|
1
|
Fidler IJ: The pathogenesis of cancer
metastasis: The 'seed and soil' hypothesis revisited. Nat Rev
Cancer. 3:453–458. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Zhao Y, Shen M, Wu L, Yang H, Yao Y, Yang
Q, Du J, Liu L, Li Y and Bai Y: Stromal cells in the tumor
microenvironment: accomplices of tumor progression? Cell Death Dis.
14:5872023. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Glabman RA, Choyke PL and Sato N:
Cancer-associated fibroblasts: Tumorigenicity and targeting for
cancer therapy. Cancers (Basel). 14:39062022. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sun H, Wang X, Wang X, Xu M and Sheng W:
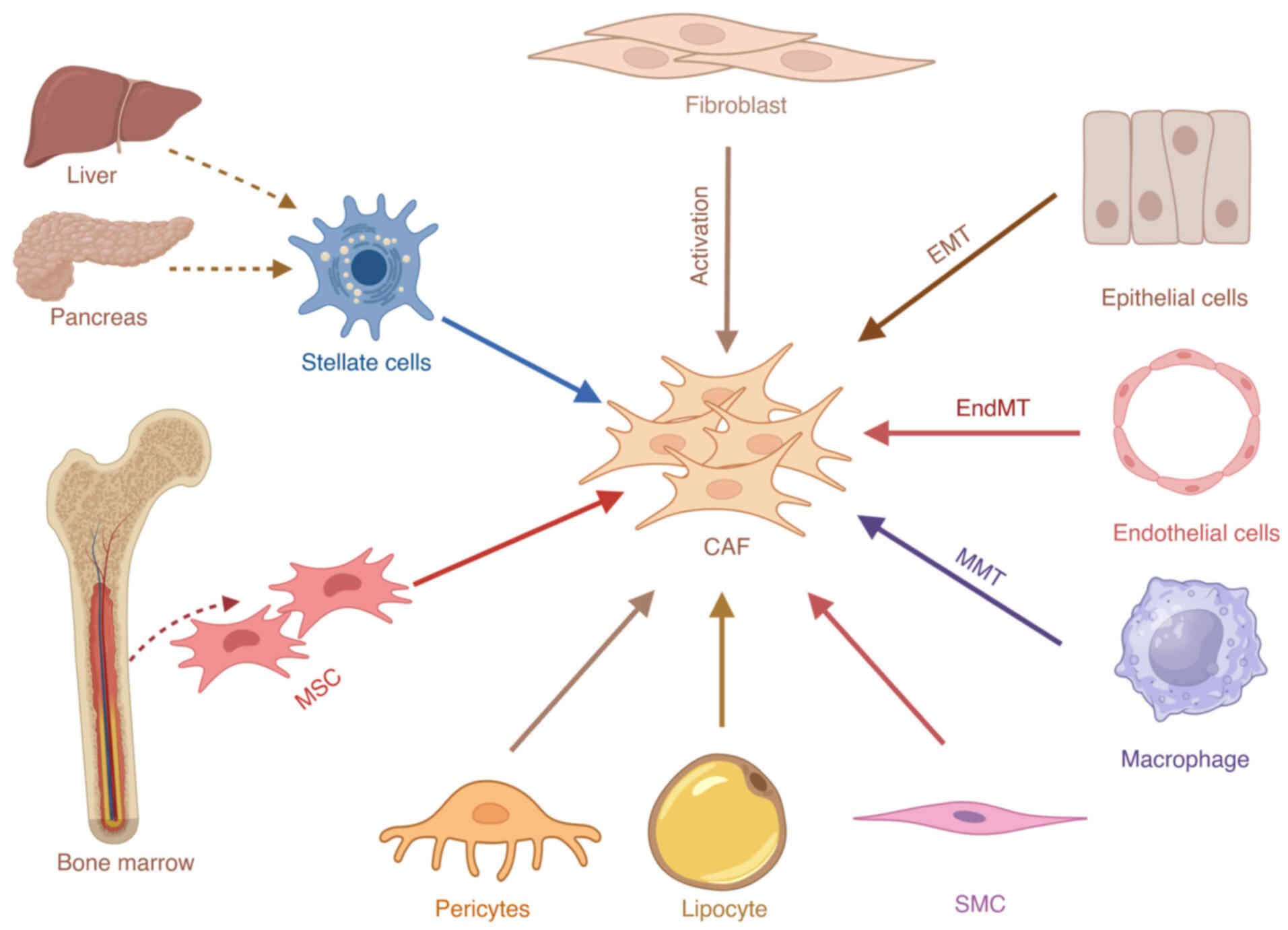
The role of cancer-associated fibroblasts in tumorigenesis of
gastric cancer. Cell Death Dis. 13:8742022. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Peng Z, Tong Z, Ren Z, Ye M and Hu K:
Cancer-associated fibroblasts and its derived exosomes: A new
perspective for reshaping the tumor microenvironment. Mol Med.
29:662023. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Li C, Teixeira AF, Zhu HJ and Ten Dijke P:
Cancer associated-fibroblast-derived exosomes in cancer
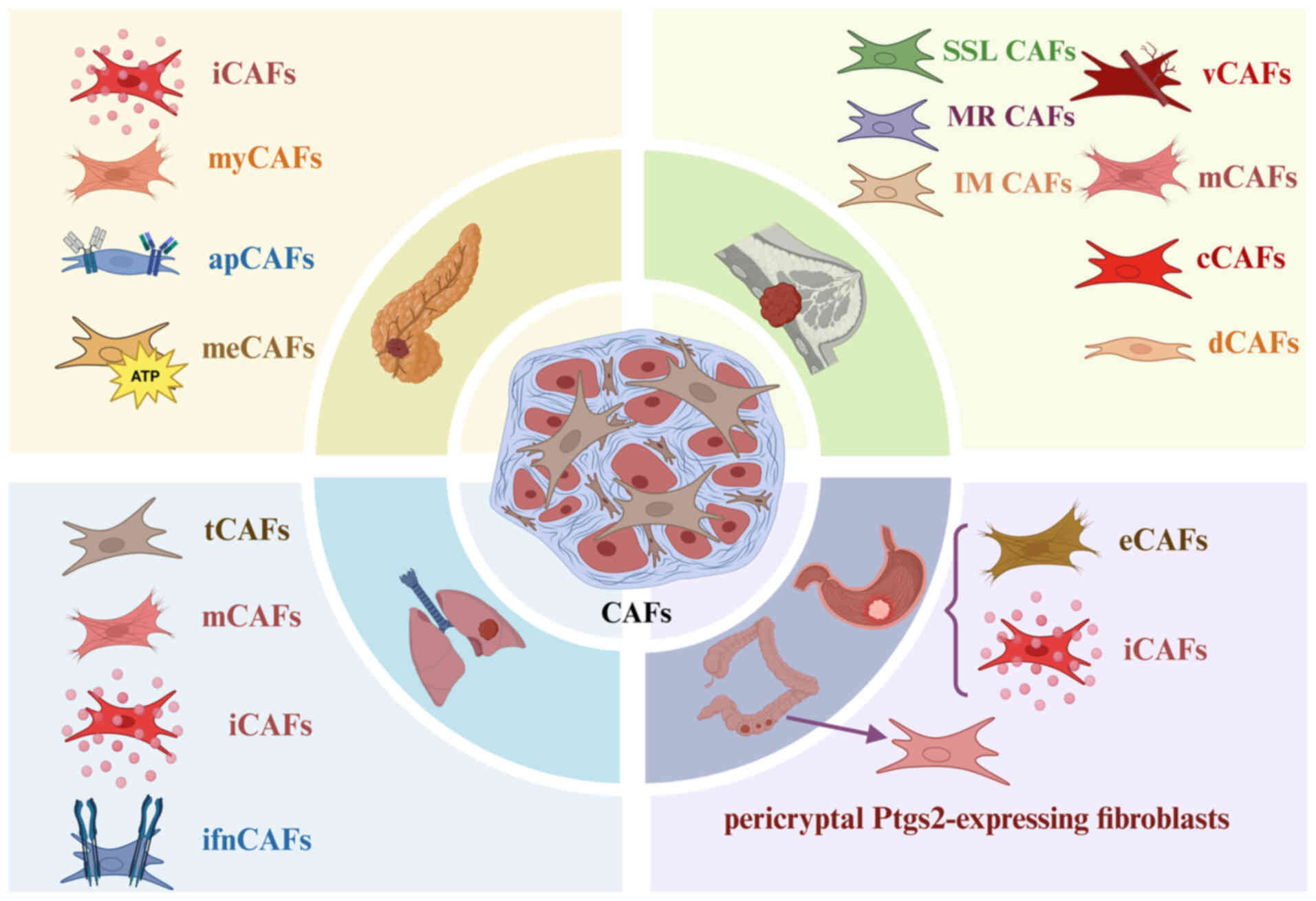
progression. Mol Cancer. 20:1542021. View Article : Google Scholar :
|
|
7
|
Mao X, Xu J, Wang W, Liang C, Hua J, Liu
J, Zhang B, Meng Q, Yu X and Shi S: Crosstalk between
cancer-associated fibroblasts and immune cells in the tumor
microenvironment: New findings and future perspectives. Mol Cancer.
