|
1
|
Estey E and Döhner H: Acute myeloid
leukaemia. Lancet. 368:1894–1907. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Pollyea DA, Kohrt HE and Medeiros BC:
Acute myeloid leukaemia in the elderly: A review. Br J Haematol.
152:524–542. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Saultz JN and Garzon R: Acute myeloid
leukemia: A concise review. J Clin Med. 5:332016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Döhner H, Weisdorf DJ and Bloomfield CD:
Acute myeloid leukemia. N Engl J Med. 373:1136–1152. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Park HJ and Gregory MA: Acute myeloid
leukemia in elderly patients: New targets, new therapies. Aging
Cancer. 4:51–73. 2023. View Article : Google Scholar
|
|
6
|
Robak T and Wierzbowska A: Current and
emerging therapies for acute myeloid leukemia. Clin Ther.
31:2349–2370. 2009. View Article : Google Scholar
|
|
7
|
Newell LF and Cook RJ: Advances in acute
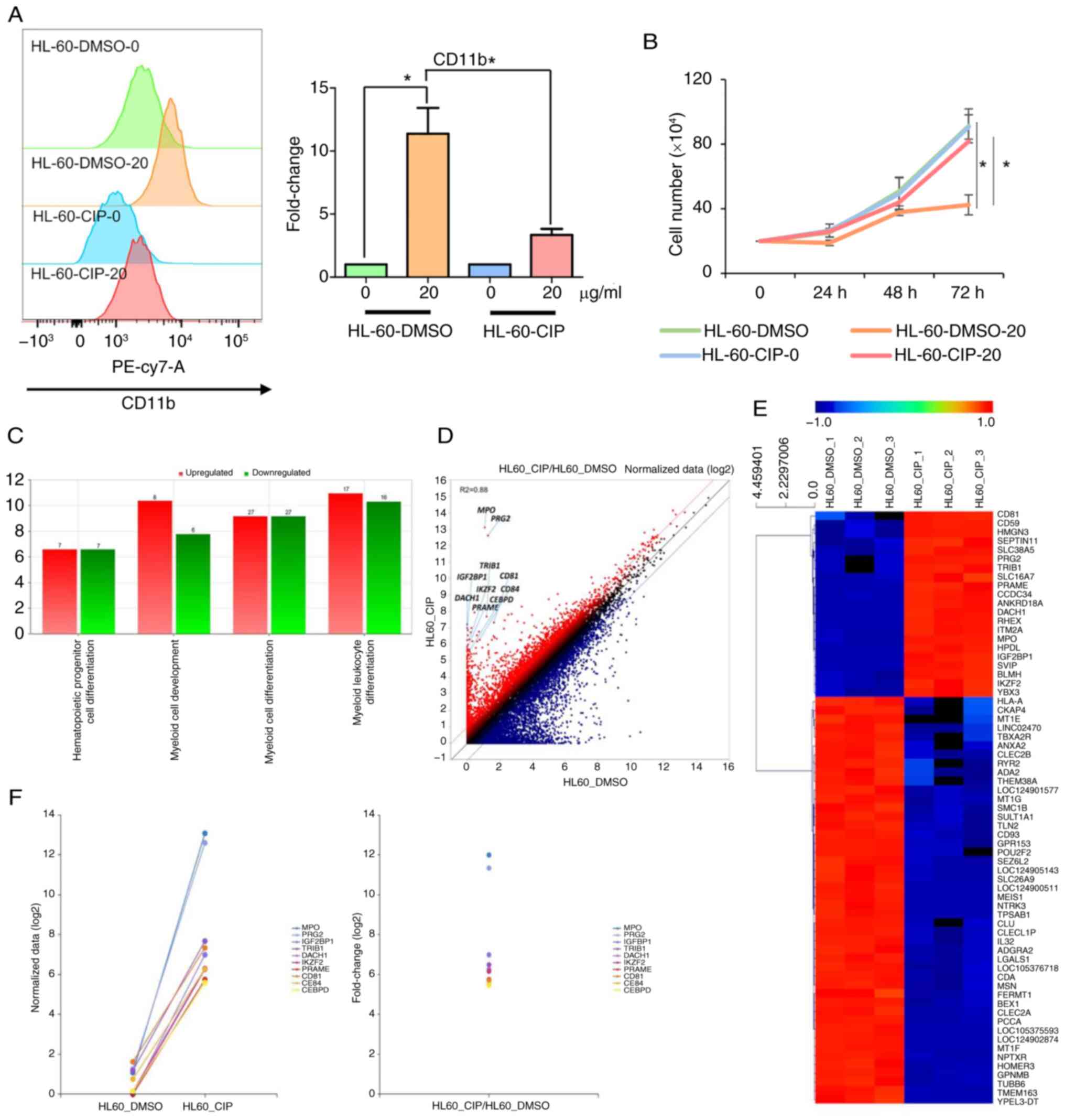
myeloid leukemia. BMJ. 375:n20262021. View Article : Google Scholar : PubMed/NCBI
|
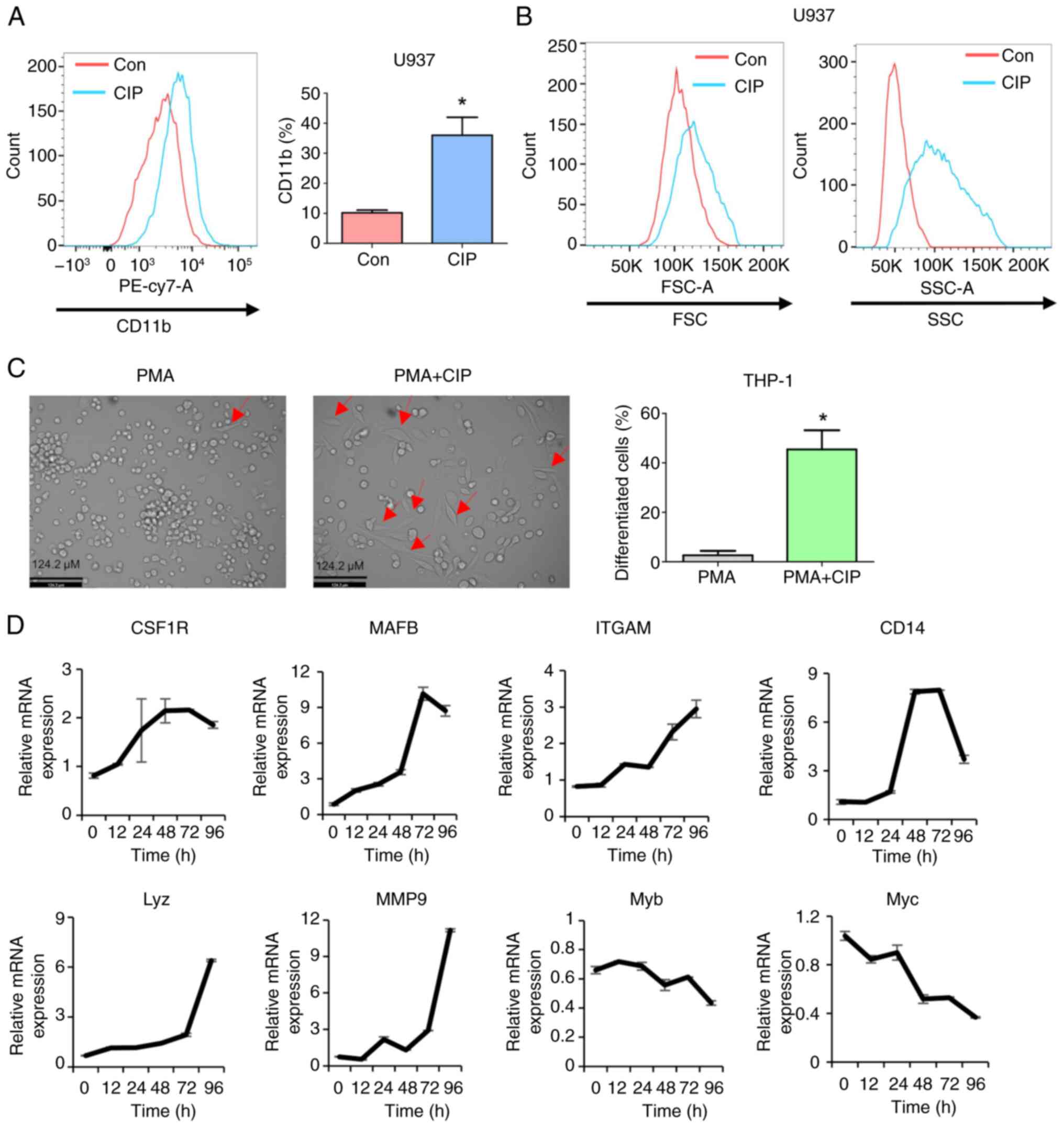
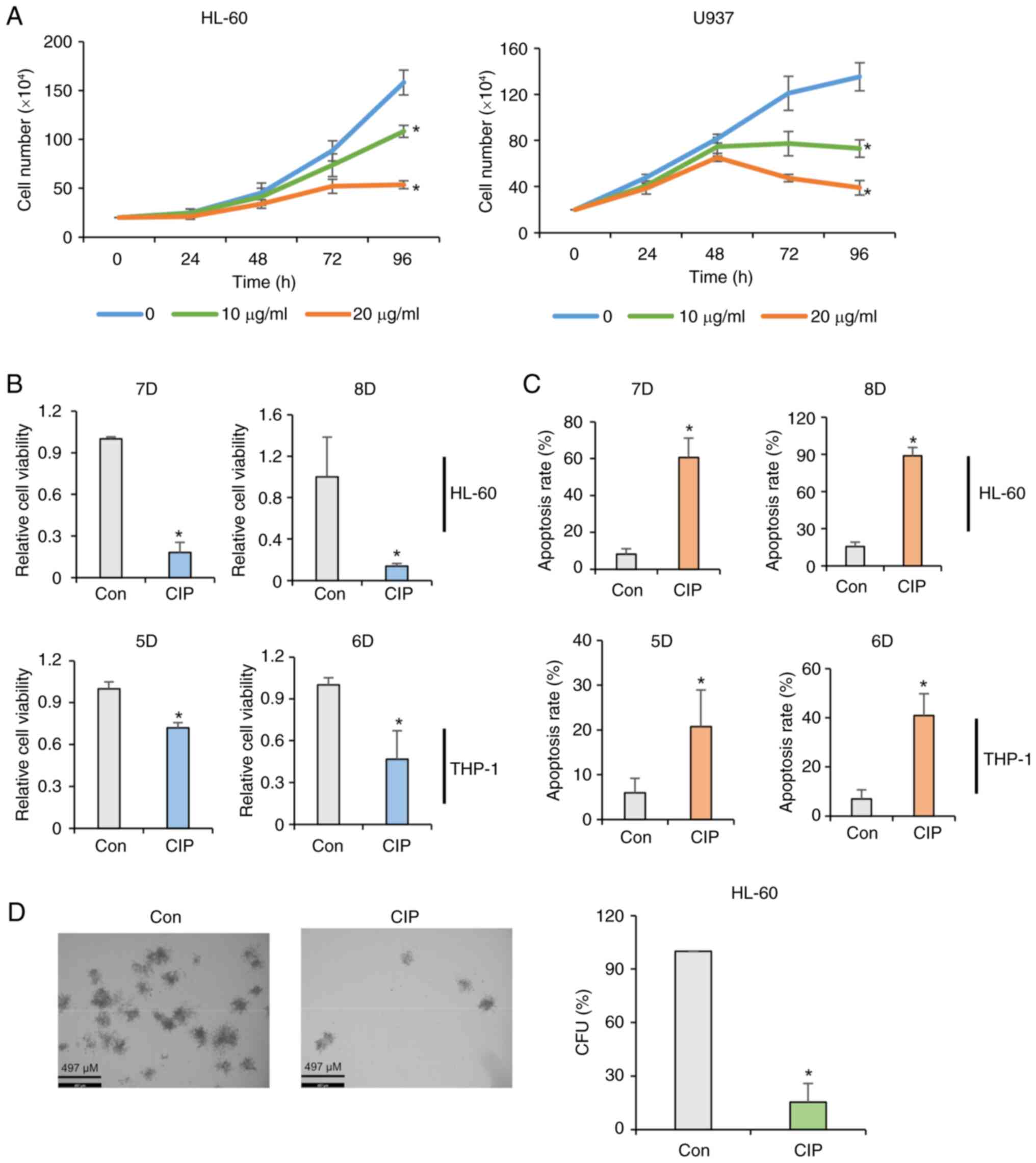
|
8
|
Kantarjian H, Kadia T, DiNardo C, Daver N,
Borthakur G, Jabbour E, Garcia-Manero G, Konopleva M and Ravandi F:
Acute myeloid leukemia: current progress and future directions.
