|
1
|
Smith C, Gasparetto M, Jordan C, Pollyea
DA and Vasiliou V: The effects of alcohol and aldehyde
dehydrogenases on disorders of hematopoiesis. Adv Exp Med Biol.
815:349–359. 2015. View Article : Google Scholar
|
|
2
|
Duan X, Hu H, Wang L and Chen L: Aldehyde
dehydrogenase 1 family: A potential molecule target for diseases.
Cell Biol Int. May 27–2024.Epub ahead of print. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lavudi K, Nuguri SM, Pandey P, Kokkanti RR
and Wang QE: ALDH and cancer stem cells: Pathways, challenges, and
future directions in targeted therapy. Life Sci. 356:1230332024.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Vlahopoulos S, Pan L, Varisli L, Dancik
GM, Karantanos T and Boldogh I: OGG1 as an epigenetic reader
affects NFκB: What this means for cancer. Cancers (Basel).
16:1482023. View Article : Google Scholar
|
|
5
|
Vlahopoulos SA: Divergent processing of
cell stress signals as the basis of cancer progression: Licensing
NFκB on Chromatin. Int J Mol Sci. 25:86212024. View Article : Google Scholar
|
|
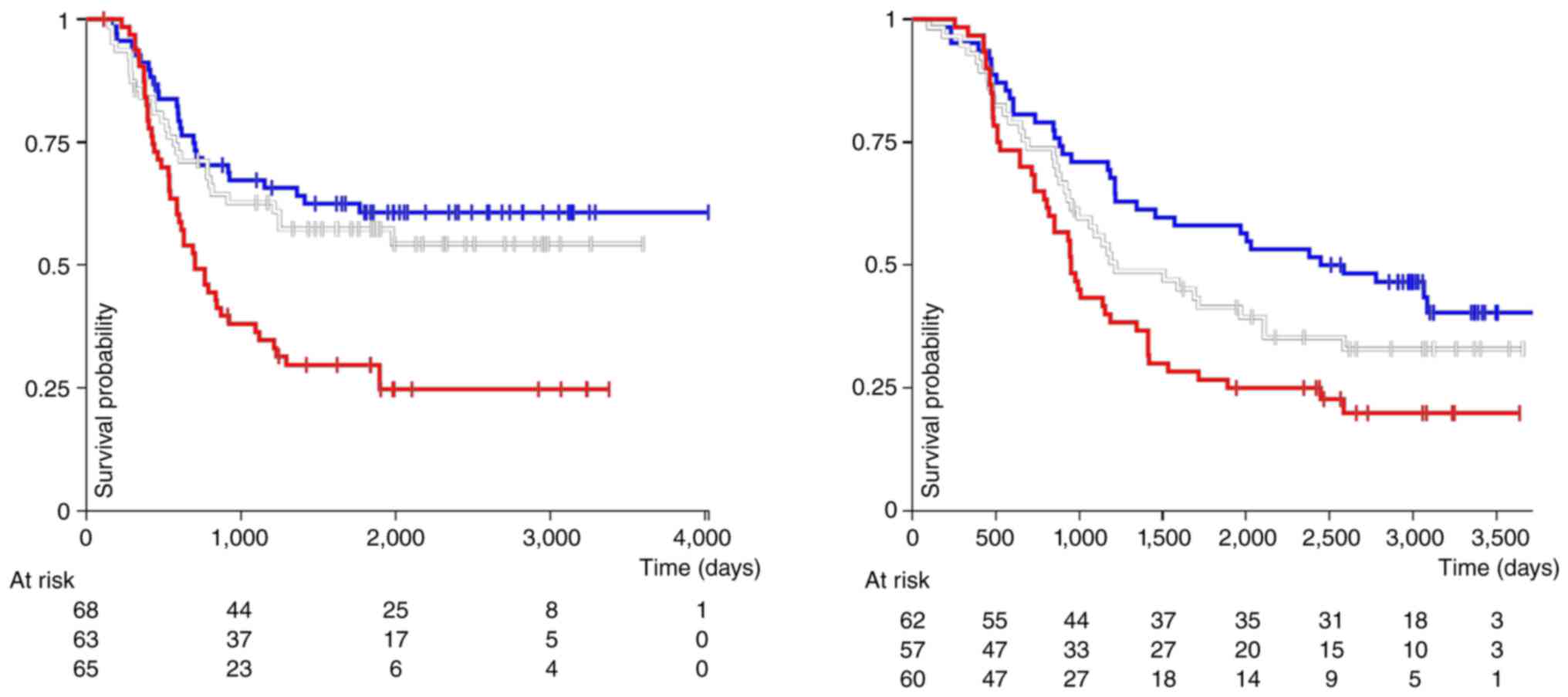
6
|
Carroll C, Manaprasertsak A, Boffelli
Castro A, van den Bos H, Spierings DCJ, Wardenaar R, Bukkuri A,
Engström N, Baratchart E, Yang M, et al: Drug-resilient Cancer Cell
Phenotype Is Acquired via Polyploidization Associated with Early
Stress Response Coupled to HIF2α Transcriptional Regulation. Cancer
Res Commun. 4:691–705. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Fredebohm J, Boettcher M, Eisen C, Gaida
MM, Heller A, Keleg S, Tost J, Greulich-Bode KM, Hotz-Wagenblatt A,
Lathrop M, et al: Establishment and characterization of a highly
tumourigenic and cancer stem cell enriched pancreatic cancer cell
line as a well defined model system. PLoS One. 7:e485032012.