20:1312021. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Arima Y, Matsueda S and Saya H:
Significance of cancer-associated fibroblasts in the interactions
of cancer cells with the tumor microenvironment of heterogeneous
tumor tissue. Cancers (Basel). 15:25362023. View Article : Google Scholar
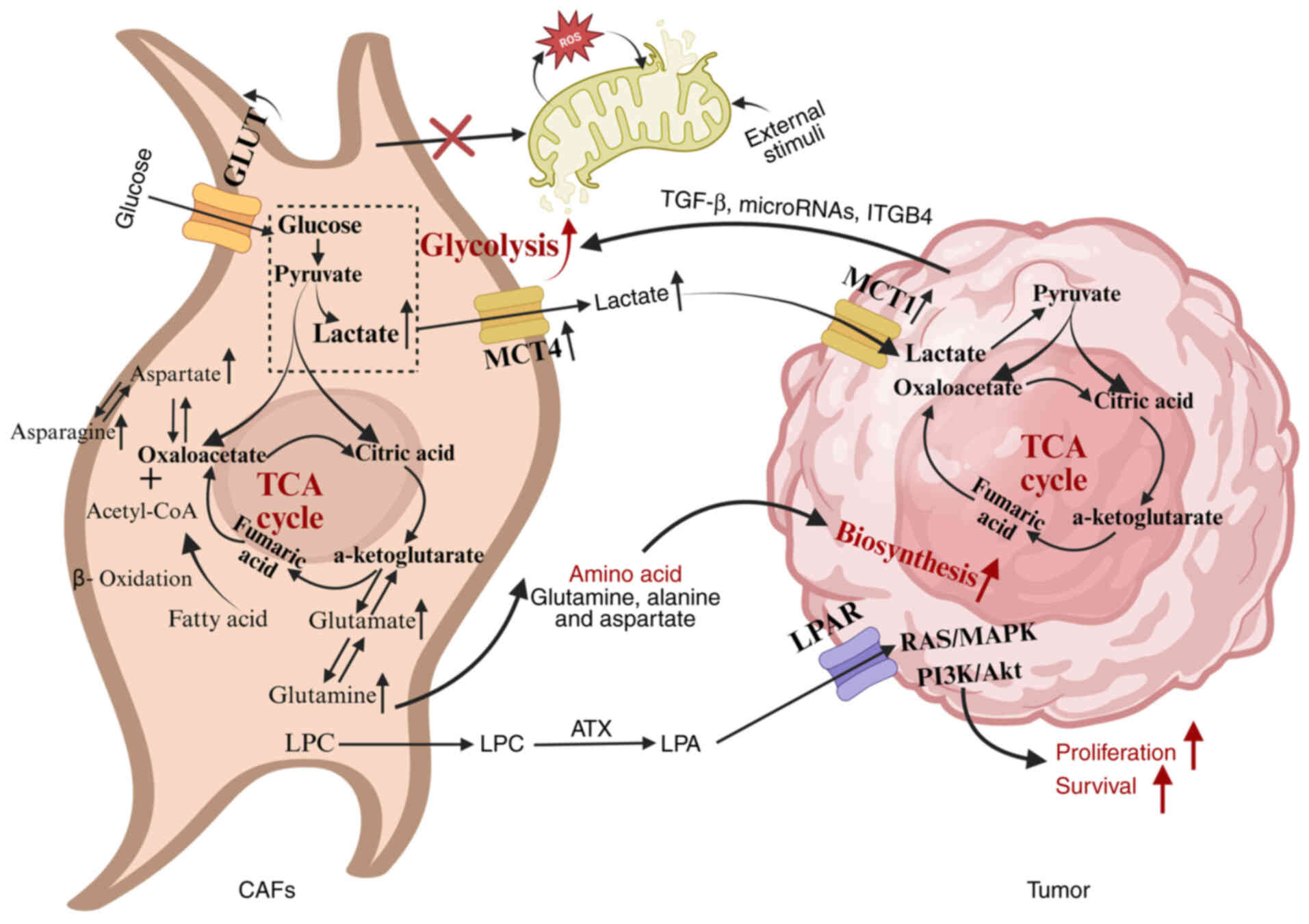
|
|
9
|
Zhang S, Xiao X, Yi Y, Wang X, Zhu L, Shen
Y, Lin D and Wu C: Tumor initiation and early tumorigenesis:
Molecular mechanisms and interventional targets. Signal Transduct
Target Ther. 9:1492024. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Martínez-Reyes I and Chandel NS:
Mitochondrial TCA cycle metabolites control physiology and disease.
Nat Commun. 11:1022020. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Akter R, Awais M, Boopathi V, Ahn JC, Yang
DC, Kang SC, Yang DU and Jung SK: Inversion of the warburg effect:
Unraveling the metabolic nexus between obesity and cancer. ACS
Pharmacol Transl Sci. 7:560–569. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Yang K, Wang X, Song C, He Z, Wang R, Xu
Y, Jiang G, Wan Y, Mei J and Mao W: The role of lipid metabolic
reprogramming in tumor microenvironment. Theranostics.
13:1774–1808. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Chen J, Cui L, Lu S and Xu S: Amino acid
metabolism in tumor biology and therapy. Cell Death Dis. 15:422024.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Medina M: Metabolic reprogramming is a
Hallmark of metabolism itself. Bioessays. 42:e20000582020.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Wu D, Zhuo L and Wang X: Metabolic
reprogramming of carcinoma-associated fibroblasts and its impact on
metabolic heterogeneity of tumors. Semin Cell Dev Biol. 64:125–131.
2017. View Article : Google Scholar
|
|
16
|
Avagliano A, Granato G, Ruocco MR, Romano
V, Belviso I, Carfora A, Montagnani S and Arcucci A: Metabolic
reprogramming of cancer associated fibroblasts: The slavery of
stromal fibroblasts. Biomed Res Int. 2018:60754032018. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Liang L, Li W, Li X, Jin X, Liao Q, Li Y
and Zhou Y: 'Reverse Warburg effect' of cancer-associated
fibroblasts (Review). Int J Oncol. 60:672022. View Article : Google Scholar
|
|
18
|
Hu D, Li Z, Zheng B, Lin X, Pan Y, Gong P,
Zhuo W, Hu Y, Chen C, Chen L, et al: Cancer-associated fibroblasts
in breast cancer: Challenges and opportunities. Cancer Commun
(Lond). 42:401–434. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Yoon H, Tang CM, Banerjee S, Delgado AL,
Yebra M, Davis J and Sicklick JK: TGF-β1-mediated transition of
resident fibroblasts to cancer-associated fibroblasts promotes
cancer metastasis in gastrointestinal stromal tumor. Oncogenesis.
