|
1
|
Zhao P, Zhao S, Huang C, Li Y, Wang J, Xu
J, Li L, Qian Z, Li W, Zhou S, et al: Efficacy and safety of
polatuzumab vedotin plus rituximab, cyclophosphamide, doxorubicin
and prednisone for previously untreated diffuse large B-cell
lymphoma: A real-world, multi-center, retrospective cohort study.
Hematol Oncol. 43:e700172025. View Article : Google Scholar
|
|
2
|
Vaughn JL, Ramdhanny A, Munir M,
Rimmalapudi S and Epperla N: A comparative analysis of transformed
indolent lymphomas and de novo diffuse large B-cell lymphoma: A
population-based cohort study. Blood Cancer J. 14:2122024.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Schmitz R, Wright GW, Huang DW, Johnson
CA, Phelan JD, Wang JQ, Roulland S, Kasbekar M, Young RM, Shaffer
AL, et al: Genetics and pathogenesis of diffuse large B-cell
lymphoma. N Engl J Med. 378:1396–1407. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Bantilan KS, Smith AN, Maurer MJ,
Teruya-Feldstein J, Matasar MJ, Moskowitz AJ, Straus DJ, Noy A,
Palomba ML, Horwitz SM, et al: Matched control analysis suggests
that R-CHOP followed by (R)-ICE may improve outcome in non-GCB
DLBCL compared with R-CHOP. Blood Adv. 8:2172–2181. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
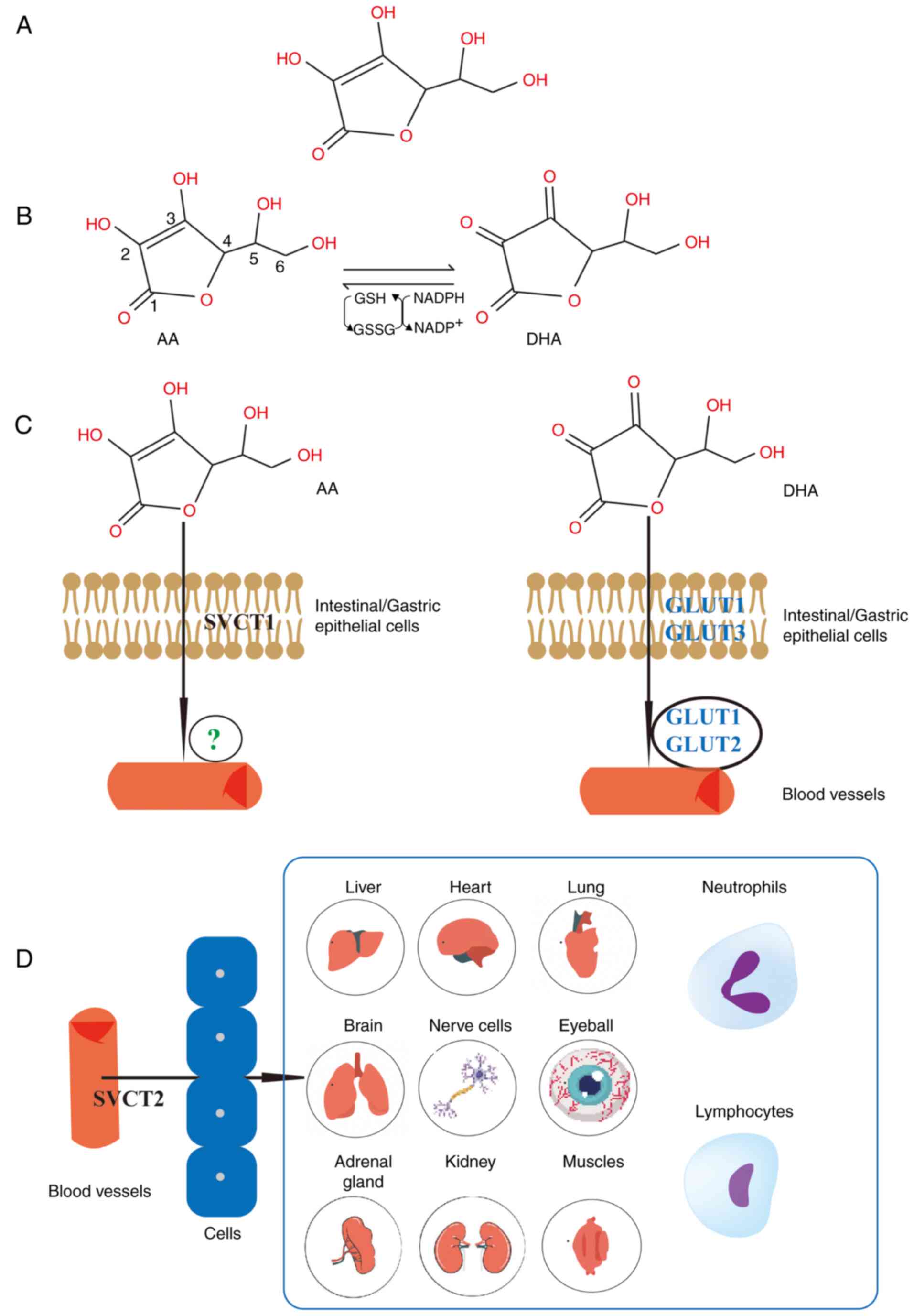
García-Sancho AM, Cabero A and Gutiérrez
NC: Treatment of relapsed or refractory diffuse large B-cell
lymphoma: New approved options. J Clin Med. 13:702023. View Article : Google Scholar
|
|
6
|
Coiffier B, Thieblemont C, Van Den Neste
E, Lepeu G, Plantier I, Castaigne S, Lefort S, Marit G, Macro M,
Sebban C, et al: Long-term outcome of patients in the LNH-98.5
trial, the first randomized study comparing rituximab-CHOP to
standard CHOP chemotherapy in DLBCL patients: a study by the Groupe
d'Etudes des Lymphomes de l'Adulte. Blood. 116:2040–2045. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Pfreundschuh M, Trümper L, Osterborg A,
Pettengell R, Trneny M, Imrie K, Ma D, Gill D, Walewski J, Zinzani
PL, et al: CHOP-like chemotherapy plus rituximab versus CHOP-like
chemotherapy alone in young patients with good-prognosis diffuse
large-B-cell lymphoma: A randomised controlled trial by the
MabThera international trial (MInT) group. Lancet Oncol. 7:379–391.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Pinzone MR, Berretta M, Cacopardo B and
Nunnari G: Epstein-barr virus- and Kaposi sarcoma-associated
herpesvirus-related malignancies in the setting of human
immunodeficiency virus infection. Semin Oncol. 42:258–271. 2015.
