|
1
|
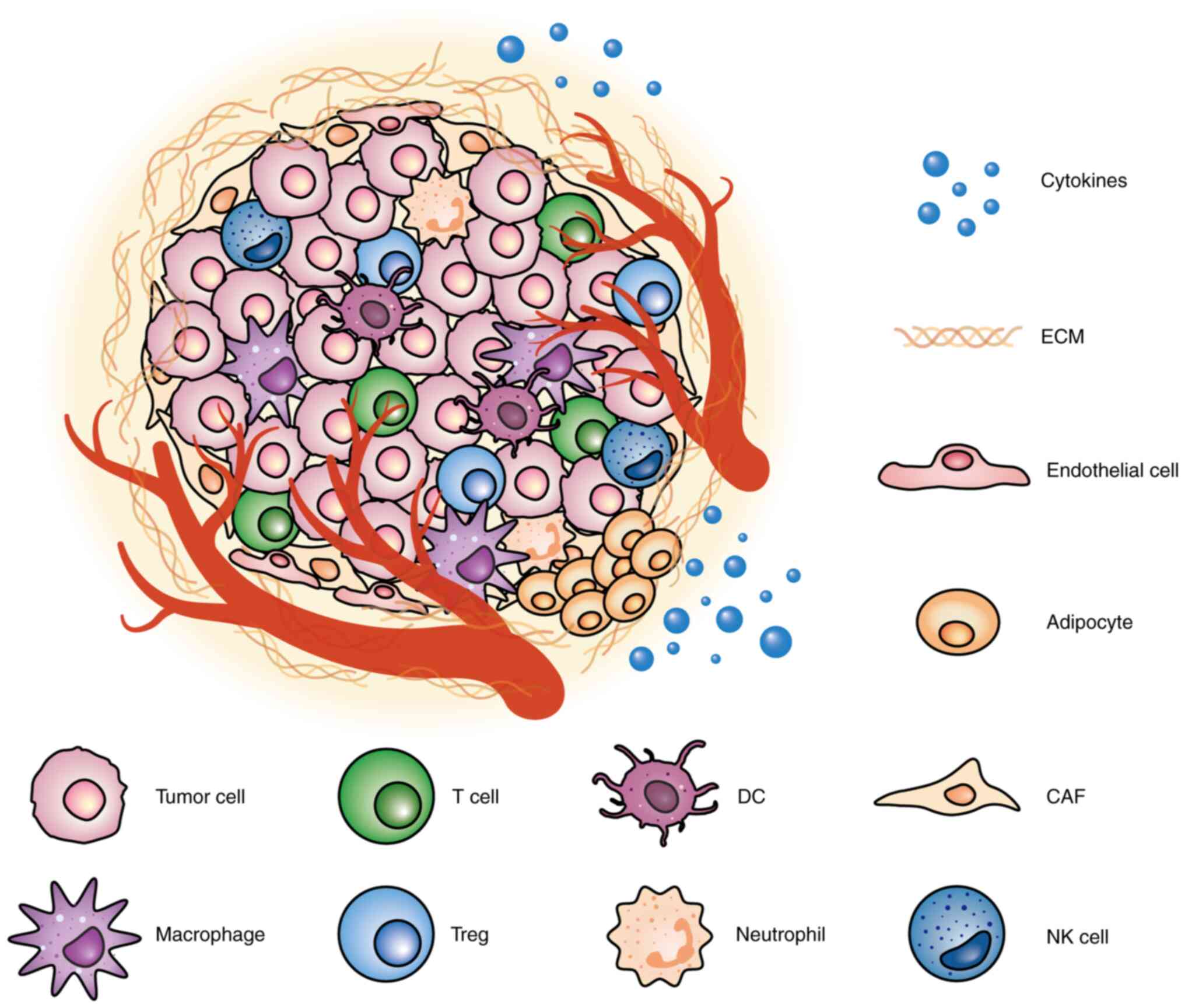
Quail DF and Joyce JA: Microenvironmental
regulation of tumor progression and metastasis. Nat Med.
19:1423–1437. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Goenka A, Khan F, Verma B, Sinha P, Dmello
CC, Jogalekar MP, Gangadaran P and Ahn BC: Tumor microenvironment
signaling and therapeutics in cancer progression. Cancer Commun
(Lond). 43:525–561. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Zhang X, Ma H, Gao Y, Liang Y, Du Y, Hao S
and Ni T: The tumor microenvironment: Signal transduction.
Biomolecules. 14:4382024. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Khosravi G, Mostafavi S, Bastan S,
Ebrahimi N, Gharibvand RS and Eskandari N: Immunologic tumor
microenvironment modulators for turning cold tumors hot. Cancer
Commun (Lond). 44:521–553. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Xiao Y and Yu D: Tumor microenvironment as
a therapeutic target in cancer. Pharmacol Ther. 221:1077532021.