Blood Cancer J. 11:412021. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Saygin C and Carraway HE: Emerging
therapies for acute myeloid leukemia. J Hematol Oncol. 10:932017.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Parisi E, Draznin J, Stoopler E, Schuster
SJ, Porter D and Sollecito TP: Acute myelogenous leukemia: Advances
and limitations of treatment. Oral Surg Oral Med Oral Pathol Oral
Radiol Endod. 93:257–263. 2002. View Article : Google Scholar : PubMed/NCBI
|
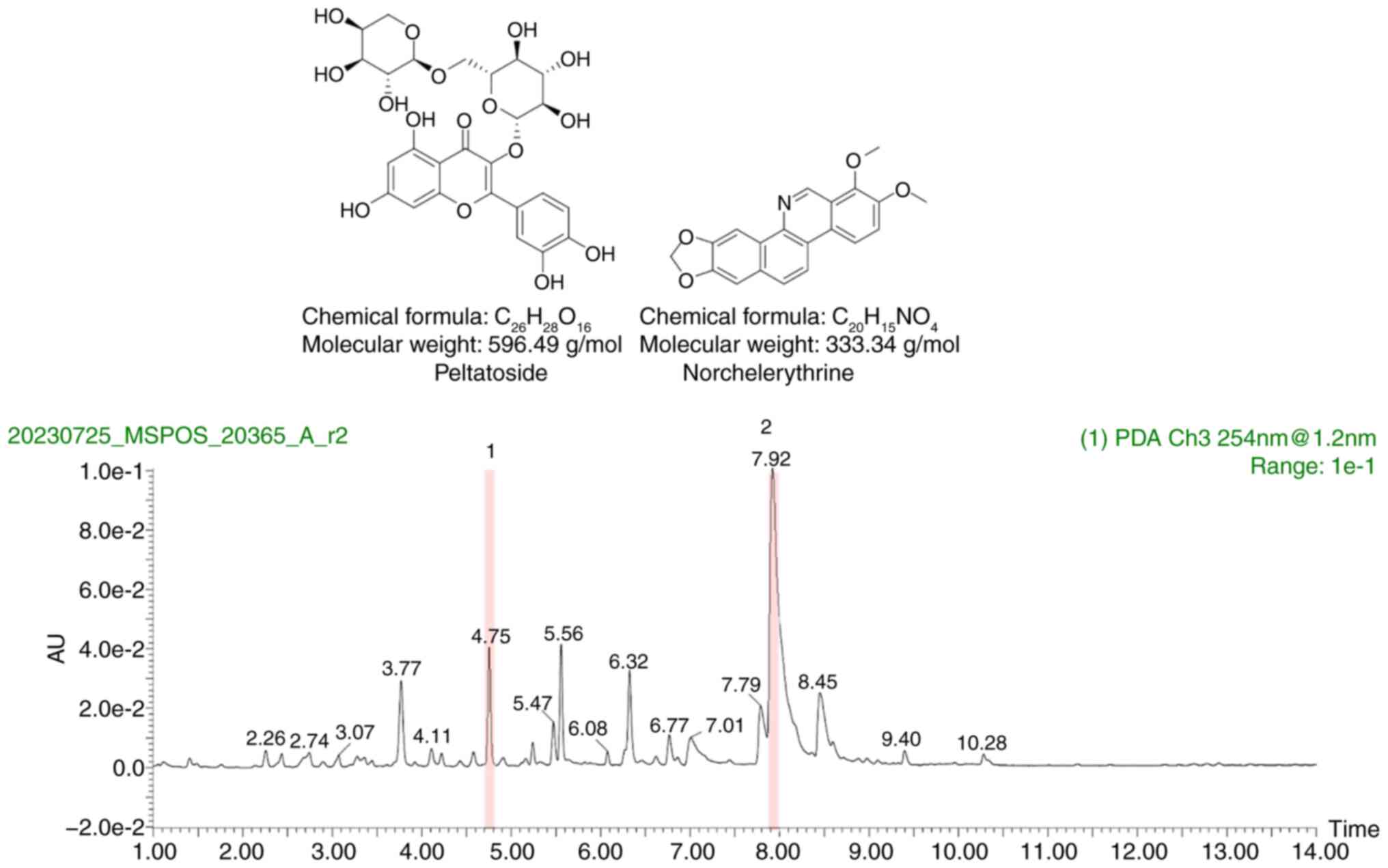
|
11
|
Bhansali RS, Pratz KW and Lai C: Recent
advances in targeted therapies in acute myeloid leukemia. J Hematol
Oncol. 16:292023. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Short NJ, Konopleva M, Kadia TM, Borthakur
G, Ravandi F, DiNardo CD and Daver N: Advances in the treatment of
acute myeloid leukemia: New drugs and new challenges. Cancer
Discov. 10:506–525. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kadia T, Ravandi F, Cortes J and
Kantarjian H: New drugs in acute myeloid leukemia. Ann Oncol.
27:770–778. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
van Dijk AD, de Bont ESJ and Kornblau SM:
Targeted therapy in acute myeloid leukemia: Current status and new
insights from a proteomic perspective. Expert Rev Proteomics.
17:1–10. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Godwin C, Gale R and Walter R: Gemtuzumab
ozogamicin in acute myeloid leukemia. Leukemia. 31:1855–1868. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ehninger A, Kramer M, Röllig C, Thiede C,
Bornhäuser M, von Bonin M, Wermke M, Feldmann A, Bachmann M,
Ehninger G and Oelschlägel U: Distribution and levels of cell
surface expression of CD33 and CD123 in acute myeloid leukemia.
