Introduction
Thymic carcinoma is a rare type of cancer, which
differs from thymoma regarding its aggressive clinical behavior.
The majority of patients with thymic carcinoma present at an
advanced stage and have a poor prognosis (1,2).
However, a proportion of the patients who achieve long-term
survival develop disease relapse and are candidates for salvage
therapy, such as re-resection, radiotherapy, or other modalities
(3–5). We herein present the 20-year clinical
course of a patient initially diagnosed with stage IVb thymic
carcinoma that developed bidirectional metastases toward the
pleural and lymph nodes, which were successfully treated with
repeated chemotherapy, surgery and radiotherapy, followed by
low-dose steroid therapy.
Case report
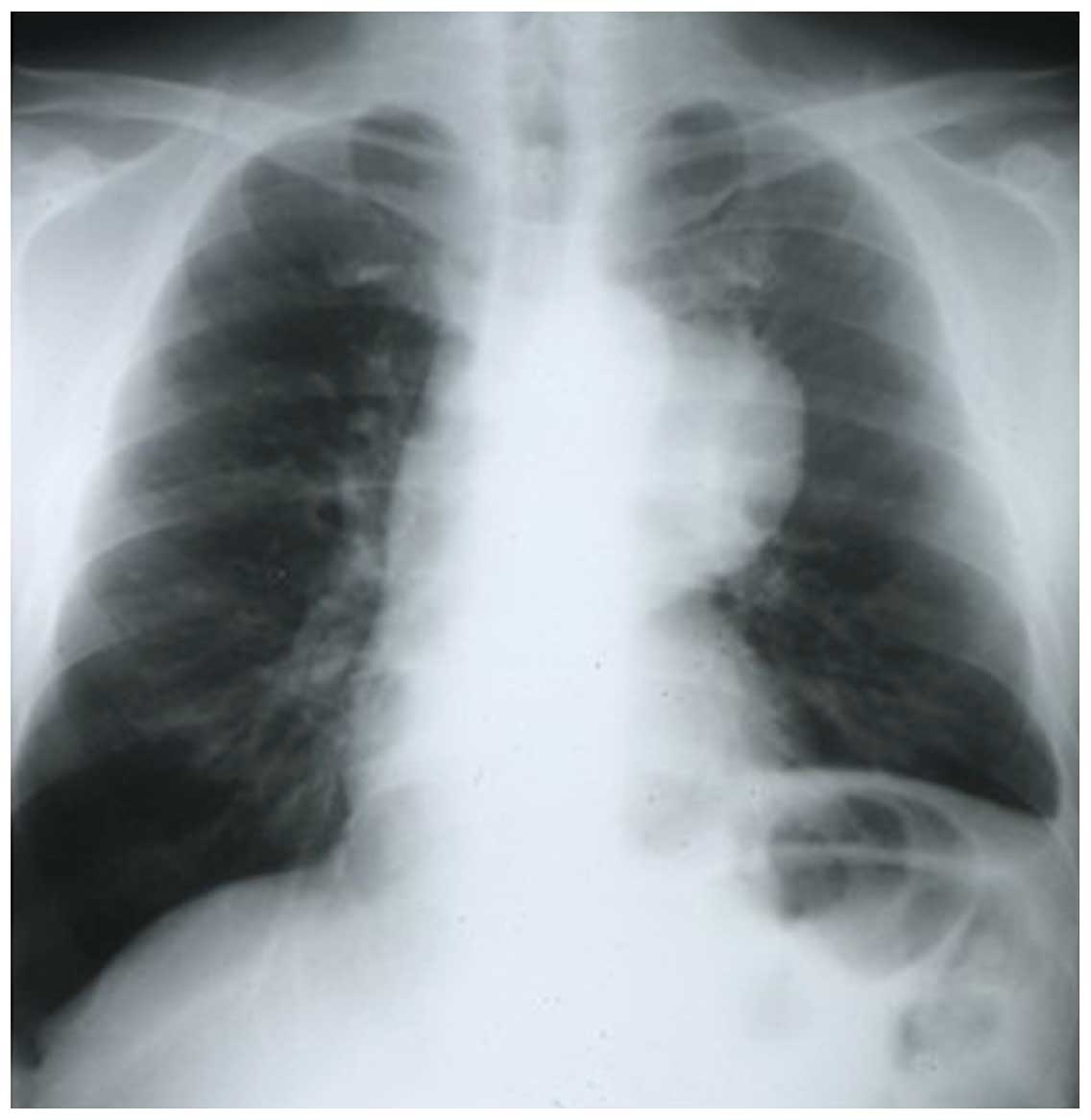
A 50-year-old man visited a regional hospital 20
years prior with hemoptysis and a febrile state. A chest X-ray
revealed a 6×5-cm solid mass in the hilum of the left lung,
directly invading the mediastinum, with left phrenic nerve palsy
(Fig. 1). Squamous cell carcinoma
was diagnosed by percutaneous needle biopsy. Based on the clinical
diagnosis of T4N0M0 lung cancer, sequential chemoradiotherapy with
two cycles of mytomycin C, vindecine and cisplatin (MVC regimen),
and radiotherapy of 60 Gy was administered. The patient was
subsequently referred to the Osaka Medical Center for surgery and
he underwent en bloc resection of the left upper lobe, mediastinal
