|
1
|
Bray F, Laversanne M, Sung H, Ferlay J,
Siegel RL, Soerjomataram I and Jemal A: Global cancer statistics
2022: GLOBOCAN estimates of incidence and mortality worldwide for
36 cancers in 185 countries. CA Cancer J Clin. 74:229–263. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Wang X, Zhang H and Chen X: Drug
resistance and combating drug resistance in cancer. Cancer Drug
Resist. 2:141–160. 2019.PubMed/NCBI
|
|
3
|
Dong D, Yu X, Xu J, Yu N, Liu Z and Sun Y:
Cellular and molecular mechanisms of gastrointestinal cancer liver
metastases and drug resistance. Drug Resist Updat. 77:1011252024.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hussain S, Singh A, Nazir SU, Tulsyan S,
Khan A, Kumar R, Bashir N, Tanwar P and Mehrotra R: Cancer drug
resistance: A fleet to conquer. J Cell Biochem. 120:14213–14225.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Carneiro BA and El-Deiry WS: Targeting
apoptosis in cancer therapy. Nat Rev Clin Oncol. 17:395–417. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Rezayatmand H, Razmkhah M and
Razeghian-Jahromi I: Drug resistance in cancer therapy: The
Pandora's Box of cancer stem cells. Stem Cell Res Ther. 13:1812022.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wang Z, Wang Y, Li Z, Xue W, Hu S and Kong
X: Lipid metabolism as a target for cancer drug resistance:
Progress and prospects. Front Pharmacol. 14:12743352023. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
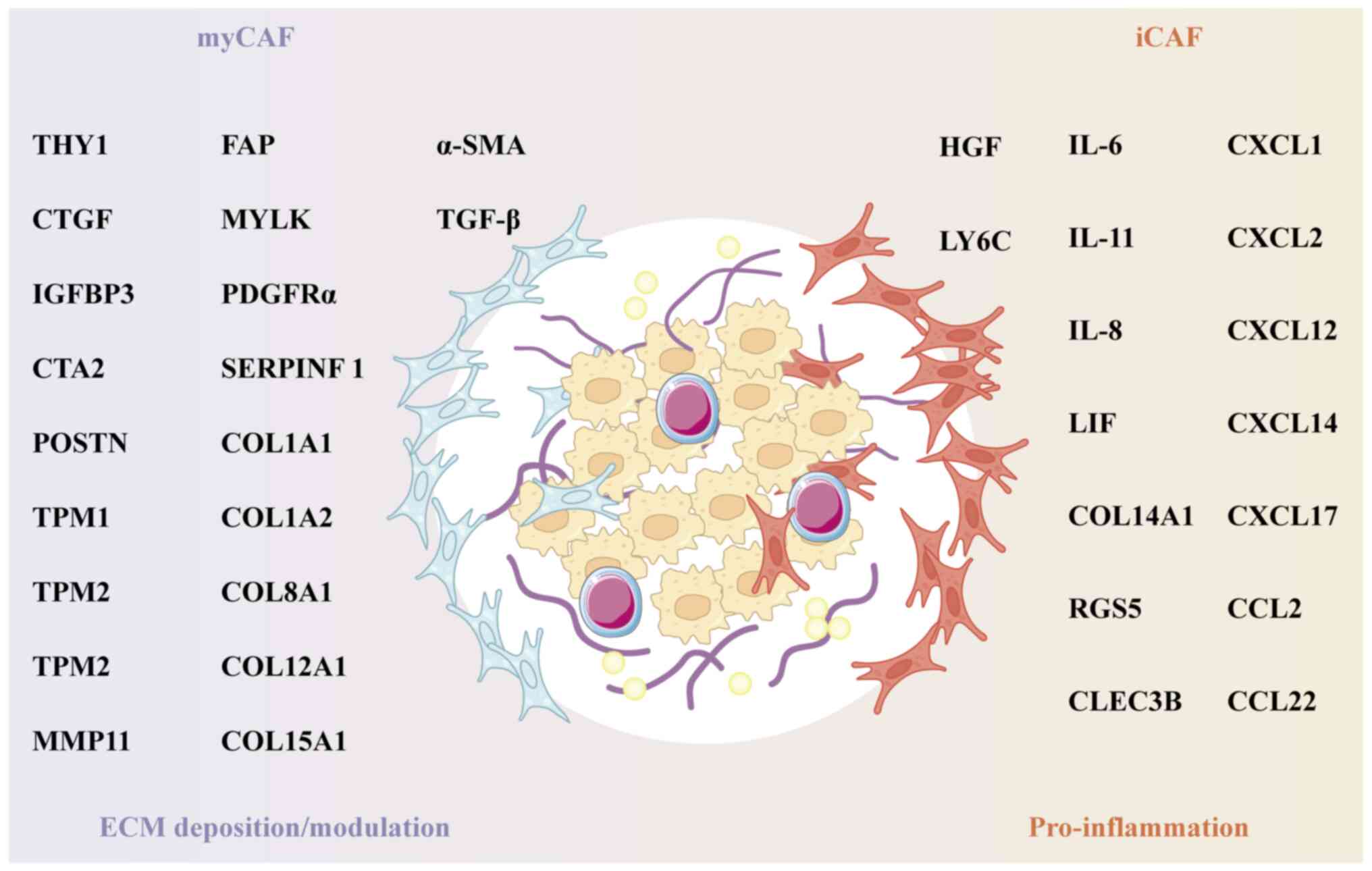
Tong X, Tang R, Xiao M, Xu J, Wang W,
Zhang B, Liu J, Yu X and Shi S: Targeting cell death pathways for
cancer therapy: Recent developments in necroptosis, pyroptosis,
ferroptosis, and cuproptosis research. J Hematol Oncol. 15:1742022.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Gao L, Wu ZX, Assaraf YG, Chen ZS and Wang
L: Overcoming anti-cancer drug resistance via restoration of tumor
suppressor gene function. Drug Resist Updat. 57:1007702021.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Nussinov R, Tsai CJ and Jang H: Anticancer
drug resistance: An update and perspective. Drug Resist Updat.
59:1007962021. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Pitt JM, Marabelle A, Eggermont A, Soria
JC, Kroemer G and Zitvogel L: Targeting the tumor microenvironment:
Removing obstruction to anticancer immune responses and
immunotherapy. Ann Oncol. 27:1482–1492. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kundu M, Butti R, Panda VK, Malhotra D,
Das S, Mitra T, Kapse P, Gosavi SW and Kundu GC: Modulation of the
tumor microenvironment and mechanism of immunotherapy-based drug
resistance in breast cancer. Mol Cancer. 23:922024. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Giraldo NA, Sanchez-Salas R, Peske JD,
Vano Y, Becht E, Petitprez F, Validire P, Ingels A, Cathelineau X,
Fridman WH and Sautès-Fridman C: The clinical role of the TME in
solid cancer. Br J Cancer. 120:45–53. 2019. View Article : Google Scholar :
|
|
14
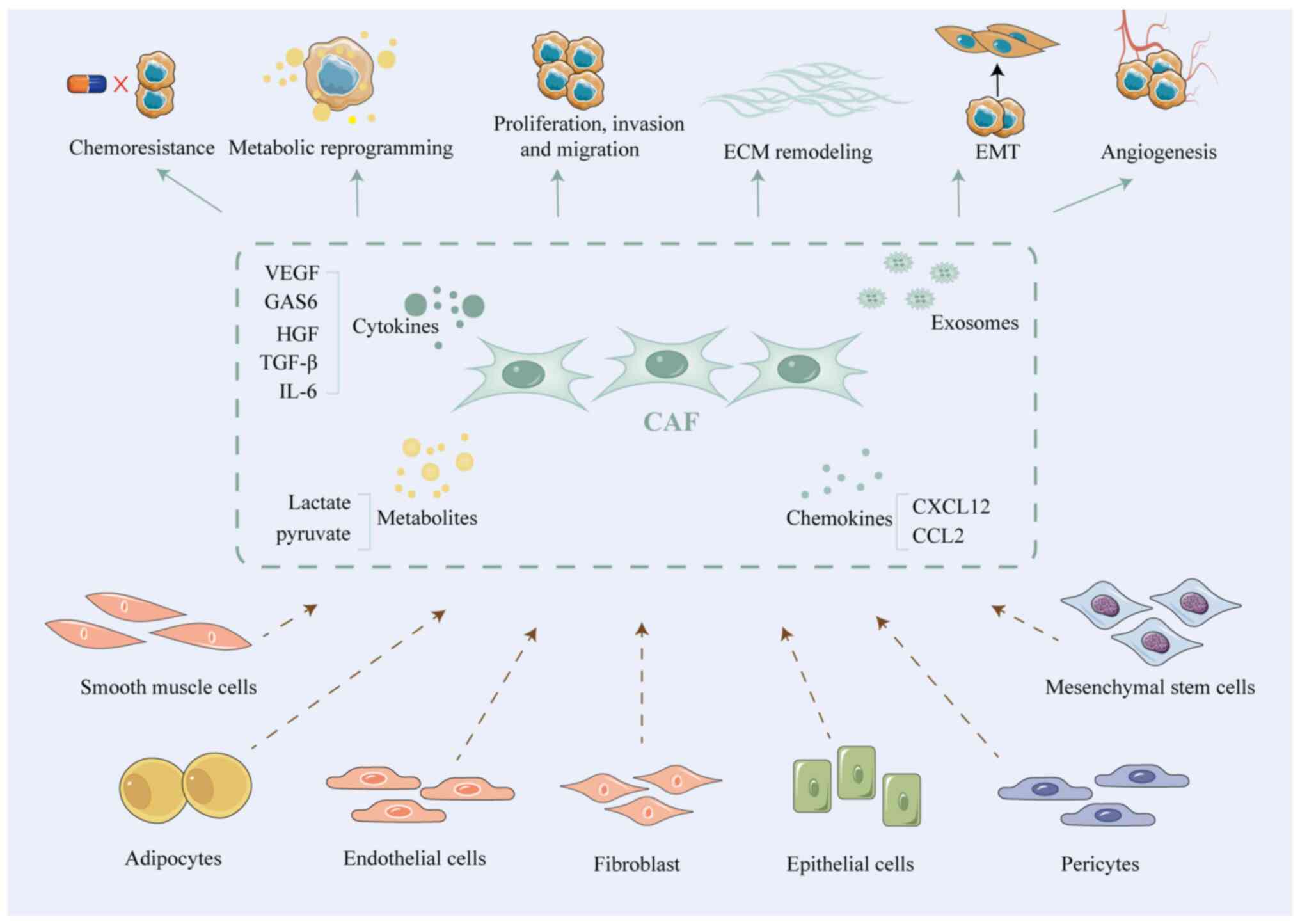
|
Peng Z, Tong Z, Ren Z, Ye M and Hu K:
Cancer-associated fibroblasts and its derived exosomes: A new
perspective for reshaping the tumor microenvironment. Mol Med.
