|
1
|
Jassim A, Rahrmann EP, Simons BD and
Gilbertson RJ: Cancers make their own luck: Theories of cancer
origins. Nat Rev Cancer. 23:710–724. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Mattiuzzi C and Lippi G: Cancer
statistics: A comparison between World Health Organization (WHO)
and Global Burden of Disease (GBD). Eur J Public Health.
30:1026–1027. 2020. View Article : Google Scholar
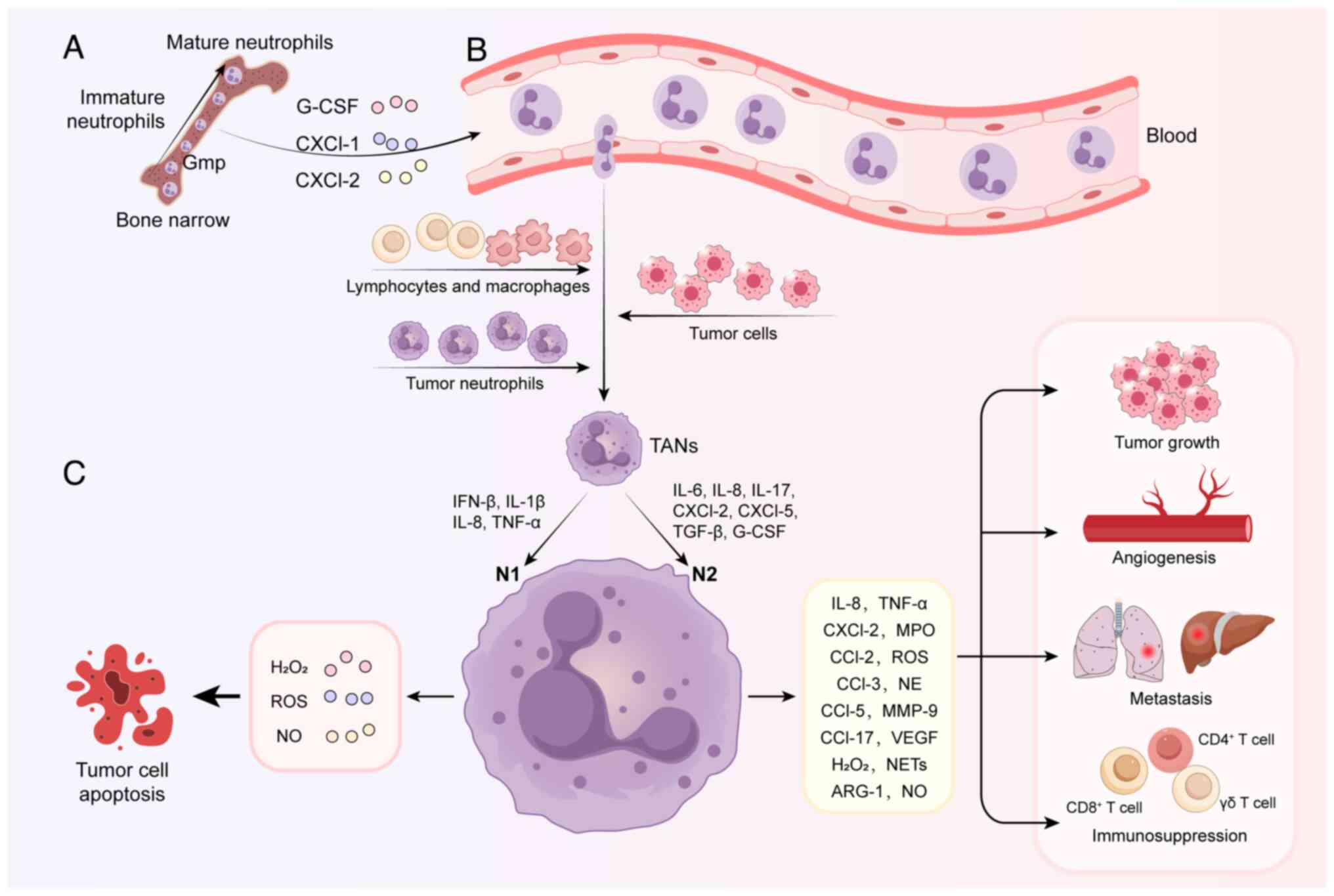
|
|
3
|
Wang J, Yang J, Narang A, He J, Wolfgang
C, Li K and Zheng L: Consensus, debate, and prospective on
pancreatic cancer treatments. J Hematol Oncol. 17:922024.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Long GV, Swetter SM, Menzies AM,
Gershenwald JE and Scolyer RA: Cutaneous melanoma. Lancet.
402:485–502. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Joshi SS and Badgwell BD: Current
treatment and recent progress in gastric cancer. CA Cancer J Clin.
71:264–279. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
de Visser KE and Joyce JA: The evolving
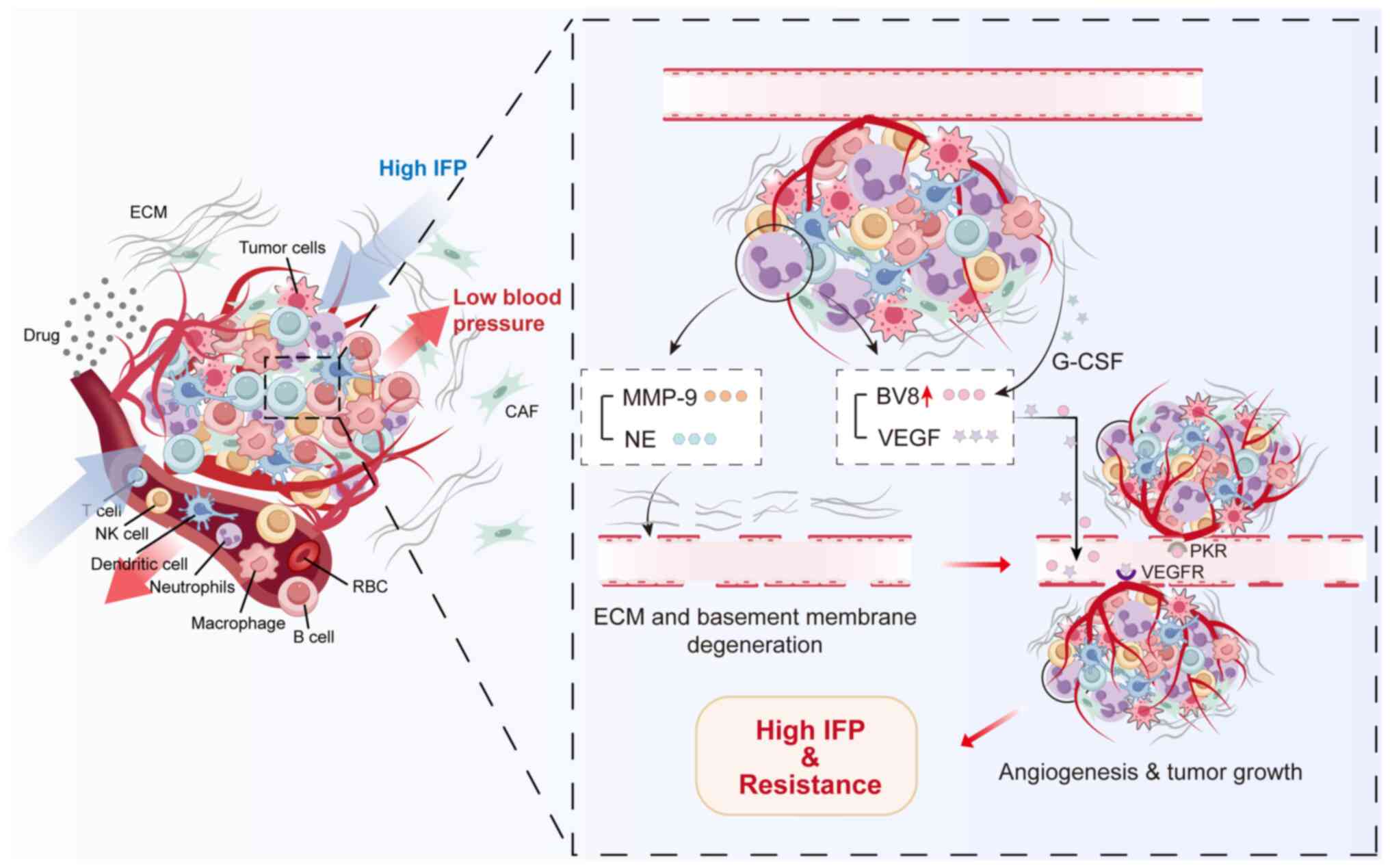
tumor microenvironment: From cancer initiation to metastatic
outgrowth. Cancer Cell. 41:374–403. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Gonçalves AC, Richiardone E, Jorge J,
Polónia B, Xavier CPR, Salaroglio IC, Riganti C, Vasconcelos MH,
Corbet C and Sarmento-Ribeiro AB: Impact of cancer metabolism on
therapy resistance-clinical implications. Drug Resist Updat.