lymph nodes, left brachiocephalic vein, pericardium and thymus via
a left hemiclamshell approach. The left brachiocephalic vein was
reconstructed using a Gore-Tex graft (Gore Medical, Flagstaff, AZ,
USA). As it was included in the radiation field, the bronchial
stump was covered with the omentum major. The final pathological
diagnosis was thymic carcinoma with mediastinal lymph node
metastasis (Masaoka stage IVb). The histological response to
chemoradiation therapy was poor (Ef-1).
The postoperative course was uneventful. Eleven
years after the initial operation, the patient underwent high
anterior resection for colon cancer at another hospital. Twelve
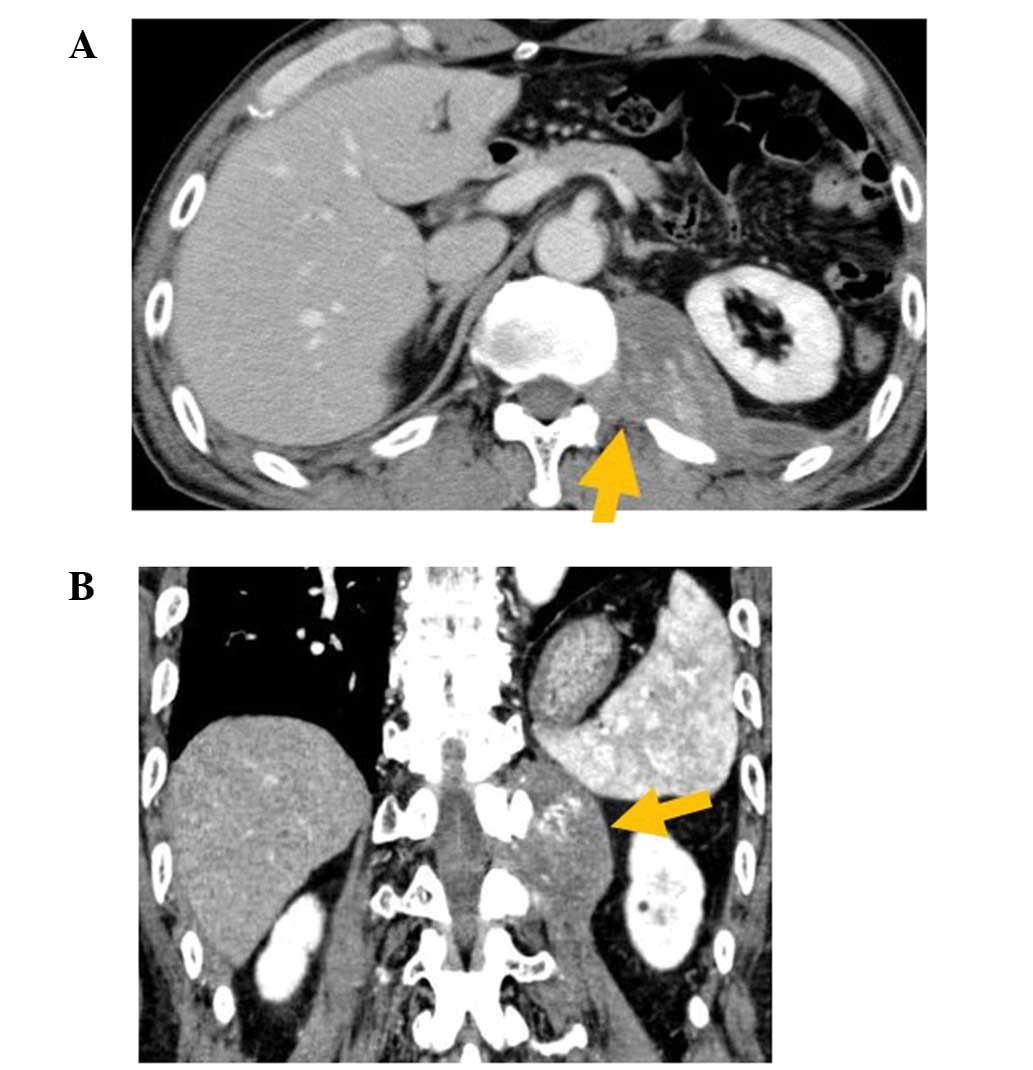
years and six months after the initial operation, a heterogeneous
mass with a maximal diameter of 10 cm in close contact with the
12th thoracic to the 2nd lumbar vertebrae was identified on
follow-up computed tomography (CT). As no definitive diagnosis was
made by needle biopsy, oral tegafur-uracil/leucovorin was
administered and a partial response was obtained. Sixteen years
after the initial operation, at 66 years of age, the patient was
referred to the Yao Municipal Hospital (Yao, Japan) for
investigation of an acute-onset left back pain. Laboratory
examinations revealed results within normal limits, including tumor
markers. A CT scan revealed a re-growing left paravertebral mass
