Lung cancer has the highest mortality rate worldwide
and seriously affects patients' health (1). According to National Cancer Center of
China statistics, 733,300 new cases of NSCLC were reported in 2015
and there were ~610,200 related deaths (2). According to GLOBOCAN 2020, 820,000
new cases of lung cancer were reported in China in 2020, accounting
for ~18% of all new cancer cases. In addition, the total number of
lung cancer deaths far exceeded that of other cancer types,
comprising ~23.8% of the total number of cancer-associated deaths
(1). Over the past decade, the
increase in lung cancer-related deaths in China has exceeded the
global average (3,4).
Non-small cell lung cancer (NSCLC) accounts for ~85%
of lung cancer cases and is the most common pathological type of
lung cancer, including adenocarcinoma and squamous cell carcinoma
(5). Surgery is the main treatment
modality for early-stage NSCLC (6). With recent developments in modern
medicine, continuous promotion of lung cancer screening and
improvements in health awareness, early-stage lung cancer has been
more readily detected. Thus, patients' operative and survival rates
have also improved. Furthermore, more attention has been paid to
improving the quality of life of patients postoperatively (7). In recent years, thoracoscopy
technology has developed rapidly and has considerable diagnostic
and therapeutic benefits in treating various respiratory diseases.
Thoracoscopy is the first choice of treatment for lung cancer due
to its low postoperative pain and complications. Among the
treatment methods, thoracoscopic lobectomy has become the main
treatment method for early-stage NSCLC, as it results in less
intraoperative bleeding and pain and comparatively fewer
complications (8-10).
Although thoracoscopic lobectomy is more conducive
to patient recovery, the probability of various complications after
thoracoscopic surgery remains high at 15.8-31.7%, mainly involving
pulmonary air and pleural effusion such that, when taking into
account the different stages of cancer, 25-70% of patients
eventually relapse (11-13). The complication rate for
thoracoscopic lobectomy due to sputum retention and weakened
respiratory muscle strength is as high as 19-59%, which seriously
affects patient recovery (14).
Given pulmonary rehabilitation of patients with NSCLC is currently
sub-optimal, the present study aimed to summarize the existing
pulmonary rehabilitation programs to help clinicians determine
better rehabilitation methods for patients with NSCLC.
The lung cancer stage, which is closely related to
the surgical method, determines whether a patient may undergo
surgery and affects surgical outcomes.
Accurate lung cancer staging is an important aspect
of patient treatment, with early diagnosis and lung cancer stage
being the most important factors influencing the treatment plan
(15). Between 1943 and 1952,
Denoix conceptualized tumor-node-metastasis (TNM) staging (16). The International Association for
the Study of Lung Cancer is the only global organization dedicated
to lung cancer study and is responsible for collating, analyzing
and updating cancer data (17).
TNM staging for lung cancer is currently in its 8th edition, with
data collected from 1999 to 2010 and the newest edition released in
2017. Compared with the 7th edition, the main differences are in
relation to tumor size, the extent of involvement and
subclassification of extrathoracic metastases (18). T staging is determined according to
the size of the tumor and its relationship with adjacent
structures, lymph node staging is determined by assessing the
regional hilar and mediastinal lymph nodes and M staging indicates
whether there is metastasis outside of the regional lymph nodes
(19).
In summary, the clinical stages of NSCLC may be
divided into four stages, according to the 8th edition of TNM lung
cancer staging: Stages I and II are early-stage NSCLCs, which
include T1-3N0M0 and
T1-2N1M0. Stages III and IV are
locally advanced and advanced NSCLCs, which include
T4N0M0,
T3-4N1-3M0, and
T1-4N0-3M1a-1c (20,21).
The appropriate treatment strategy depends on the degree of
mediastinal lymph node involvement, which determines whether the
tumor is resected alone or in combination with chemoradiotherapy or
immunotherapy (Table I) (22-26).
The sharp increase in the number of patients with early-stage NSCLC
and the reduction in the number of patients with locally advanced
and advanced NSCLC may be explained as follows: With increased
health awareness, there has been an increase in the number of
patients undergoing physical examinations. However, improved
medical care also depends on high computed tomography resolution
and the use of other advanced instruments and equipment.
In thoracoscopic lobectomy, the surgeon uses a
thoracoscope to observe the status of the chest cavity in real-time
on a television screen. Surgery is performed using between one and
four incisions ≤5 cm (without opening the ribs) with complete
lobectomy (27,28). Video-assisted thoracic surgery
(VATS) lobectomy has become the technique of choice for resection
of early-stage lung cancer at numerous institutions. In the
National Comprehensive Cancer Network NSCLC guidelines, there is a
call for 'strong consideration' of VATS lobectomy (27,29).
Treatment-intent pneumonectomy should be considered for stage I
lung cancer. Several studies have suggested that segmentectomy
should be strongly considered for tumors <2 cm in size, as the
results are comparable to lobectomy and the approach is similar for
tumors measuring 2.1-3 cm (30-33).
In addition, certain studies have demonstrated the efficacy of
sublobar resection for solid predominant tumors ≤2 cm (34,35).
Patients with stage II lung cancer also benefit from surgical
resection; however, there is insufficient evidence concerning the
optimal extent of surgical resection, and adjuvant chemotherapy
with a platinum-containing dual-drug regimen as a treatment for
stage IIB lung cancer has also been recommended (36). A recent retrospective study
provided inconclusive results regarding sublobar resection vs.
lobectomy in this patient population (37). Patients with stage III lung cancer
benefit from a multidisciplinary evaluation, including
pneumonectomy, neoadjuvant therapy and immunotherapy, which is a
comprehensive treatment regime (38,39).
For locally advanced lung cancer or patients with stage IV disease,
where lobectomy, bilobectomy or sleeve lobectomy cannot completely
resect tumors, VATS pneumonectomy is the first treatment of choice,
which is similar to open pneumonectomy, or opting for an integrated
and personalized application of immunotherapy (40). While guidelines or expert consensus
provide reference standards, each patient differs and should be
considered on an individual basis.
VATS is a thoracic surgical procedure that uses a
small camera to enter a patient's chest through a small incision.
It is currently the main surgical method in thoracic surgery
(41). In a comparison of VATS
with open lobectomy, VATS was indicated to have several advantages.
VATS has been associated with reduced pain and blood transfusions,
a shorter duration of chest tube intubation and hospital stay, and
fewer perioperative complications and arrhythmias. VATS is one of
the most recommended surgical methods for treating lung cancer
(Table II) (42,43).
Compared to the open lobectomy in terms of rehabilitation,
thoracoscopic lobectomy has more advantages in length of stay (6
vs. 4 days) and chest tube duration (4 vs. 3 days). In 2007, in
relation to treating phase I and II NSCLC, the American College of
Chest Physicians identified VATS lobectomy as an acceptable
alternative to thoracoscopic surgery (44).
With recent developments in thoracoscopy technology,
surgeons performing VATS have gradually switched from the use of
multiple incisions to double incisions, with one incision used as
an observation hole and the other used to perform the procedure. In
single utility port thoracoscopic surgery, one surgical incision is
made for observation and to perform the operation. In general, the
efficacy of VATS in the treatment of lung cancer is comparable to
standard thoracotomy (45-47). Single utility port thoracoscopic
surgery is suitable for T-stage T1-T3 (grade
II) and N-stage N0-N2 (grade I) lung cancer
(43,48). Single utility port thoracoscopic
lung surgery has the following advantages: Less bleeding, a shorter
operative time and faster recovery than standard multiport
thoracoscopic surgery (49,50).
However, the postoperative complication rate for single utility
port thoracoscopic surgery has been reported to be between 3 and
40% (51). Several recent studies
have investigated how to best select the location of the
single-hole thoracoscopic incision and whether to place a drainage
tube to improve the surgical effect (52-55).
Decisions made concerning whether to perform single or multiple
incisions or whether to place a drainage tube or not vary from
patient to patient, in relation to promoting rapid recovery.