29:662023. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
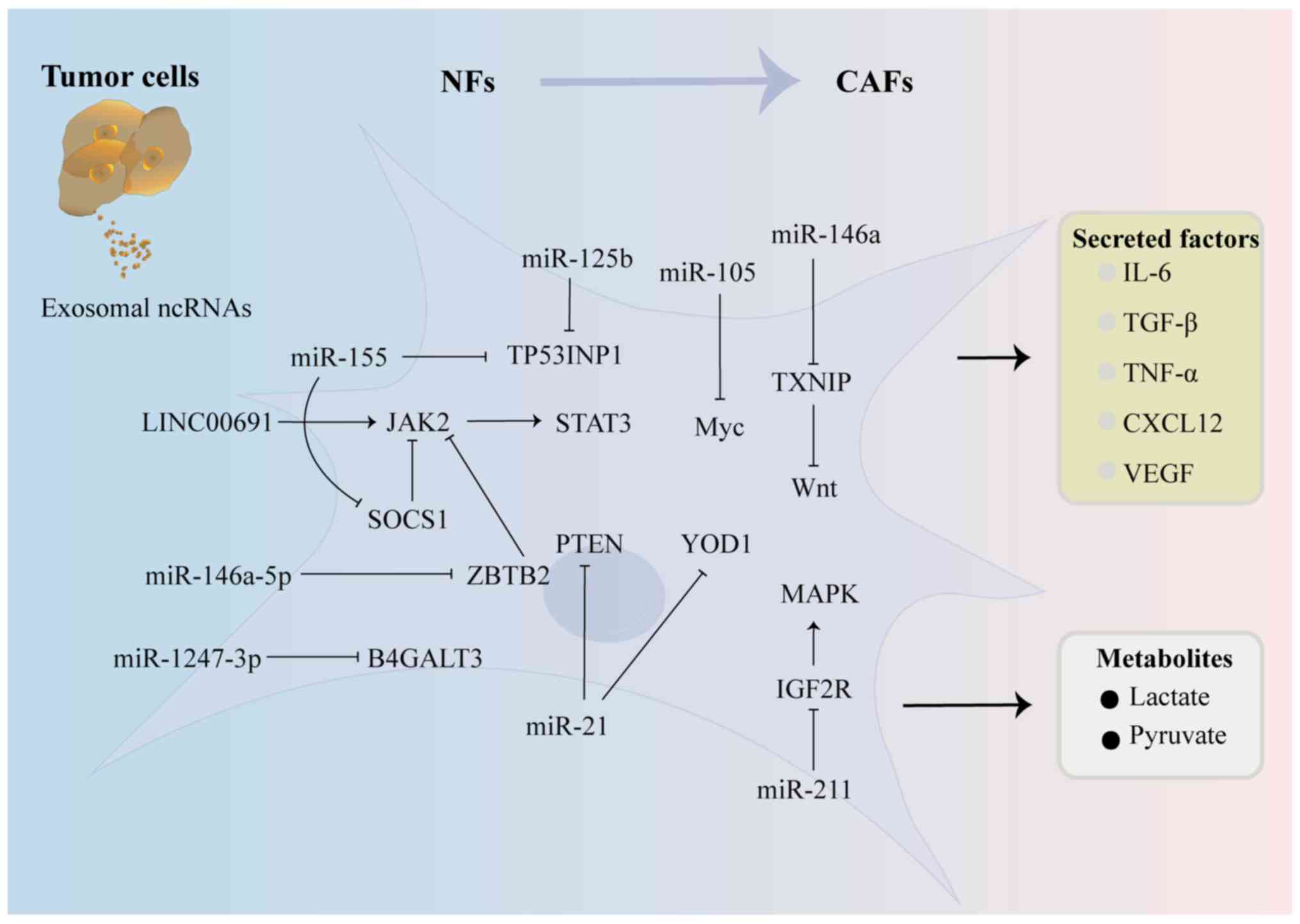
Loh JJ and Ma S: The role of
cancer-associated fibroblast as a dynamic player in mediating
cancer stemness in the tumor microenvironment. Front Cell Dev Biol.
9:7276402021. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Wu F, Yang J, Liu J, Wang Y, Mu J, Zeng Q,
Deng S and Zhou H: Signaling pathways in cancer-associated
fibroblasts and targeted therapy for cancer. Signal Transduct
Target Ther. 6:2182021. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Rimal R, Desai P, Daware R, Hosseinnejad
A, Prakash J, Lammers T and Singh S: Cancer-associated fibroblasts:
Origin, function, imaging, and therapeutic targeting. Adv Drug
Deliv Rev. 189:1145042022. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Mao X, Xu J, Wang W, Liang C, Hua J, Liu
J, Zhang B, Meng Q, Yu X and Shi S: Crosstalk between
cancer-associated fibroblasts and immune cells in the tumor
microenvironment: New findings and future perspectives. Mol Cancer.
20:1312021. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Fiori ME, Di Franco S, Villanova L, Bianca
P, Stassi G and De Maria R: Cancer-associated fibroblasts as
abettors of tumor progression at the crossroads of EMT and therapy
resistance. Mol Cancer. 18:702019. View Article : Google Scholar : PubMed/NCBI
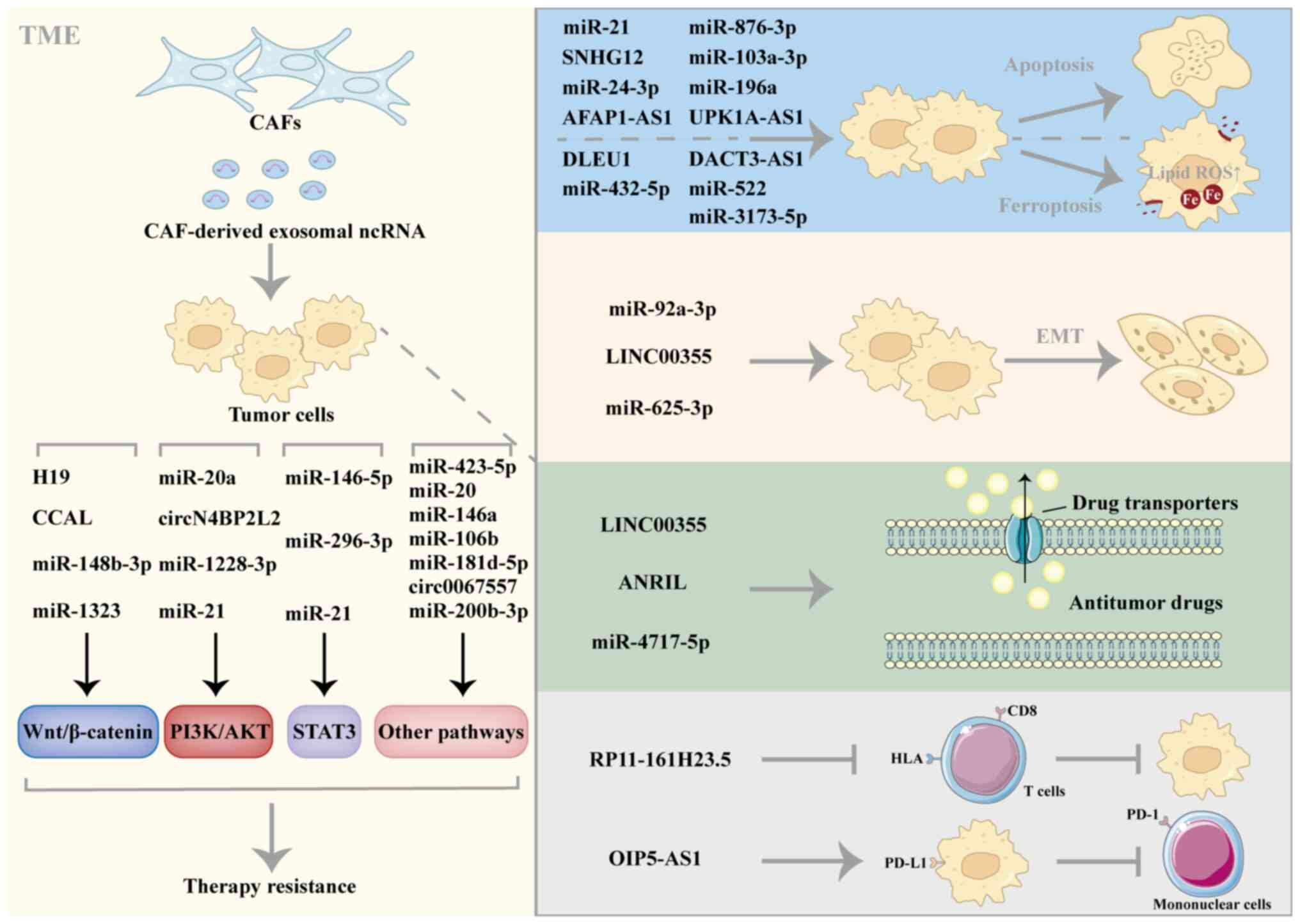
|
|
20
|
Zhang L and Yu D: Exosomes in cancer
development, metastasis, and immunity. Biochim Biophys Acta Rev
Cancer. 1871:455–468. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Li C, Ni YQ, Xu H, Xiang QY, Zhao Y, Zhan
JK, He JY, Li S and Liu YS: Roles and mechanisms of exosomal
non-coding RNAs in human health and diseases. Signal Transduct
Target Ther. 6:3832021. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Nemeth K, Bayraktar R, Ferracin M and
Calin GA: Non-coding RNAs in disease: From mechanisms to
therapeutics. Nat Rev Genet. 25:211–232. 2024. View Article : Google Scholar
|
|
23
|
Hill M and Tran N: miRNA interplay:
Mechanisms and consequences in cancer. Dis Model Mech.
14:dmm0476622021. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Bhan A, Soleimani M and Mandal SS: Long
noncoding RNA and cancer: A new paradigm. Cancer Res. 77:3965–3981.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Liu X, Zhang Y, Zhou S, Dain L, Mei L and
Zhu G: Circular RNA: An emerging frontier in RNA therapeutic
targets, RNA therapeutics, and mRNA vaccines. J Control Release.
348:84–94. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Ibrahim FM, Saleh RO, Uinarni H, Bokov DO,
Menon SV, Zarifovich KB, Misra N, Al-Hamdani MM, Husseen B and
Jawad MA: Exosomal noncoding RNA (ncRNA) in breast cancer
pathogenesis and therapy; two sides of the same coin. Exp Cell Res.
444:1143592025. View Article : Google Scholar
|
|
27
|
Saadh MJ, Allela OQB, Kareem RA, Ballal S,
Chahar M, Saini S, Prasad GVS, Sameer HN, Hamad AK, Athab ZH and
Adil M: The role of exosomal non-coding RNAs in the breast cancer
tumor microenvironment. Funct Integr Genomics. 25:322025.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Alipoor SD and Chang H: Exosomal miRNAs in
the tumor microenvironment of multiple myeloma. Cells. 12:10302023.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Huang Q, Zhong X, Li J, Hu R, Yi J, Sun J,
Xu Y and Zhou X: Exosomal ncRNAs: Multifunctional contributors to
the immunosuppressive tumor microenvironment of hepatocellular
carcinoma. Biomed Pharmacother. 173:1164092024. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Hussen BM, Abdullah ST, Abdullah SR,
Younis YM, Hidayat HJ, Rasul MF and Mohamadtahr S: Exosomal
non-coding RNAs: Blueprint in colorectal cancer metastasis and
therapeutic targets. Noncoding RNA Res. 8:615–632. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Li W, Wang X, Li C, Chen T and Yang Q:
Exosomal non-coding RNAs: Emerging roles in bilateral communication
between cancer cells and macrophages. Mol Ther. 30:1036–1053. 2022.
View Article : Google Scholar :
|
|
32
|
Entezari M, Sadrkhanloo M, Rashidi M,
Asnaf SE, Taheriazam A, Hashemi M, Ashrafizadeh M, Zarrabi A,
Rabiee N, Hushmandi K, et al: Non-coding RNAs and macrophage
interaction in tumor progression. Crit Rev Oncol Hematol.
173:1036802022. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Zhang J, Yu D, Ji C, Wang M, Fu M, Qian Y
and Zhang X, Ji R, Li C, Gu J and Zhang X: Exosomal
miR-4745-5p/3911 from N2-polarized tumor-associated neutrophils
promotes gastric cancer metastasis by regulating SLIT2. Mol Cancer.
23:1982024. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Zhao Y, Jia Y, Wang J, Chen X, Han J, Zhen
S, Yin S, Lv W, Yu F, Wang J, et al: circNOX4 activates an
inflammatory fibroblast niche to promote tumor growth and
metastasis in NSCLC via FAP/IL-6 axis. Mol Cancer. 23:472024.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Golestannejad P, Monkaresi M, Zhian
Zargaran F, Khosravani M, Asgari P, Mobaraki H, Gorjizad M, Hasany
S, Senobari Ghezeljehmeidan A, Hemmati S, et al: Role of cancer
associated fibroblast (CAF) derived miRNAs on head and neck
malignancies microenvironment: A systematic review. BMC Cancer.
25:5822025. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Ye F, Liang Y, Wang Y, Le Yang R, Luo D,
Li Y, Jin Y, Han D, Chen B, Zhao W, et al: Cancer-associated
fibroblasts facilitate breast cancer progression through exosomal
circTBPL1-mediated intercellular communication. Cell Death Dis.
14:4712023. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Shelton M, Anene CA, Nsengimana J, Roberts
W, Newton-Bishop J and Boyne JR: The role of CAF derived exosomal
microRNAs in the tumour microenvironment of melanoma. Biochim
Biophys Acta Rev Cancer. 1875:1884562021. View Article : Google Scholar
|
|
38
|
Sun S, Zhang Y, Li Y and Wei L: Crosstalk
between colorectal cancer cells and cancer-associated fibroblasts
in the tumor microenvironment mediated by exosomal noncoding RNAs.