10:132021. View Article : Google Scholar
|
|
20
|
Hartupee J and Mann DL: Role of
inflammatory cells in fibroblast activation. J Mol Cell Cardiol.
93:143–148. 2016. View Article : Google Scholar :
|
|
21
|
Erez N, Truitt M, Olson P, Arron ST and
Hanahan D: Cancer-associated fibroblasts are activated in incipient
neoplasia to orchestrate tumor-promoting inflammation in an
NF-kappaB-dependent manner. Cancer Cell. 17:135–147. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Sanz-Moreno V, Gaggioli C, Yeo M,
Albrengues J, Wallberg F, Viros A, Hooper S, Mitter R, Féral CC,
Cook M, et al: ROCK and JAK1 signaling cooperate to control
actomyosin contractility in tumor cells and stroma. Cancer Cell.
20:229–245. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Shen H, Yu X, Yang F, Zhang Z, Shen J, Sun
J, Choksi S, Jitkaew S and Shu Y: Reprogramming of normal
fibroblasts into cancer-associated fibroblasts by miRNAs-Mediated
CCL2/VEGFA signaling. PLoS Genet. 12:e10062442016. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Calvo F, Ege N, Grande-Garcia A, Hooper S,
Jenkins RP, Chaudhry SI, Harrington K, Williamson P, Moeendarbary
E, Charras G and Sahai E: Mechanotransduction and YAP-dependent
matrix remodelling is required for the generation and maintenance
of cancer-associated fibroblasts. Nat Cell Biol. 15:637–646. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Sahai E, Astsaturov I, Cukierman E,
DeNardo DG, Egeblad M, Evans RM, Fearon D, Greten FR, Hingorani SR,
Hunter T, et al: A framework for advancing our understanding of
cancer-associated fibroblasts. Nat Rev Cancer. 20:174–186. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Yin C, Evason KJ, Asahina K and Stainier
DY: Hepatic stellate cells in liver development, regeneration, and
cancer. J Clin Invest. 123:1902–1910. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Omary MB, Lugea A, Lowe AW and Pandol SJ:
The pancreatic stellate cell: A star on the rise in pancreatic
diseases. J Clin Invest. 117:50–59. 2007. View Article : Google Scholar :
|
|
28
|
Wang F, Li L, Piontek K, Sakaguchi M and
Selaru FM: Exosome miR-335 as a novel therapeutic strategy in
hepatocellular carcinoma. Hepatology. 67:940–954. 2018. View Article : Google Scholar
|
|
29
|
Peng Y and Li Z and Li Z: GRP78 secreted
by tumor cells stimulates differentiation of bone marrow
mesenchymal stem cells to cancer-associated fibroblasts. Biochem
Biophys Res Commun. 440:558–563. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Shangguan L, Ti X, Krause U, Hai B, Zhao
Y, Yang Z and Liu F: Inhibition of TGF-β/Smad signaling by BAMBI
blocks differentiation of human mesenchymal stem cells to
carcinoma-associated fibroblasts and abolishes their protumor
effects. Stem Cells. 30:2810–2819. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Weber CE, Kothari AN, Wai PY, Li NY,
Driver J, Zapf MA, Franzen CA, Gupta GN, Osipo C, Zlobin A, et al:
Osteopontin mediates an MZF1-TGF-β1-dependent transformation of
mesenchymal stem cells into cancer-associated fibroblasts in breast
cancer. Oncogene. 34:4821–4833. 2015. View Article : Google Scholar
|
|
32
|
Iwano M, Plieth D, Danoff TM, Xue C, Okada
H and Neilson EG: Evidence that fibroblasts derive from epithelium
during tissue fibrosis. J Clin Invest. 110:341–350. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Zeisberg EM, Potenta S, Xie L, Zeisberg M
and Kalluri R: Discovery of endothelial to mesenchymal transition
as a source for carcinoma-associated fibroblasts. Cancer Res.
67:10123–10128. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Tang PC, Chung JY, Xue VW, Xiao J, Meng
XM, Huang XR, Zhou S, Chan AS, Tsang AC, Cheng AS, et al: Smad3
promotes cancer-associated fibroblasts generation via
macrophage-myofibroblast transition. Adv Sci (Weinh).
9:e21012352022. View Article : Google Scholar
|
|
35
|
Tang PM, Zhang YY, Xiao J, Tang PC, Chung
JY, Li J, Xue VW, Huang XR, Chong CC, Ng CF, et al: Neural
transcription factor Pou4f1 promotes renal fibrosis via
macrophage-myofibroblast transition. Proc Natl Acad Sci USA.
117:20741–20752. 2020. View Article : Google Scholar
|
|
36
|
Dulauroy S, Di Carlo SE, Langa F, Eberl G
and Peduto L: Lineage tracing and genetic ablation of ADAM12(+)
perivascular cells identify a major source of profibrotic cells
during acute tissue injury. Nat Med. 18:1262–1270. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Jotzu C, Alt E, Welte G, Li J, Hennessy
BT, Devarajan E, Krishnappa S, Pinilla S, Droll L and Song YH:
Adipose tissue derived stem cells differentiate into
carcinoma-associated fibroblast-like cells under the influence of
tumor derived factors. Cell Oncol (Dordr). 34:55–67. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Wikström P, Marusic J, Stattin P and Bergh
A: Low stroma androgen receptor level in normal and tumor prostate
tissue is related to poor outcome in prostate cancer patients.
Prostate. 69:799–809. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Gieniec KA, Butler LM, Worthley DL and
Woods SL: Cancer-associated fibroblasts-heroes or villains? Br J
Cancer. 121:293–302. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Kanzaki R and Pietras K: Heterogeneity of
cancer-associated fibroblasts: Opportunities for precision
medicine. Cancer Sci. 111:2708–2717. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Nurmik M, Ullmann P, Rodriguez F, Haan S
and Letellier E: In search of definitions: Cancer-associated
fibroblasts and their markers. Int J Cancer. 146:895–905. 2020.
View Article : Google Scholar
|
|
42
|
Hu H, Piotrowska Z, Hare PJ, Chen H,
Mulvey HE, Mayfield A, Noeen S, Kattermann K, Greenberg M, Williams
A, et al: Three subtypes of lung cancer fibroblasts define distinct
therapeutic paradigms. Cancer Cell. 39:1531–1547.e10. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Zhang H, Yue X, Chen Z, Liu C, Wu W, Zhang
N, Liu Z, Yang L, Jiang Q, Cheng Q, et al: Define cancer-associated
fibroblasts (CAFs) in the tumor microenvironment: new opportunities
in cancer immunotherapy and advances in clinical trials. Mol
Cancer. 22:1592023. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Luo H, Xia X, Huang LB, An H, Cao M, Kim
GD, Chen HN, Zhang WH, Shu Y, Kong X, et al: Pan-cancer single-cell
analysis reveals the heterogeneity and plasticity of
cancer-associated fibroblasts in the tumor microenvironment.
13:66192022.PubMed/NCBI
|
|
45
|
Öhlund D, Handly-Santana A, Biffi G,
Elyada E, Almeida AS, Ponz-Sarvise M, Corbo V, Oni TE, Hearn SA,
Lee EJ, et al: Distinct populations of inflammatory fibroblasts and
myofibroblasts in pancreatic cancer. J Exp Med. 214:579–596. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Elyada E, Bolisetty M, Laise P, Flynn WF,
Courtois ET, Burkhart RA, Teinor JA, Belleau P, Biffi G, Lucito MS,
et al: Cross-species single-cell analysis of pancreatic ductal
adenocarcinoma reveals antigen-presenting cancer-associated
fibroblasts. Cancer Discov. 9:1102–1123. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Cords L, Engler S, Haberecker M, Rüschoff
JH, Moch H, de Souza N and Bodenmiller B: Cancer-associated
fibroblast phenotypes are associated with patient outcome in
non-small cell lung cancer. Cancer Cell. 42:396–412.e5. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Li X, Sun Z, Peng G, Xiao Y, Guo J, Wu B,
Li X, Zhou W, Li J, Li Z, et al: Single-cell RNA sequencing reveals
a pro-invasive cancer-associated fibroblast subgroup associated
with poor clinical outcomes in patients with gastric cancer.
