Introduction
Lung cancer is an aggressive malignancy and remains
the most common cause of cancer-related mortality worldwide.
Pulmonary resection is currently the most effective treatment for
patients with non-small-cell lung cancer. However, even if patients
undergo curative surgical resection for primary lung cancer, they
are at risk for developing metachronous second primary lung
cancers. The risk of developing a metachronous second primary lung
cancer in patients who survive resection of a non-small-cell lung
cancer is 1–2%/patient/year (1,2). The
standard surgical treatment for patients with resectable
non-small-cell lung cancer is pulmonary lobectomy (3). However, patients with metachronous
second primary lung cancer are frequently unable to tolerate
lobectomy due to their low cardiopulmonary functional reserve,
advanced age and medical comorbidities. There is currently no
definitive guideline on surgical therapy for metachronous second
primary lung cancer. Metachronous second primary lung cancers are
often defined using the criteria proposed by Martini and Melamed
(4). These criteria, provided that
the histological type is the same as that of the primary lung
cancer, comprise the following: A disease-free interval between
cancers of ≥2 years; the second cancer originating from carcinoma
in situ; first and second primary lung cancers occurring in
different lobes, with no carcinoma detectable in the lymph nodes
common to both; and no extrapulmonary metastasis present at the
time of diagnosis. However, a disease-free interval of at least 2
years is arguable, as chest computed tomography (CT) currently
allows for earlier detection of tumors and the incidence of
adenocarcinoma has increased (5).
Recent studies reported that a disease-free interval of <2 or
>2 years was not associated with survival differences in
patients with diagnosed metachronous second primary lung cancer
(5–7).
In this study, we retrospectively analyzed surgically treated
metachronous second primary lung cancers that occurred ≥5 years
after the initial surgery.
Materials and methods
Patients and follow-up
Of the 947 patients who underwent surgical resection
for primary lung cancer at our institution between January, 2000
and December, 2012, 12 patients (1.3%) who underwent second surgery
for metachronous second primary lung cancer were enrolled in this
study; the interval between the initial and second surgeries was ≥5
years. The pathologists in our hospital confirmed the diagnosis of
metachronous lung cancer by examining the surgical specimens from
the initial and second surgeries under a microscope. More than 5
years after the initial resection of the primary lung cancer, all
12 patients were followed up every 3–6 months. In the outpatient
setting, the patients underwent chest X-ray or CT and evaluation of
tumor markers. The following parameters were extracted from medical
records: Patient gender, age, tumor size, tumor location, surgical
procedure, histological type, pathological TNM stage, time of
initial and second surgeries and patient outcome. Survival was
calculated from the date of the second resection to the date of the
last follow-up or death. All the patients were staged according to
the seventh edition of the TNM classification (8).
Statistical analysis
Statistical analysis was performed using JMP
software, version 8.0.1 (SAS Institute Inc., Cary, NC, USA). The
cumulative survival rates were calculated by the Kaplan-Meier
method using the date of second surgery as the starting point.
Survival differences were determined by the log-rank analysis.
P<0.05 was considered to indicate statistically significant
differences.
Results
Patient characteristics
The study group consisted of 7 men and 5 women. The
median age of the patients at the second surgery was 70.5 years
(range, 27–83 years). The characteristics of the primary lung
cancers are shown in Table I and
those of metachronous second primary lung cancers in Table II. The median interval between the
first and second surgeries was 10.0 years (range, 5.0–18.0 years).
Of the 12 patients, 5 had intervals of ≥10 years from the initial
resection of primary lung cancer to the occurrence of metachronous
second primary lung cancer. There was no reported intraoperative
mortality. Postoperative complications occurred in 4 patients
(33%). A total of 2 patients (16%) required home oxygen therapy, 1
of whom had suffered acute respiratory failure postoperatively. Two
additional complications were atrial fibrillation in 1 patient (8%)
and heart failure in 1 patient (8%). The median follow-up from the
date of the second surgery was 28.7 months (range, 6–153 months).