59:1007972021. View Article : Google Scholar
|
|
8
|
Kalli M, Poskus MD, Stylianopoulos T and
Zervantonakis IK: Beyond matrix stiffness: Targeting force-induced
cancer drug resistance. Trends Cancer. 9:937–954. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Chen D, Gu X, Nurzat Y, Xu L, Li X, Wu L,
Jiao H, Gao P, Zhu X, Yan D, et al: Writers, readers, and erasers
RNA modifications and drug resistance in cancer. Mol Cancer.
23:1782024. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
He J, Qiu Z, Fan J, Xie X, Sheng Q and Sui
X: Drug tolerant persister cell plasticity in cancer: A
revolutionary strategy for more effective anticancer therapies.
Signal Transduct Target Ther. 9:2092024. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Nussinov R, Tsai C-J and Jang H:
Anticancer drug resistance: An update and perspective. Drug Resist
Updat. 59:1007962021. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Polak R, Zhang ET and Kuo CJ: Cancer
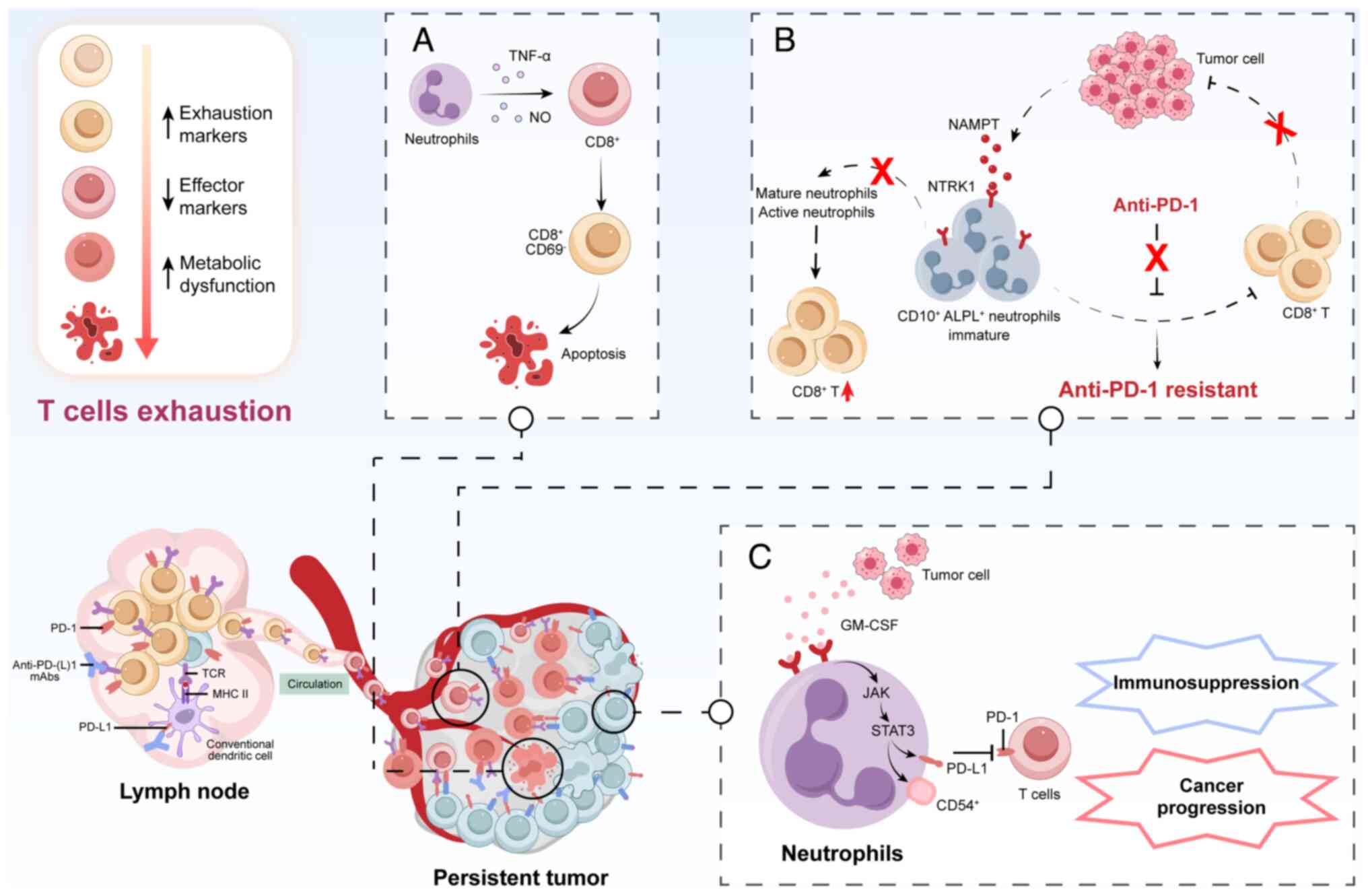
organoids 2.0: Modelling the complexity of the tumour immune
microenvironment. Nat Rev Cancer. 24:523–539. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Hessmann E, Buchholz SM, Demir IE, Singh
SK, Gress TM, Ellenrieder V and Neesse A: Microenvironmental
determinants of pancreatic cancer. Physiol Rev. 100:1707–1751.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Koenderman L and Vrisekoop N: Neutrophils
in cancer: From biology to therapy. Cell Mol Immunol. 22:4–23.
2025. View Article : Google Scholar :
|
|
15
|
Liu S, Wu W, Du Y, Yin H, Chen Q, Yu W,
Wang W, Yu J, Liu L, Lou W and Pu N: The evolution and
heterogeneity of neutrophils in cancers: Origins, subsets,
functions, orchestrations and clinical applications. Mol Cancer.
22:1482023. View Article : Google Scholar : PubMed/NCBI
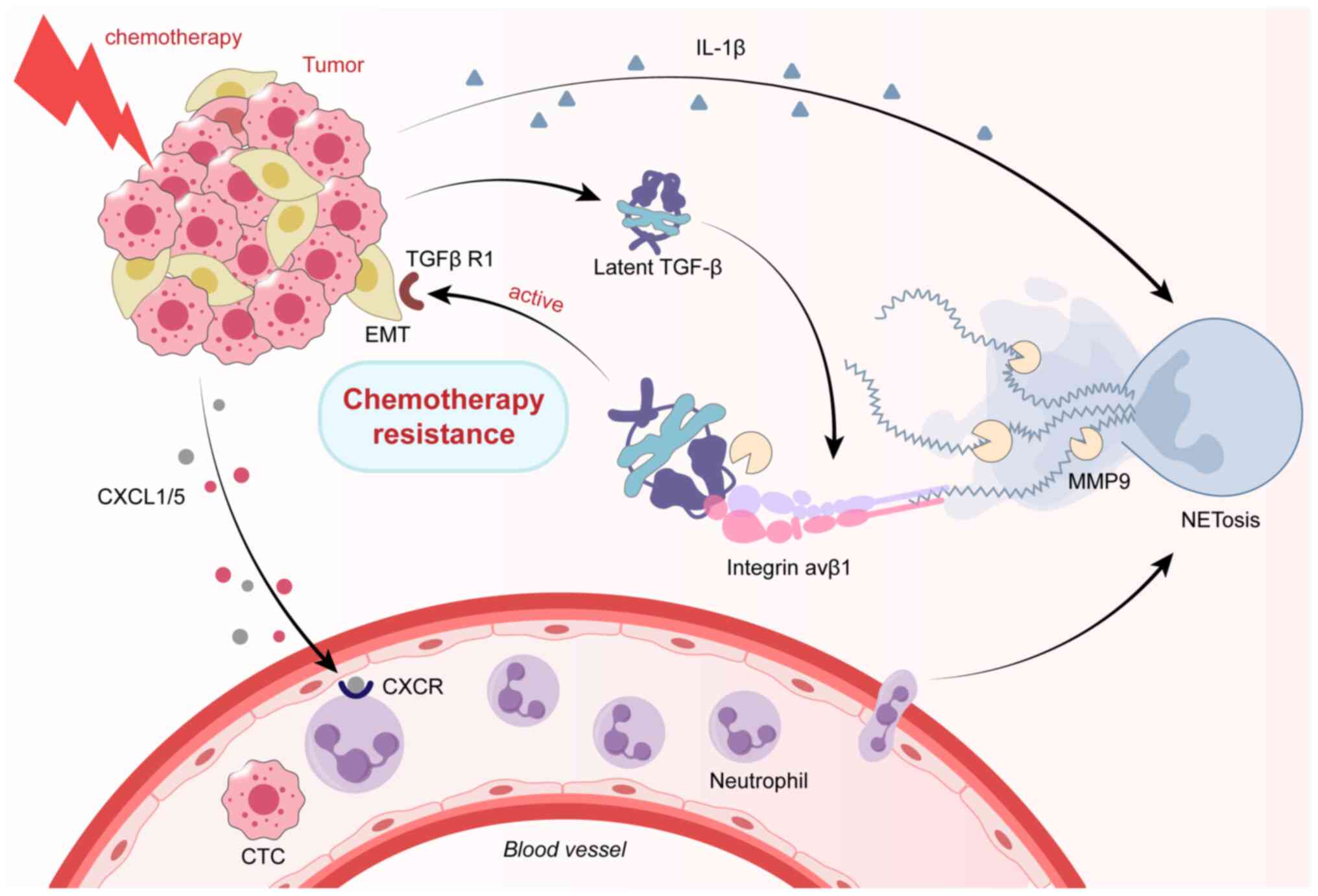
|
|
16
|
Zhang J, Gu J, Wang X, Ji C, Yu D, Wang M,
Pan J, Santos HA, Zhang H and Zhang X: Engineering and targeting
neutrophils for cancer therapy. Adv Mater. 36:e23103182024.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
van Vlerken-Ysla L, Tyurina YY, Kagan VE
and Gabrilovich DI: Functional states of myeloid cells in cancer.