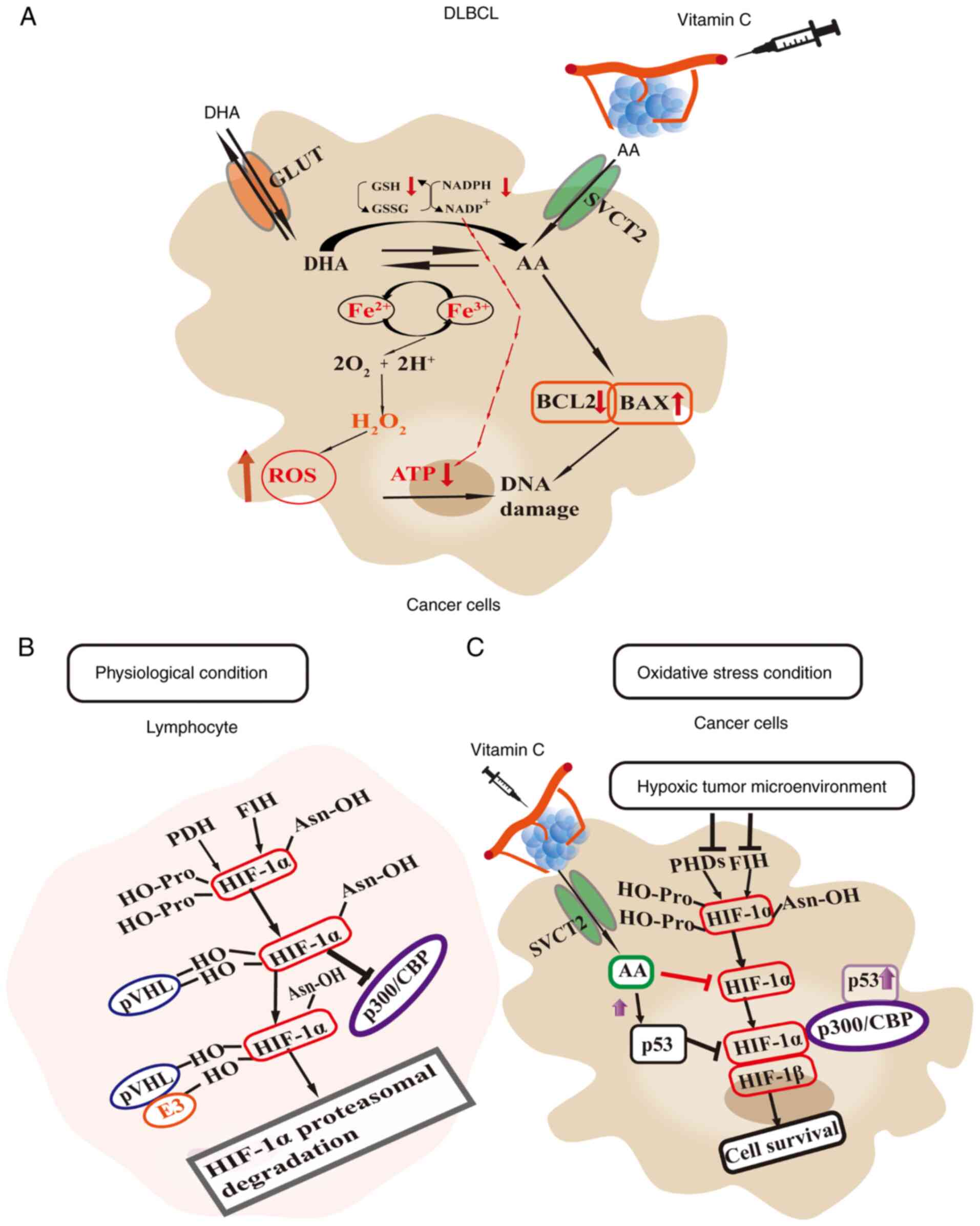
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Chapman JR, Bouska AC, Zhang W, Alderuccio
JP, Lossos IS, Rimsza LM, Maguire A, Yi S, Chan WC, Vega F and Song
JY: EBV-positive HIV-associated diffuse large B cell lymphomas are
characterized by JAK/STAT (STAT3) pathway mutations and unique
clinicopathologic features. Br J Haematol. 194:870–878. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Gianella S, Anderson CM, Var SR, Oliveira
MF, Lada SM, Vargas MV, Massanella M, Little SJ, Richman DD, Strain
MC, et al: Replication of human herpesviruses is associated with
higher HIV DNA levels during antiretroviral therapy started at
early phases of HIV infection. J Virol. 90:3944–3952. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Wang SS: Epidemiology and etiology of
diffuse large B-cell lymphoma. Semin Hematol. 60:255–266. 2023.
View Article : Google Scholar
|
|
12
|
Ekström Smedby K, Vajdic CM, Falster M,
Engels EA, Martínez-Maza O, Turner J, Hjalgrim H, Vineis P, Seniori
Costantini A, Bracci PM, et al: Autoimmune disorders and risk of
non-Hodgkin lymphoma subtypes: A pooled analysis within the
InterLymph consortium. Blood. 111:4029–4038. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Yang L, Liang Y, Pu J, Cai L, Gao R, Han
F, Chang K, Pan S, Wu Z, Zhang Y, et al: Dysregulated serum lipid
profile is associated with inflammation and disease activity in
primary Sjögren's syndrome: A retrospective study in China. Immunol
Lett. 267:1068652024. View Article : Google Scholar
|
|
14
|
Almasmoum HA: Molecular complexity of
diffuse large B-cell lymphoma: A molecular perspective and
therapeutic implications. J Appl Genet. 65:57–72. 2024. View Article : Google Scholar
|
|
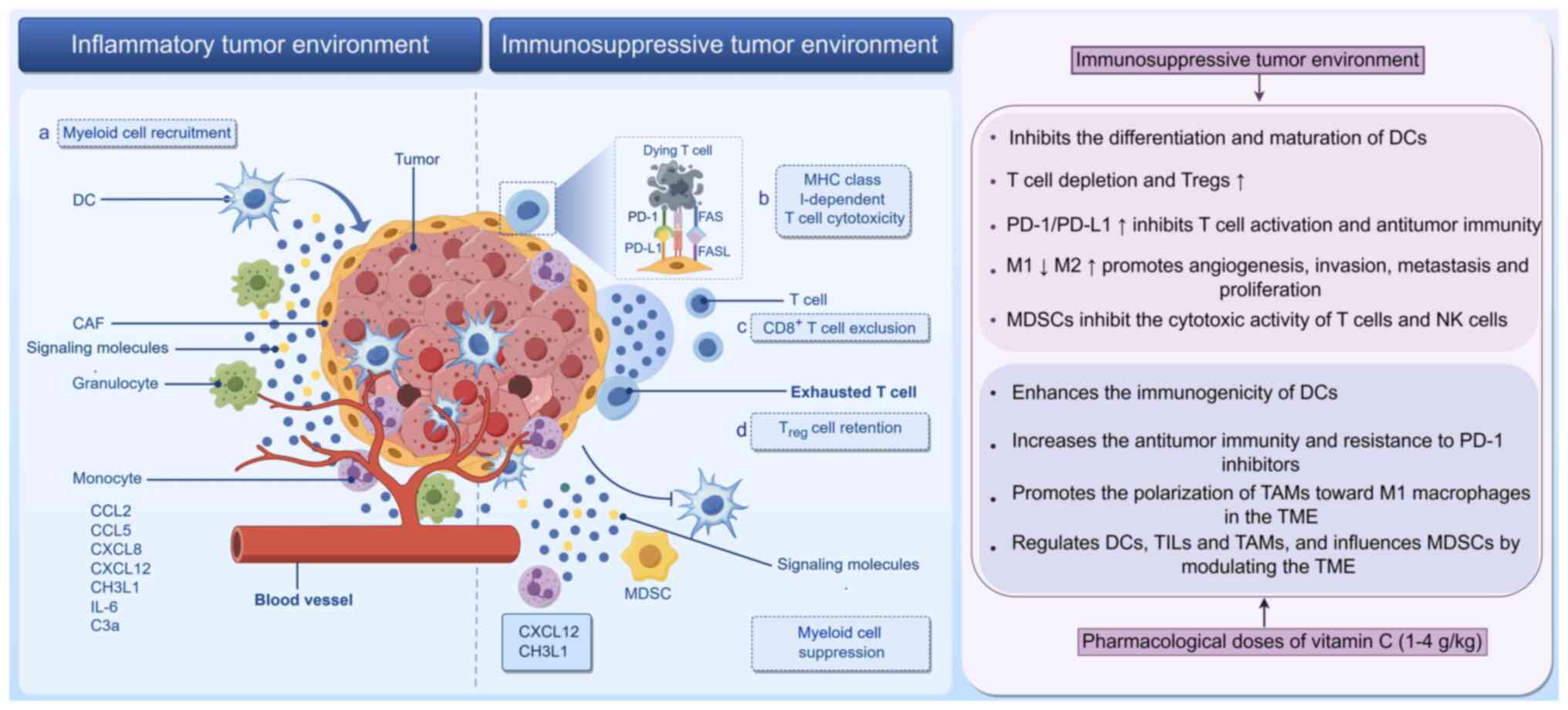
15
|
Serganova I, Chakraborty S, Yamshon S,
Isshiki Y, Bucktrout R, Melnick A, Béguelin W and Zappasodi R:
Epigenetic, metabolic, and immune crosstalk in
germinal-center-derived B-cell lymphomas: Unveiling new
vulnerabilities for rational combination therapies. Front Cell Dev
Biol. 9:8051952022. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Horn H, Ziepert M, Becher C, Barth TF,
Bernd HW, Feller AC, Klapper W, Hummel M, Stein H, Hansmann ML, et
al: MYC status in concert with BCL2 and BCL6 expression predicts
outcome in diffuse large B-cell lymphoma. Blood. 121:2253–2263.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Riedell PA and Smith SM: Double hit and
double expressors in lymphoma: Definition and treatment. Cancer.
124:4622–4632. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Cioroianu AI, Stinga PI, Sticlaru L,
Cioplea MD, Nichita L, Popp C and Staniceanu F: Tumor
microenvironment in diffuse large B-cell lymphoma: role and
prognosis. Anal Cell Pathol (Amst). 2019:85863542019.
|
|
19
|
Momivand M, Razaghi M, Mohammadi F,
Hoseinzadeh E and Najafi-Vosough R: The status of serum 25(OH)D
levels is related to breast cancer. Cancer Treat Res Commun.