View Article : Google Scholar :
|
|
6
|
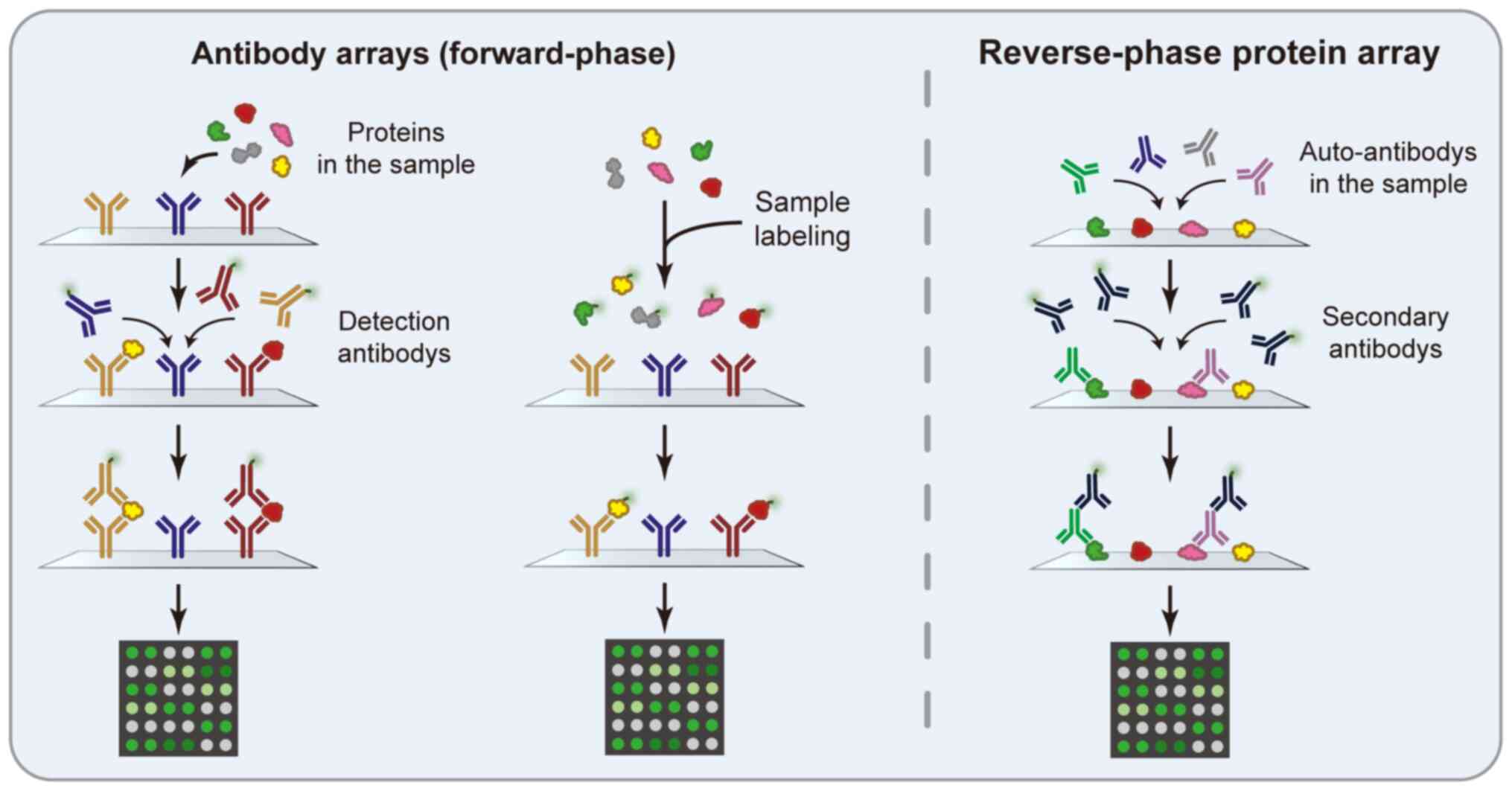
Wilson JJ, Burgess R, Mao Y, Luo S, Tang
H, Jones VS, Weisheng B, Huang RY, Chen X and Huang RP: Antibody
arrays in biomarker discovery. Adv Clin Chem. 69:255–324. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Goetz JG, Minguet S, Navarro-Lerida I,
Lacoste J, Ang LH and Fiering S; Reproducibility Project: Cancer
Biology: Biomechanical remodeling of the microenvironment by
stromal caveolin-1 favors tumor invasion and metastasis. Cell.