Theranostics. 12:620–638. 2022. View Article : Google Scholar :
|
|
49
|
Roulis M, Kaklamanos A, Schernthanner M,
Bielecki P, Zhao J, Kaffe E, Frommelt LS, Qu R, Knapp MS, Henriques
A, et al: Paracrine orchestration of intestinal tumorigenesis by a
mesenchymal niche. Nature. 580:524–529. 2020. View Article : Google Scholar :
|
|
50
|
Bartoschek M, Oskolkov N, Bocci M, Lövrot
J, Larsson C, Sommarin M, Madsen CD, Lindgren D, Pekar G, Karlsson
G, et al: Spatially and functionally distinct subclasses of breast
cancer-associated fibroblasts revealed by single cell RNA
sequencing. Nat Commun. 9:51502018. View Article : Google Scholar :
|
|
51
|
Kazakova AN, Lukina MM, Anufrieva KS,
Bekbaeva IV, Ivanova OM, Shnaider PV, Slonov A, Arapidi GP and
Shender VO: Exploring the diversity of cancer-associated
fibroblasts: Insights into mechanisms of drug resistance. Front
Cell Dev Biol. 12:14031222024. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Huang H, Wang Z, Zhang Y, Pradhan RN,
Ganguly D, Chandra R, Murimwa G, Wright S, Gu X, Maddipati R, et
al: Mesothelial cell-derived antigen-presenting cancer-associated
fibroblasts induce expansion of regulatory T cells in pancreatic
cancer. Cancer Cell. 40:656–673.e7. 2022. View Article : Google Scholar
|
|
53
|
Biffi G, Oni TE, Spielman B, Hao Y, Elyada
E, Park Y, Preall J and Tuveson DA: IL1-Induced JAK/STAT signaling
is antagonized by TGFβ to shape CAF heterogeneity in pancreatic
ductal adenocarcinoma. Cancer Discov. 9:282–301. 2019. View Article : Google Scholar
|
|
54
|
Wang Y, Liang Y, Xu H, Zhang X, Mao T, Cui
J, Yao J, Wang Y, Jiao F, Xiao X, et al: Single-cell analysis of
pancreatic ductal adenocarcinoma identifies a novel fibroblast
subtype associated with poor prognosis but better immunotherapy
response. Cell Discov. 7:362021. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Niu N, Shen X, Wang Z, Chen Y, Weng Y, Yu
F, Tang Y, Lu P, Liu M, Wang L, et al: Tumor cell-intrinsic
epigenetic dysregulation shapes cancer-associated fibroblasts
heterogeneity to metabolically support pancreatic cancer. Cancer
Cell. 42:869–884.e9. 2024. View Article : Google Scholar
|
|
56
|
Lambrechts D, Wauters E, Boeckx B, Aibar
S, Nittner D, Burton O, Bassez A, Decaluwé H, Pircher A, Van den
Eynde K, et al: Phenotype molding of stromal cells in the lung
tumor microenvironment. Nat Med. 24:1277–1289. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Foster DS, Januszyk M, Delitto D, Yost KE,
Griffin M, Guo J, Guardino N, Delitto AE, Chinta M, Burcham AR, et
al: Multiomic analysis reveals conservation of cancer-associated
fibroblast phenotypes across species and tissue of origin. Cancer
Cell. 40:1392–1406.e7. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Ma C, Yang C, Peng A, Sun T, Ji X, Mi J,
Wei L, Shen S and Feng Q: Pan-cancer spatially resolved single-cell
analysis reveals the crosstalk between cancer-associated
fibroblasts and tumor microenvironment. Mol Cancer. 22:1702023.
View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Nong S, Han X, Xiang Y, Qian Y, Wei Y,
Zhang T, Tian K, Shen K, Yang J and Ma X: Metabolic reprogramming
in cancer: Mechanisms and therapeutics. MedComm (2020). 4:e2182023.
View Article : Google Scholar
|
|
60
|
Li Z, Sun C and Qin Z: Metabolic
reprogramming of cancer-associated fibroblasts and its effect on
cancer cell reprogramming. Theranostics. 11:8322–8336. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Mamun AA, Hayashi H, Yamamura A, Nayeem MJ
and Sato M: Hypoxia induces the translocation of glucose
transporter 1 to the plasma membrane in vascular endothelial cells.
J Physiol Sci. 70:442020. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Snell CE, Turley H, McIntyre A, Li D,
Masiero M, Schofield CJ, Gatter KC, Harris AL and Pezzella F:
Proline-hydroxylated hypoxia-inducible factor 1α (HIF-1α)
upregulation in human tumours. PLoS One. 9:e889552014. View Article : Google Scholar
|
|
63
|
Xu G, Li M, Wu J, Qin C, Tao Y and He H:
Circular RNA circ-NRIP1 sponges microRNA-138-5p to maintain
hypoxia-induced resistance to 5-fluorouracil through
HIF-1α-dependent glucose metabolism in gastric carcinoma. Cancer
Manag Res. 12:2789–2802. 2020. View Article : Google Scholar
|
|
64
|
Zhang D, Wang Y, Shi Z, Liu J, Sun P, Hou
X, Zhang J, Zhao S, Zhou BP and Mi J: Metabolic reprogramming of
cancer-associated fibroblasts by IDH3α downregulation. Cell Rep.
10:1335–1348. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Rodríguez-García A, Samsó P, Fontova P,
Simon-Molas H, Manzano A, Castaño E, Rosa JL, Martinez-Outshoorn U,
Ventura F, Navarro-Sabaté À and Bartrons R: TGF-β1 targets Smad,
p38 MAPK, and PI3K/Akt signaling pathways to induce PFKFB3 gene
expression and glycolysis in glioblastoma cells. FEBS J.
284:3437–3454. 2017. View Article : Google Scholar
|
|
66
|
Wei X, Hou Y, Long M, Jiang L and Du Y:
Molecular mechanisms underlying the role of hypoxia-inducible
factor-1 α in metabolic reprogramming in renal fibrosis. Front
Endocrinol (Lausanne). 13:9273292022. View Article : Google Scholar
|
|
67
|
Shi X, Yang J, Deng S, Xu H, Wu D, Zeng Q,
Wang S, Hu T, Wu F and Zhou H: TGF-β signaling in the tumor
metabolic microenvironment and targeted therapies. J Hematol Oncol.
15:1352022. View Article : Google Scholar
|
|
68
|
Wang SF, Tseng LM and Lee HC: Role of
mitochondrial alterations in human cancer progression and cancer
immunity. J Biomed Sci. 30:612023. View Article : Google Scholar :
|
|
69
|
Shimura T, Sasatani M, Kawai H, Kamiya K,
Kobayashi J, Komatsu K and Kunugita N: Radiation-Induced
myofibroblasts promote tumor growth via mitochondrial ROS-Activated
TGFβ Signaling. Mol Cancer Res. 16:1676–1686. 2018. View Article : Google Scholar
|
|
70
|
Chakraborty PK, Mustafi SB, Xiong X,
Dwivedi SKD, Nesin V, Saha S, Zhang M, Dhanasekaran D, Jayaraman M,
Mannel R, et al: MICU1 drives glycolysis and chemoresistance in
ovarian cancer. Nat Commun. 8:146342017. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Sung JS, Kang CW, Kang S, Jang Y, Chae YC,
Kim BG and Cho NH: ITGB4-mediated metabolic reprogramming of
cancer-associated fibroblasts. Oncogene. 39:664–676. 2020.