42:1008702024. View Article : Google Scholar
|
|
20
|
Jang Y and Kim CY: The role of vitamin e
isoforms and metabolites in cancer prevention: Mechanistic insights
into sphingolipid metabolism modulation. Nutrients. 16:41152024.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Paller CJ, Zahurak ML, Mandl A, Metri NA,
Lalji A, Heath E, Kelly WK, Hoimes C, Barata P, Taksey J, et al:
High-dose intravenous vitamin C combined with docetaxel in men with
metastatic castration-resistant prostate cancer: A randomized
placebo-controlled phase II trial. Cancer Res Commun. 4:2174–2182.
2024. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Gillberg L, Ørskov AD, Nasif A, Ohtani H,
Madaj Z, Hansen JW, Rapin N, Mogensen JB, Liu M, Dufva IH, et al:
Oral vitamin C supplementation to patients with myeloid cancer on
azacitidine treatment: Normalization of plasma vitamin C induces
epigenetic changes. Clin Epigenetics. 11:1432019. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
O'Leary BR, Alexander MS, Du J, Moose DL,
Henry MD and Cullen JJ: Pharmacological ascorbate inhibits
pancreatic cancer metastases via a peroxide-mediated mechanism. Sci
Rep. 10:176492020. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Furqan M, Abu-Hejleh T, Stephens LM,
Hartwig SM, Mott SL, Pulliam CF, Petronek M, Henrich JB, Fath MA,
Houtman JC, et al: Pharmacological ascorbate improves the response
to platinum-based chemotherapy in advanced stage non-small cell
lung cancer. Redox Biol. 53:1023182022. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Bodeker KL, Smith BJ, Berg DJ,
Chandrasekharan C, Sharif S, Fei N, Vollstedt S, Brown H, Chandler
M, Lorack A, et al: A randomized trial of pharmacological
ascorbate, gemcitabine, and nab-paclitaxel for metastatic
pancreatic cancer. Redox Biol. 77:1033752024. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Su X, Shen Z, Yang Q, Sui F, Pu J, Ma J,
Ma S, Yao D, Ji M and Hou P: Vitamin C kills thyroid cancer cells
through ROS-dependent inhibition of MAPK/ERK and PI3K/AKT pathways
via distinct mechanisms. Theranostics. 9:4461–4473. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Zhou J, Chen C, Chen X, Fei Y, Jiang L and
Wang G: Vitamin C promotes apoptosis and cell cycle arrest in oral
squamous cell carcinoma. Front Oncol. 10:9762020. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Su X, Li P, Han B, Jia H, Liang Q, Wang H,
Gu M, Cai J, Li S, Zhou Y, et al: Vitamin C sensitizes
BRAFV600E thyroid cancer to PLX4032 via inhibiting the
feedback activation of MAPK/ERK signal by PLX4032. J Exp Clin
Cancer Res. 40:342021. View Article : Google Scholar
|
|
29
|
Zhao X, Liu M, Li C, Liu X, Zhao J, Ma H,
Zhang S and Qu J: High dose vitamin C inhibits PD-L1 by ROS-pSTAT3
signal pathway and enhances T cell function in TNBC. Int
Immunopharmacol. 126:1113212024. View Article : Google Scholar
|
|
30
|
Lv H, Zong Q, Chen C, Lv G, Xiang W, Xing
F, Jiang G, Yan B, Sun X, Ma Y, et al: TET2-mediated tumor cGAS
triggers endothelial STING activation to regulate vasculature
remodeling and anti-tumor immunity in liver cancer. Nat Commun.
15:62024. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Williams DJ, Edwards D, Pun S, Chaliha M,
Burren B, Tinggi U and Sultanbawa Y: Organic acids in Kakadu plum
(Terminalia ferdinandiana): The good (ellagic), the bad (oxalic)
and the uncertain (ascorbic). Food Res Int. 89:237–244. 2016.
View Article : Google Scholar
|
|
32
|
Böttger F, Vallés-Martí A, Cahn L and
Jimenez CR: High-dose intravenous vitamin C, a promising
multi-targeting agent in the treatment of cancer. J Exp Clin Cancer
Res. 40:3432021. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Ngo B, Van Riper JM, Cantley LC and Yun J:
Targeting cancer vulnerabilities with high-dose vitamin C. Nat Rev
Cancer. 19:271–282. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Chang JE, Voorhees PM, Kolesar JM, Ahuja
HG, Sanchez FA, Rodriguez GA, Kim K, Werndli J, Bailey HH and Kahl
BS: Phase II study of arsenic trioxide and ascorbic acid for
relapsed or refractory lymphoid malignancies: A wisconsin oncology
network study. Hematol Oncol. 27:11–16. 2009. View Article : Google Scholar
|
|
35
|
Kawada H, Sawanobori M, Tsuma-Kaneko M,
Wasada I, Miyamoto M, Murayama H, Toyosaki M, Onizuka M, Tsuboi K,
Tazume K, et al: Phase I clinical trial of intravenous l-ascorbic
acid following salvage chemotherapy for relapsed B-cell
non-Hodgkin's lymphoma. Tokai J Exp Clin Med. 39:111–115.
2014.PubMed/NCBI
|
|
36
|
Carr AC and Maggini S: Vitamin C and
immune function. Nutrients. 9:12112017. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Padayatty SJ and Levine M: Vitamin C: The
known and the unknown and goldilocks. Oral Dis. 22:463–493. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Bhoot HR, Zamwar UM, Chakole S and
Anjankar A: Dietary sources, bioavailability, and functions of
ascorbic acid (vitamin C) and its role in the common cold, tissue
healing, and iron metabolism. Cureus. 15:e493082023.PubMed/NCBI
|
|
39
|
Bowry SK: Dialysis membranes today. Int J
Artif Organs. 25:447–460. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Bürzle M, Suzuki Y, Ackermann D, Miyazaki
H, Maeda N, Clémençon B, Burrier R and Hediger MA: The
sodium-dependent ascorbic acid transporter family SLC23. Mol
Aspects Med. 34:436–454. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Lykkesfeldt J and Tveden-Nyborg P: The
pharmacokinetics of vitamin C. Nutrients. 11:24122019. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Doseděl M, Jirkovský E, Macáková K,
Krčmová LK, Javorská L, Pourová J, Mercolini L, Remião F, Nováková
L, Mladěnka P, et al: Vitamin C-sources, physiological role,
kinetics, deficiency, use, toxicity, and determination. Nutrients.
13:6152021. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Hasselholt S, Tveden-Nyborg P and
Lykkesfeldt J: Distribution of vitamin C is tissue specific with
early saturation of the brain and adrenal glands following
differential oral dose regimens in guinea pigs. Br J Nutr.
113:1539–1549. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Mohammed BM, Fisher BJ, Kraskauskas D,
Ward S, Wayne JS, Brophy DF, Fowler AA III, Yager DR and Natarajan
R: Vitamin C promotes wound healing through novel pleiotropic
mechanisms. Int Wound J. 13:572–584. 2016. View Article : Google Scholar
|
|
45
|
Moores J: Vitamin C: A wound healing
perspective. Br J Community Nurs. Suppl:S6S8–S11. 2013. View Article : Google Scholar
|
|
46
|
Fisher BJ, Kraskauskas D, Martin EJ,
Farkas D, Puri P, Massey HD, Idowu MO, Brophy DF, Voelkel NF,
Fowler AA III and Natarajan R: Attenuation of sepsis-induced organ
injury in mice by vitamin C. JPEN J Parenter Enteral Nutr.
38:825–839. 2014. View Article : Google Scholar
|
|
47
|
Carr AC, Shaw GM, Fowler AA and Natarajan
R: Ascorbate-dependent vasopressor synthesis: A rationale for
vitamin C administration in severe sepsis and septic shock? Crit
Care. 19:4182015. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Bozonet SM, Carr AC, Pullar JM and Vissers
MC: Enhanced human neutrophil vitamin C status, chemotaxis and
oxidant generation following dietary supplementation with vitamin
C-rich SunGold kiwifruit. Nutrients. 7:2574–2588. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Hong JM, Kim JH, Kang JS, Lee WJ and Hwang
YI: Vitamin C is taken up by human T cells via sodium-dependent
vitamin C transporter 2 (SVCT2) and exerts inhibitory effects on
the activation of these cells in vitro. Anat Cell Biol. 49:88–98.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Molina N, Morandi AC, Bolin AP and Otton
R: Comparative effect of fucoxanthin and vitamin C on oxidative and
functional parameters of human lymphocytes. Int Immunopharmacol.
22:41–50. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
van Gorkom GNY, Klein Wolterink RGJ, Van
Elssen CHMJ, Wieten L, Germeraad WTV and Bos GMJ: Influence of
vitamin C on lymphocytes: An overview. Antioxidants (Basel).