The overall 5-year survival rate following resection of
metachronous second primary lung cancer was 56.5% and the median
survival was 68.4 months. A total of 5 patients developed tumor
recurrence after the second surgery. Among 4 patients who underwent
lobectomy or more extensive resections, only 1 patient developed
local recurrence. Of the 8 patients who underwent sublobar
resection, 3 developed local recurrence and 2 developed distant
metastasis, including 1 patient who experienced both. All 4
patients who developed recurrence following sublobar resection for
metachronous second primary lung cancer had advanced-stage disease.
By contrast, all 3 patients who underwent sublobar resection for
T1aN0M0 metachronous second primary lung cancer have been
recurrence-free over the 13–153 months after the second
surgery.
 | Table I.Patient characteristics at the initial
surgery (n=12). |
Table I.
Patient characteristics at the initial
surgery (n=12).
| Characteristics | No. (%) |
|---|
| Gender |
|
| Male | 7
(58.3) |
|
Female | 5
(41.7) |
| Histology of primary
lung cancer |
|
|
Adenocarcinoma | 11 (91.7) |
| Squamous
cell carcinoma | 1 (8.3) |
| Surgery for primary
lung cancer |
|
|
Lobectomy | 9
(75.1) |
| Lobectomy
+ segmentectomy | 1 (8.3) |
|
Bilobectomy | 1 (8.3) |
|
Pneumonectomy | 1 (8.3) |
| pStage of primary
lung cancer |
|
| IA | 4
(33.4) |
| IB | 3
(25.0) |
| IIA | 1 (8.3) |
| IIB | 1 (8.3) |
| IIIA | 3
(25.0) |
 | Table II.Patient characteristics at the second
surgery (n=12). |
Table II.
Patient characteristics at the second
surgery (n=12).
| Characteristics | No. (%) |
|---|
| Age at second
surgery, years |
|
| Median
(range) | 70.5 (27–83) |
| Interval between
first and second surgery, years |
|
| Median
(range) | 10.0 (5.0–18.0) |
| Surgery for second
primary lung cancer |
|
| Wedge
resection | 5
(41.7) |
|
Segmentectomy | 3
(25.0) |
|
Lobectomy | 3
(25.0) |
|
Completion pneumonectomy | 1 (8.3) |
| Histology of second
primary lung cancer |
|
|
