|
1
|
Riley RS, June CH, Langer R and Mitchell
MJ: Delivery technologies for cancer immunotherapy. Nat Rev Drug
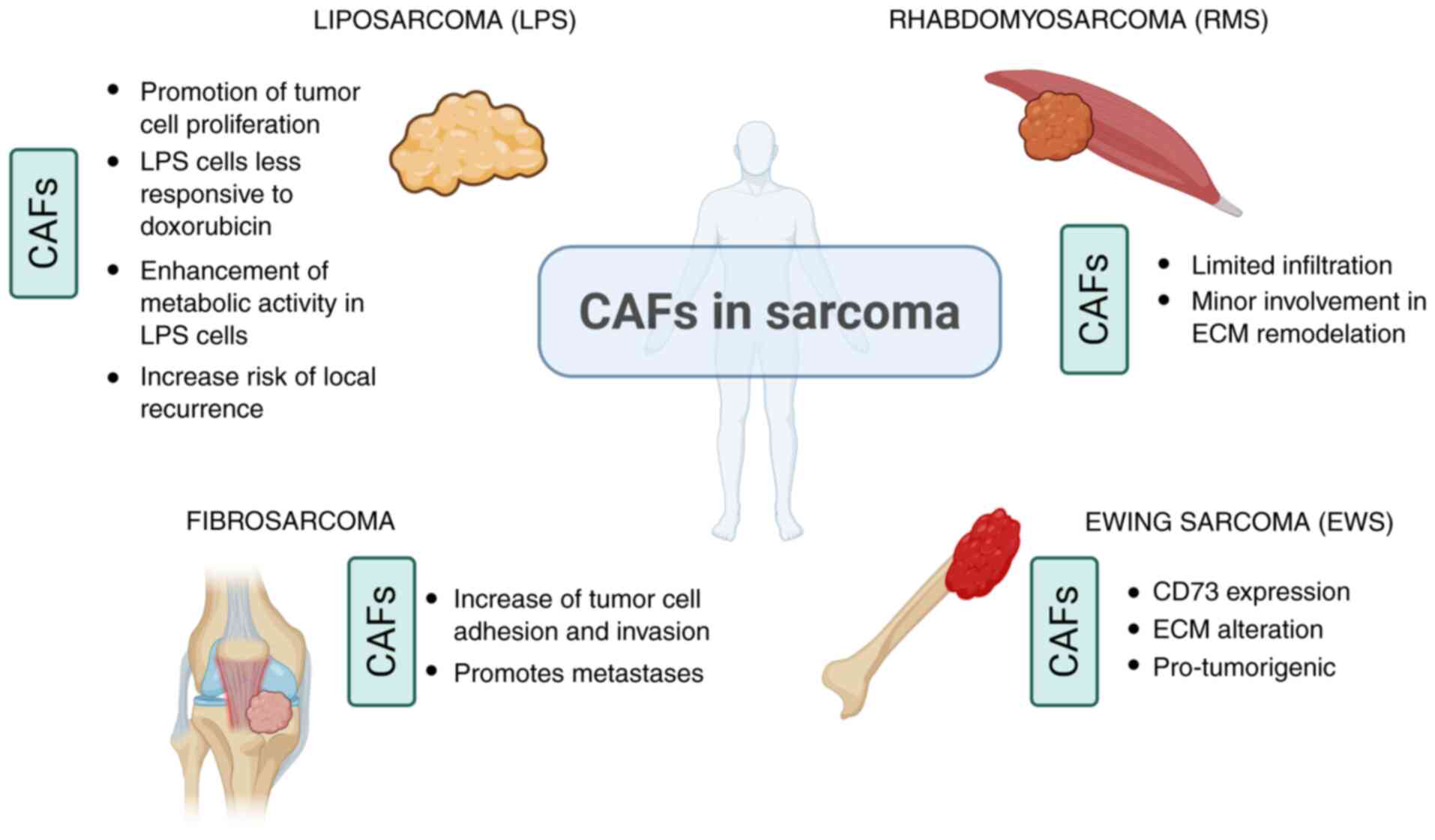
Discov. 18:175–196. 2019. View Article : Google Scholar : PubMed/NCBI
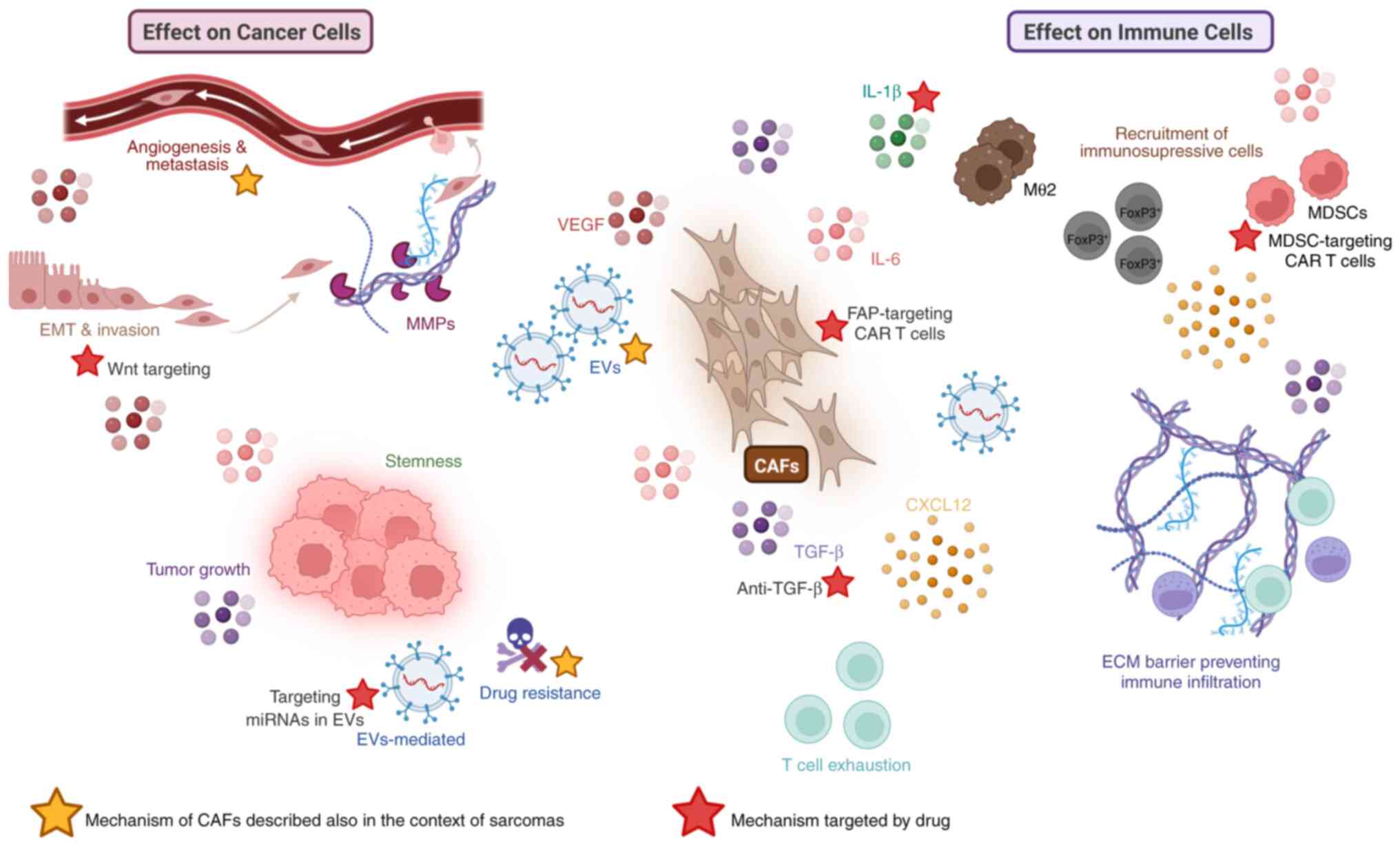
|
|
2
|
Mondal M, Guo J, He P and Zhou D: Recent
advances of oncolytic virus in cancer therapy. Hum Vaccin
Immunother. 16:2389–2402. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Soerjomataram I and Bray F: Planning for
tomorrow: Global cancer incidence and the role of prevention
2020-2070. Nat Rev Clin Oncol. 18:663–672. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Chen X and Song E: Turning foes to
friends: Targeting cancer-associated fibroblasts. Nat Rev Drug
Discov. 18:99–115. 2019. View Article : Google Scholar
|
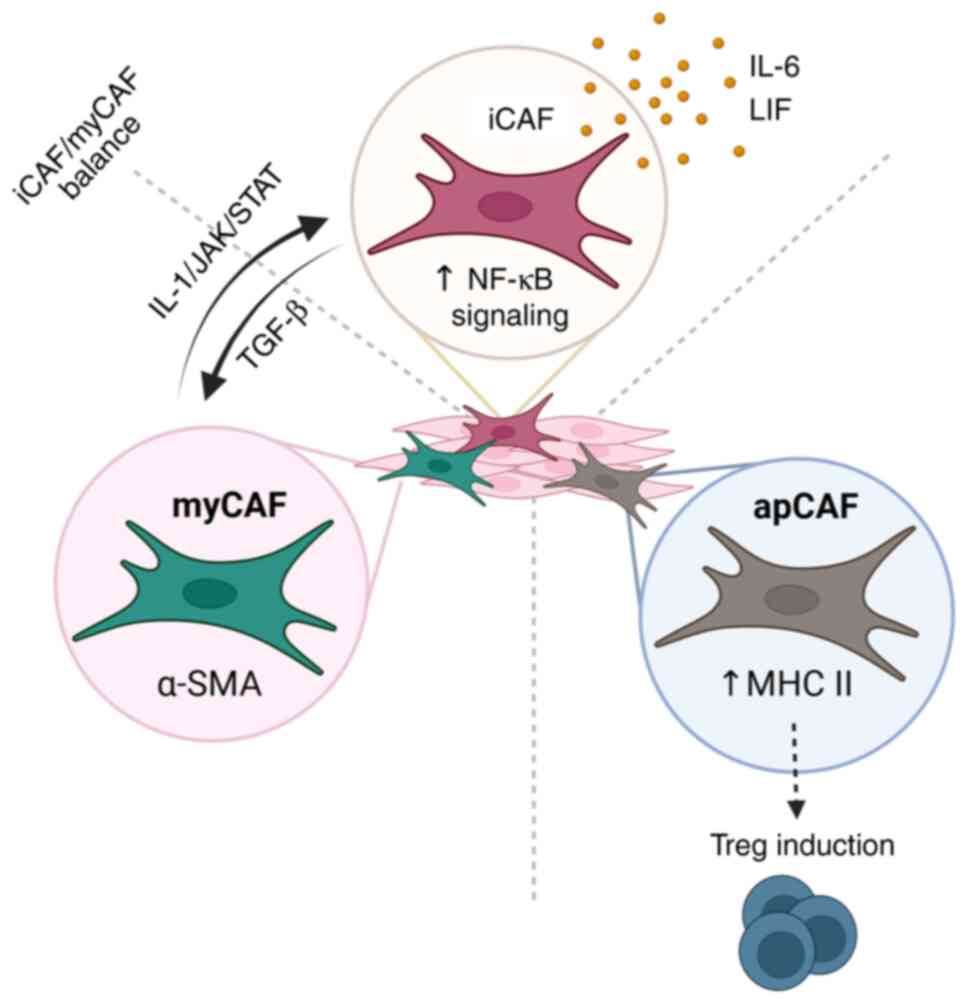
|
5
|
D'Agostino S, Tombolan L, Saggioro M,
Frasson C, Rampazzo E, Pellegrini S, Favaretto F, Biz C, Ruggieri
P, Gamba P, et al: Rhabdomyosarcoma cells produce their own
extracellular matrix with minimal involvement of Cancer-associated
fibroblasts: A preliminary study. Front Oncol. 10:6009802020.