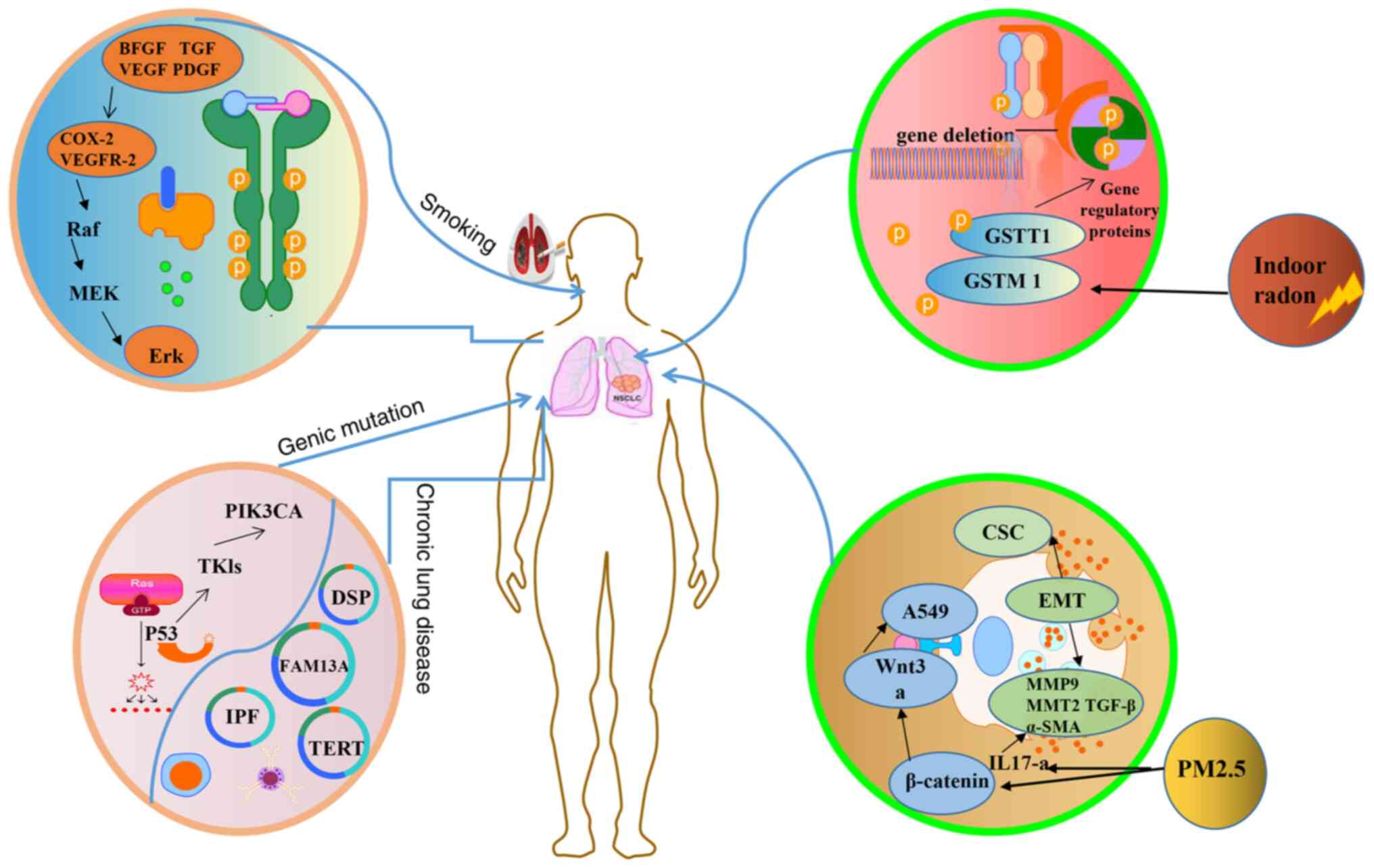
Obtaining an in-depth understanding of the
pathogenesis of lung cancer facilitates the diagnosis and treatment
of NSCLC, and the rehabilitation efficacy and prognosis of patients
with NSCLC would be likely to improve. The pathogenesis of lung
cancer is related to smoking, radon exposure, air pollution and
gene mutation (Fig. 1).
Radon, a chemically inert radioactive gas of natural
origin, produced from uranium and radium in crustal rocks and
soils, is the second most common cause of lung cancer (59,60).
Inhalation of high levels of indoor radon has been demonstrated to
cause DNA mutations and increases risks through depositing decay
products in lung epithelial cells (61-63).
Air pollution is a risk factor for lung cancer, as
it induces adverse effects on the respiratory system, especially
after exposure to fine particulate matter (PM2.5). PM2.5 exposure
leads to lung injury through inflammation, oxidative stress and
apoptosis, which increases the morbidity and mortality of
respiratory and circulatory diseases (64). PM2.5 promotes the occurrence and
development of lung cancer. Compared with tumor-bearing mice in a
normal environment, mice exposed to PM2.5 have been indicated to
have a higher number of tumor nodules and higher matrix
metalloproteinase-1 and vascular endothelial growth factor protein
levels, leading to the occurrence of lung cancer (65,66).
Chronic lung diseases such as tuberculosis and
bronchiectasis increase the risk of lung cancer. Several studies
have indicated that respiratory diseases are closely related to the
morbidity rate of lung cancer (67,68).
With the rapid development of modern biomedicine, it
has become increasingly important to explore the differentially
expressed genes in NSCLC. Epidermal growth factor receptor (EGFR)
gene mutation is a common gene mutation in NSCLC (69). EGFR gene mutation is a common
driver of gene mutations in East Asian populations with NSCLC. TP53
is a tumor suppressor. Previous studies have indicated that TP53
mutations exist in 35-60% of patients with NSCLC, accounting for
>50% of the mutation frequency in lung cancer (70). In addition, studies of microRNAs
have also broadened the understanding of the pathogenesis of lung
cancer.
NSCLC is a chronic disease that frequently requires
rehabilitation. Achieving smoking cessation is never too late for
patients with NSCLC. Patients should seek to inhale fresh air and
increase their exercise levels in a natural environment. Further
studies concerning the identification of molecular mechanisms
underlying lung cancer metastasis are required, which may then
provide new opportunities to eradicate lung cancer metastasis and
guide further research and rehabilitation. A better understanding
of the pathogenesis of lung cancer is likely to be helpful in
developing a multimodal treatment approach that combines lifestyle
changes, exercise programs and nutritional support to address
rehabilitation challenges faced by patients with NSCLC.
Although the surgical treatment of NSCLC has
demonstrated certain progress, its postoperative complications and
recurrence rates remain unsatisfactory. For completely resected
stage I NSCLC, local or distant recurrence occurs in 20-40% of
patients, with a high risk of recurrence per patient annually,
namely, 6-7% in the first four years (71,72).
Despite the use of adjuvant chemotherapy, the risk of developing
stage I and III disease has been reported to range from 45 to 76%
(73). Three- and five-year OS
rates after open lobectomy are ~82 and 66%, respectively (74). Table
II provides the five-year OS rates for sublobar, lobectomy,
stage III and advanced NSCLCs (75-80).
Molecular testing was performed for nonsurgical and stage IV NSCLC
and treatment was guided according to molecular typing. Despite
current surgical techniques and skilled nursing, 19-59% of patients
experience postoperative lung complications (14), which then increase hospital stays
and hospitalization costs, and may result in poor quality of life.
Previous studies have indicated that dyspnea, physical activity
tolerance, stair-climbing ability and quality of life may worsen
and persist for ≥6 months postoperatively (81-83).
Based on these findings, rehabilitation after NSCLC is essential
and continued efforts are required to reduce these high
complication and recurrence rates.
Pulmonary rehabilitation is defined as
'comprehensive intervention based on a thorough patient assessment
after patient-tailored treatment, including but not limited to
exercise training, education and behavioral modification, aimed at
improving the physical and mental well-being of patients with
chronic respiratory disease and promoting long-term adherence to
health-promoting behaviors' (84).
Pulmonary rehabilitation includes exercises to strengthen
respiratory muscles and educational programs which, in combination,
may be expected to contribute to improved rehabilitation outcomes
(85-88). Pulmonary rehabilitation is
essential in a variety of clinical situations, and National
Institute for Health and Clinical Excellence guidelines state that
it may reduce mortality and pulmonary complication rates and may
improve lung function (89,90).
Several studies have indicated that pulmonary rehabilitation may
also improve quality of life, forced expiratory volume in 1 sec and
forced vital capacity, and reduce lung cancer complication and
mortality rates (91-94). The value of pulmonary
rehabilitation for patients with NSCLC after surgery merits
increased attention.