Blood Cancer J. 4:e2182014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Tabata R, Chi S, Yuda J and Minami Y:
Emerging immunotherapy for acute myeloid leukemia. Int J Mol Sci.
22:19442021. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Taussig DC, Pearce DJ, Simpson C,
Rohatiner AZ, Lister TA, Kelly G, Luongo JL, Danet-Desnoyers GA and
Bonnet D: Hematopoietic stem cells express multiple myeloid
markers: Implications for the origin and targeted therapy of acute
myeloid leukemia. Blood. 106:4086–4092. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Walter RB, Appelbaum FR, Estey EH and
Bernstein ID: Acute myeloid leukemia stem cells and CD33-targeted
immunotherapy. Blood. 119:6198–6208. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Damle NK and Frost P: Antibody-targeted
chemotherapy with immunoconjugates of calicheamicin. Curr Opin
Pharmacol. 3:386–390. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Castelli G, Pelosi E and Testa U: Targeted
therapies in the treatment of adult acute myeloid leukemias:
Current status and future perspectives. Int J Hematol Oncol.
5:143–164. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Yan M and Liu Q: Differentiation therapy:
A promising strategy for cancer treatment. Chin J Cancer. 35:32016.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Madan V and Koeffler HP: Differentiation
therapy of myeloid leukemia: Four decades of development.
Haematologica. 106:26–38. 2021.
|
|
24
|
Stubbins RJ and Karsan A: Differentiation
therapy for myeloid malignancies: Beyond cytotoxicity. Blood Cancer
J. 11:1932021. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
de Thé H: Differentiation therapy
revisited. Nat Rev Cancer. 18:117–127. 2018. View Article : Google Scholar
|
|
26
|
Veiga M, Costa EM, Silva S and Pintado M:
Impact of plant extracts upon human health: A review. Crit Rev Food
Sci Nutr. 60:873–886. 2020. View Article : Google Scholar
|
|
27
|
Altemimi A, Lakhssassi N, Baharlouei A,
Watson DG and Lightfoot DA: Phytochemicals: Extraction, isolation,
and identification of bioactive compounds from plant extracts.
Plants (Basel). 6:422017.PubMed/NCBI
|
|
28
|
Dixit S and Ali H: Anticancer activity of
medicinal plant extract-A review. J Chem Cheml Sci. 1:79–85.
2010.
|
|
29
|
Li W, Huang H, Zhang Y, Fan T, Liu X, Xing
W and Niu X: Anti-inflammatory effect of tetrahydrocoptisine from
Corydalis impatiens is a function of possible inhibition of TNF-α,
IL-6 and NO production in lipopolysaccharide-stimulated peritoneal
macrophages through inhibiting NF-κB activation and MAPK pathway.
Eur J Pharmacol. 715:62–71. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Yang C, Zhang C, Wang Z, Tang Z, Kuang H
and Kong ANT: Corynoline isolated from Corydalis bungeana Turcz.
exhibits anti-inflammatory effects via modulation of Nfr2 and
MAPKs. Molecules. 21:9752016. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Zheng J, Zhao Y, Lun Q, Song Y, Shi S, Gu
X, Pan B, Qu C, Li J and Tu P: Corydalis edulis Maxim. Promotes
insulin secretion via the activation of protein kinase Cs (PKCs) in
mice and pancreatic β cells. Sci Rep. 7:404542017. View Article : Google Scholar
|
|
32
|
Xu Z, Chen X, Zhang Q, Chen L and Wang Y:
Corydalis yanhusuo W.T. Wang extract inhibits MCF-7 cell
proliferation by inducing cell cycle G2/M arrest. Am J Chin Med.
39:579–586. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Oh MT, Eom HS and Chi GY:
Antiproliferative effect and apoptotic mechanism of extract of
Corydalis yanhusuo on human hepatocarcinoma cells. J Physiol Pathol
Korean Med. 21:1437–1449. 2007.
|
|
34
|
Lu JJ, Bao JL, Chen XP, Huang M and Wang
YT: Alkaloids isolated from natural herbs as the anticancer agents.