146:148–163. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Chen W, Ho C, Chang Y, Chen HY, Lin CA,
Ling TY, Yu SL, Yuan SS, Chen YJ, Lin CY, et al: Cancer-associated
fibroblasts regulate the plasticity of lung cancer stemness via
paracrine signalling. Nat Commun. 5:34722014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Bellei B, Caputo S, Migliano E, Lopez G,
Marcaccini V, Cota C and Picardo M: Simultaneous targeting tumor
cells and cancer-associated fibroblasts with a
paclitaxel-hyaluronan bioconjugate: In vitro evaluation in
non-melanoma skin cancer. Biomedicines. 9:5972021. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Costa A, Kieffer Y, Scholer-Dahirel A,
Pelon F, Bourachot B, Cardon M, Sirven P, Magagna I, Fuhrmann L,
Bernard C, et al: Fibroblast Heterogeneity and immunosuppressive
environment in human breast cancer. Cancer Cell. 33:463–479. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Hu H, Piotrowska Z, Hare PJ, Chen H,
Mulvey HE, Mayfield A, Noeen S, Kattermann K, Greenberg M, Williams
A, et al: Three subtypes of lung cancer fibroblasts define distinct
therapeutic paradigms. Cancer Cell. 39:1531–1547. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Affo S, Nair A, Brundu F, Ravichandra A,
Bhattacharjee S, Matsuda M, Chin L, Filliol A, Wen W, Song X, et
al: Promotion of cholangiocarcinoma growth by diverse
cancer-associated fibroblast subpopulations. Cancer Cell.
39:866–882. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
LeBleu VS, Taduri G, O'Connell J, Teng Y,
Cooke VG, Woda C, Sugimoto H and Kalluri R: Origin and function of
myofibroblasts in kidney fibrosis. Nat Med. 19:1047–1053. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Jotzu C, Alt E, Welte G, Li J, Hennessy
BT, Devarajan E, Krishnappa S, Pinilla S, Droll L and Song YH:
Adipose tissue derived stem cells differentiate into
carcinoma-associated fibroblast-like cells under the influence of
tumor derived factors. Cell Oncol (Dordr). 34:55–67. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Elenbaas B and Weinberg RA: Heterotypic
signaling between epithelial tumor cells and fibroblasts in
carcinoma formation. Exp Cell Res. 264:169–184. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Fang T, Lv H, Lv G, Li T, Wang C, Han Q,
Yu L, Su B, Guo L, Huang S, et al: Tumor-derived exosomal
miR-1247-3p induces cancer-associated fibroblast activation to
foster lung metastasis of liver cancer. Nat Commun. 9:1912018.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Comito G, Giannoni E, Segura CP,
Barcellos-de-Souza P, Raspollini MR, Baroni G, Lanciotti M, Serni S
and Chiarugi P: Cancer-associated fibroblasts and M2-polarized
macrophages synergize during prostate carcinoma progression.
Oncogene. 33:2423–2431. 2014. View Article : Google Scholar
|
|
18
|
Rhim AD, Oberstein PE, Thomas DH, Mirek
ET, Palermo CF, Sastra SA, Dekleva EN, Saunders T, Becerra CP,
Tattersall IW, et al: Stromal elements act to restrain, rather than
support, pancreatic ductal adenocarcinoma. Cancer Cell. 25:735–747.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ozdemir BC, Pentcheva-Hoang T, Carstens
JL, Zheng X, Wu CC, Simpson TR, Laklai H, Sugimoto H, Kahlert C,
Novitskiy SV, et al: Depletion of carcinoma-associated fibroblasts
and fibrosis induces immunosuppression and accelerates pancreas
cancer with reduced survival. Cancer Cell. 25:719–734. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Vinogradov S, Warren G and Wei X:
Macrophages associated with tumors as potential targets and
therapeutic intermediates. Nanomedicine(Lond). 9:695–707. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Larionova I, Cherdyntseva N, Liu T,
Patysheva M, Rakina M and Kzhyshkowska J: Interaction of
tumor-associated macrophages and cancer chemotherapy.
Oncoimmunology. 8:15960042019. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Rodriguez-Garcia A, Lynn RC, Poussin M,
Eiva MA, Shaw LC, O'Connor RS, Minutolo NG, Casado-Medrano V, Lopez
G, Matsuyama T and Powell DJ Jr: CAR-T cell-mediated depletion of
immunosuppressive tumor-associated macrophages promotes endogenous
antitumor immunity and augments adoptive immunotherapy. Nat Commun.
12:8772021. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Takeya M and Komohara Y: Role of
tumor-associated macrophages in human malignancies: Friend or foe?
