|
1
|
Sung H, Ferlay J, Siegel RL, Laversanne M,
Soerjomataram I, Jemal A and Bray F: Global cancer statistics 2020:
GLOBOCAN estimates of incidence and mortality worldwide for 36
cancers in 185 countries. CA Cancer J Clin. 71:209–249. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Xia C, Dong X, Li H, Cao M, Sun D, He S,
Yang F, Yan X, Zhang S, Li N and Chen W: Cancer statistics in China
and United States, 2022: Profiles, trends, and determinants. Chin
Med J (Engl). 135:584–590. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Salji M, Hendry J, Patel A, Ahmad I, Nixon
C and Leung HY: Peri-prostatic fat volume measurement as a
predictive tool for castration resistance in advanced prostate
cancer. Eur Urol Focus. 4:858–866. 2018. View Article : Google Scholar
|
|
4
|
Yang L, Jin M, Park SJ, Seo SY and Jeong
KW: SETD1A promotes proliferation of castration-resistant prostate
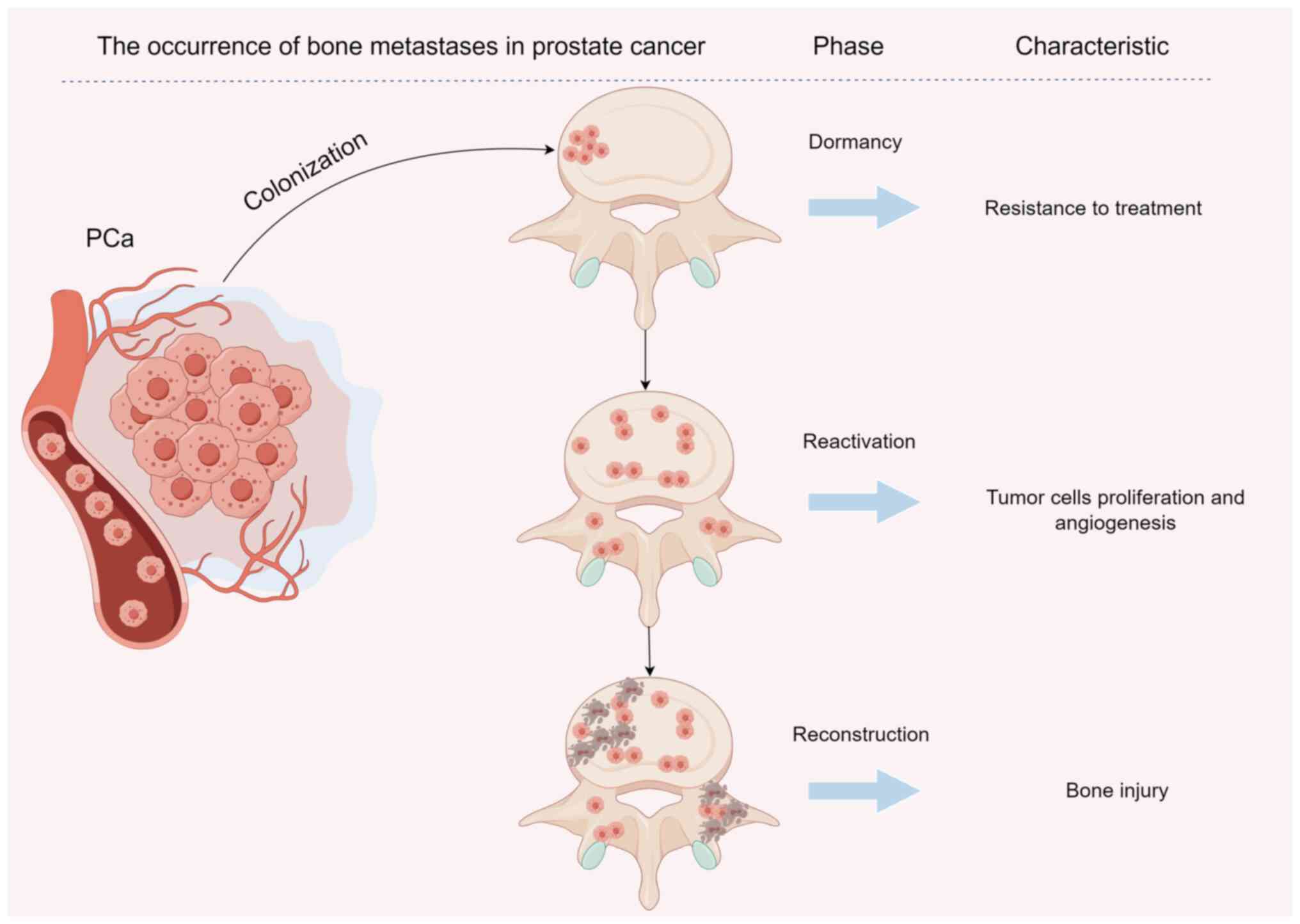
cancer cells via FOXM1 transcription. Cancers (Basel). 12:17362020.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Chi JT, Lin PH, Tolstikov V, Oyekunle T,
Chen EY, Bussberg V, Greenwood B, Sarangarajan R, Narain NR,
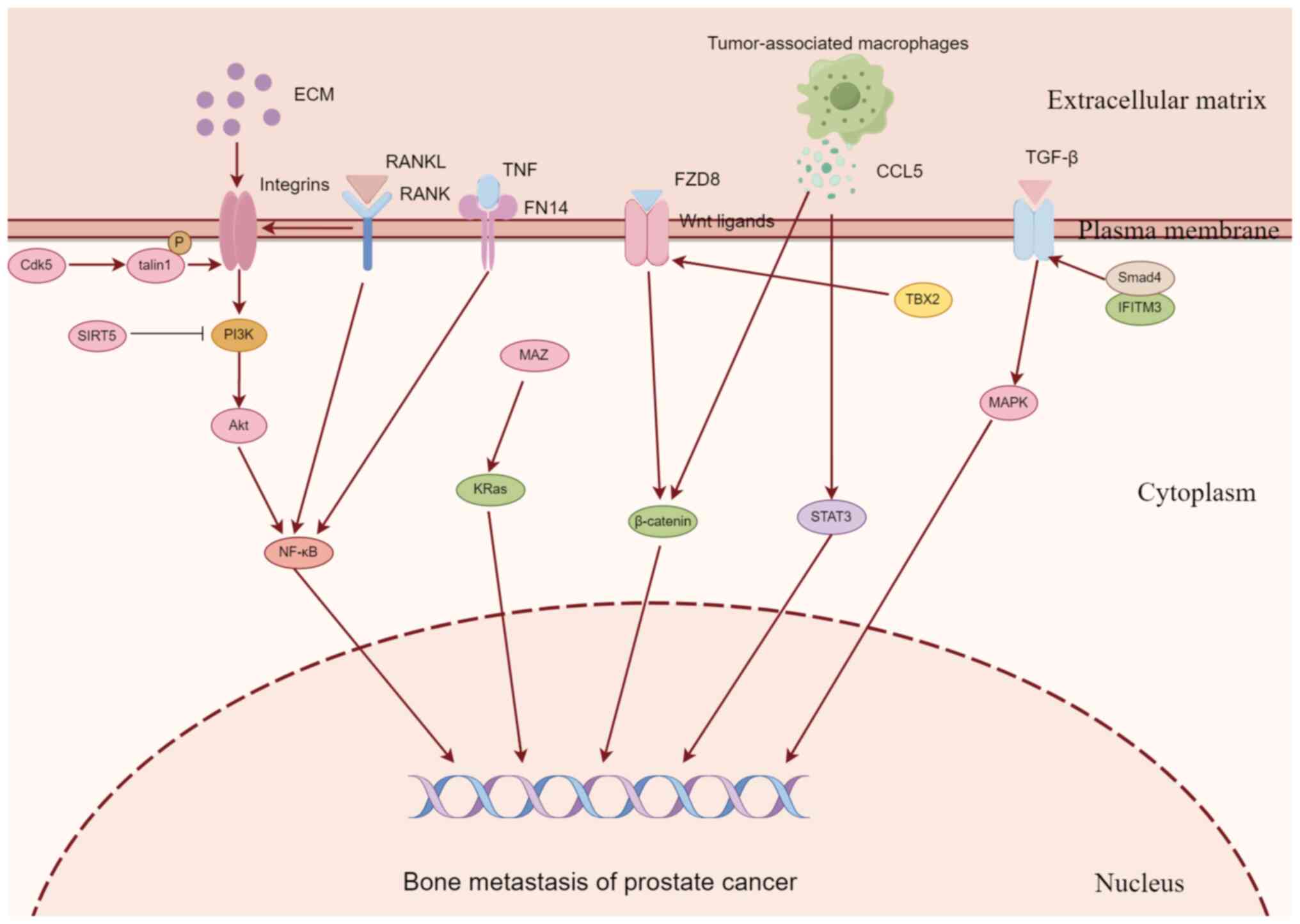
Kiebish MA and Freedland SJ: Metabolomic effects of androgen
deprivation therapy treatment for prostate cancer. Cancer Med.
9:3691–3702. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Yu Z, Zou H, Wang H, Li Q and Yu D:
Identification of key gene signatures associated with bone
metastasis in castration-resistant prostate cancer using
co-expression analysis. Front Oncol. 10:5715242021. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Lee S, Mendoza TR, Burner DN, Muldong MT,
Wu CCN, Arreola-Villanueva C, Zuniga A, Greenburg O, Zhu WY,
Murtadha J, et al: Novel dormancy mechanism of castration
resistance in bone metastatic prostate cancer organoids. Int J Mol
Sci. 23:32032022. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Clézardin P, Coleman R, Puppo M, Ottewell
P, Bonnelye E, Paycha F, Confavreux CB and Holen I: Bone
metastasis: Mechanisms, therapies, and biomarkers. Physiol Rev.
101:797–855. 2021. View Article : Google Scholar
|
|
9
|
Clarke NW, Hart CA and Brown MD: Molecular
mechanisms of metastasis in prostate cancer. Asian J Androl.
11:57–67. 2009. View Article : Google Scholar
|
|
10
|
Talreja DB: Importance of antiresorptive
therapies for patients with bone metastases from solid tumors.
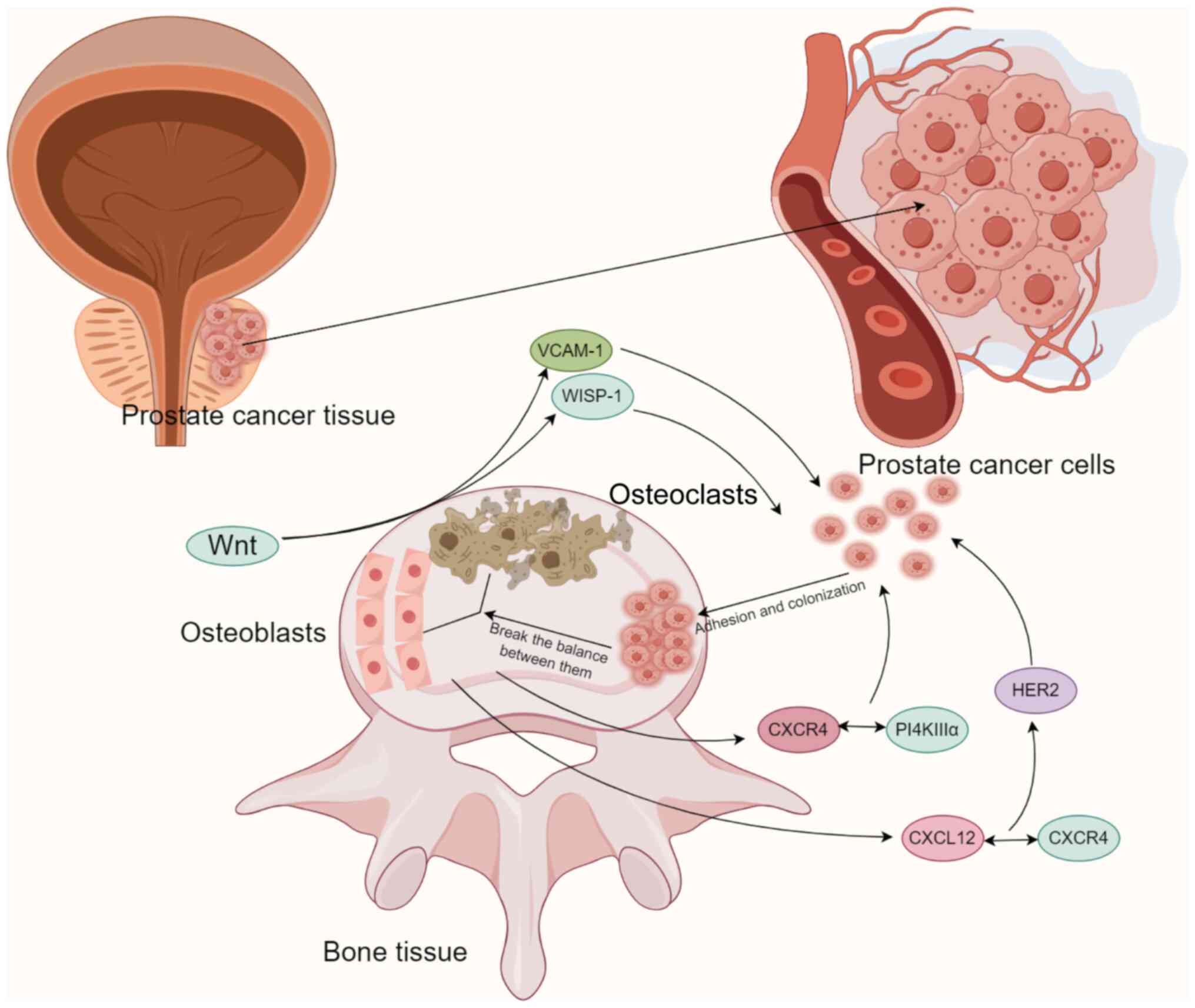