View Article : Google Scholar
|
|
6
|
Sarkar M, Nguyen T, Gundre E, Ogunlusi O,
El-Sobky M, Giri B and Sarkar TR: Cancer-associated fibroblasts:
The chief architect in the tumor microenvironment. Front Cell Dev
Biol. 11:10890682023. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Pillozzi S, Bernini A, Palchetti I,
Crociani O, Antonuzzo L, Campanacci D and Scoccianti G: Soft tissue
sarcoma: An insight on biomarkers at molecular, metabolic and
cellular level. Cancers. 13:30442021. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sahai E, Astsaturov I, Cukierman E,
DeNardo DG, Egeblad M, Evans RM, Fearon D, Greten FR, Hingorani SR,
Hunter T, et al: A framework for advancing our understanding of
cancer-associated fibroblasts. Nat Rev Cancer. 20:174–186. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Maia A, Schollhorn A, Schuhmacher J and
Gouttefangeas C: CAF-immune cell crosstalk and its impact in
immunotherapy. Semin Immunopathol. 45:203–214. 2023. View Article : Google Scholar :
|
|
10
|
Kennel KB, Bozlar M, De Valk AF and Greten
FR: Cancer-associated fibroblasts in inflammation and antitumor
immunity. Clin Cancer Res. 29:1009–1016. 2023. View Article : Google Scholar :
|
|
11
|
Huang H, Wang Z, Zhang Y, Pradhan RN,
Ganguly D, Chandra R, Murimwa G, Wright S, Gu X, Maddipati R, et
al: Mesothelial cell-derived antigen-presenting cancer-associated
fibroblasts induce expansion of regulatory T cells in pancreatic
cancer. Cancer Cell. 40:656–673.e7. 2022. View Article : Google Scholar :
|
|
12
|
Kakarla S, Chow KK, Mata M, Shaffer DR,
Song XT, Wu MF, Liu H, Wang LL, Rowley DR, Pfizenmaier K and
Gottschalk S: Antitumor effects of chimeric receptor engineered
human T cells directed to tumor stroma. Mol Ther. 21:1611–1620.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Chen B, Chan WN, Xie F, Mui CW, Liu X,
Cheung AHK, Lung RWM, Chow C, Zhang Z, Fang C, et al: The molecular
classification of cancer-associated fibroblasts on a pan-cancer
single-cell transcriptional atlas. Clin Transl Med. 13:e15162023.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ohlund D, Elyada E and Tuveson D:
Fibroblast heterogeneity in the cancer wound. J Exp Med.
211:1503–1523. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Tsoumakidou M: The advent of immune
stimulating CAFs in cancer. Nat Rev Cancer. 23:258–269. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Choi KJ, Nam JK, Kim JH, Choi SH and Lee
YJ: Endothelial-to-mesenchymal transition in anticancer therapy and
normal tissue damage. Exp Mol Med. 52:781–792. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Lamouille S, Xu J and Derynck R: Molecular
mechanisms of epithelial-mesenchymal transition. Nat Rev Mol Cell
Biol. 15:178–196. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Taguchi A, Kawana K, Tomio K, Yamashita A,
Isobe Y, Nagasaka K, Koga K, Inoue T, Nishida H, Kojima S, et al:
Matrix metalloproteinase (MMP)-9 in cancer-associated fibroblasts
(CAFs) is suppressed by omega-3 polyunsaturated fatty acids in
vitro and in vivo. PLoS One. 9:e896052014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Cavazzoni A and Digiacomo G: Role of
cytokines and other soluble factors in tumor development: Rationale
for new therapeutic strategies. Cells. 12:25322023. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
O'Connell JT, Sugimoto H, Cooke VG,
MacDonald BA, Mehta AI, LeBleu VS, Dewar R, Rocha RM, Brentani RR,
Resnick MB, et al: VEGF-A and Tenascin-C produced by S100A4+
stromal cells are important for metastatic colonization. Proc Natl
Acad Sci USA. 108:16002–16007. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Liu T, Han C, Wang S, Fang P, Ma Z, Xu L
and Yin R: Cancer-associated fibroblasts: An emerging target of
Anti-cancer immunotherapy. J Hematol Oncol. 12:862019. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Robertson-Tessi M, Gillies RJ, Gatenby RA
and Anderson AR: Impact of metabolic heterogeneity on tumor growth,
invasion, and treatment outcomes. Cancer Res. 75:1567–1579. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Wu D, Zhuo L and Wang X: Metabolic
reprogramming of carcinoma-associated fibroblasts and its impact on
metabolic heterogeneity of tumors. Semin Cell Dev Biol. 64:125–131.
2017. View Article : Google Scholar
|
|
24
|
Martinez-Outschoorn UE, Lisanti MP and
Sotgia F: Catabolic cancer-associated fibroblasts transfer energy
and biomass to anabolic cancer cells, fueling tumor growth. Semin
Cancer Biol. 25:47–60. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
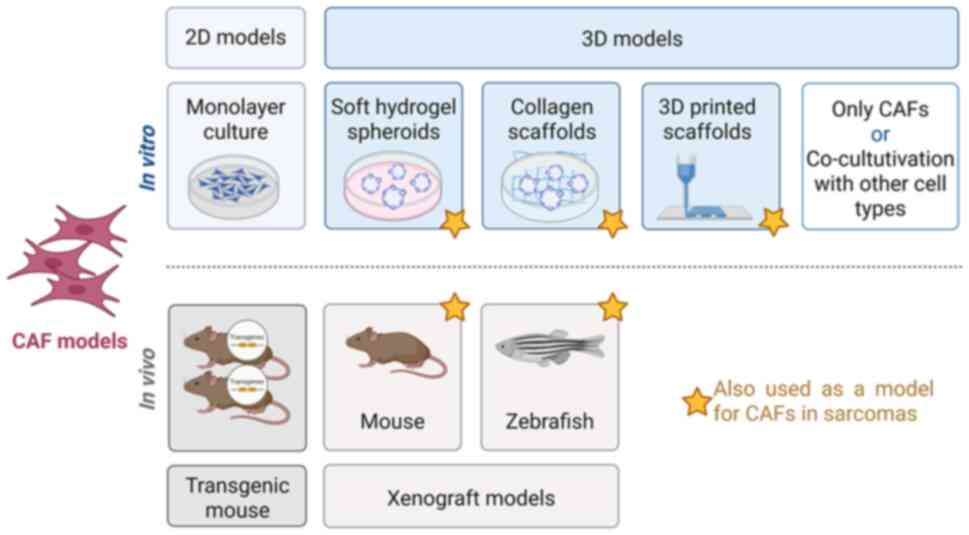
25
|
Tavares-Valente D, Baltazar F, Moreira R
and Queiros O: Cancer cell bioenergetics and pH regulation
influence breast cancer cell resistance to paclitaxel and
doxorubicin. J Bioenerg Biomembr. 45:467–475. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Guo Z, Zhang H, Fu Y, Kuang J, Zhao B,
Zhang L, Lin J, Lin S, Wu D and Xie G: Cancer-associated
fibroblasts induce growth and radioresistance of breast cancer
cells through paracrine IL-6. Cell Death Discov. 9:62023.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Yoshida GJ: Regulation of heterogeneous
cancer-associated fibroblasts: The molecular pathology of activated
signaling pathways. J Exp Clin Cancer Res. 39:1122020. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Biffi G, Oni TE, Spielman B, Hao Y, Elyada
E, Park Y, Preall J and Tuveson D: IL1-Induced JAK/STAT signaling
is antagonized by TGFβ to Shape CAF heterogeneity in pancreatic
ductal adenocarcinomacinoma. Cancer Discov. 9:282–301. 2019.
View Article : Google Scholar
|
|
29
|
Rimal R, Desai P, Daware R, Hosseinnejad
A, Prakash J, Lammers T and Singh S: Cancer-associated fibroblasts:
Origin, function, imaging, and therapeutic targeting. Adv Drug
Deliv Rev. 189:1145042022. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Strizova Z, Bartunkova J and Smrz D: The
challenges of adoptive cell transfer in the treatment of human
renal cell carcinoma. Cancer Immunol Immunother. 68:1831–1838.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Chen Y, Yang S, Tavormina J, Tampe D,
Zeisberg M, Wang H, Mahadevan KK, Wu CJ, Sugimoto H, Chang CC, et
al: Oncogenic collagen I homotrimers from cancer cells bind to α3β1
integrin and impact tumor microbiome and immunity to promote
pancreatic cancer. Cancer Cell. 40:818–834.e9. 2022. View Article : Google Scholar
|
|
32
|
Taborska P, Lukac P, Stakheev D,
Rajsiglova L, Kalkusova K, Strnadova K, Lacina L, Dvorankova B,
Novotny J, Kolar M, et al: Novel PD-L1- and collagen-expressing
patient-derived cell line of undifferentiated pleomorphic sarcoma
(JBT19) as a model for cancer immunotherapy. Sci Rep. 13:190792023.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Sun X, Wu B, Chiang HC, Deng H, Zhang X,
Xiong W, Liu J, Rozeboom AM, Harris BT, Blommaert E, et al: Tumour
DDR1 promotes collagen fibre alignment to instigate immune
exclusion. Nature. 599:673–678. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Meyaard L: The inhibitory collagen
receptor LAIR-1 (CD305). J Leukoc Biol. 83:799–803. 2008.
View Article : Google Scholar
|
|
35
|
Horn LA, Chariou PL, Gameiro SR, Qin H,
Iida M, Fousek K, Meyer TJ, Cam M, Flies D, Langermann S, et al:
Remodeling the tumor microenvironment via blockade of LAIR-1 and
TGF-β signaling enables PD-L1-mediated tumor eradication. J Clin
Invest. 132:e1551482022. View Article : Google Scholar
|
|
36
|
Cheng Y, Li H, Deng Y, Tai Y, Zeng K,
Zhang Y, Liu W, Zhang Q and Yang Y: Cancer-associated fibroblasts
induce PDL1+ neutrophils through the IL6-STAT3 pathway that foster
immune suppression in hepatocellular carcinoma. Cell Death Dis.
9:4222018. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Cao H, Cheng HS, Wang JK, Tan NS and Tay
CY: A 3D physio-mimetic interpenetrating network-based platform to
decode the pro and anti-tumorigenic properties of cancer-associated
fibroblasts. Acta Biomater. 132:448–460. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Ozdemir BC, Pentcheva-Hoang T, Carstens
JL, Zheng X, Wu CC, Simpson TR, Laklai H, Sugimoto H, Kahlert C,
Novitskiy SV, et al: Depletion of carcinoma-associated fibroblasts
and fibrosis induces immunosuppression and accelerates pancreas
cancer with reduced survival. Cancer Cell. 25:719–734. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Rhim AD, Oberstein PE, Thomas DH, Mirek
ET, Palermo CF, Sastra SA, Dekleva EN, Saunders T, Becerra CP,
Tattersall IW, et al: Stromal elements act to restrain, rather than
support, pancreatic ductal adenocarcinoma. Cancer Cell. 25:735–747.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Alkasalias T, Flaberg E, Kashuba V,
Alexeyenko A, Pavlova T, Savchenko A, Szekely L, Klein G and Guven
H: Inhibition of tumor cell proliferation and motility by
fibroblasts is both contact and soluble factor dependent. Proc Natl
Acad Sci USA. 111:17188–17193. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Gorchs L, Ahmed S, Mayer C, Knauf A,
Fernández Moro C, Svensson M, Heuchel R, Rangelova E, Bergman P and
Kaipe H: The vitamin D analogue calcipotriol promotes an
anti-tumorigenic phenotype of human pancreatic CAFs but reduces T
cell mediated immunity. Sci Rep. 10:174442020. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Mao X, Xu J, Wang W, Liang C, Hua J, Liu
J, Zhang B, Meng Q, Yu X and Shi S: Crosstalk between
cancer-associated fibroblasts and immune cells in the tumor
microenvironment: New findings and future perspectives. Mol Cancer.