that extended into the 1st intervertebral foramen (Fig. 2). Magnetic resonance imaging
demonstrated that the mass exhibited a low signal intensity on
T1-weighted images and a high signal intensity on T2-weighted and
diffusion-weighted images. At that time, pleural recurrence of the
thymic carcinoma at the costodiaphragmatic recess or a neurogenic
tumor was suspected, and surgery was performed for the purpose of a
definitive diagnosis and treatment. Intraoperatively, a mass sized
8.5×4.0×7.0 cm was identified at the bottom of the left chest
cavity, in close contact with the 12th thoracic and 1st lumbar
vertebrae, and the 11th and 12th ribs. Although the mass was
resected with the surrounding connective tissue, including the
ribs, the resection was incomplete due to the invasive nature of
the mass at the intervertebral foramen. Pathologically, the mass
was composed of highly atypical epithelioid cells with nuclear
atypia and eosinophilic cytoplasm in a fibrotic stroma. The Ki-67
index was 27%, with positive reactivity for CD5 and cytokeratin
AE1/AE3, and negative reactivity for c-Kit, synaptophysin,
chromogranin and thyroid transcription factor 1. The final
diagnosis of the mass was pleural dissemination of the thymic
carcinoma.
After the operation, 46 Gy/23 fr of adjuvant
radiation therapy was delivered to the resection margin site,
including the intervertebral foramen. The postoperative course was
uneventful and the left back pain disappeared.