Pathol Int. 66:491–505. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Biswas SK and Mantovani A: Macrophage
plasticity and interaction with lymphocyte subsets: Cancer as a
paradigm. Nat Immunol. 11:889–896. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
van Dalen FJ, van Stevendaal MHME,
Fennemann FL, Verdoes M and Ilina O: Molecular repolarisation of
tumour-associated macrophages. Molecules. 24:92018. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Cheng H, Wang Z, Fu L and Xu T: Macrophage
polarization in the development and progression of ovarian cancers:
An overview. Front Oncol. 9:4212019. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Li S, Yu J, Huber A, Kryczek I, Wang Z,
Jiang L, Li X, Du W, Li G, Wei S, et al: Metabolism drives
macrophage heterogeneity in the tumor microenvironment. Cell Rep.
39:1106092022. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Wang Y, Tiruthani K, Li S, Hu M, Zhong G,
Tang Y, Roy S, Zhang L, Tan J, Liao C and Liu R: mRNA delivery of a
bispecific single-domain antibody to polarize tumor-associated
macrophages and synergize immunotherapy against liver malignancies.
Adv Mater. 33:e20076032021. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Su S, Liu Q, Chen J, Chen J, Chen F, He C,
Huang D, Wu W, Lin L, Huang W, et al: A positive feedback loop
between mesenchymal-like cancer cells and macrophages is essential
to breast cancer metastasis. Cancer Cell. 25:605–620. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Vickman RE, Broman MM, Lanman NA, Franco
OE, Sudyanti PAG, Ni Y, Ji Y, Helfand BT, Petkewicz J, Paterakos
MC, et al: Heterogeneity of human prostate carcinoma-associated
fibroblasts implicates a role for subpopulations in myeloid cell
recruitment. Prostate. 80:173–185. 2020. View Article : Google Scholar
|
|
31
|
Augsten M, Hagglof C, Olsson E, Stolz C,
Tsagozis P, Levchenko T, Frederick MJ, Borg A, Micke P, Egevad L
and Ostman A: CXCL14 is an autocrine growth factor for fibroblasts
and acts as a multi-modal stimulator of prostate tumor growth. Proc
Natl Acad Sci USA. 106:3414–3419. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Seckinger A, Delgado JA, Moser S, Moreno
L, Neuber B, Grab A, Lipp S, Merino J, Prosper F, Emde M, et al:
Target expression, generation, preclinical activity, and
pharmacokinetics of the BCMA-T cell bispecific antibody EM801 for
multiple myeloma treatment. Cancer Cell. 31:396–410. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Zhang X, Xu J, Zhu H, Wang Y, Wang L, Fan
L, Wu YJ, Li JY and Xu W: Negative prognostic impact of low
absolute CD4(+) T cell counts in peripheral blood in mantle cell
lymphoma. Cancer Sci. 107:1471–1476. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Arpaia N, Campbell C, Fan X, Dikiy S, van
der Veeken J, deRoos P, Liu H, Cross JR, Pfeffer K, Coffer PJ and
Rudensky AY: Metabolites produced by commensal bacteria promote
peripheral regulatory T-cell generation. Nature. 504:451–455. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Chen X, Du Y, Hu Q and Huang Z:
Tumor-derived CD4+CD25+regulatory T cells inhibit dendritic cells
function by CTLA-4. Pathol Res Pract. 213:245–249. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Burkholder B, Huang R, Burgess R, Luo S,
Jones VS, Zhang W, Lv ZQ, Gao CY, Wang BL, Zhang YM and Huang RP:
Tumor-induced perturbations of cytokines and immune cell networks.
Biochim Biophys Acta. 1845:182–201. 2014.PubMed/NCBI
|
|
37
|
Talmadge JE and Gabrilovich DI: History of
myeloid-derived suppressor cells. Nat Rev Cancer. 13:739–752. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Hegde S, Leader AM and Merad M: MDSC:
Markers, development, states, and unaddressed complexity. Immunity.
54:875–884. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Wang L, Si W, Yu X, Piffko A, Dou X, Ding
X, Bugno J, Yang K, Wen C, Zhang L, et al: Epitranscriptional
regulation of TGF-beta pseudoreceptor BAMBI by m6A/YTHDF2 drives
extrinsic radioresistance. J Clin Invest. 133:e1729192023.
View Article : Google Scholar
|
|
40
|
Zhou J, Xu H, Li X, Liu H, Sun Z, Li J,
Tang Y, Gao H, Zhao K, Ding C and Gao X: Targeting tumorous
Circ-E-Cadherinencoded C-E-Cad inhibits the recruitment and
function of breast cancer-associated myeloid-derived suppressor
cells. Pharmacol Res. 204:1072042024. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Gregory AD and Houghton AM:
Tumor-associated neutrophils: New targets for cancer therapy.
Cancer Res. 71:2411–2416. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Coffelt SB, Wellenstein MD and de Visser
KE: Neutrophils in cancer: Neutral no more. Nat Rev Cancer.