20:1312021. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Bartoschek M, Oskolkov N, Bocci M, Lövrot
J, Larsson C, Sommarin M, Madsen CD, Lindgren D, Pekar G, Karlsson
G, et al: Spatially and functionally distinct subclasses of breast
cancer-associated fibroblasts revealed by single cell RNA
sequencing. Nat Commun. 9:51502018. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Newman L: Oncologic anthropology: Global
variations in breast cancer risk, biology, and outcome. J Surg
Oncol. 128:959–966. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Ma J, Chan JJ, Toh CH and Yap YS: Emerging
systemic therapy options beyond CDK4/6 inhibitors for hormone
receptor-positive HER2-negative advanced breast cancer. NPJ Breast
Cancer. 9:742023. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Pandey K, Katuwal NB, Park N, Hur J, Cho
YB, Kim SK, Lee SA, Kim I, Lee SR and Moon YW: Combination of
abemaciclib following eribulin overcomes Palbociclib-resistant
breast cancer by inhibiting the G2/M cell cycle phase. Cancers
(Basel). 14:2102022. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Piwocka O, Musielak M, Piotrowski I,
Kulcenty K, Adamczyk B, Fundowicz M, Suchorska WM and Malicki J:
Primary cancer-associated fibroblasts exhibit high heterogeneity
among breast cancer subtypes. Rep Pract Oncol Radiother.
28:159–171. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Kieffer Y, Hocine HR, Gentric G, Pelon F,
Bernard C, Bourachot B, Lameiras S, Albergante L, Bonneau C, Guyard
A, et al: Single-cell analysis reveals fibroblast clusters linked
to immunotherapy resistance in cancer. Cancer Discov. 10:1330–1351.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Yamashita M, Ogawa T, Zhang X, Hanamura N,
Kashikura Y, Takamura M, Yoneda M and Shiraishi T: Role of stromal
myofibroblasts in invasive breast cancer: Stromal expression of
alpha-smooth muscle actin correlates with worse clinical outcome.
Breast Cancer. 19:170–176. 2012. View Article : Google Scholar
|
|
50
|
Pelon F, Bourachot B, Kieffer Y, Magagna
I, Mermet-Meillon F, Bonnet I, Costa A, Givel AM, Attieh Y,
Barbazan J, et al: Cancer-associated fibroblast heterogeneity in
axillary lymph nodes drives metastases in breast cancer through
complementary mechanisms. Nat Commun. 11:4042020. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Ershaid N, Sharon Y, Doron H, Raz Y, Shani
O, Cohen N, Monteran L, Leider-Trejo L, Ben-Shmuel A, Yassin M, et
al: NLRP3 inflammasome in fibroblasts links tissue damage with
inflammation in breast cancer progression and metastasis. Nat
Commun. 10:43752019. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Yang SS, Ma S, Dou H, Liu F, Zhang SY,
Jiang C, Xiao M and Huang YX: Breast cancer-derived exosomes
regulate cell invasion and metastasis in breast cancer via miR-146a
to activate cancer associated fibroblasts in tumor
microenvironment. Exp Cell Res. 391:1119832020. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Ren J, Smid M, Iaria J, Salvatori DCF, van
Dam H, Zhu HJ, Martens JWM and Ten Dijke P: Cancer-associated
fibroblast-derived Gremlin 1 promotes breast cancer progression.
Breast Cancer Res. 21:1092019. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Wu HJ, Hao M, Yeo SK and Guan JL: FAK
signaling in cancer-associated fibroblasts promotes breast cancer
cell migration and metastasis by exosomal miRNAs-mediated
intercellular communication. Oncogene. 39:2539–2549. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Chatterjee A, Jana S, Chatterjee S,
Wastall LM, Mandal G, Nargis N, Roy H, Hughes TA and Bhattacharyya
A: MicroRNA-222 reprogrammed cancer-associated fibroblasts enhance
growth and metastasis of breast cancer. Br J Cancer. 121:679–689.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Mizrahi JD, Surana R, Valle JW and Shroff
RT: Pancreatic cancer. Lancet. 395:2008–2020. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Sohal DPS, Kennedy EB, Cinar P, Conroy T,
Copur MS, Crane CH, Garrido-Laguna I, Lau MW, Johnson T,
Krishnamurthi S, et al: Metastatic pancreatic cancer: ASCO
guideline update. J Clin Oncol. 38:3217–3230. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Bekkali NLH and Oppong KW: Pancreatic
ductal adenocarcinoma epidemiology and risk assessment: Could we
prevent? Possibility for an early diagnosis. Endosc Ultrasound.
6(Suppl 3): S58–S61. 2017. View Article : Google Scholar
|
|
59
|
Hosein AN, Brekken RA and Maitra A:
Pancreatic cancer stroma: An update on therapeutic targeting
strategies. Nat Rev Gastroenterol Hepatol. 17:487–505. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Manoukian P, Bijlsma M and van Laarhoven
H: The cellular origins of Cancer-associated fibroblasts and their
opposing contributions to pancreatic cancer growth. Front Cell Dev
Biol. 9:7439072021. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Geng X, Chen H, Zhao L, Hu J, Yang W, Li
G, Cheng C, Zhao Z, Zhang T, Li L and Sun B: Cancer-associated
fibroblast (CAF) heterogeneity and targeting therapy of CAFs in
pancreatic cancer. Front Cell Dev Biol. 9:6551522021. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Ohlund D, Handly-Santana A, Biffi G,
Elyada E, Almeida AS, Ponz-Sarvise M, Corbo V, Oni TE, Hearn SA,
Lee EJ, et al: Distinct populations of inflammatory fibroblasts and
myofibroblasts in pancreatic cancer. J Exp Med. 214:579–596. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Kim HW, Lee JC, Paik KH, Kang J, Kim J and
Hwang JH: Serum interleukin-6 is associated with pancreatic ductal
adenocarcinoma progression pattern. Medicine (Baltimore).
96:e59262017. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Goulet CR, Champagne A, Bernard G, Vandal
D, Chabaud S, Pouliot F and Bolduc S: Cancer-associated fibroblasts
induce epithelial-mesenchymal transition of bladder cancer cells
through paracrine IL-6 signalling. BMC Cancer. 19:1372019.
View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Mirzaei S, Saghari S, Bassiri F, Raesi R,
Zarrabi A, Hushmandi K, Sethi G and Tergaonkar V: NF-κB as a
regulator of cancer metastasis and therapy response: A focus on
epithelial-mesenchymal transition. J Cell Physiol. 237:2770–2795.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Rebelo R, Xavier CPR, Giovannetti E and
Vasconcelos MH: Fibroblasts in pancreatic cancer: Molecular and
clinical perspectives. Trends Mol Med. 29:439–453. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Richards KE, Zeleniak AE, Fishel ML, Wu J,
Littlepage LE and Hill R: Cancer-associated fibroblast exosomes
regulate survival and proliferation of pancreatic cancer cells.
Oncogene. 36:1770–1778. 2017. View Article : Google Scholar :
|
|
68
|
Aronsson L, Bengtsson A, Toren W,
Andersson R and Ansari D: Intraductal papillary mucinous carcinoma
versus pancreatic ductal adenocarcinoma: A systematic review and
meta-analysis. Int J Surg. 71:91–99. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Aronsson L, Andersson R and Ansari D:
Intraductal papillary mucinous neoplasm of the
pancreas-epidemiology, risk factors, diagnosis, and management.
Scand J Gastroenterol. 52:803–815. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Bernard V, Semaan A, Huang J, San Lucas
FA, Mulu FC, Stephens BM, Guerrero PA, Huang Y, Zhao J, Kamyabi N,
et al: Single-cell transcriptomics of pancreatic cancer precursors
demonstrates epithelial and microenvironmental heterogeneity as an
early event in neoplastic progression. Clin Cancer Res.
25:2194–2205. 2019. View Article : Google Scholar
|
|
71
|
Storandt MH, Zemla TM, Patell K, Naleid N,
Gile JJ, Tran NH, Chakrabarti S, Jin Z, Borad M and Mahipal A:
Atezolizumab plus bevacizumab as first-line systemic therapy for
hepatocellular carcinoma: A multi-institutional cohort study.
Oncologist. 29:986–996. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Selene II, Ozen M and Patel RA:
Hepatocellular carcinoma: Advances in systemic therapy. Semin
Intervent Radiol. 41:56–62. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Singal AG, Llovet JM, Yarchoan M, Mehta N,
Heimbach JK, Dawson LA, Jou JH, Kulik LM, Agopian VG, Marrero JA,
et al: AASLD practice guidance on prevention, diagnosis, and
treatment of hepatocellular carcinoma. Hepatology. 78:1922–1965.
2023. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Loh JJ, Li TW, Zhou L, Wong TL, Liu X, Ma
VWS, Lo CM, Man K, Lee TK, Ning W, et al: FSTL1 secreted by
activated fibroblasts promotes hepatocellular carcinoma metastasis
and stemness. Cancer Res. 81:5692–5705. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Liu J, Chen S, Wang W, Ning BF, Chen F,
Shen W, Ding J, Chen W, Xie WF, Zhang X, et al: Cancer-associated
fibroblasts promote hepatocellular carcinoma metastasis through
chemokine-activated hedgehog and TGF-β pathways. Cancer Lett.
379:49–59. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Jia CC, Wang TT, Liu W, Fu BS, Hua X, Wang
GY, Li TJ, Li X, Wu XY, Tai Y, et al: Cancer-associated fibroblasts
from hepatocellular carcinoma promote malignant cell proliferation
by HGF secretion. PLoS One. 8:e632432013. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Xiong S, Wang R, Chen Q, Luo J, Wang J,
Zhao Z, Li Y, Wang Y, Wang X and Cheng B: Cancer-associated
fibroblasts promote stem cell-like properties of hepatocellular
carcinoma cells through IL-6/STAT3/Notch signaling. Am J Cancer
Res. 8:302–316. 2018.PubMed/NCBI
|
|
78
|
Li Y, Wang R, Xiong S, Wang X, Zhao Z, Bai
S, Wang Y, Zhao Y and Cheng B: Cancer-associated fibroblasts
promote the stemness of CD24+ liver cells via paracrine signaling.
J Mol Med (Berl). 97:243–255. 2019. View Article : Google Scholar
|
|
79
|
Zhu GQ, Tang Z, Huang R, Qu WF, Fang Y,
Yang R, Tao CY, Gao J, Wu XL, Sun HX, et al: CD36+
cancer-associated fibroblasts provide immunosuppressive
microenvironment for hepatocellular carcinoma via secretion of
macrophage migration inhibitory factor. Cell Discov. 9:252023.
View Article : Google Scholar :
|
|
80
|
Eun JW, Yoon JH, Ahn HR, Kim S, Kim YB,
Lim SB, Park W, Kang TW, Baek GO, Yoon MG, et al: Cancer-associated
fibroblast-derived secreted phosphoprotein 1 contributes to
resistance of hepatocellular carcinoma to sorafenib and lenvatinib.