View Article : Google Scholar : PubMed/NCBI
|
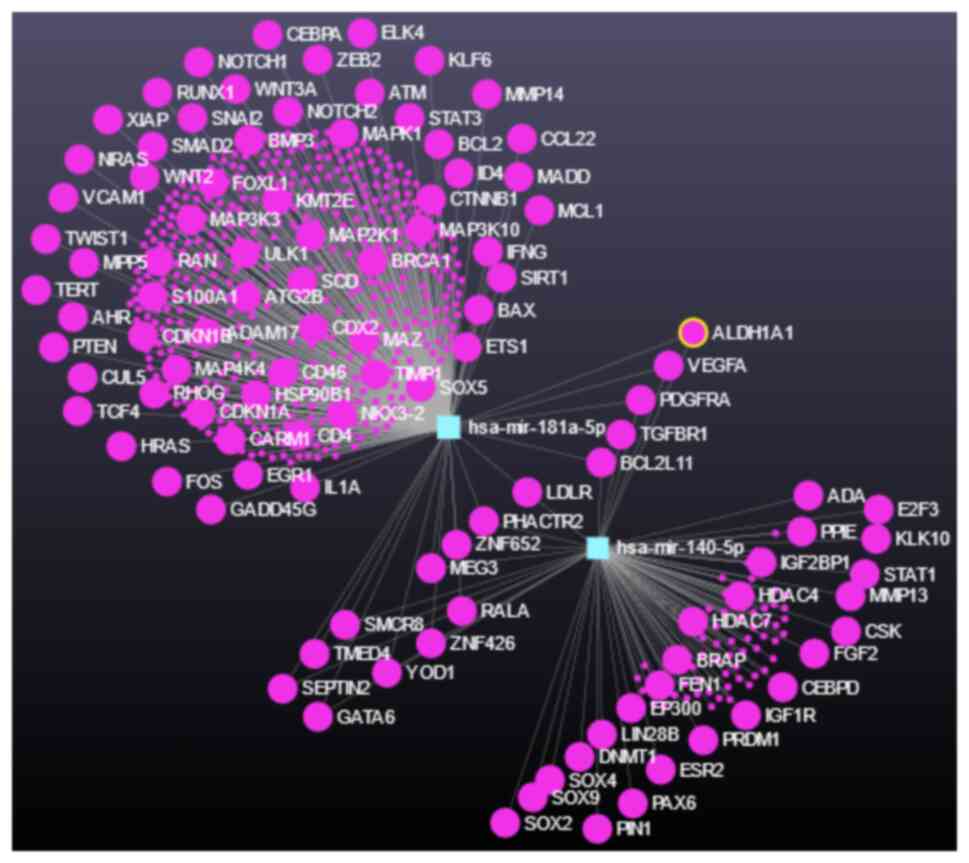
|
8
|
Kaigorodova EV, Kozik AV and Grishchenko
MY: Decoding Metastasis: From cell death to fusion in cancer
progression. Curr Cancer Drug Targets. Jul 15–2024.Epub ahead of
print. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Truskowski K, Amend SR and Pienta KJ:
Dormant cancer cells: Programmed quiescence, senescence, or both?
Cancer Metastasis Rev. 42:37–47. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Park MN: The therapeutic potential of a
strategy to prevent acute myeloid leukemia stem cell reprogramming
in older patients. Int J Mol Sci. 24:120372023. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Dancik GM, Varisli L and Vlahopoulos SA:
The molecular context of oxidant stress response in cancer
establishes ALDH1A1 as a Critical Target: What this means for acute
myeloid leukemia. Int J Mol Sci. 24:93722023. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Shortall K, Djeghader A, Magner E and
Soulimane T: Insights into aldehyde dehydrogenase enzymes: A
structural perspective. Front Mol Biosci. 8:6595502021. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Gasparetto M and Smith CA: ALDHs in normal
and malignant hematopoietic cells: Potential new avenues for
treatment of AML and other blood cancers. Chem Biol Interact.
