182
|
Noell S, Ritz R, Wolburg-Buchholz K,
Wolburg H and Fallier-Becker P: An allograft glioma model reveals
the depen-dence of aquaporin-4 expression on the brain
microenvironment. PLoS One. 7:e365552012. View Article : Google Scholar
|
|
183
|
Warth A, Kröger S and Wolburg H:
Redistribution of aqua-porin-4 in human glioblastoma correlates
with loss of agrin immunoreactivity from brain capillary basal
laminae. Acta Neuropathol. 107:311–318. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
184
|
Markert JM, Fuller CM, Gillespie GY,
Bubien JK, McLean LA, Hong RL, Lee K, Gullans SR, Mapstone TB and
Benos DJ: Differential gene expression profiling in human brain
tumors. Physiol Genomics. 5:21–33. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
185
|
Papadopoulos MC and Saadoun S: Key roles
of aquaporins in tumor biology. Biochim Biophys Acta.
1848:2576–2583. 2015. View Article : Google Scholar
|
|
186
|
Labak CM, Wang PY, Arora R, Guda MR,
Asuthkar S, Tsung AJ and Velpula KK: Glucose transport: Meeting the
metabolic demands of cancer, and applications in glioblastoma
treatment. Am J Cancer Res. 6:1599–1608. 2016.PubMed/NCBI
|
|
187
|
Castro MA, Pozo M, Cortés C, García Mde L,
Concha II and Nualart F: Intracellular ascorbic acid inhibits
transport of glucose by neurons, but not by astrocytes. J
Neurochem. 102:773–782. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
188
|
Azzalin A, Nato G, Parmigiani E, Garello
F, Buffo A and Magrassi L: Inhibitors of GLUT/SLC2A enhance the
action of BCNU and temozolomide against high-grade gliomas.
Neoplasia. 19:364–373. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
189
|
Astuya A, Caprile T, Castro M, Salazar K,
García Mde L, Reinicke K, Rodríguez F, Vera JC, Millán C, Ulloa V,
et al: Vitamin C uptake and recycling among normal and tumor cells
from the central nervous system. J Neurosci Res. 79:146–156. 2005.
View Article : Google Scholar
|
|
190
|
Chen S, Roffey DM, Dion CA, Arab A and Wai
EK: Effect of perioperative vitamin C supplementation on
postoperative pain and the incidence of chronic regional pain
syndrome: A systematic review and meta-analysis. Clin J Pain.
32:179–185. 2016. View Article : Google Scholar
|
|
191
|
Salazar K, Martínez F, Pérez-Martín M,
Cifuentes M, Trigueros L, Ferrada L, Espinoza F, Saldivia N,
Bertinat R, Forman K, et al: SVCT2 expression and function in
reactive astrocytes is a common event in different brain
pathologies. Mol Neurobiol. 55:5439–5452. 2018. View Article : Google Scholar
|
|
192
|
Heneka MT, Carson MJ, El Khoury J,
Landreth GE, Brosseron F, Feinstein DL, Jacobs AH, Wyss-Coray T,
Vitorica J, Ransohoff RM, et al: Neuroinflammation in Alzheimer's
disease. Lancet Neurol. 14:388–405. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
193
|
Berger UV, Lu XC, Liu W, Tang Z, Slusher
BS and Hediger MA: Effect of middle cerebral artery occlusion on
mRNA expression for the sodium-coupled vitamin C transporter SVCT2
in rat brain. J Neurochem. 86:896–906. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
194
|
Savini I, Rossi A, Catani MV, Ceci R and
Avigliano L: Redox regulation of vitamin C transporter SVCT2 in
C2C12 myotubes. Biochem Biophys Res Commun. 361:385–390. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
195
|
Reuter S, Gupta SC, Chaturvedi MM and
Aggarwal BB: Oxidative stress, inflammation, and cancer: How are
they linked? Free Radic Biol Med. 49:1603–1616. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
196
|
Harris HR, Orsini N and Wolk A: Vitamin C
and survival among women with breast cancer: A meta-analysis. Eur J
Cancer. 50:1223–1231. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
197
|
Wilson MK, Baguley BC, Wall C, Jameson MB
and Findlay MP: Review of high-dose intravenous vitamin C as an
anticancer agent. Asia Pac J Clin Oncol. 10:22–37. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
198
|
Hunnisett A, Davies S, McLaren-Howard J,
Gravett P, Finn M and Gueret-Wardle D: Lipoperoxides as an index of
free radical activity in bone marrow transplant recipients.