Cancer Manag Res. 4:287–297. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Coleman RE: Clinical features of
metastatic bone disease and risk of skeletal morbidity. Clin Cancer
Res. 12:6243s–6249s. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Nørgaard M, Jensen AØ, Jacobsen JB, Cetin
K, Fryzek JP and Sørensen HT: Skeletal related events, bone
metastasis and survival of prostate cancer: A population based
cohort study in Denmark (1999 to 2007). J Urol. 184:162–167. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Zhang X: Interactions between cancer cells
and bone microenvironment promote bone metastasis in prostate
cancer. Cancer Commun (Lond). 39:762019. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kang J, La Manna F, Bonollo F, Sampson N,
Alberts IL, Mingels C, Afshar-Oromieh A, Thalmann GN and
Karkampouna S: Tumor microenvironment mechanisms and bone
metastatic disease progression of prostate cancer. Cancer Lett.
530:156–169. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Singh DK, Patel VG, Oh WK and
Aguirre-Ghiso JA: Prostate cancer dormancy and reactivation in bone
marrow. J Clin Med. 10:26482021. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Bedeschi M, Marino N, Cavassi E, Piccinini
F and Tesei A: Cancer-associated fibroblast: Role in prostate
cancer progression to metastatic disease and therapeutic
resistance. Cells. 12:8022023. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Kim JM, Lin C, Stavre Z, Greenblatt MB and
Shim JH: Osteoblast-osteoclast communication and bone homeostasis.
Cells. 9:20732020. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Mughees M, Kaushal JB, Sharma G, Wajid S,
Batra SK and Siddiqui JA: Chemokines and cytokines: Axis and allies
in prostate cancer pathogenesis. Semin Cancer Biol. 86:497–512.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Gartrell BA, Coleman R, Efstathiou E,
Fizazi K, Logothetis CJ, Smith MR, Sonpavde G, Sartor O and Saad F:
Metastatic prostate cancer and the bone: Significance and
therapeutic options. Eur Urol. 68:850–858. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ban J, Fock V, Aryee DNT and Kovar H:
Mechanisms, diagnosis and treatment of bone metastases. Cells.
10:29442021. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Deng X, He G, Liu J, Luo F, Peng X, Tang
S, Gao Z, Lin Q, Keller JM, Yang T and Keller ET: Recent advances
in bone-targeted therapies of metastatic prostate cancer. Cancer