Cancer Cell. 41:490–504. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Que H, Fu Q, Lan T, Tian X and Wei X:
Tumor-associated neutrophils and neutrophil-targeted cancer
therapies. Biochim Biophys Acta Rev Cancer. 1877:1887622022.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Xue R, Zhang Q, Cao Q, Kong R, Xiang X,
Liu H, Feng M, Wang F, Cheng J, Li Z, et al: Liver tumour immune
microenvironment subtypes and neutrophil heterogeneity. Nature.
612:141–147. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Jaillon S, Ponzetta A, Di Mitri D, Santoni
A, Bonecchi R and Mantovani A: Neutrophil diversity and plasticity
in tumour progression and therapy. Nat Rev Cancer. 20:485–503.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Mantovani A, Cassatella MA, Costantini C
and Jaillon S: Neutrophils in the activation and regulation of
innate and adaptive immunity. Nat Rev Immunol. 11:519–531. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Fridlender ZG, Sun J, Kim S, Kapoor V,
Cheng G, Ling L, Worthen GS and Albelda SM: Polarization of
tumor-associated neutrophil phenotype by TGF-beta: 'N1' versus 'N2'
TAN. Cancer Cell. 16:183–194. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Shaul ME and Fridlender ZG:
Tumour-associated neutrophils in patients with cancer. Nat Rev Clin
Oncol. 16:601–620. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Salcher S, Sturm G, Horvath L, Untergasser
G, Kuempers C, Fotakis G, Panizzolo E, Martowicz A, Trebo M, Pall
G, et al: High-resolution single-cell atlas reveals diversity and
plasticity of tissue-resident neutrophils in non-small cell lung
cancer. Cancer Cell. 40:1503–1520.e8. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ng MSF, Kwok I, Tan L, Shi C,
Cerezo-Wallis D, Tan Y, Leong K, Calvo GF, Yang K, Zhang Y, et al:
Deterministic reprogramming of neutrophils within tumors. Science.
383:eadf64932024. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Wu Y, Ma J, Yang X, Nan F, Zhang T, Ji S,
Rao D, Feng H, Gao K, Gu X, et al: Neutrophil profiling illuminates
anti-tumor antigen-presenting potency. Cell. 187:1422–1439.e24.
2024. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Wang L, Liu Y, Dai Y, Tang X, Yin T, Wang
C, Wang T, Dong L, Shi M, Qin J, et al: Single-cell RNA-seq
analysis reveals BHLHE40-driven pro-tumour neutrophils with
hyperactivated glycolysis in pancreatic tumour microenvironment.
Gut. 72:958–971. 2023. View Article : Google Scholar
|
|
28
|
Xia L, Oyang L, Lin J, Tan S, Han Y, Wu N,
Yi P, Tang L, Pan Q, Rao S, et al: The cancer metabolic
reprogramming and immune response. Mol Cancer. 20:282021.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Tian S, Chu Y, Hu J, Ding X, Liu Z, Fu D,
Yuan Y, Deng Y, Wang G, Wang L and Wang Z: Tumour-associated
neutrophils secrete AGR2 to promote colorectal cancer metastasis
via its receptor CD98hc-xCT. Gut. 71:2489–2501. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Tie Y, Tang F, Wei YQ and Wei XW:
Immunosuppressive cells in cancer: Mechanisms and potential
therapeutic targets. J Hematol Oncol. 15:612022. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Lianyuan T, Gang L, Ming T, Dianrong X,
Chunhui Y, Zhaolai M and Bin J: Tumor associated neutrophils
promote the metastasis of pancreatic ductal adenocarcinoma. Cancer
Biol Ther. 21:937–945. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Amorim C, Docasar CL, Guimarães-Bastos D,
Frony AC, Barja-Fidalgo C, Renovato-Martins M and Moraes JA:
Extracellular vesicles derived from MDA-MB-231 cells trigger
neutrophils to a pro-tumor profile. Cells. 11:18752022. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Qin F, Liu X, Chen J, Huang S, Wei W, Zou
Y, Liu X, Deng K, Mo S, Chen J, et al: Anti-TGF-β attenuates tumor
growth via polarization of tumor associated neutrophils towards an
anti-tumor phenotype in colorectal cancer. J Cancer. 11:2580–2592.
2020. View Article : Google Scholar :
|
|
34
|
Peng H, Shen J, Long X, Zhou X, Zhang J,
Xu X, Huang T, Xu H, Sun S, Li C, et al: Local release of TGF-β
inhibitor modulates tumor-associated neutrophils and enhances
pancreatic cancer response to combined irreversible electroporation
and immunotherapy. Adv Sci (Weinh). 9:e21052402022. View Article : Google Scholar
|
|
35
|
Tan Q, Ma X, Yang B, Liu Y, Xie Y, Wang X,
Yuan W and Ma J: Periodontitis pathogen Porphyromonas gingivalis
promotes pancreatic tumorigenesis via neutrophil elastase from
tumor-associated neutrophils. Gut Microbes. 14:20737852022.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Li S, Cong X, Gao H, Lan X, Li Z, Wang W,
Song S, Wang Y, Li C, Zhang H, et al: Tumor-associated neutrophils
induce EMT by IL-17a to promote migration and invasion in gastric
cancer cells. J Exp Clin Cancer Res. 38:62019. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Zhang J, Yu D, Ji C, Wang M, Fu M, Qian Y
and Zhang X, Ji R, Li C, Gu J and Zhang X: Exosomal
miR-4745-5p/3911 from N2-polarized tumor-associated neutrophils
promotes gastric cancer metastasis by regulating SLIT2. Mol Cancer.
23:1982024. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Bodac A, Mayet A, Rana S, Pascual J,
Bowler AD, Roh V, Fournier N, Craciun L, Demetter P, Radtke F and
Meylan E: Bcl-xL targeting eliminates ageing tumor-promoting
neutrophils and inhibits lung tumor growth. EMBO Mol Med.
16:158–184. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Zhang S, Sun L, Zuo J and Feng D: Tumor
associated neutrophils governs tumor progression through an
IL-10/STAT3/PD-L1 feedback signaling loop in lung cancer. Transl
Oncol. 40:1018662024. View Article : Google Scholar
|
|
40
|
Huang X, Nepovimova E, Adam V, Sivak L,
Heger Z, Valko M, Wu Q and Kuca K: Neutrophils in cancer
immunotherapy: Friends or foes? Mol Cancer. 23:1072024. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Bird L: Neutrophils become pro-angiogenic
in tumours. Nat Rev Immunol. 24:1572024. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Maas RR, Soukup K, Fournier N, Massara M,
Galland S, Kornete M, Wischnewski V, Lourenco J, Croci D,
Álvarez-Prado ÁF, et al: The local microenvironment drives
activation of neutrophils in human brain tumors. Cell.
186:4546–4566.e27. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Qu X, Zhuang G, Yu L, Meng G and Ferrara
N: Induction of Bv8 expression by granulocyte colony-stimulating
factor in CD11b+Gr1+ cells: Key role of Stat3 signaling. J Biol
Chem. 287:19574–19584. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Fetz AE, Radic MZ and Bowlin GL:
Neutrophils in biomaterial-guided tissue regeneration: Matrix
reprogramming for angiogenesis. Tissue Eng Part B Rev. 27:95–106.
2021. View Article : Google Scholar
|
|
45
|
Vannitamby A, Seow HJ, Anderson G, Vlahos
R, Thompson M, Steinfort D, Irving LB and Bozinovski S:
Tumour-associated neutrophils and loss of epithelial PTEN can
promote corticosteroid-insensitive MMP-9 expression in the
chronically inflamed lung microenvironment. Thorax. 72:1140–1143.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Mizuno R, Kawada K, Itatani Y, Ogawa R,
Kiyasu Y and Sakai Y: The role of tumor-associated neutrophils in
colorectal cancer. Int J Mol Sci. 20:5292019. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Wang Y, Liu F, Chen L, Fang C, Li S, Yuan
S, Qian X, Yin Y, Yu B, Fu B, et al: Neutrophil extracellular traps
(NETs) promote non-small cell lung cancer metastasis by suppressing
lncRNA MIR503HG to activate the NF-κB/NLRP3 inflammasome pathway.
