Introduction
Magnetic resonance imaging (MRI) is an elective
imaging investigation method used for the detection, staging and
follow-up of prostate cancer patients. The specific MRI imaging
characteristics of prostate cancer, i.e., low T2 signal intensity,
restricted diffusion area, low apparent diffusion coefficient and
contrast enhancement, suggest the diagnosis, enable TNM staging and
may guide prostate biopsy. Therefore, we consider that, in patients
with such MRI lesions, histopathological examination is required to
confirm the diagnosis of malignancy, although prostate-specific
antigen (PSA) levels and digital rectal examination (DRE) findings
may be normal. The aim of this study was to demonstrate a high
similitude between prostate cancer and an inflammatory disease,
such as granulomatous prostatitis, on MRI examination.
Case report
A 64-year-old patient with a medical history of
heavy smoking (43 pack-years index) and atrial fibrillation-flutter
was diagnosed with a small (3 cm), solitary, non-muscle invasive
bladder tumor. The bladder tumor was diagnosed as low-grade (G1)
urothelial carcinoma, without invasion of the chorion (Ta). It is
important to mention that, during transurethral resection of the
blader (TURB), the patient developed a major cardiac arrhythmia,
which ultimately required cardiac electroconversion. Despite the
fact that the patient had a low risk of disease recurrence and
progression (1), we recommended
bacillus Calmette-Guérin (BCG) immunotherapy (Lamm protocol)
(2), due to the smoking history
and the high risk of anaesthesia due to the cardiac pathology.
Following BCG induction treatment (6 weekly instillations), at 3
months after TURB the first control cystoscopy would have been
recommended. However, as the patient exhibited a low level of pain
tolerance, which would require a form of general anaesthesia, in
order to avoid a possible recurrence of the cardiac arrhythmia, we
decided to perform a pelvic MRI scan instead of a flexible
cystoscopy.
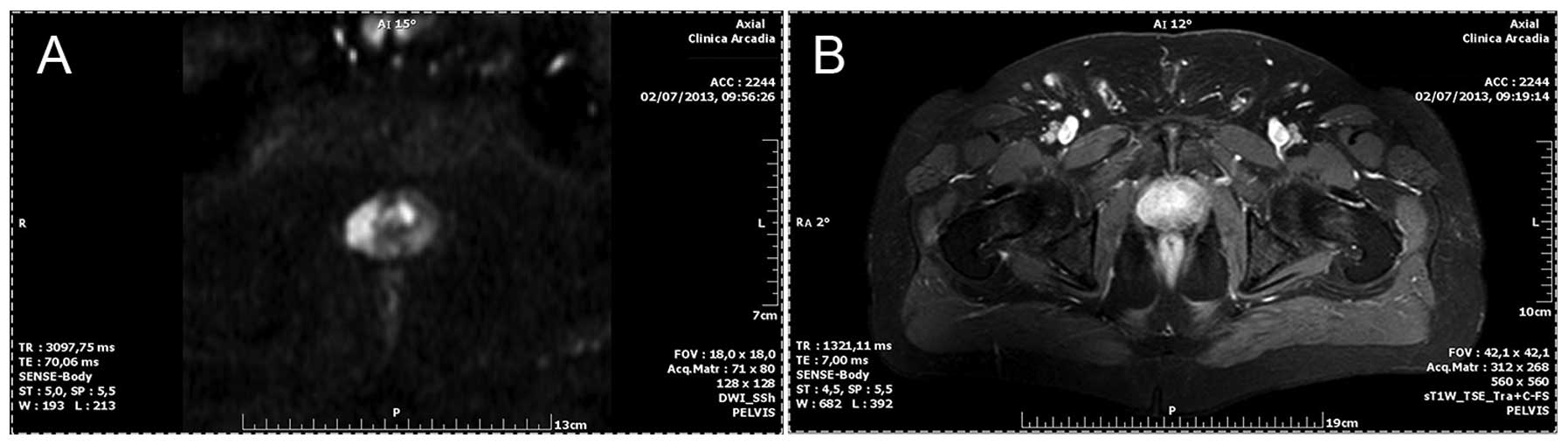
The MRI revealed normal bladder mucosa but also
revealed a 19×27×21 mm area in the peripheral region of the right
prostatic lobe, exhibiting certain malignant characteristics,
namely low T2 signal intensity, restricted diffusion (Fig. 1A) and contrast enhancement
(Fig. 1B), compared to the rest of
the prostate gland. The prostate had only been evaluated by digital
rectal examination (DRE), abdominal ultrasonography and computed
tomography (CT), without any findings suggestive of pathological
lesions. PSA measurement had been postponed due to all the urethral
manoeuvering. Therefore, 3 months after TURB and 1 month after BCG
immunotherapy and the first MRI examination, the PSA level was
borderline (3.9 ng/ml; normal range, 0–4 ng/ml), with a prostate
volume of 40.14 cm3. Therefore, we decided to continue
with the clinical, biological and imaging monitoring of the bladder
and prostatic lesions. Six weeks after the first stage of local
immunotherapy induction, the patient underwent the second stage of
BCG induction (3 instillations). To evaluate the prostate lesions,
we decided to perform a second MRI examination 3 months after the
first MRI scan. The MRI findings were a 6.4-mm marginal thickening
of the left bladder wall and prostate lesions suggestive of
malignancy (low T2 signal intensity, restricted diffusion area and
contrast enhancement) in both lobes: an area with a maximum
diameter of 23.3 mm in the right lobe and an area of 14 mm in the
left lobe (Fig. 2A and B). The progressive nature of the prostate
lesions (involvement of both lobes) was not associated with an
increase in PSA levels, which were marginally decreased (3.6
ng/ml).