7:412018. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Zhang X, Zhang Y, Wang C and Wang X: TET
(Ten-eleven translocation) family proteins: Structure, biological
functions and applications. Signal Transduct Target Ther.
8:2972023. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Yue X, Trifari S, Äijö T, Tsagaratou A,
Pastor WA, Zepeda-Martínez JA, Lio CW, Li X, Huang Y, Vijayanand P,
et al: Control of Foxp3 stability through modulation of TET
activity. J Exp Med. 213:377–397. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Warren CFA, Wong-Brown MW and Bowden NA:
BCL-2 family isoforms in apoptosis and cancer. Cell Death Dis.
10:1772019. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Singh R, Letai A and Sarosiek K:
Regulation of apoptosis in health and disease: The balancing act of
BCL-2 family proteins. Nat Rev Mol Cell Biol. 20:175–193. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Deng X, Gao F and May WS Jr: Bcl2 retards
G1/S cell cycle transition by regulating intracellular ROS. Blood.
102:3179–3185. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Güler A, Yardımcı BK and Özek NŞ: Human
anti-apoptotic Bcl-2 and Bcl-xL proteins protect yeast cells from
aging induced oxidative stress. Biochimie. 229:69–83. 2025.
View Article : Google Scholar
|
|
58
|
Yu X, Wang Y, Tan J, Li Y, Yang P, Liu X,
Lai J, Zhang Y, Cai L, Gu Y, et al: Inhibition of NRF2 enhances the
acute myeloid leukemia cell death induced by venetoclax via the
ferroptosis pathway. Cell Death Discov. 10:352024. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Sies H: Oxidative stress: A concept in
redox biology and medicine. Redox Biol. 4:180–183. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Assi M: The differential role of reactive
oxygen species in early and late stages of cancer. Am J Physiol
Regul Integr Comp Physiol. 313:R646–R653. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Hayes JD, Dinkova-Kostova AT and Tew KD:
Oxidative stress in cancer. Cancer Cell. 38:167–197. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Sahoo BM, Banik BK, Borah P and Jain A:
Reactive oxygen species (ROS): Key components in cancer therapies.
Anticancer Agents Med Chem. 22:215–222. 2022. View Article : Google Scholar
|
|
63
|
Ebrahim AS, Sabbagh H, Liddane A, Raufi A,
Kandouz M and Al-Katib A: Hematologic malignancies: Newer
strategies to counter the BCL-2 protein. J Cancer Res Clin Oncol.
142:2013–2022. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Ashkenazi A, Fairbrother WJ, Leverson JD
and Souers AJ: From basic apoptosis discoveries to advanced
selective BCL-2 family inhibitors. Nat Rev Drug Discov. 16:273–284.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Sermer D, Bobillo S, Dogan A, Zhang Y,
Seshan V, Lavery JA, Batlevi C, Caron P, Hamilton A, Hamlin P, et
al: Extra copies of MYC, BCL2, and BCL6 and outcome in patients
with diffuse large B-cell lymphoma. Blood Adv. 4:3382–3390. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Cerón R, Martínez A, Ramos C, De la Cruz
A, García A, Mendoza I, Palmeros G, Montaño Figueroa EH, Navarrete
J, Jiménez-Morales S, et al: Overexpression of BCL2, BCL6, VEGFR1
and TWIST1 in circulating tumor cells derived from patients with
DLBCL decreases event-free survival. Onco Targets Ther.
15:1583–1595. 2022. View Article : Google Scholar
|
|
67
|
Low IC, Kang J and Pervaiz S: Bcl-2: A
prime regulator of mitochondrial redox metabolism in cancer cells.
Antioxid Redox Signal. 15:2975–2987. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Krishna S, Low ICC and Pervaiz S:
Regulation of mitochondrial metabolism: Yet another facet in the
biology of the oncoprotein Bcl-2. Biochem J. 435:545–551. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Eno CO, Zhao G, Olberding KE and Li C: The
Bcl-2 proteins Noxa and Bcl-xL co-ordinately regulate oxidative
stress-induced apoptosis. Biochem J. 444:69–78. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Lagadinou ED, Sach A, Callahan K, Rossi
RM, Neering SJ, Minhajuddin M, Ashton JM, Pei S, Grose V, O'Dwyer
KM, et al: BCL-2 inhibition targets oxidative phosphorylation and
selectively eradicates quiescent human leukemia stem cells. Cell
Stem Cell. 12:329–341. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Lv H, Wang C, Fang T, Li T, Lv G, Han Q,
Yang W and Wang H: Vitamin C preferentially kills cancer stem cells
in hepatocellular carcinoma via SVCT-2. NPJ Precis Oncol. 2:12018.
View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Ghanem A, Melzer AM, Zaal E, Neises L,
Baltissen D, Matar O, Glennemeier-Marke H, Almouhanna F, Theobald
J, Abu El Maaty MA, et al: Ascorbate kills breast cancer cells by
rewiring metabolism via redox imbalance and energy crisis. Free
Radic Biol Med. 163:196–209. 2021. View Article : Google Scholar
|
|
73
|
Chen Q, Espey MG, Krishna MC, Mitchell JB,
Corpe CP, Buettner GR, Shacter E and Levine M: Pharmacologic
ascorbic acid concentrations selectively kill cancer cells: Action
as a pro-drug to deliver hydrogen peroxide to tissues. Proc Natl
Acad Sci USA. 102:13604–13609. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Fan D, Liu X, Shen Z, Wu P, Zhong L and
Lin F: Cell signaling pathways based on vitamin C and their
application in cancer therapy. Biomed Pharmacother. 162:1146952023.
View Article : Google Scholar : PubMed/NCBI
|
|
75
|
El-Garawani IM, El-Nabi SH, El-Shafey S,
Elfiky M and Nafie E: Coffea arabica bean extracts and vitamin C: A
novel combination unleashes MCF-7 cell death. Curr Pharm
Biotechnol. 21:23–36. 2020. View Article : Google Scholar
|
|
76
|
Chen MS, Zhao HK, Cheng YY, Yuan ZH and
Zhang YL: Toxic effects of vitamin C combined with temozolomide on
glioma cells and its mechanism. Zhongguo Ying Yong Sheng Li Xue Za
Zhi. 36:616–621. 2020.In Chinese.
|
|
77
|
Liongue C, Almohaisen F and Ward AC: B
cell lymphoma 6 (BCL6): A conserved regulator of immunity and
beyond. Int J Mol Sci. 25:109682024. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Basso K and Dalla-Favera R: Roles of BCL6
in normal and transformed germinal center B cells. Immunol Rev.
247:172–183. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Phan RT and Dalla-Favera R: The BCL6
proto-oncogene suppresses p53 expression in germinal-centre B
cells. Nature. 432:635–639. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Kerckaert JP, Deweindt C, Tilly H, Quief
S, Lecocq G and Bastard C: LAZ3, a novel zinc-finger encoding gene,
is disrupted by recurring chromosome 3q27 translocations in human
lymphomas. Nat Genet. 5:66–70. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Johnston RJ, Poholek AC, DiToro D, Yusuf
I, Eto D, Barnett B, Dent AL, Craft J and Crotty S: Bcl6 and
Blimp-1 are reciprocal and antagonistic regulators of T follicular
helper cell differentiation. Science. 325:1006–1010. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Zan H, Wu X, Komori A, Holloman WK and
Casali P: AID-dependent generation of resected double-strand DNA
breaks and recruitment of Rad52/Rad51 in somatic hypermutation.
Immunity. 18:727–738. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Liu Y, Feng J, Yuan K, Wu Z, Hu L, Lu Y,
Li K, Guo J, Chen J, Ma C and Pang X: The oncoprotein BCL6 enables
solid tumor cells to evade genotoxic stress. Elife. 11:e692552022.
View Article : Google Scholar : PubMed/NCBI
|
|
84
|
McLachlan T, Matthews WC, Jackson ER,
Staudt DE, Douglas AM, Findlay IJ, Persson ML, Duchatel RJ, Mannan
A, Germon ZP and Dun MD: B-cell lymphoma 6 (BCL6): From master
regulator of humoral immunity to oncogenic driver in pediatric
cancers. Mol Cancer Res. 20:1711–1723. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Louwen F, Kreis NN, Ritter A, Friemel A,
Solbach C and Yuan J: BCL6, a key oncogene, in the placenta,
pre-eclampsia and endometriosis. Hum Reprod Update. 28:890–909.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Leeman-Neill RJ and Bhagat G: BCL6 as a
therapeutic target for lymphoma. Expert Opin Ther Targets.