View Article : Google Scholar
|
|
72
|
Li X, Yang Y, Zhang B, Lin X, Fu X, An Y,
Zou Y, Wang JX, Wang Z and Yu T: Lactate metabolism in human health
and disease. Signal Transduct Target Ther. 7:3052022. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Qiao Y, Liu Y, Ran R, Zhou Y, Gong J, Liu
L, Zhang Y, Wang H, Fan Y, Fan Y, et al: Lactate metabolism and
lactylation in breast cancer: mechanisms and implications. Cancer
Metastasis Rev. 44:482025. View Article : Google Scholar :
|
|
74
|
Kozlov AM, Lone A, Betts DH and Cumming
RC: Lactate preconditioning promotes a HIF-1α-mediated metabolic
shift from OXPHOS to glycolysis in normal human diploid
fibroblasts. Sci Rep. 10:83882020. View Article : Google Scholar
|
|
75
|
Ishihara S, Hata K, Hirose K, Okui T,
Toyosawa S, Uzawa N, Nishimura R and Yoneda T: The lactate sensor
GPR81 regulates glycolysis and tumor growth of breast cancer. Sci
Rep. 12:62612022. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Luo M, Zhu J, Ren J, Tong Y, Wang L, Ma S
and Wang J: Lactate increases tumor malignancy by promoting tumor
small extracellular vesicles production via the
GPR81-cAMP-PKA-HIF-1α axis. Front Oncol. 12:10365432022. View Article : Google Scholar
|
|
77
|
Yang L, Gilbertsen A, Xia H, Benyumov A,
Smith K, Herrera J, Racila E, Bitterman PB and Henke CA: Hypoxia
enhances IPF mesenchymal progenitor cell fibrogenicity via the
lactate/GPR81/HIF1α pathway. JCI insight. 8:e1638202023. View Article : Google Scholar
|
|
78
|
Fontana F, Giannitti G, Marchesi S and
Limonta P: The PI3K/Akt pathway and glucose metabolism: A dangerous
liaison in cancer. Int J Biol Sci. 20:3113–3125. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Payen VL, Porporato PE, Baselet B and
Sonveaux P: Metabolic changes associated with tumor metastasis,
part 1: Tumor pH, glycolysis and the pentose phosphate pathway.
Cell Mol Life Sci. 73:1333–1348. 2016. View Article : Google Scholar
|
|
80
|
Mestre-Farrera A, Bruch-Oms M, Peña R,
Rodríguez-Morató J, Alba-Castellón L, Comerma L, Quintela-Fandino
M, Duñach M, Baulida J, Pozo ÓJ and García de Herreros A:
Glutamine-directed migration of cancer-activated fibroblasts
facilitates epithelial tumor invasion. Cancer Res. 81:438–451.
2021. View Article : Google Scholar
|
|
81
|
He C, Peng M, Zeng X, Dong H, Sun Z, Xu J,
Liu M, Liu L, Huang Y, Peng Z, et al: Microenvironmental G
protein-coupled estrogen receptor-mediated glutamine metabolic
coupling between cancer-associated fibroblasts and triple-negative
breast cancer cells governs tumour progression. Clin Transl Med.
14:e701312024. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Sousa CM, Biancur DE, Wang X, Halbrook CJ,
Sherman MH, Zhang L, Kremer D, Hwang RF, Witkiewicz AK, Ying H, et
al: Pancreatic stellate cells support tumour metabolism through
autophagic alanine secretion. Nature. 536:479–483. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Kay EJ, Paterson K, Riera-Domingo C,
Sumpton D, Däbritz JHM, Tardito S, Boldrini C, Hernandez-Fernaud
JR, Athineos D, Dhayade S, et al: Cancer-associated fibroblasts
require proline synthesis by PYCR1 for the deposition of
pro-tumorigenic extracellular matrix. Nat Metab. 4:693–710. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Kay EJ, Zanivan S and Rufini A: Proline
metabolism shapes the tumor microenvironment: From collagen
deposition to immune evasion. Curr Opin Biotechnol. 84:1030112023.
View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Huynh TYL, Zareba I, Baszanowska W,
Lewoniewska S and Palka J: Understanding the role of key amino
acids in regulation of proline dehydrogenase/proline oxidase
(prodh/pox)-dependent apoptosis/autophagy as an approach to
targeted cancer therapy. Mol Cell Biochem. 466:35–44. 2020.
View Article : Google Scholar
|
|
86
|
Ino Y, Yamazaki-Itoh R, Oguro S, Shimada
K, Kosuge T, Zavada J, Kanai Y and Hiraoka N: Arginase II expressed
in cancer-associated fibroblasts indicates tissue hypoxia and
predicts poor outcome in patients with pancreatic cancer. PLoS One.
8:e551462013. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Jin HR, Wang J, Wang ZJ, Xi MJ, Xia BH,
Deng K and Yang JL: Lipid metabolic reprogramming in tumor
microenvironment: From mechanisms to therapeutics. J Hematol Oncol.
16:1032023. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Jabbari K, Cheng Q, Winkelmaier G, Furuta
S and Parvin B: CD36(+) fibroblasts secrete protein ligands that
growth-suppress triple-negative breast cancer cells while elevating
adipogenic markers for a model of cancer-associated fibroblast. Int
J Mol Sci. 23:127442022. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Zhu GQ, Tang Z, Huang R, Qu WF, Fang Y,
Yang R, Tao CY, Gao J, Wu XL, Sun HX, et al: CD36(+)
cancer-associated fibroblasts provide immunosuppressive
microenvironment for hepatocellular carcinoma via secretion of
macrophage migration inhibitory factor. Cell Discov. 9:252023.
View Article : Google Scholar
|
|
90
|
Lopes-Coelho F, André S, Félix A and Serpa
J: Breast cancer metabolic cross-talk: Fibroblasts are hubs and
breast cancer cells are gatherers of lipids. Mol Cell Endocrinol.
462(Pt B): 93–106. 2018. View Article : Google Scholar
|
|
91
|
Wu F, Yang J, Liu J, Wang Y, Mu J, Zeng Q,
Deng S and Zhou H: Signaling pathways in cancer-associated
fibroblasts and targeted therapy for cancer. Signal Transduct
Target Ther. 6:2182021. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Zhang Y, Gu Z, Wan J, Lou X, Liu S, Wang
Y, Bian Y, Wang F, Li Z and Qin Z: Stearoyl-CoA Desaturase-1
dependent lipid droplets accumulation in cancer-associated
fibroblasts facilitates the progression of lung cancer. Int J Biol
Sci. 18:6114–6128. 2022. View Article : Google Scholar :
|
|
93
|
Santi A, Caselli A, Ranaldi F, Paoli P,
Mugnaioni C, Michelucci E and Cirri P: Cancer associated
fibroblasts transfer lipids and proteins to cancer cells through
cargo vesicles supporting tumor growth. Biochim Biophys Acta.
1853:3211–3223. 2015. View Article : Google Scholar
|
|
94
|
Beach JA, Aspuria PJ, Cheon DJ, Lawrenson
K, Agadjanian H, Walsh CS, Karlan BY and Orsulic S: Sphingosine
kinase 1 is required for TGF-β mediated fibroblastto-myofibroblast
differentiation in ovarian cancer. Oncotarget. 7:4167–4182. 2016.
View Article : Google Scholar
|
|
95
|
Auciello FR, Bulusu V, Oon C, Tait-Mulder
J, Berry M, Bhattacharyya S, Tumanov S, Allen-Petersen BL, Link J,
Kendsersky ND, et al: A stromal lysolipid-autotaxin signaling axis
promotes pancreatic tumor progression. Cancer Discov. 9:617–627.