Cancer Commun (Lond). 43:455–479. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Xia S, Pan Y, Liang Y, Xu J and Cai X: The
microenvironmental and metabolic aspects of sorafenib resistance in
hepatocellular carcinoma. EBioMedicine. 51:1026102020. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Yu L, Liu Q, Huo J, Wei F and Guo W:
Cancer-associated fibroblasts induce immunotherapy resistance in
hepatocellular carcinoma animal model. Cell Mol Biol
(Noisy-le-Grand). 66:36–40. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Lotfollahzadeh S, Recio-Boiles A and Cagir
B: Colon cancer. StatPearls. Treasure Island (FL) with ineligible
companies. Disclosure: Alejandro Recio-Boiles declares no relevant
financial relationships with ineligible companies. Disclosure: Burt
Cagir declares no relevant financial relationships with ineligible
companies.2024.
|
|
84
|
Constantinou V and Constantinou C:
Focusing on colorectal cancer in young adults (Review). Mol Clin
Oncol. 20:82024. View Article : Google Scholar
|
|
85
|
Siegel RL, Wagle NS, Cercek A, Smith RA
and Jemal A: Colorectal cancer statistics, 2023. CA Cancer J Clin.
73:233–254. 2023.PubMed/NCBI
|
|
86
|
Zeineddine FA, Zeineddine MA, Yousef A, Gu
Y, Chowdhury S, Dasari A, Huey RW, Johnson B, Kee B, Lee MS, et al:
Survival improvement for patients with metastatic colorectal cancer
over twenty years. NPJ Precis Oncol. 7:162023. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Morris VK, Kennedy EB, Baxter NN, Benson
AB III, Cercek A, Cho M, Ciombor KK, Cremolini C, Davis A, Deming
DA, et al: Treatment of metastatic colorectal cancer: ASCO
Guideline. J Clin Oncol. 41:678–700. 2023. View Article : Google Scholar
|
|
88
|
Deng L, Jiang N, Zeng J, Wang Y and Cui H:
The versatile roles of Cancer-associated fibroblasts in colorectal
cancer and therapeutic implications. Front Cell Dev Biol.
9:7332702021. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Wikberg ML, Edin S, Lundberg IV, Van
Guelpen B, Dahlin AM, Rutegård J, Stenling R, Oberg A and Palmqvist
R: High intratumoral expression of fibroblast activation protein
(FAP) in colon cancer is associated with poorer patient prognosis.
Tumour Biol. 34:1013–1020. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Hu JL, Wang W, Lan XL, Zeng ZC, Liang YS,
Yan YR, Song FY, Wang FF, Zhu XH, Liao WJ, et al: CAFs secreted
exosomes promote metastasis and chemotherapy resistance by
enhancing cell stemness and epithelial-mesenchymal transition in
colorectal cancer. Mol Cancer. 18:912019. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Aizawa T, Karasawa H, Funayama R, Shirota
M, Suzuki T, Maeda S, Suzuki H, Yamamura A, Naitoh T, Nakayama K
and Unno M: Cancer-associated fibroblasts secrete Wnt2 to promote
cancer progression in colorectal cancer. Cancer Med. 8:6370–6382.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Siegel RL, Giaquinto AN and Jemal A:
Cancer statistics, 2024. CA Cancer J Clin. 74:12–49.
2024.PubMed/NCBI
|
|
93
|
Gridelli C, Rossi A, Carbone DP, Guarize
J, Karachaliou N, Mok T, Petrella F, Spaggiari L and Rosell R:
Non-small-cell lung cancer. Nat Rev Dis Primers. 1:150092015.
View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Herbst RS, Morgensztern D and Boshoff C:
The biology and management of Non-small cell lung cancer. Nature.
553:446–454. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Kim SH, Choe C, Shin YS, Jeon MJ, Choi SJ,
Lee J, Bae GY, Cha HJ and Kim J: Human lung cancer-associated
fibroblasts enhance motility of Non-small cell lung cancer cells in
co-culture. Anticancer Res. 33:2001–2009. 2013.PubMed/NCBI
|
|
96
|
An J, Enomoto A, Weng L, Kato T, Iwakoshi
A, Ushida K, Maeda K, Ishida-Takagishi M, Ishii G, Ming S, et al:
Significance of cancer-associated fibroblasts in the regulation of
gene expression in the leading cells of invasive lung cancer. J
Cancer Res Clin Oncol. 139:379–388. 2013. View Article : Google Scholar
|
|
97
|
Chen WJ, Ho CC, Chang YL, Chen HY, Lin CA,
Ling TY, Yu SL, Yuan SS, Chen YJ, Lin CY, et al: Cancer-associated
fibroblasts regulate the plasticity of lung cancer stemness via
paracrine signalling. Nat Commun. 5:34722014. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Wang L, Cao L, Wang H, Liu B, Zhang Q,
Meng Z, Wu X, Zhou Q and Xu K: Cancer-associated fibroblasts
enhance metastatic potential of lung cancer cells through
IL-6/STAT3 signaling pathway. Oncotarget. 8:76116–76128. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Vicent S, Sayles LC, Vaka D, Khatri P,
Gevaert O, Chen R, Zheng Y, Gillespie AK, Clarke N, Xu Y, et al:
Cross-species functional analysis of cancer-associated fibroblasts
identifies a critical role for CLCF1 and IL-6 in non-small cell
lung cancer in vivo. Cancer Res. 72:5744–5756. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Yang F, Yan Y, Yang Y, Hong X, Wang M,
Yang Z, Liu B and Ye L: MiR-210 in exosomes derived from CAFs
promotes non-small cell lung cancer migration and invasion through
PTEN/PI3K/AKT pathway. Cell Signal. 73:1096752020. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Xiang H, Ramil CP, Hai J, Zhang C, Wang H,
Watkins AA, Afshar R, Georgiev P, Sze MA, Song XS, et al:
Cancer-associated fibroblasts promote immunosuppression by inducing
ROS-generating monocytic MDSCs in lung squamous cell carcinoma.
Cancer Immunol Res. 8:436–450. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Kanwal B, Biswas S, Seminara RS and Jeet
C: Immunotherapy in advanced Non-small cell lung cancer patients:
Ushering chemotherapy through the checkpoint inhibitors? Cureus.
10:e32542018.PubMed/NCBI
|
|
103
|
Herzog BH, Baer JM, Borcherding N,
Kingston NL, Belle JI, Knolhoff BL, Hogg GD, Ahmad F, Kang LI,
Petrone J, et al: Tumor-associated fibrosis impairs immune
surveillance and response to immune checkpoint blockade in
non-small cell lung cancer. Sci Transl Med. 15:eadh80052023.
View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Jenkins L, Jungwirth U, Avgustinova A,
Iravani M, Mills A, Haider S, Harper J and Isacke CM:
Cancer-associated fibroblasts suppress CD8+ T-cell infiltration and
confer resistance to Immune-checkpoint blockade. Cancer Res.
82:2904–2917. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Tauriello DVF: Targeting CAFs to improve
Anti-PD-1 checkpoint immunotherapy. Cancer Res. 83:655–656. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Shintani Y, Kimura T, Funaki S, Ose N,
Kanou T and Fukui E: Therapeutic targeting of Cancer-associated
fibroblasts in the Non-small cell lung cancer tumor
microenvironment. Cancers (Basel). 15:3352023. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Li M, Wu B, Li L, Lv C and Tian Y:
Reprogramming of cancer-associated fibroblasts combined with immune
checkpoint inhibitors: A potential therapeutic strategy for
cancers. Biochimica et biophysica acta. Rev Cancer.
1878:1889452023. View Article : Google Scholar
|
|
108
|
Rawla P: Epidemiology of prostate cancer.
World J Oncol. 10:63–89. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Culp MB, Soerjomataram I, Efstathiou JA,
Bray F and Jemal A: Recent global patterns in prostate cancer
incidence and mortality rates. Eur Urol. 77:38–52. 2020. View Article : Google Scholar
|
|
110
|
Hammerer P and Manka L: Androgen
deprivation therapy for advanced prostate cancer. Urologic
Oncology. Merseburger AS and Burger M: Springer International
Publishing; Cham: pp. 255–276. 2019, View Article : Google Scholar
|
|
111
|
Figueiredo A, Costa L, Mauricio MJ,
Figueira L, Ramos R and Martins-da-Silva C: Nonmetastatic
castration-resistant prostate cancer: Current challenges and
trends. Clin Drug Investig. 42:631–642. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Bubendorf L, Schopfer A, Wagner U, Sauter
G, Moch H, Willi N, Gasser TC and Mihatsch MJ: Metastatic patterns
of prostate cancer: An autopsy study of 1,589 patients. Hum Pathol.
31:578–583. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Begley LA, Kasina S, MacDonald J and
Macoska JA: The inflammatory microenvironment of the aging prostate
facilitates cellular proliferation and hypertrophy. Cytokine.
43:194–199. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Levesque C and Nelson PS: Cellular
constituents of the prostate stroma: Key contributors to prostate
cancer progression and therapy resistance. Cold Spring Harb
Perspect Med. 8:a0305102018. View Article : Google Scholar
|
|
115
|
ChallaSivaKanaka S, Vickman RE, Kakarla M,
Hayward SW and Franco OE: Fibroblast heterogeneity in prostate
carcinogenesis. Cancer Lett. 525:76–83. 2022. View Article : Google Scholar :
|
|
116
|
Franco OE and Hayward SW: Targeting the
tumor stroma as a novel therapeutic approach for prostate cancer.
Adv Pharmacol. 65:267–313. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Jung Y, Kim JK, Shiozawa Y, Wang J, Mishra
A, Joseph J, Berry JE, McGee S, Lee E, Sun H, et al: Recruitment of
mesenchymal stem cells into prostate tumours promotes metastasis.
Nat Commun. 4:17952013. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Bavik C, Coleman I, Dean JP, Knudsen B,
Plymate S and Nelson PS: The gene expression program of prostate
fibroblast senescence modulates neoplastic epithelial cell
proliferation through paracrine mechanisms. Cancer Res. 66:794–802.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Bedeschi M, Marino N, Cavassi E, Piccinini
F and Tesei A: Cancer-associated fibroblast: Role in prostate
cancer progression to metastatic disease and therapeutic
resistance. Cells. 12:8022023. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Bonollo F, Thalmann GN, Kruithof-de Julio
M and Karkampouna S: The role of Cancer-Associated fibroblasts in
prostate cancer tumorigenesis. Cancers (Basel). 12:18872020.
View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Lavie D, Ben-Shmuel A, Erez N and
Scherz-Shouval R: Cancer-associated fibroblasts in the single-cell
era. Nat Cancer. 3:793–807. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Nguyen EV, Pereira BA, Lawrence MG, Ma X,
Rebello RJ, Chan H, Niranjan B, Wu Y, Ellem S, Guan X, et al:
Proteomic profiling of human prostate Cancer-associated fibroblasts
(CAF) reveals LOXL2-dependent regulation of the tumor
microenvironment. Mol Cell Proteomics. 18:1410–1427. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Wadosky KM and Koochekpour S: Molecular
mechanisms underlying resistance to androgen deprivation therapy in
prostate cancer. Oncotarget. 7:64447–64470. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Boudadi K and Antonarakis ES: Resistance
to novel antiandrogen therapies in metastatic Castration-resistant
prostate cancer. Clin Med Insights Oncol. 10(Suppl 1): S1–S9.