16:431–446. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Shaul ME and Fridlender ZG:
Tumour-associated neutrophils in patients with cancer. Nat Rev Clin
Oncol. 16:601–620. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Melstrom LG, Salazar MD and Diamond DJ:
The pancreatic cancer microenvironment: A true double agent. J Surg
Oncol. 116:7–15. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Kalafati L, Kourtzelis I,
Schulte-Schrepping J, Li X, Hatzioannou A, Grinenko T, Hagag E,
Sinha A, Has C, Dietz S, et al: Innate immune training of
granulopoiesis promotes anti-tumor activity. Cell. 183:771–785.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Cui C, Chakraborty K, Tang XA, Zhou G,
Schoenfelt KQ, Becker KM, Hoffman A, Chang YF, Blank A, Reardon CA,
et al: Neutrophil elastase selectively kills cancer cells and
attenuates tumorigenesis. Cell. 184:3163–3177. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Xiao Y, Cong M, Li J, He D, Wu Q, Tian P,
Wang Y, Yang S, Liang C, Liang Y, et al: Cathepsin C promotes
breast cancer lung metastasis by modulating neutrophil infiltration
and neutrophil extracellular trap formation. Cancer Cell.
39:423–437. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Jaillon S, Ponzetta A, Di Mitri D, Santoni
A, Bonecchi R and Mantovani A: Neutrophil diversity and plasticity
in tumour progression and therapy. Nat Rev Cancer. 20:485–503.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Xu X, Ye L, Zhang Q, Shen H, Li S, Zhang
X, Ye M and Liang T: Group-2 innate lymphoid cells promote HCC
progression through CXCL2-neutrophil-induced immunosuppression.
Hepatology. 74:2526–2543. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Kuang Z, Wilson JJ, Luo S, Zhu S and Huang
R: Deciphering asthma biomarkers with protein profiling technology.
Int J Inflamm. 2015:6306372015.
|
|
51
|
Dicarlo M, Bianchi N, Ferretti C, Orciani
M, Di Primio R and Mattioli-Belmonte M: Evidence supporting a
paracrine effect of IGF-1/VEGF on human mesenchymal stromal cell
commitment. Cells Tissues Organs. 201:333–341. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Goel HL and Mercurio AM: VEGF targets the
tumour cell. Nat Rev Cancer. 13:871–882. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Iams WT and Lovly CM: Molecular pathways:
Clinical applications and future direction of insulin-like growth
factor-1 receptor pathway blockade. Clin Cancer Res. 21:4270–4277.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Sanchez-Lopez E, Flashner-Abramson E,
Shalapour S, Zhong Z, Taniguchi K, Levitzki A and Karin M:
Targeting colorectal cancer via its microenvironment by inhibiting
IGF-1 receptor-insulin receptor substrate and STAT3 signaling.
Oncogene. 35:2634–2644. 2016. View Article : Google Scholar :
|
|
55
|
Ikushima H and Miyazono K: TGFbeta
signalling: A complex web in cancer progression. Nat Rev Cancer.
10:415–424. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Etscheid M, Beer N, Kress JA, Seitz R and
Dodt J: Inhibition of bFGF/EGF-dependent endothelial cell
proliferation by the hyaluronan-binding protease from human plasma.
Eur J Cell Biol. 82:597–604. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Mueller MM and Fusenig NE: Friends or
foes-bipolar effects of the tumour stroma in cancer. Nat Rev
Cancer. 4:839–849. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Sahai E, Astsaturov I, Cukierman E,
DeNardo DG, Egeblad M, Evans RM, Fearon D, Greten FR, Hingorani SR,
Hunter T, et al: A framework for advancing our understanding of
cancer-associated fibroblasts. Nat Rev Cancer. 20:174–186. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Shi Z, Yang W, Chen L, Yang DH, Zhou Q,
Zhu J, Chen JJ, Huang RC, Chen ZS and Huang RP: Enhanced
chemosensitization in multidrug-resistant human breast cancer cells
by inhibition of IL-6 and IL-8 production. Breast Cancer Res Treat.
135:737–747. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Mannino MH, Zhu Z, Xiao H, Bai Q,
Wakefield MR and Fang Y: The paradoxical role of IL-10 in immunity
and cancer. Cancer Lett. 367:103–107. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Kasprzak A: The role of tumor
microenvironment cells in colorectal cancer (CRC) cachexia. Int J
Mol Sci. 22:15652021. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Lan T, Chen L and Wei X: Inflammatory
cytokines in cancer: Comprehensive understanding and clinical
progress in gene therapy. Cells. 10:1002021. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Villanueva J, Philip J, Entenberg D,
Chaparro CA, Tanwar MK, Holland EC and Tempst P: Serum peptide
profiling by magnetic particle-assisted, automated sample
processing and MALDI-TOF mass spectrometry. Anal Chem.