Adenocarcinoma | 10 (83.3) |
| Squamous
cell carcinoma | 2
(16.7) |
| Site of second
primary tumor |
|
|
Ipsilateral | 4
(33.3) |
|
Contralateral | 8
(66.7) |
| T stage of second
primary lung cancer |
|
| T1a | 6
(50.0) |
| T1b | 2
(16.7) |
| T2a | 3
(25.0) |
| T3 | 1 (8.3) |
| N stage of second
primary lung cancer |
|
| N0 | 10 (83.4) |
| N1 | 1 (8.3) |
| N2 | 1 (8.3) |
| pStage of second
primary lung cancer |
|
| IA | 7
(58.3) |
| IB | 3
(25.0) |
| IIIA | 2
(16.7) |
Survival analysis
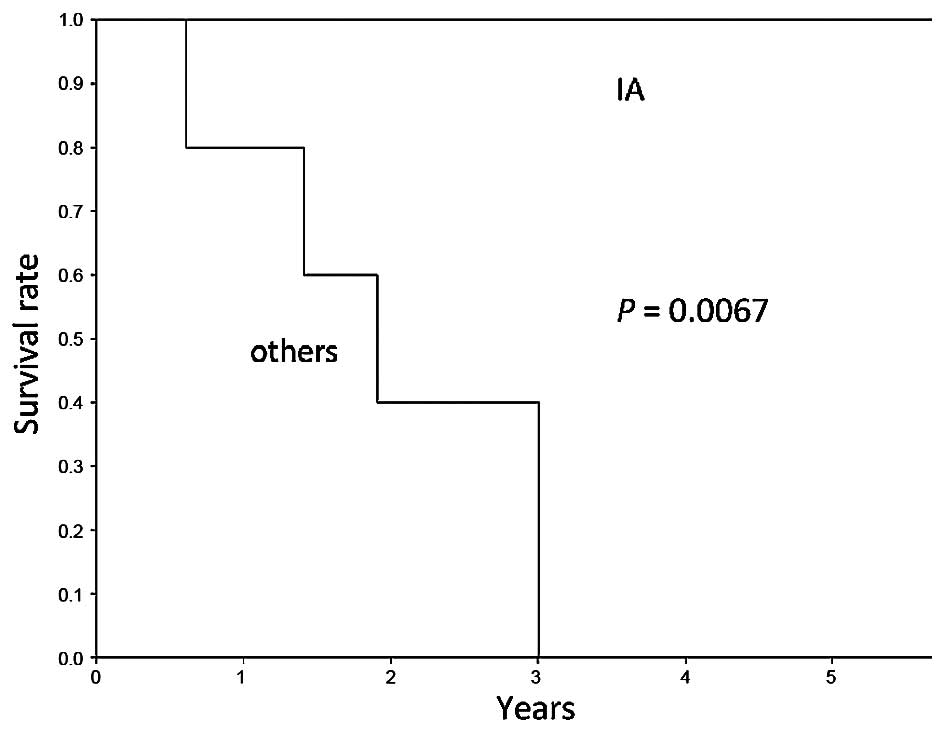
The 5-year survival rate was 100% for patients with
stage IA disease and 0% for patients with higher-stage disease
(P=0.0067) (Fig. 1). The 5-year
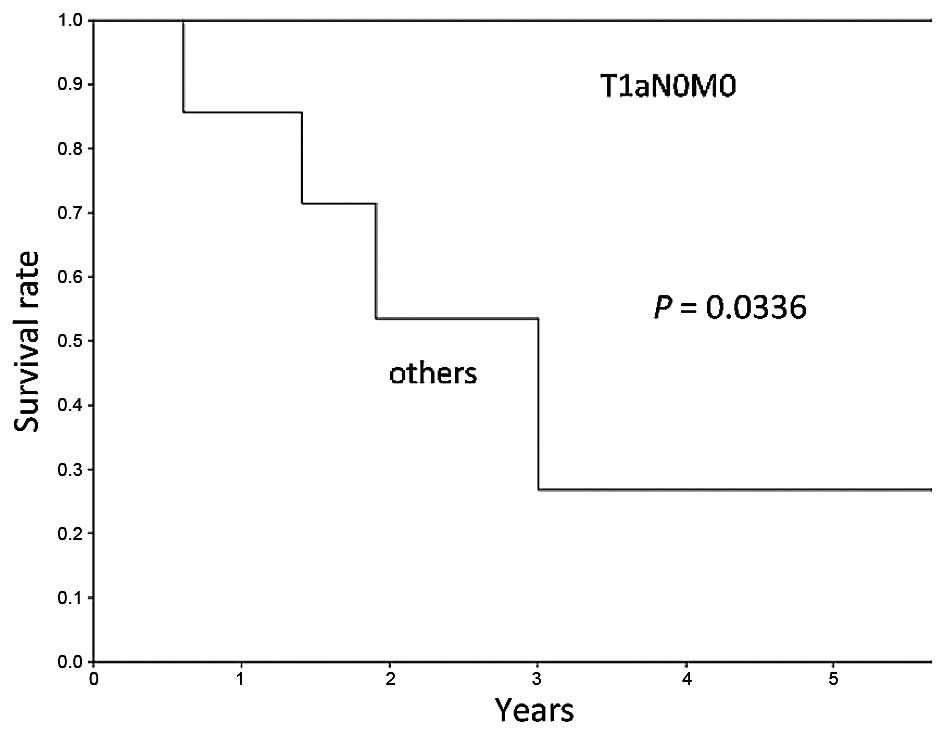
survival rate was 100% for patients with T1aN0M0 disease and 26.7%
for patients with non-T1aN0M0 disease (P=0.0336) (Fig. 2). Notably, all the patients with
T1aN0M0 disease remain alive without recurrence. Patients with
early-stage disease exhibited a significantly longer overall
survival compared with patients with advanced-stage disease.
Discussion
Patients who undergo surgical resection of primary
lung cancer are at risk for developing metachronous second primary
lung cancers. The potential risk of emergence of metachronous
second primary lung cancers persists for ≥5 years after the initial
surgery for primary lung cancer. In this study, 1.3% of patients
with primary lung cancer developed metachronous second primary lung
cancers ≥5 years after the initial surgery. Among the 12 patients,
5 had an interval of ≥10 years between complete resection of the
primary lung cancer and the appearance of metachronous second
primary lung cancer. Hamaji et al (7) reported that 33.6% of metachronous second
primary lung cancers developed ≥5 years after the resection of the
primary lung cancer and 6.9% developed ≥10 years later. Asaph et
al (9) reported that 38% of
metachronous second primary lung cancers developed ≥5 years
following resection of the primary lung cancer.