Treat Rev. 40:730–738. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Baci D, Bruno A, Cascini C, Gallazzi M,
Mortara L, Sessa F, Pelosi G, Albini A and Noonan DM:
Acetyl-L-carnitine downregulates invasion (CXCR4/CXCL12, MMP-9) and
angiogenesis (VEGF, CXCL8) pathways in prostate cancer cells:
Rationale for prevention and interception strategies. J Exp Clin
Cancer Res. 38:4642019. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Midavaine É, Côté J and Sarret P: The
multifaceted roles of the chemokines CCL2 and CXCL12 in osteophilic
metastatic cancers. Cancer Metastasis Rev. 40:427–445. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Cioni B, Nevedomskaya E, Melis MHM, van
Burgsteden J, Stelloo S, Hodel E, Spinozzi D, de Jong J, van der
Poel H, de Boer JP, et al: Loss of androgen receptor signaling in
prostate cancer-associated fibroblasts (CAFs) promotes CCL2- and
CXCL8-mediated cancer cell migration. Mol Oncol. 12:1308–1323.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Siddiqui JA, Seshacharyulu P, Muniyan S,
Pothuraju R, Khan P, Vengoji R, Chaudhary S, Maurya SK, Lele SM,
Jain M, et al: GDF15 promotes prostate cancer bone metastasis and
colonization through osteoblastic CCL2 and RANKL activation. Bone
Res. 10:62022. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Li Y, He Y, Butler W, Xu L, Chang Y, Lei
K, Zhang H, Zhou Y, Gao AC, Zhang Q, et al: Targeting cellular
heterogeneity with CXCR2 blockade for the treatment of
therapy-resistant prostate cancer. Sci Transl Med. 11:eaax04282019.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Singh R, Kapur N, Mir H, Singh N, Lillard
JW Jr and Singh S: CXCR6-CXCL16 axis promotes prostate cancer by
mediating cytoskeleton rearrangement via Ezrin activation and αvβ3
integrin clustering. Oncotarget. 7:7343–7353. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Connell B, Kopach P, Ren W, Joshi R, Naber
S, Zhou M and Mathew P: Aberrant integrin αv and α5 expression in
prostate adenocarcinomas and bone-metastases is consistent with a
bone-colonizing phenotype. Transl Androl Urol. 9:1630–1638. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Massagué J and Obenauf AC: Metastatic
colonization by circulating tumour cells. Nature. 529:298–306.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Quayle L, Ottewell PD and Holen I: Bone
metastasis: Molecular mechanisms implicated in tumour cell dormancy
in breast and prostate cancer. Curr Cancer Drug Targets.