Front Immunol. 14:11616282023. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Zhao J, Shen J, Mao L, Yang T, Liu J and
Hongbin S: Cancer associated fibroblast secreted miR-432-5p targets
CHAC1 to inhibit ferroptosis and promote acquired chemoresistance
in prostate cancer. Oncogene. 43:2104–2114. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Qi R, Bai Y, Li K, Liu N, Xu Y, Dal E,
Wang Y, Lin R, Wang H, Liu Z, et al: Cancer-associated fibroblasts
suppress ferroptosis and induce gemcitabine resistance in
pancreatic cancer cells by secreting exosome-derived
ACSL4-targeting miRNAs. Drug Resist Updat. 68:1009602023.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Zhuang J, Shen L, Li M, Sun J, Hao J, Li
J, Zhu Z, Ge S, Zhang D, Guo H, et al: Cancer-associated
fibroblast-derived miR-146a-5p generates a niche that promotes
bladder cancer stemness and chemoresistance. Cancer Res.
83:1611–1627. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Sahai E, Astsaturov I, Cukierman E,
DeNardo DG, Egeblad M, Evans RM, Fearon D, Greten FR, Hingorani SR,
Hunter T, et al: A framework for advancing our understanding of
cancer-associated fibroblasts. Nat Rev Cancer. 20:174–186. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Farhood B, Najafi M and Mortezaee K:
Cancer-associated fibroblasts: Secretions, interactions, and
therapy. J Cell Biochem. 120:2791–2800. 2019. View Article : Google Scholar
|
|
44
|
Joshi RS, Kanugula SS, Sudhir S, Pereira
MP, Jain S and Aghi MK: The role of cancer-associated fibroblasts
in tumor progression. Cancers. 13:13992021. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Arina A, Idel C, Hyjek EM, Alegre ML, Wang
Y, Bindokas VP, Weichselbaum RR and Schreiber H: Tumor-associated
fibroblasts predominantly come from local and not circulating
precursors. Proc Natl Acad Sci USA. 113:7551–7556. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Raz Y, Cohen N, Shani O, Bell RE,
Novitskiy SV, Abramovitz L, Levy C, Milyavsky M, Leider-Trejo L,
Moses HL, et al: Bone marrow-derived fibroblasts are a functionally
distinct stromal cell population in breast cancer. J Exp Med.
215:3075–3093. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Peng Y and Li Z and Li Z: GRP78 secreted
by tumor cells stimulates differentiation of bone marrow
mesenchymal stem cells to cancer-associated fibroblasts. Biochem
Biophys Res Commun. 440:558–563. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Potenta S, Zeisberg E and Kalluri R: The
role of endothelial-to-mesenchymal transition in cancer
progression. Br J Cancer. 99:1375–1379. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Fischer KR, Durrans A, Lee S, Sheng J, Li
F, Wong ST, Choi H, El Rayes T, Ryu S, Troeger J, et al:
Epithelial-to-mesenchymal transition is not required for lung
metastasis but contributes to chemoresistance. Nature. 527:472–476.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Jotzu C, Alt E, Welte G, Li J, Hennessy
BT, Devarajan E, Krishnappa S, Pinilla S, Droll L and Song YH:
Adipose tissue derived stem cells differentiate into
carcinoma-associated fibroblast-like cells under the influence of
tumor derived factors. Cell Oncol (Dordr). 34:55–67. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Rinkevich Y, Mori T, Sahoo D, Xu PX,
Bermingham JR Jr and Weissman IL: Identification and prospective
isolation of a mesothelial precursor lineage giving rise to smooth
muscle cells and fibroblasts for mammalian internal organs, and
their vasculature. Nat Cell Biol. 14:1251–1260. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Bartoschek M, Oskolkov N, Bocci M, Lövrot
J, Larsson C, Sommarin M, Madsen CD, Lindgren D, Pekar G, Karlsson
G, et al: Spatially and functionally distinct subclasses of breast
cancer-associated fibroblasts revealed by single cell RNA
sequencing. Nat Commun. 9:51502018. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Pan C, Liu P, Ma D, Zhang S, Ni M, Fang Q
and Wang J: Bone marrow mesenchymal stem cells in microenvironment
transform into cancer-associated fibroblasts to promote the
progression of B-cell acute lymphoblastic leukemia. Biomed
Pharmacother. 130:1106102020. View Article : Google Scholar
|
|
54
|
Sun X, Cai W, Li H, Gao C, Ma X, Guo Y, Fu
D, Xiao D, Zhang Z, Wang Y, et al: Endothelial-like
cancer-associated fibroblasts facilitate pancreatic cancer
metastasis via vasculogenic mimicry and paracrine signalling. Gut.
Mar 23–2025.Epub ahead of print. View Article : Google Scholar
|
|
55
|
Hamabe-Horiike T, Harada SI, Yoshida K,
Kinoshita J, Yamaguchi T and Fushida S: Adipocytes contribute to
tumor progression and invasion of peritoneal metastasis by
interacting with gastric cancer cells as cancer associated
fibroblasts. Cancer Rep (Hoboken). 6:e16472023.
|
|
56
|
Huang H, Wang Z, Zhang Y, Pradhan RN,
Ganguly D, Chandra R, Murimwa G, Wright S, Gu X, Maddipati R, et
al: Mesothelial cell-derived antigen-presenting cancer-associated
fibroblasts induce expansion of regulatory T cells in pancreatic
cancer. Cancer Cell. 40:656–673.e7. 2022. View Article : Google Scholar :
|
|
57
|
Bu L, Baba H, Yoshida N, Miyake K, Yasuda
T, Uchihara T, Tan P and Ishimoto T: Biological heterogeneity and
versatility of cancer-associated fibroblasts in the tumor
microenvironment. Oncogene. 38:4887–4901. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Biffi G and Tuveson DA: Diversity and
biology of cancer-associated fibroblasts. Physiol Rev. 101:147–176.
2021. View Article : Google Scholar :
|
|
59
|
Chhabra Y and Weeraratna AT: Fibroblasts
in cancer: Unity in heterogeneity. Cell. 186:1580–1609. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Sugimoto H, Mundel TM, Kieran MW and
Kalluri R: Identification of fibroblast heterogeneity in the tumor
microenvironment. Cancer Biol Ther. 5:1640–1646. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Cortez E, Roswall P and Pietras K:
Functional subsets of mesenchymal cell types in the tumor
microenvironment. Semin Cancer Biol. 25:3–9. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Kim SJ, Kim SA, Choi YA, Park DY and Lee
J: Alpha-smooth muscle actin-positive perivascular cells in
diabetic retina and choroid. Int J Mol Sci. 21:21582020. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Wu Y, Wu C, Shi T, Cai Q, Wang T, Xiong Y,
Zhang Y, Jiang W, Lu M, Chen Z, et al: FAP expression in adipose
tissue macrophages promotes obesity and metabolic inflammation.
Proc Natl Acad Sci USA. 120:e23030751202023. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Kang SH, Oh SY, Lee HJ, Kwon TG, Kim JW,
Lee ST, Choi SY and Hong SH: Cancer-associated fibroblast subgroups
showing differential promoting effect on HNSCC progression. Cancers
(Basel). 13:6542021. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Kennel KB, Bozlar M, De Valk AF and Greten
FR: Cancer-associated fibroblasts in inflammation and antitumor
immunity. Clin Cancer Res. 29:1009–1016. 2023. View Article : Google Scholar :
|
|
66
|
Caligiuri G and Tuveson DA: Activated
fibroblasts in cancer: Perspectives and challenges. Cancer Cell.
41:434–449. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Öhlund D, Handly-Santana A, Biffi G,
Elyada E, Almeida AS, Ponz-Sarvise M, Corbo V, Oni TE, Hearn SA,
Lee EJ, et al: Distinct populations of inflammatory fibroblasts and
myofibroblasts in pancreatic cancer. J Exp Med. 214:579–596. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Elyada E, Bolisetty M, Laise P, Flynn WF,
Courtois ET, Burkhart RA, Teinor JA, Belleau P, Biffi G, Lucito MS,
et al: Cross-species single-cell analysis of pancreatic ductal
adenocarcinoma reveals antigen-presenting cancer-associated
fibroblasts. Cancer Discov. 9:1102–1123. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Costa A, Kieffer Y, Scholer-Dahirel A,
Pelon F, Bourachot B, Cardon M, Sirven P, Magagna I, Fuhrmann L,
Bernard C, et al: Fibroblast heterogeneity and immunosuppressive
environment in human breast cancer. Cancer Cell. 33:463–479.e10.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Shi T, Yao L, Han Y, Hao P and Lu P:
Quantitative phosphoproteomics reveals system-wide phosphorylation
network altered by spry in mouse mammary stromal fibroblasts. Int J
Mol Sci. 20:54002019. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Cords L, Tietscher S, Anzeneder T,
Langwieder C, Rees M, de Souza N and Bodenmiller B:
Cancer-associated fibroblast classification in single-cell and
spatial proteomics data. Nat Commun. 14:42942023. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Schwörer S, Cimino FV, Ros M, Tsanov KM,
Ng C, Lowe SW, Carmona-Fontaine C and Thompson CB: Hypoxia
potentiates the inflammatory fibroblast phenotype promoted by
pancreatic cancer cell-derived cytokines. Cancer Res. 83:1596–1610.
2023. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Biffi G, Oni TE, Spielman B, Hao Y, Elyada
E, Park Y, Preall J and Tuveson DA: IL1-induced JAK/STAT signaling
is antagonized by TGFβ to shape CAF heterogeneity in pancreatic
ductal adenocarcinoma. Cancer Discov. 9:282–301. 2019. View Article : Google Scholar
|
|
74
|
Huang J, Zhang L, Wan D, Zhou L, Zheng S,
Lin S and Qiao Y: Extracellular matrix and its therapeutic
potential for cancer treatment. Signal Transduct Target Ther.
6:1532021. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Piersma B, Hayward MK and Weaver VM:
Fibrosis and cancer: A strained relationship. Biochim Biophys Acta
Rev Cancer. 1873:1883562020. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Naba A, Clauser KR, Ding H, Whittaker CA,
Carr SA and Hynes RO: The extracellular matrix: Tools and insights
for the 'omics' era. Matrix Biol. 49:10–24. 2016. View Article : Google Scholar
|
|
77
|
Zeltz C, Primac I, Erusappan P, Alam J,
Noel A and Gullberg D: Cancer-associated fibroblasts in
desmoplastic tumors: Emerging role of integrins. Semin Cancer Biol.
62:166–181. 2020. View Article : Google Scholar
|
|
78
|
Santi A, Kugeratski FG and Zanivan S:
Cancer associated fibroblasts: The architects of stroma remodeling.
Proteomics. 18:e17001672018. View Article : Google Scholar
|
|
79
|
Najafi M, Farhood B and Mortezaee K:
Extracellular matrix (ECM) stiffness and degradation as cancer
drivers. J Cell Biochem. 120:2782–2790. 2019. View Article : Google Scholar
|
|
80
|
Peng D, Fu M, Wang M, Wei Y and Wei X:
Targeting TGF-β signal transduction for fibrosis and cancer
therapy. Mol Cancer. 21:1042022. View Article : Google Scholar
|
|
81
|
Patwardhan S, Mahadik P, Shetty O and Sen
S: ECM stiffness-tuned exosomes drive breast cancer motility
through thrombospondin-1. Biomaterials. 279:1211852021. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Wei SC, Fattet L, Tsai JH, Guo Y, Pai VH,
Majeski HE, Chen AC, Sah RL, Taylor SS, Engler AJ and Yang J:
Matrix stiffness drives epithelial-mesenchymal transition and
tumour metastasis through a TWIST1-G3BP2 mechanotransduction
pathway. Nat Cell Biol. 17:678–688. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Jiang Y, Zhang H, Wang J, Liu Y, Luo T and
Hua H: Targeting extracellular matrix stiffness and
mechanotransducers to improve cancer therapy. J Hematol Oncol.
15:342022. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Li ZL, Wang ZJ, Wei GH, Yang Y and Wang
XW: Changes in extracellular matrix in different stages of
colorectal cancer and their effects on proliferation of cancer
cells. World J Gastrointest Oncol. 12:267–275. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Erdogan B and Webb DJ: Cancer-associated
fibroblasts modulate growth factor signaling and extracellular
matrix remodeling to regulate tumor metastasis. Biochem Soc Trans.
45:229–236. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Jabłońska-Trypuć A, Matejczyk M and
Rosochacki S: Matrix metalloproteinases (MMPs), the main
extracellular matrix (ECM) enzymes in collagen degradation, as a
target for anticancer drugs. J Enzyme Inhib Med Chem. 31:177–183.