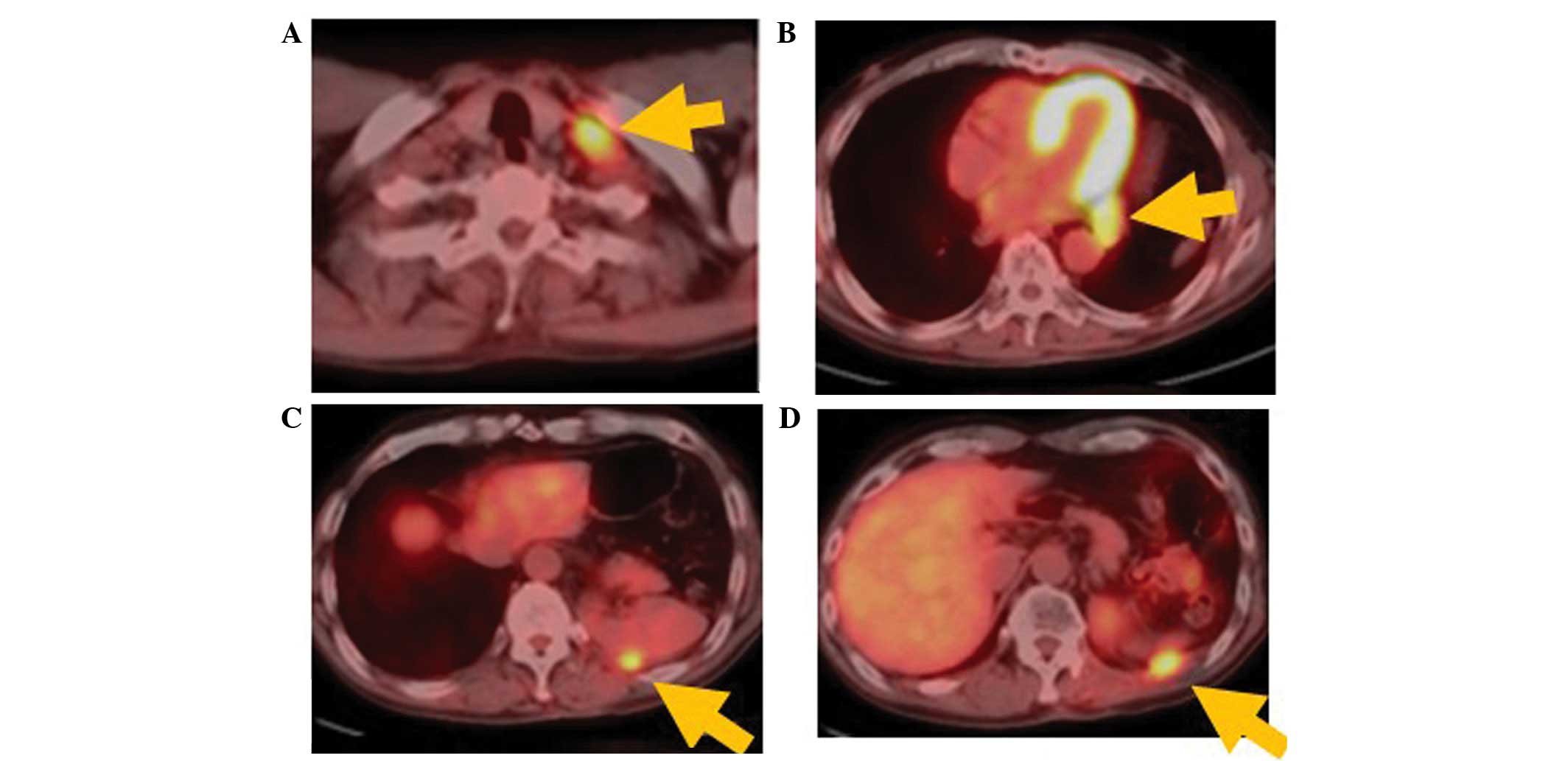
Twenty months following metastasectomy, positron
emission tomography/CT revealed a left subclavicular lymph node
metastasis and three new pleural metastases (Fig. 3). The patient received systemic
chemotherapy comprising three cycles of carboplatin (area under the
curve 5 on day 1, every 21 days) and paclitaxel (200
mg/m2 on day 1, every 21 days). The effects were minimal
and the response was classified as stable disease. Therefore,
radiation therapy was delivered (46 Gy/23 fr) to all four lesions.