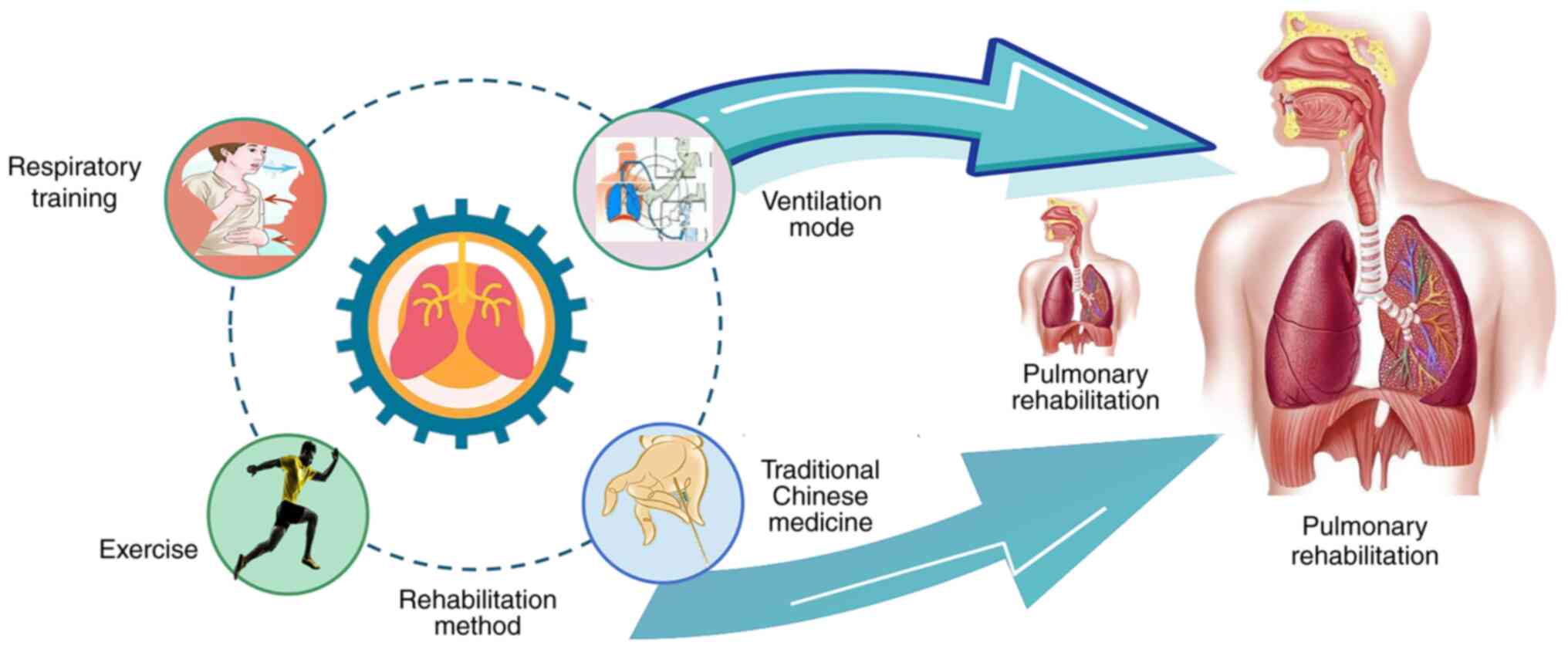
Poor pulmonary rehabilitation affects quality of
life and imposes a heavy burden on societies and families. To date,
no specific treatment program has been approved to enhance
pulmonary rehabilitation. Current evidence in relation to advances
in interventions and strategies for pulmonary rehabilitation are
summarized in the following sections (Figs. 2 and 3).
Medical rehabilitation programs in advanced Western
countries have demonstrated great potential for rehabilitation and
have a positive role in improving rehabilitation outcomes (Table III).
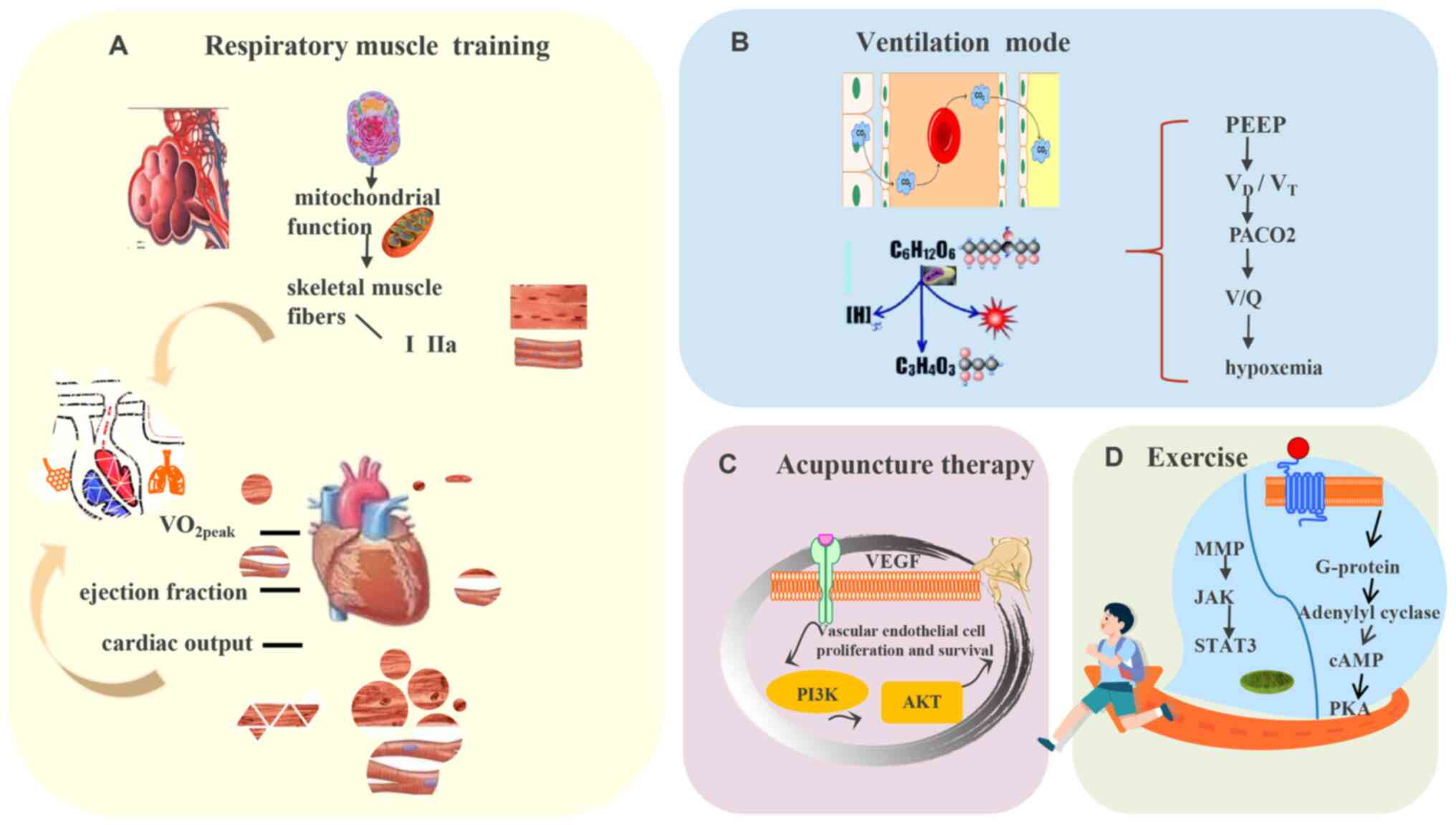
Studies have indicated that respiratory muscle
strength training, particularly inspiratory muscle strength
training, may significantly improve respiratory function, enhance
exercise capacity and reduce dyspnea. Studies on prospective
pulmonary rehabilitation have indicated that a routine
postoperative pulmonary rehabilitation program led by a physical
therapist (including breathing pattern, positive pressure
breathing, resistance, abdominal wall and respiratory muscle
strength training) for 1-6 months has a positive effect on lung
function, quality of life, exercise tolerance and emotional
disorders (95). A study of
respiratory muscle strength preservation with inspiratory muscle
training (IMT) demonstrated that IMT did not preserve respiratory
muscle strength but improved oxygenation in high-risk patients
postoperatively (96). In another
study, six weeks of IMT and aerobic exercise in postoperative
patients with lung cancer were reported to improve respiratory
muscle strength and exercise capacity after VATS (97). Based on these studies, respiratory
muscle strength training appears to be a useful rehabilitation
measure for complications such as postoperative dyspnea and cough,
and may have an important role in preventing postoperative
complications.
With advances in mechanical ventilation studies and
continuous improvements in ventilation modes, significant attention
has been paid to the use of lung protective ventilation strategies
in treatment. Surgery causes a variety of lung injuries. One-lung
ventilation (OLV) is the most commonly used technique for
maintaining intraoperative ventilation and oxygenation. However,
selecting an appropriate mechanical ventilation strategy to
minimize lung injury and other adverse clinical outcomes remains
challenging.
Extensive investigations have been performed to
determine the most appropriate modality of mechanical ventilation.
One systematic review provided recommendations for each grade.
Specifically, recommendations were made to maintain a partial
pressure of carbon dioxide of 50-70 mmHg, a pressure volume with a
tidal volume (Vt) of 6-8 ml/kg and a positive end-expiratory
pressure (PEEP) of 5 cmH2O. It was also recommended to
control mechanical ventilation using an inhalation to exhalation
ratio of 1:1, with pressure-controlled (PC) or PC
ventilation-polygraphy recommended rather than volume-controlled
ventilation, as well as ensuring continuous positive airway
pressure, which is beneficial for improving short-term oxygenation
(98). A previous study suggested
that protective ventilation and flurbiprofen ester pretreatment may
alleviate stress-induced immunosuppression, providing further
options for clinical treatment (99). One study indicated that lung
protective ventilation combined with low Vt and PEEP during
anesthetic induction in lung cancer surgery resulted in improved
postoperative outcomes compared with high Vt without PEEP (100). Two other studies reported similar
results (101,102). The benefits of low Vt strategies
and PEEP values during OLV for better clinical outcomes have been
discussed in certain studies; however, the benefits were not found
to be statistically significant (103,104). One study reported that a
combination of low Vt ventilation and moderate-to-high PEEP (≥5 cm
H2O) provided good lung protection for surgical patients
receiving general anesthesia (105).