Front Immunol. 13:8675162022. View Article : Google Scholar
|
|
48
|
Adrover JM, McDowell SAC, He XY, Quail DF
and Egeblad M: NETworking with cancer: The bidirectional interplay
between cancer and neutrophil extracellular traps. Cancer Cell.
41:505–526. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Chu C, Wang X, Yang C, Chen F, Shi L, Xu
W, Wang K, Liu B, Wang C, Sun D and Ding W: Neutrophil
extracellular traps drive intestinal microvascular endothelial
ferroptosis by impairing Fundc1-dependent mitophagy. Redox Biol.
67:1029062023. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Zheng F, Ma L, Li X, Wang Z, Gao R, Peng
C, Kang B, Wang Y, Luo T, Wu J, et al: Neutrophil extracellular
traps induce glomerular endothelial cell dysfunction and pyroptosis
in diabetic kidney disease. Diabetes. 71:2739–2750. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Ngo AT, Skidmore A, Oberg J, Yarovoi I,
Sarkar A, Levine N, Bochenek V, Zhao G, Rauova L, Kowalska MA, et
al: Platelet factor 4 limits neutrophil extracellular trap- and
cell-free DNA-induced thrombogenicity and endothelial injury. JCI
Insight. 8:e1710542023. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Teijeira Á, Garasa S, Gato M, Alfaro C,
Migueliz I, Cirella A, de Andrea C, Ochoa MC, Otano I, Etxeberria
I, et al: CXCR1 and CXCR2 chemokine receptor agonists produced by
tumors induce neutrophil extracellular traps that interfere with
immune cytotoxicity. Immunity. 52:856–871.e8. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Cristinziano L, Modestino L, Antonelli A,
Marone G, Simon HU, Varricchi G and Galdiero MR: Neutrophil
extracellular traps in cancer. Semin Cancer Biol. 79:91–104. 2022.
View Article : Google Scholar
|
|
54
|
Pan JJ, Xie SZ, Zheng X, Xu JF, Xu H, Yin
RQ, Luo YL, Shen L, Chen ZR, Chen YR, et al: Acetyl-CoA metabolic
accumulation promotes hepatocellular carcinoma metastasis via
enhancing CXCL1-dependent infiltration of tumor-associated
neutrophils. Cancer Lett. 592:2169032024. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Sun B, Qin W, Song M, Liu L, Yu Y, Qi X
and Sun H: neutrophil suppresses tumor cell proliferation via
fas/fas ligand pathway mediated cell cycle arrested. Int J Biol
Sci. 14:2103–2113. 2018. View Article : Google Scholar :
|
|
56
|
Blaisdell A, Crequer A, Columbus D,
Daikoku T, Mittal K, Dey SK and Erlebacher A: Neutrophils oppose
uterine epithelial carcinogenesis via debridement of hypoxic tumor
cells. Cancer Cell. 28:785–799. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Gershkovitz M, Caspi Y, Fainsod-Levi T,
Katz B, Michaeli J, Khawaled S, Lev S, Polyansky L, Shaul ME,
Sionov RV, et al: TRPM2 mediates neutrophil killing of disseminated
tumor cells. Cancer Res. 78:2680–2690. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Li Y, Wu S, Zhao Y, Dinh T, Jiang D,
Selfridge JE, Myers G, Wang Y, Zhao X, Tomchuck S, et al:
Neutrophil extracellular traps induced by chemotherapy inhibit
tumor growth in murine models of colorectal cancer. J Clin Invest.
134:e1750312024. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Antuamwine BB, Bosnjakovic R, Hofmann-Vega
F, Wang X, Theodosiou T, Iliopoulos I and Brandau S: N1 versus N2
and PMN-MDSC: A critical appraisal of current concepts on
tumor-associated neutrophils and new directions for human oncology.
Immunol Rev. 314:250–279. 2023. View Article : Google Scholar
|
|
60
|
Koga Y, Matsuzaki A, Suminoe A, Hattori H
and Hara T: Neutrophil-derived TNF-related apoptosis-inducing
ligand (TRAIL): A novel mechanism of antitumor effect by
neutrophils. Cancer Res. 64:1037–1043. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Cui C, Chakraborty K, Tang XA, Zhou G,
Schoenfelt KQ, Becker KM, Hoffman A, Chang YF, Blank A, Reardon CA,
et al: Neutrophil elastase selectively kills cancer cells and
attenuates tumorigenesis. Cell. 184:3163–3177.e21. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Hirschhorn D, Budhu S, Kraehenbuehl L,
Gigoux M, Schröder D, Chow A, Ricca JM, Gasmi B, De Henau O,
Mangarin LMB, et al: T cell immunotherapies engage neutrophils to
eliminate tumor antigen escape variants. Cell. 186:1432–1447.e17.
2023. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Zhou Z, Wang P, Sun R, Li J, Hu Z, Xin H,
Luo C, Zhou J, Fan J and Zhou S: Tumor-associated neutrophils and
macrophages interaction contributes to intrahepatic
cholangiocarcinoma progression by activating STAT3. J Immunother
Cancer. 9:e0019462021. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Singhal S, Rao AS, Stadanlick J, Bruns K,
Sullivan NT, Bermudez A, Honig-Frand A, Krouse R, Arambepola S, Guo
E, et al: Human tumor-associated macrophages and neutrophils
regulate antitumor antibody efficacy through lethal and sublethal
trogocytosis. Cancer Res. 84:1029–1047. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Wu L and Zhang XH: Tumor-associated
neutrophils and macrophages-heterogenous but not chaotic. Front
Immunol. 11:5539672020. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Haider P, Kral-Pointner JB, Mayer J,
Richter M, Kaun C, Brostjan C, Eilenberg W, Fischer MB, Speidl WS,
Hengstenberg C, et al: Neutrophil extracellular trap degradation by
differently polarized macrophage subsets. Arterioscler Thromb Vasc
Biol. 40:2265–2278. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Prame Kumar K, Nicholls AJ and Wong CHY:
Partners in crime: Neutrophils and monocytes/macrophages in
inflammation and disease. Cell Tissue Res. 371:551–565. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Borella R, De Biasi S, Paolini A, Boraldi
F, Lo Tartaro D, Mattioli M, Fidanza L, Neroni A, Caro-Maldonado A,
Meschiari M, et al: Metabolic reprograming shapes neutrophil
functions in severe COVID-19. Eur J Immunol. 52:484–502. 2022.
View Article : Google Scholar
|
|
69
|
Cannarile MA, Weisser M, Jacob W, Jegg AM,
Ries CH and Rüttinger D: Colony-stimulating factor 1 receptor
(CSF1R) inhibitors in cancer therapy. J Immunother Cancer.
5:532017. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Cho H, Seo Y, Loke KM, Kim SW, Oh SM, Kim
JH, Soh J, Kim HS, Lee H, Kim J, et al: Cancer-stimulated CAFs
enhance monocyte differentiation and protumoral TAM Activation via
IL6 and GM-CSF Secretion. Clin Cancer Res. 24:5407–5421. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Schmidt E, Distel L, Erber R,
Büttner-Herold M, Rosahl MC, Ott OJ, Strnad V, Hack CC, Hartmann A,
Hecht M, et al: Tumor-associated neutrophils are a negative
prognostic factor in early luminal breast cancers lacking
immunosuppressive macrophage recruitment. Cancers (Basel).
16:31602024. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Puerta-Arias JD, Mejía SP and González Á:
The role of the interleukin-17 axis and neutrophils in the
pathogenesis of endemic and systemic mycoses. Front Cell Infect
Microbiol. 10:5953012020. View Article : Google Scholar
|
|
73
|
Murata K, Murao A, Aziz M and Wang P:
Extracellular CIRP induces novel Nectin-2+ (CD112+) neutrophils to
promote Th1 differentiation in sepsis. J Immunol. 210:310–321.
2023. View Article : Google Scholar
|
|
74
|
Parackova Z, Bloomfield M, Klocperk A and
Sediva A: Neutrophils mediate Th17 promotion in COVID-19 patients.
J Leukoc Biol. 109:73–76. 2021. View Article : Google Scholar
|
|
75
|
Mishalian I, Bayuh R, Eruslanov E,
Michaeli J, Levy L, Zolotarov L, Singhal S, Albelda SM, Granot Z
and Fridlender ZG: Neutrophils recruit regulatory T-cells into
tumors via secretion of CCL17-a new mechanism of impaired antitumor
immunity. Int J Cancer. 135:1178–1186. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Luo H, Ikenaga N, Nakata K, Higashijima N,
Zhong P, Kubo A, Wu C, Tsutsumi C, Shimada Y, Hayashi M, et al:
Tumor-associated neutrophils upregulate Nectin2 expression,
creating the immunosuppressive microenvironment in pancreatic
ductal adenocarcinoma. J Exp Clin Cancer Res. 43:2582024.