The chest CT showed that the left subclavicular lymph node
metastasis had markedly shrunk, but the pleural metastases showed
no marked changes. No new lesions appeared over the next 11 months.
Therefore, complete excision of the three pleural masses was
conducted with clearance of all the intervening connective tissue,
combined with partial resections of the diaphragm and lung, 18
years after the initial operation.
One month after surgery, the patient developed
eosinophilic pneumonia in the left lung. Oral administration of
prednisolone (30 mg/day) was initiated to control the pneumonia.
Two months after surgery, the dose was tapered by 5 mg/day every 2
weeks. The eosinophilic pneumonia, as well as the patient's general
condition, including wound pain, markedly improved, and he
requested continuous daily oral administration of 5 mg
prednisolone.
The patient is currently disease-free and has
received low-dose prednisolone for 20 months.
Discussion
Thymic epithelial neoplasms are a relatively rare
type of cancer, with an annual incidence of 0.15/100,000
person-years (6). The 2004 WHO
classification clearly separates thymic carcinoma from thymoma
(7). Thymic carcinoma accounts for
<1–4% of thymic epithelial neoplasms. A previous report
indicated that the incidence of nodal metastases in patients with
thymic carcinoma was 26.8% (1). It
has been confirmed by several studies that patients with thymic
carcinoma receiving complete resection (R0) exhibit a more
favorable long-term survival compared with those who undergo
incomplete resection or do not receive surgery (1,5).
There is currently no standard guideline for the
management of recurrent thymic carcinoma. Wright et al
reported that the recurrence rate of type C thymoma (thymic
carcinoma) is 50% (8). The majority
of recurrences appear as pleural dissemination, mediastinal
relapse, or both. Most thymic carcinomas present at an advanced
stage and have a high frequency of relapse, even after complete
resection, which indicates the need for a multidisciplinary
therapeutic approach (5).
Multidisciplinary therapy, including re-excision, radiotherapy and
chemotherapy, is recommended. However, the impact of these
modalities on the clinical outcome is unclear. Surgery may be a
reasonable option in patients with localized recurrence that can be
completely resected (3,4). Radiotherapy may improve local control
and also confer some survival benefits (5,9).
Chemotherapy is based on low-level evidence: Platinum-based doublet
chemotherapy has achieved some beneficial effects (10).
According to a Japanese nationwide database study,
stage IVb thymic carcinoma patients showed a relatively favorable
survival if they underwent R0 resection for locoregional nodal and
pulmonary metastases, with 37% 10-year recurrence-free survival and
39% 10-year overall survival (5). We
were able to perform R0 resection for the primary site in our
patient, with combined resection of the left upper lobe of the
lung, left brachiocephalic vein and pericardium after
chemoradiotherapy. There has been no recurrence at the primary site
for 20 years. Repeated metastases at the bottom of the left chest
cavity and left subclavicular lymph nodes were controlled with
chemotherapy, surgery and radiotherapy. Over the last 20 months, we
have continued to administer low-dose oral prednisolone (5 mg/day),
without recurrence.
Glucocorticoids are often administered to patients
with thymomas to treat associated symptoms of myasthenia gravis,
rather than the tumor itself. Funakoshi et al reported that
thymoma and thymic carcinoma express glucocorticoid receptors, and
glucocorticoids may directly affect tumor cells in addition to
affecting associated lymphocytes (11). There have been a few reports
describing the marked clinical response of refractory thymoma, but
not of thymic carcinoma (12).