15:469–480. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Yumoto K, Eber MR, Wang J, Cackowski FC,
Decker AM, Lee E, Nobre AR, Aguirre-Ghiso JA, Jung Y and Taichman
RS: Axl is required for TGF-β2-induced dormancy of prostate cancer
cells in the bone marrow. Sci Rep. 6:365202016. View Article : Google Scholar
|
|
32
|
Kobayashi A, Okuda H, Xing F, Pandey PR,
Watabe M, Hirota S, Pai SK, Liu W, Fukuda K, Chambers C, et al:
Bone morphogenetic protein 7 in dormancy and metastasis of prostate
cancer stem-like cells in bone. J Exp Med. 208:2641–2655. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Park M, Cho YJ, Kim B, Ko YJ, Jang Y, Moon
YH, Hyun H and Lim W: RANKL immunisation inhibits prostate cancer
metastasis by modulating EMT through a RANKL-dependent pathway. Sci
Rep. 11:121862021. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Ren D, Dai Y, Yang Q, Zhang X, Guo W, Ye
L, Huang S, Chen X, Lai Y, Du H, et al: Wnt5a induces and maintains
prostate cancer cells dormancy in bone. J Exp Med. 216:428–449.
2019. View Article : Google Scholar :
|
|
35
|
Ruppender N, Larson S, Lakely B, Kollath
L, Brown L, Coleman I, Coleman R, Nguyen H, Nelson PS, Corey E, et
al: Cellular adhesion promotes prostate cancer cells escape from
dormancy. PLoS One. 10:e01305652015. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Rojas A, Liu G, Coleman I, Nelson PS,
Zhang M, Dash R, Fisher PB, Plymate SR and Wu JD: IL-6 promotes
prostate tumorigenesis and progression through autocrine
cross-activation of IGF-IR. Oncogene. 30:2345–2355. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Danilucci TM, Santos PK, Pachane BC,
Pisani GFD, Lino RLB, Casali BC, Altei WF and Selistre-de-Araujo
HS: Recombinant RGD-disintegrin DisBa-01 blocks integrin
αvβ3 and impairs VEGF signaling in
endothelial cells. Cell Commun Signal. 17:272019. View Article : Google Scholar
|
|
38
|
Hashemi M, Taheriazam A, Daneii P,
Hassanpour A, Kakavand A, Rezaei S, Hejazi ES, Aboutalebi M,
Gholamrezaie H, Saebfar H, et al: Targeting PI3K/Akt signaling in
prostate cancer therapy. J Cell Commun Signal. 17:423–443. 2023.
View Article : Google Scholar :
|
|
39
|
Cooper CR and Pienta KJ: Cell adhesion and
chemotaxis in prostate cancer metastasis to bone: A minireview.
Prostate Cancer Prostatic Dis. 3:6–12. 2000. View Article : Google Scholar
|
|
40
|
Yin JJ, Pollock CB and Kelly K: Mechanisms
of cancer metastasis to the bone. Cell Res. 15:57–62. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Zhang Y, Liang J, Liu P, Wang Q, Liu L and
Zhao H: The RANK/RANKL/OPG system and tumor bone metastasis:
Potential mechanisms and therapeutic strategies. Front Endocrinol
(Lausanne). 13:10638152022. View Article : Google Scholar
|
|
42
|
Wong SK, Mohamad NV, Giaze TR, Chin KY,
Mohamed N and Ima-Nirwana S: Prostate cancer and bone metastases:
The underlying mechanisms. Int J Mol Sci. 20:25872019. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Kim SW, Kim JS, Papadopoulos J, Choi HJ,
He J, Maya M, Langley RR, Fan D, Fidler IJ and Kim SJ: Consistent
interactions between tumor cell IL-6 and macrophage TNF-α enhance
the growth of human prostate cancer cells in the bone of nude
mouse. Int Immunopharmacol. 11:862–872. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Baldessari C, Pipitone S, Molinaro E,
Cerma K, Fanelli M, Nasso C, Oltrecolli M, Pirola M, D'Agostino E,
Pugliese G, et al: Bone metastases and health in prostate cancer:
From pathophysiology to clinical implications. Cancers (Basel).
15:15182023. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Vičić I and Belev B: The pathogenesis of
bone metastasis in solid tumors: A review. Croat Med J. 62:270–282.
2021. View Article : Google Scholar
|
|
46
|
Yu H, Lin L, Zhang Z, Zhang H and Hu H:
Targeting NF-κB pathway for the therapy of diseases: Mechanism and
clinical study. Signal Transduct Target Ther. 5:2092020. View Article : Google Scholar
|
|
47
|
Verzella D, Fischietti M, Capece D,
Vecchiotti D, Del Vecchio F, Cicciarelli G, Mastroiaco V, Tessitore
A, Alesse E and Zazzeroni F: Targeting the NF-κB pathway in
prostate cancer: A promising therapeutic approach? Curr Drug
Targets. 17:311–320. 2016. View Article : Google Scholar
|
|
48
|
Al-Rashidi RR, Noraldeen SAM, Kareem AK,
Mahmoud AK, Kadhum WR, Ramírez-Coronel AA, Iswanto AH, Obaid RF,
Jalil AT, Mustafa YF, et al: Malignant function of nuclear
factor-kappaB axis in prostate cancer: Molecular interactions and
regulation by non-coding RNAs. Pharmacol Res. 194:1067752023.
View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Zhu W, Hu X, Xu J, Cheng Y, Shao Y and
Peng Y: Effect of PI3K/Akt signaling pathway on the process of
prostate cancer metastasis to bone. Cell Biochem Biophys.