22:143–152. 2018. View Article : Google Scholar
|
|
87
|
Huang C and Melnick A: Mechanisms of
action of BCL6 during germinal center B cell development. Sci China
Life Sci. 58:1226–1232. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Krull JE, Wenzl K, Hartert KT, Manske MK,
Sarangi V, Maurer MJ, Larson MC, Nowakowski GS, Ansell SM, McPhail
E, et al: Somatic copy number gains in MYC, BCL2, and BCL6
identifies a subset of aggressive alternative-DH/TH DLBCL patients.
Blood Cancer J. 10:1172020. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Ting CY, Chang KM, Kuan JW, Sathar J, Chew
LP, Wong OJ, Yusuf Y, Wong L, Samsudin AT, Pana MNBM, et al:
Clinical significance of BCL2, C-MYC, and BCL6 genetic
abnormalities, epstein-barr virus infection, CD5 protein
expression, germinal center B Cell/non-germinal center B-cell
subtypes, co-expression of MYC/BCL2 proteins and co-expression of
MYC/BCL2/BCL6 proteins in diffuse large B-cell lymphoma: a clinical
and pathological correlation study of 120 patients. Int J Med Sci.
16:556–566. 2019. View Article : Google Scholar :
|
|
90
|
Ferretti GDS, Quarti J, Dos Santos G,
Rangel LP and Silva JL: Anticancer therapeutic strategies targeting
p53 aggregation. Int J Mol Sci. 23:110232022. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Bieging KT, Mello SS and Attardi LD:
Unravelling mechanisms of p53-mediated tumour suppression. Nat Rev
Cancer. 14:359–370. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Williams AB and Schumacher B: p53 in the
DNA-damage-repair process. Cold Spring Harb Perspect Med.
6:a0260702016. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Sermeus A and Michiels C: Reciprocal
influence of the p53 and the hypoxic pathways. Cell Death Dis.
2:e1642011. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Miyata S, Ishii T and Kitanaka S:
Reduction of HIF-1α/PD-L1 by catalytic topoisomerase inhibitor
induces cell death through caspase activation in cancer cells under
hypoxia. Anticancer Res. 44:49–59. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Madan E, Parker TM, Pelham CJ, Palma AM,
Peixoto ML, Nagane M, Chandaria A, Tomás AR, Canas-Marques R,
Henriques V, et al: HIF-transcribed p53 chaperones HIF-1α. Nucleic
Acids Res. 47:10212–10234. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Ismail S, Elshimali Y, Daoud A and
Alshehabi Z: Immunohistochemical expression of transcription
factors PAX5, OCT2, BCL6 and transcription regulator P53 in
Non-Hodgkin lymphomas: A diagnostic cross-sectional study. Ann Med
Surg (Lond). 78:1037862022.PubMed/NCBI
|
|
97
|
Choi SH, Koh DI, Cho SY, Kim MK, Kim KS
and Hur MW: Temporal and differential regulation of
KAISO-controlled transcription by phosphorylated and acetylated p53
highlights a crucial regulatory role of apoptosis. J Biol Chem.
294:12957–12974. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Margalit O, Amram H, Amariglio N, Simon
AJ, Shaklai S, Granot G, Minsky N, Shimoni A, Harmelin A, Givol D,
et al: BCL6 is regulated by p53 through a response element
frequently disrupted in B-cell non-Hodgkin lymphoma. Blood.
107:1599–1607. 2006. View Article : Google Scholar
|
|
99
|
Kaźmierczak-Barańska J, Boguszewska K,
Adamus-Grabicka A and Karwowski BT: Two faces of vitamin
C-antioxidative and pro-oxidative agent. Nutrients. 12:15012020.
View Article : Google Scholar
|
|
100
|
Xiong Y, Xu S, Fu B, Tang W, Zaky MY, Tian
R, Yao R, Zhang S, Zhao Q, Nian W, et al: Vitamin C-induced
competitive binding of HIF-1α and p53 to ubiquitin E3 ligase CBL
contributes to anti-breast cancer progression through p53
deacetylation. Food Chem Toxicol. 168:1133212022. View Article : Google Scholar
|
|
101
|
Kim J, Lee SD, Chang B, Jin DH, Jung SI,
Park MY, Han Y, Yang Y, Il Kim K, Lim JS, et al: Enhanced antitumor
activity of vitamin C via p53 in cancer cells. Free Radic Biol Med.
53:1607–1615. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Huang K: Chemical inducers of proximity:
Precision tools for apoptosis in transcriptional regulation. Signal
Transduct Target Ther. 9:3642024. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Duffy MJ, O'Grady S, Tang M and Crown J:
MYC as a target for cancer treatment. Cancer Treat Rev.
94:1021542021. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Das SK, Lewis BA and Levens D: MYC: A
complex problem. Trends Cell Biol. 33:235–246. 2023. View Article : Google Scholar :
|
|
105
|
Ellenbroek BD, Kahler JP, Arella D, Lin C,
Jespers W, Züger EA, Drukker M and Pomplun SJ: Development of
DuoMYC: A synthetic cell penetrant miniprotein that efficiently
inhibits the oncogenic transcription factor MYC. Angew Chem Int Ed
Engl. 64:e2024160822025. View Article : Google Scholar :
|
|
106
|
Baluapuri A, Wolf E and Eilers M: Target
gene-independent functions of MYC oncoproteins. Nat Rev Mol Cell
Biol. 21:255–267. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Liu Z, Chen SS, Clarke S, Veschi V and
Thiele CJ: Targeting MYCN in pediatric and adult cancers. Front
Oncol. 10:6236792021. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Massó-Vallés D, Beaulieu ME and Soucek L:
MYC, MYCL, and MYCN as therapeutic targets in lung cancer. Expert
Opin Ther Targets. 24:101–114. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Stoelzle T, Schwarb P, Trumpp A and Hynes
NE: c-Myc affects mRNA translation, cell proliferation and
progenitor cell function in the mammary gland. BMC Biol. 7:632009.
View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Felipe I, Martínez-de-Villarreal J, Patel
K, Martínez-Torrecuadrada J, Grossmann LD, Roncador G, Cubells M,
Farrell A, Kendsersky N, Sabroso-Lasa S, et al: BPTF cooperates
with MYCN and MYC to link neuroblastoma cell cycle control to
epigenetic cellular states. bioRxiv [Preprint]: 2024.02.11.579816.
2024.
|
|
111
|
Mahdavi P, Panahipoor Javaherdehi A,
Khanjanpoor P, Aminian H, Zakeri M, Zafarani A and Razizadeh MH:
The role of c-Myc in Epstein-Barr virus-associated cancers:
Mechanistic insights and therapeutic implications. Microb Pathog.
197:1070252024. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Yoon J, Jeon T, Kwon JA and Yoon SY:
Characterization of MYC rearrangements in multiple myeloma: An
optical genome mapping approach. Blood Cancer J. 14:1652024.
View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Jakobsen ST and Siersbæk R:
Transcriptional regulation by MYC: An emerging new model. Oncogene.
44:1–7. 2025. View Article : Google Scholar
|
|
114
|
Bisso A, Filipuzzi M, Gamarra Figueroa GP,
Brumana G, Biagioni F, Doni M, Ceccotti G, Tanaskovic N, Morelli
MJ, Pendino V, et al: Cooperation between MYC and β-catenin in
liver tumorigenesis requires Yap/Taz. Hepatology. 72:1430–1443.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Dhanasekaran R, Deutzmann A,
Mahauad-Fernandez WD, Hansen AS, Gouw AM and Felsher DW: The MYC
oncogene-the grand orchestrator of cancer growth and immune
evasion. Nat Rev Clin Oncol. 19:23–36. 2022. View Article : Google Scholar
|
|
116
|
Baena E, Ortiz M, Martínez-A C and de
Alborán IM: c-Myc is essential for hematopoietic stem cell
differentiation and regulates Lin(-)Sca-1(+)c-Kit(-) cell
generation through p21. Exp Hematol. 35:1333–1343. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Sewastianik T, Prochorec-Sobieszek M,
Chapuy B and Juszczyński P: MYC deregulation in lymphoid tumors:
Molecular mechanisms, clinical consequences and therapeutic
implications. Biochim Biophys Acta. 1846:457–467. 2014.PubMed/NCBI
|
|
118
|
Susanibar-Adaniya S and Barta SK: 2021
Update on diffuse large B cell lymphoma: A review of current data
and potential applications on risk stratification and management.
Am J Hematol. 96:617–629. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Candelaria M, Cerrato-Izaguirre D,
Gutierrez O, Diaz-Chavez J, Aviles A, Dueñas-Gonzalez A and Malpica
L: Characterizing the mutational landscape of diffuse large B-cell
lymphoma in a prospective cohort of mexican patients. Int J Mol
Sci. 25:93282024. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Hashmi AA, Iftikhar SN, Nargus G, Ahmed O,
Asghar IA, Shirazi UA, Afzal A, Irfan M and Ali J: Double-expressor
phenotype (BCL-2/c-MYC co-expression) of diffuse large B-cell
lymphoma and its clinicopathological correlation. Cureus.