Although the glucocorticoid receptor expression of tumor cells was
not investigated in our patient, low-dose prednisolone, which was
administered to treat eosinophilic pneumonia, may promote the
response of resistant cells to multidisciplinary treatment and
maintain a disease-free status in our patient.
In conclusion, the multidisciplinary treatment
described herein may achieve long-term survival in patients with
stage IVb thymic carcinoma.
References
|
1
|
Kondo K and Monden Y: Therapy for thymic
epithelial tumors: A clinical study of 1320 patients from Japan.
Ann Thorac Surg. 76:878–885. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Suster S and Rosai J: Thymic carcinoma. A
clinicopathologic study of 60 cases. Cancer. 67:1025–1032. 1991.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Toyokawa G, Taguchi K, Kojo M, Toyozawa R,
Inamasu E, Morodomi Y, Shiraishi Y, Takenaka T, Hirai F, Yamaguchi
M, et al: Recurrence of thymic neuroendocrine carcinoma 24 year
after total excision: A case report. Oncol Lett. 6:147–149.
2013.PubMed/NCBI
|
|
4
|
Bott MJ, Wang H, Travis W, Riely GJ, Bains
M, Downey R, Rusch V and Huang J: Management and outcomes of
relapse after treatment of thymoma and thymic carcinoma. Ann Thorac
Surg. 92:1984–1992. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hishida T, Nomura S, Yano M, Asamura H,
Yamashita M, Ohde Y, Kondo K, Date H, Okumura M and Nagai K:
Japanese Association for Research on the Thymus (JART): Long-term
outcome and prognostic factors of surgically treated thymic
carcinoma: Results of 306 cases from a Japanese nationwide database
study. Eur J Cardiothorac Surg. 49:835–841. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ebgels EA and Pfeiffer RM: Malignant
thymoma in the United states: Demographic patterns in incidence and
associations with subsequent malignancies. Int J Cancer.
105:546–551. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Travis WD, Brambilla E, Muller-Hermelink
HK and Hariis CC: World health organization classification of
tumorsPathology and genetics of tumors of the lung, pleura, thymus
and heart. Chapter. 3rd. IARC Press; Lyon: pp. pp145–pp975.
2004
|
|
8
|
Wright CD, Wain JC, Wong DR, Donahue DM,
Gaissert HA, Grillo HC and Mathisen DJ: Predictors of recurrence in
thymic tumors: Importance of invasion, world health organization
histology and size. J Thorac Cardiovasc Surg. 130:1413–1421. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ogawa K, Toita T, Uno T, Fuwa N,
Kakinohana Y, Kamata M, Koja K, Kinjo T, Adachi G and Murayama S:
Treatment and prognosis of thymic carcinoma: A retrospective
analysis of 40 cases. Cancer. 94:3115–3119. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Nakamura Y, Kunito H, Kubota K, Sekine I,
Shinkai T, Tamura T, Kodama T, Sumi M, Kohno S and Saijo N:
Platinum-based chemotherapy with or without thoracic radiation
therapy in patients with unresectable thymic carcinoma. Jpn J Clin
Oncol. 30:385–388. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Funakoshi Y, Shiono H, Inoue M, Kadota Y,
Ohta M, Matsuda H, Okumura M and Eimoto T: Glucocorticoids induce
G1 cell cycle arrest in human neoplastic thymic epithelial cells. K
Cancer Res Clin Oncol. 131:314–322. 2005. View Article : Google Scholar
|
|
12
|
Kodama K, Doi S, Higashiyama M, Yokouchi
H, Yasuda T and Funai H: Dramatic response of postthymomectomy
myasthenia gravis with multiple lung nodules to corticosteroids.
Ann Thorac Surg. 64:555–557. 1997. View Article : Google Scholar : PubMed/NCBI
|