276:46–51. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Yue H, Hu Z, Hu R, Guo Z, Zheng Y, Wang Y
and Zhou Y: ALDH1A1 in Cancers: Bidirectional function, drug
resistance, and regulatory mechanism. Front Oncol. 12:9187782022.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zhou Y, Huang G, Cai X, Liu Y, Qian B and
Li D: Global, regional, and national burden of acute myeloid
leukemia, 1990-2021: a systematic analysis for the global burden of
disease study 2021. Biomark Res. 12:1012024. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Magni M, Shammah S, Schiró R, Mellado W,
Dalla-Favera R and Gianni AM: Induction of
cyclophosphamide-resistance by aldehyde-dehydrogenase gene
transfer. Blood. 87:1097–1103. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Moreb JS, Maccow C, Schweder M and
Hecomovich J: Expression of antisense RNA to aldehyde dehydrogenase
class-1 sensitizes tumor cells to 4-hydroperoxycyclophosphamide in
vitro. J Pharmacol Exp Ther. 293:390–396. 2000.PubMed/NCBI
|
|
18
|
Smith C, Gasparetto M, Humphries K,
Pollyea DA, Vasiliou V and Jordan CT: Aldehyde dehydrogenases in
acute myeloid leukemia. Ann N Y Acad Sci. 1310:58–68. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Cheung AM, Wan TS, Leung JC, Chan LY,
Huang H, Kwong YL, Liang R and Leung AY: Aldehyde dehydrogenase
activity in leukemic blasts defines a subgroup of acute myeloid
leukemia with adverse prognosis and superior NOD/SCID engrafting
potential. Leukemia. 21:1423–1430. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Dancik GM, Voutsas IF and Vlahopoulos S:
Aldehyde dehydrogenase enzyme functions in acute leukemia stem
cells. Front Biosci (Sch Ed). 14:82022. View Article : Google Scholar
|
|
21
|
Hoang VT, Buss EC, Wang W, Hoffmann I,
Raffel S, Zepeda-Moreno A, Baran N, Wuchter P, Eckstein V, Trumpp
A, et al: The rarity of ALDH(+) cells is the key to separation of
normal versus leukemia stem cells by ALDH activity in AML patients.
Int J Cancer. 137:525–536. 2015. View Article : Google Scholar
|
|
22
|
Gasparetto M, Pei S, Minhajuddin M, Khan
N, Pollyea DA, Myers JR, Ashton JM, Becker MW, Vasiliou V,
Humphries KR, et al: Targeted therapy for a subset of acute myeloid
leukemias that lack expression of aldehyde dehydrogenase 1A1.
Haematologica. 102:1054–1065. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Batten DJ, Crofts JJ and Chuzhanova N:
Towards In Silico identification of genes contributing to
similarity of patients' multi-omics profiles: A case study of acute
myeloid leukemia. Genes (Basel). 14:17952023. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Dancik GM, Voutsas IF and Vlahopoulos S:
Lower RNA expression of ALDH1A1 distinguishes the favorable risk
group in acute myeloid leukemia. Mol Biol Rep. 49:3321–3331. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Dancik GM, Varisli L, Tolan V and
Vlahopoulos S: Aldehyde dehydrogenase genes as prospective
actionable targets in acute myeloid leukemia. Genes (Basel).
14:18072023. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Venton G, Pérez-Alea M, Baier C, Fournet
G, Quash G, Labiad Y, Martin G, Sanderson F, Poullin P, Suchon P,
et al: Aldehyde dehydrogenases inhibition eradicates leukemia stem
cells while sparing normal progenitors. Blood Cancer J. 6:e4692016.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Pei S, Minhajuddin M, Adane B, Khan N,
Stevens BM, Mack SC, Lai S, Rich JN, Inguva A, Shannon KM, et al:
AMPK/FIS1-Mediated mitophagy is required for self-renewal of human
AML stem cells. Cell Stem Cell. 23:86–100.e6. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Marcucci G, Mrózek K, Radmacher MD, Garzon
R and Bloomfield CD: The prognostic and functional role of
microRNAs in acute myeloid leukemia. Blood. 117:1121–1129. 2011.
View Article : Google Scholar :
|
|
29
|
Xiang M, Birkbak NJ, Vafaizadeh V, Walker
SR, Yeh JE, Liu S, Kroll Y, Boldin M, Taganov K, Groner B, et al:
STAT3 induction of miR-146b forms a feedback loop to inhibit the
NF-κB to IL-6 signaling axis and STAT3-driven cancer phenotypes.
Sci Signal. 7:ra112014. View Article : Google Scholar
|
|
30
|
Karin M: NF-kappaB as a critical link
between inflammation and cancer. Cold Spring Harb Perspect Biol.
1:a0001412009. View Article : Google Scholar
|
|
31
|
Vlahopoulos SA, Cen O, Hengen N, Agan J,
Moschovi M, Critselis E, Adamaki M, Bacopoulou F, Copland JA,
Boldogh I, et al: Dynamic aberrant NF-κB spurs tumorigenesis: a new
model encompassing the microenvironment. Cytokine Growth Factor
Rev. 26:389–403. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Jimbu L, Mesaros O, Joldes C, Neaga A,
Zaharie L and Zdrenghea M: MicroRNAs associated with a bad
prognosis in acute myeloid leukemia and their impact on macrophage
polarization. Biomedicines. 12:1212024. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Wallace JA and O'Connell RM: MicroRNAs and
acute myeloid leukemia: Therapeutic implications and emerging
concepts. Blood. 130:1290–1301. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Boudreau RL, Jiang P, Gilmore BL, Spengler
RM, Tirabassi R, Nelson JA, Ross CA, Xing Y and Davidson BL:
Transcriptome-wide discovery of microRNA binding sites in human
brain. Neuron. 81:294–305. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Lee SH, Lee CR, Rigas NK, Kim RH, Kang MK,
Park NH and Shin KH: Human papillomavirus 16 (HPV16) enhances tumor
growth and cancer stemness of HPV-negative oral/oropharyngeal
squamous cell carcinoma cells via miR-181 regulation.