76:1560–1570. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Govorukhina NI, Keizer-Gunnink A, van der
Zee AGJ, de Jong S, de Bruijn HWA and Bischoff R: Sample
preparation of human serum for the analysis of tumor markers.
Comparison of different approaches for albumin and gamma-globulin
depletion. J Chromatogr A. 1009:171–178. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Tirumalai RS, Chan KC, Prieto DA, Issaq
HJ, Conrads TP and Veenstra TD: Characterization of the low
molecular weight human serum proteome. Mol Cell Proteomics.
2:1096–1103. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Beutgen VM, Shinkevich V, Porschke J,
Meena C, Steitz AM, von Strandmann P, Graumann J and Gómez-Serrano
M: Secretome analysis using affinity proteomics and immunoassays: A
focus on tumor biology. Mol Cell Proteomics. 23:1008302024.
View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Ding Z, Wang N, Ji N and Chen Z:
Proteomics technologies for cancer liquid biopsies. Mol Cancer.
21:532022. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Sutandy FXR, Qian J, Chen C and Zhu H:
Overview of protein microarrays. Curr Protoc Protein Sci Chapter.
27:21–27. 2013.
|
|
69
|
Sanchez-Carbayo M: Antibody arrays:
Technical considerations and clinical applications in cancer. Clin
Chem. 52:1651–1659. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Huang R, Jiang W, Yang J, Mao YQ, Zhang Y,
Yang W, Yang D, Burkholder B, Huang RF and Huang RP: A biotin
label-based antibody array for high-content profiling of protein
expression. Cancer Genom Proteom. 7:129–141. 2010.
|
|
71
|
Wei W, Zhou H, Chen P, Huang XL, Huang L,
Liang LJ, Guo CH, Zhou CF, Yu L, Fan LS and Wang W:
Cancer-associated fibroblast-derived PAI-1 promotes lymphatic
metastasis via the induction of EndoMT in lymphatic endothelial
cells. J Exp Clin Canc Res. 42:1602023. View Article : Google Scholar
|
|
72
|
Wei WF, Chen XJ, Liang LJ, Yu L, Wu XG,
Zhou CF, Wang ZC, Fan LS, Hu Z, Liang L and Wang W:
Periostin+ cancer-associated fibroblasts promote lymph
node metastasis by impairing the lymphatic endothelial barriers in
cervical squamous cell carcinoma. Mol Oncol. 15:210–227. 2021.
View Article : Google Scholar
|
|
73
|
Sun C, Li X, Guo E, Li N, Zhou B, Lu H,
Huang J, Xia M, Shan W, Wang B, et al: MCP-1/CCR-2 axis in
adipocytes and cancer cell respectively facilitates ovarian cancer
peritoneal metastasis. Oncogene. 39:1681–1695. 2020. View Article : Google Scholar
|
|
74
|
Ryan D, Koziol J and ElShamy WM: Targeting
AXL and RAGE to prevent geminin overexpression-induced
triple-negative breast cancer metastasis. Sci Rep. 9:191502019.
View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Han K, Kim A and Kim D: Enhanced
anti-cancer effects of conditioned medium from hypoxic human adult
dermal fibroblasts on cervical cancer cells. Int J Mol Sci.
23:51342022. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Huang S, He L, Zhao Y, Wei Y, Wang Q, Gao
Y and Jiang X: TREM1+ tumor-associated macrophages secrete CCL7 to
promote hepatocellular carcinoma metastasis. J Cancer Res Clin.
150:3202024. View Article : Google Scholar
|
|
77
|
Zheng Y, Wang N, Wang S, Zhang J, Yang B
and Wang Z: Chronic psychological stress promotes breast cancer
pre-metastatic niche formation by mobilizing splenic MDSCs via
TAM/CXCL1 signaling. J Exp Clin Canc Res. 42:1292023. View Article : Google Scholar
|
|
78
|
Tatsuno R, Ichikawa J, Komohara Y, Pan C,
Kawasaki T, Enomoto A, Aoki K, Hayakawa K, Iwata S, Jubashi T and
Haro H: Pivotal role of IL-8 derived from the interaction between
osteosarcoma and tumor-associated macrophages in osteosarcoma
growth and metastasis via the FAK pathway. Cell Death Dis.
15:1082024. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Kim SY, Park S, Kim S and Ko J:
CD133-containing microvesicles promote cancer progression by
inducing M2-like tumor-associated macrophage polarization in the
tumor microenvironment of colorectal cancer. Carcinogenesis.