2016.
|
|
125
|
Chandrasekar T, Yang JC, Gao AC and Evans
CP: Mechanisms of resistance in castration-resistant prostate
cancer (CRPC). Transl Androl Urol. 4:365–380. 2015.
|
|
126
|
Leach DA and Buchanan G: Stromal androgen
receptor in prostate cancer development and progression. Cancers
(Basel). 9:102017. View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Cioni B, Nevedomskaya E, Melis MHM, van
Burgsteden J, Stelloo S, Hodel E, Spinozzi D, de Jong J, van der
Poel H, de Boer JP, et al: Loss of androgen receptor signaling in
prostate cancer-associated fibroblasts (CAFs) promotes CCL2- and
CXCL8-mediated cancer cell migration. Mol Oncol. 12:1308–1323.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Eder T, Weber A, Neuwirt H, Grünbacher G,
Ploner C, Klocker H, Sampson N and Eder IE: Cancer-associated
fibroblasts modify the response of prostate cancer cells to
androgen and Anti-androgens in Three-dimensional spheroid culture.
Int J Mol Sci. 17:14582016. View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Cheteh EH, Augsten M, Rundqvist H, Bianchi
J, Sarne V, Egevad L, Bykov VJ, Östman A and Wiman KG: Human
cancer-associated fibroblasts enhance glutathione levels and
antagonize drug-induced prostate cancer cell death. Cell Death Dis.
8:e28482017. View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Baumhoer D, Hench J and Amary F: Recent
advances in molecular profiling of bone and soft tissue tumors.
Skeletal Radiol. 53:1925–1936. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Anderson WJ and Doyle LA: Updates from the
2020 World health organization classification of soft tissue and
bone tumours. Histopathology. 78:644–657. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Ehnman M, Chaabane W, Haglund F and
Tsagkozis P: The tumor microenvironment of pediatric sarcoma:
Mesenchymal mechanisms regulating cell migration and metastasis.
Curr Oncol Rep. 21:902019. View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Plikus MV, Wang X, Sinha S, Forte E,
Thompson SM, Herzog EL, Driskell RR, Rosenthal N, Biernaskie J and
Fibroblasts Horsley V: Origins, definitions, and functions in
health and disease. Cell. 184:3852–3872. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
134
|
Resag A, Toffanin G, Benesova I, Müller L,
Potkrajcic V, Ozaniak A, Lischke R, Bartunkova J, Rosato A, Jöhrens
K, et al: The immune contexture of liposarcoma and its clinical
implications. Cancers. 14:45782022. View Article : Google Scholar : PubMed/NCBI
|
|
135
|
Jones JEC, Rabhi N, Orofino J, Gamini R,
Perissi V, Vernochet C and Farmer SR: The adipocyte acquires a
fibroblast-like transcriptional signature in response to a high fat
diet. Sci Rep. 10:23802020. View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Lendahl U, Muhl L and Betsholtz C:
Identification, discrimination and heterogeneity of fibroblasts.
Nat Commun. 13:34092022. View Article : Google Scholar : PubMed/NCBI
|
|
137
|
Bochet L, Lehuede C, Dauvillier S, Wang
YY, Dirat B, Laurent V, Dray C, Guiet R, Maridonneau-Parini I, Le
Gonidec S, et al: Adipocyte-derived fibroblasts promote tumor
progression and contribute to the desmoplastic reaction in breast
cancer. Cancer Res. 73:5657–5668. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Bouche C and Quail DF: Fueling the tumor
microenvironment with cancer-associated adipocytes. Cancer Res.
83:1170–1172. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
139
|
Harati K, Daigeler A, Hirsch T, Jacobsen
F, Behr B, Wallner C, Lehnhardt M and Becerikli M: Tumor-associated
fibroblasts promote the proliferation and decrease the doxorubicin
sensitivity of liposarcoma cells. Int J Mol Med. 37:1535–1541.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
140
|
Xu C, Yan L, Guan X, Wang Z, Wu J, Lv A,
Liu D, Liu F, Dong B, Zhao M, et al: Tsp2 facilitates
tumor-associated fibroblasts formation and promotes tumor
progression in retroperitoneal liposarcoma. Int J Biol Sci.
18:5038–5055. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
141
|
Kalluri R: The biology and function of
fibroblasts in cancer. Nat Rev Cancer. 16:582–598. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
142
|
Skapek SX, Ferrari A, Gupta AA, Lupo PJ,
Butler E, Shipley J, Barr FG and Hawkins DS: Rhabdomyosarcoma. Nat
Rev Dis Primers. 5:12019. View Article : Google Scholar : PubMed/NCBI
|
|
143
|
Hettmer S and Wagers AJ: Muscling in:
Uncovering the origins of rhabdomyosarcoma. Nat Med. 16:171–173.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
144
|
Chapman MA, Meza R and Lieber RL: Skeletal
muscle fibroblasts in health and disease. Differentiation.
92:108–115. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
145
|
Tarnowski M, Grymula K, Liu R, Tarnowska
J, Drukala J, Ratajczak J, Mitchell RA, Ratajczak MZ and Kucia M:
Macrophage migration inhibitory factor is secreted by
rhabdomyosarcoma cells, modulates tumor metastasis by binding to
CXCR4 and CXCR7 receptors and inhibits recruitment of
cancer-associated fibroblasts. Mol Cancer Res. 8:1328–1343. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
146
|
Wysoczynski M, Shin DM, Kucia M and
Ratajczak MZ: Selective upregulation of interleukin-8 by human
rhabdomyosarcomas in response to hypoxia: Therapeutic implications.
Int J Cancer. 126:371–381. 2010. View Article : Google Scholar
|
|
147
|
Awaji M, Saxena S, Wu L, Prajapati DR,
Purohit A, Varney ML, Kumar S, Rachagani S, Ly QP, Jain M, et al:
CXCR2 signaling promotes secretory cancer-associated fibroblasts in
pancreatic ductal adenocarcinoma. FASEB J. 34:9405–9418. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
148
|
Dhayni K, Zibara K, Issa H, Kamel S and
Bennis Y: Targeting CXCR1 and CXCR2 receptors in cardiovascular
diseases. Pharmacol Ther. 237:1082572022. View Article : Google Scholar : PubMed/NCBI
|
|
149
|
Ghayad SE, Rammal G, Ghamloush F, Basma H,
Nasr R, Diab-Assaf M, Chelala C and Saab R: Exosomes derived from
embryonal and alveolar rhabdomyosarcoma carry differential miRNA
cargo and promote invasion of recipient fibroblasts. Sci Rep.
6:370882016. View Article : Google Scholar : PubMed/NCBI
|
|
150
|
Fahs A, Hussein N, Zalzali H, Ramadan F,
Ghamloush F, Tamim H, El Homsi M, Badran B, Boulos F, Tawil A, et
al: CD147 promotes tumorigenesis via Exosome-mediated signaling in
rhabdomyosarcoma. Cells. 11:22672022. View Article : Google Scholar : PubMed/NCBI
|
|
151
|
Burns J, Wilding CP, Krasny L, Zhu X,
Chadha M, Tam YB, Ps H, Mahalingam AH, Lee ATJ, Arthur A, et al:
The proteomic landscape of soft tissue sarcomas. Nature Commun.
14:38342023. View Article : Google Scholar
|
|
152
|
Stork T, Hegedus B, Guder W, Hamacher R,
Hardes J, Kaths M, Plönes T, Pöttgen C, Schildhaus HU, Streitbürger
A, et al: Prognostic factors for leiomyosarcoma with isolated
metastases to the lungs: Impact of metastasectomy. Ann Surg Oncol.
29:4429–4436. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
153
|
Tseng WW, Swallow CJ, Strauss DC, Bonvalot
S, Rutkowski P, Ford SJ, Gonzalez RJ, Gladdy RA, Gyorki DE,
Fairweather M, et al: Management of locally recurrent
retroperitoneal sarcoma in the Adult: An updated consensus approach
from the transatlantic australasian retroperitoneal sarcoma working
group. Ann Surg Oncol. 29:7335–7348. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
154
|
Tran V and Slavin J: Immunohistochemistry
in bone and soft tissue tumours. Sarcoma: A Practical Guide to
Multidisciplinary Management. Choong PFM: Springer Singapore;
Singapore: pp. 119–134. 2021, View Article : Google Scholar
|
|
155
|
Porrello G, Cannella R, Randazzo A,
Badalamenti G, Brancatelli G and Vernuccio F: CT and MR imaging of
retroperitoneal sarcomas: A practical guide for the radiologist.
Cancers (Basel). 15:29852023. View Article : Google Scholar : PubMed/NCBI
|
|
156
|
Kerrison WGJ, Thway K, Jones RL and Huang
PH: The biology and treatment of leiomyosarcomas. Crit Rev Oncol
Hematol. 184:1039552023. View Article : Google Scholar : PubMed/NCBI
|
|
157
|
Tai Y, Woods EL, Dally J, Kong D, Steadman
R, Moseley R and Midgley AC: Myofibroblasts: Function, formation,
and scope of molecular therapies for skin fibrosis. Biomolecules.
11:10952021. View Article : Google Scholar : PubMed/NCBI
|
|
158
|
Nagao Y, Yokoi A, Yoshida K, Kitagawa M,
Asano-Inami E, Kato T, Ishikawa M, Yamamoto Y and Kajiyama H:
Uterine leiomyosarcoma cell-derived extracellular vesicles induce
the formation of cancer-associated fibroblasts. Biochim Biophys
Acta Mol Basis Dis. 1870:1671032024. View Article : Google Scholar : PubMed/NCBI
|
|
159
|
Canter RJ, Beal S, Borys D, Martinez SR,
Bold RJ and Robbins AS: Interaction of histologic subtype and
histologic grade in predicting survival for soft-tissue sarcomas. J
Am Coll Surg. 210:191–198.e2. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
160
|
Sun H, Liu J, Hu F, Xu M, Leng A, Jiang F
and Chen K: Current research and management of undifferentiated
pleomorphic sarcoma/myofibrosarcoma. Front Genet. 14:11094912023.
View Article : Google Scholar : PubMed/NCBI
|
|
161
|
Ozzello L, Stout AP and Murray MR:
Cultural characteristics of malignant histiocytomas and fibrous
xanthomas. Cancer. 16:331–344. 1963. View Article : Google Scholar : PubMed/NCBI
|
|
162
|
O'Brien JE and Stout AP: Malignant fibrous
xanthomas. Cancer. 17:1445–1455. 1964. View Article : Google Scholar : PubMed/NCBI
|
|
163
|
Iwasaki H, Isayama T, Johzaki H and
Kikuchi M: Malignant fibrous histiocytoma. Evidence of perivascular
mesenchymal cell origin immunocytochemical studies with monoclonal
anti-MFH antibodies. Am J Pathol. 128:528–537. 1987.PubMed/NCBI
|
|
164
|
Erlandson RA and Antonescu CR: The rise
and fall of malignant fibrous histiocytoma. Ultrastruct Pathol.
28:283–289. 2004. View Article : Google Scholar
|
|
165
|
Widemann BC and Italiano A: Biology and
management of undifferentiated pleomorphic sarcoma,
myxofibrosarcoma, and malignant peripheral nerve sheath tumors:
State of the art and perspectives. J Clin Oncol. 36:160–167. 2018.
View Article : Google Scholar :
|
|
166
|
Osanai T, Yamakawa M, Suda A and Watanabe
Y: Metamorphosed fibroblasts and their relation to the histogenesis
of malignant fibrous histiocytoma in experimental murine model.
Histol Histopathol. 15:697–705. 2000.PubMed/NCBI
|
|
167
|
Taxy JB and Battifora H: Malignant fibrous
histiocytoma. An electron microscopic study. Cancer. 40:254–267.