13:e131552021.PubMed/NCBI
|
|
121
|
Wu G, Liu T, Li H, Li Y, Li D and Li W:
c-MYC and reactive oxygen species play roles in tetrandrine-induced
leukemia differentiation. Cell Death Dis. 9:4732018. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Koo JI, Sim DY, Lee HJ, Ahn CH, Park J,
Park SY, Lee D, Shim BS, Kim B and Kim SH: Apoptotic and
anti-Warburg effect of Morusin via ROS mediated inhibition of
FOXM1/c-Myc signaling in prostate cancer cells. Phytother Res.
37:4473–4487. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Meng L, Gao J, Mo W, Wang B, Shen H, Cao
W, Ding M, Diao W, Chen W, Zhang Q, et al: MIOX inhibits autophagy
to regulate the ROS-driven inhibition of STAT3/c-Myc-mediated
epithelial-mesenchymal transition in clear cell renal cell
carcinoma. Redox Biol. 68:1029562023. View Article : Google Scholar
|
|
124
|
Yao L, Wu P, Yao F, Huang B, Zhong F and
Wang X: ZCCHC4 regulates esophageal cancer progression and
cisplatin resistance through ROS/c-myc axis. Sci Rep. 15:51492025.
View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Donati G, Nicoli P, Verrecchia A,
Vallelonga V, Croci O, Rodighiero S, Audano M, Cassina L, Ghsein A,
Binelli G, et al: Oxidative stress enhances the therapeutic action
of a respiratory inhibitor in MYC-driven lymphoma. EMBO Mol Med.
15:e169102023. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Firouzjaei AA and Mohammadi-Yeganeh S: The
intricate interplay between ferroptosis and efferocytosis in
cancer: Unraveling novel insights and therapeutic opportunities.
Front Oncol. 14:14242182024. View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Ahn M, Ali A and Seo JH: Mitochondrial
regulation in the tumor microenvironment: Targeting mitochondria
for immunotherapy. Front Immunol. 15:14538862024. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Shen M and Kang Y: Complex interplay
between tumor microenvironment and cancer therapy. Front Med.
12:426–439. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Manea AJ and Ray SK: Advanced
bioinformatics analysis and genetic technologies for targeting
autophagy in glioblastoma multiforme. Cells. 12:8972023. View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Pitt JM, Marabelle A, Eggermont A, Soria
JC, Kroemer G and Zitvogel L: Targeting the tumor microenvironment:
Removing obstruction to anticancer immune responses and
immunotherapy. Ann Oncol. 27:1482–1492. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Tong X, Tang R, Xiao M, Xu J, Wang W,
Zhang B, Liu J, Yu X and Shi S: Targeting cell death pathways for
cancer therapy: Recent developments in necroptosis, pyroptosis,
ferroptosis, and cuproptosis research. J Hematol Oncol. 15:1742022.
View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Babar Q, Saeed A, Tabish TA, Sarwar M and
Thorat ND: Targeting the tumor microenvironment: Potential strategy
for cancer therapeutics. Biochim Biophys Acta Mol Basis Dis.
1869:1667462023. View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Worbs T, Hammerschmidt SI and Förster R:
Dendritic cell migration in health and disease. Nat Rev Immunol.
17:30–48. 2017. View Article : Google Scholar
|
|
134
|
Wculek SK, Cueto FJ, Mujal AM, Melero I,
Krummel MF and Sancho D: Dendritic cells in cancer immunology and
immunotherapy. Nat Rev Immunol. 20:7–24. 2020. View Article : Google Scholar
|
|
135
|
Gardner A and Ruffell B: Dendritic cells
and cancer immunity. Trends Immunol. 37:855–865. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Noubade R, Majri-Morrison S and Tarbell
KV: Beyond cDC1: Emerging roles of DC crosstalk in cancer immunity.
Front Immunol. 10:10142019. View Article : Google Scholar : PubMed/NCBI
|
|
137
|
Böttcher JP and Reis e Sousa C: The role
of type 1 conventional dendritic cells in cancer immunity. Trends
Cancer. 4:784–792. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Wculek SK, Amores-Iniesta J, Conde-Garrosa
R, Khouili SC, Melero I and Sancho D: Effective cancer
immunotherapy by natural mouse conventional type-1 dendritic cells
bearing dead tumor antigen. J Immunother Cancer. 7:1002019.
View Article : Google Scholar : PubMed/NCBI
|
|
139
|
Binnewies M, Mujal AM, Pollack JL, Combes
AJ, Hardison EA, Barry KC, Tsui J, Ruhland MK, Kersten K,
Abushawish MA, et al: Unleashing type-2 dendritic cells to drive
protective antitumor CD4+ T cell immunity. Cell.
177:556–571.e16. 2019. View Article : Google Scholar
|
|
140
|
Ruhland MK, Roberts EW, Cai E, Mujal AM,
Marchuk K, Beppler C, Nam D, Serwas NK, Binnewies M and Krummel MF:
Visualizing synaptic transfer of tumor antigens among dendritic
cells. Cancer Cell. 37:786–799.e5. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
141
|
Holicek P, Guilbaud E, Klapp V, Truxova I,
Spisek R, Galluzzi L and Fucikova J: Type I interferon and cancer.
Immunol Rev. 321:115–127. 2024. View Article : Google Scholar
|
|
142
|
Chrisikos TT, Zhou Y, Slone N, Babcock R,
Watowich SS and Li HS: Molecular regulation of dendritic cell
development and function in homeostasis, inflammation, and cancer.
Mol Immunol. 110:24–39. 2019. View Article : Google Scholar
|
|
143
|
Veglia F and Gabrilovich DI: Dendritic
cells in cancer: The role revisited. Curr Opin Immunol. 45:43–51.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
144
|
Han SH and Ju MH: Characterizing the tumor
microenvironment and its correlation with cDC1-related gene
expression in gastric cancer. J Immunol Res. 2024:44681452024.
View Article : Google Scholar : PubMed/NCBI
|
|
145
|
Kießler M, Plesca I, Sommer U, Wehner R,
Wilczkowski F, Müller L, Tunger A, Lai X, Rentsch A, Peuker K, et
al: Tumor-infiltrating plasmacytoid dendritic cells are associated
with survival in human colon cancer. J Immunother Cancer.
9:e0018132021. View Article : Google Scholar
|
|
146
|
Aspord C, Leccia MT, Charles J and Plumas
J: Melanoma hijacks plasmacytoid dendritic cells to promote its own
progression. Oncoimmunology. 3:e274022014. View Article : Google Scholar : PubMed/NCBI
|
|
147
|
De Sá Fernandes C, Novoszel P, Gastaldi T,
Krauß D, Lang M, Rica R, Kutschat AP, Holcmann M, Ellmeier W,
Seruggia D, et al: The histone deacetylase HDAC1 controls dendritic
cell development and anti-tumor immunity. Cell Rep. 43:1143082024.
View Article : Google Scholar : PubMed/NCBI
|
|
148
|
Verneau J, Sautés-Fridman C and Sun CM:
Dendritic cells in the tumor microenvironment: Prognostic and
theranostic impact. Semin Immunol. 48:1014102020. View Article : Google Scholar : PubMed/NCBI
|
|
149
|
Ennishi D: The biology of the tumor
microenvironment in DLBCL: Targeting the 'don't eat me' signal. J
Clin Exp Hematop. 61:210–215. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
150
|
Jeong YJ, Kim JH, Hong JM, Kang JS, Kim
HR, Lee WJ and Hwang YI: Vitamin C treatment of mouse bone
marrow-derived dendritic cells enhanced CD8(+) memory T cell
production capacity of these cells in vivo. Immunobiology.
219:554–564. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
151
|
Kim HW, Cho SI, Bae S, Kim H, Kim Y, Hwang
YI, Kang JS and Lee WJ: Vitamin C up-regulates expression of CD80,
CD86 and MHC class II on dendritic cell line, DC-1 via the
activation of p38 MAPK. Immune Netw. 12:277–283. 2012. View Article : Google Scholar
|
|
152
|
Morante-Palacios O, Godoy-Tena G,
Calafell-Segura J, Ciudad L, Martínez-Cáceres EM, Sardina JL and
Ballestar E: Vitamin C enhances NF-κB-driven epigenomic
reprogramming and boosts the immunogenic properties of dendritic
cells. Nucleic Acids Res. 50:10981–10994. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
153
|
Magrì A, Germano G, Lorenzato A, Lamba S,
Chilà R, Montone M, Amodio V, Ceruti T, Sassi F, Arena S, et al:
High-dose vitamin C enhances cancer immunotherapy. Sci Transl Med.