View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Sun R, Xiong Y, Liu H, Gao C, Su L, Weng
J, Yuan X, Zhang D and Feng J: Tumor-associated neutrophils
suppress antitumor immunity of NK cells through the PD-L1/PD-1
axis. Transl Oncol. 13:1008252020. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Tumino N, Besi F, Di Pace AL, Mariotti FR,
Merli P, Li Pira G, Galaverna F, Pitisci A, Ingegnere T, Pelosi A,
et al: PMN-MDSC are a new target to rescue graft-versus-leukemia
activity of NK cells in haplo-HSC transplantation. Leukemia.
34:932–937. 2020. View Article : Google Scholar :
|
|
79
|
Pelosi A, Besi F, Tumino N, Merli P,
Quatrini L, Li Pira G, Algeri M, Moretta L and Vacca P: NK Cells
and PMN-MDSCs in the graft from G-CSF mobilized haploidentical
donors display distinct gene expression profiles from those of the
non-mobilized counterpart. Front Immunol. 12:6573292021. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Mouchemore KA and Anderson RL:
Immunomodulatory effects of G-CSF in cancer: Therapeutic
implications. Semin Immunol. 54:1015122021. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Ogura K, Sato-Matsushita M, Yamamoto S,
Hori T, Sasahara M, Iwakura Y, Saiki I, Tahara H and Hayakawa Y: NK
cells control tumor-promoting function of neutrophils in mice.
Cancer Immunol Res. 6:348–357. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Li X, Xie G, Chen J, Wang Y, Zhai J and
Shen L: Tumour cell-derived serglycin promotes IL-8 secretion of
CAFs in gastric cancer. Br J Cancer. 131:271–282. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Song M, He J, Pan QZ, Yang J, Zhao J,
Zhang YJ, Huang Y, Tang Y, Wang Q, He J, et al: Cancer-associated
fibroblast-mediated cellular crosstalk supports hepatocellular
carcinoma progression. Hepatology. 73:1717–1735. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Li C, Chen T, Liu J, Wang Y, Zhang C, Guo
L, Shi D, Zhang T, Wang X and Li J: FGF19-Induced inflammatory CAF
promoted neutrophil extracellular trap formation in the liver
metastasis of colorectal cancer. Adv Sci (Weinh). 10:e23026132023.
View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Dudeck J, Kotrba J, Immler R, Hoffmann A,
Voss M, Alexaki VI, Morton L, Jahn SR, Katsoulis-Dimitriou K,
Winzer S, et al: Directional mast cell degranulation of tumor
necrosis factor into blood vessels primes neutrophil extravasation.
Immunity. 54:468–483.e5. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Li JY, Chen YP, Li YQ, Liu N and Ma J:
Chemotherapeutic and targeted agents can modulate the tumor
microenvironment and increase the efficacy of immune checkpoint
blockades. Mol Cancer. 20:272021. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Oliveira G and Wu CJ: Dynamics and
specificities of T cells in cancer immunotherapy. Nat Rev Cancer.
23:295–316. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Yi M, Zheng X, Niu M, Zhu S, Ge H and Wu
K: Combination strategies with PD-1/PD-L1 blockade: Current
advances and future directions. Mol Cancer. 21:282022. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Chu X, Tian W, Wang Z, Zhang J and Zhou R:
Co-inhibition of TIGIT and PD-1/PD-L1 in cancer immunotherapy:
Mechanisms and clinical trials. Mol Cancer. 22:932023. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Wu M, Huang Q, Xie Y, Wu X, Ma H, Zhang Y
and Xia Y: Improvement of the anticancer efficacy of PD-1/PD-L1
blockade via combination therapy and PD-L1 regulation. J Hematol
Oncol. 15:242022. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Gjuka D, Adib E, Garrison K, Chen J, Zhang
Y, Li W, Boutz D, Lamb C, Tanno Y, Nassar A, et al: Enzyme-mediated
depletion of methylthioadenosine restores T cell function in
MTAP-deficient tumors and reverses immunotherapy resistance. Cancer
Cell. 41:1774–1787.e9. 2023. View Article : Google Scholar
|
|
92
|
Niederlova V, Tsyklauri O, Kovar M and
Stepanek O: IL-2-driven CD8+ T cell phenotypes: Implications for
immunotherapy. Trends Immunol. 44:890–901. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Si J, Shi X, Sun S, Zou B, Li Y, An D, Lin
X, Gao Y, Long F, Pang B, et al: Hematopoietic progenitor kinase1
(HPK1) mediates T cell dysfunction and is a druggable target for T
cell-based immunotherapies. Cancer Cell. 38:551–566.e11. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Miao S, Rodriguez BL and Gibbons DL: The
multifaceted role of neutrophils in NSCLC in the era of immune
checkpoint inhibitors. Cancers (Basel). 16:25072024. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Xu P, Zhang X, Chen K, Zhu M, Jia R, Zhou
Q, Yang J, Dai J, Jin Y and Shi K: Tumor cell-derived
microparticles induced by methotrexate augment T-cell antitumor
responses by downregulating expression of PD-1 in neutrophils.
Cancer Immunol Res. 11:501–514. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Meng Y, Ye F, Nie P, Zhao Q, An L, Wang W,
Qu S, Shen Z, Cao Z, Zhang X, et al: Immunosuppressive CD10+ALPL+
neutrophils promote resistance to anti-PD-1 therapy in HCC by
mediating irreversible exhaustion of T cells. J Hepatol.
79:1435–1449. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Xie P, Yu M, Zhang B, Yu Q, Zhao Y, Wu M,
Jin L, Yan J, Zhou B, Liu S, et al: CRKL dictates anti-PD-1
resistance by mediating tumor-associated neutrophil infiltration in
hepatocellular carcinoma. J Hepatol. 81:93–107. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Michaeli J, Shaul ME, Mishalian I, Hovav
AH, Levy L, Zolotriov L, Granot Z and Fridlender ZG:
Tumor-associated neutrophils induce apoptosis of non-activated CD8
T-cells in a TNFα and NO-dependent mechanism, promoting a
tumor-supportive environment. Oncoimmunology. 6:e13569652017.
View Article : Google Scholar
|
|
99
|
Wang TT, Zhao YL, Peng LS, Chen N, Chen W,
Lv YP, Mao FY, Zhang JY, Cheng P, Teng YS, et al: Tumour-activated
neutrophils in gastric cancer foster immune suppression and disease
progression through GM-CSF-PD-L1 pathway. Gut. 66:1900–1911. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Kaltenmeier C, Yazdani HO, Morder K,
Geller DA, Simmons RL and Tohme S: Neutrophil extracellular traps
promote T cell exhaustion in the tumor microenvironment. Front
Immunol. 12:7852222021. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Xia Y, He J, Zhang H, Wang H, Tetz G,
Maguire CA, Wang Y, Onuma A, Genkin D, Tetz V, et al: AAV-mediated
gene transfer of DNase I in the liver of mice with colorectal
cancer reduces liver metastasis and restores local innate and
adaptive immune response. Mol Oncol. 14:2920–2935. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Zhang H, Wang Y, Onuma A, He J, Wang H,
Xia Y, Lal R, Cheng X, Kasumova G, Hu Z, et al: Neutrophils
extracellular traps inhibition improves PD-1 blockade immunotherapy
in colorectal cancer. Cancers (Basel). 13:53332021. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Peng JJ, Wang L, Li Z, Ku CL and Ho PC:
Metabolic challenges and interventions in CAR T cell therapy. Sci
Immunol. 8:eabq30162023. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Albelda SM: CAR T cell therapy for
patients with solid tumours: Key lessons to learn and unlearn. Nat
Rev Clin Oncol. 21:47–66. 2024. View Article : Google Scholar
|
|
105
|
Bulliard Y, Andersson BS, Baysal MA,
Damiano J and Tsimberidou AM: Reprogramming T cell differentiation
and exhaustion in CAR-T cell therapy. J Hematol Oncol. 16:1082023.
View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Pan K, Farrukh H, Chittepu VCSR, Xu H, Pan
CX and Zhu Z: CAR race to cancer immunotherapy: from CAR T, CAR NK
to CAR macrophage therapy. J Exp Clin Cancer Res. 41:1192022.
View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Hong M, Clubb JD and Chen YY: Engineering
CAR-T cells for next-generation cancer therapy. Cancer Cell.
38:473–488. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Zhang H, Yu P, Tomar VS, Chen X, Atherton
MJ, Lu Z, Zhang HG, Li S, Ortiz A, Gui J, et al: Targeting PARP11
to avert immunosuppression and improve CAR T therapy in solid
tumors. Nat Cancer. 3:808–820. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
The Lancet Oncology: CAR T-cell therapy
for solid tumours. Lancet Oncol. 22:8932021. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Li X, Zhu T, Wang R, Chen J, Tang L, Huo
W, Huang X and Cao Q: Genetically programmable vesicles for
enhancing CAR-T therapy against solid tumors. Adv Mater.
35:e22111382023. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Krishnan SR and Bebawy M: Circulating
biosignatures in multiple myeloma and their role in multidrug
resistance. Mol Cancer. 22:792023. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Wen X, Huang Z, Yang X, He X, Li L, Chen
H, Wang K, Guo Q and Liu J: Development of an aptamer capable of
multidrug resistance reversal for tumor combination chemotherapy.