1977. View Article : Google Scholar : PubMed/NCBI
|
|
168
|
Wood GS, Beckstead JH, Turner RR,
Hendrickson MR, Kempson RL and Warnke RA: Malignant fibrous
histiocytoma tumor cells resemble fibroblasts. Am J Surg Pathol.
10:323–335. 1986. View Article : Google Scholar : PubMed/NCBI
|
|
169
|
Chang Y, Cho B, Kim S and Kim J: Direct
conversion of fibroblasts to osteoblasts as a novel strategy for
bone regeneration in elderly individuals. Exp Mol Med. 51:1–8.
2019.PubMed/NCBI
|
|
170
|
Neumann E, Lefevre S, Zimmermann B, Gay S
and Muller-Ladner U: Rheumatoid arthritis progression mediated by
activated synovial fibroblasts. Trends Mol Med. 16:458–468. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
171
|
Setty BA, Gikandi A and DuBois SG: Ewing
sarcoma drug therapy: Current standard of care and emerging agents.
Paediatr Drugs. 25:389–397. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
172
|
Riggi N, Suva ML and Stamenkovic I:
Ewing's Sarcoma. N Engl J Med. 384:154–164. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
173
|
Volchenboum SL, Andrade J, Huang L,
Barkauskas DA, Krailo M, Womer RB, Ranft A, Potratz J, Dirksen U,
Triche TJ and Lawlor ER: Gene expression profiling of ewing sarcoma
tumors reveals the prognostic importance of Tumor-stromal
interactions: A report from the Children's oncology group. J Pathol
Clin Res. 1:83–94. 2015. View
Article : Google Scholar : PubMed/NCBI
|
|
174
|
Wrenn ED, Apfelbaum AA, Rudzinski ER, Deng
X, Jiang W, Sud S, Van Noord RA, Newman EA, Garcia NM, Miyaki A, et
al: Cancer-associated Fibroblast-like tumor cells remodel the ewing
sarcoma tumor microenvironment. Clin Cancer Res. 29:5140–5154.
2023. View Article : Google Scholar : PubMed/NCBI
|
|
175
|
Li S, Zhang H, Liu J and Shang G: Targeted
therapy for osteosarcoma: A review. J Cancer Res Clin Oncol.
149:6785–6797. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
176
|
Panez-Toro I, Munoz-Garcia J,
Vargas-Franco JW, Renodon-Cornière A, Heymann MF, Lézot F and
Heymann D: Advances in osteosarcoma. Curr Osteoporos Rep.
21:330–343. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
177
|
Misaghi A, Goldin A, Awad M and Kulidjian
AA: Osteosarcoma: A comprehensive review. SICOT J. 4:122018.
View Article : Google Scholar : PubMed/NCBI
|
|
178
|
Hu J, Lazar AJ, Ingram D, Wang WL, Zhang
W, Jia Z, Ragoonanan D, Wang J, Xia X, Mahadeo K, et al: Cell
membrane-anchored and tumor-targeted IL-12 T-cell therapy destroys
cancer-associated fibroblasts and disrupts extracellular matrix in
heterogenous osteosarcoma xenograft models. J Immunother Cancer.
12:e0069912024. View Article : Google Scholar : PubMed/NCBI
|
|
179
|
Wang JW, Wu XF, Gu XJ and Jiang XH:
Exosomal miR-1228 from Cancer-associated fibroblasts promotes cell
migration and invasion of osteosarcoma by directly targeting SCAI.
Oncol Res. 27:979–986. 2019. View Article : Google Scholar
|
|
180
|
Mazumdar A, Urdinez J, Boro A, Migliavacca
J, Arlt MJE, Muff R, Fuchs B, Snedeker JG and Gvozdenovic A:
Osteosarcoma-derived extracellular vesicles induce lung fibroblast
reprogramming. Int J Mol Sci. 21:54512020. View Article : Google Scholar : PubMed/NCBI
|
|
181
|
Zhang Y, Liu Z, Yang X, Lu W, Chen Y, Lin
Y, Wang J, Lin S and Yun JP: H3K27 acetylation activated-COL6A1
promotes osteosarcoma lung metastasis by repressing STAT1 and
activating pulmonary cancer-associated fibroblasts. Theranostics.
11:1473–1492. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
182
|
David MS, Kelly E and Zoellner H: Opposite
cytokine synthesis by fibroblasts in contact co-culture with
osteosarcoma cells compared with transwell co-cultures. Cytokine.
62:48–51. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
183
|
Xu Y, Chen P, Liu D, Xu Q, Meng H and Wang
X: Exploration of s new biomarker in osteosarcoma and association
with clinical outcomes: TOP2A+ cancer associated fibroblasts. J
Gene Med. 25:e35282023. View Article : Google Scholar
|
|
184
|
Liu Y, Han X, Han Y, Bi J, Wu Y, Xiang D,
Zhang Y, Bi W, Xu M and Li J: Integrated transcriptomic analysis
systematically reveals the heterogeneity and molecular
characterization of cancer-associated fibroblasts in osteosarcoma.
Gene. 907:1482862024. View Article : Google Scholar : PubMed/NCBI
|
|
185
|
LeBleu VS and Neilson EG: Origin and
functional heterogeneity of fibroblasts. FASEB. 34:3519–3536. 2020.
View Article : Google Scholar
|
|
186
|
Pittenger MF, Discher DE, Peault BM,
Phinney DG, Hare JM and Caplan AI: Mesenchymal stem cell
perspective: Cell biology to clinical progress. NPJ Regen Med.
4:222019. View Article : Google Scholar : PubMed/NCBI
|
|
187
|
Sannino G, Marchetto A, Kirchner T and
Grunewald TGP: Epithelial-to-mesenchymal and
mesenchymal-to-epithelial transition in mesenchymal tumors: A
paradox in sarcomas? Cancer Res. 77:4556–4561. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
188
|
Mehta A and Stanger BZ: Lineage
Plasticity: The new cancer hallmark on the block. Cancer Res.
84:184–191. 2024. View Article : Google Scholar :
|
|
189
|
Strating E, Verhagen MP, Wensink E,
Dünnebach E, Wijler L, Aranguren I, De la Cruz AS, Peters NA,
Hageman JH, van der Net MMC, et al: Co-cultures of colon cancer
cells and cancer-associated fibroblasts recapitulate the aggressive
features of mesenchymal-like colon cancer. Front Immunol.
14:10539202023. View Article : Google Scholar : PubMed/NCBI
|
|
190
|
Jeong SY, Lee JH, Shin Y, Chung S and Kuh
HJ: Co-culture of tumor spheroids and fibroblasts in a collagen
Matrix-incorporated microfluidic chip mimics reciprocal activation
in solid tumor microenvironment. PLoS One. 11:e01590132016.
View Article : Google Scholar : PubMed/NCBI
|
|
191
|
Abercrombie M, Heaysman JE and Karthauser
HM: Social behaviour of cells in tissue culture. III. Mutual
influence of sarcoma cells and fibroblasts. Exp Cell Res.
13:276–291. 1957. View Article : Google Scholar : PubMed/NCBI
|
|
192
|
Abercrombie M and Heaysman JE: Invasive
behavior between sarcoma and fibroblast populations in cell
culture. J Natl Cancer Inst. 56:561–570. 1976. View Article : Google Scholar : PubMed/NCBI
|
|
193
|
Johnson GS, Friedman RM and Pastan I:
Restoration of several morphological characteristics of normal
fibroblasts in sarcoma cells treated with adenosine-3': 5'-cyclic
monophosphate and its derivatives. Proc Natl Acad Sci USA.
68:425–429. 1971. View Article : Google Scholar
|
|
194
|
Dahlberg WK, Little JB, Fletcher JA, Suit
HD and Okunieff P: Radiosensitivity in vitro of human soft tissue
sarcoma cell lines and skin fibroblasts derived from the same
patients. Int J Radiat Biol. 63:191–198. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
195
|
Fisher C: Low-grade sarcomas with
CD34-positive fibroblasts and Low-grade myofibroblastic sarcomas.
Ultrastruct Pathol. 28:291–305. 2004. View Article : Google Scholar
|
|
196
|
Broz MT, Ko EY, Ishaya K, Xiao J, De
Simone M, Hoi XP, Piras R, Gala B, Tessaro FHG, Karlstaedt A, et
al: Metabolic targeting of cancer associated fibroblasts overcomes
T-cell exclusion and chemoresistance in Soft-tissue sarcomas. Nat
Commun. 15:24982024. View Article : Google Scholar : PubMed/NCBI
|
|
197
|
Liu Y, Sinjab A, Min J, Han G, Paradiso F,
Zhang Y, Wang R, Pei G, Dai Y, Liu Y, et al: Conserved spatial
subtypes and cellular neighborhoods of cancer-associated
fibroblasts revealed by single-cell spatial multi-omics. Cancer
Cell. 43:905–924.e6. 2025. View Article : Google Scholar : PubMed/NCBI
|
|
198
|
Kazakova AN, Lukina MM, Anufrieva KS,
Bekbaeva IV, Ivanova OM, Shnaider PV, Slonov A, Arapidi GP and
Shender VO: Exploring the diversity of cancer-associated
fibroblasts: Insights into mechanisms of drug resistance. Front
Cell Dev Biol. 12:14031222024. View Article : Google Scholar : PubMed/NCBI
|
|
199
|
Chen Y, McAndrews KM and Kalluri R:
Clinical and therapeutic relevance of cancer-associated
fibroblasts. Nat Rev Clin Oncol. 18:792–804. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
200
|
Wang LC, Lo A, Scholler J, Sun J, Majumdar
RS, Kapoor V, Antzis M, Cotner CE, Johnson LA, Durham AC, et al:
Targeting fibroblast activation protein in tumor stroma with
chimeric antigen receptor T cells can inhibit tumor growth and
augment host immunity without severe toxicity. Cancer Immunol Res.
2:154–166. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
201
|
Liu Y, Sun Y, Wang P, Li S, Dong Y, Zhou
M, Shi B, Jiang H, Sun R and Li Z: FAP-targeted CAR-T suppresses
MDSCs recruitment to improve the antitumor efficacy of
claudin18.2-targeted CAR-T against pancreatic cancer. J Transl Med.
21:2552023. View Article : Google Scholar : PubMed/NCBI
|
|
202
|
Gao Y, Li X, Zeng C, Liu C, Hao Q, Li W,
Zhang K, Zhang W, Wang S, Zhao H, et al: CD63+ Cancer-associated
fibroblasts confer tamoxifen resistance to breast cancer cells
through exosomal miR-22. Adv Sci (Weinh). 7:20025182020. View Article : Google Scholar
|
|
203
|
Zhou P, Du X, Jia W, Feng K and Zhang Y:
Engineered extracellular vesicles for targeted reprogramming of
cancer-associated fibroblasts to potentiate therapy of pancreatic
cancer. Signal Transduct Target Ther. 9:1512024. View Article : Google Scholar : PubMed/NCBI
|
|
204
|
Peng D, Fu M, Wang M, Wei Y and Wei X:
Targeting TGF-β signal transduction for fibrosis and cancer
therapy. Mol Cancer. 21:1042022. View Article : Google Scholar
|
|
205
|
Akhmetshina A, Palumbo K, Dees C, Bergmann
C, Venalis P, Zerr P, Horn A, Kireva T, Beyer C, Zwerina J, et al:
Activation of canonical Wnt signalling is required for
TGF-beta-mediated fibrosis. Nat Commun. 3:7352012. View Article : Google Scholar
|
|
206
|
Xu L, Cui WH, Zhou WC, Li DL, Li LC, Zhao
P, Mo XT, Zhang Z and Gao J: Activation of Wnt/β-catenin signalling
is required for TGF-β/Smad2/3 signalling during myofibroblast
proliferation. J Cell Mol Med. 21:1545–1554. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
207
|
Giguelay A, Turtoi E, Khelaf L, Tosato G,
Dadi I, Chastel T, Poul MA, Pratlong M, Nicolescu S, Severac D, et
al: The landscape of cancer-associated fibroblasts in colorectal
cancer liver metastases. Theranostics. 12:7624–7639. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
208
|
Li H, Liu W, Zhang X and Wang Y:
Cancer-associated fibroblast-secreted collagen triple helix repeat
containing-1 promotes breast cancer cell migration, invasiveness
and epithelial-mesenchymal transition by activating the
Wnt/β-catenin pathway. Oncol Lett. 22:8142021.
|
|
209
|
Avgustinova A, Iravani M, Robertson D,
Fearns A, Gao Q, Klingbeil P, Hanby AM, Speirs V, Sahai E, Calvo F
and Isacke CM: Tumour cell-derived Wnt7a recruits and activates
fibroblasts to promote tumour aggressiveness. Nat Commun.