Preliminary observations. Biol Trace Elem Res. 47:125–132. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
199
|
Nan-Ya K, Kajihara M, Kojima N and Degawa
M: Usefulness of urinary kidney injury molecule-1 (Kim-1) as a
biomarker for cisplatin-induced sub-chronic kidney injury. J Appl
Toxicol. 35:124–132. 2015. View Article : Google Scholar
|
|
200
|
Schoenfeld JD, Sibenaller ZA, Mapuskar KA,
Wagner BA, Cramer-Morales KL, Furqan M, Sandhu S, Carlisle TL,
Smith MC, Abu Hejleh T, et al: O2− and
H2O2-mediated disruption of fe metabolism
causes the differential susceptibility of NSCLC and GBM cancer
cells to pharmacological ascorbate. Cancer Cell. 31:487–500.e8.
2017. View Article : Google Scholar
|
|
201
|
Attia M, Essa EA, Zaki RM and Elkordy AA:
An overview of the antioxidant effects of ascorbic acid and alpha
lipoic acid (in liposomal forms) as adjuvant in cancer treatment.
Antioxidants (Basel). 9:3592020. View Article : Google Scholar
|
|
202
|
Milletti F: Cell-penetrating peptides:
Classes, origin, and current landscape. Drug Discov Today.
17:850–860. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
203
|
Hultqvist G, Syvänen S, Fang XT, Lannfelt
L and Sehlin D: Bivalent brain shuttle increases antibody uptake by
monovalent binding to the transferrin receptor. Theranostics.
7:308–318. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
204
|
Staquicini FI, Ozawa MG, Moya CA, Driessen
WH, Barbu EM, Nishimori H, Soghomonyan S, Flores LG, Liang X II,
Paolillo V, et al: Systemic combinatorial peptide selection yields
a non-canonical iron-mimicry mechanism for targeting tumors in a
mouse model of human glioblastoma. J Clin Invest. 121:161–173.
2011. View Article : Google Scholar :
|
|
205
|
Tong HI, Kang W, Davy PM, Shi Y, Sun S,
Allsopp RC and Lu Y: Monocyte trafficking, engraftment, and
delivery of nanoparticles and an exogenous gene into the acutely
inflamed brain tissue-evaluations on monocyte-based delivery system
for the central nervous system. PLoS One. 11:e01540222016.
View Article : Google Scholar
|
|
206
|
Di Tacchio M, Macas J, Weissenberger J,
Sommer K, Bähr O, Steinbach JP, Senft C, Seifert V, Glas M,
Herrlinger U, et al: Tumor vessel normalization, immunostimulatory
reprogramming, and improved survival in glioblastoma with combined
inhibition of PD-1, angiopoietin-2, and VEGF. Cancer Immunol Res.
7:1910–1927. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
207
|
Przystal JM, Waramit S, Pranjol MZI, Yan
W, Chu G, Chongchai A, Samarth G, Olaciregui NG, Tabatabai G,
Carcaboso AM, et al: Efficacy of systemic temozolomide-activated
phage-targeted gene therapy in human glioblastoma. EMBO Mol Med.
11:e84922019. View Article : Google Scholar : PubMed/NCBI
|
|
208
|
Carr A, Wohlrab C, Young P and Bellomo R:
Stability of intravenous vitamin C solutions: A technical report.
Crit Care Resusc. 20:180–181. 2018.PubMed/NCBI
|