72:171–177. 2015. View Article : Google Scholar
|
|
50
|
Ziaee S and Chung LW: Induction of
integrin α2 in a highly bone metastatic human prostate cancer cell
line: Roles of RANKL and AR under three-dimensional suspension
culture. Mol Cancer. 13:2082014. View Article : Google Scholar
|
|
51
|
Yin J, Liu YN, Tillman H, Barrett B,
Hewitt S, Ylaya K, Fang L, Lake R, Corey E, Morrissey C, et al:
AR-regulated TWEAK-FN14 pathway promotes prostate cancer bone
metastasis. Cancer Res. 74:4306–4317. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Lee C, Whang YM, Campbell P, Mulcrone PL,
Elefteriou F, Cho SW and Park SI: Dual targeting c-met and VEGFR2
in osteoblasts suppresses growth and osteolysis of prostate cancer
bone metastasis. Cancer Lett. 414:205–213. 2018. View Article : Google Scholar
|
|
53
|
Choi SY, Jeon JM, Na AY, Kwon OK, Bang IH,
Ha YS, Bae EJ, Park BH, Lee EH, Kwon TG, et al: SIRT5 directly
inhibits the PI3K/AKT pathway in prostate cancer cell lines. Cancer
Genomics Proteomics. 19:50–59. 2022. View Article : Google Scholar :
|
|
54
|
Chen JR, Zhao JT and Xie ZZ:
Integrin-mediated cancer progression as a specific target in
clinical therapy. Biomed Pharmacother. 155:1137452022. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Hamidi H and Ivaska J: Every step of the
way: Integrins in cancer progression and metastasis. Nat Rev
Cancer. 18:533–548. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Li M, Wang Y, Li M, Wu X, Setrerrahmane S
and Xu H: Integrins as attractive targets for cancer therapeutics.
Acta Pharm Sin B. 11:2726–2737. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Giancotti FG and Ruoslahti E: Integrin
signaling. Science. 285:1028–1032. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Hynes RO: Integrins: Versatility,
modulation, and signaling in cell adhesion. Cell. 69:11–25. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Cooper J and Giancotti FG: Integrin
signaling in cancer: Mechanotransduction, stemness, epithelial
plasticity, and therapeutic resistance. Cancer Cell. 35:347–367.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Jin JK, Tien PC, Cheng CJ, Song JH, Huang
C, Lin SH and Gallick GE: Talin1 phosphorylation activates β1
integrins: A novel mechanism to promote prostate cancer bone
metastasis. Oncogene. 34:1811–1821. 2015. View Article : Google Scholar
|
|
61
|
Chen PC, Tang CH, Lin LW, Tsai CH, Chu CY,
Lin TH and Huang YL: Thrombospondin-2 promotes prostate cancer bone
metastasis by the up-regulation of matrix metalloproteinase-2
through down-regulating miR-376c expression. J Hematol Oncol.
10:332017. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Krishnamurthy N and Kurzrock R: Targeting
the Wnt/beta-catenin pathway in cancer: Update on effectors and
inhibitors. Cancer Treat Rev. 62:50–60. 2018. View Article : Google Scholar
|
|
63
|
Yu F, Yu C, Li F, Zuo Y, Wang Y, Yao L, Wu
C, Wang C and Ye L: Wnt/β-catenin signaling in cancers and targeted
therapies. Signal Transduct Target Ther. 6:3072021. View Article : Google Scholar
|
|
64
|
Li Q, Ye L, Zhang X, Wang M, Lin C, Huang
S, Guo W, Lai Y, Du H, Li J, et al: FZD8, a target of p53, promotes
bone metastasis in prostate cancer by activating canonical
Wnt/β-catenin signaling. Cancer Lett. 402:166–176. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Nandana S, Tripathi M, Duan P, Chu CY,
Mishra R, Liu C, Jin R, Yamashita H, Zayzafoon M, Bhowmick NA, et
al: Bone metastasis of prostate cancer can be therapeutically
targeted at the TBX2-WNT signaling axis. Cancer Res. 77:1331–1344.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Peng S, Chen X, Huang C, Yang C, Situ M,
Zhou Q, Ling Y, Huang H, Huang M, Zhang Y, et al: UBE2S as a novel
ubiquitinated regulator of p16 and β-catenin to promote bone
metastasis of prostate cancer. Int J Biol Sci. 18:3528–3543. 2022.
View Article : Google Scholar :
|
|
67
|
Tang DG: Understanding and targeting
prostate cancer cell heterogeneity and plasticity. Semin Cancer
Biol. 82:68–93. 2022. View Article : Google Scholar :
|
|
68
|
Wolf I, Gratzke C and Wolf P: Prostate
cancer stem cells: Clinical aspects and targeted therapies. Front
Oncol. 12:9357152022. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Pittet MJ, Michielin O and Migliorini D:
Clinical relevance of tumour-associated macrophages. Nat Rev Clin
Oncol. 19:402–421. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Huang R, Wang S, Wang N, Zheng Y, Zhou J,
Yang B, Wang X, Zhang J, Guo L, Wang S, et al: CCL5 derived from
tumor-associated macrophages promotes prostate cancer stem cells
and metastasis via activating β-catenin/STAT3 signaling. Cell Death
Dis. 11:2342020. View Article : Google Scholar
|
|
71
|
Zhang S, Lv C, Niu Y, Li C, Li X, Shang Y,
Zhang Y, Zhang Y, Zhang Y and Zeng Y: RBM3 suppresses stemness
remodeling of prostate cancer in bone microenvironment by
modulating N6-methyladenosine on CTNNB1 mRNA. Cell Death Dis.
14:912023. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Meng X, Vander Ark A, Daft P, Woodford E,
Wang J, Madaj Z and Li X: Loss of TGF-β signaling in osteoblasts
increases basic-FGF and promotes prostate cancer bone metastasis.
Cancer Lett. 418:109–118. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Liu X, Chen L, Fan Y, Hong Y, Yang X, Li
Y, Lu J, Lv J, Pan X, Qu F, et al: IFITM3 promotes bone metastasis
of prostate cancer cells by mediating activation of the TGF-β
signaling pathway. Cell Death Dis. 10:5172019. View Article : Google Scholar
|
|
74
|
Yan Z, Jin S, Wei Z, Huilian H, Zhanhai Y,
Yue T, Juan L, Jing L, Libo Y and Xu L: Discoidin domain receptor 2
facilitates prostate cancer bone metastasis via regulating
parathyroid hormone-related protein. Biochim Biophys Acta.
1842:1350–1363. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Lin SR, Mokgautsi N and Liu YN: Ras and
Wnt interaction contribute in prostate cancer bone metastasis.