Under those conditions (irregularity of the left
bladder wall and progression of the prostate lesions suggesting
malignant degeneration), we considered that the cardiac risk of
general anesthesia in order to perform a more invasive local
procedure was justified. Thus, we performed TURB (although,
macroscopically, the bladder mucosa was normal) and transrectal
ultrasound (TRUS)-guided biopsy (although the suspicious prostate
areas were inhomogeneous rather than hypoechoic) and collected 7
samples from the right lobe and 3 from the left lobe (3). The histopathological examination
revealed a granulomatous inflammation with giant epithelioid cells,
without malignant cells, in any of the bladder and prostate
samples.
As the patient was in a good general condition,
without any micturition-related complaints, periodical evaluation
with DRE, PSA, TRUS and even MRI and the continuation of BCG
immunotherapy were recommended.
Discussion
Granulomatous prostatitis secondary to BCG
immunotherapy is a well-known pathological entity (4); however, due to its low incidence, it
tends to be overlooked. Previous studies based on histopathological
reports (5, 6) proved that 75–100% of the patients who
undergo BCG instillations develop granulomatous inflammatory
lesions in the prostate. In the majority of the cases the patients
are asymptomatic and only rarely (0.9–1.3%) are there clinical
complaints, slight induration of the prostate or elevated PSA level
(7, 8). In these patients, imaging
examinations (TRUS, CT and MRI) may exhibit a number of
similarities to prostate cancer (9), for which reason a prostate biopsy may
be mandatory to determine the diagnosis (7). The diagnosis of granulomatous
prostatitis does not require specific therapy with antibiotics
(izoniazid and rifampicin for 3–6 months) in the absence of
clinical symptoms, but rather close monitoring (10), which may be a major issue due to
the poor data availability in the literature regarding the
progression of local findings and PSA level alterations. Under such
conditions, we consider that regular complete evaluation (DRE, PSA,
TRUS and even MRI) may help avoid further unnecessary prostate
biopsy, particularly in patients at high risk due to associated
illness.
This case report was an apparently common case of
non-muscle invasive bladder tumor that presented with a series of
particularities in the patient (previous heavy smoker, low pain
tolerance, induction of cardiac arrhythmia with anaesthesia and
stress exacerbation) as well as in the MRI findings, suggesting a
possible associated prostate carcinoma. Radiologists agree that low
T2 signal intensity, diffusion restriction and contrast enhancement
on MRI are specific to prostate cancer (particularly in the
peripheral areas), although some of these findings, particularly
low T2 signal in the transition zone, may be specific to
granulomatous prostatitis (9).