The first external validation of the ERAS Society
thoracic guidelines suggested that the thoracic ERAS program for
lung resection reduced the length of stay, morbidity rate, opioid
use and direct costs without a change in readmission (106). Exercise tolerance declines during
the complex postoperative period. A recent study found a strong and
significant association among peak aerobic capacity, quadriceps
muscle function and lung diffusing capacity, suggesting that lower
extremity muscle function is a determinant of exercise tolerance in
patients with lung cancer after pneumonectomy (7). This finding provides a good
indication for rapid postoperative recovery. Exercise also has an
important role in recovery after lung cancer surgery. A study on
the effects of supervised exercise training on athletic
performance, physical activity and sedentary behaviors suggested
that clinical populations may benefit from participating in
exercise training programs (21).
Similarly, personalized home physical activity has also been
reported to improve postoperative quality of life and cancer
biomarkers in patients with NSCLC (107). Skórkowska-Telich owska et
al (108) indicated that
Nordic walking is an effective exercise to increase patients' body
weight and prevent muscle decay, which supported the beneficial
effects of aerobic exercise on rapid recovery in patients with lung
disease. The attention of physicians is primarily focused on
intraoperative anesthetic management and surgical intervention. For
instance, intraoperative paravertebral or intravenous lidocaine or
non-intubated thoracoscopic surgery have been attempted in lung
resection (109).
TCM also has a role in the prevention and treatment
of chronic diseases. Specifically, since the outbreak of
Coronavirus disease-2019 in 2020, TCM has been used throughout the
entire treatment process and has made positive contributions. These
findings support the innovative use of TCM and indicate that TCM
supports the recovery of patients with NSCLC.
Acupuncture therapy is a characteristic therapy of
TCM. Directly acting on acupoints may effectively improve the
respiratory reflex center, remove harmful air in the body, promote
physical recovery and improve physical function. Patients with lung
cancer inevitably experience pain due to tumor location and spread,
as well as from surgical treatment, which seriously affects their
quality of life (110,111). Two systematic reviews have
indicated that acupuncture may effectively relieve pain, regulate
inflammation by stimulating the central nervous system and
significantly reduce the expression of tumor necrosis factor-α,
interleukin-1β (IL-1β) and IL-6 (112,113). Up to 90% of patients with lung
cancer experience side effects such as fatigue after chemotherapy
(114). Currently, there is a
lack of effective pharmacological interventions for the treatment
of cancer-related fatigue (CRF). Hence, complementary and
alternative medicine is gaining popularity among patients with
cancer and is frequently used to manage cancer-related side
effects. Another systematic review and meta-analysis indicated that
acupuncture and auricular acupressure combination treatment worked
better than acupuncture alone to relieve CRF in patients with lung
cancer (115). According to a
study by Wei et al (116),
the incidence rate of cancer-related insomnia in patients with lung
cancer has increased to 68.4%. A recent randomized controlled trial
(RCT) reported the efficacy and safety of acupuncture in the
treatment of insomnia in patients with lung cancer, with
acupuncture potentially providing a promising therapeutic
intervention for the clinical treatment of insomnia in lung cancer
survivors (117). For NSCLC,
postoperative pain, anxiety, insomnia, fatigue and other symptoms
affecting the quality of life of patients are conventionally
treated with medication to relieve patients' symptoms (118,119). Recently, acupuncture, as a
medical alternative therapy, has been extensively applied to
improve the postoperative rehabilitation of patients with
NSCLC.
These studies have involved postoperative or
perioperative rehabilitation programs; however, the role of
preoperative rehabilitation has yet to be fully elucidated. In one
study involving a preoperative pulmonary rehabilitation program,
preoperative resistance training in addition to breathing exercises
improved patients' preoperative condition and possibly prevented
postoperative functional decline (124). Similarly, a systematic review
indicated that preoperative exercise therapy may have beneficial
effects on various constitutional variables and postoperative
complications in patients with lung cancer planning surgery
(66,97). It remains to be elucidated whether
preoperative intervention may lead to the deferral of an operation
to a more appropriate time and further studies are recommended.
However, it would appear that preoperative rehabilitation may be a
useful adjunct with numerous advantages and certain disadvantages.
Overall, it is important that a patient's freedom of choice is
respected when being advised by a physician.
With regard to NSCLC, there are consensus guidelines
concerning the identification of important factors and the grade of
perceived risk; however, the implementation of post-operative
rehabilitation measures remains unclear. Currently, various
respiratory training methods are used in patients with NSCLC.
However, the training method, timing and duration are not uniform,
and the guidelines do not clearly indicate the best rehabilitation
plan for patients undergoing lung cancer surgery. It remains
unclear whether short-term preoperative pulmonary rehabilitation
improves the clinical prognosis of patients. Questions remain, such
as whether it may help promote ineligible patients with lung cancer
to meet surgical requirements or whether it reduces postoperative
complications in high-risk patients with lung cancer. Currently,
accelerated rehabilitation surgery management is widely used in
thoracoscopic lung cancer surgery; however, numerous measures are
limited to the perioperative period, and rehabilitation quantity
and quality after discharge require to be further improved. In
addition, physical activity potentially improves postoperative
outcomes; however, the available evidence is weak and larger
longitudinal studies are required. A multidisciplinary team
approach is crucial in the management of all stages of lung cancer;
however, the optimal rehabilitation program remains to be
determined.
Studies on postoperative pulmonary rehabilitation of
patients with NSCLC range from conventional research to TCM. The
current study first presented the basic epidemiology of lung
cancer. Lung cancer TNM stages (according to the 8th edition) and
surgical approaches were then examined, including thoracoscopic
surgery, which provided a context of postoperative rehabilitation
in patients with NSCLC. Finally, the current conventional medical
and TCM rehabilitation programs that may achieve better
rehabilitation effects were discussed.
With the rapid development of modern medical and
examination techniques, a significant number of NSCLCs are detected
early and treated surgically. However, with population aging, it
remains challenging to determine how to effectively improve the
prognosis and quality of life of patients with NSCLC after surgery.
It is necessary to optimize the current health management model to
ensure efficient care for patients with NSCLC. Various types of
respiratory training have differing effects. However, if a training
method is complex, patients may experience difficulties and
adherence to exercise may be reduced, which is likely to negatively
affect their rehabilitation. Therefore, future studies are
recommended to determine tailored breathing training methods and
the selection and duration of these training methods, in accordance
with an individual's characteristics. With the development of TCM,
its advantages have become gradually clearer. However, patients
undergoing acupuncture and auricular points are frequently
restricted owing to the rehabilitation cycle, location and cost,
and may not be able to meet all of their long-term rehabilitation
needs. Therefore, TCM supplementary therapies that are not affected
by location and have low cost and good effects, such as TCC, the
six-character formula and Baduanjin, should be encouraged (125). Furthermore, the positive effect
of certain single TCM interventions remains elusive and a
combination of TCM may be more effective, which is a recommended
area for further research. Clinical trials with large sample sizes
and multicenter, randomized and accurate statistical analysis
methods are required.
The present study systematically analyzed the
importance of pulmonary rehabilitation and the rehabilitation
measures applied in integrated TCM and in conventional medicine.
The advantages and disadvantages of current treatment strategies
were also summarized. Although there has been clear progress,
certain challenges remain. Further research to improve pulmonary
postoperative rehabilitation programs for patients with NSCLC is
required.
Not applicable.
XES, CLL and FL were involved in the conception of
the review; HFH, SL and SHW reviewed and edited the final
manuscript. XES and WPH drafted the manuscript. All authors have
read and approved the final manuscript. Data authentication is not
applicable.
Not applicable.
Not applicable.
The authors declare that they have no competing
interests.
Not applicable.
This work was supported by the Nursery Fund Project of the
Second Affiliated Hospital of Fujian Medical University (grant no.
2021MP25).
|
1
|
Sung H, Ferlay J, Siegel RL, Laversanne M,
Soerjomataram I, Jemal and Bray F: Global cancer statistics 2020:
GLOBOCAN estimates of incidence and mortality worldwide for 36
cancers in 185 countries. CA Cancer J Clin. 71:209–249. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Chen W, Zheng R, Baade PD, Zhang S, Zeng
H, Bray F, Jemal A, Yu XQ and He J: Cancer statistics in China,
2015. CA Cancer J Clin. 66:115–132. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Wang N, Mengersen K, Tong S, Kimlin M,
Zhou M and Hu W: Global, regional, and national burden of lung
cancer and its attributable risk factors, 1990 to 2017. Cancer.