Evid Based Complement Alternat Med. 2012:4850422012. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Habli Z, Toumieh G, Fatfat M, Rahal ON and
Gali-Muhtasib H: Emerging cytotoxic alkaloids in the battle against
cancer: Overview of molecular mechanisms. Molecules. 22:2502017.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Spirin P, Shyrokova E, Lebedev T, Vagapova
E, Smirnova P, Kantemirov A, Dyshlovoy SA, Amsberg GV, Zhidkov M
and Prassolov V: Cytotoxic marine alkaloid 3,10-dibromofascaplysin
induces apoptosis and synergizes with cytarabine resulting in
leukemia cell death. Mar Drugs. 19:4892021. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Wang XD, Li CY, Jiang MM, Li D, Wen P,
Song X, Chen JD, Guo LX, Hu XP, Li GQ, et al: Induction of
apoptosis in human leukemia cells through an intrinsic pathway by
cathachunine, a unique alkaloid isolated from Catharanthus roseus.
Phytomedicine. 23:641–653. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Silva SLR, Dias IRSB, Rodrigues ACBDC,
Costa RGA, Oliveira MS, Barbosa GADC, Soares MBP, Dias RB, Valverde
LF, Rocha CAG, et al: Emetine induces oxidative stress, cell
differentiation and NF-κB inhibition, suppressing AML
stem/progenitor cells. Cell Death Discov. 10:2012024. View Article : Google Scholar
|
|
39
|
Gupta K, Chakrabarti A, Rana S, Ramdeo R,
Roth BL, Agarwal ML, Tse W, Agarwal MK and Wald DN: Securinine, a
myeloid differentiation agent with therapeutic potential for AML.
PLoS One. 6:e212032011. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Wu G, Liu T, Li H, Li Y, Li D and Li W:
c-MYC and reactive oxygen species play roles in tetrandrine-induced
leukemia differentiation. Cell Death Dis. 9:4732018. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar
|
|
42
|
Woo YR, Kwon CS, Lee JE, Jeon BE, Kim TJ,
Choo J, Seo YS and Kim SW: Ajania pacifica (Nakai) K. bremer and
humphries extract limits MYC expression to induce apoptosis in
diffuse large B cell lymphoma. Curr Issues Mol Biol. 46:4580–4594.
2024. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Kwon CS, Lee JE, Jeon BE, Woo YR, Kim YS,
Kim JW, Park CJ, Jang SY and Kim SW: Anti-leukemic effects of
Idesia polycarpa Maxim branch on human B-cell acute lymphoblastic
leukemia cells. Curr Issues Mol Biol. 45:4035–4049. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Lee JE, Kwon CS, Jeon BE, Kim WR, Lee DH,
Koh S, Kim HS and Kim SW: Genome-wide gene expression profiling
defines the mechanism of anticancer effect of colorectal cancer
cell-derived conditioned medium on acute myeloid leukemia. Genes
(Basel). 13:8832022. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Jeon BE, Kwon CS, Lee JE, Moon K, Cha J,
Park I, Koh S, Yoon M, Kim SW and Kim JN: Anticancer activity of
continentalic acid in B-cell lymphoma. Molecules. 26:68452021.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Vidriales MB, Orfao A, López-Berges MC,
González M, López-Macedo A, García MA, Galende J and San Miguel JF:
Light scatter characteristics of blast cells in acute myeloid
leukaemia: Association with morphology and immunophenotype. J Clin
Pathol. 48:456–462. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Mol BA, Wasinda JJ, Xu YF, Gentle NL and
Meyer V: 1,25-Dihydroxyvitamin D3 augments low-dose
PMA-based monocyte-to-macrophage differentiation in THP-1 cells. J
Immunol Methods. 532:1137162024. View Article : Google Scholar
|
|
48
|
Kelly LM, Englmeier U, Lafon I, Sieweke MH
and Graf T: MafB is an inducer of monocytic differentiation. EMBO
J. 19:1987–1997. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Sykes DB, Kfoury YS, Mercier FE, Wawer MJ,
Law JM, Haynes MK, Lewis TA, Schajnovitz A, Jain E, Lee D, et al:
Inhibition of dihydroorotate dehydrogenase overcomes
differentiation blockade in acute myeloid leukemia. Cell.
167:171–186.e15. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Hosseini M, Rezvani HR, Aroua N, Bosc C,
Farge T, Saland E, Guyonnet-Dupérat V, Zaghdoudi S, Jarrou L,
Larrue C, et al: Targeting myeloperoxidase disrupts mitochondrial
redox balance and overcomes cytarabine resistance in human acute
myeloid leukemia. Cancer Res. 79:5191–5203. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Liu Q and Dong F: Gfi-1 inhibits the
expression of eosinophil major basic protein (MBP) during
G-CSF-induced neutrophilic differentiation. Int J Hematol.