Molecules. 25:23802020. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Yang Q, Lang C, Wu Z, Dai Y, He S, Guo W,
Huang S, Du H, Ren D and Peng X: MAZ promotes prostate cancer bone
metastasis through transcriptionally activating the KRas-dependent
RalGEFs pathway. J Exp Clin Cancer Res. 38:3912019. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Eswarakumar VP, Lax I and Schlessinger J:
Cellular signaling by fibroblast growth factor receptors. Cytokine
Growth Factor Rev. 16:139–149. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Labanca E, Yang J, Shepherd PDA, Wan X,
Starbuck MW, Guerra LD, Anselmino N, Bizzotto JA, Dong J,
Chinnaiyan AM, et al: Fibroblast growth factor receptor 1 drives
the metastatic progression of prostate cancer. Eur Urol Oncol.
5:164–175. 2022. View Article : Google Scholar
|
|
79
|
Tai HC, Chang AC, Yu HJ, Huang CY, Tsai
YC, Lai YW, Sun HL, Tang CH and Wang SW: Osteoblast-derived
WNT-induced secreted protein 1 increases VCAM-1 expression and
enhances prostate cancer metastasis by down-regulating miR-126.
Oncotarget. 5:7589–7598. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Chang AC, Chen PC, Lin YF, Su CM, Liu JF,
Lin TH, Chuang SM and Tang CH: Osteoblast-secreted WISP-1 promotes
adherence of prostate cancer cells to bone via the VCAM-1/integrin
α4β1 system. Cancer Lett. 426:47–56. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Liu Q, Li A, Tian Y, Wu JD, Liu Y, Li T,
Chen Y, Han X and Wu K: The CXCL8-CXCR1/2 pathways in cancer.
Cytokine Growth Factor Rev. 31:61–71. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Hao Q, Vadgama JV and Wang P: CCL2/CCR2
signaling in cancer pathogenesis. Cell Commun Signal. 18:822020.
View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Johnson CS and Cook LM: Osteoid
cell-derived chemokines drive bone-metastatic prostate cancer.
Front Oncol. 13:11005852023. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Govindarajan B, Sbrissa D, Pressprich M,
Kim S, Vaishampayan U, Cher ML and Chinni S: Adaptor proteins
mediate CXCR4 and PI4KA crosstalk in prostate cancer cells and the
significance of PI4KA in bone tumor growth. Res Sq [Preprint]:
rs.3.rs-2590830. 2023.
|
|
85
|
Conley-LaComb MK, Semaan L, Singareddy R,
Li Y, Heath EI, Kim S, Cher ML and Chinni SR: Pharmacological
targeting of CXCL12/CXCR4 signaling in prostate cancer bone
metastasis. Mol Cancer. 15:682016. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Zhang B, Li Y, Wu Q, Xie L, Barwick B, Fu
C, Li X, Wu D, Xia S, Chen J, et al: Acetylation of KLF5 maintains
EMT and tumorigenicity to cause chemoresistant bone metastasis in
prostate cancer. Nat Commun. 12:17142021. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Zhang Z, Karthaus WR, Lee YS, Gao VR, Wu
C, Russo JW, Liu M, Mota JM, Abida W, Linton E, et al: Tumor
microenvironment-derived NRG1 promotes antiandrogen resistance in
prostate cancer. Cancer Cell. 38:279–296.e9. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Yin C, Wang M, Wang Y, Lin Q, Lin K, Du H,
Lang C, Dai Y and Peng X: BHLHE22 drives the immunosuppressive bone
tumor microenvironment and associated bone metastasis in prostate
cancer. J Immunother Cancer. 11:e0055322023. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Kolonin MG, Sergeeva A, Staquicini DI,
Smith TL, Tarleton CA, Molldrem JJ, Sidman RL, Marchiò S,
Pasqualini R and Arap W: Interaction between tumor cell surface
receptor RAGE and proteinase 3 mediates prostate cancer metastasis
to bone. Cancer Res. 77:3144–3150. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Zhao Z, Li E, Luo L, Zhao S, Liu L, Wang
J, Kang R and Luo J: A PSCA/PGRN-NF-κB-integrin-α4 axis promotes
prostate cancer cell adhesion to bone marrow endothelium and
enhances metastatic potential. Mol Cancer Res. 18:501–513. 2020.
View Article : Google Scholar
|
|
91
|
Geng X, Chang B and Shan J: Role and
correlation of exosomes and integrins in bone metastasis of
prostate cancer. Andrologia. 54:e145502022. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Borel M, Lollo G, Magne D, Buchet R,
Brizuela L and Mebarek S: Prostate cancer-derived exosomes promote
osteoblast differentiation and activity through phospholipase D2.
Biochim Biophys Acta Mol Basis Dis. 1866:1659192020. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Urabe F, Kosaka N, Yamamoto Y, Ito K,
Otsuka K, Soekmadji C, Egawa S, Kimura T and Ochiya T: Metastatic
prostate cancer-derived extracellular vesicles facilitate
osteoclastogenesis by transferring the CDCP1 protein. J Extracell
Vesicles. 12:e123122023. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Yu G, Shen P, Lee YC, Pan J, Song JH, Pan
T, Lin SC, Liang X, Wang G, Panaretakis T, et al: Multiple pathways
coordinating reprogramming of endothelial cells into osteoblasts by
BMP4. iScience. 24:1023882021. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Lee YC, Lin SC, Yu G, Zhu M, Song JH,
Rivera K, Pappin DJ, Logothetis CJ, Panaretakis T, Wang G, et al:
Prostate tumor-induced stromal reprogramming generates tenascin C
that promotes prostate cancer metastasis through YAP/TAZ
inhibition. Oncogene. 41:757–769. 2022. View Article : Google Scholar :
|
|
96
|
Wang H, Zhang M, Lu W and Yuan C: Prostate
cancer cell-derived spondin 2 boosts osteogenic factor levels in
osteoblasts via the PI3K/AKT/mTOR pathway. Oncol Rep. 49:232023.
View Article : Google Scholar
|
|
97
|
Fizazi K, Carducci M, Smith M, Damião R,
Brown J, Karsh L, Milecki P, Shore N, Rader M, Wang H, et al:
Denosumab versus zoledronic acid for treatment of bone metastases
in men with castration-resistant prostate cancer: A randomised,
double-blind study. Lancet. 377:813–822. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Henry D, Vadhan-Raj S, Hirsh V, von Moos
R, Hungria V, Costa L, Woll PJ, Scagliotti G, Smith G, Feng A, et
al: Delaying skeletal-related events in a randomized phase 3 study
of denosumab versus zoledronic acid in patients with advanced
cancer: An analysis of data from patients with solid tumors.