126:4220–4234. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Wei W, Zeng H, Zheng R, Zhang S, An L,
Chen R, Wang S, Sun K, Matsuda T, Bray F and He J: Cancer
registration in China and its role in cancer prevention and
control. Lancet Oncol. 21:e342–e349. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Wadowska K, Błasiak P, Rzechonek A,
Bil-Lula I and Śliwińska-Mossoń M: New insights on old biomarkers
involved in tumor microenvironment changes and their diagnostic
relevance in non-small cell lung carcinoma. Biomolecules.
11:12082021. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Allehebi A, Kattan KA, Rujaib MA, Dayel
FA, Black E, Mahrous M, AlNassar M, Hussaini HA, Twairgi AA,
Abdelhafeiz N, et al: Management of early-stage resected non-small
cell lung cancer: Consensus statement of the lung cancer
consortium. Cancer Treat Res Commun. 31:1005382022. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zhong WZ; Chinese Thoracic Oncology Group;
Chinese Society of Lung Cancer; Lung Cancer Group of Oncology
Branch Chinese Medical Association; Multidisciplinary Team
Diagnosis and Treatment Committee, Chinses Medical Doctor
Association: Chinses expert consensus on the multidisciplinary team
diagnosis and treatment of lung cancer. Zhonghua Zhong Liu Za Zhi.
42:817–828. 2020.In Chinese. PubMed/NCBI
|
|
8
|
Moyer J, Lee H and Vu L: Thoracoscopic
lobectomy for congenital lung lesions. Clin Perinatol. 44:781–794.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Zhang J, Zhao H, Lv L, Yuan J and Sun Y:
Uniportal thoracoscopic pulmonary lobectomy in the treatment of
lung cancer. Pak J Med Sci. 36:182–186. 2020.PubMed/NCBI
|
|
10
|
Song Y, Zheng C, Zhou S, Cui H, Wang J,
Wang J, Wang W, Liu L and Liu J: The application analysis of 8F
ultrafine chest drainage tube for thoracoscopic lobectomy of lung
cancer. J Cardiothorac Surg. 16:1042021. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Liang W, Cai K, Chen C, Chen H, Chen Q, Fu
J, Hu J, Jiang T, Jiao W, Li S, et al: Expert consensus on
neoadjuvant immunotherapy for non-small cell lung cancer. Transl
Lung Cancer Res. 9:2696–2715. 2020.
|
|
12
|
Zheng Y, Mao M, Ji M, Zheng Q, Liu L, Zhao
Z, Wang H, Wei X, Wang Y, Chen J, et al: Does a pulmonary
rehabilitation based ERAS program (PREP) affect pulmonary
complication incidence, pulmonary function and quality of life
after lung cancer surgery? Study protocol for a multicenter
randomized controlled trial. BMC Pulm Med. 20:442020.PubMed/NCBI
|
|
13
|
Bailey KL, Merchant N, Seo YJ, Elashoff D,
Benharash P and Yanagawa J: Short-term readmissions after open,
thoracoscopic, and robotic lobectomy for lung cancer based on the
nationwide readmissions database. World J Surg. 43:1377–1384.
2019.PubMed/NCBI
|
|
14
|
Yasuura Y, Maniwa T, Mori K, Miyata N,
Mizuno K, Shimizu R, Kayata H, Kojima H, Isaka M and Ohde Y:
Quantitative computed tomography for predicting cardiopulmonary
complications after lobectomy for lung cancer in patients with
chronic obstructive pulmonary disease. Gen Thorac Cardiovasc Surg.
67:697–703. 2019.PubMed/NCBI
|
|
15
|
Rami-Porta R, Bolejack V, Giroux DJ,
Chansky K, Crowley J, Asamura H and Goldstraw P; International
Association for the Study of Lung Cancer Staging and Prognostic
Factors Committee, Advisory Board Members and Participating
Institutions: The IASLC lung cancer staging project: The new
database to inform the eighth edition of the TNM classification of
lung cancer. J Thorac Oncol. 9:1618–1624. 2014.PubMed/NCBI
|
|
16
|
Rami-Porta R, Asamura H, Travis WD and
Rusch VW: Lung cancer-major changes in the American joint committee
on cancer eighth edition cancer staging manual. CA Cancer J Clin.
67:138–155. 2017.PubMed/NCBI
|
|
17
|
Giroux DJ, Van Schil P, Asamura H,
Rami-Porta R, Chansky K, Crowley JJ, Rusch VW and Kernstine K;
International Association for the Study of Lung Cancer Staging and
Prognostic Factors Committee: The IASLC lung cancer staging
project: A renewed call to participation. J Thorac Oncol.
13:801–809. 2018.PubMed/NCBI
|
|
18
|
Lim W, Ridge CA, Nicholson AG and
Mirsadraee S: The 8th lung cancer TNM classification and clinical
staging system: Review of the changes and clinical implications.
Quant Imaging Med Surg. 8:709–718. 2018.PubMed/NCBI
|
|
19
|
Mirsadraee S, Oswal D, Alizadeh Y, Caulo A
and van Beek E Jr: The 7th lung cancer TNM classification and
staging system: Review of the changes and implications. World J
Radiol. 4:128–134. 2012.PubMed/NCBI
|
|
20
|
Tan WL, Chua KLM, Lin CC, Lee VHF, Tho LM,
Chan AW, Ho GF, Reungwetwattana T, Yang JC, Kim DW, et al: Asian
thoracic oncology research group expert consensus statement on
optimal management of stage III NSCLC. J Thorac Oncol. 15:324–343.
2020.
|
|
21
|
Rami-Porta R, Bolejack V, Crowley J, Ball
D, Kim J, Lyons G, Rice T, Suzuki K, Thomas CF Jr, Travis WD, et
al: The IASLC lung cancer staging project: Proposals for the
revisions of the T descriptors in the forthcoming eighth edition of
the TNM classification for lung cancer. J Thorac Oncol.
10:990–1003. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Amin MB, Greene FL, Edge SB, Compton CC,
Gershenwald JE, Brookland RK, Meyer L, Gress DM, Byrd DR and
Winchester DP: The eighth edition AJCC cancer staging manual:
Continuing to build a bridge from a population-based to a more
'personalized' approach to cancer staging. CA Cancer J Clin.
67:93–99. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Lababede O and Meziane MA: The eighth
edition of TNM staging of lung cancer: Reference chart and
diagrams. Oncologist. 23:844–848. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ettinger DS, Aisner DL, Wood DE, Akerley
W, Bauman J, Chang JY, Chirieac LR, D'Amico TA, Dilling TJ,
Dobelbower M, et al: NCCN guidelines insights: Non-small cell lung
cancer, version 5.2018. J Natl Compr Canc Netw. 16:807–821. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Moulla Y, Gradistanac T, Wittekind C,
Eichfeld U, Gockel I and Dietrich A: Predictive risk factors for
lymph node metastasis in patients with resected non-small cell lung
cancer: A case control study. J Cardiothorac Surg. 14:112019.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Bezjak A, Temin S, Franklin G, Giaccone G,
Govindan R, Johnson ML, Rimner A, Schneider BJ, Strawn J and Azzoli
CG: Definitive and adjuvant radiotherapy in locally advanced
non-small-cell lung cancer: American society of clinical oncology
clinical practice guideline endorsement of the american society for
radiation oncology evidence-based clinical practice guideline. J
Clin Oncol. 33:2100–2105. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Berfield KS, Farjah F and Mulligan MS:
Video-assisted thoracoscopic lobectomy for lung cancer. Ann Thorac
Surg. 107:603–609. 2019. View Article : Google Scholar
|
|
28
|
McKenna RJ Jr, Houck W and Fuller CB:
Video-assisted thoracic surgery lobectomy: Experience with 1,100
cases. Ann Thorac Surg. 81:421–426. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Ettinger DS, Wood DE, Aisner DL, Akerley
W, Bauman J, Chirieac LR, D'Amico TA, DeCamp MM, Dilling TJ,
Dobelbower M, et al: Non-small cell lung cancer, version 5.2017,
NCCN clinical practice guidelines in oncology. J Natl Compr Canc
Netw. 15:504–535. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Cao J, Yuan P, Wang Y, Xu J, Yuan X, Wang
Z, Lv W and Hu J: Survival rates after lobectomy, segmentectomy,
and wedge resection for non-small cell lung cancer. Ann Thorac
Surg. 105:1483–1491. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Li F, Zhao Y, Yuan L, Wang S and Mao Y:
Oncologic outcomes of segmentectomy vs lobectomy in pathologic
stage IA (≤2 cm) invasive lung adenocarcinoma: A population-based
study. J Surg Oncol. 121:1132–1139. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Kodama K, Higashiyama M, Okami J, Tokunaga
T, Imamura F, Nakayama T, Inoue A and Kuriyama K: Oncologic
outcomes of segmentectomy versus lobectomy for clinical T1a N0 M0
non-small cell lung cancer. Ann Thorac Surg. 101:504–511. 2016.