Papillomavirus Res. 1:116–125. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Liu X, Liao W, Peng H, Luo X, Luo Z, Jiang
H and Xu L: miR-181a promotes G1/S transition and cell
proliferation in pediatric acute myeloid leukemia by targeting ATM.
J Cancer Res Clin Oncol. 142:77–87. 2016. View Article : Google Scholar
|
|
37
|
Nanbakhsh A, Visentin G, Olive D, Janji B,
Mussard E, Dessen P, Meurice G, Zhang Y, Louache F, Bourhis JH and
Chouaib S: miR-181a modulates acute myeloid leukemia susceptibility
to natural killer cells. Oncoimmunology. 4:e9964752015. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Huang X, Schwind S, Santhanam R, Eisfeld
AK, Chiang CL, Lankenau M, Yu B, Hoellerbauer P, Jin Y, Tarighat
SS, et al: Targeting the RAS/MAPK pathway with miR-181a in acute
myeloid leukemia. Oncotarget. 7:59273–59286. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Seipel K, Messerli C, Wiedemann G, Bacher
U and Pabst T: MN1, FOXP1 and hsa-miR-181a-5p as prognostic markers
in acute myeloid leukemia patients treated with intensive induction
chemotherapy and autologous stem cell transplantation. Leuk Res.
89:1062962020. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Fletcher D, Brown E, Javadala J,
Uysal-Onganer P and Guinn BA: microRNA expression in acute myeloid
leukaemia: New targets for therapy? EJHaem. 3:596–608. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Gong X, Xu B, Zi L and Chen X: miR-625
reverses multidrug resistance in gastric cancer cells by directly
targeting ALDH1A1. Cancer Manag Res. 11:6615–6624. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Ma L, Wang YY and Jiang P: LncRNA
LINC00909 promotes cell proliferation and metastasis in pediatric
acute myeloid leukemia via miR-625-mediated modulation of
Wnt/β-catenin signaling. Biochem Biophys Res Commun. 527:654–661.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Shang Z, Ming X, Wu J and Xiao Y:
Downregulation of circ_0012152 inhibits proliferation and induces
apoptosis in acute myeloid leukemia cells through the
miR-625-5p/SOX12 axis. Hematol Oncol. 39:539–548. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Aliabedi B, Mousavi SH, Ebrahimi M,
Alizadeh S, Hedayati Asl AA, Mohammad M and Samieyan Dehkordi S:
Hsa-miR-625 Upregulation promotes apoptosis in acute myeloid
leukemia cell line by targeting integrin-linked kinase pathway.
Asian Pac J Cancer Prev. 23:1159–1167. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Samieyan Dehkordi S, Mousavi SH, Ebrahimi
M, Alizadeh SH, Hedayati Asl AA, Mohammad M and Aliabedi B:
Upregulation of hsa-miR-625-5p inhibits invasion of acute myeloid
leukemia cancer cells through ILK/AKT Pathway. Cell J. 24:76–84.
2022.PubMed/NCBI
|
|
46
|
Li Q, Yao Y, Eades G, Liu Z, Zhang Y and
Zhou Q: Downregulation of miR-140 promotes cancer stem cell
formation in basal-like early stage breast cancer. Oncogene.
33:2589–2600. 2014. View Article : Google Scholar :
|
|
47
|
Li H, Bi K, Feng S, Wang Y and Zhu C:
MiR-140 Targets lncRNA DNAJC3-AS1 to Suppress Cell Proliferation in
Acute Myeloid Leukemia. Mediterr J Hematol Infect Dis.
14:e20220052022. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Wang Y, Wang F, Lu Y, Li Y, Ran H, Yan F
and Tian Y: MiR-140 targets lncRNA FAM230B to suppress cell
proliferation in acute myeloid leukemia running title: MiR-140
targets FAM230B in AML. Hematology. 27:700–705. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Huang J, Jin S, Guo R, Wu W, Yang C, Qin
Y, Chen Q, He X, Qu J and Yang Z: Histone lysine demethylase KDM5B
facilitates proliferation and suppresses apoptosis in human acute
myeloid leukemia cells through the miR-140-3p/BCL2 axis. RNA.
30:435–447. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Huang HY, Lin YC, Cui S, Huang Y, Tang Y,
Xu J, Bao J, Li Y, Wen J, Zuo H, et al: miRTarBase update 2022: an
informative resource for experimentally validated miRNA-target
interactions. Nucleic Acids Res. 50(D1): D222–D230. 2022.
View Article : Google Scholar
|
|
51
|
Kariuki D, Asam K, Aouizerat BE, Lewis KA,
Florez JC and Flowers E: Review of databases for experimentally
validated human microRNA-mRNA interactions. Database (Oxford).
2023:baad0142023. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Kern F, Aparicio-Puerta E, Li Y, Fehlmann
T, Kehl T, Wagner V, Ray K, Ludwig N, Lenhof HP, Meese E and Keller
A: miRTargetLink 2.0-interactive miRNA target gene and target
pathway networks. Nucleic Acids Res. 49(W1): W409–W416. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Wang W, Li Y, Liu N, Gao Y and Li L:
MiR-23b controls ALDH1A1 expression in cervical cancer stem cells.