95:640–647. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Zhou J, Bi C, Ching YQ, Chooi JY, Lu X,
Quah JY, Toh SH, Chan ZL, Tan TZ, Chong PS and Chng WJ: Inhibition
of LIN28B impairs leukemia cell growth and metabolism in acute
myeloid leukemia. J Hematol Oncol. 10:1382017. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Yoshino S, Yokoyama T, Sunami Y, Takahara
T, Nakamura A, Yamazaki Y, Tsutsumi S, Aburatani H and Nakamura T:
Trib1 promotes acute myeloid leukemia progression by modulating the
transcriptional programs of Hoxa9. Blood. 137:75–88. 2021.
View Article : Google Scholar :
|
|
54
|
Lee JW, Kim HS, Kim S, Hwang J, Kim YH,
Lim GY, Sohn WJ, Yoon SR, Kim JY, Park TS, et al: DACH1 regulates
cell cycle progression of myeloid cells through the control of
cyclin D, Cdk 4/6 and p21Cip1. Biochem Biophys Res Commun.
420:91–95. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Park SM, Cho H, Thornton AM, Barlowe TS,
Chou T, Chhangawala S, Fairchild L, Taggart J, Chow A, Schurer A,
et al: IKZF2 drives leukemia stem cell self-renewal and inhibits
myeloid differentiation. Cell Stem Cell. 24:153–165.e7. 2019.
View Article : Google Scholar :
|
|
56
|
Kirkey DC, Loeb AM, Castro S, McKay CN,
Perkins L, Pardo L, Leonti AR, Tang TT, Loken MR, Brodersen LE, et
al: Therapeutic targeting of PRAME with mTCRCAR T cells in acute
myeloid leukemia. Blood Adv. 7:1178–1189. 2023. View Article : Google Scholar :
|
|
57
|
Boyer T, Guihard S, Roumier C, Peyrouze P,
Gonzales F, Berthon C, Quesnel B, Preudhomme C, Behal H, Duhamel A,
et al: Tetraspanin CD81 is an adverse prognostic marker in acute
myeloid leukemia. Oncotarget. 7:62377–62385. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Prajapati S, Meydan C, Dillon R, Dunham N,
Fan H, Gandara JA, Lee T, Neelamraju Y, Sheridan C, Wang Z, et al:
Loss of CCAAT-enhancer binding protein delta promotes acute myeloid
leukemia cell proliferation and survival by upregulating cyclin D1
expression. Blood. 142(Suppl 1): S13802023. View Article : Google Scholar
|
|
59
|
Zhu Y, Park M, Murtadha M, Caserta E,
Nguyen LXT, Singer M, Estepa MD, Nigam L, Dona' AA, Sanchez JF, et
al: CD84 is a therapeutically targetable driver of leukemogenesis
via disruption of energy supply in acute myeloid leukemia. Blood.
140(Suppl 1): S89–S90. 2022. View Article : Google Scholar
|
|
60
|
Sauer H, Wartenberg M and Hescheler J:
Reactive oxygen species as intracellular messengers during cell
growth and differentiation. Cell Physiol Biochem. 11:173–186. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Prieto-Bermejo R, Romo-González M,
Pérez-Fernández A, Ijurko C and Hernández-Hernández Á: Reactive
oxygen species in haematopoiesis: Leukaemic cells take a walk on
the wild side. J Exp Clin Cancer Res. 37:1252018. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Murata T, Kohno S, Ogawa K, Ito C,
Itoigawa M, Ito M, Hikita K and Kaneda N: Cytotoxic activity of
dimeric acridone alkaloids derived from Citrus plants towards human
leukaemia HL-60 cells. J Pharm Pharmacol. 72:1445–1457. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Long Q, Xiao X, Yi P, Liu Y, Varier KM,
Rao Q, Song J, Qiu J, Wang C, Liu W, et al: L20, a Calothrixin B
analog, induces intrinsic apoptosis on HEL cells through
ROS/γ-H2AX/p38 MAPK pathway. Biomed Pharmacother. 137:1113362021.
View Article : Google Scholar
|
|
64
|
Alhuthali HM, Bradshaw TD, Lim KH, Kam TS
and Seedhouse CH: The natural alkaloid Jerantinine B has activity
in acute myeloid leukemia cells through a mechanism involving
c-Jun. BMC Cancer. 20:6292020. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Santos MA, Faryabi RB, Ergen AV, Day AM,
Malhowski A, Canela A, Onozawa M, Lee JE, Callen E,
Gutierrez-Martinez P, et al: DNA-damage-induced differentiation of
leukaemic cells as an anti-cancer barrier. Nature. 514:107–111.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Nicolae CM, O'Connor MJ, Constantin D and
Moldovan GL: NFκB regulates p21 expression and controls DNA
damage-induced leukemic differentiation. Oncogene. 37:3647–3656.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
De Kouchkovsky I and Abdul-Hay M: Acute
myeloid leukemia: A comprehensive review and 2016 update. Blood
Cancer J. 6:e4412016. View Article : Google Scholar
|
|
68
|
Johnson DE and Redner RL: An ATRActive
future for differentiation therapy in AML. Blood Rev. 29:263–268.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Zhang Ying ZY, Qin MinJian QM and Xie
GuoYong XG: Analysis of alkaloid compositions from Corydalis incise
2008. https://www.cabidigitallibrary.org/doi/full/10.5555/20093000856.