View Article : Google Scholar
|
|
33
|
Landreneau RJ, Normolle DP, Christie NA,
Awais O, Wizorek JJ, Abbas G, Pennathur A, Shende M, Weksler B,
Luketich JD and Schuchert MJ: Recurrence and survival outcomes
after anatomic segmentectomy versus lobectomy for clinical stage I
non-small-cell lung cancer: A propensity-matched analysis. J Clin
Oncol. 32:2449–2455. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Nakamura K, Saji H, Nakajima R, Okada M,
Asamura H, Shibata T, Nakamura S, Tada H and Tsuboi M: A phase III
randomized trial of lobectomy versus limited resection for
small-sized peripheral non-small cell lung cancer
(JCOG0802/WJOG4607L). Jpn J Clin Oncol. 40:271–274. 2010.
View Article : Google Scholar
|
|
35
|
Suzuki K, Saji H, Aokage K, Watanabe SI,
Okada M, Mizusawa J, Nakajima R, Tsuboi M, Nakamura S, Nakamura K,
et al: Comparison of pulmonary segmentectomy and lobectomy: Safety
results of a randomized trial. J Thorac Cardiovasc Surg.
158:895–907. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Wang Z, Cheng Y, An T, Gao H, Wang K, Zhou
Q, Hu Y, Song Y, Ding C, Peng F, et al: Detection of EGFR mutations
in plasma circulating tumour DNA as a selection criterion for
first-line gefitinib treatment in patients with advanced lung
adenocarcinoma (BENEFIT): A phase 2, single-arm, multicentre
clinical trial. Lancet Respir Med. 6:681–690. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Sinn K, Gschwandtner E, Steindl A and
Taghavi S: Hoda MA. EP117–15. comparison of long-term outcome of
wedge resection, anatomical segmentectomy and lobectomy in stage
I-II non-small cell lung cancer. J Thorac Oncol. 14(Suppl):
S10892019. View Article : Google Scholar
|
|
38
|
Spicer JD, Shewale JB, Nelson DB, Mitchell
KG, Bott MJ, Vallières E, Wilshire CL, Vaporciyan AA, Swisher SG,
Jones DR, et al: Multimodality therapy for N2 non-small cell lung
cancer: An evolving paradigm. Ann Thorac Surg. 107:277–284. 2019.
View Article : Google Scholar
|
|
39
|
Dickhoff C, Senan S, Schneiders FL,
Veltman J, Hashemi S, Daniels JMA, Fransen M, Heineman DJ, Radonic
T, van de Ven PM, et al: Ipilimumab plus nivolumab and
chemoradiotherapy followed by surgery in patients with resectable
and borderline resectable T3-4N0-1 non-small cell lung cancer: The
INCREASE trial. BMC Cancer. 20:7642020. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Haam S: Video-assisted thoracic surgery
pneumonectomy. J Chest Sur. 54:253–257. 2021. View Article : Google Scholar
|
|
41
|
Ng CS, Wan S, Lee TW, Wan IY, Arifi AA and
Yim AP: Video-assisted thoracic surgery in spontaneous
pneumothorax. Can Respir J. 9:122–127. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Paul S, Altorki NK, Sheng S, Lee PC,
Harpole DH, Onaitis MW, Stiles BM, Port JL and D'Amico TA:
Thoracoscopic lobectomy is associated with lower morbidity than
open lobectomy: A propensity-matched analysis from the STS
database. J Thorac Cardiovasc Surg. 139:366–378. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Han D, Cao Y, Wu H, Wang H, Jiang L, Zhao
D, Yao F, Li S, Zhang C, Zheng B, et al: Uniportal video-assisted
thoracic surgery for the treatment of lung cancer: A consensus
report from Chinese society for thoracic and cardiovascular surgery
(CSTCVS) and Chinese association of thoracic surgeons (CATS).
Transl Lung Cancer Res. 9:971–987. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Scott WJ, Howington J, Feigenberg S,
Movsas B and Pisters K; American College of Chest Physicians:
Treatment of non-small cell lung cancer stage I and stage II: ACCP
evidence-based clinical practice guidelines (2nd edition). Chest.
132(3 Suppl): 234S–242S. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Dziedzic D and Orlowski T: The role of
VATS in lung cancer surgery: Current status and prospects for
development. Minim Invasive Surg. 2015:9384302015.PubMed/NCBI
|
|
46
|
Ng CS, Gonzalez-Rivas D, D'Amico TA and
Rocco G: Uniportal VATS-a new era in lung cancer surgery. J Thorac
Dis. 7:1489–1491. 2015.PubMed/NCBI
|
|
47
|
Gao Y, Abulimiti A, He D, Ran A and Luo D:
Comparison of single- and triple-port VATS for lung cancer: A
meta-analysis. Open Med (Wars). 16:1228–1239. 2021. View Article : Google Scholar
|
|
48
|
Bertolaccini L, Batirel H, Brunelli A,
Gonzalez-Rivas D, Ismail M, Ucar AM, Ng CSH, Scarci M, Sihoe ADL,
Ugalde PA, et al: Corrigendum to 'uniportal video-assisted thoracic
surgery lobectomy: A consensus report from the uniportal VATS
interest group (UVIG) of the European society of thoracic surgeons
(ESTS)'. Eur J Cardiothorac Surg. 2019.56:224–9. View Article : Google Scholar : PubMed/NCBI
Eur J Cardiothorac Surg. 56:628–629. 2019.
View Article : Google Scholar
|
|
49
|
Wang BY, Liu CY, Hsu PK, Shih CS and Liu
CC: Single-incision versus multiple-incision thoracoscopic
lobectomy and segmentectomy: A propensity-matched analysis. Ann
Surg. 261:793–799. 2015. View Article : Google Scholar
|
|
50
|
Han KN, Kim HK, Lee HJ and Choi YH:
Single-port video-assisted thoracoscopic pulmonary segmentectomy: A
report on 30 cases†. Eur J Cardiothorac Surg. 49(Suppl 1): i42–i47.
2016.
|
|
51
|
Sihoe ADL: Uniportal lung cancer surgery:
State of the evidence. Ann Thorac Surg. 107:962–972. 2019.
View Article : Google Scholar
|
|
52
|
Shen Y, Zhang Y, Sun J, Gu J, Yuan Y and
Wang Q: Transaxillary uniportal video assisted thoracoscopic
surgery for right upper lobectomy. J Thorac Dis. 10:E214–E217.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Zieliński M, Nabialek T and Pankowski J:
Transcervical uniportal pulmonary lobectomy. J Vis Surg. 4:422018.
View Article : Google Scholar
|
|
54
|
Palleschi A, Mendogni P, Mariolo AV,
Nosotti M and Rosso L: An alternative chest tube placement after
uniportal video-assisted thoracic surgery. J Thorac Dis.
10:3078–3080. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Kao CN, Chang CW, Hsieh MC, Liu YW and
Chou SH: Pre-embedding subcutaneous suture for chest-tube insertion
in uniportal video-assisted thoracoscopic surgery. J Thorac Dis.
9:E938–E940. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Global Burden of Disease 2019 Cancer
Collaboration; Kocarnik JM, Compton K, Dean FE, Fu W, Gaw BL,
Harvey JD, Henrikson HJ, Lu D, Pennini A, et al: Cancer incidence,
mortality, years of life lost, years lived with disability, and
disability-adjusted life years for 29 cancer groups from 2010 to
2019: A systematic analysis for the global burden of disease study
2019. JAMA Oncol. 8:420–444. 2022. View Article : Google Scholar :
|
|
57
|
Yang X, Man J, Chen H, Zhang T, Yin X, He
Q and Lu M: Temporal trends of the lung cancer mortality
attributable to smoking from 1990 to 2017: A global, regional and
national analysis. Lung Cancer. 152:49–57. 2021. View Article : Google Scholar
|
|
58
|
Jeon J, Holford TR, Levy DT, Feuer EJ, Cao
P, Tam J, Clarke L, Clarke J, Kong CY and Meza R: Smoking and Lung
cancer mortality in the United States from 2015 to 2065: A
comparative modeling approach. Ann Intern Med. 169:684–693. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
59
|
No authors listed. WHO Guidelines Approved
by the Guidelines Review Committee WHO Handbook on indoor radon: A
public health perspective. Geneva: World Health Organization;
2009
|
|
60
|
Kim SH, Hwang WJ, Cho JS and Kang DR:
Attributable risk of lung cancer deaths due to indoor radon
exposure. Ann Occup Environ Med. 28:82016. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Peterson E, Aker A, Kim J, Li Y, Brand K
and Copes R: Lung cancer risk from radon in Ontario, Canada: How
many lung cancers can we prevent? Cancer Causes Control.