Support Care Cancer. 22:679–687. 2014. View Article : Google Scholar
|
|
99
|
Shenderov E, Boudadi K, Fu W, Wang H,
Sullivan R, Jordan A, Dowling D, Harb R, Schonhoft J, Jendrisak A,
et al: Nivolumab plus ipilimumab, with or without enzalutamide, in
AR-V7-expressing metastatic castration-resistant prostate cancer: A
phase-2 nonrandomized clinical trial. Prostate. 81:326–338. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Subudhi SK, Siddiqui BA, Aparicio AM,
Yadav SS, Basu S, Chen H, Jindal S, Tidwell RSS, Varma A,
Logothetis CJ, et al: Combined CTLA-4 and PD-L1 blockade in
patients with chemotherapy-naïve metastatic castration-resistant
prostate cancer is associated with increased myeloid and neutrophil
immune subsets in the bone microenvironment. J Immunother Cancer.
9:e0029192021. View Article : Google Scholar
|
|
101
|
McNeel DG, Eickhoff JC, Wargowski E,
Johnson LE, Kyriakopoulos CE, Emamekhoo H, Lang JM, Brennan MJ and
Liu G: Phase 2 trial of T-cell activation using MVI-816 and
pembrolizumab in patients with metastatic, castration-resistant
prostate cancer (mCRPC). J Immunother Cancer. 10:e0041982022.
View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Kantoff PW, Higano CS, Shore ND, Berger
ER, Small EJ, Penson DF, Redfern CH, Ferrari AC, Dreicer R, Sims
RB, et al: Sipuleucel-T immunotherapy for castration-resistant
prostate cancer. N Engl J Med. 363:411–422. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Su P, Zhang M and Kang X: Targeting c-Met
in the treatment of urologic neoplasms: Current status and
challenges. Front Oncol. 13:10710302023. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Azad AA, Beardsley EK, Hotte SJ, Ellard
SL, Klotz L, Chin J, Kollmannsberger C, Mukherjee SD and Chi KN: A
randomized phase II efficacy and safety study of vandetanib
(ZD6474) in combination with bicalutamide versus bicalutamide alone
in patients with chemotherapy naïve castration-resistant prostate
cancer. Invest New Drugs. 32:746–752. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Maroto P, Porta C, Capdevila J, Apolo AB,
Viteri S, Rodriguez-Antona C, Martin L and Castellano D:
Cabozantinib for the treatment of solid tumors: A systematic
review. Ther Adv Med Oncol. 14:175883592211071122022. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Smith M, De Bono J, Sternberg C, Le Moulec
S, Oudard S, De Giorgi U, Krainer M, Bergman A, Hoelzer W, De Wit
R, et al: Phase III Study of cabozantinib in previously treated
metastatic castration-resistant prostate cancer: COMET-1. J Clin
Oncol. 34:3005–3013. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Sadaghiani MS, Sheikhbahaei S, Werner RA,
Pienta KJ, Pomper MG, Gorin MA, Solnes LB and Rowe SP:
177 Lu-PSMA radioligand therapy effectiveness in
metastatic castration-resistant prostate cancer: An updated
systematic review and meta-analysis. Prostate. 82:826–835. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Kim YJ and Kim YI: Therapeutic responses
and survival effects of 177Lu-PSMA-617 radioligand therapy in
metastatic castrate-resistant prostate cancer: A meta-analysis.
Clin Nucl Med. 43:728–734. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Thang SP, Violet J, Sandhu S, Iravani A,
Akhurst T, Kong G, Ravi Kumar A, Murphy DG, Williams SG, Hicks RJ
and Hofman MS: Poor outcomes for patients with metastatic
castration-resistant prostate cancer with low prostate-specific
membrane antigen (PSMA) expression deemed ineligible for
177Lu-labelled PSMA radioligand therapy. Eur Urol Oncol.
2:670–676. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Ma J, Li L, Liao T, Gong W and Zhang C:
Efficacy and safety of 225Ac-PSMA-617-targeted alpha
therapy in metastatic castration-resistant prostate cancer: A
systematic review and meta-analysis. Front Oncol. 12:7966572022.
View Article : Google Scholar
|
|
111
|
Ballal S, Yadav MP, Sahoo RK, Tripathi M,
Dwivedi SN and Bal C: 225 Ac-PSMA-617-targeted alpha
therapy for the treatment of metastatic castration-resistant
prostate cancer: A systematic review and meta-analysis. Prostate.
81:580–591. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Gao X, Li L, Cai X, Huang Q, Xiao J and
Cheng Y: Targeting nanoparticles for diagnosis and therapy of bone
tumors: Opportunities and challenges. Biomaterials. 265:1204042021.
View Article : Google Scholar
|
|
113
|
Chen G, Arns S and Young RN: Determination
of the rat in vivo pharmacokinetic profile of a bone-targeting
dual-action pro-drug for treatment of osteoporosis. Bioconjug Chem.
26:1095–1103. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Bighetti-Trevisan RL, Sousa LO, Castilho
RM and Almeida LO: Cancer stem cells: Powerful targets to improve
current anticancer therapeutics. Stem Cells Int. 2019:96180652019.
View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Garcia-Mayea Y, Mir C, Masson F, Paciucci
R and LLeonart ME: Insights into new mechanisms and models of
cancer stem cell multidrug resistance. Semin Cancer Biol.
60:166–180. 2020. View Article : Google Scholar
|
|
116
|
Riganti C, Contino M, Guglielmo S, Perrone
MG, Salaroglio IC, Milosevic V, Giampietro R, Leonetti F, Rolando
B, Lazzarato L, et al: Design, biological evaluation, and molecular
modeling of tetrahydroisoquinoline derivatives: Discovery of a
potent p-glycoprotein ligand overcoming multidrug resistance in
cancer stem cells. J Med Chem. 62:974–986. 2019. View Article : Google Scholar
|
|
117
|
Cho Y and Kim YK: Cancer stem cells as a
potential target to overcome multidrug resistance. Front Oncol.
10:7642020. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Wang X, Ma Z, Xiao Z, Liu H, Dou Z, Feng X
and Shi H: Chk1 knockdown confers radiosensitization in prostate
cancer stem cells. Oncol Rep. 28:2247–2254. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Mei W, Lin X, Kapoor A, Gu Y, Zhao K and
Tang D: The contributions of prostate cancer stem cells in prostate
cancer initiation and metastasis. Cancers (Basel). 11:4342019.