2016. View Article : Google Scholar
|
|
87
|
Cazet AS, Hui MN, Elsworth BL, Wu SZ,
Roden D, Chan CL, Skhinas JN, Collot R, Yang J, Harvey K, et al:
Targeting stromal remodeling and cancer stem cell plasticity
overcomes chemoresistance in triple negative breast cancer. Nat
Commun. 9:28972018. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Shi Y, Gao W, Lytle NK, Huang P, Yuan X,
Dann AM, Ridinger-Saison M, DelGiorno KE, Antal CE, Liang G, et al:
Targeting LIF-mediated paracrine interaction for pancreatic cancer
therapy and monitoring. Nature. 569:131–135. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Kaur A, Ecker BL, Douglass SM, Kugel CH
III, Webster MR, Almeida FV, Somasundaram R, Hayden J, Ban E,
Ahmadzadeh H, et al: Remodeling of the collagen matrix in aging
skin promotes melanoma metastasis and affects immune cell motility.
Cancer Discov. 9:64–81. 2019. View Article : Google Scholar :
|
|
90
|
Zhang X, Dong Y, Zhao M, Ding L, Yang X,
Jing Y, Song Y, Chen S, Hu Q and Ni Y: ITGB2-mediated metabolic
switch in CAFs promotes OSCC proliferation by oxidation of NADH in
mitochondrial oxidative phosphorylation system. Theranostics.
10:12044–12059. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Fang Z, Xu J, Zhang B, Wang W, Liu J,
Liang C, Hua J, Meng Q, Yu X and Shi S: The promising role of
noncoding RNAs in cancer-associated fibroblasts: An overview of
current status and future perspectives. J Hematol Oncol.
13:1542020. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Zeng Y, Li B, Liang Y, Reeves PM, Qu X,
Ran C, Liu Q, Callahan MV, Sluder AE, Gelfand JA, et al: Dual
blockade of CXCL12-CXCR4 and PD-1-PD-L1 pathways prolongs survival
of ovarian tumor-bearing mice by prevention of immunosuppression in
the tumor microenvironment. FASEB J. 33:6596–6608. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Wei R, Li J, Lin W, Pang X, Yang H, Lai S,
Wei X, Jiang X, Yuan Y and Yang R: Nanoparticle-mediated blockade
of CXCL12/CXCR4 signaling enhances glioblastoma immunotherapy:
Monitoring early responses with MRI radiomics. Acta Biomater.
177:414–430. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Feig C, Jones JO, Kraman M, Wells RJ,
Deonarine A, Chan DS, Connell CM, Roberts EW, Zhao Q, Caballero OL,
et al: Targeting CXCL12 from FAP-expressing carcinoma-associated
fibroblasts synergizes with anti-PD-L1 immunotherapy in pancreatic
cancer. Proc Natl Acad Sci USA. 110:20212–20217. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Wang H, Liang Y, Liu Z, Zhang R, Chao J,
Wang M, Liu M, Qiao L, Xuan Z, Zhao H and Lu L: POSTN+
cancer-associated fibroblasts determine the efficacy of
immunotherapy in hepatocellular carcinoma. J Immunother Cancer.
12:e0087212024. View Article : Google Scholar :
|
|
96
|
Chen C, Guo Q, Liu Y, Hou Q, Liao M, Guo
Y, Zang Y, Wang F, Liu H, Luan X, et al: Single-cell and spatial
transcriptomics reveal POSTN+ cancer-associated
fibroblasts correlated with immune suppression and tumour
progression in non-small cell lung cancer. Clin Transl Med.
13:e15152023. View Article : Google Scholar
|
|
97
|
Li Z, Sun C and Qin Z: Metabolic
reprogramming of cancer-associated fibroblasts and its effect on
cancer cell reprogramming. Theranostics. 11:8322–8336. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Zhang S, Wang J, Chen Y, Liang W, Liu H,
Du R, Sun Y, Hu C and Shang Z: CAFs-derived lactate enhances the
cancer stemness through inhibiting the MST1 ubiquitination
degradation in OSCC. Cell Biosci. 14:1442024. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Bertero T, Oldham WM, Grasset EM, Bourget
I, Boulter E, Pisano S, Hofman P, Bellvert F, Meneguzzi G, Bulavin
DV, et al: Tumor-stroma mechanics coordinate amino acid
availability to sustain tumor growth and malignancy. Cell Metab.
29:124–140.e10. 2019. View Article : Google Scholar :
|
|
100
|
Kim I, Choi S, Yoo S, Lee M and Kim IS:
Cancer-associated fibroblasts in the hypoxic tumor
microenvironment. Cancers (Basel). 14:33212022. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Wei X, Chen Y, Jiang X, Peng M, Liu Y, Mo
Y, Ren D, Hua Y, Yu B, Zhou Y, et al: Mechanisms of vasculogenic
mimicry in hypoxic tumor microenvironments. Mol Cancer. 20:72021.
View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Cadamuro M, Brivio S, Mertens J, Vismara
M, Moncsek A, Milani C, Fingas C, Cristina Malerba M, Nardo G,
Dall'Olmo L, et al: Platelet-derived growth factor-D enables liver
myofibroblasts to promote tumor lymphangiogenesis in
cholangiocarcinoma. J Hepatol. 70:700–709. 2019. View Article : Google Scholar
|
|
103
|
Li P, Zhang H, Chen T, Zhou Y, Yang J and
Zhou J: Cancer-associated fibroblasts promote proliferation,
angiogenesis, metastasis and immunosuppression in gastric cancer.
Matrix Biol. 132:59–71. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Dai S, Liu Y, Liu Z, Li R, Luo F, Li Y,
Dai L and Peng X: Cancer-associated fibroblasts mediate resistance
to anti-EGFR therapies in cancer. Pharmacol Res. 206:1073042024.
View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Kobayashi H, Enomoto A, Woods SL, Burt AD,
Takahashi M and Worthley DL: Cancer-associated fibroblasts in
gastrointestinal cancer. NaNat Rev Gastroenterol Hepatol.
16:282–295. 2019. View Article : Google Scholar
|
|
106
|
Mucciolo G, Araos Henríquez J, Jihad M,
Pinto Teles S, Manansala JS, Li W, Ashworth S, Lloyd EG, Cheng PSW,
Luo W, et al: EGFR-activated myofibroblasts promote metastasis of
pancreatic cancer. Cancer Cell. 42:101–118.e11. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Bordignon P, Bottoni G, Xu X, Popescu AS,
Truan Z, Guenova E, Kofler L, Jafari P, Ostano P, Röcken M, et al:
Dualism of FGF and TGF-β signaling in heterogeneous
cancer-associated fibroblast activation with ETV1 as a critical
determinant. Cell Rep. 28:2358–2372.e6. 2019. View Article : Google Scholar
|
|
108
|
Likonen D, Pinchasi M, Beery E, Sarsor Z,
Signorini LF, Gervits A, Sharan R, Lahav M, Raanani P and Uziel O:
Exosomal telomerase transcripts reprogram the microRNA
transcriptome profile of fibroblasts and partially contribute to
CAF formation. Sci Rep. 12:164152022. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Tang XH, Guo T, Gao XY, Wu XL, Xing XF, Ji
JF and Li ZY: Exosome-derived noncoding RNAs in gastric cancer:
Functions and clinical applications. Mol Cancer. 20:992021.
View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Cosentino G, Romero-Cordoba S, Plantamura
I, Cataldo A and Iorio MV: miR-9-mediated inhibition of EFEMP1
contributes to the acquisition of pro-tumoral properties in normal
fibroblasts. Cells. 9:21432020. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Li J, Guan J, Long X, Wang Y and Xiang X:
mir-1-mediated paracrine effect of cancer-associated fibroblasts on
lung cancer cell proliferation and chemoresistance. Oncol Rep.
35:3523–3531. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Zhang L, Yao J, Li W and Zhang C:
Micro-RNA-21 regulates cancer-associated fibroblast-mediated drug
resistance in pancreatic cancer. Oncol Res. 26:827–835. 2018.
View Article : Google Scholar
|
|
113
|
Xia B, Gu X, Xu T, Yan M, Huang L, Jiang
C, Li M, Zhai G, Zhang G, Wu J, et al: Exosomes-mediated transfer
of LINC00691 regulates the formation of CAFs and promotes the
progression of gastric cancer. BMC Cancer. 23:9282023. View Article : Google Scholar
|
|
114
|
Pang W, Su J, Wang Y, Feng H, Dai X, Yuan
Y, Chen X and Yao W: Pancreatic cancer-secreted miR-155 implicates
in the conversion from normal fibroblasts to cancer-associated
fibroblasts. Cancer Sci. 106:1362–1369. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Li F, Zhang F, Wang T, Xie Z, Luo H, Dong
W, Zhang J, Ren C and Peng W: A self-amplifying loop of TP53INP1
and P53 drives oxidative stress-induced apoptosis of bone marrow
mesenchymal stem cells. Apoptosis. 29:882–897. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Vennin C, Mélénec P, Rouet R, Nobis M,
Cazet AS, Murphy KJ, Herrmann D, Reed DA, Lucas MC, Warren SC, et
al: CAF hierarchy driven by pancreatic cancer cell p53-status
creates a pro-metastatic and chemoresistant environment via
perlecan. Nat Commun. 10:36372019. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Fang T, Lv H, Lv G, Li T, Wang C, Han Q,
Yu L, Su B, Guo L, Huang S, et al: Tumor-derived exosomal
miR-1247-3p induces cancer-associated fibroblast activation to
foster lung metastasis of liver cancer. Nat Commun. 9:1912018.
View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Zhou Y, Ren H, Dai B, Li J, Shang L, Huang
J and Shi X: Hepatocellular carcinoma-derived exosomal miRNA-21
contributes to tumor progression by converting hepatocyte stellate
cells to cancer-associated fibroblasts. J Exp Clin Cancer Res.
37:3242018. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Ye B, Duan Y, Zhou M, Wang Y, Lai Q, Yue
K, Cao J, Wu Y, Wang X and Jing C: Hypoxic tumor-derived exosomal
miR-21 induces cancer-associated fibroblast activation to promote
head and neck squamous cell carcinoma metastasis. Cell Signal.
108:1107252023. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Hu T and Hu J: Melanoma-derived exosomes
induce reprogramming fibroblasts into cancer-associated fibroblasts
via Gm26809 delivery. Cell Cycle. 18:3085–3094. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Dror S, Sander L, Schwartz H, Sheinboim D,
Barzilai A, Dishon Y, Apcher S, Golan T, Greenberger S, Barshack I,
et al: Melanoma miRNA trafficking controls tumour primary niche
formation. Nat Cell Biol. 18:1006–1017. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Vu LT, Peng B, Zhang DX, Ma V,
Mathey-Andrews CA, Lam CK, Kiomourtzis T, Jin J, McReynolds L,
Huang L, et al: Tumor-secreted extracellular vesicles promote the
activation of cancer-associated fibroblasts via the transfer of
microRNA-125b. J Extracell Vesicles. 8:15996802019. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Yang SS, Ma S, Dou H, Liu F, Zhang SY,
Jiang C, Xiao M and Huang YX: Breast cancer-derived exosomes
regulate cell invasion and metastasis in breast cancer via miR-146a
to activate cancer associated fibroblasts in tumor
microenvironment. Exp Cell Res. 391:1119832020. View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Baroni S, Romero-Cordoba S, Plantamura I,
Dugo M, D'Ippolito E, Cataldo A, Cosentino G, Angeloni V, Rossini
A, Daidone MG and Iorio MV: Exosome-mediated delivery of miR-9
induces cancer-associated fibroblast-like properties in human
breast fibroblasts. Cell Death Dis. 7:e23122016. View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Tong Y, Yang L, Yu C, Zhu W, Zhou X, Xiong
Y, Wang W, Ji F, He D and Cao X: Tumor-secreted exosomal lncRNA
POU3F3 promotes cisplatin resistance in ESCC by inducing fibroblast
differentiation into CAFs. Mol Ther Oncolytics. 18:1–13. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Wang D, Wang X, Song Y, Si M, Sun Y, Liu
X, Cui S, Qu X and Yu X: Exosomal miR-146a-5p and miR-155-5p
promote CXCL12/CXCR7-induced metastasis of colorectal cancer by
crosstalk with cancer-associated fibroblasts. Cell Death Dis.