24:2013–2020. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Al-Zoughool M and Krewski D: Health
effects of radon: A review of the literature. Int J Radiat Biol.
85:57–69. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Enflo A: Lung cancer risks from
residential radon among smokers and non-smokers. J Radiol Prot.
22:A95–A99. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Al-Rubaie A, Wise AF, Sozo F, De Matteo R,
Samuel CS, Harding R and Ricardo SD: The therapeutic effect of
mesenchymal stem cells on pulmonary myeloid cells following
neonatal hyperoxic lung injury in mice. Respir Res. 19:1142018.
View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Ning J, Li P, Zhang B, Han B, Su X, Wang
Q, Wang X, Li B, Kang H, Zhou L, et al: miRNAs deregulation in
serum of mice is associated with lung cancer related pathway
deregulation induced by PM2.5. Environ Pollut. 254:1128752019.
View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Yang B and Xiao C: PM2.5 exposure
significantly improves the exacerbation of A549 tumor-bearing
CB17-SCID mice. Environ Toxicol Pharmacol. 60:169–175. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Jiang L, Sun YQ, Langhammer A, Brumpton
BM, Chen Y, Nilsen TI, Leivseth L, Wahl SGF and Mai XM: Asthma and
asthma symptom control in relation to incidence of lung cancer in
the HUNT study. Sci Rep. 11:45392021. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Szalontai K, Gémes N, Furák J, Varga T,
Neuperger P, Balog JÁ, Puskás LG and Szebeni GJ: Chronic
obstructive pulmonary disease: Epidemiology, biomarkers, and paving
the way to lung cancer. J Clin Med. 10:28892021. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Huang J and Wang H: Targeted therapy and
mechanism of drug resistance in non-small cell lung cancer with
epidermal growth factor receptor gene mutation. Zhongguo Fei Ai Za
Zhi. 25:183–192. 2022.In Chinese. PubMed/NCBI
|
|
70
|
Halvorsen AR, Silwal-Pandit L, Meza-Zepeda
LA, Vodak D, Vu P, Sagerup C, Hovig E, Myklebost O, Børresen-Dale
AL, Brustugun OT and Helland Å: TP53 mutation spectrum in smokers
and never smoking lung cancer patients. Front Genet. 7:852016.
View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Winton T, Livingston R, Johnson D, Rigas
J, Johnston M, Butts C, Cormier Y, Goss G, Inculet R, Vallieres E,
et al: Vinorelbine plus cisplatin vs observation in resected
non-small-cell lung cancer. N Engl J Med. 352:2589–2597. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Lou F, Huang J, Sima CS, Dycoco J, Rusch V
and Bach PB: Patterns of recurrence and second primary lung cancer
in early-stage lung cancer survivors followed with routine computed
tomography surveillance. J Thorac Cardiovasc Surg. 145:75–82. 2013.
View Article : Google Scholar
|
|
73
|
Pignon JP, Tribodet H, Scagliotti GV,
Douillard JY, Shepherd FA, Stephens RJ, Dunant A, Torri V, Rosell
R, Seymour L, et al: Lung adjuvant cisplatin evaluation: A pooled
analysis by the LACE collaborative group. J Clin Oncol.
26:3552–3559. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Tandberg DJ, Tong BC, Ackerson BG and
Kelsey CR: Surgery versus stereotactic body radiation therapy for
stage I non-small cell lung cancer: A comprehensive review. Cancer.
124:667–678. 2018. View Article : Google Scholar
|
|
75
|
Choi SY, Moon MH and Moon Y: The prognosis
of small-sized non-small cell lung cancer with visceral pleural
invasion after sublobar resection. Transl Cancer Res. 9:6431–6443.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Zheng YW, Li RM, Zhang XW and Ren XB:
Current adoptive immunotherapy in non-small cell lung cancer and
potential influence of therapy outcome. Cancer Invest. 31:197–205.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Malik PS and Raina V: Lung cancer:
Prevalent trends & emerging concepts. Indian J Med Res.
141:5–7. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Detterbeck FC, Chansky K, Groome P,
Bolejack V, Crowley J, Shemanski L, Kennedy C, Krasnik M, Peake M,
Rami-Porta R, et al: The IASLC lung cancer staging project:
Methodology and validation used in the development of proposals for
revision of the stage classification of NSCLC in the forthcoming
(eighth) edition of the TNM classification of lung cancer. J Thorac
Oncol. 11:1433–1446. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Yoon SM, Shaikh T and Hallman M:
Therapeutic management options for stage III non-small cell lung
cancer. World J Clin Oncol. 8:1–20. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Iyengar P, Kavanagh BD, Wardak Z, Smith I,
Ahn C, Gerber DE, Dowell J, Hughes R, Abdulrahman R, Camidge DR, et
al: Phase II trial of stereotactic body radiation therapy combined
with erlotinib for patients with limited but progressive metastatic
non-small-cell lung cancer. J Clin Oncol. 32:3824–3830. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Jack S, West MA, Raw D, Marwood S, Ambler
G, Cope TM, Shrotri M, Sturgess RP, Calverley PM, Ottensmeier CH
and Grocott MP: The effect of neoadjuvant chemotherapy on physical
fitness and survival in patients undergoing oesophagogastric cancer
surgery. Eur J Surg Oncol. 40:1313–1320. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Ni HJ, Pudasaini B, Yuan XT, Li HF and
Yuan P: Exercise training for patients pre- and postsurgically
treated for non-small cell lung cancer: A systematic review and
meta-analysis. Integr Cancer Ther. 16:63–73. 2017. View Article : Google Scholar
|
|
83
|
Pan H, Pei Y, Li B, Wang Y, Liu J and Lin
H: Tai Chi Chuan in postsurgical non-small cell lung cancer
patients: Study protocol for a randomized controlled trial. Trials.
19:22018. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Rochester CL, Vogiatzis I, Holland AE,
Lareau SC, Marciniuk DD, Puhan MA, Spruit MA, Masefield S, Casaburi
R, Clini EM, et al: An official american thoracic society/European
respiratory society policy statement: Enhancing implementation,
use, and delivery of pulmonary rehabilitation. Am J Respir Crit
Care Med. 192:1373–1386. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Hill K, Vogiatzis I and Burtin C: The
importance of components of pulmonary rehabilitation, other than
exercise training, in COPD. Eur Respir Rev. 22:405–413. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Wouters EF, Posthuma R, Koopman M, Liu WY,
Sillen MJ, Hajian B, Sastry M, Spruit MA and Franssen FM: An update
on pulmonary rehabilitation techniques for patients with chronic
obstructive pulmonary disease. Expert Rev Respir Med. 14:149–161.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Wilson JS, O'Neill B, Reilly J, MacMahon J
and Bradley JM: Education in pulmonary rehabilitation: The
patient's perspective. Arch Phys Med Rehabil. 88:1704–1709. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Aldhahir AM, Rajeh AMA, Aldabayan YS,
Drammeh S, Subbu V, Alqahtani JS, Hurst JR and Mandal S:
Nutritional supplementation during pulmonary rehabilitation in
COPD: A systematic review. Chron Respir Dis.
17:14799731209049532020. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Poston G, Tait D, Beattie R, Byrne C,
Chapman J, Devereux L, Glynne-Jones R, Harrison M, Holman C, Ilyas
M, et al: National institute for health and clinical excellence:
The diagnosis and management of colorectal cancer: Full guideline.
2011.
|
|
90
|
Jamison DT, Gelband H, Horton S, Jha P,
Laxminarayan R, Mock CN and Nugent R: Disease control priorities:
Improving health and reducing poverty. 3rd edition. Washington
(DC): The International Bank for Reconstruction and Development/The
World Bank; 2017
|
|
91
|
Tiep B, Sun V, Koczywas M, Kim J, Raz D,
Hurria A and Hayter J: Pulmonary rehabilitation and palliative care
for the lung cancer patient. J Hosp Palliat Nurs. 17:462–468. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Vagvolgyi A, Rozgonyi Z, Kerti M, Agathou
G, Vadasz P and Varga J: Effectiveness of pulmonary rehabilitation
and correlations in between functional parameters, extent of
thoracic surgery and severity of post-operative complications:
Randomized clinical trial. J Thorac Dis. 10:3519–3531. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Choi J, Yang Z, Lee J, Lee JH, Kim HK,
Yong HS and Lee SY: Usefulness of pulmonary rehabilitation in
non-small cell lung cancer patients based on pulmonary function
tests and muscle analysis using computed tomography images. Cancer
Res Treat. 54:793–802. 2022. View Article : Google Scholar
|
|
94
|
Mao X, Ni Y, Niu Y and Jiang L: The
clinical value of pulmonary rehabilitation in reducing
postoperative complications and mortality of lung cancer resection:
A systematic review and meta-analysis. Front Surg. 8:6854852021.