2019. View Article : Google Scholar :
|
|
96
|
Charo C, Holla V, Arumugam T, Hwang R,
Yang P, Dubois RN, Menter DG, Logsdon CD and Ramachandran V:
Prostaglandin E2 regulates pancreatic stellate cell activity via
the EP4 receptor. Pancreas. 42:467–474. 2013. View Article : Google Scholar :
|
|
97
|
Martinez-Outschoorn UE, Lin Z,
Whitaker-Menezes D, Howell A, Lisanti MP and Sotgia F: Ketone
bodies and two-compartment tumor metabolism: Stromal ketone
production fuels mitochondrial biogenesis in epithelial cancer
cells. Cell Cycle. 11:3956–3963. 2012. View Article : Google Scholar :
|
|
98
|
Chirieac LR: Tumor cell proliferation,
proliferative index and mitotic count in lung cancer. Transl Lung
Cancer Res. 5:554–556. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Feitelson MA, Arzumanyan A, Kulathinal RJ,
Blain SW, Holcombe RF, Mahajna J, Marino M, Martinez-Chantar ML,
Nawroth R, Sanchez-Garcia I, et al: Sustained proliferation in
cancer: Mechanisms and novel therapeutic targets. Semin Cancer
Biol. 35(Suppl): S25–S54. 2015. View Article : Google Scholar
|
|
100
|
Prieto-Fernández L, Montoro-Jiménez I, de
Luxan-Delgado B, Otero-Rosales M, Rodrigo JP, Calvo F,
García-Pedrero JM and Álvarez-Teijeiro S: Dissecting the functions
of cancer-associated fibroblasts to therapeutically target head and
neck cancer microenvironment. Biomed Pharmacother. 161:1145022023.
View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Martinez-Outschoorn UE, Lisanti MP and
Sotgia F: Catabolic cancer-associated fibroblasts transfer energy
and biomass to anabolic cancer cells, fueling tumor growth. Semin
Cancer Biol. 25:47–60. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Fiaschi T, Marini A, Giannoni E, Taddei
ML, Gandellini P, De Donatis A, Lanciotti M, Serni S, Cirri P and
Chiarugi P: Reciprocal metabolic reprogramming through lactate
shuttle coordinately influences tumor-stroma interplay. Cancer Res.
72:5130–5140. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Becker LM, O'Connell JT, Vo AP, Cain MP,
Tampe D, Bizarro L, Sugimoto H, McGow AK, Asara JM, Lovisa S, et
al: Epigenetic reprogramming of cancer-associated fibroblasts
deregulates glucose metabolism and facilitates progression of
breast cancer. Cell Rep. 31:1077012020. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Li Y, Zhao Z, Liu W and Li X: SNHG3
Functions as miRNA sponge to promote breast cancer cells growth
through the metabolic reprogramming. Appl Biochem Biotechnol.
191:1084–1099. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Zhang X, Dong Y, Zhao M, Ding L, Yang X,
Jing Y, Song Y, Chen S, Hu Q and Ni Y: ITGB2-mediated metabolic
switch in CAFs promotes OSCC proliferation by oxidation of NADH in
mitochondrial oxidative phosphorylation system. Theranostics.
10:12044–12059. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Bertero T, Oldham WM, Grasset EM, Bourget
I, Boulter E, Pisano S, Hofman P, Bellvert F, Meneguzzi G, Bulavin
DV, et al: Tumor-Stroma mechanics coordinate amino acid
availability to sustain tumor growth and malignancy. Cell Metab.
29:124–140.e10. 2019. View Article : Google Scholar
|
|
107
|
Yang L, Achreja A, Yeung TL, Mangala LS,
Jiang D, Han C, Baddour J, Marini JC, Ni J, Nakahara R, et al:
Targeting stromal glutamine synthetase in tumors disrupts tumor
microenvironment-regulated cancer cell growth. Cell Metab.
24:685–700. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Linares JF, Cordes T, Duran A,
Reina-Campos M, Valencia T, Ahn CS, Castilla EA, Moscat J, Metallo
CM and Diaz-Meco MT: ATF4-induced metabolic reprograming is a
synthetic vulnerability of the p62-deficient tumor stroma. Cell
Metab. 26:817–829.e6. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Mishra R, Haldar S, Placencio V, Madhav A,
Rohena-Rivera K, Agarwal P, Duong F, Angara B, Tripathi M, Liu Z,
et al: Stromal epigenetic alterations drive metabolic and
neuroendocrine prostate cancer reprogramming. J Clin Invest.
128:4472–4484. 2018. View Article : Google Scholar :
|
|
110
|
Gerashchenko TS, Novikov NM, Krakhmal NV,
Zolotaryova SY, Zavyalova MV, Cherdyntseva NV, Denisov EV and
Perelmuter VM: Markers of cancer cell invasion: Are they good
enough? J Clin Med. 8:10922019. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Bànkfalvi A and Piffkò J: Prognostic and
predictive factors in oral cancer: The role of the invasive tumour
front. J Oral Pathol Med. 29:291–298. 2000. View Article : Google Scholar
|
|
112
|
Sahai E: Mechanisms of cancer cell
invasion. Curr Opin Genet Dev. 15:87–96. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Wirtz D, Konstantopoulos K and Searson PC:
The physics of cancer: The role of physical interactions and
mechanical forces in metastasis. Nat Rev Cancer. 11:512–522. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Nagelkerke A, Bussink J, Rowan AE and Span
PN: The mechanical microenvironment in cancer: How physics affects
tumours. Semin Cancer Biol. 35:62–70. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Liu QP, Luo Q, Deng B, Ju Y and Song GB:
Stiffer matrix accelerates migration of hepatocellular carcinoma
cells through enhanced aerobic glycolysis via the MAPK-YAP
signaling. Cancers (Basel). 12:4902020. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Wu X, Zhou Z, Xu S, Liao C, Chen X, Li B,
Peng J, Li D and Yang L: Extracellular vesicle packaged
LMP1-activated fibroblasts promote tumor progression via autophagy
and stroma-tumor metabolism coupling. Cancer Lett. 478:93–106.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Gong J, Lin Y, Zhang H, Liu C, Cheng Z,
Yang X, Zhang J, Xiao Y, Sang N, Qian X, et al: Reprogramming of
lipid metabolism in cancer-associated fibroblasts potentiates
migration of colorectal cancer cells. Cell Death Dis. 11:2672020.
View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Wang H, Liu F, Wu X, Zhu G, Tang Z, Qu W,
Zhao Q, Huang R, Tian M, Fang Y, et al: Cancer-associated
fibroblasts contributed to hepatocellular carcinoma recurrence and
metastasis via CD36-mediated fatty-acid metabolic reprogramming.
Exp Cell Res. 435:1139472024. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Sun K, Tang S, Hou Y, Xi L, Chen Y, Yin J,
Peng M, Zhao M, Cui X and Liu M: Oxidized ATM-mediated glycolysis
enhancement in breast cancer-associated fibroblasts contributes to
tumor invasion through lactate as metabolic coupling. EBioMedicine.
41:370–383. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Shan T, Chen S, Chen X, Lin WR, Li W, Ma
J, Wu T, Cui X, Ji H, Li Y and Kang Y: Cancer-associated
fibroblasts enhance pancreatic cancer cell invasion by remodeling
the metabolic conversion mechanism. Oncol Rep. 37:1971–1979. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Siemann DW and Horsman MR: Modulation of
the tumor vasculature and oxygenation to improve therapy. Pharmacol
Ther. 153:107–124. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Ribatti D and Pezzella F: Overview on the
different patterns of tumor vascularization. Cells. 10:6392021.
View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Katayama Y, Uchino J, Chihara Y, Tamiya N,
Kaneko Y, Yamada T and Takayama K: Tumor neovascularization and
developments in therapeutics. Cancers (Basel). 11:3162019.