13:3802022. View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Becker LM, O'Connell JT, Vo AP, Cain MP,
Tampe D, Bizarro L, Sugimoto H, McGow AK, Asara JM, Lovisa S, et
al: Epigenetic reprogramming of cancer-associated fibroblasts
deregulates glucose metabolism and facilitates progression of
breast cancer. Cell Rep. 31:1077012020. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Pavlides S, Whitaker-Menezes D,
Castello-Cros R, Flomenberg N, Witkiewicz AK, Frank PG, Casimiro
MC, Wang C, Fortina P, Addya S, et al: The reverse Warburg effect:
Aerobic glycolysis in cancer associated fibroblasts and the tumor
stroma. Cell Cycle. 8:3984–4001. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Kitamura F, Semba T, Yasuda-Yoshihara N,
Yamada K, Nishimura A, Yamasaki J, Nagano O, Yasuda T, Yonemura A,
Tong Y, et al: Cancer-associated fibroblasts reuse cancer-derived
lactate to maintain a fibrotic and immunosuppressive
microenvironment in pancreatic cancer. JCI Insight. 8:e1630222023.
View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Zhang C, Zhou W, Xu H, Xu J, Li J, Liu X,
Lu X, Dai J, Jiang Y, Wang W, et al: Cancer-associated fibroblasts
promote EGFR-TKI resistance via the CTHRC1/glycolysis/H3K18la
positive feedback loop. Oncogene. 44:1400–1414. 2025. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Yan W, Wu X, Zhou W, Fong MY, Cao M, Liu
J, Liu X, Chen CH, Fadare O, Pizzo DP, et al: Cancer-cell-secreted
exosomal miR-105 promotes tumour growth through the MYC-dependent
metabolic reprogramming of stromal cells. Nat Cell Biol.
20:597–609. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
132
|
He R, Hu C, Yuan Y, Li T, Tian Q, Huang T,
Lin Q, Zheng S, Chen C, Fu Z and Chen R: Glycolysis reprogramming
in CAFs promotes oxaliplatin resistance in pancreatic cancer
through circABCC4 mediated PKM2 nuclear translocation. Cell Death
Dis. 16:1262025. View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Kazakova AN, Lukina MM, Anufrieva KS,
Bekbaeva IV, Ivanova OM, Shnaider PV, Slonov A, Arapidi GP and
Shender VO: Exploring the diversity of cancer-associated
fibroblasts: Insights into mechanisms of drug resistance. Front
Cell Dev Biol. 12:14031222024. View Article : Google Scholar : PubMed/NCBI
|
|
134
|
Long X, Xiong W, Zeng X, Qi L, Cai Y, Mo
M, Jiang H, Zhu B, Chen Z and Li Y: Cancer-associated fibroblasts
promote cisplatin resistance in bladder cancer cells by increasing
IGF-1/ERβ/Bcl-2 signalling. Cell Death Dis. 10:3752019. View Article : Google Scholar
|
|
135
|
Zhang T, Zhang P and Li HX: CAFs-derived
exosomal miRNA-130a confers cisplatin resistance of NSCLC cells
through PUM2-dependent packaging. Int J Nanomedicine. 16:561–577.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Yip HYK and Papa A: Signaling pathways in
cancer: Therapeutic targets, combinatorial treatments, and new
developments. Cells. 10:6592021. View Article : Google Scholar : PubMed/NCBI
|
|
137
|
Zhang YE: Non-smad signaling pathways of
the TGF-β family. Cold Spring Harb Perspect Biol. 9:a0221292017.
View Article : Google Scholar
|
|
138
|
Moon JY, Manh Hung LV, Unno T and Cho SK:
Nobiletin enhances chemosensitivity to adriamycin through
modulation of the Akt/GSK3β/β-catenin/MYCN/MRP1 signaling pathway
in A549 human non-small-cell lung cancer cells. Nutrients.
10:18292018. View Article : Google Scholar
|
|
139
|
Tomar VS, Patil V and Somasundaram K:
Temozolomide induces activation of Wnt/β-catenin signaling in
glioma cells via PI3K/Akt pathway: Implications in glioma therapy.
Cell Biol Toxicol. 36:273–278. 2020. View Article : Google Scholar
|
|
140
|
Sun Z, Jiang Q, Gao B, Zhang X, Bu L, Wang
L, Lin Y, Xie W, Li J and Guo J: AKT blocks SIK1-mediated
repression of STAT3 to promote breast tumorigenesis. Cancer Res.
83:1264–1279. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
141
|
Belarif L, Mary C, Jacquemont L, Mai HL,
Danger R, Hervouet J, Minault D, Thepenier V, Nerrière-Daguin V,
Nguyen E, et al: IL-7 receptor blockade blunts antigen-specific
memory T cell responses and chronic inflammation in primates. Nat
Commun. 9:44832018. View Article : Google Scholar : PubMed/NCBI
|
|
142
|
Wang X, Jiang W, Du Y, Zhu D, Zhang J,
Fang C, Yan F and Chen ZS: Targeting feedback activation of
signaling transduction pathways to overcome drug resistance in
cancer. Drug Resist Updat. 65:1008842022. View Article : Google Scholar : PubMed/NCBI
|
|
143
|
Fang Z, Meng Q, Xu J, Wang W, Zhang B, Liu
J, Liang C, Hua J, Zhao Y, Yu X and Shi S: Signaling pathways in
cancer-associated fibroblasts: Recent advances and future
perspectives. Cancer Commun (Lond). 43:3–41. 2023. View Article : Google Scholar
|
|
144
|
Butti R, Khaladkar A, Bhardwaj P and
Prakasam G: Heterotypic signaling of cancer-associated fibroblasts
in shaping the cancer cell drug resistance. Cancer Drug Resist.
6:182–204. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
145
|
Keresztes D, Kerestély M, Szarka L, Kovács
BM, Schulc K, Veres DV and Csermely P: Cancer drug resistance as
learning of signaling networks. Biomed Pharmacother.
183:1178802025. View Article : Google Scholar : PubMed/NCBI
|
|
146
|
Xue W, Yang L, Chen C, Ashrafizadeh M,
Tian Y and Sun R: Wnt/β-catenin-driven EMT regulation in human
cancers. Cell Mol Life Sci. 81:792024. View Article : Google Scholar
|
|
147
|
Zhao H, Ming T, Tang S, Ren S, Yang H, Liu
M, Tao Q and Xu H: Wnt signaling in colorectal cancer: Pathogenic
role and therapeutic target. Mol Cancer. 21:1442022. View Article : Google Scholar : PubMed/NCBI
|
|
148
|
Wang Y, Zheng L, Shang W, Yang Z, Li T,
Liu F, Shao W, Lv L, Chai L, Qu L, et al: Wnt/beta-catenin
signaling confers ferroptosis resistance by targeting GPX4 in
gastric cancer. Cell Death Differ. 29:2190–2202. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
149
|
Essex A, Pineda J, Acharya G, Xin H and
Evans J; Reproducibility Project: Cancer Biology: Replication
study: Wnt activity defines colon cancer stem cells and is
regulated by the microenvironment. ELife. 8:e454262019. View Article : Google Scholar
|
|
150
|
Ren J, Ding L, Zhang D, Shi G, Xu Q, Shen
S, Wang Y, Wang T and Hou Y: Carcinoma-associated fibroblasts
promote the stemness and chemoresistance of colorectal cancer by
transferring exosomal lncRNA H19. Theranostics. 8:3932–3948. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
151
|
Deng X, Ruan H, Zhang X, Xu X, Zhu Y, Peng
H, Zhang X, Kong F and Guan M: Long noncoding RNA CCAL transferred
from fibroblasts by exosomes promotes chemoresistance of colorectal
cancer cells. Int J Cancer. 146:1700–1716. 2020. View Article : Google Scholar
|
|
152
|
Shan G, Zhou X, Gu J, Zhou D, Cheng W, Wu
H, Wang Y, Tang T and Wang X: Downregulated exosomal
microRNA-148b-3p in cancer associated fibroblasts enhance
chemosensitivity of bladder cancer cells by downregulating the
Wnt/β-catenin pathway and upregulating PTEN. Cell Oncol (Dordr).
44:45–59. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
153
|
Cao L, Weng K, Li L, Lin G, Zhao Y, Gao Y,
Huang X, Chen Q, Wang J, Zheng C, et al: BATF2 inhibits the stem
cell-like properties and chemoresistance of gastric cancer cells
through PTEN/AKT/β-catenin pathway. Theranostics. 14:7007–7022.
2024. View Article : Google Scholar :
|
|
154
|
Fang F, Guo C, Zheng W, Wang Q and Zhou L:
Exosome-mediated transfer of miR-1323 from cancer-associated
fibroblasts confers radioresistance of C33A cells by targeting
PABPN1 and activating Wnt/β-catenin signaling pathway in cervical
cancer. Reprod Sci. 29:1809–1821. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
155
|
Zou S, Tong Q, Liu B, Huang W, Tian Y and
Fu X: Targeting STAT3 in cancer immunotherapy. Mol Cancer.
19:1452020. View Article : Google Scholar : PubMed/NCBI
|
|
156
|
Hu Y, Dong Z and Liu K: Unraveling the
complexity of STAT3 in cancer: Molecular understanding and drug
discovery. J Exp Clin Cancer Res. 43:232024. View Article : Google Scholar : PubMed/NCBI
|
|
157
|
Pan MS, Wang H, Ansari KH, Li XP, Sun W
and Fan YZ: Gallbladder cancer-associated fibroblasts promote
vasculogenic mimicry formation and tumor growth in gallbladder
cancer via upregulating the expression of NOX4, a poor prognosis
factor, through IL-6-JAK-STAT3 signal pathway. J Exp Clin Cancer
Res. 39:2342020. View Article : Google Scholar : PubMed/NCBI
|
|
158
|
Yu Z, Zhang Q, Wei S, Zhang Y, Zhou T,
Zhang Q, Shi R, Zinovkin D, Pranjol ZI, Zhang J and Wang H:
CD146+CAFs promote progression of endometrial cancer by
inducing angiogenesis and vasculogenic mimicry via IL-10/JAK1/STAT3
pathway. Cell Commun Signal. 22:1702024. View Article : Google Scholar
|
|
159
|
Tao L, Huang G, Wang R, Pan Y, He Z, Chu
X, Song H and Chen L: Cancer-associated fibroblasts treated with
cisplatin facilitates chemoresistance of lung adenocarcinoma
through IL-11/IL-11R/STAT3 signaling pathway. Sci Rep. 6:384082016.
View Article : Google Scholar : PubMed/NCBI
|
|
160
|
Li J, Wang Y, Wang Z, Wei Y, Diao P, Wu Y,
Wang D, Jiang H, Wang Y and Cheng J: Super-enhancer driven
LIF/LIFR-STAT3-SOX2 regulatory feedback loop promotes cancer
stemness in head and neck squamous cell carcinoma. Adv Sci (Weinh).
11:e24044762024. View Article : Google Scholar : PubMed/NCBI
|
|
161
|
Hu C, Xia R, Zhang X, Li T, Ye Y, Li G, He
R, Li Z, Lin Q, Zheng S and Chen R: circFARP1 enables
cancer-associated fibroblasts to promote gemcitabine resistance in
pancreatic cancer via the LIF/STAT3 axis. Mol Cancer. 21:242022.
View Article : Google Scholar : PubMed/NCBI
|
|
162
|
Sun L, Ke M, Yin M, Zeng Y, Ji Y, Hu Y, Fu
S and Zhang C: Extracellular vesicle-encapsulated microRNA-296-3p
from cancer-associated fibroblasts promotes ovarian cancer
development through regulation of the PTEN/AKT and SOCS6/STAT3
pathways. Cancer Sci. 115:155–169. 2024. View Article : Google Scholar
|
|
163
|
Zhao Q, Huang L, Qin G, Qiao Y, Ren F,
Shen C, Wang S, Liu S, Lian J, Wang D, et al: Cancer-associated
fibroblasts induce monocytic myeloid-derived suppressor cell
generation via IL-6/exosomal miR-21-activated STAT3 signaling to
promote cisplatin resistance in esophageal squamous cell carcinoma.
Cancer Lett. 518:35–48. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
164
|
Cao LQ, Yang XW, Chen YB, Zhang DW, Jiang
XF and Xue P: Exosomal miR-21 regulates the TETs/PTENp1/PTEN
pathway to promote hepatocellular carcinoma growth. Mol Cancer.
18:1482019. View Article : Google Scholar : PubMed/NCBI
|
|
165
|
Gupta S, Silveira DA, Lorenzoni PR,
Mombach JCM and Hashimoto RF: LncRNA PTENP1/miR-21/PTEN axis
modulates EMT and drug resistance in cancer: Dynamic boolean
modeling for cell fates in DNA damage response. Int J Mol Sci.