|
|
70
|
Manske RHF: The alkaloids of fumariaceous
plants. XLIV. Corydalis incisa (Thunb.) Pers. and the constitutions
of adlumidine and capnoidine. J Am Chem Soc. 72:3207–3208. 1950.
View Article : Google Scholar
|
|
71
|
Kametani T, Ihara M and Honda T:
Morphinandienone alkaloids from Corydalis incisa. Phytochemistry.
10:1881–1883. 1971. View Article : Google Scholar
|
|
72
|
Nonaka G and Nishioka I: Alkaloids of
Corydalis incisa PERS. V. The structures of corydalispirone and
corydalisol. Chem Pharm Bull. 23:294–298. 1975. View Article : Google Scholar
|
|
73
|
Nonaka G and Nishioka I: Alkaloids of
Corydalis incisa PERS. III. The structures of corydamine
hydrochloride and N-formyl corydamine. Chem Pharm Bull.
21:1410–1414. 1973. View Article : Google Scholar
|
|
74
|
Nonaka G and Nishioka I: Alkaloids of
Corydalis incisa PERS. VI. The structures of benzo [c]
phenanthridine-type alkaloids, 12-hydroxycorynoline and
11-epicorynoline. Chem Pharm Bull. 23:521–526. 1975. View Article : Google Scholar
|
|
75
|
Sulaiman M, Jannat K, Nissapatorn V,
Rahmatullah M, Paul AK, de Lourdes Pereira M, Rajagopal M, Suleiman
M, Butler MS, Break MKB, et al: Antibacterial and antifungal
alkaloids from Asian angiosperms: Distribution, mechanisms of
action, structure-activity, and clinical potentials. Antibiotics
(Basel). 11:11462022. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Luo X, Pedro L, Milic V, Mulhovo S, Duarte
A, Duarte N and Ferreira MJ: Antibacterial benzofuran neolignans
and benzophenanthridine alkaloids from the roots of Zanthoxylum
capense. Planta Med. 78:148–153. 2012. View Article : Google Scholar
|
|
77
|
Wang CF, You CX, Yang K, Guo SS, Geng ZF,
Fan L, Du SS, Deng ZW and Wang YY: Antifeedant activities of
methanol extracts of four Zanthoxylum species and
benzophenanthridines from stem bark of Zanthoxylum schinifolium
against Tribolium castaneum. Ind Crops Prod. 74:407–411. 2015.
View Article : Google Scholar
|
|
78
|
Pang SQ, Wang GQ, Lin JS, Diao Y and Xu
RA: Cytotoxic activity of the alkaloids from Broussonetia
papyrifera fruits. Pharm Biol. 52:1315–1319. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Chang YC, Chang FR, Khalil AT, Hsieh PW
and Wu YC: Cytotoxic benzophenanthridine and benzylisoquinoline
alkaloids from Argemone mexicana. Z Naturforsch C J Biosci.
58:521–526. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Chen JJ, Fang HY, Duh CY and Chen IS: New
indolopyridoquinazoline, benzo[c]phenanthridines and cytotoxic
constituents from Zanthoxylum integrifoliolum. Planta Med.
71:470–475. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Weiss CN and Ito K: DNA damage: A sensible
mediator of the differentiation decision in hematopoietic stem
cells and in leukemia. Int J Mol Sci. 16:6183–6201. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Baer C, Walter W, Stengel A, Hutter S,
Meggendorfer M, Kern W, Haferlach C and Haferlach T: Molecular
classification of AML-MRC reveals a distinct profile and identifies
MRC-like patients with poor overall survival. Blood. 134(Suppl 1):
S27352019. View Article : Google Scholar
|
|
83
|
Arber DA and Erba HP: Diagnosis and
treatment of patients with acute myeloid leukemia with
myelodysplasia-related changes (AML-MRC). Am J Clin Pathol.
154:731–741. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Zheng S, Bian H, Li J, Shen Y, Yang Y and
Hu W: Differentiation therapy: Unlocking phenotypic plasticity of
hepatocellular carcinoma. Crit Rev Oncol Hematol. 180:1038542022.
View Article : Google Scholar : PubMed/NCBI
|