Proc Natl Acad Sci USA. 121:e23211161212024. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Mousset A, Lecorgne E, Bourget I, Lopez P,
Jenovai K, Cherfils-Vicini J, Dominici C, Rios G, Girard-Riboulleau
C, Liu B, et al: Neutrophil extracellular traps formed during
chemotherapy confer treatment resistance via TGF-β activation.
Cancer Cell. 41:757–775.e10. 2023. View Article : Google Scholar
|
|
114
|
Saw PE, Chen J and Song E: ChemoNETosis: A
road to tumor therapeutic resistance. Cancer Cell. 41:655–657.
2023. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Yang Y, Yu S, Lv C and Tian Y: NETosis in
tumour microenvironment of liver: From primary to metastatic
hepatic carcinoma. Ageing Res Rev. 97:1022972024. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Kong X, Zhang Y, Xiang L, You Y, Duan Y,
Zhao Y, Li S, Wu R, Zhang J, Zhou L and Duan L: Fusobacterium
nucleatum-triggered neutrophil extracellular traps facilitate
colorectal carcinoma progression. J Exp Clin Cancer Res.
42:2362023. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Zhang Y, Yang Y, Hu X, Wang Z, Li L and
Chen P: PADs in cancer: Current and future. Biochim Biophys Acta
Rev Cancer. 1875:1884922021. View Article : Google Scholar
|
|
118
|
Zhan X, Wu R, Kong XH, You Y, He K, Sun
XY, Huang Y, Chen WX and Duan L: Elevated neutrophil extracellular
traps by HBV-mediated S100A9-TLR4/RAGE-ROS cascade facilitate the
growth and metastasis of hepatocellular carcinoma. Cancer Commun
(Lond). 43:225–245. 2023. View Article : Google Scholar
|
|
119
|
Mousset A, Bellone L, Gaggioli C and
Albrengues J: NETscape or NEThance: Tailoring anti-cancer therapy.
Trends Cancer. 10:655–667. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Ramachandran IR, Condamine T, Lin C,
Herlihy SE, Garfall A, Vogl DT, Gabrilovich DI and Nefedova Y: Bone
marrow PMN-MDSCs and neutrophils are functionally similar in
protection of multiple myeloma from chemotherapy. Cancer Lett.
371:117–124. 2016. View Article : Google Scholar :
|
|
121
|
Tamura K, Miyato H, Kanamaru R, Sadatomo
A, Takahashi K, Ohzawa H, Koyanagi T, Saga Y, Takei Y, Fujiwara H,
et al: Neutrophil extracellular traps (NETs) reduce the diffusion
of doxorubicin which may attenuate its ability to induce apoptosis
of ovarian cancer cells. Heliyon. 8:e097302022. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Goenka A, Khan F, Verma B, Sinha P, Dmello
CC, Jogalekar MP, Gangadaran P and Ahn BC: Tumor microenvironment
signaling and therapeutics in cancer progression. Cancer Commun
(Lond). 43:525–561. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Zhang R, Dong M, Tu J, Li F, Deng Q, Xu J,
He X, Ding J, Xia J, Sheng D, et al: PMN-MDSCs modulated by CCL20
from cancer cells promoted breast cancer cell stemness through
CXCL2-CXCR2 pathway. Signal Transduct Target Ther. 8:972023.
View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Kang J, La Manna F, Bonollo F, Sampson N,
Alberts IL, Mingels C, Afshar-Oromieh A, Thalmann GN and
Karkampouna S: Tumor microenvironment mechanisms and bone
metastatic disease progression of prostate cancer. Cancer Lett.
530:156–169. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Capucetti A, Albano F and Bonecchi R:
Multiple roles for chemokines in neutrophil biology. Front Immunol.
11:12592020. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Rajarathnam K, Schnoor M, Richardson RM
and Rajagopal S: How do chemokines navigate neutrophils to the
target site: Dissecting the structural mechanisms and signaling
pathways. Cell Signal. 54:69–80. 2019. View Article : Google Scholar :
|
|
127
|
Bianchi A, De Castro Silva I, Deshpande
NU, Singh S, Mehra S, Garrido VT, Guo X, Nivelo LA, Kolonias DS,
Saigh SJ, et al: Cell-Autonomous Cxcl1 Sustains Tolerogenic
Circuitries and Stromal Inflammation via Neutrophil-Derived TNF in
Pancreatic Cancer. Cancer Discov. 13:1428–1453. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Chao T, Furth EE and Vonderheide RH:
CXCR2-Dependent accumulation of tumor-associated neutrophils
regulates T-cell immunity in pancreatic ductal adenocarcinoma.
Cancer Immunol Res. 4:968–982. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Corsaro A, Tremonti B, Bajetto A, Barbieri
F, Thellung S and Florio T: Chemokine signaling in tumors:
potential role of CXC chemokines and their receptors as
glioblastoma therapeutic targets. Expert Opin Ther Targets.
28:937–952. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Powell D, Lou M, Barros Becker F and
Huttenlocher A: Cxcr1 mediates recruitment of neutrophils and
supports proliferation of tumor-initiating astrocytes in vivo. Sci
Rep. 8:132852018. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Jablonska J, Wu CF, Andzinski L, Leschner
S and Weiss S: CXCR2-mediated tumor-associated neutrophil
recruitment is regulated by IFN-β. Int J Cancer. 134:1346–1358.
2014. View Article : Google Scholar
|
|
132
|
Haider C, Hnat J, Wagner R, Huber H,
Timelthaler G, Grubinger M, Coulouarn C, Schreiner W, Schlangen K,
Sieghart W, et al: Transforming growth factor-β and Axl induce
CXCL5 and neutrophil recruitment in hepatocellular carcinoma.
Hepatology. 69:222–236. 2019. View Article : Google Scholar
|
|
133
|
Zhou SL, Yin D, Hu ZQ, Luo CB, Zhou ZJ,
Xin HY, Yang XR, Shi YH, Wang Z, Huang XW, et al: A positive
feedback loop between cancer stem-like cells and tumor-associated
neutrophils controls hepatocellular carcinoma progression.
Hepatology. 70:1214–1230. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
134
|
Zhou SL, Zhou ZJ, Hu ZQ, Huang XW, Wang Z,
Chen EB, Fan J, Cao Y, Dai Z and Zhou J: Tumor-associated
neutrophils recruit macrophages and T-regulatory cells to promote
progression of hepatocellular carcinoma and resistance to
sorafenib. Gastroenterology. 150:1646–1658.e17. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
135
|
He J, Zhou M, Yin J, Wan J, Chu J, Jia J,
Sheng J, Wang C, Yin H and He F: METTL3 restrains papillary thyroid
cancer progression via m6A/c-Rel/IL-8-mediated neutrophil
infiltration. Mol Ther. 29:1821–1837. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Schimek V, Strasser K, Beer A, Göber S,
Walterskirchen N, Brostjan C, Müller C, Bachleitner-Hofmann T,
Bergmann M, Dolznig H and Oehler R: Tumour cell apoptosis modulates
the colorectal cancer immune microenvironment via
interleukin-8-dependent neutrophil recruitment. Cell Death Dis.
13:1132022. View Article : Google Scholar : PubMed/NCBI
|
|
137
|
Bellomo G, Rainer C, Quaranta V, Astuti Y,
Raymant M, Boyd E, Stafferton R, Campbell F, Ghaneh P, Halloran CM,
et al: Chemotherapy-induced infiltration of neutrophils promotes
pancreatic cancer metastasis via Gas6/AXL signalling axis. Gut.
71:2284–2299. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Nywening TM, Belt BA, Cullinan DR, Panni
RZ, Han BJ, Sanford DE, Jacobs RC, Ye J, Patel AA, Gillanders WE,
et al: Targeting both tumour-associated CXCR2+ neutrophils and
CCR2+ macrophages disrupts myeloid recruitment and improves
chemotherapeutic responses in pancreatic ductal adenocarcinoma.
Gut. 67:1112–1123. 2018. View Article : Google Scholar
|
|
139
|
Cheng Y, Ma XL, Wei YQ and Wei XW:
Potential roles and targeted therapy of the CXCLs/CXCR2 axis in
cancer and inflammatory diseases. Biochim Biophys Acta Rev Cancer.
1871:289–312. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
140
|
Schott AF, Goldstein LJ, Cristofanilli M,
Ruffini PA, McCanna S, Reuben JM, Perez RP, Kato G and Wicha M:
Phase Ib pilot study to evaluate reparixin in combination with
weekly paclitaxel in patients with HER-2-negative metastatic breast
cancer. Clin Cancer Res. 23:5358–5365. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
141
|
Jiang H, Cui J, Chu H, Xu T, Xie M, Jing
X, Xu J, Zhou J and Shu Y: Targeting IL8 as a sequential therapy
strategy to overcome chemotherapy resistance in advanced gastric
cancer. Cell Death Discov. 8:2352022. View Article : Google Scholar : PubMed/NCBI
|
|
142
|
Cheng Y, Mo F, Li Q, Han X, Shi H, Chen S,
Wei Y and Wei X: Targeting CXCR2 inhibits the progression of lung
cancer and promotes therapeutic effect of cisplatin. Mol Cancer.