25:82642024. View Article : Google Scholar : PubMed/NCBI
|
|
166
|
He Y, Sun MM, Zhang GG, Yang J, Chen KS,
Xu WW and Li B: Targeting PI3K/Akt signal transduction for cancer
therapy. Signal Transduct Target Ther. 6:4252021. View Article : Google Scholar : PubMed/NCBI
|
|
167
|
Murugan AK: mTOR: Role in cancer,
metastasis and drug resistance. Semin Cancer Biol. 59:92–111. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
168
|
Haddadi N, Lin Y, Travis G, Simpson AM,
Nassif NT and McGowan EM: PTEN/PTENP1: 'Regulating the regulator of
RTK-dependent PI3K/Akt signalling', new targets for cancer therapy.
Mol Cancer. 17:372018. View Article : Google Scholar : PubMed/NCBI
|
|
169
|
Shi L, Zhu W, Huang Y, Zhuo L, Wang S,
Chen S, Zhang B and Ke B: Cancer-associated fibroblast-derived
exosomal microRNA-20a suppresses the PTEN/PI3K-AKT pathway to
promote the progression and chemoresistance of non-small cell lung
cancer. Clin Transl Med. 12:e9892022. View Article : Google Scholar : PubMed/NCBI
|
|
170
|
Qu Z, Yang KD, Luo BH and Zhang F:
CAFs-secreted exosomal cricN4BP2L2 promoted colorectal cancer
stemness and chemoresistance by interacting with EIF4A3. Exp Cell
Res. 418:1132662022. View Article : Google Scholar : PubMed/NCBI
|
|
171
|
Li L, Liu D, Chen T, Wei C, Qiao Y, Liu W,
Liang Y, Liang Z, Chen C, Li D, et al: Hypoxia-enhanced YAP1-EIF4A3
interaction drives circ_0007386 circularization by competing with
CRIM1 pre-mRNA linear splicing and promotes non-small cell lung
cancer progression. J Exp Clin Cancer Res. 43:2002024. View Article : Google Scholar : PubMed/NCBI
|
|
172
|
Ju C, Zhou M, Du D, Wang C, Yao J, Li H,
Luo Y, He F and He J: EIF4A3-mediated circ_0042881 activates the
RAS pathway via miR-217/SOS1 axis to facilitate breast cancer
progression. Cell Death Dis. 14:5592023. View Article : Google Scholar : PubMed/NCBI
|
|
173
|
Zhang Y, Pan Q and Shao Z: Extracellular
vesicles derived from cancer-associated fibroblasts carry
tumor-promotive microRNA-1228-3p to enhance the resistance of
hepatocellular carcinoma cells to sorafenib. Hum Cell. 36:296–311.
2023. View Article : Google Scholar
|
|
174
|
Deng K, Zou F, Xu J, Xu D and Luo Z:
Cancer-associated fibroblasts promote stemness maintenance and
gemcitabine resistance via HIF-1α/miR-21 axis under hypoxic
conditions in pancreatic cancer. Mol Carcinog. 63:524–537. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
175
|
Xin X, Cheng X, Zeng F, Xu Q and Hou L:
The role of TGF-β/SMAD signaling in hepatocellular carcinoma: From
mechanism to therapy and prognosis. Int J Biol Sci. 20:1436–1451.
2024. View Article : Google Scholar :
|
|
176
|
Huang X, Jie S, Li W, Li H, Ni J and Liu
C: miR-122-5p targets GREM2 to protect against
glucocorticoid-induced endothelial damage through the BMP signaling
pathway. Mol Cell Endocrinol. 544:1115412022. View Article : Google Scholar : PubMed/NCBI
|
|
177
|
Shan G, Gu J, Zhou D, Li L, Cheng W, Wang
Y, Tang T and Wang X: Cancer-associated fibroblast-secreted
exosomal miR-423-5p promotes chemotherapy resistance in prostate
cancer by targeting GREM2 through the TGF-β signaling pathway. Exp
Mol Med. 52:1809–1822. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
178
|
Leng Z, Li Y, Zhou G, Lv X, Ai W, Li J and
Hou L: Krüppel-like factor 4 regulates stemness and mesenchymal
properties of colorectal cancer stem cells through the
TGF-β1/Smad/snail pathway. J Cell Mol Med. 24:1866–1877. 2020.
View Article : Google Scholar
|
|
179
|
Liu T, Jiang L, Bai Q, Wu S, Yu X, Wu T,
Wang J, Zhang X, Li H, Zhao K and Wang L: CLDN6 suppresses
migration and invasion of MCF-7 and SKBR-3 breast cancer cells by
blocking the SMAD/Snail/MMP-2/9 axis. Bull Exp Biol Med.
175:376–381. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
180
|
Richards KE, Zeleniak AE, Fishel ML, Wu J,
Littlepage LE and Hill R: Cancer-associated fibroblast exosomes
regulate survival and proliferation of pancreatic cancer cells.
Oncogene. 36:1770–1778. 2017. View Article : Google Scholar :
|
|
181
|
Sun J, Du R, Li X, Liu C, Wang D, He X, Li
G, Zhang K, Wang S, Hao Q, et al: CD63+
cancer-associated fibroblasts confer CDK4/6 inhibitor resistance to
breast cancer cells by exosomal miR-20. Cancer Lett.
588:2167472024. View Article : Google Scholar
|
|
182
|
Fang Y, Zhou W, Rong Y, Kuang T, Xu X, Wu
W, Wang D and Lou W: Exosomal miRNA-106b from cancer-associated
fibroblast promotes gemcitabine resistance in pancreatic cancer.
Exp Cell Res. 383:1115432019. View Article : Google Scholar : PubMed/NCBI
|
|
183
|
Pan S, Deng Y, Fu J, Zhang Y, Zhang Z and
Qin X: N6-methyladenosine upregulates miR-181d-5p in exosomes
derived from cancer-associated fibroblasts to inhibit 5-FU
sensitivity by targeting NCALD in colorectal cancer. Int J Oncol.
60:142022. View Article : Google Scholar :
|
|
184
|
Yang C, Zhang Y, Yan M, Wang J, Wang J,
Wang M, Xuan Y, Cheng H, Ma J, Chai C, et al: Exosomes derived from
cancer-associated fibroblasts promote tumorigenesis, metastasis and
chemoresistance of colorectal cancer by upregulating circ_0067557
to target Lin28. BMC Cancer. 24:642024. View Article : Google Scholar : PubMed/NCBI
|
|
185
|
Luo D, Liang Y, Wang Y, Ye F, Jin Y, Li Y,
Han D, Wang Z, Chen B, Zhao W, et al: Long non-coding RNA
MIDEAS-AS1 inhibits growth and metastasis of triple-negative breast
cancer via transcriptionally activating NCALD. Breast Cancer Res.
25:1092023. View Article : Google Scholar : PubMed/NCBI
|
|
186
|
Zhang J, Ratanasirintrawoot S,
Chandrasekaran S, Wu Z, Ficarro SB, Yu C, Ross CA, Cacchiarelli D,
Xia Q, Seligson M, et al: LIN28 regulates stem cell metabolism and
conversion to primed pluripotency. Cell Stem Cell. 19:66–80. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
187
|
Gong W, Guo Y, Yuan H, Chai R, Wan Z,
Zheng B, Hu X, Chen B, Gao S, Dai Q, et al: Loss of exosomal
miR-200b-3p from hypoxia cancer-associated fibroblasts promotes
tumorigenesis and reduces sensitivity to 5-flourouracil in
colorectal cancer via upregulation of ZEB1 and E2F3. Cancer Gene
Ther. 30:905–916. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
188
|
Obeng E: Apoptosis (programmed cell death)
and its signals-a review. Braz J Biol. 81:1133–1143. 2021.
View Article : Google Scholar
|
|
189
|
Xu X, Lai Y and Hua ZC: Apoptosis and
apoptotic body: Disease message and therapeutic target potentials.
Biosci Rep. 39:BSR201809922019. View Article : Google Scholar :
|
|
190
|
Moyer A, Tanaka K and Cheng EH: Apoptosis
in cancer biology and therapy. Annu Rev Pathol. 20:303–328. 2025.
View Article : Google Scholar : PubMed/NCBI
|
|
191
|
Sahoo G, Samal D, Khandayataray P and
Murthy MK: A review on caspases: Key regulators of biological
activities and apoptosis. Mol Neurobiol. 60:5805–5837. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
192
|
Singh P and Lim B: Targeting apoptosis in
cancer. Curr Oncol Rep. 24:273–284. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
193
|
Au Yeung CL, Co NN, Tsuruga T, Yeung TL,
Kwan SY, Leung CS, Li Y, Lu ES, Kwan K, Wong KK, et al: Exosomal
transfer of stroma-derived miR21 confers paclitaxel resistance in
ovarian cancer cells through targeting APAF1. Nat Commun.
7:111502016. View Article : Google Scholar : PubMed/NCBI
|
|
194
|
Zhou Z, Arroum T, Luo X, Kang R, Lee YJ,
Tang D, Hüttemann M and Song X: Diverse functions of cytochrome c
in cell death and disease. Cell Death Differ. 31:387–404. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
195
|
Sun LH, Tian D, Yang ZC and Li JL:
Exosomal miR-21 promotes proliferation, invasion and therapy
resistance of colon adenocarcinoma cells through its target PDCD4.
Sci Rep. 10:82712020. View Article : Google Scholar : PubMed/NCBI
|
|
196
|
Zhao MY, Wang LM, Liu J, Huang X, Liu J
and Zhang YF: MiR-21 suppresses anoikis through targeting PDCD4 and
PTEN in human esophageal adenocarcinoma. Curr Med Sci. 38:245–251.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
197
|
Wei X, Wang W, Wang L, Zhang Y, Zhang X,
Chen M, Wang F, Yu J, Ma Y and Sun G: MicroRNA-21 induces
5-fluorouracil resistance in human pancreatic cancer cells by
regulating PTEN and PDCD4. Cancer Med. 5:693–702. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
198
|
King LE, Hohorst L and García-Sáez AJ:
Expanding roles of BCL-2 proteins in apoptosis execution and
beyond. J Cell Sci. 136:jcs2607902023. View Article : Google Scholar : PubMed/NCBI
|
|
199
|
O'Neill KL, Huang K, Zhang J, Chen Y and
Luo X: Inactivation of prosurvival Bcl-2 proteins activates Bax/Bak
through the outer mitochondrial membrane. Genes Dev. 30:973–988.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
200
|
Kang SH, Oh SY, Lee KY, Lee HJ, Kim MS,
Kwon TG, Kim JW, Lee ST, Choi SY and Hong SH: Differential effect
of cancer-associated fibroblast-derived extracellular vesicles on
cisplatin resistance in oral squamous cell carcinoma via
miR-876-3p. Theranostics. 14:460–479. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
201
|
Price D, Muterspaugh R, Clegg B, Williams
A, Stephens A, Guthrie J, Heyl D and Evans HG: IGFBP-3 blocks
hyaluronan-CD44 signaling, leading to increased
acetylcholinesterase levels in A549 cell media and apoptosis in a
p53-dependent manner. Sci Rep. 10:50832020. View Article : Google Scholar : PubMed/NCBI
|
|
202
|
Wang H, Wang H, Li K, Li S and Sun B:
IGFBP-3 Is the key target of sanguinarine in promoting apoptosis in
hepatocellular carcinoma. Cancer Manag Res. 12:1007–1015. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
203
|
Wang H, Huang H, Wang L, Liu Y, Wang M,
Zhao S, Lu G and Kang X: Cancer-associated fibroblasts secreted
miR-103a-3p suppresses apoptosis and promotes cisplatin resistance
in non-small cell lung cancer. Aging (Albany NY). 13:14456–14468.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
204
|
Zhang HW, Shi Y, Liu JB, Wang HM, Wang PY,
Wu ZJ, Li L, Gu LP, Cao PS, Wang GR, et al: Cancer-associated
fibroblast-derived exosomal microRNA-24-3p enhances colon cancer
cell resistance to MTX by down-regulating CDX2/HEPH axis. J Cell
Mol Med. 25:3699–3713. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
205
|
Qin X, Guo H, Wang X, Zhu X, Yan M, Wang
X, Xu Q, Shi J, Lu E, Chen W and Zhang J: Exosomal miR-196a derived
from cancer-associated fibroblasts confers cisplatin resistance in
head and neck cancer through targeting CDKN1B and ING5. Genome
Biol. 20:122019. View Article : Google Scholar : PubMed/NCBI
|
|
206
|
Yang H, Villani RM, Wang H, Simpson MJ,
Roberts MS, Tang M and Liang X: The role of cellular reactive
oxygen species in cancer chemotherapy. J Exp Clin Cancer Res.