BMC Cancer. 17:2922017. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Barrera-Ramirez J, Lavoie JR, Maganti HB,
Stanford WL, Ito C, Sabloff M, Brand M, Rosu-Myles M, Le Y and
Allan DS: Micro-RNA profiling of exosomes from marrow-derived
mesenchymal stromal cells in patients with acute myeloid leukemia:
Implications in Leukemogenesis. Stem Cell Rev Rep. 13:817–825.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Jiang W, Min J, Sui X, Qian Y, Liu Y, Liu
Z, Zhou H, Li X and Gong Y: MicroRNA-26a-5p and microRNA-23b-3p
up-regulate peroxiredoxin III in acute myeloid leukemia. Leuk
Lymphoma. 56:460–471. 2015. View Article : Google Scholar :
|
|
56
|
Gaál Z, Oláh É, Rejtő L, Bálint BL and
Csernoch L: Expression Levels of Warburg-Effect Related microRNAs
Correlate with each Other and that of Histone Deacetylase Enzymes
in Adult Hematological Malignancies with Emphasis on Acute Myeloid
Leukemia. Pathol Oncol Res. 23:207–216. 2017. View Article : Google Scholar
|
|
57
|
Sethupathy P, Corda B and Hatzigeorgiou
AG: TarBase: A comprehensive database of experimentally supported
animal microRNA targets. RNA. 12:192–197. 2006. View Article : Google Scholar :
|
|
58
|
Chang L, Zhou G, Soufan O and Xia J:
miRNet 2.0: Network-based visual analytics for miRNA functional
analysis and systems biology. Nucleic Acids Res. 48(W1): W244–W251.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Calin GA, Dumitru CD, Shimizu M, Bichi R,
Zupo S, Noch E, Aldler H, Rattan S, Keating M, Rai K, et al:
Frequent deletions and down-regulation of micro-RNA genes miR15 and
miR16 at 13q14 in chronic lymphocytic leukemia. Proc Natl Acad Sci
USA. 99:15524–15529. 2002. View Article : Google Scholar
|
|
60
|
Liberati FR, Di Russo S, Barolo L, Peruzzi
G, Farina MV, Spizzichino S, Di Fonzo F, Quaglio D, Pisano L, Botta
B, et al: Combined Delivery of miR-15/16 through Humanized ferritin
nanocages for the treatment of chronic lymphocytic leukemia.
Pharmaceutics. 16:4022024. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Gao SM, Yang J, Chen C, Zhang S, Xing CY,
Li H, Wu J and Jiang L: miR-15a/16-1 enhances retinoic
acid-mediated differentiation of leukemic cells and is up-regulated
by retinoic acid. Leuk Lymphoma. 52:2365–2371. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Kim KT, Carroll AP, Mashkani B, Cairns MJ,
Small D and Scott RJ: MicroRNA-16 is down-regulated in mutated FLT3
expressing murine myeloid FDC-P1 cells and interacts with Pim-1.
PLoS One. 7:e445462012. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Abraham M, Klein S, Bulvik B, Wald H,
Weiss ID, Olam D, Weiss L, Beider K, Eizenberg O and Wald O, et al:
The CXCR4 inhibitor BL-8040 induces the apoptosis of AML blasts by
downregulating ERK, BCL-2, MCL-1 and cyclin-D1 via altered
miR-15a/16-1 expression. Leukemia. 31:2336–2346. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Abdellateif MS, Hassan NM, Kamel MM and
El-Meligui YM: Bone marrow microRNA-34a is a good indicator for
response to treatment in acute myeloid leukemia. Oncol Res.
32:577–584. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Ma W, Xiao GG, Mao J, Lu Y, Song B, Wang
L, Fan S, Fan P, Hou Z, Li J, et al: Dysregulation of the
miR-34a-SIRT1 axis inhibits breast cancer stemness. Oncotarget.
6:10432–10444. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Hsieh PL, Liao YW, Hsieh CW, Chen PN and
Yu CC: Soy isoflavone genistein impedes cancer stemness and
mesenchymal transition in head and neck cancer through activating
miR-34a/RTCB Axis. Nutrients. 12:19242020. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Xu C, Cao X, Cao X, Liu L, Qiu Y, Li X,
Zhou L, Ning Y, Ren K and Cao J: Isovitexin Inhibits Stemness and
Induces Apoptosis in Hepatocellular Carcinoma SK-Hep-1 Spheroids by
Upregulating miR-34a Expression. Anticancer Agents Med Chem.
20:1654–1663. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Fuster O, Llop M, Dolz S, García P, Such
E, Ibáñez M, Luna I, Gómez I, López M, Cervera J, et al: Adverse
prognostic value of MYBL2 overexpression and association with
microRNA-30 family in acute myeloid leukemia patients. Leuk Res.