20:622021. View Article : Google Scholar : PubMed/NCBI
|
|
143
|
Kiri S and Ryba T: Cancer, metastasis, and
the epigenome. Mol Cancer. 23:1542024. View Article : Google Scholar : PubMed/NCBI
|
|
144
|
Fang Y, Wang S, Han S, Zhao Y, Yu C, Liu H
and Li N: Targeted protein degrader development for cancer:
Advances, challenges, and opportunities. Trends Pharmacol Sci.
44:303–317. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
145
|
Liu ZL, Chen HH, Zheng LL, Sun LP and Shi
L: Angiogenic signaling pathways and anti-angiogenic therapy for
cancer. Signal Transduct Target Ther. 8:1982023. View Article : Google Scholar : PubMed/NCBI
|
|
146
|
Zhang T, Jia Y, Yu Y, Zhang B, Xu F and
Guo H: Targeting the tumor biophysical microenvironment to reduce
resistance to immunotherapy. Adv Drug Deliv Rev. 186:1143192022.
View Article : Google Scholar : PubMed/NCBI
|
|
147
|
Yang M, Mu Y, Yu X, Gao D, Zhang W, Li Y,
Liu J, Sun C and Zhuang J: Survival strategies: How tumor hypoxia
microenvironment orchestrates angiogenesis. Biomed Pharmacother.
176:1167832024. View Article : Google Scholar : PubMed/NCBI
|
|
148
|
Li H, Qiu Z, Li F and Wang C: The
relationship between MMP-2 and MMP-9 expression levels with breast
cancer incidence and prognosis. Oncol Lett. 14:5865–5870.
2017.PubMed/NCBI
|
|
149
|
Negri L and Ferrara N: The prokineticins:
Neuromodulators and mediators of inflammation and myeloid
cell-dependent angiogenesis. Physiol Rev. 98:1055–1082. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
150
|
Shojaei F and Ferrara N: Refractoriness to
antivascular endothelial growth factor treatment: Role of myeloid
cells. Cancer Res. 68:5501–5504. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
151
|
Shojaei F, Wu X, Zhong C, Yu L, Liang XH,
Yao J, Blanchard D, Bais C, Peale FV, van Bruggen N, et al: Bv8
regulates myeloid-cell-dependent tumour angiogenesis. Nature.
450:825–831. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
152
|
Majidpoor J and Mortezaee K: Angiogenesis
as a hallmark of solid tumors-clinical perspectives. Cell Oncol
(Dordr). 44:715–737. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
153
|
Chung AS, Wu X, Zhuang G, Ngu H, Kasman I,
Zhang J, Vernes JM, Jiang Z, Meng YG, Peale FV, et al: An
interleukin-17-mediated paracrine network promotes tumor resistance
to anti-angiogenic therapy. Nat Med. 19:1114–1123. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
154
|
Li TJ, Jiang YM, Hu YF, Huang L, Yu J,
Zhao LY, Deng HJ, Mou TY, Liu H, Yang Y, et al:
Interleukin-17-producing neutrophils link inflammatory stimuli to
disease progression by promoting angiogenesis in gastric cancer.
Clin Cancer Res. 23:1575–1585. 2017. View Article : Google Scholar
|
|
155
|
Lee JM, McNamee CJ, Toloza E, Negrao MV,
Lin J, Shum E, Cummings AL, Kris MG, Sepesi B, Bara I, et al:
Neoadjuvant targeted therapy in resectable NSCLC: Current and
future perspectives. J Thorac Oncol. 18:1458–1477. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
156
|
Napolitano S, Martini G, Ciardiello D, Del
Tufo S, Martinelli E, Troiani T and Ciardiello F: Targeting the
EGFR signalling pathway in metastatic colorectal cancer. Lancet
Gastroenterol Hepatol. 9:664–676. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
157
|
Damare R, Engle K and Kumar G: Targeting
epidermal growth factor receptor and its downstream signaling
pathways by natural products: A mechanistic insight. Phytother Res.
38:2406–2447. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
158
|
Wang X, Jiang W, Du Y, Zhu D, Zhang J,
Fang C, Yan F and Chen ZS: Targeting feedback activation of
signaling transduction pathways to overcome drug resistance in
cancer. Drug Resist Updat. 65:1008842022. View Article : Google Scholar : PubMed/NCBI
|
|
159
|
Kim GT, Hahn KW, Yoon SY, Sohn KY and Kim
JW: PLAG exerts anti-metastatic effects by interfering with
neutrophil elastase/PAR2/EGFR signaling in A549 lung cancer
orthotopic model. Cancers (Basel). 12:5602020. View Article : Google Scholar : PubMed/NCBI
|
|
160
|
Swain SM, Shastry M and Hamilton E:
Targeting HER2-positive breast cancer: Advances and future
directions. Nat Rev Drug Discov. 22:101–126. 2023. View Article : Google Scholar
|
|
161
|
Sato T, Takahashi S, Mizumoto T, Harao M,
Akizuki M, Takasugi M, Fukutomi T and Yamashita J: Neutrophil
elastase and cancer. Surg Oncol. 15:217–222. 2006. View Article : Google Scholar
|
|
162
|
Schlessinger J: Common and distinct
elements in cellular signaling via EGF and FGF receptors. Science.
306:1506–1507. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
163
|
Singh JK, Farnie G, Bundred NJ, Simões BM,
Shergill A, Landberg G, Howell SJ and Clarke RB: Targeting CXCR1/2
significantly reduces breast cancer stem cell activity and
increases the efficacy of inhibiting HER2 via HER2-dependent and
-independent mechanisms. Clin Cancer Res. 19:643–656. 2013.
View Article : Google Scholar
|
|
164
|
Slamon DJ, Leyland-Jones B, Shak S, Fuchs
H, Paton V, Bajamonde A, Fleming T, Eiermann W, Wolter J, Pegram M,
et al: Use of chemotherapy plus a monoclonal antibody against HER2
for metastatic breast cancer that overexpresses HER2. N Engl J Med.
344:783–792. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
165
|
Singhal A, Li BT and O'Reilly EM:
Targeting KRAS in cancer. Nat Med. 30:969–983. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
166
|
Biller LH and Schrag D: Diagnosis and
treatment of metastatic colorectal cancer: A review. JAMA.
325:669–685. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
167
|
Zhu G, Pei L, Xia H, Tang Q and Bi F: Role
of oncogenic KRAS in the prognosis, diagnosis and treatment of
colorectal cancer. Mol Cancer. 20:1432021. View Article : Google Scholar : PubMed/NCBI
|
|
168
|
Shang A, Gu C, Zhou C, Yang Y, Chen C,
Zeng B, Wu J, Lu W, Wang W, Sun Z and Li D: Exosomal KRAS mutation
promotes the formation of tumor-associated neutrophil extracellular
traps and causes deterioration of colorectal cancer by inducing
IL-8 expression. Cell Commun Signal. 18:522020. View Article : Google Scholar : PubMed/NCBI
|
|
169
|
Pickup MW, Owens P, Gorska AE, Chytil A,
Ye F, Shi C, Weaver VM, Kalluri R, Moses HL and Novitskiy SV:
Development of aggressive pancreatic ductal adenocarcinomas depends
on granulocyte colony stimulating factor secretion in carcinoma
cells. Cancer Immunol Res. 5:718–729. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
170
|
Nolan E, Bridgeman VL, Ombrato L, Karoutas
A, Rabas N, Sewnath CAN, Vasquez M, Rodrigues FS, Horswell S, Faull
P, et al: Radiation exposure elicits a neutrophil-driven response
in healthy lung tissue that enhances metastatic colonization. Nat
Cancer. 3:173–187. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
171
|
Wisdom AJ, Hong CS, Lin AJ, Xiang Y,
Cooper DE, Zhang J, Xu ES, Kuo HC, Mowery YM, Carpenter DJ, et al:
Neutrophils promote tumor resistance to radiation therapy. Proc
Natl Acad Sci USA. 116:18584–18589. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
172
|
Zheng X, Song X, Zhu G, Pan D, Li H, Hu J,
Xiao K, Gong Q, Gu Z, Luo K and Li W: Nanomedicine combats drug
resistance in lung cancer. Adv Mater. 36:e23089772024. View Article : Google Scholar
|
|
173
|
Xu K, Guo H, Xia A, Wang Z, Wang S and
Wang Q: Non-coding RNAs in radiotherapy resistance: Roles and
therapeutic implications in gastrointestinal cancer. Biomed
Pharmacother. 161:1144852023. View Article : Google Scholar : PubMed/NCBI
|
|
174
|
Wu Y, Song Y, Wang R and Wang T: Molecular
mechanisms of tumor resistance to radiotherapy. Mol Cancer.
22:962023. View Article : Google Scholar : PubMed/NCBI
|
|
175
|
An L, Li M and Jia Q: Mechanisms of
radiotherapy resistance and radiosensitization strategies for
esophageal squamous cell carcinoma. Mol Cancer. 22:1402023.