45:300–310. 2024. View Article : Google Scholar
|
|
80
|
Licarete E, Rauca VF, Luput L, Patras L,
Sesarman A and Banciu M: The prednisolone phosphate-induced
suppression of the angiogenic function of tumor-associated
macrophages enhances the antitumor effects of doxorubicin on
B16.F10 murine melanoma cells in vitro. Oncol Rep. 42:2694–2705.
2019.PubMed/NCBI
|
|
81
|
Wang Y, Chen J, Yang L, Li J, Wu W, Huang
M, Lin L and Su S: Tumor-contacted neutrophils promote metastasis
by a CD90-TIMP-1 juxtacrine-paracrine loop. Clin Cancer Res.
25:1957–1969. 2019. View Article : Google Scholar
|
|
82
|
Lee T, Chen T, Kuo Y, Lan H, Yang M and
Chu P: Tumor-associated tissue eosinophilia promotes angiogenesis
and metastasis in head and neck squamous cell carcinoma. Neoplasia.
35:1008552023. View Article : Google Scholar
|
|
83
|
Benzing C, Lam H, Tsang CM, Rimmer A,
Arroyo-Berdugo Y, Calle Y and Wells CM: TIMP-2 secreted by
monocyte-like cells is a potent suppressor of invadopodia formation
in pancreatic cancer cells. BMC Cancer. 19:12142019. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Li Y, Jiang M, Aye L, Luo L, Zhang Y, Xu
F, Wei Y, Peng D, He X, Gu J, et al: UPP1 promotes lung
adenocarcinoma progression through the induction of an
immunosuppressive microenvironment. Nat Commun. 15:12002024.
View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Zhu H, Liu Y, Liu D, Ma YD, Hu ZY, Wang
XY, Gu CS, Zhong Y, Long T, Kan HP and Li ZG: Role of
TGFβ3-Smads-Sp1 axis in DcR3-mediated immune escape of
hepatocellular carcinoma. Oncogenesis. 8:432019. View Article : Google Scholar
|
|
86
|
Xie G, Cheng T, Lin J, Zhang L, Zheng J,
Liu Y, Xie G, Wang B and Yuan Y: Local angiotensin II contributes
to tumor resistance to checkpoint immunotherapy. J Immunother
Cancer. 6:882018. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Jiang K, Zhang Q, Fan Y, Li J, Zhang J,
Wang W, Fan J, Guo Y, Liu S, Hao D, et al: MYC inhibition
reprograms tumor immune microenvironment by recruiting T
lymphocytes and activating the CD40/CD40L system in osteosarcoma.
Cell Death Discov. 8:1172022. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Wang X, Wang F, Zhang Z, Yang X, Zhang R
and Song J: STK3 suppresses ovarian cancer progression by
activating NF-κB signaling to recruit CD8+ T-Cells. J Immunol Res.
2020:1–17. 2020. View Article : Google Scholar
|
|
89
|
Zhang L, Cascio S, Mellors JW, Buckanovich
RJ and Osmanbeyoglu HU: Single-cell analysis reveals the stromal
dynamics and tumor-specific characteristics in the microenvironment
of ovarian cancer. Commun Biol. 7:2023.06.07.544095. 2024.
|
|
90
|
Sheng N, Shindo K, Ohuchida K, Shinkawa T,
Zhang B, Feng H, Yamamoto T, Moriyama T, Ikenaga N, Nakata K, et
al: TAK1 promotes an immunosuppressive tumor microenvironment
through cancer-associated fibroblast phenotypic conversion in
pancreatic ductal adenocarcinoma. Clin Cancer Res. 30:5138–5153.
2024. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Nakamura K, Kiniwa Y and Okuyama R: CCL5
production by fibroblasts through a local renin-angiotensin system
in malignant melanoma affects tumor immune responses. J Cancer Res
Clin. 147:1993–2001. 2021. View Article : Google Scholar
|
|
92
|
SenGupta S, Hein LE, Xu Y, Zhang J,
Konwerski JR, Li Y, Johnson C, Cai D, Smith JL and Parent CA:
Triple-negative breast cancer cells recruit neutrophils by
secreting TGF-β and CXCR2 ligands. Front Immunol. 12:6599962021.
View Article : Google Scholar
|
|
93
|
Ogawa R, Yamamoto T, Hirai H, Hanada K,
Kiyasu Y, Nishikawa G, Mizuno R, Inamoto S, Itatani Y, Sakai Y and
Kawada K: Loss of SMAD4 promotes colorectal cancer progression by
recruiting tumor-associated neutrophils via the CXCL1/8-CXCR2 axis.