37:1690–1696. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Farzadfard E, Kalantari T and Tamaddon G:
Serum Expression of Seven MicroRNAs in Chronic Lymphocytic Leukemia
Patients. J Blood Med. 11:97–102. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Shiah SG, Hsiao JR, Chang HJ, Hsu YM, Wu
GH, Peng HY, Chou ST, Kuo CC and Chang JY: MiR-30a and miR-379
modulate retinoic acid pathway by targeting DNA methyltransferase
3B in oral cancer. J Biomed Sci. 27:462020. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Nurwidya F, Takahashi F, Winardi W, Tajima
K, Mitsuishi Y, Murakami A, Kobayashi I, Nara T, Hashimoto M, Kato
M, et al: Zinc-finger E-box-binding homeobox 1 (ZEB1) plays a
crucial role in the maintenance of lung cancer stem cells resistant
to gefitinib. Thorac Cancer. 12:1536–1548. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Hashida S, Yamamoto H, Shien K, Miyoshi Y,
Ohtsuka T, Suzawa K, Watanabe M, Maki Y, Soh J, Asano H, et al:
Acquisition of cancer stem cell-like properties in non-small cell
lung cancer with acquired resistance to afatinib. Cancer Sci.
106:1377–1384. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Pyzer AR, Stroopinsky D, Rosenblatt J,
Anastasiadou E, Rajabi H, Washington A, Tagde A, Chu JH, Coll M,
Jiao AL, et al: MUC1 inhibition leads to decrease in PD-L1 levels
via upregulation of miRNAs. Leukemia. 31:2780–2790. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Havelange V, Stauffer N, Heaphy CC,
Volinia S, Andreeff M, Marcucci G, Croce CM and Garzon R:
Functional implications of microRNAs in acute myeloid leukemia by
integrating microRNA and messenger RNA expression profiling.
Cancer. 117:4696–4706. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Thomsen KG, Terp MG, Lund RR, Søkilde R,
Elias D, Bak M, Litman T, Beck HC, Lyng MB and Ditzel HJ: miR-155,
identified as anti-metastatic by global miRNA profiling of a
metastasis model, inhibits cancer cell extravasation and
colonization in vivo and causes significant signaling alterations.
Oncotarget. 6:29224–29239. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Metzeler KH, Maharry K, Kohlschmidt J,
Volinia S, Mrózek K, Becker H, Nicolet D, Whitman SP, Mendler JH,
Schwind S, et al: A stem cell-like gene expression signature
associates with inferior outcomes and a distinct microRNA
expression profile in adults with primary cytogenetically normal
acute myeloid leukemia. Leukemia. 27:2023–2031. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Rizzo M, Mariani L, Pitto L, Rainaldi G
and Simili M: miR-20a and miR-290, multi-faceted players with a
role in tumourigenesis and senescence. J Cell Mol Med.
14:2633–2640. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Gerrits A, Walasek MA, Olthof S, Weersing
E, Ritsema M, Zwart E, van Os R, Bystrykh LV and de Haan G: Genetic
screen identifies microRNA cluster 99b/let-7e/125a as a regulator
of primitive hematopoietic cells. Blood. 119:377–387. 2012.
View Article : Google Scholar
|
|
79
|
Li Y, Vecchiarelli-Federico LM, Li YJ,
Egan SE, Spaner D, Hough MR and Ben-David Y: The miR-17-92 cluster
expands multipotent hematopoietic progenitors whereas imbalanced
expression of its individual oncogenic miRNAs promotes leukemia in
mice. Blood. 119:4486–4498. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Bousquet M, Harris MH, Zhou B and Lodish
HF: MicroRNA miR-125b causes leukemia. Proc Natl Acad Sci USA.
107:21558–21563. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Buettner R, Nguyen LXT, Kumar B, Morales
C, Liu C, Chen LS, Pemovska T, Synold TW, Palmer J, Thompson R, et
al: 8-chloro-adenosine activity in FLT3-ITD acute myeloid leukemia.
J Cell Physiol. 234:16295–16303. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Testa U and Pelosi E: MicroRNAs expressed
in hematopoietic stem/progenitor cells are deregulated in acute
myeloid leukemias. Leuk Lymphoma. 56:1466–1474. 2015. View Article : Google Scholar
|
|
83
|
Xu D, Jiang J, He G, Zhou H and Ji C:
miR-143-3p represses leukemia cell proliferation by inhibiting
KAT6A expression. Anticancer Drugs. 33:e662–e669. 2022. View Article : Google Scholar
|
|
84
|
Buggins AG, Milojkovic D, Arno MJ, Lea NC,
Mufti GJ, Thomas NS and Hirst WJ: Microenvironment produced by
acute myeloid leukemia cells prevents T cell activation and
proliferation by inhibition of NF-kappaB, c-Myc, and pRb pathways.
J Immunol. 167:6021–6030. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Sun YX, Kong HL, Liu CF, Yu S, Tian T, Ma
DX and Ji CY: The imbalanced profile and clinical significance of T
helper associated cytokines in bone marrow microenvironment of the
patients with acute myeloid leukemia. Hum Immunol. 75:113–118.