7:103052016. View Article : Google Scholar : PubMed/NCBI
|
|
210
|
Sun Y, Campisi J, Higano C, Beer TM,
Porter P, Coleman I, True L and Nelson PS: Treatment-induced damage
to the tumor microenvironment promotes prostate cancer therapy
resistance through WNT16B. Nat Med. 18:1359–1368. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
211
|
Kramer N, Schmollerl J, Unger C, Nivarthi
H, Rudisch A, Unterleuthner D, Scherzer M, Riedl A, Artaker M,
Crncec I, et al: Autocrine WNT2 signaling in fibroblasts promotes
colorectal cancer progression. Oncogene. 36:5460–5472. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
212
|
Zhang C, Fei Y, Wang H, Hu S, Liu C, Hu R
and Du Q: CAFs orchestrates tumor immune microenvironment-A new
target in cancer therapy? Front Pharmacol. 14:11133782023.
View Article : Google Scholar : PubMed/NCBI
|
|
213
|
Huang TX, Tan XY, Huang HS, Li YT, Liu BL,
Liu KS, Chen X, Chen Z, Guan XY, Zou C and Fu L: Targeting
cancer-associated fibroblast-secreted WNT2 restores dendritic
cell-mediated antitumour immunity. Gut. 71:333–344. 2022.
View Article : Google Scholar
|
|
214
|
Moynihan KD, Kumar MP, Sultan H, Pappas
DC, Park T, Chin SM, Bessette P, Lan RY, Nguyen HC, Mathewson ND,
et al: IL-2 targeted to CD8+ T cells promotes robust effector T
cell responses and potent antitumor immunity. Cancer Discov.
14:1206–1225. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
215
|
Siebert N, Leopold J, Zumpe M,
Troschke-Meurer S, Biskupski S, Zikoridse A and Lode HN: The
immunocytokine FAP-IL-2v enhances anti-neuroblastoma efficacy of
the anti-GD2 antibody dinutuximab beta. Cancers. 14:48422022.
View Article : Google Scholar :
|
|
216
|
Rivas EI, Linares J, Zwick M, Gómez-Llonin
A, Guiu M, Labernadie A, Badia-Ramentol J, Lladó A, Bardia L,
Pérez-Núñez I, et al: Targeted immunotherapy against distinct
cancer-associated fibroblasts overcomes treatment resistance in
refractory HER2+ breast tumors. Nat Commun. 13:53102022. View Article : Google Scholar : PubMed/NCBI
|
|
217
|
Karthik R, Deshpande NU, Iago de Castro S,
Anna B, Ifeanyichukwu O, Haleh A, Andrews A, Vanessa G, Siddharth
M, Samara S, et al: Abstract C021: Granulocytic MDSC-derived NLRP3
inflammasome activation is a novel regulator of inflammatory CAF
skewness in pancreatic cancer. In: Proceedings of the AACR Special
Conference in Cancer Research: Pancreatic Cancer; 2023 Sep 27-30;
Boston, Massachusetts. Philadelphia (PA), AACR. Cancer Res.
84(Suppl 2)2024.Abstract nr C021.
|
|
218
|
Shao X, Zhao X, Wang B, Fan J, Wang J and
An H: Tumor microenvironment targeted nano-drug delivery systems
for multidrug resistant tumor therapy. Theranostics. 15:1689–1714.
2025. View Article : Google Scholar : PubMed/NCBI
|
|
219
|
Crane JN, Graham DS, Mona CE, Nelson SD,
Samiei A, Dawson DW, Dry SM, Masri MG, Crompton JG, Benz MR, et al:
Fibroblast activation protein expression in sarcomas. Sarcoma.
2023:24804932023. View Article : Google Scholar : PubMed/NCBI
|
|
220
|
Miettinen M: Immunohistochemistry of soft
tissue tumours-review with emphasis on 10 markers. Histopathology.
64:101–118. 2014. View Article : Google Scholar
|
|
221
|
Zhang H, Yue X, Chen Z, Liu C, Wu W, Zhang
N, Liu Z, Yang L, Jiang Q, Cheng Q, et al: Define cancer-associated
fibroblasts (CAFs) in the tumor microenvironment: New opportunities
in cancer immunotherapy and advances in clinical trials. Mol
Cancer. 22:1592023. View Article : Google Scholar : PubMed/NCBI
|
|
222
|
Brahmi M, Lesluyes T, Dufresne A,
Toulmonde M, Italiano A, Mir O, Le Cesne A, Valentin T, Chevreau C,
Bonvalot S, et al: Expression and prognostic significance of PDGF
ligands and receptors across soft tissue sarcomas. ESMO Open.
6:1000372021. View Article : Google Scholar : PubMed/NCBI
|
|
223
|
Robin YM, Penel N, Perot G, Neuville A,
Vélasco V, Ranchère-Vince D, Terrier P and Coindre JM: Transgelin
is a novel marker of smooth muscle differentiation that improves
diagnostic accuracy of leiomyosarcomas: A comparative
immunohistochemical reappraisal of myogenic markers in 900 soft
tissue tumors. Mod Pathol. 26:502–510. 2013. View Article : Google Scholar
|
|
224
|
Dagher R, Cohen M, Williams G, Rothmann M,
Gobburu J, Robbie G, Rahman A, Chen G, Staten A, Griebel D and
Pazdur R: Approval summary: Imatinib mesylate in the treatment of
metastatic and/or unresectable malignant gastrointestinal stromal
tumors. Clin Cancer Res. 8:3034–3038. 2002.PubMed/NCBI
|
|
225
|
Tap WD, Jones RL, Van Tine BA, Chmielowski
B, Elias AD, Adkins D, Agulnik M, Cooney MM, Livingston MB, Pennock
G, et al: Olaratumab and doxorubicin versus doxorubicin alone for
treatment of soft-tissue sarcoma: An open-label phase 1b and
randomised phase 2 trial. Lancet. 388:488–497. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
226
|
Tap WD, Wagner AJ, Schoffski P,
Martin-Broto J, Krarup-Hansen A, Ganjoo KN, Yen CC, Abdul Razak AR,
Spira A, Kawai A, et al: Effect of doxorubicin plus olaratumab vs
doxorubicin plus placebo on survival in patients with advanced soft
tissue sarcomas: The ANNOUNCE randomized clinical trial. JAMA.
323:1266–1276. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
227
|
Martin-Broto J, Hindi N, Grignani G,
Martinez-Trufero J, Redondo A, Valverde C, Stacchiotti S,
Lopez-Pousa A, D'Ambrosio L, Gutierrez A, et al: Nivolumab and
sunitinib combination in advanced soft tissue sarcomas: A
multicenter, Single-arm, phase Ib/II trial. J Immunother Cancer.
8:e0015612020. View Article : Google Scholar : PubMed/NCBI
|
|
228
|
Shahvali S, Rahiman N, Jaafari MR and
Arabi L: Targeting fibroblast activation protein (FAP): Advances in
CAR-T cell, antibody, and vaccine in cancer immunotherapy. Drug
Deliv Transl Res. 13:2041–2056. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
229
|
Xiao W, Wang J, Wen X, Xu B, Que Y, Yu K,
Xu L, Zhao J, Pan Q, Zhou P and Zhang X: Chimeric antigen
receptor-modified T-cell therapy for platelet-derived growth factor
receptor α-positive rhabdomyosarcoma. Cancer. 126(Suppl 9):
S2093–S2100. 2020. View Article : Google Scholar
|
|
230
|
Vogt KC, Silberman PC, Lin Q, Han JE,
Laflin A, Gellineau HA, Heller DA and Scheinberg DA:
Microenvironment actuated CAR T cells improve solid tumor efficacy
without toxicity. Sci Adv. 11:eads34032025. View Article : Google Scholar : PubMed/NCBI
|
|
231
|
Dharani S, Cho H, Fernandez JP, Juillerat
A, Valton J, Duchateau P, Poirot L and Das S: TALEN-edited
allogeneic inducible dual CAR T cells enable effective targeting of
solid tumors while mitigating off-tumor toxicity. Mol Ther.
32:3915–3931. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
232
|
Liu H, Yang W and Jiang J: Targeting tumor
metabolism to augment CD8+ T cell anti-tumor immunity. J Pharm
Anal. 15:1011502025. View Article : Google Scholar :
|
|
233
|
Ben-Ami E, Perret R, Huang Y, Courgeon F,
Gokhale PC, Laroche-Clary A, Eschle BK, Velasco V, Le Loarer F,
Algeo MP, et al: LRRC15 targeting in Soft-tissue sarcomas:
Biological and clinical implications. Cancers (Basel). 12:572020.
View Article : Google Scholar
|
|
234
|
Slemmons KK, Mukherjee S, Meltzer P,
Purcell JW and Helman LJ: LRRC15 antibody-drug conjugates show
promise as osteosarcoma therapeutics in preclinical studies.
Pediatr Blood Cancer. 68:e287712021. View Article : Google Scholar
|
|
235
|
Brennen WN, Isaacs JT and Denmeade SR:
Rationale behind targeting fibroblast activation protein-expressing
carcinoma-associated fibroblasts as a novel chemotherapeutic
strategy. Mol Cancer Ther. 11:257–266. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
236
|
Giammarile F, Knoll P, Paez D, Estrada
Lobato E, Calapaqui Teran AK and Delgado Bolton RC: Fibroblast
activation protein inhibitor (FAPI) PET imaging in sarcomas: A new
frontier in nuclear medicine. Semin Nucl Med. 54:340–344. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
237
|
Greifenstein L, Gunkel A, Hoehne A,
Osterkamp F, Smerling C, Landvogt C, Mueller C and Baum RP:
3BP-3940, a highly potent FAP-targeting peptide for
theranostics-production, validation and first in human experience
with Ga-68 and Lu-177. iScience. 26:1085412023. View Article : Google Scholar
|
|
238
|
Xie N, Shen G, Gao W, Huang Z, Huang C and
Fu L: Neoantigens: Promising targets for cancer therapy. Signal
Transduct Target Ther. 8:92023. View Article : Google Scholar : PubMed/NCBI
|
|
239
|
Kirane A, Lee D and Ariyan C: Surgical
considerations in Tumor-infiltrating lymphocyte therapy: Challenges
and opportunities. Transplant Cell Ther. 31(Suppl 1): S591–S598.