12:eaay87072020. View Article : Google Scholar : PubMed/NCBI
|
|
154
|
Chopp L, Redmond C, O'Shea JJ and Schwartz
DM: From thymus to tissues and tumors: A review of T-cell biology.
J Allergy Clin Immunol. 151:81–97. 2023. View Article : Google Scholar
|
|
155
|
Lawrence T: The nuclear factor NF-kappaB
pathway in inflammation. Cold Spring Harb Perspect Biol.
1:a0016512009. View Article : Google Scholar
|
|
156
|
Kina E, Larouche JD, Thibault P and
Perreault C: The cryptic immunopeptidome in health and disease.
Trends Genet. 41:162–169. 2025. View Article : Google Scholar
|
|
157
|
Zhao Y, Shao Q and Peng G: Exhaustion and
senescence: Two crucial dysfunctional states of T cells in the
tumor microenvironment. Cell Mol Immunol. 17:27–35. 2020.
View Article : Google Scholar :
|
|
158
|
Knez J, Kovačič B and Goropevšek A: The
role of regulatory T-cells in the development of endometriosis. Hum
Reprod. deae1032024.Epub ahead of print. PubMed/NCBI
|
|
159
|
Sawant DV, Yano H, Chikina M, Zhang Q,
Liao M, Liu C, Callahan DJ, Sun Z, Sun T, Tabib T, et al: Adaptive
plasticity of IL-10+ and IL-35+
Treg cells cooperatively promotes tumor T cell
exhaustion. Nat Immunol. 20:724–735. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
160
|
Yi M, Niu M, Wu Y, Ge H, Jiao D, Zhu S,
Zhang J, Yan Y, Zhou P, Chu Q and Wu K: Combination of oral STING
agonist MSA-2 and anti-TGF-β/PD-L1 bispecific antibody YM101: A
novel immune cocktail therapy for non-inflamed tumors. J Hematol
Oncol. 15:1422022. View Article : Google Scholar
|
|
161
|
Naulaerts S, Datsi A, Borras DM, Antoranz
Martinez A, Messiaen J, Vanmeerbeek I, Sprooten J, Laureano RS,
Govaerts J, Panovska D, et al: Multiomics and spatial mapping
characterizes human CD8+ T cell states in cancer. Sci
Transl Med. 15:eadd10162023. View Article : Google Scholar
|
|
162
|
Li S, Li K, Wang K, Yu H, Wang X, Shi M,
Liang Z, Yang Z, Hu Y, Li Y, et al: Low-dose radiotherapy combined
with dual PD-L1 and VEGFA blockade elicits antitumor response in
hepatocellular carcinoma mediated by activated intratumoral
CD8+ exhausted-like T cells. Nat Commun. 14:77092023.
View Article : Google Scholar
|
|
163
|
Opinto G, Vegliante MC, Negri A, Skrypets
T, Loseto G, Pileri SA, Guarini A and Ciavarella S: The tumor
microenvironment of DLBCL in the computational era. Front Oncol.
10:3512020. View Article : Google Scholar : PubMed/NCBI
|
|
164
|
Thommen DS, Koelzer VH, Herzig P, Roller
A, Trefny M, Dimeloe S, Kiialainen A, Hanhart J, Schill C, Hess C,
et al: A transcriptionally and functionally distinct
PD-1+ CD8+ T cell pool with predictive
potential in non-small-cell lung cancer treated with PD-1 blockade.
Nat Med. 24:994–1004. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
165
|
van der Leun AM, Thommen DS and Schumacher
TN: CD8+ T cell states in human cancer: Insights from
single-cell analysis. Nat Rev Cancer. 20:218–232. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
166
|
Dolina JS, Van Braeckel-Budimir N, Thomas
GD and Salek-Ardakani S: CD8+ T cell exhaustion in
cancer. Front Immunol. 12:7152342021. View Article : Google Scholar
|
|
167
|
Baitsch L, Fuertes-Marraco SA, Legat A,
Meyer C and Speiser DE: The three main stumbling blocks for
anticancer T cells. Trends Immunol. 33:364–372. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
168
|
Thinyakul C, Sakamoto Y, Shimoda M, Liu Y,
Thongchot S, Reda O, Nita A, Sakamula R, Sampattavanich S, Maeda A,
et al: Hippo pathway in cancer cells induces
NCAM1+αSMA+ fibroblasts to modulate tumor
microenvironment. Commun Biol. 7:13432024. View Article : Google Scholar
|
|
169
|
Sarhan D, Hippen KL, Lemire A, Hying S,
Luo X, Lenvik T, Curtsinger J, Davis Z, Zhang B, Cooley S, et al:
Adaptive NK cells resist regulatory T-cell suppression driven by
IL37. Cancer Immunol Res. 6:766–775. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
170
|
Li L, Nong J, Li J, Fang L, Pan M, Qiu H,
Huang S, Li Y, Wei M and Yin H: Dendrobine suppresses tumor growth
by regulating the PD-1/PD-L1 checkpoint pathway in lung cancer.
Curr Cancer Drug Targets. Sep 18–2024.Epub ahead of print.
View Article : Google Scholar
|
|
171
|
Tang Q, Chen Y, Li X, Long S, Shi Y, Yu Y,
Wu W, Han L and Wang S: The role of PD-1/PD-L1 and application of
immune-checkpoint inhibitors in human cancers. Front Immunol.
13:9644422022. View Article : Google Scholar : PubMed/NCBI
|
|
172
|
Ma J, Pang X, Li J, Zhang W and Cui W: The
immune checkpoint expression in the tumor immune microenvironment
of DLBCL: Clinicopathologic features and prognosis. Front Oncol.
12:10693782022. View Article : Google Scholar : PubMed/NCBI
|
|
173
|
Roussel M, Le KS, Granier C, Llamas
Gutierrez F, Foucher E, Le Gallou S, Pangault C, Xerri L, Launay V,
Lamy T, et al: Functional characterization of PD1+TIM3+
tumor-infiltrating T cells in DLBCL and effects of PD1 or TIM3
blockade. Blood Adv. 5:1816–1829. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
174
|
Forde PM, Spicer J, Lu S, Provencio M,
Mitsudomi T, Awad MM, Felip E, Broderick SR, Brahmer JR, Swanson
SJ, et al: Neoadjuvant nivolumab plus chemotherapy in resectable
lung cancer. N Engl J Med. 386:1973–1985. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
175
|
Sheikh S and Kuruvilla J: Pembrolizumab
for the treatment of diffuse large B-cell lymphoma. Expert Opin
Biol Ther. 19:1119–1126. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
176
|
Luchtel RA, Bhagat T, Pradhan K, Jacobs WR
Jr, Levine M, Verma A and Shenoy N: High-dose ascorbic acid
synergizes with anti-PD1 in a lymphoma mouse model. Proc Natl Acad
Sci USA. 117:1666–1677. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
177
|
Bedhiafi T, Inchakalody VP, Fernandes Q,
Mestiri S, Billa N, Uddin S, Merhi M and Dermime S: The potential
role of vitamin C in empowering cancer immunotherapy. Biomed
Pharmacother. 146:1125532022. View Article : Google Scholar
|
|
178
|
Xu YP, Lv L, Liu Y, Smith MD, Li WC, Tan
XM, Cheng M, Li Z, Bovino M, Aubé J and Xiong Y: Tumor suppressor
TET2 promotes cancer immunity and immunotherapy efficacy. J Clin
Invest. 129:4316–4331. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
179
|
Li H, Li Y, Zhang T, Liu S, Song C, Wang
K, Yan W, Wang Z, Yang Q, Yang X and Wang H: Genome-wide CRISPR
screen reveals specific role of type I interferon signaling pathway
in Newcastle disease virus establishment of persistent infection.
Vet Microbiol. 300:1102882025. View Article : Google Scholar
|
|
180
|
Shapouri-Moghaddam A, Mohammadian S,
Vazini H, Taghadosi M, Esmaeili SA, Mardani F, Seifi B, Mohammadi
A, Afshari JT and Sahebkar A: Macrophage plasticity, polarization,
and function in health and disease. J Cell Physiol. 233:6425–6440.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
181
|
Perry CJ, Muñoz-Rojas AR, Meeth KM,
Kellman LN, Amezquita RA, Thakral D, Du VY, Wang JX, Damsky W,
Kuhlmann AL, et al: Myeloid-targeted immunotherapies act in synergy
to induce inflammation and antitumor immunity. J Exp Med.