2014. View Article : Google Scholar
|
|
86
|
Alhattab DM, Isaioglou I, Alshehri S, Khan
ZN, Susapto HH, Li Y, Marghani Y, Alghuneim AA, Díaz-Rúa R,
Abdelrahman S, et al: Fabrication of a three-dimensional bone
marrow niche-like acute myeloid Leukemia disease model by an
automated and controlled process using a robotic multicellular
bioprinting system. Biomater Res. 27:1112023. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Ito S, Minamizaki T, Kohno S, Sotomaru Y,
Kitaura Y, Ohba S, Sugiyama T, Aubin JE, Tanimoto K and Yoshiko Y:
Overexpression of miR-125b in osteoblasts improves age-related
changes in bone mass and quality through suppression of osteoclast
formation. Int J Mol Sci. 22:67452021. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Pais H, Nicolas FE, Soond SM, Swingler TE,
Clark IM, Chantry A, Moulton V and Dalmay T: Analyzing mRNA
expression identifies Smad3 as a microRNA-140 target regulated only
at protein level. RNA. 16:489–494. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Varisli L and Vlahopoulos S:
Epithelial-Mesenchymal transition in acute leukemias. Int J Mol
Sci. 25:21732024. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Imodoye SO, Adedokun KA, Muhammed AO,
Bello IO, Muhibi MA, Oduola T and Oyenike MA: Understanding the
complex milieu of epithelial-mesenchymal transition in cancer
metastasis: New insight into the roles of transcription factors.
Front Oncol. 11:7628172021. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Mani SA, Guo W, Liao MJ, Eaton EN, Ayyanan
A, Zhou AY, Brooks M, Reinhard F, Zhang CC, Shipitsin M, et al: The
epithelial-mesenchymal transition generates cells with properties
of stem cells. Cell. 133:704–715. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Kong D, Banerjee S, Ahmad A, Li Y, Wang Z,
Sethi S and Sarkar FH: Epithelial to mesenchymal transition is
mechanistically linked with stem cell signatures in prostate cancer
cells. PLoS One. 5:e124452010. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Muraoka-Cook RS, Shin I, Yi JY, Easterly
E, Barcellos-Hoff MH, Yingling JM, Zent R and Arteaga CL: Activated
type I TGFbeta receptor kinase enhances the survival of mammary
epithelial cells and accelerates tumor progression. Oncogene.
25:3408–3423. 2006. View Article : Google Scholar
|
|
94
|
Gorodetska I, Lukiyanchuk V, Gawin M,
Sliusar M, Linge A, Lohaus F, Hölscher T, Kati Erdmann, Fuessel S,
Borkowetz A, et al: Blood-based detection of MMP11 as a marker of
prostate cancer progression regulated by the ALDH1A1-TGF-β1
signaling mechanism. bioRxiv: https://doi.org/10.1101/2024.07.16.603771.
|
|
95
|
Singh B, Murphy RF, Ding XZ, Roginsky AB,
Bell RH and Adrian TE: On the role of transforming growth
factor-beta in the growth inhibitory effects of retinoic acid in
human pancreatic cancer cells. Mol Cancer. 6:822007. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Seyhan AA: Trials and Tribulations of
MicroRNA Therapeutics. Int J Mol Sci. 25:14692024. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Hong DS, Kang YK, Borad M, Sachdev J,
Ejadi S, Lim HY, Brenner AJ, Park K, Lee JL, Kim TY, et al: Phase 1
study of MRX34, a liposomal miR-34a mimic, in patients with
advanced solid tumours. Br J Cancer. 122:1630–1637. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Witten L and Slack FJ: miR-155 as a novel
clinical target for hematological malignancies. Carcinogenesis.
41:2–7. 2020. View Article : Google Scholar
|
|
99
|
Gallant-Behm CL, Piper J, Lynch JM, Seto
AG, Hong SJ, Mustoe TA, Maari C, Pestano LA, Dalby CM, Jackson AL,
et al: A MicroRNA-29 Mimic (Remlarsen) Represses Extracellular
Matrix Expression and Fibroplasia in the Skin. J Invest Dermatol.
139:1073–1081. 2019. View Article : Google Scholar
|
|
100
|
Chioccioli M, Roy S, Newell R, Sauler M,
Ahangari F, Ding S, DeIuliis J, Aurelien N, Montgomery RL and
Kaminski N: A lung targeted miR-29 mimic as a therapy for pulmonary
fibrosis. EBioMedicine. 85:1043042022. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Narendra G, Raju B, Verma H and Silakari
O: Identification of potential genes associated with ALDH1A1
overexpression and cyclophosphamide resistance in chronic
myelogenous leukemia using network analysis. Med Oncol. 38:1232021.
View Article : Google Scholar : PubMed/NCBI
|
|
102
|
van Zandwijk N, Pavlakis N, Kao SC, Linton
A, Boyer MJ, Clarke S, Huynh Y, Chrzanowska A, Fulham MJ, Bailey
DL, et al: Safety and activity of microRNA-loaded minicells in
patients with recurrent malignant pleural mesothelioma: A
first-in-man, phase 1, open-label, dose-escalation study. Lancet
Oncol. 18:1386–1396. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Zanjirband M, Rahgozar S and Aberuyi N:
miR-16-5p enhances sensitivity to RG7388 through targeting PPM1D
expression (WIP1) in childhood acute lymphoblastic leukemia. Cancer
Drug Resist. 6:242–256. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Zhang J, Mullighan CG, Harvey RC, Wu G,
Chen X, Edmonson M, Buetow KH, Carroll WL, Chen IM, Devidas M, et
al: Key pathways are frequently mutated in high-risk childhood
acute lymphoblastic leukemia: a report from the Children's Oncology
Group. Blood. 118:3080–3087. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Huang BJ, Smith JL, Farrar JE, Wang YC,
Umeda M, Ries RE, Leonti AR, Crowgey E, Furlan SN, Tarlock K, et
al: Integrated stem cell signature and cytomolecular risk
determination in pediatric acute myeloid leukemia. Nat Commun.