View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Dudley AC and Griffioen AW: Pathological
angiogenesis: Mechanisms and therapeutic strategies. Angiogenesis.
26:313–347. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Zhu Y, Li X, Wang L, Hong X and Yang J:
Metabolic reprogramming and crosstalk of cancer-related fibroblasts
and immune cells in the tumor microenvironment. Front Endocrinol
(Lausanne). 13:9882952022. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Bonuccelli G, Whitaker-Menezes D,
Castello-Cros R, Pavlides S, Pestell RG, Fatatis A, Witkiewicz AK,
Vander Heiden MG, Migneco G, Chiavarina B, et al: The reverse
Warburg effect: glycolysis inhibitors prevent the tumor promoting
effects of caveolin-1 deficient cancer associated fibroblasts. Cell
Cycle. 9:1960–1971. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Yang J, Shi X, Yang M, Luo J, Gao Q, Wang
X, Wu Y, Tian Y, Wu F and Zhou H: Glycolysis reprogramming in
cancer-associated fibroblasts promotes the growth of oral cancer
through the lncRNA H19/miR-675-5p/PFKFB3 signaling pathway. Int J
Oral Sci. 13:122021. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Li X, Jiang E, Zhao H, Chen Y, Xu Y, Feng
C, Li J and Shang Z: Glycometabolic reprogramming-mediated
proangiogenic phenotype enhancement of cancer-associated
fibroblasts in oral squamous cell carcinoma: role of PGC-1α/PFKFB3
axis. Br J Cancer. 127:449–461. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Zhou Y, Ren H, Dai B, Li J, Shang L, Huang
J and Shi X: Hepatocellular carcinoma-derived exosomal miRNA-21
contributes to tumor progression by converting hepatocyte stellate
cells to cancer-associated fibroblasts. J Exp Clin Cancer Res.
37:3242018. View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Hsu WH, LaBella KA, Lin Y, Xu P, Lee R,
Hsieh CE, Yang L, Zhou A, Blecher JM, Wu CJ, et al: Oncogenic KRAS
drives lipofibrogenesis to promote angiogenesis and colon cancer
progression. Cancer Discov. 13:2652–2673. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Verginadis II, Avgousti H, Monslow J,
Skoufos G, Chinga F, Kim K, Leli NM, Karagounis IV, Bell BI,
Velalopoulou A, et al: A stromal integrated stress response
activates perivascular cancer-associated fibroblasts to drive
angiogenesis and tumour progression. Nat Cell Biol. 24:940–953.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Qian CN, Mei Y and Zhang J: Cancer
metastasis: Issues and challenges. Chin J Cancer. 36:382017.
View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Fares J, Fares MY, Khachfe HH, Salhab HA
and Fares Y: Molecular principles of metastasis: A hallmark of
cancer revisited. Signal Transduct Target Ther. 5:282020.
View Article : Google Scholar : PubMed/NCBI
|
|
134
|
Eble JA and Niland S: The extracellular
matrix in tumor progression and metastasis. Clin Exp Metastasis.
36:171–198. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
135
|
Curtis M, Kenny HA, Ashcroft B, Mukherjee
A, Johnson A, Zhang Y, Helou Y, Batlle R, Liu X, Gutierrez N, et
al: Fibroblasts mobilize tumor cell glycogen to promote
proliferation and metastasis. Cell Metab. 29:141–155.e9. 2019.
View Article : Google Scholar :
|
|
136
|
Wang Y, Wang X, Bai B, Shaha A, He X, He
Y, Ye Z, Shah VH and Kang N: Targeting Src SH3 domain-mediated
glycolysis of HSC suppresses transcriptome, myofibroblastic
activation, and colorectal liver metastasis. Hepatology.
80:578–594. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
137
|
Zhang C, Wang XY, Zhang P, He TC, Han JH,
Zhang R, Lin J, Fan J, Lu L, Zhu WW, et al: Cancer-derived exosomal
HSPC111 promotes colorectal cancer liver metastasis by
reprogramming lipid metabolism in cancer-associated fibroblasts.
Cell Death Dis. 13:572022. View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Li Q, Zhu CC, Ni B, Zhang ZZ, Jiang SH, Hu
LP, Wang X, Zhang XX, Huang PQ, Yang Q, et al: Lysyl oxidase
promotes liver metastasis of gastric cancer via facilitating the
reciprocal interactions between tumor cells and cancer associated
fibroblasts. EBioMedicine. 49:157–171. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
139
|
Tian Y, Wang X, Wu C, Qiao J, Jin H and Li
H: A protracted war against cancer drug resistance. Cancer Cell
Int. 24:3262024. View Article : Google Scholar : PubMed/NCBI
|
|
140
|
Lei ZN, Tian Q, Teng QX, Wurpel JND, Zeng
L, Pan Y and Chen ZS: Understanding and targeting resistance
mechanisms in cancer. MedComm (2020). 4:e2652023. View Article : Google Scholar : PubMed/NCBI
|
|
141
|
Dhanyamraju PK: Drug resistance mechanisms
in cancers: Execution of pro-survival strategies. J Biomed Res.
38:95–121. 2024. View Article : Google Scholar : PubMed/NCBI
|
|
142
|
Zaal EA and Berkers CR: The influence of
metabolism on drug response in cancer. Front Oncol. 8:5002018.
View Article : Google Scholar : PubMed/NCBI
|
|
143
|
Broekgaarden M, Anbil S, Bulin AL, Obaid
G, Mai Z, Baglo Y, Rizvi I and Hasan T: Modulation of redox
metabolism negates cancer-associated fibroblasts-induced treatment
resistance in a heterotypic 3D culture platform of pancreatic
cancer. Biomaterials. 222:1194212019. View Article : Google Scholar : PubMed/NCBI
|
|
144
|
Ko YH, Lin Z, Flomenberg N, Pestell RG,
Howell A, Sotgia F, Lisanti MP and Martinez-Outschoorn UE:
Glutamine fuels a vicious cycle of autophagy in the tumor stroma
and oxidative mitochondrial metabolism in epithelial cancer cells:
Implications for preventing chemotherapy resistance. Cancer Biol
Ther. 12:1085–1097. 2011. View Article : Google Scholar
|
|
145
|
Raez LE, Papadopoulos K, Ricart AD,
Chiorean EG, Dipaola RS, Stein MN, Rocha Lima CM, Schlesselman JJ,
Tolba K, Langmuir VK, et al: A phase I dose-escalation trial of
2-deoxy-D-glucose alone or combined with docetaxel in patients with
advanced solid tumors. Cancer Chemother Pharmacol. 71:523–530.
2013. View Article : Google Scholar
|
|
146
|
Mohanti BK, Rath GK, Anantha N, Kannan V,
Das BS, Chandramouli BA, Banerjee AK, Das S, Jena A, Ravichandran
R, et al: Improving cancer radiotherapy with 2-deoxy-D-glucose:
Phase I/II clinical trials on human cerebral gliomas. Int J Radiat
Oncol Biol Phys. 35:103–111. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
147
|
Di Cosimo S, Ferretti G, Papaldo P,
Carlini P, Fabi A and Cognetti F: Lonidamine: Efficacy and safety
in clinical trials for the treatment of solid tumors. Drugs Today
(Barc). 39:157–174. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
148
|
Kelly W, Diaz Duque AE, Michalek J, Konkel
B, Caflisch L, Chen Y, Pathuri SC, Madhusudanannair-Kunnuparampil
V, Floyd J and Brenner A: Phase II investigation of TVB-2640
(Denifanstat) with bevacizumab in patients with first relapse
high-grade astrocytoma. Clin Cancer Res. 29:2419–2425. 2023.