2025. View Article : Google Scholar : PubMed/NCBI
|
|
240
|
Fan S, Wang W, Che W, Xu Y, Jin C, Dong L
and Xia Q: Nanomedicines targeting metabolic pathways in the tumor
microenvironment: Future perspectives and the role of AI.
Metabolites. 15:2012025. View Article : Google Scholar : PubMed/NCBI
|
|
241
|
Di Dedda C, Vignali D, Piemonti L and
Monti P: Pharmacological targeting of GLUT1 to control Autoreactive
T cell responses. Int J Mol Sci. 20:49622019. View Article : Google Scholar : PubMed/NCBI
|
|
242
|
Macintyre AN, Gerriets VA, Nichols AG,
Michalek RD, Rudolph MC, Deoliveira D, Anderson SM, Abel ED, Chen
BJ, Hale LP and Rathmell JC: The glucose transporter Glut1 is
selectively essential for CD4 T cell activation and effector
function. Cell Metab. 20:61–72. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
243
|
Sung KE, Su X, Berthier E, Pehlke C,
Friedl A and Beebe DJ: Understanding the impact of 2D and 3D
fibroblast cultures on in vitro breast cancer models. PLoS One.
8:e763732013. View Article : Google Scholar : PubMed/NCBI
|
|
244
|
Tolle RC, Gaggioli C and Dengjel J:
Three-dimensional cell culture conditions affect the proteome of
cancer-associated fibroblasts. J Proteome Res. 17:2780–2789. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
245
|
Shao H, Moller M, Wang D, Ting A, Boulina
M and Liu ZJ: A Novel stromal Fibroblast-modulated 3D tumor
spheroid model for studying Tumor-stroma interaction and drug
discovery. J Vis Exp. Feb 28–2020. View
Article : Google Scholar
|
|
246
|
Chen H, Cheng Y, Wang X, Wang J, Shi X, Li
X, Tan W and Tan Z: 3D printed in vitro tumor tissue model of
colorectal cancer. Theranostics. 10:12127–12143. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
247
|
Mondal A, Gebeyehu A, Miranda M, Bahadur
D, Patel N, Ramakrishnan S, Rishi AK and Singh M: Characterization
and printability of Sodium alginate-Gelatin hydrogel for
bioprinting NSCLC co-culture. Sci Rep. 9:199142019. View Article : Google Scholar
|
|
248
|
Kuen J, Darowski D, Kluge T and Majety M:
Pancreatic cancer cell/fibroblast co-culture induces M2 like
macrophages that influence therapeutic response in a 3D model. PLoS
One. 12:e01820392017. View Article : Google Scholar : PubMed/NCBI
|
|
249
|
Jobe NP, Rosel D, Dvořánková B, Kodet O,
Lacina L, Mateu R, Smetana K and Brábek J: Simultaneous blocking of
IL-6 and IL-8 is sufficient to fully inhibit CAF-induced human
melanoma cell invasiveness. Histochem Cell Biol. 146:205–217. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
250
|
Balachander GM, Talukdar PM, Debnath M,
Rangarajan A and Chatterjee K: Inflammatory role of
Cancer-associated fibroblasts in invasive breast tumors revealed
using a fibrous polymer scaffold. ACS Appl Mater Interfaces.
10:33814–33826. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
251
|
Linxweiler J, Hajili T, Körbel C, Berchem
C, Zeuschner P, Müller A, Stöckle M, Menger MD, Junker K and Saar
M: Cancer-associated fibroblasts stimulate primary tumor growth and
metastatic spread in an orthotopic prostate cancer xenograft model.
Sci Reps. 10:125752020. View Article : Google Scholar
|
|
252
|
Miyazaki Y, Oda T, Inagaki Y, Kushige H,
Saito Y, Mori N, Takayama Y, Kumagai Y, Mitsuyama T and Kida YS:
Adipose-derived mesenchymal stem cells differentiate into
heterogeneous cancer-associated fibroblasts in a stroma-rich
xenograft model. Sci Rep. 11:46902021. View Article : Google Scholar : PubMed/NCBI
|
|
253
|
Wahbi W, Awad S, Salo T and Al-Samadi A:
Stroma modulation of radiation response in head and neck squamous
cell carcinoma: Insights from zebrafish larvae xenografts. Exp Cell
Res. 435:1139112024. View Article : Google Scholar : PubMed/NCBI
|
|
254
|
Foster DS, Januszyk M, Delitto D, Yost KE,
Griffin M, Guo J, Guardino N, Delitto AE, Chinta M, Burcham AR, et
al: Multiomic analysis reveals conservation of cancer-associated
fibroblast phenotypes across species and tissue of origin. Cancer
Cell. 40:1392–1406.e7. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
255
|
Cho C, Mukherjee R, Peck AR, Sun Y,
McBrearty N, Katlinski KV, Gui J, Govindaraju PK, Puré E, Rui H and
Fuchs SY: Cancer-associated fibroblasts downregulate type I
interferon receptor to stimulate intratumoral stromagenesis.
Oncogene. 39:6129–6137. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
256
|
Helms EJ, Berry MW, Chaw RC, DuFort CC,
Sun D, Onate MK, Oon C, Bhattacharyya S, Sanford-Crane H, Horton W,
et al: Mesenchymal lineage heterogeneity underlies nonredundant
functions of pancreatic Cancer-associated fibroblasts. Cancer
Discov. 12:484–501. 2022. View Article : Google Scholar
|
|
257
|
De Vita A, Recine F, Miserocchi G, Pieri
F, Spadazzi C, Cocchi C, Vanni S, Liverani C, Farnedi A, Fabbri F,
et al: The potential role of the extracellular matrix in the
activity of trabectedin in UPS and L-sarcoma: Evidences from a
patient-derived primary culture case series in tridimensional and
zebrafish models. J Exp Clin Cancer Res. 40:1652021. View Article : Google Scholar : PubMed/NCBI
|
|
258
|
Molina ER, Chim LK, Salazar MC, Koons GL,
Menegaz BA, Ruiz-Velasco A, Lamhamedi-Cherradi SE, Vetter AM,
Satish T, Cuglievan B, et al: 3D Tissue-engineered tumor model for
Ewing's sarcoma that incorporates Bone-like ECM and mineralization.
ACS Biomater Sci Eng. 6:539–552. 2020. View Article : Google Scholar
|
|
259
|
Moghimi N, Hosseini SA, Dalan AB,
Mohammadrezaei D, Goldman A and Kohandel M: Controlled tumor
heterogeneity in a co-culture system by 3D bio-printed
tumor-on-chip model. Sci Rep. 13:136482023. View Article : Google Scholar : PubMed/NCBI
|
|
260
|
Yang D, Jones MG, Naranjo S, Rideout WM
III, Min KHJ, Ho R, Wu W, Replogle JM, Page JL, Quinn JJ, et al:
Lineage tracing reveals the phylodynamics, plasticity, and paths of
tumor evolution. Cell. 185:1905–1923.e25. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
261
|
Simeonov KP, Byrns CN, Clark ML, Norgard
RJ, Martin B, Stanger BZ, Shendure J, McKenna A and Lengner CJ:
Single-cell lineage tracing of metastatic cancer reveals selection
of hybrid EMT states. Cancer Cell. 39:1150–1162.e9. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
262
|
Liu J, Liu C, Ma Y, Pan X, Chu R, Yao S,
Chen J, Liu C, Chen Z, Sheng C, et al: STING inhibitors sensitize
platinum chemotherapy in ovarian cancer by inhibiting the
CGAS-STING pathway in cancer-associated fibroblasts (CAFs). Cancer
Lett. 588:2167002024. View Article : Google Scholar : PubMed/NCBI
|
|
263
|
de Kruijf EM, van Nes JG, van de Velde CJ,
Putter H, Smit VT, Liefers GJ, Kuppen PJ, Tollenaar RA and Mesker
WE: Tumor-stroma ratio in the primary tumor is a prognostic factor
in early breast cancer patients, especially in triple-negative
carcinoma patients. Breast Cancer Res Treat. 125:687–696. 2011.
View Article : Google Scholar
|
|
264
|
Huijbers A, Tollenaar RA, v Pelt GW,
Zeestraten EC, Dutton S, McConkey CC, Domingo E, Smit VT, Midgley
R, Warren BF, et al: The proportion of tumor-stroma as a strong
prognosticator for stage II and III colon cancer patients:
Validation in the VICTOR trial. Ann Oncol. 24:179–185. 2013.
View Article : Google Scholar
|
|
265
|
De Vlieghere E, Verset L, Demetter P,
Bracke M and De Wever O: Cancer-associated fibroblasts as target
and tool in cancer therapeutics and diagnostics. Virchows Arch.
467:367–382. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
266
|
Kanzaki R and Pietras K: Heterogeneity of
cancer-associated fibroblasts: Opportunities for precision
medicine. Cancer Sci. 111:2708–2717. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
267
|
Wang Q, Zhang X, Du K, Wu X, Zhou Y, Chen
D and Zeng L: Machine learning identifies characteristics molecules
of cancer associated fibroblasts significantly correlated with the
prognosis, immunotherapy response and immune microenvironment in
lung adenocarcinoma. Front Oncol. 12:10592532022. View Article : Google Scholar : PubMed/NCBI
|
|
268
|
Shen C, Rawal S, Brown R, Zhou H, Agarwal
A, Watson MA, Cote RJ and Yang C: Automatic detection of
circulating tumor cells and cancer associated fibroblasts using
deep learning. Sci Rep. 13:57082023. View Article : Google Scholar : PubMed/NCBI
|
|
269
|
Agnoletto C, Caruso C and Garofalo C:
Heterogeneous circulating tumor cells in sarcoma: Implication for
clinical practice. Cancers (Basel). 13:21892021. View Article : Google Scholar : PubMed/NCBI
|
|
270
|
Yang Z, Zhou D and Huang J: Identifying
explainable machine learning models and a novel SFRP2+ fibroblast
signature as predictors for precision medicine in ovarian cancer.
Int J Mol Sci. 24:169422023. View Article : Google Scholar :
|
|
271
|
Min KW, Kim DH, Noh YK, Son BK, Kwon MJ
and Moon JY: Cancer-associated fibroblasts are associated with poor
prognosis in solid type of lung adenocarcinoma in a machine
learning analysis. Sci Rep. 11:167792021. View Article : Google Scholar : PubMed/NCBI
|
|
272
|
Huang B, Chen Q, Ye Z, Zeng L, Huang C,
Xie Y, Zhang R and Shen H: Construction of a matrix
Cancer-associated fibroblast signature Gene-based risk prognostic
signature for directing immunotherapy in patients with breast
cancer using Single-cell analysis and machine learning. Int J Mol
Sci. 24:131752023. View Article : Google Scholar : PubMed/NCBI
|
|
273
|
Ao Z, Shah SH, Machlin LM, Parajuli R,
Miller PC, Rawal S, Williams AJ, Cote RJ, Lippman ME, Datar RH and
El-Ashry D: Identification of Cancer-associated fibroblasts in
circulating blood from patients with metastatic breast cancer.
Cancer Res. 75:4681–4687. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
274
|
Booijink R, Terstappen LWMM, Dathathri E,
Isebia K, Kraan J, Martens J and Bansal R: Identification of
functional and diverse circulating cancer-associated fibroblasts in
metastatic Castration-naive prostate cancer patients. Mol Oncol.
19:2074–2091. 2024. View Article : Google Scholar
|
|
275
|
Lu T, Oomens L, Terstappen L and Prakash
J: In vivo detection of circulating cancer-associated fibroblasts
in breast tumor mouse xenograft: Impact of tumor stroma and
chemotherapy. Cancers (Basel). 15:11272023. View Article : Google Scholar : PubMed/NCBI
|