215:877–893. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
182
|
Ngambenjawong C, Gustafson HH and Pun SH:
Progress in tumor-associated macrophage (TAM)-targeted
therapeutics. Adv Drug Deliv Rev. 114:206–221. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
183
|
Afra F, Eftekhar SP, Farid AS and Ala M:
Non-coding RNAs in cancer immunotherapy: A solution to overcome
immune resistance. Prog Mol Biol Transl Sci. 209:215–240. 2024.
View Article : Google Scholar
|
|
184
|
Zhu W, Liu L, Wu J, Gao R, Fu L, Yang X,
Zou Y, Zhang S and Luo D: SMYD3 activates the TCA cycle to promote
M1-M2 conversion in macrophages. Int Immunopharmacol.
127:1113292024. View Article : Google Scholar
|
|
185
|
Fang C, Zhong R, Lu S, Yu G, Liu Z, Yan C,
Gao J, Tang Y, Wang Y, Zhao Q and Feng X: TREM2 promotes macrophage
polarization from M1 to M2 and suppresses osteoarthritis through
the NF-κB/CXCL3 axis. Int J Biol Sci. 20:1992–2007. 2024.
View Article : Google Scholar :
|
|
186
|
Basak U, Sarkar T, Mukherjee S,
Chakraborty S, Dutta A, Dutta S, Nayak D, Kaushik S, Das T and Sa
G: Tumor-associated macrophages: an effective player of the tumor
microenvironment. Front Immunol. 14:12952572023. View Article : Google Scholar : PubMed/NCBI
|
|
187
|
Daetwyler E, Wallrabenstein T, König D,
Cappelli LC, Naidoo J, Zippelius A and Läubli H:
Corticosteroid-resistant immune-related adverse events: A
systematic review. J Immunother Cancer. 12:e0074092024. View Article : Google Scholar : PubMed/NCBI
|
|
188
|
Ma Z, Yang M, Foda MF, Zhang K, Li S,
Liang H, Zhao Y and Han H: Polarization of tumor-associated
macrophages promoted by vitamin C-loaded liposomes for cancer
immunotherapy. ACS Nano. 16:17389–17401. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
189
|
Xu Y, Guo X, Wang G and Zhou C: Vitamin C
inhibits metastasis of peritoneal tumors by preventing spheroid
formation in ID8 murine epithelial peritoneal cancer model. Front
Pharmacol. 11:6452020. View Article : Google Scholar : PubMed/NCBI
|
|
190
|
Yao H, Xu J, Wang J, Zheng N, Yue J, Mi J,
Zheng L, Dai B, Huang W, Yung S, et al: Combination of magnesium
ions and vitamin C alleviates synovitis and osteophyte formation in
osteoarthritis of mice. Bioact Mater. 6:1341–1352. 2020.PubMed/NCBI
|
|
191
|
Najjar YG and Finke JH: Clinical
perspectives on targeting of myeloid derived suppressor cells in
the treatment of cancer. Front Oncol. 3:492013. View Article : Google Scholar : PubMed/NCBI
|
|
192
|
Hashimoto A, Sarker D, Reebye V, Jarvis S,
Sodergren MH, Kossenkov A, Sanseviero E, Raulf N, Vasara J,
Andrikakou P, et al: Upregulation of C/EBPα inhibits suppressive
activity of myeloid cells and potentiates antitumor response in
mice and patients with cancer. Clin Cancer Res. 27:5961–5978. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
193
|
Holtzhausen A, Harris W, Ubil E, Hunter
DM, Zhao J, Zhang Y, Zhang D, Liu Q, Wang X, Graham DK, et al: TAM
family receptor kinase inhibition reverses MDSC-mediated
suppression and augments anti-PD-1 therapy in melanoma. Cancer
Immunol Res. 7:1672–1686. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
194
|
Azzaoui I, Uhel F, Rossille D, Pangault C,
Dulong J, Le Priol J, Lamy T, Houot R, Le Gouill S, Cartron G, et
al: T-cell defect in diffuse large B-cell lymphomas involves
expansion of myeloid-derived suppressor cells. Blood.
128:1081–1092. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
195
|
Sadeghi M, Dehnavi S, Sharifat M, Amiri AM
and Khodadadi A: Innate immune cells: Key players of orchestra in
modulating tumor microenvironment (TME). Heliyon. 10:e274802024.
View Article : Google Scholar : PubMed/NCBI
|
|
196
|
Johnson B: Targeting myeloid-derived
suppressor cell trafficking as a novel immunotherapeutic approach
in microsatellite stable colorectal cancer. Cancers (Basel).
15:54842023. View Article : Google Scholar : PubMed/NCBI
|
|
197
|
Wu Y, Yi M, Niu M, Mei Q and Wu K:
Myeloid-derived suppressor cells: An emerging target for anticancer
immunotherapy. Mol Cancer. 21:1842022. View Article : Google Scholar : PubMed/NCBI
|
|
198
|
Dhar S, Chakravarti M, Ganguly N, Saha A,
Dasgupta S, Bera S, Sarkar A, Roy K, Das J, Bhuniya A, et al: High
monocytic MDSC signature predicts multi-drug resistance and cancer
relapse in non-Hodgkin lymphoma patients treated with R-CHOP. Front
Immunol. 14:13039592024. View Article : Google Scholar : PubMed/NCBI
|
|
199
|
Wu C, Wu X, Liu X, Yang P, Xu J, Chai Y,
Guo Q, Wang Z and Zhang L: Prognostic significance of monocytes and
monocytic myeloid-derived suppressor cells in diffuse large B-cell
lymphoma treated with R-CHOP. Cell Physiol Biochem. 39:521–530.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
200
|
Ali Y, Monini C, Russeil E, Létang JM,
Testa E, Maigne L and Beuve M: Estimate of the biological dose in
hadrontherapy using GATE. Cancers (Basel). 14:16672022. View Article : Google Scholar : PubMed/NCBI
|
|
201
|
Adibi A, Tokat ÜM, Özgü E, Aydın E,
Demiray İ and Demiray M: PARP inhibitor combinations with high-dose
vitamin C in the treatment of Ewing sarcoma: Two case reports and
mechanistic overview. Ther Adv Med Oncol. 15:175883592312138412023.
View Article : Google Scholar : PubMed/NCBI
|
|
202
|
Wang F, He MM, Xiao J, Zhang YQ, Yuan XL,
Fang WJ, Zhang Y, Wang W, Hu XH, Ma ZG, et al: A randomized,
open-label, multicenter, phase 3 study of high-dose vitamin c plus
FOLFOX ± bevacizumab versus FOLFOX ± bevacizumab in unresectable
untreated metastatic colorectal cancer (VITALITY study). Clin
Cancer Res. 28:4232–4239. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
203
|
Zasowska-Nowak A, Nowak PJ and
Ciałkowska-Rysz A: High-dose vitamin C in advanced-stage cancer
patients. Nutrients. 13:7352021. View Article : Google Scholar : PubMed/NCBI
|
|
204
|
Polireddy K, Dong R, Reed G, Yu J, Chen P,
Williamson S, Violet PC, Pessetto Z, Godwin AK, Fan F, et al: High
dose parenteral ascorbate inhibited pancreatic cancer growth and
metastasis: Mechanisms and a phase I/IIa study. Sci Rep.
7:171882017. View Article : Google Scholar : PubMed/NCBI
|
|
205
|
Wang L and Lou X: A predictive model for
gastric cancer-specific death after gastrectomy: A competing-risk
nomogram. Iran J Public Health. 53:2350–2361. 2024.PubMed/NCBI
|
|
206
|
Chen P, Reed G, Jiang J, Wang Y, Sunega J,
Dong R, Ma Y, Esparham A, Ferrell R, Levine M, et al:
Pharmacokinetic evaluation of intravenous vitamin C: A classic
pharmacokinetic study. Clin Pharmacokinet. 61:1237–1249. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
207
|
Linowiecka K, Foksinski M and Brożyna AA:
Vitamin C transporters and their implications in carcinogenesis.
Nutrients. 12:38692020. View Article : Google Scholar : PubMed/NCBI
|
|
208
|
Cheng YQ, Wang SB, Liu JH, Jin L, Liu Y,
Li CY, Su YR, Liu YR, Sang X, Wan Q, et al: Modifying the tumour
microenvironment and reverting tumour cells: New strategies for
treating malignant tumours. Cell Prolif. 53:e128652020. View Article : Google Scholar : PubMed/NCBI
|
|
209
|
Praditi C, Bozonet SM, Dachs GU and
Vissers M: Ascorbate uptake and retention by breast cancer cell
lines and the intracellular distribution of sodium-dependent
vitamin C transporter 2. Antioxidants (Basel). 12:19292023.
View Article : Google Scholar : PubMed/NCBI
|