View Article : Google Scholar : PubMed/NCBI
|
|
176
|
Peng J, Yin X, Yun W, Meng X and Huang Z:
Radiotherapyinduced tumor physical microenvironment remodeling to
overcome immunotherapy resistance. Cancer Lett. 559:2161082023.
View Article : Google Scholar
|
|
177
|
Beckers C, Pruschy M and Vetrugno I: Tumor
hypoxia and radiotherapy: A major driver of resistance even for
novel radiotherapy modalities. Semin Cancer Biol. 98:19–30. 2024.
View Article : Google Scholar
|
|
178
|
Wang X, Li X, Wu Y, Hong J and Zhang M:
The prognostic significance of tumor-associated neutrophils and
circulating neutrophils in glioblastoma (WHO CNS5 classification).
BMC Cancer. 23:202023. View Article : Google Scholar : PubMed/NCBI
|
|
179
|
Jeon HY, Ham SW, Kim JK, Jin X, Lee SY,
Shin YJ, Choi CY, Sa JK, Kim SH, Chun T, et al: Ly6G+ inflammatory
cells enable the conversion of cancer cells to cancer stem cells in
an irradiated glioblastoma model. Cell Death Differ. 26:2139–2156.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
180
|
Ruiz-Fernández de Córdoba B, Moreno H,
Valencia K, Perurena N, Ruedas P, Walle T, Pezonaga-Torres A,
Hinojosa J, Guruceaga E, Pineda-Lucena A, et al: Tumor ENPP1
(CD203a)/ haptoglobin axis exploits myeloid-derived suppressor
cells to promote post-radiotherapy local recurrence in breast
cancer. Cancer Discov. 12:1356–1377. 2022. View Article : Google Scholar
|
|
181
|
Ancey PB, Contat C, Boivin G, Sabatino S,
Pascual J, Zangger N, Perentes JY, Peters S, Abel ED, Kirsch DG, et
al: GLUT1 expression in tumor-associated neutrophils promotes lung
cancer growth and resistance to radiotherapy. Cancer Res.
81:2345–2357. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
182
|
Shinde-Jadhav S, Mansure JJ, Rayes RF,
Marcq G, Ayoub M, Skowronski R, Kool R, Bourdeau F, Brimo F, Spicer
J and Kassouf W: Role of neutrophil extracellular traps in
radiation resistance of invasive bladder cancer. Nat Commun.
12:27762021. View Article : Google Scholar : PubMed/NCBI
|
|
183
|
Li H, Zeng J, You Q, Zhang M, Shi Y, Yang
X, Gu W, Liu Y, Hu N, Wang Y, et al: X-ray-activated
nanoscintillators integrated with tumor-associated neutrophils
polarization for improved radiotherapy in metastatic colorectal
cancer. Biomaterials. 316:1230312025. View Article : Google Scholar
|
|
184
|
Rys RN and Calcinotto A: Senescent
neutrophils: A hidden role in cancer progression. Trends Cell Biol.
S0962-8924(24)00187-9. 2024.Epub ahead of print. View Article : Google Scholar : PubMed/NCBI
|
|
185
|
Treffers LW, Ten Broeke T, Rösner T,
Jansen JHM, van Houdt M, Kahle S, Schornagel K, Verkuijlen PJJH,
Prins JM, Franke K, et al: IgA-mediated killing of tumor cells by
neutrophils is enhanced by CD47-SIRPα checkpoint inhibition. Cancer
Immunol Res. 8:120–130. 2020. View Article : Google Scholar
|
|
186
|
Brandsma AM, Ten Broeke T, Nederend M,
Meulenbroek LA, van Tetering G, Meyer S, Jansen JH, Beltrán
Buitrago MA, Nagelkerke SQ, Németh I, et al: Simultaneous targeting
of FcγRs and FcαRI enhances tumor cell killing. Cancer Immunol Res.
3:1316–1324. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
187
|
Borrok MJ, Luheshi NM, Beyaz N, Davies GC,
Legg JW, Wu H, Dall'Acqua WF and Tsui P: Enhancement of
antibody-dependent cell-mediated cytotoxicity by endowing IgG with
FcαRI (CD89) binding. MAbs. 7:743–751. 2015. View Article : Google Scholar :
|
|
188
|
Kumbhojkar N, Prakash S, Fukuta T,
Adu-Berchie K, Kapate N, An R, Darko S, Chandran Suja V, Park KS,
Gottlieb AP, et al: Neutrophils bearing adhesive polymer
micropatches as a drug-free cancer immunotherapy. Nat Biomed Eng.
8:579–592. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
189
|
Quaas A, Pamuk A, Klein S, Quantius J,
Rehkaemper J, Bar utcu AG, Rueschoff J, Zander T, Gebauer F,
Hillmer A, et al: Sex-specific prognostic effect of CD66b-positive
tumor-infiltrating neutrophils (TANs) in gastric and esophageal
adenocarcinoma. Gastric Cancer. 24:1213–1226. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
190
|
Peng H, Wu X, Liu S, He M, Tang C, Wen Y,
Xie C, Zhong R, Li C, Xiong S, et al: Cellular dynamics in tumour
microenvironment along with lung cancer progression underscore
spatial and evolutionary heterogeneity of neutrophil. Clin Transl
Med. 13:e13402023. View Article : Google Scholar : PubMed/NCBI
|
|
191
|
Zhang J, Zhang M, Lou J, Wu L, Zhang S,
Liu X, Ke Y, Zhao S, Song Z, Bai X, et al: Machine learning
integration with single-cell transcriptome sequencing datasets
reveals the impact of tumor-associated neutrophils on the immune
microenvironment and immunotherapy outcomes in gastric cancer. Int
J Mol Sci. 25:127152024. View Article : Google Scholar : PubMed/NCBI
|
|
192
|
Ye L, Zhang T, Kang Z, Guo G, Sun Y, Lin
K, Huang Q, Shi X, Ni Z, Ding N, et al: Tumor-infiltrating immune
cells act as a marker for prognosis in colorectal cancer. Front
Immunol. 10:23682019. View Article : Google Scholar : PubMed/NCBI
|
|
193
|
Nøst TH, Alcala K, Urbarova I, Byrne KS,
Guida F, Sandanger TM and Johansson M: Systemic inflammation
markers and cancer incidence in the UK Biobank. Eur J Epidemiol.
36:841–848. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
194
|
Mosca M, Nigro MC, Pagani R, De Giglio A
and Di Federico A: Neutrophil-to-lymphocyte ratio (NLR) in NSCLC,
gastrointestinal, and other solid tumors: Immunotherapy and beyond.
Biomolecules. 13:18032023. View Article : Google Scholar : PubMed/NCBI
|
|
195
|
Cupp MA, Cariolou M, Tzoulaki I, Aune D,
Evangelou E and Berlanga-Taylor AJ: Neutrophil to lymphocyte ratio
and cancer prognosis: An umbrella review of systematic reviews and
meta-analyses of observational studies. BMC Med. 18:3602020.
View Article : Google Scholar : PubMed/NCBI
|
|
196
|
Ethier JL, Desautels D, Templeton A, Shah
PS and Amir E: Prognostic role of neutrophil-to-lymphocyte ratio in
breast cancer: A systematic review and meta-analysis. Breast Cancer
Res. 19:22017. View Article : Google Scholar : PubMed/NCBI
|
|
197
|
Pecqueux M, Brückner F, Oehme F, Hempel S,
Baenke F, Riediger C, Distler M, Weitz J and Kahlert C:
Preoperative IL-8 levels as prognostic indicators of overall
survival: An extended follow-up in a prospective cohort with
colorectal liver metastases. BMC Cancer. 24:902024. View Article : Google Scholar : PubMed/NCBI
|
|
198
|
Hsu YJ, Chern YJ, Wu ZE, Yu YL, Liao CK,
Tsai WS, You JF and Lee CW: The oncologic outcome and prognostic
factors for solitary colorectal liver metastasis after liver
resection. J Gastrointest Surg. 28:267–275. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
199
|
Huang W, Jiang Y, Xiong W, Sun Z, Chen C,
Yuan Q, Zhou K, Han Z, Feng H, Chen H, et al: Noninvasive imaging
of the tumor immune microenvironment correlates with response to
immunotherapy in gastric cancer. Nat Commun. 13:50952022.
View Article : Google Scholar : PubMed/NCBI
|
|
200
|
Tan S, Zheng Q, Zhang W, Zhou M, Xia C and
Feng W: Prognostic value of inflammatory markers NLR, PLR, and LMR
in gastric cancer patients treated with immune checkpoint
inhibitors: A meta-analysis and systematic review. Front Immunol.
15:14087002024. View Article : Google Scholar : PubMed/NCBI
|
|
201
|
He G, Zhang H, Zhou J, Wang B, Chen Y,
Kong Y, Xie X, Wang X, Fei R, Wei L, et al: Peritumoural
neutrophils negatively regulate adaptive immunity via the
PD-L1/PD-1 signalling pathway in hepatocellular carcinoma. J Exp
Clin Cancer Res. 34:1412015. View Article : Google Scholar : PubMed/NCBI
|