37:2662018. View Article : Google Scholar : PubMed/NCBI
|
|
207
|
Zhou X, Tong Y, Yu C, Pu J, Zhu W, Zhou Y,
Wang Y, Xiong Y and Sun X: FAP positive cancer-associated
fibroblasts promote tumor progression and radioresistance in
esophageal squamous cell carcinoma by transferring exosomal lncRNA
AFAP1-AS1. Mol Carcinog. 63:1922–1937. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
208
|
Zhang X, Zheng S, Hu C, Li G, Lin H, Xia
R, Ye Y, He R, Li Z, Lin Q, et al: Cancer-associated
fibroblast-induced lncRNA UPK1A-AS1 confers platinum resistance in
pancreatic cancer via efficient double-strand break repair.
Oncogene. 41:2372–2389. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
209
|
Zhang C, Liu X, Jin S, Chen Y and Guo R:
Ferroptosis in cancer therapy: A novel approach to reversing drug
resistance. Mol Cancer. 21:472022. View Article : Google Scholar : PubMed/NCBI
|
|
210
|
Dixon SJ, Lemberg KM, Lamprecht MR, Skouta
R, Zaitsev EM, Gleason CE, Patel DN, Bauer AJ, Cantley AM, Yang WS,
et al: Ferroptosis: An iron-dependent form of nonapoptotic cell
death. Cell. 149:1060–1072. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
211
|
Tang L, Zhang Y, Qian Z and Shen X: The
mechanism of Fe(2+)-initiated lipid peroxidation in liposomes: The
dual function of ferrous ions, the roles of the pre-existing lipid
peroxides and the lipid peroxyl radical. Biochem J. 352:27–36.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
212
|
Dixon SJ and Stockwell BR: The role of
iron and reactive oxygen species in cell death. Nat Chem Biol.
10:9–17. 2014. View Article : Google Scholar
|
|
213
|
Maiorino M, Conrad M and Ursini F: GPx4,
lipid peroxidation, and cell death: Discoveries, rediscoveries, and
open issues. Antioxid Redox Signal. 29:61–74. 2018. View Article : Google Scholar
|
|
214
|
Yang WS, SriRamaratnam R, Welsch ME,
Shimada K, Skouta R, Viswanathan VS, Cheah JH, Clemons PA, Shamji
AF, Clish CB, et al: Regulation of ferroptotic cancer cell death by
GPX4. Cell. 156:317–331. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
215
|
Li J, Li Y, Wang D, Liao R and Wu Z: PLAG1
interacts with GPX4 to conquer vulnerability to sorafenib induced
ferroptosis through a PVT1/miR-195-5p axis-dependent manner in
hepatocellular carcinoma. J Exp Clin Cancer Res. 43:1432024.
View Article : Google Scholar : PubMed/NCBI
|
|
216
|
Chen X, Li J, Kang R, Klionsky DJ and Tang
D: Ferroptosis: Machinery and regulation. Autophagy. 17:2054–2081.
2021. View Article : Google Scholar :
|
|
217
|
Zhao J, Yang S, Lv C and Liu Y:
Cancer-associated fibroblasts suppressed ferroptosis in
glioblastoma via upregulating lncRNA DLEU1. Am J Physiol Cell
Physiol. 324:C1039–C1052. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
218
|
Wang L, Liu Y, Du T, Yang H, Lei L, Guo M,
Ding HF, Zhang J, Wang H, Chen X and Yan C: ATF3 promotes
erastin-induced ferroptosis by suppressing system Xc. Cell Death
Differ. 27:662–675. 2020. View Article : Google Scholar
|
|
219
|
Qu X, Liu B, Wang L, Liu L, Zhao W, Liu C,
Ding J, Zhao S, Xu B, Yu H, et al: Loss of cancer-associated
fibroblast-derived exosomal DACT3-AS1 promotes malignant
transformation and ferroptosis-mediated oxaliplatin resistance in
gastric cancer. Drug Resist Updat. 68:1009362023. View Article : Google Scholar : PubMed/NCBI
|
|
220
|
Chen X, Wang Z, Li C, Zhang Z, Lu S, Wang
X, Liang Q, Zhu X, Pan C, Wang Q, et al: SIRT1 activated by AROS
sensitizes glioma cells to ferroptosis via induction of NAD+
depletion-dependent activation of ATF3. Redox Biol. 69:1030302024.
View Article : Google Scholar : PubMed/NCBI
|
|
221
|
Zhang T, Yao C, Zhou X, Liu S, Qi L, Zhu
S, Zhao C, Hu D and Shen W: Glutathione-degrading enzymes in the
complex landscape of tumors (review). Int J Oncol. 65:722024.
View Article : Google Scholar :
|
|
222
|
Ma XH, Liu JH, Liu CY, Sun WY, Duan WJ,
Wang G, Kurihara H, He RR, Li YF, Chen Y and Shang H:
ALOX15-launched PUFA-phospholipids peroxidation increases the
susceptibility of ferroptosis in ischemia-induced myocardial
damage. Signal Transduct Target Ther. 7:2882022. View Article : Google Scholar : PubMed/NCBI
|
|
223
|
Ding K, Liu C, Li L, Yang M, Jiang N, Luo
S and Sun L: Acyl-CoA synthase ACSL4: An essential target in
ferroptosis and fatty acid metabolism. Chin Med J (Engl).
136:2521–2537. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
224
|
Zhang H, Deng T, Liu R, Ning T, Yang H,
Liu D, Zhang Q, Lin D, Ge S, Bai M, et al: CAF secreted miR-522
suppresses ferroptosis and promotes acquired chemo-resistance in
gastric cancer. Mol Cancer. 19:432020. View Article : Google Scholar : PubMed/NCBI
|
|
225
|
Pan G, Liu Y, Shang L, Zhou F and Yang S:
EMT-associated microRNAs and their roles in cancer stemness and
drug resistance. Cancer Commun (Lond). 41:199–217. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
226
|
Du B and Shim JS: Targeting
epithelial-mesenchymal transition (EMT) to overcome drug resistance
in cancer. Molecules. 21:9652016. View Article : Google Scholar : PubMed/NCBI
|
|
227
|
Erin N, Grahovac J, Brozovic A and Efferth
T: Tumor microenvironment and epithelial mesenchymal transition as
targets to overcome tumor multidrug resistance. Drug Resist Updat.
53:1007152020. View Article : Google Scholar : PubMed/NCBI
|
|
228
|
Hu JL, Wang W, Lan XL, Zeng ZC, Liang YS,
Yan YR, Song FY, Wang FF, Zhu XH, Liao WJ, et al: CAFs secreted
exosomes promote metastasis and chemotherapy resistance by
enhancing cell stemness and epithelial-mesenchymal transition in
colorectal cancer. Mol Cancer. 18:912019. View Article : Google Scholar : PubMed/NCBI
|
|
229
|
Li N, Babaei-Jadidi R, Lorenzi F,
Spencer-Dene B, Clarke P, Domingo E, Tulchinsky E, Vries RGJ, Kerr
D, Pan Y, et al: An FBXW7-ZEB2 axis links EMT and tumour
microenvironment to promote colorectal cancer stem cells and
chemoresistance. Oncogenesis. 8:132019. View Article : Google Scholar : PubMed/NCBI
|
|
230
|
Han G, Wu D, Yang Y, Li Z, Zhang J and Li
C: CrkL meditates CCL20/CCR6-induced EMT in gastric cancer.
Cytokine. 76:163–169. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
231
|
Hu JH, Tang HN and Wang YH:
Cancer-associated fibroblast exosome LINC00355 promotes
epithelial-mesenchymal transition and chemoresistance in colorectal
cancer through the miR-34b-5p/CRKL axis. Cancer Gene Ther.
31:259–272. 2024. View Article : Google Scholar
|
|
232
|
Zhang Y, Yin C, Wei C, Xia S, Qiao Z,
Zhang XW, Yu B, Zhou J and Wang R: Exosomal miR-625-3p secreted by
cancer-associated fibroblasts in colorectal cancer promotes EMT and
chemotherapeutic resistance by blocking the CELF2/WWOX pathway.
Pharmacol Res. 186:1065342022. View Article : Google Scholar : PubMed/NCBI
|
|
233
|
Khawaled S, Nigita G, Distefano R, Oster
S, Suh SS, Smith Y, Khalaileh A, Peng Y, Croce CM, Geiger T, et al:
Pleiotropic tumor suppressor functions of WWOX antagonize
metastasis. Signal Transduct Target Ther. 5:432020. View Article : Google Scholar : PubMed/NCBI
|
|
234
|
Kadioglu O, Saeed MEM, Munder M, Spuller
A, Greten HJ and Efferth T: Effect of ABC transporter expression
and mutational status on survival rates of cancer patients. Biomed
Pharmacother. 131:1107182020. View Article : Google Scholar : PubMed/NCBI
|
|
235
|
To KKW, Huang Z, Zhang H, Ashby CR Jr and
Fu L: Utilizing non-coding RNA-mediated regulation of ATP binding
cassette (ABC) transporters to overcome multidrug resistance to
cancer chemotherapy. Drug Resist Updat. 73:1010582024. View Article : Google Scholar : PubMed/NCBI
|
|
236
|
Luo G, Zhang Y, Wu Z, Zhang L, Liang C and
Chen X: Exosomal LINC00355 derived from cancer-associated
fibroblasts promotes bladder cancer cell resistance to cisplatin by
regulating miR-34b-5p/ABCB1 axis. Acta Biochim Biophys Sin
(Shanghai). 53:558–566. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
237
|
Zhang D, Ding L, Li Y, Ren J, Shi G, Wang
Y, Zhao S, Ni Y and Hou Y: Midkine derived from cancer-associated
fibroblasts promotes cisplatin-resistance via up-regulation of the
expression of lncRNA ANRIL in tumour cells. Sci Rep. 7:162312017.
View Article : Google Scholar : PubMed/NCBI
|
|
238
|
Kunou S, Shimada K, Takai M, Sakamoto A,
Aoki T, Hikita T, Kagaya Y, Iwamoto E, Sanada M, Shimada S, et al:
Exosomes secreted from cancer-associated fibroblasts elicit
anti-pyrimidine drug resistance through modulation of its
transporter in malignant lymphoma. Oncogene. 40:3989–4003. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
239
|
Cheng SH, Chiou HC, Wang JW and Lin MH:
Reciprocal regulation of cancer-associated fibroblasts and tumor
microenvironment in gastrointestinal cancer: Implications for
cancer dormancy. Cancers (Basel). 15:25132023. View Article : Google Scholar : PubMed/NCBI
|
|
240
|
Hulpke S and Tampé R: The MHC I loading
complex: A multitasking machinery in adaptive immunity. Trends
Biochem Sci. 38:412–420. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
241
|
Yao H, Huang C, Zou J, Liang W, Zhao Y,
Yang K, Zhong Z, Zhou S, Li J, Li Y, et al: Extracellular
vesicle-packaged lncRNA from cancer-associated fibroblasts promotes
immune evasion by downregulating HLA-A in pancreatic cancer. J
Extracell Vesicles. 13:e124842024. View Article : Google Scholar : PubMed/NCBI
|
|
242
|
Jiang Y, Wang K, Lu X, Wang Y and Chen J:
Cancer-associated fibroblasts-derived exosomes promote lung cancer
progression by OIP5-AS1/miR-142-5p/ PD-L1 axis. Mol Immunol.
140:47–58. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
243
|
Boussiotis VA: Molecular and biochemical
aspects of the PD-1 checkpoint pathway. N Engl J Med.
375:1767–1778. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
244
|
Shintani Y, Fujiwara A, Kimura T, Kawamura
T, Funaki S, Minami M and Okumura M: IL-6 Secreted from
cancer-associated fibroblasts mediates chemoresistance in NSCLC by
increasing epithelial-mesenchymal transition signaling. J Thorac
Oncol. 11:1482–1492. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
245
|
Cheteh EH, Sarne V, Ceder S, Bianchi J,
Augsten M, Rundqvist H, Egevad L, Östman A and Wiman KG:
Interleukin-6 derived from cancer-associated fibroblasts attenuates
the p53 response to doxorubicin in prostate cancer cells. Cell
Death Discov. 6:422020. View Article : Google Scholar : PubMed/NCBI
|
|
246
|
Lau EY, Lo J, Cheng BY, Ma MK, Lee JM, Ng
JK, Chai S, Lin CH, Tsang SY, Ma S, et al: Cancer-associated
fibroblasts regulate tumor-initiating cell plasticity in
hepatocellular carcinoma through c-Met/FRA1/HEY1 signaling. Cell
Rep. 15:1175–1189. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
247
|
Deying W, Feng G, Shumei L, Hui Z, Ming L
and Hongqing W: CAF-derived HGF promotes cell proliferation and
drug resistance by up-regulating the c-Met/PI3K/Akt and GRP78
signalling in ovarian cancer cells. Biosci Rep. 37:BSR201604702017.