View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Domanska UM, Timmer-Bosscha H, Nagengast
WB, Oude Munnink TH, Kruizinga RC, Ananias HJ, Kliphuis NM, Huls G,
De Vries EG, de Jong IJ and Walenkamp AM: CXCR4 inhibition with
AMD3100 sensitizes prostate cancer to docetaxel chemotherapy.
Neoplasia. 14:709–718. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Ni J, Cozzi P, Beretov J, Duan W, Bucci J,
Graham P and Li Y: Epithelial cell adhesion molecule (EpCAM) is
involved in prostate cancer chemotherapy/radiotherapy response in
vivo. BMC Cancer. 18:10922018. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Yao L and Zhang X: Interaction between
prostate cancer stem cells and bone microenvironment regulates
prostate cancer bone metastasis and treatment resistance. J Cancer.
13:2757–2767. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Klaff R, Varenhorst E, Berglund A, Hedlund
PO, Sjöberg F and Sandblom G; SPCG-5 Study Group: Clinical
presentation and predictors of survival related to extent of bone
metastasis in 900 prostate cancer patients. Scand J Urol.
50:352–359. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Fizazi K, Massard C, Smith M, Rader M,
Brown J, Milecki P, Shore N, Oudard S, Karsh L, Carducci M, et al:
Bone-related parameters are the main prognostic factors for overall
survival in men with bone metastases from castration-resistant
prostate cancer. Eur Urol. 68:42–50. 2015. View Article : Google Scholar
|
|
125
|
Zhang J, Sun J, Bakht S and Hassan W:
Recent development and future prospects of molecular targeted
therapy in prostate cancer. Curr Mol Pharmacol. 15:159–169.
2022.
|
|
126
|
Liang XW, Liu B, Chen JC, Cao Z, Chu FR,
Lin X, Wang SZ and Wu JC: Characteristics and molecular mechanism
of drug-tolerant cells in cancer: A review. Front Oncol.
13:11774662023. View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Cai C, He HH, Gao S, Chen S, Yu Z, Gao Y,
Chen S, Chen MW, Zhang J, Ahmed M, et al: Lysine-specific
demethylase 1 has dual functions as a major regulator of androgen
receptor transcriptional activity. Cell Rep. 9:1618–1627. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Yatim A, Benne C, Sobhian B,
Laurent-Chabalier S, Deas O, Judde JG, Lelievre JD, Levy Y and
Benkirane M: NOTCH1 nuclear interactome reveals key regulators of
its transcriptional activity and oncogenic function. Mol Cell.
48:445–458. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Wissmann M, Yin N, Müller JM, Greschik H,
Fodor BD, Jenuwein T, Vogler C, Schneider R, Günther T, Buettner R,
et al: Cooperative demethylation by JMJD2C and LSD1 promotes
androgen receptor-dependent gene expression. Nat Cell Biol.
9:347–353. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Lynch JT, Harris WJ and Somervaille TC:
LSD1 inhibition: A therapeutic strategy in cancer? Expert Opin Ther
Targets. 16:1239–1249. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Maes T, Mascaró C, Ortega A, Lunardi S,
Ciceri F, Somervaille TC and Buesa C: KDM1 histone lysine
demethylases as targets for treatments of oncological and
neurodegenerative disease. Epigenomics. 7:609–626. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Liang Y, Ahmed M, Guo H, Soares F, Hua JT,
Gao S, Lu C, Poon C, Han W, Langstein J, et al: LSD1-mediated
epigenetic reprogramming drives CENPE expression and prostate
cancer progression. Cancer Res. 77:5479–5490. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Lu X, Fong KW, Gritsina G, Wang F, Baca
SC, Brea LT, Berchuck JE, Spisak S, Ross J, Morrissey C, et al:
HOXB13 suppresses de novo lipogenesis through HDAC3-mediated
epigenetic reprogramming in prostate cancer. Nat Genet. 54:670–683.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
134
|
Meacham CE and Morrison SJ: Tumour
heterogeneity and cancer cell plasticity. Nature. 501:328–337.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
135
|
Tanay A and Regev A: Scaling single-cell
genomics from phenomenology to mechanism. Nature. 541:331–338.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Apostolopoulos V, Thalhammer T, Tzakos AG
and Stojanovska L: Targeting antigens to dendritic cell receptors
for vaccine development. J Drug Deliv. 2013:8697182013. View Article : Google Scholar : PubMed/NCBI
|
|
137
|
Kwon ED, Drake CG, Scher HI, Fizazi K,
Bossi A, van den Eertwegh AJ, Krainer M, Houede N, Santos R,
Mahammedi H, et al: Ipilimumab versus placebo after radiotherapy in
patients with metastatic castration-resistant prostate cancer that
had progressed after docetaxel chemotherapy (CA184-043): A
multicentre, randomised, double-blind, phase 3 trial. Lancet Oncol.
15:700–712. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Fizazi K, Drake CG, Beer TM, Kwon ED,
Scher HI, Gerritsen WR, Bossi A, den Eertwegh AJMV, Krainer M,
Houede N, et al: Final analysis of the ipilimumab versus placebo
following radiotherapy phase III trial in postdocetaxel metastatic
castration-resistant prostate cancer identifies an excess of
long-term survivors. Eur Urol. 78:822–830. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
139
|
Hillerdal V, Ramachandran M, Leja J and
Essand M: Systemic treatment with CAR-engineered T cells against
PSCA delays subcutaneous tumor growth and prolongs survival of
mice. BMC Cancer. 14:302014. View Article : Google Scholar : PubMed/NCBI
|
|
140
|
Zhou JE, Yu J, Wang Y, Wang H, Wang J,
Wang Y, Yu L and Yan Z: ShRNA-mediated silencing of PD-1 augments
the efficacy of chimeric antigen receptor T cells on subcutaneous
prostate and leukemia xenograft. Biomed Pharmacother.
137:1113392021. View Article : Google Scholar : PubMed/NCBI
|
|
141
|
Wang D, Shao Y, Zhang X, Lu G and Liu B:
IL-23 and PSMA-targeted duo-CAR T cells in prostate cancer
eradication in a preclinical model. J Transl Med. 18:232020.
View Article : Google Scholar : PubMed/NCBI
|