In the present study, surgery for metachronous
second primary lung cancers ≥5 years after the initial surgery for
primary lung cancer was performed safely, with a good prognosis for
patients with early-stage metachronous second primary lung cancers,
even for those who underwent sublobar resection. The overall 5-year
survival rate for the second resection was 56.5%, which is similar
to previously reported rates (5–7, 10–12). The
5-year survival rate following metachronous second primary lung
cancer has been reported to range from 26 to 66% in various series
(5–7,
10–12). There was no operative mortality in the
present study. Regarding the pathological stage of the metachronous
second primary lung cancers, patients with stage IA disease had a
good prognosis, with a 5-year overall survival rate of 100%. This
result is consistent with those of previous reports (5,10).
All the patients with T1aN0M0 disease remained alive
at the last follow-up, which ranged from 13 to 153 months. Hamaji
et al (7) reported that tumors
≤2 cm in diameter were associated with better survival. The present
results indicate that surgery is particularly beneficial for
patients with early-stage metachronous second primary lung
cancer.
Lobectomy is the standard surgery for primary lung
cancer (3). However, patients with
metachronous second primary lung cancers occasionally undergo
sublobar resection due to their restricted cardiopulmonary
functional reserve, advanced age and medical comorbidities. The
most suitable surgical approach for metachronous second primary
lung cancer has not yet been established. If metachronous second
primary lung cancer is located on the same side as the primary
tumor, postoperative adhesions may make surgery difficult. In this
study, metachronous second primary lung cancer was ipsilaterally
located in 4 patients; all the cases had stage IA disease. No
patients succumbed to the disease within the first 5 years
following surgery. In this study, the type of resection did not
predict survival. Among patients who underwent sublobar resection,
those with T1aN0M0 disease exhibited a good prognosis. By contrast,
other patients tended to have a worse prognosis due to a high rate
of tumor recurrence (80%). Notably, in the present study,
recurrence was observed more frequently in patients who underwent
sublobar resection compared to those who underwent more extensive
resection. To the best of our knowledge, the number of studies
reporting the differences associated with type of resection and
tumor recurrence rates following surgery for metachronous second
primary lung cancer is currently limited. Zuin et al
(13) reported that lobectomy for
metachronous and synchronous second primary lung cancer exhibited a
statistically significant positive association with survival rate.
By contrast, other surgical series reported that type of resection
(sublobar vs. more extensive) for metachronous second primary lung
cancer did not predict survival (6,10,11). Zuin et al (13) observed no difference in recurrence
rates between patients who underwent lobectomy (3.3%) and those who
underwent sublobar resection (5%) for metachronous and synchronous
second primary lung cancers. The present results indicate that
sublobar resection is a safe and effective surgical approach for
patients with T1aN0M0 metachronous second primary lung cancer and
that lobectomy is the most beneficial surgical procedure for
patients with non-T1aN0M0 disease.
There is currently no consensus regarding the
optimal follow-up strategy long after curative resection of primary
lung cancer. The surveillance guidelines and practices vary widely
with respect to imaging frequency and modalities (14). Certain studies have suggested that
surveillance CT scanning may be effective for the detection of
early-stage metachronous second primary lung cancers (15,16). To
detect early-stage metachronous second primary lung cancer,
prolonged close surveillance for ≥5 years following resection of
primary lung cancer is crucial. Even if patients who underwent
initial surgery for primary lung cancer have been disease-free for
5 years, long-term follow-up should be considered for early
detection of potential metachronous second primary lung cancer. The
optimal strategy for long-term follow-up following curative
resection of primary lung cancer remains to be determined in future
studies.
There were several limitations to this study, mainly
its retrospective nature and limited sample size; notwithstanding,
we consider the information obtained by this study valuable.