View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Tenconi S, Mainini C, Rapicetta C, Braglia
L, Galeone C, Cavuto S, Merlo DF, Costi S, Paci M, Piro R and
Fugazzaro S: Rehabilitation for lung cancer patients undergoing
surgery: Results of the PUREAIR randomized trial. Eur J Phys
Rehabil Med. 57:1002–1011. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Brocki BC, Andreasen JJ, Langer D, Souza
DS and Westerdahl E: Postoperative inspiratory muscle training in
addition to breathing exercises and early mobilization improves
oxygenation in high-risk patients after lung cancer surgery: A
randomized controlled trial. Eur J Cardiothorac Surg. 49:1483–1491.
2016. View Article : Google Scholar
|
|
97
|
Liu JF, Kuo NY, Fang TP, Chen JO, Lu HI
and Lin HL: A six-week inspiratory muscle training and aerobic
exercise improves respiratory muscle strength and exercise capacity
in lung cancer patients after video-assisted thoracoscopic surgery:
A randomized controlled trial. Clin Rehabil. 35:840–850. 2021.
View Article : Google Scholar
|
|
98
|
Gao S, Zhang Z, Brunelli A, Chen C, Chen
C, Chen G, Chen H, Chen JS, Cassivi S, Chai Y, et al: The society
for translational medicine: Clinical practice guidelines for
mechanical ventilation management for patients undergoing
lobectomy. J Thorac Dis. 9:3246–3254. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Yuan J, Cen S, Li J, Wang K, Chen Q, Li H
and Zhang Y: Effect of lung protective ventilation combined with
flurbiprofen axetil on immune function during thoracoscopic radical
resection of lung cancer. Front Surg. 9:8404202022. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Marret E, Cinotti R, Berard L, Piriou V,
Jobard J, Barrucand B, Radu D, Jaber S and Bonnet F; PPV study
group: Protective ventilation during anaesthesia reduces major
postoperative complications after lung cancer surgery: A
double-blind randomised controlled trial. Eur J Anaesthesiol.
35:727–735. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Yang M, Ahn HJ, Kim K, Kim JA, Yi CA, Kim
MJ and Kim HJ: Does a protective ventilation strategy reduce the
risk of pulmonary complications after lung cancer surgery?: A
randomized controlled trial. Chest. 139:530–537. 2011. View Article : Google Scholar
|
|
102
|
Lederman D, Easwar J, Feldman J and
Shapiro V: Anesthetic considerations for lung resection:
Preoperative assessment, intraoperative challenges and
postoperative analgesia. Ann Transl Med. 7:3562019. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Amar D, Zhang H, Pedoto A, Desiderio DP,
Shi W and Tan KS: Protective lung ventilation and morbidity after
pulmonary resection: A propensity score-matched analysis. Anesth
Analg. 125:190–199. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Kiss T, Wittenstein J, Becker C, Birr K,
Cinnella G, Cohen E, El Tahan MR, Falcão LF, Gregoretti C, Granell
M, et al: Protective ventilation with high versus low positive
end-expiratory pressure during one-lung ventilation for thoracic
surgery (PROTHOR): Study protocol for a randomized controlled
trial. Trials. 20:2132019. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Deng QW, Tan WC, Zhao BC, Wen SH, Shen JT
and Xu M: Intraoperative ventilation strategies to prevent
postoperative pulmonary complications: A network meta-analysis of
randomised controlled trials. Br J Anaesth. 124:324–335. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Haro GJ, Sheu B, Marcus SG, Sarin A,
Campbell L, Jablons DM and Kratz JR: Perioperative lung resection
outcomes after implementation of a multidisciplinary,
evidence-based thoracic ERAS program. Ann Surg. 274:e1008–e1013.
2021. View Article : Google Scholar
|
|
107
|
Mittaz Hager AG, Mathieu N,
Lenoble-Hoskovec C, Swanenburg J, de Bie R and Hilfiker R: Effects
of three home-based exercise programmes regarding falls, quality of
life and exercise-adherence in older adults at risk of falling:
Protocol for a randomized controlled trial. BMC Geriatr. 19:132019.
View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Skórkowska-Telichowska K, Kropielnicka K,
Bulińska K, Pilch U, Woźniewski M, Szuba A and Jasiński R: Nordic
walking in the second half of life. Aging Clin Exp Res.
28:1035–1046. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Xian H, Li Y, Zou B, Chen Y, Yin H, Li X
and Pan Y: Identification of TIMELESS and RORA as key clock
molecules of non-small cell lung cancer and the comprehensive
analysis. BMC Cancer. 22:1072022. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Iyer S, Taylor-Stokes G and Roughley A:
Symptom burden and quality of life in advanced non-small cell lung
cancer patients in France and Germany. Lung Cancer. 81:288–293.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Simmons CP, Macleod N and Laird BJ:
Clinical management of pain in advanced lung cancer. Clin Med
Insights Oncol. 6:331–346. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Yang FM, Yao L, Wang SJ, Guo Y, Xu ZF,
Zhang CH, Zhang K, Fang YX and Liu YY: Current tracking on
effectiveness and mechanisms of acupuncture therapy: A literature
review of high-quality studies. Chin J Integr Med. 26:310–320.
2020. View Article : Google Scholar
|
|
113
|
Kuang R, Xiong G, Lv W, Zhao Y, Yu M and
Jiang J: Efficacy and safety of acupuncture combined with
analgesics on lung cancer pain: A protocol for systematic review
and meta-analysis. Medicine (Baltimore). 100:e262252021. View Article : Google Scholar
|
|
114
|
Ebede CC, Jang Y and Escalante CP:
Cancer-related fatigue in cancer survivorship. Med Clin North Am.
101:1085–1097. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Li H and Liu H: Combined effects of
acupuncture and auricular acupressure for relieving cancer-related
fatigue in patients during lung cancer chemotherapy: A protocol for
systematic review and meta-analysis. Medicine (Baltimore).
100:e275022021. View Article : Google Scholar
|
|
116
|
Wei TT, Chen XC, Hou YX and Radiotherapy
DO: Relationship between cancer-related insomnia and relevant
symptoms of tumor in patients with lung cancer during chemotherapy.
Chin Gen Pract. 2015.
|
|
117
|
Yue H, Zhou S, Wu H, Yin X, Li S, Liang T,
Li Y, Fang Z, Zhang X, Wang L, et al: Efficacy and safety of
electro-acupuncture (EA) on insomnia in patients with lung cancer:
Study protocol of a randomized controlled trial. Trials.
21:7882020. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Turcott JG, Del Rocío Guillen Núñez M,
Flores-Estrada D, Oñate-Ocaña LF, Zatarain-Barrón ZL, Barrón F and
Arrieta O: The effect of nabilone on appetite, nutritional status,
and quality of life in lung cancer patients: A randomized,
double-blind clinical trial. Support Care Cancer. 26:3029–3038.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Matsutani N and Kawamura M: Significant
improvement of chronic pain by Pregabalin after thoracotomy: Report
of four cases. Surg Today. 43:915–917. 2013. View Article : Google Scholar
|
|
120
|
Chen P, Wang D, Shen H, Yu L, Gao Q, Mao
L, Jiang F, Luo Y, Xie M, Zhang Y, et al: Physical activity and
health in Chinese children and adolescents: Expert consensus
statement (2020). Br J Sports Med. 54:1321–1331. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Song Y, Sun D, István B, Thirupathi A,
Liang M, Teo EC and Gu Y: Current evidence on traditional Chinese
exercise for cancers: A systematic review of randomized controlled
trials. Int J Environ Res Public Health. 17:50112020. View Article : Google Scholar :
|
|
122
|
Liu J, Chen P, Wang R, Yuan Y, Wang X and
Li C: Effect of Tai Chi on mononuclear cell functions in patients
with non-small cell lung cancer. BMC Complement Altern Med.
15:32015. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Zhang LL, Wang SZ, Chen HL and Yuan AZ:
Tai Chi exercise for cancer-related fatigue in patients with lung
cancer under-going chemotherapy: A randomized controlled trial. J
Pain Symptom Manage. 51:504–511. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Sebio García R, Yáñez-Brage MI, Giménez
Moolhuyzen E, Salorio Riobo M, Lista Paz A and Borro Mate JM:
Preoperative exercise training prevents functional decline after
lung resection surgery: A randomized, single-blind controlled
trial. Clin Rehabil. 31:1057–1067. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Huang L, Xie D, Yu Y, Liu H, Shi Y, Shi T
and Wen C: TCMID 2.0: A comprehensive resource for TCM. Nucleic
Acids Res. 46(D1): D1117–D1120. 2018. View Article : Google Scholar :
|