13:54872022. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Won Lee G, Thangavelu M, Joung Choi M,
Yeong Shin E, Sol Kim H, Seon Baek J, Woon Jeong Y, Eun Song J,
Carlomagno C, Miguel Oliveira J, et al: Exosome mediated transfer
of miRNA-140 promotes enhanced chondrogenic differentiation of bone
marrow stem cells for enhanced cartilage repair and regeneration. J
Cell Biochem. 121:3642–3652. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Wang N, Liu X, Tang Z, Wei X, Dong H, Liu
Y, Wu H, Wu Z, Li X, Ma X and Guo Z: Increased BMSC exosomal
miR-140-3p alleviates bone degradation and promotes bone
restoration by targeting Plxnb1 in diabetic rats. J
Nanobiotechnology. 20:972022. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Rajagopal K, Arjunan P, Marepally S and
Madhuri V: Controlled differentiation of mesenchymal stem cells
into Hyaline Cartilage in miR-140-Activated Collagen Hydrogel.
Cartilage. 13(2_suppl): 571S–581S. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Zhou Y, Jia H, Hu A, Liu R, Zeng X and
Wang H: Nanoparticles targeting delivery antagomir-483-5p to bone
marrow mesenchymal stem cells treat osteoporosis by increasing bone
formation. Curr Stem Cell Res Ther. 18:115–126. 2023. View Article : Google Scholar
|
|
110
|
Diener C, Keller A and Meese E: Emerging
concepts of miRNA therapeutics: From cells to clinic. Trends Genet.
38:613–626. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Kim T and Croce CM: MicroRNA: Trends in
clinical trials of cancer diagnosis and therapy strategies. Exp Mol
Med. 55:1314–1321. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Grillone K, Caridà G, Luciano F, Cordua A,
Di Martino MT, Tagliaferri P and Tassone P: A systematic review of
non-coding RNA therapeutics in early clinical trials: A new
perspective against cancer. J Transl Med. 22:7312024. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Truong VA, Chang YH, Dang TQ, Tu Y, Tu J,
Chang CW, Chang YH, Liu GS and Hu YC: Programmable editing of
primary MicroRNA switches stem cell differentiation and improves
tissue regeneration. Nat Commun. 15:83582024. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Wen C, Xu X, Zhang Y, Xia J, Liang Y and
Xu L: Bone targeting nanoparticles for the treatment of
osteoporosis. Int J Nanomedicine. 19:1363–1383. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Gu J, Jiang L, Chen Z and Qi J: A simple
nanoplatform of thermo-sensitive liposomes and gold nanorods to
treat bone metastasis through improved chemotherapy combined with
photothermal therapy. Int J Pharm X. 8:1002822024.PubMed/NCBI
|
|
116
|
Li S, Kang Y and Zeng Y: Targeting tumor
and bone microenvironment: Novel therapeutic opportunities for
castration-resistant prostate cancer patients with bone metastasis.
Biochim Biophys Acta Rev Cancer. 1879:1890332024. View Article : Google Scholar
|
|
117
|
Xu M and Li S: Nano-drug delivery system
targeting tumor microenvironment: A prospective strategy for
melanoma treatment. Cancer Lett. 574:2163972023. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
de Janon A, Mantalaris A and Panoskaltsis
N: Three-Dimensional Human Bone Marrow Organoids for the Study and
Application of Normal and Abnormal Hematoimmunopoiesis. J Immunol.
210:895–904. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Herrera-Carrillo E, Liu YP and Berkhout B:
Improving miRNA Delivery by Optimizing miRNA expression cassettes
in diverse virus vectors. Hum Gene Ther Methods. 28:177–190. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Calloni R and Bonatto D: Scaffolds for
Artificial miRNA expression in animal cells. Hum Gene Ther Methods.
26:162–174. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Lundstrom K: Trans-amplifying RNA hitting
new grounds: Gene regulation by microRNA. Mol Ther Nucleic Acids.
35:1021912024. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Yıldız A, Hasani A, Hempel T, Köhl N,
Beicht A, Becker R, Hubich-Rau S, Suchan M, Poleganov MA, Sahin U
and Beissert T: Trans-amplifying RNA expressing functional miRNA
mediates target gene suppression and simultaneous transgene
expression. Mol Ther Nucleic Acids. 35:1021622024. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Goldman MJ, Craft B, Hastie M, Repečka K,
McDade F, Kamath A, Banerjee A, Luo Y, Rogers D, Brooks AN, et al:
Visualizing and interpreting cancer genomics data via the Xena
platform. Nat Biotechnol. 38:675–678. 2020. View Article : Google Scholar : PubMed/NCBI
|