In conclusion, the potential risk of metachronous
second primary lung cancer may persist for ≥5 years after the
initial surgery for primary lung cancer. Surgery for metachronous
second primary lung cancer may be safely performed, with
satisfactory outcomes for early-stage metachronous second primary
lung cancer. We recommend that close long-term follow-up following
surgical resection for primary cancer is continued for early
detection of possible metachronous second primary lung cancer to
ensure the best possible outcome, even in patients who undergo
sublobar resection.
Acknowledgements
This study was supported in part by a Grants-in-Aid
(nos. 24592098 and 26462140) for Scientific Research (C) from the
Japanese Ministry of Education, Culture, Sports, Science and
Technology.
References
|
1
|
Johnson BE: Second lung cancers in
patients after treatment for an initial lung cancer. J Natl Cancer
Inst. 90:1335–1345. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Johnson BE, Cortazar P and Chute JP:
Second lung cancers in patients successfully treated for lung
cancer. Semin Oncol. 24:492–499. 1997.PubMed/NCBI
|
|
3
|
Ginsberg RJ and Rubinstein LVLung Cancer
Study Group: Randomized trial of lobectomy versus limited resection
for T1 N0 non-small cell lung cancer. Ann Thorac Surg. 60:615–623.
1995. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Martini N and Melamed MR: Multiple primary
lung cancers. J Thorac Cardiovasc Surg. 70:606–612. 1975.PubMed/NCBI
|
|
5
|
Lee BE, Port JL, Stiles BM, Saunders J,
Paul S, Lee PC and Altorki N: TNM stage is the most important
determinant of survival in metachronous lung cancer. Ann Thorac
Surg. 88:1100–1105. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Battafarano RJ, Force SD, Meyers BF, Bell
J, Guthrie TJ, Cooper JD and Patterson GA: Benefits of resection
for metachronous lung cancer. J Thorac Cardiovasc Surg.
127:836–842. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hamaji M, Allen MS, Cassivi SD, Deschamps
C, Nichols FC, Wigle DA and Shen KR: Surgical treatment of
metachronous second primary lung cancer after complete resection of
non-small cell lung cancer. J Thorac Cardiovasc Surg. 145:683–691.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Detterbeck FC, Boffa DJ and Tanoue LT: The
new lung cancer staging system. Chest. 136:260–271. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Asaph JW, Keppel JF, Handy JR Jr, Douville
EC, Tsen AC and Ott GY: Surgery for second lung cancers. Chest.
118:1621–1625. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
van Rens MT, Zanen P, de la Rivière AB,
Elbers HR, van Swieten HA and van den Bosch JM: Survival after
resection of metachronous non-small cell lung cancer in 127
patients. Ann Thorac Surg. 71:309–313. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Aziz TM, Saad RA, Glasser J, Jilaihawi AN
and Prakash D: The management of second primary lung cancers. A
single centre experience in 15 years. Eur J Cardiothorac Surg.
21:527–533. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Haraguchi S, Koizumi K, Hirata T, Hirai K,
Mikami I, Kubokura H, Nakajima Y and Shimizu K: Surgical treatment
of metachronous nonsmall cell lung cancer. Ann Thorac Cardiovasc
Surg. 16:319–325. 2010.PubMed/NCBI
|
|
13
|
Zuin A, Andriolo LG, Marulli G, Schiavon
M, Nicotra S, Calabrese F, Romanello P and Rea F: Is lobectomy
really more effective than sublobar resection in the surgical
treatment of second primary lung cancer? Eur J Cardiothorac Surg.
44:e120–e125. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Rubins J, Unger M and Colice GLAmerican
College of Chest Physicians: Follow-up and surveillance of the lung
cancer patient following curative intent therapy: ACCP
evidence-based clinical practice guideline (2nd edition). Chest.
132 (Suppl 3):355S–367S. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lou F, Huang J, Sima CS, Dycoco J, Rusch V
and Bach PB: Patterns of recurrence and second primary lung cancer
in early-stage lung cancer survivors followed with routine computed
tomography surveillance. J Thorac Cardiovasc Surg. 145:75–82. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Lamont JP, Kakuda JT, Smith D, Wagman LD
and Grannis FW Jr: Systematic postoperative radiologic follow-up in
patients with non-small cell lung cancer for detecting second
primary lung cancer in stage IA. Arch Surg. 137:935–940. 2002.
View Article : Google Scholar : PubMed/NCBI
|