View Article : Google Scholar : PubMed/NCBI
|
|
248
|
Wang B, Liu W, Liu C, Du K, Guo Z, Zhang
G, Huang Z, Lin S, Cen B, Tian Y, et al: Cancer-associated
fibroblasts promote radioresistance of breast cancer cells via the
HGF/c-met signaling pathway. Int J Radiat Oncol Biol Phys.
116:640–654. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
249
|
Wei L, Ye H, Li G, Lu Y, Zhou Q, Zheng S,
Lin Q, Liu Y, Li Z and Chen R: Cancer-associated fibroblasts
promote progression and gemcitabine resistance via the SDF-1/SATB-1
pathway in pancreatic cancer. Cell Death Dis. 9:10652018.
View Article : Google Scholar : PubMed/NCBI
|
|
250
|
Zhang F, Cui JY, Gao HF, Yu H, Gao FF,
Chen JL and Chen L: Cancer-associated fibroblasts induce
epithelial-mesenchymal transition and cisplatin resistance in
ovarian cancer via CXCL12/CXCR4 axis. Future Oncol. 16:2619–2633.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
251
|
Jin Y, Bian S, Wang H, Mo J, Fei H, Li L,
Chen T and Jiang H: CRMP2 derived from cancer associated
fibroblasts facilitates progression of ovarian cancer via
HIF-1α-glycolysis signaling pathway. Cell Death Dis. 13:6752022.
View Article : Google Scholar
|
|
252
|
Luo M, Luo Y, Mao N, Huang G, Teng C, Wang
H, Wu J, Liao X and Yang J: Cancer-associated fibroblasts
accelerate malignant progression of non-small cell lung cancer via
connexin 43-formed unidirectional gap junctional intercellular
communication. Cell Physiol Biochem. 51:315–336. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
253
|
Chelakkot C, Chelakkot VS, Shin Y and Song
K: Modulating glycolysis to improve cancer therapy. Int J Mol Sci.
24:26062023. View Article : Google Scholar : PubMed/NCBI
|
|
254
|
Ippolito L, Comito G, Parri M, Iozzo M,
Duatti A, Virgilio F, Lorito N, Bacci M, Pardella E, Sandrini G, et
al: Lactate rewires lipid metabolism and sustains a
metabolic-epigenetic axis in prostate cancer. Cancer Res.
82:1267–1282. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
255
|
Cao Y: Adipocyte and lipid metabolism in
cancer drug resistance. J Clin Invest. 129:3006–3017. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
256
|
Yang L, Achreja A, Yeung TL, Mangala LS,
Jiang D, Han C, Baddour J, Marini JC, Ni J, Nakahara R, et al:
Targeting stromal glutamine synthetase in tumors disrupts tumor
microenvironment-regulated cancer cell growth. Cell Metab.
24:685–700. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
257
|
Li J, Li Y, Fu L, Chen H, Du F, Wang Z,
Zhang Y, Huang Y, Miao J and Xiao Y: Targeting ncRNAs to overcome
metabolic reprogramming-mediated drug resistance in cancer
(review). Int J Oncol. 66:352025. View Article : Google Scholar :
|
|
258
|
Yang J, Shi X, Yang M, Luo J, Gao Q, Wang
X, Wu Y, Tian Y, Wu F and Zhou H: Glycolysis reprogramming in
cancer-associated fibroblasts promotes the growth of oral cancer
through the lncRNA H19/miR-675-5p/PFKFB3 signaling pathway. Int J
Oral Sci. 13:122021. View Article : Google Scholar : PubMed/NCBI
|
|
259
|
Tao S, Gao Y, Wang X, Wu C, Zhang Y, Zhu H
and Li J: CAF-derived exosomal LINC01711 promotes breast cancer
progression by activating the miR-4510/NELFE axis and enhancing
glycolysis. FASEB J. 39:e704712025. View Article : Google Scholar : PubMed/NCBI
|
|
260
|
Zhang C, Wang XY, Zhang P, He TC, Han JH,
Zhang R, Lin J, Fan J, Lu L, Zhu WW, et al: Cancer-derived exosomal
HSPC111 promotes colorectal cancer liver metastasis by
reprogramming lipid metabolism in cancer-associated fibroblasts.
Cell Death Dis. 13:572022. View Article : Google Scholar : PubMed/NCBI
|
|
261
|
Smith AG and Macleod KF: Autophagy, cancer
stem cells and drug resistance. J Pathol. 247:708–718. 2019.
View Article : Google Scholar :
|
|
262
|
Dikic I and Elazar Z: Mechanism and
medical implications of mammalian autophagy. Nat Rev Mol Cell Biol.
19:349–364. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
263
|
Zhu S, Mao J, Zhang X, Wang P, Zhou Y,
Tong J, Peng H, Yang B and Fu Q: CAF-derived exosomal lncRNA FAL1
promotes chemoresistance to oxaliplatin by regulating autophagy in
colorectal cancer. Dig Liver Dis. 56:330–342. 2024. View Article : Google Scholar
|
|
264
|
Towers CG, Wodetzki D and Thorburn A:
Autophagy and cancer: Modulation of cell death pathways and cancer
cell adaptations. J Cell Biol. 219:e2019090332020.
|
|
265
|
Liao JK, Zhou B, Zhuang XM, Zhuang PL,
Zhang DM and Chen WL: Cancer-associated fibroblasts confer
cisplatin resistance of tongue cancer via autophagy activation.
Biomed Pharmacother. 97:1341–1348. 2018. View Article : Google Scholar
|
|
266
|
Gao Q, Fang X, Chen Y, Li Z and Wang M:
Exosomal lncRNA UCA1 from cancer-associated fibroblasts enhances
chemoresistance in vulvar squamous cell carcinoma cells. J Obstet
Gynaecol Res. 47:73–87. 2021. View Article : Google Scholar
|
|
267
|
Chen X and Song E: Turning foes to
friends: Targeting cancer-associated fibroblasts. Nat Rev Drug
Discov. 18:99–115. 2019. View Article : Google Scholar
|
|
268
|
Chen B, Dragomir MP, Yang C, Li Q, Horst D
and Calin GA: Targeting non-coding RNAs to overcome cancer therapy
resistance. Signal Transduct Target Ther. 7:1212022. View Article : Google Scholar : PubMed/NCBI
|
|
269
|
Ran FA, Hsu PD, Lin CY, Gootenberg JS,
Konermann S, Trevino AE, Scott DA, Inoue A, Matoba S, Zhang Y and
Zhang F: Double nicking by RNA-guided CRISPR Cas9 for enhanced
genome editing specificity. Cell. 154:1380–1389. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
270
|
Shtam TA, Kovalev RA, Varfolomeeva EY,
Makarov EM, Kil YV and Filatov MV: Exosomes are natural carriers of
exogenous siRNA to human cells in vitro. Cell Commun Signal.
11:882013. View Article : Google Scholar : PubMed/NCBI
|
|
271
|
Kamali MJ, Salehi M, Fatemi S, Moradi F,
Khoshghiafeh A and Ahmadifard M: Locked nucleic acid LNA): A modern
approach to cancer diagnosis and treatment. Exp Cell Res.
423:1134422023. View Article : Google Scholar
|
|
272
|
Rupaimoole R and Slack FJ: MicroRNA
therapeutics: Towards a new era for the management of cancer and
other diseases. Nat Rev Drug Discov. 16:203–222. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
273
|
Kwok A, Raulf N and Habib N: Developing
small activating RNA as a therapeutic: Current challenges and
promises. Ther Deliv. 10:151–164. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
274
|
Zheng B, Mai Q, Jiang J and Zhou Q: The
therapeutic potential of small activating RNAs for colorectal
carcinoma. Curr Gene Ther. 19:140–146. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
275
|
Fu J, Dong H, Wu J and Jin Y: Emerging
progress of RNA-based antitumor therapeutics. Int J Biol Sci.
19:3159–3183. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
276
|
Guo W, Wu Z, Chen J, Guo S, You W, Wang S,
Ma J, Wang H, Wang X, Wang H, et al: Nanoparticle delivery of
miR-21-3p sensitizes melanoma to anti-PD-1 immunotherapy by
promoting ferroptosis. J Immunother Cancer. 10:e0043812022.
View Article : Google Scholar : PubMed/NCBI
|
|
277
|
Xin X, Kumar V, Lin F, Kumar V, Bhattarai
R, Bhatt VR, Tan C and Mahato RI: Redox-responsive nanoplatform for
codelivery of miR-519c and gemcitabine for pancreatic cancer
therapy. Sci Adv. 6:eabd67642020. View Article : Google Scholar : PubMed/NCBI
|
|
278
|
Li B, Shao H, Gao L, Li H, Sheng H and Zhu
L: Nano-drug co-delivery system of natural active ingredients and
chemotherapy drugs for cancer treatment: A review. Drug Deliv.
29:2130–2161. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
279
|
Tassone P, Di Martino MT, Arbitrio M,
Fiorillo L, Staropoli N, Ciliberto D, Cordua A, Scionti F, Bertucci
B, Salvino A, et al: Safety and activity of the first-in-class
locked nucleic acid (LNA) miR-221 selective inhibitor in refractory
advanced cancer patients: A first-in-human, phase 1, open-label,
dose-escalation study. J Hematol Oncol. 16:682023. View Article : Google Scholar : PubMed/NCBI
|
|
280
|
Beg MS, Brenner AJ, Sachdev J, Borad M,
Kang YK, Stoudemire J, Smith S, Bader AG, Kim S and Hong DS: Phase
I study of MRX34, a liposomal miR-34a mimic, administered twice
weekly in patients with advanced solid tumors. Invest New Drugs.
35:180–188. 2017. View Article : Google Scholar
|
|
281
|
Rasmussen LJH, Schultz M, Gaardsting A,
Ladelund S, Garred P, Iversen K, Eugen-Olsen J, Helms M, David KP,
Kjaer A, et al: Inflammatory biomarkers and cancer: CRP and suPAR
as markers of incident cancer in patients with serious nonspecific
symptoms and signs of cancer. Int J Cancer. 141:191–199. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
282
|
Zhu M, Gao Y, Zhu K, Yuan Y, Bai H and
Meng L: Exosomal miRNA as biomarker in cancer diagnosis and
prognosis: A review. Medicine (Baltimore). 103:e400822024.
View Article : Google Scholar : PubMed/NCBI
|
|
283
|
Montani F and Bianchi F: Circulating
cancer biomarkers: The macro-revolution of the Micro-RNA.
EBioMedicine. 5:4–6. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
284
|
Li C, Teixeira AF, Zhu HJ and Ten Dijke P:
Cancer associated-fibroblast-derived exosomes in cancer
progression. Mol Cancer. 20:1542021. View Article : Google Scholar : PubMed/NCBI
|
|
285
|
Xu W, Liu S, Ma L, Cheng L, Li Q, Qing L,
Yang Y and Dong Z: Identification of miRNA signature in
cancer-associated fibroblast to predict recurrent prostate cancer.
Comput Biol Med. 180:1089892024. View Article : Google Scholar : PubMed/NCBI
|
|
286
|
Alzhrani R, Alsaab HO, Petrovici A, Bhise
K, Vanamala K, Sau S, Krinock MJ and Iyer AK: Improving the
therapeutic efficiency of noncoding RNAs in cancers using targeted
drug delivery systems. Drug Discov Today. 25:718–730. 2020.
View Article : Google Scholar :
|
|
287
|
Winkle M, El-Daly SM, Fabbri M and Calin
GA: Noncoding RNA therapeutics-challenges and potential solutions.
Nat Rev Drug Discov. 20:629–651. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
288
|
Hong DS, Kang YK, Borad M, Sachdev J,
Ejadi S, Lim HY, Brenner AJ, Park K, Lee JL, Kim TY, et al: Phase 1
study of MRX34, a liposomal miR-34a mimic, in patients with
advanced solid tumours. Br J Cancer. 122:1630–1637. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
289
|
Patil S, Gao YG, Lin X, Li Y, Dang K, Tian
Y, Zhang WJ, Jiang SF, Qadir A and Qian AR: The development of
functional non-viral vectors for gene delivery. Int J Mol Sci.
20:54912019. View Article : Google Scholar : PubMed/NCBI
|
|
290
|
Yahya EB and Alqadhi AM: Recent trends in
cancer therapy: A review on the current state of gene delivery.
Life Sci. 269:1190872021. View Article : Google Scholar : PubMed/NCBI
|