Specialized literature confirms that BCG prostatitis is indicated
by low T2 signal on MRI, but does not present data that BCG
inflammatory prostatitis may present with all the characteristics
of prostate carcinoma, namely diffusion restriction and contrast
enhancement in peripheral lesions. Furthermore, following BCG
immunotherapy, it is possible to observe a thickening of the
bladder wall on MRI examination (9), which was the case in our patient, at
6 months after TURB. The difficulty of imaging differentiation
between granulomatous prostatitis and prostate cancer, the
possibility of bladder tumor recurrence and the progressive nature
of the prostate lesions indicated by repeated MRI examinations,
prompted us to perform invasive bladder/prostate procedures,
although all the other examinations (DRE, PSA, TRUS and CT) were
not suggestive of prostate malignancy. To improve the accuracy of
MRI examination in prostate cancer detection, radiologists
recommend an MRI device with a 3-Tesla (3-T) magnet and an
endorectal coil that may enable a better multi-parametric
examination (high-resolution T2-weighted images, dynamic
contrast-enhanced, diffusion-weighted imaging/apparent diffusion
coefficient maps, MR spectroscopic imaging) and a more correct
assessment of Prostate Imaging Reporting and Data System score
(11). It would be optimal, for
the patient as well as for the urologist, that prostate malignancy
was excluded by histopathological examination; in addition, the
identical MRI presentation may lead to difficulties in further
monitoring the prostate. If the MRI image of the prostate remains
unchanged, prostate monitoring should be performed by DRE, PSA
measurement and TRUS, so that repeated prostate biopsy (saturation
protocol) is the last diagnostic option, performed only if new
elements, clearly suggestive of prostate cancer, appear.
In conclusion, we must consider that there are
several clinical, biological and imaging similarities between
granulomatous prostatitis and prostate cancer. In patients with
normal DRE and normal PSA levels who recently underwent BCG
immunotherapy, an abnormal MRI imaging may not be considered
strongly indicative of prostate cancer, even if the imaging
characteristics are specific to cancer. A multi-parametric MRI
examination, using a 3-T magnet and an endorectal coil, may be more
useful in differentiating between prostate pathologies. The
decision to perform a prostate biopsy must be well justified, to
avoid unnecessary procedures, particularly in patients with a high
procedure risk due to associated illness.
References
|
1
|
Babjuk M, Burger M, Zigeuner R, et al:
European Association of Urology: EAU guidelines of
non-muscle-invasive urothelial carcinoma of the bladder: update
2013. Eur Urol. 64:639–653. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Lamm DL, Blumenstein BA, Crissman JD, et
al: Maintenance bacillus Calmette-Guerin immunotherapy for
recurrent Ta, T1 and carcinoma in situ transitional cell carcinoma
of the bladder: a randomized Southwest Oncology Group Study. J
Urol. 163:1124–1129. 2000. View Article : Google Scholar
|
|
3
|
Heidenreich A, Bellmunt J, Bolla M, et al:
European Association of Urology: EAU guidelines on prostate cancer.
Part 1: screening, diagnosis, and treatment of clinically localised
disease. Eur Urol. 59:61–71. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Lamm DL, Stogdill VD, Stogdill BJ and
Crispen RG: Complications of bacillus Calmette-Guérin immunotherapy
in 1,278 patients with bladder cancer. J Urol. 135:272–274.
1986.
|
|
5
|
LaFontaine PD, Middelman BR, Graham SD Jr
and Sanders WH: Incidence of granulomatous prostatitis and
acid-fast bacilli after intravesical BCG therapy. Urology.
49:363–366. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Oates RD, Stilmant MM, Freedlund MC and
Siroky MB: Granulomatous prostatitis following bacillus
Calmette-Guérin immunotherapy of bladder cancer. J Urol.
140:751–754. 1988.
|
|
7
|
Lamm DL, van der Meijden PM, Morales A, et
al: Incidence and treatment of complication of bacillus
Calmette-Guérin intravesical therapy in superficial bladder cancer.
J Urol. 147:596–600. 1992.
|
|
8
|
Leibovici D, Zisman A, Chen-Levyi Z, et
al: Elevated prostate specific antigen serum levels after
intravesical instillation of bacillus Calmette-Guérin. J Urol.
164:1546–1549. 2000.PubMed/NCBI
|
|
9
|
Ma W, Kang SK, Hricak H, Gerst SR and
Zhang J: Imaging appearance of granulomatous disease after
intravesical Bacille Calmette-Guérin (BCG) treatment of bladder
carcinoma. AJR Am J Roentgenol. 192:1494–1500. 2009.PubMed/NCBI
|
|
10
|
Witjes JA, Palou J, Soloway M, et al:
Clinical practice recommendations for the prevention and management
of intravesical therapy-associated adverse events. Eur Urol. Suppl
7:667–674. 2008. View Article : Google Scholar
|
|
11
|
Barentsz JO, Richenberg J, Clements R, et
al: European Society of Urogenital Radiology: ESUR prostate MR
guidelines 2012. Eur Radiol. 22:746–757. 2012. View Article : Google Scholar : PubMed/NCBI
|