Clin Cancer Res. 25:2887–2899. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Germann M, Zangger N, Sauvain M, Sempoux
C, Bowler AD, Wirapati P, Kandalaft LE, Delorenzi M, Tejpar S,
Coukos G and Radtke F: Neutrophils suppress tumor-infiltrating T
cells in colon cancer via matrix metalloproteinase-mediated
activation of TGFβ. Embo Mol Med. 12:e106812020. View Article : Google Scholar
|
|
95
|
Chan Y, Tan H, Lu Y, Zhang C, Cheng CS, Wu
J, Wang N and Feng Y: Pancreatic melatonin enhances anti-tumor
immunity in pancreatic adenocarcinoma through regulating
tumor-associated neutrophils infiltration and NETosis. Acta Pharm
Sin B. 13:1554–1567. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Su S, Chen J, Yao H, Liu J, Yu S, Lao L,
Wang M, Luo M, Xing Y, Chen F, et al:
CD10+GPR77+ cancer-associated fibroblasts
promote cancer formation and chemoresistance by sustaining cancer
stemness. Cell. 172:841–856. 2018. View Article : Google Scholar
|
|
97
|
Zeng W, Xiong L, Wu W, Li S, Liu J, Yang
L, Lao L, Huang P, Zhang M, Chen H, et al: CCL18 signaling from
tumor-associated macrophages activates fibroblasts to adopt a
chemoresistance-inducing phenotype. Oncogene. 42:224–237. 2023.
View Article : Google Scholar :
|
|
98
|
Papaccio F, Kovacs D, Bellei B, Caputo S,
Migliano E, Cota C and Picardo M: Profiling cancer-associated
fibroblasts in melanoma. Int J Mol Sci. 22:72552021. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Zhou B, Sun C, Li N, Shan W, Lu H, Guo L,
Guo E, Xia M, Weng D, Meng L, et al: Cisplatin-induced CCL5
secretion from CAFs promotes cisplatin-resistance in ovarian cancer
via regulation of the STAT3 and PI3K/Akt signaling pathways. Int J
Oncol. 48:2087–2097. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Che Y, Wang J, Li Y, Lu Z, Huang J, Sun S,
Mao S, Lei Y, Zang R, Sun N and He J: Cisplatin-activated PAI-1
secretion in the cancer-associated fibroblasts with paracrine
effects promoting esophageal squamous cell carcinoma progression
and causing chemoresistance. Cell Death Dis. 9:7592018. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Chrisochoidou Y, Roy R, Farahmand P,
Gonzalez G, Doig J, Krasny L, Rimmer EF, Willis AE, MacFarlane M
and Huang PH: Crosstalk with lung fibroblasts shapes the growth and
therapeutic response of mesothelioma cells. Cell Death Dis.
14:7252023. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Wang C, Wang Y, Hong T, Ye J, Chu C, Zuo
L, Zhang J and Cui X: Targeting a positive regulatory loop in the
tumor-macrophage interaction impairs the progression of clear cell
renal cell carcinoma. Cell Death Differ. 28:932–951. 2021.
View Article : Google Scholar :
|
|
103
|
Liu H, Liang Z, Zhou C, Zeng Z, Wang F, Hu
T, He X, Wu X, Wu X and Lan P: Mutant KRAS triggers functional
reprogramming of tumor-associated macrophages in colorectal cancer.
Signal Transduct Target Ther. 6:1442021. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Re OL, Mazza T, Giallongo S, Sanna P,
Rappa F, Luong TV, Volti GL, Drovakova A, Roskams T, Van Haele M,
et al: Loss of histone macroH2A1 in hepatocellular carcinoma cells
promotes paracrine-mediated chemoresistance and CD4+
CD25+ FoxP3+ regulatory T cells activation.
Theranostics. 10:910–924. 2020. View Article : Google Scholar :
|
|
105
|
Guo Z, Zhang H, Fu Y, Kuang J, Zhao B,
Zhang L, Lin J, Lin S, Wu D and Xie G: Cancer-associated
fibroblasts induce growth and radioresistance of breast cancer
cells through paracrine IL-6. Cell Death Discov. 9:62023.
View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Chu T, Yang J, Huang T and Liu H:
Crosstalk with cancer-associated fibroblasts increases the growth
and radiation survival of cervical cancer cells. Radiat Res.
181:540–547. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Cao Y, Yin Y, Wang X, Wu Z, Liu Y, Zhang
F, Lin J, Huang Z and Zhou L: Sublethal irradiation promotes the
metastatic potential of hepatocellular carcinoma cells. Cancer Sci.
112:265–274. 2021. View Article : Google Scholar :
|
|
108
|
Arshad A, Deutsch E and Vozenin M:
Simultaneous irradiation of fibroblasts and carcinoma cells repress
the secretion of soluble factors able to stimulate carcinoma cell
migration. PLoS One. 10:e1154472015. View Article : Google Scholar
|