View Article : Google Scholar : PubMed/NCBI
|
|
149
|
Svensson RU, Parker SJ, Eichner LJ, Kolar
MJ, Wallace M, Brun SN, Lombardo PS, Van Nostrand JL, Hutchins A,
Vera L, et al: Inhibition of acetyl-CoA carboxylase suppresses
fatty acid synthesis and tumor growth of non-small-cell lung cancer
in preclinical models. Nat Med. 22:1108–1119. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
150
|
Schlaepfer IR and Joshi M: CPT1A-mediated
fat oxidation, mechanisms, and therapeutic potential.
Endocrinology. 161:bqz0462020. View Article : Google Scholar : PubMed/NCBI
|
|
151
|
Yao CH, Liu GY, Wang R, Moon SH, Gross RW
and Patti GJ: Identifying off-target effects of etomoxir reveals
that carnitine palmitoyltransferase I is essential for cancer cell
proliferation independent of β-oxidation. PLoS Biol.
16:e20037822018. View Article : Google Scholar
|
|
152
|
Gugiatti E, Tenca C, Ravera S, Fabbi M,
Ghiotto F, Mazzarello AN, Bagnara D, Reverberi D, Zarcone D,
Cutrona G, et al: A reversible carnitine palmitoyltransferase
(CPT1) inhibitor offsets the proliferation of chronic lymphocytic
leukemia cells. Haematologica. 103:e531–e536. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
153
|
Harding JJ, Telli M, Munster P, Voss MH,
Infante JR, DeMichele A, Dunphy M, Le MH, Molineaux C, Orford K, et
al: A Phase I Dose-Escalation and Expansion Study of Telaglenastat
in Patients with Advanced or Metastatic Solid Tumors. Clin Cancer
Res. 27:4994–5003. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
154
|
Yang WH, Qiu Y, Stamatatos O, Janowitz T
and Lukey MJ: Enhancing the Efficacy of Glutamine Metabolism
Inhibitors in Cancer Therapy. Trends Cancer. 7:790–804. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
155
|
Wicker CA, Hunt BG, Krishnan S, Aziz K,
Parajuli S, Palackdharry S, Elaban WR, Wise-Draper TM, Mills GB,
Waltz SE and Takiar V: Glutaminase inhibition with telaglenastat
(CB-839) improves treatment response in combination with ionizing
radiation in head and neck squamous cell carcinoma models. Cancer
Lett. 502:180–188. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
156
|
Han J, Li Q, Chen Y and Yang Y: Recent
metabolomics analysis in tumor metabolism reprogramming. Front Mol
Biosci. 8:7639022021. View Article : Google Scholar : PubMed/NCBI
|
|
157
|
Ciavardelli D, Bellomo M, Consalvo A,
Crescimanno C and Vella V: Metabolic alterations of thyroid cancer
as potential therapeutic targets. Biomed Res Int. 2017:25450312017.
View Article : Google Scholar : PubMed/NCBI
|
|
158
|
Wang YA, Li XL, Mo YZ, Fan CM, Tang L,
Xiong F, Guo C, Xiang B, Zhou M, Ma J, et al: Effects of tumor
metabolic microenvironment on regulatory T cells. Mol Cancer.
17:1682018. View Article : Google Scholar : PubMed/NCBI
|
|
159
|
Wright K, Ly T, Kriet M, Czirok A and
Thomas SM: Cancer-Associated Fibroblasts: Master tumor
microenvironment modifiers. Cancers (Basel). 15:18992023.
View Article : Google Scholar : PubMed/NCBI
|
|
160
|
Sun L, Yang X, Yuan Z and Wang H:
Metabolic reprogramming in immune response and tissue inflammation.
Arterioscler Thromb Vasc Biol. 40:1990–2001. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
161
|
Lindner T, Loktev A, Giesel F, Kratochwil
C, Altmann A and Haberkorn U: Targeting of activated fibroblasts
for imaging and therapy. EJNMMI Radiopharm Chem. 4:162019.
View Article : Google Scholar : PubMed/NCBI
|
|
162
|
Yang D, Liu J, Qian H and Zhuang Q:
Cancer-associated fibroblasts: From basic science to anticancer
therapy. Exp Mol Med. 55:1322–1332. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
163
|
Zhao Z, Li T, Sun L, Yuan Y and Zhu Y:
Potential mechanisms of cancer-associated fibroblasts in
therapeutic resistance. Biomed Pharmacother. 166:1154252023.
View Article : Google Scholar : PubMed/NCBI
|
|
164
|
Wang M, Xue W, Yuan H, Wang Z and Yu L:
Nano-Drug delivery systems targeting CAFs: A promising treatment
for pancreatic cancer. Int J Nanomedicine. 19:2823–2849. 2024.
View Article : Google Scholar : PubMed/NCBI
|
|
165
|
Giuliani S, Accetta C, di Martino S, De
Vitis C, Messina E, Pescarmona E, Fanciulli M, Ciliberto G, Mancini
R and Falcone I: Metabolic reprogramming in melanoma: An epigenetic
point of view. Pharmaceuticals (Basel). 18:8532025. View Article : Google Scholar : PubMed/NCBI
|
|
166
|
Kumar D, New J, Vishwakarma V, Joshi R,
Enders J, Lin F, Dasari S, Gutierrez WR, Leef G, Ponnurangam S, et
al: Cancer-Associated fibroblasts drive glycolysis in a targetable
signaling loop implicated in head and neck squamous cell carcinoma
progression. Cancer Res. 78:3769–3782. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
167
|
Francescone R, Barbosa Vendramini-Costa D,
Franco-Barraza J, Wagner J, Muir A, Lau AN, Gabitova L, Pazina T,
Gupta S, Luong T, et al: Netrin G1 promotes pancreatic
tumorigenesis through cancer-associated fibroblast-driven
nutritional support and immunosuppression. Cancer Discov.
11:446–479. 2021. View Article : Google Scholar
|
|
168
|
Balaban S, Nassar ZD, Zhang AY,
Hosseini-Beheshti E, Centenera MM, Schreuder M, Lin HM, Aishah A,
Varney B, Liu-Fu F, et al: Extracellular fatty acids are the major
contributor to lipid synthesis in prostate cancer. Mol Cancer Res.
17:949–962. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
169
|
Yu M, Guo G, Huang L, Deng L, Chang CS,
Achyut BR, Canning M, Xu N, Arbab AS, Bollag RJ, et al: CD73 on
cancer-associated fibroblasts enhanced by the
A2B-mediated feedforward circuit enforces an immune
checkpoint. Nat Commun. 11:5152020. View Article : Google Scholar
|
|
170
|
Broz MT, Ko EY, Ishaya K, Xiao J, De
Simone M, Hoi XP, Piras R, Gala B, Tessaro FHG, Karlstaedt A, et
al: Metabolic targeting of cancer associated fibroblasts overcomes
T-cell exclusion and chemoresistance in soft-tissue sarcomas. Nat
Commun. 15:24982024. View Article : Google Scholar : PubMed/NCBI
|
|
171
|
Emberley E, Pan A, Chen J, Dang R, Gross
M, Huang T, Li W, MacKinnon A, Singh D, Sotirovska N, et al: The
glutaminase inhibitor telaglenastat enhances the antitumor activity
of signal transduction inhibitors everolimus and cabozantinib in
models of renal cell carcinoma. PLoS One. 16:e02592412021.
View Article : Google Scholar : PubMed/NCBI
|
|
172
|
Wang Z, Wang Y, Li Z, Xue W, Hu S and Kong
X: Lipid metabolism as a target for cancer drug resistance:
Progress and prospects. Front Pharmacol. 14:12743352023. View Article : Google Scholar :
|
|
173
|
Wang Z, Tang Y, Tan Y, Wei Q and Yu W:
Cancer-associated fibroblasts in radiotherapy: Challenges and new
opportunities. Cell Commun Signal. 17:472019. View Article : Google Scholar : PubMed/NCBI
|