Introduction
Lung cancer has the highest mortality rate
worldwide, with a 5-year survival of only 15% (1). Non-small-cell lung cancer (NSCLC) is
considered to be the most frequent type of lung cancer, accounting
for 85% of the total number of cases (1). Unfortunately, the disease is usually
progressed at diagnosis and locoregional strategies are no longer
considered as therapeutic options. Until recently, cytotoxic
chemotherapy was the only treatment option for advanced disease,
with a median overall survival of 12 months (1).
NSCLC comprises several subtypes in terms of
histological and morphological characteristics, exhibiting
significant genetic variability (2).
Lung adenocarcinomas carrying epidermal growth factor receptor
(EGFR) mutations were recently identified as a unique group of
entities, based on common etiopathogenetic characteristics and
unique tumor biology; importantly, they all depend on EGFR for
their proliferation and metastasis (2). The introduction of reversible EGFR
tyrosine kinase inhibitors (TKIs), such as erlotinib, has changed
the management of metastatic disease in this subset of patients
(3).
Interestingly, although erlotinib is highly
effective in patients with EGFR mutations, it may occasionally
prove useful, even in the absence of mutations. For example,
Shepherd et al concluded that, in pretreated patients,
erlotinib achieved a response rate of 8.9% and the median duration
of the response was 7.9 months, irrespective of their mutation
status (4). The progression-free and
overall survival were 2.2 and 6.7 months, respectively, which were
significantly superior to those in patients receiving best
supportive care (4). The exact
mechanism underlying the effectiveness of erlotinib in this setting
remains unknown, and every effort to explain this benefit is highly
speculative.
We herein present the cases of 2 patients with
advanced disease who were treated with oral erlotinib and achieved
remarkable disease stabilization for several years, despite
harbouring no EGFR mutations (EGFR wild-type).
Case 1
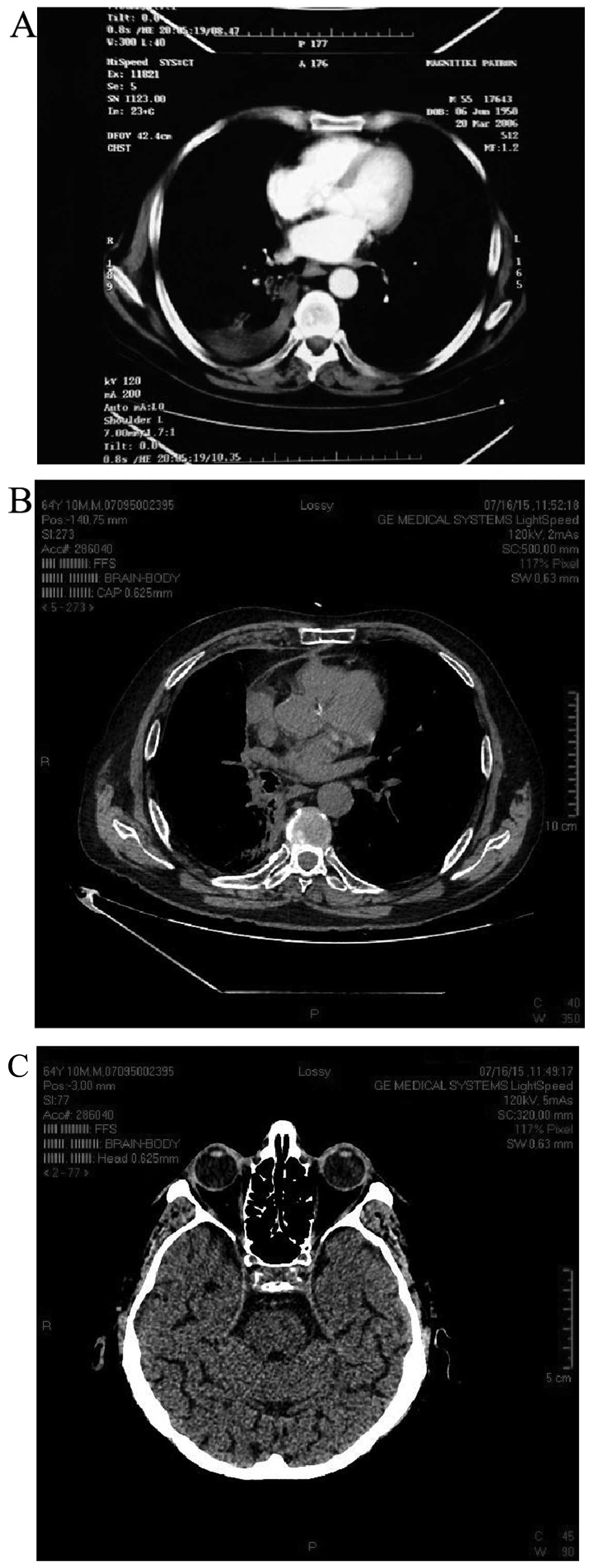
A 54 year-old male patient, who was a former smoker,
was referred to the Division of Oncology, Department of Internal
Medicine, University Hospital of Patras Medical School (Patras,
Greece) with lung adenocarcinoma in February, 2005. The diagnosis
was made following bronchoscopy and cytological material
examination, obtained after a thoracic computed tomography (CT)
scan revealed a 3-cm mass in the upper segment of the right lower
lobe, with enlarged ipsilateral hilar and mediastinal lymph nodes.
Imaging also revealed enlarged contralateral (left) cervical and
supraclavicular lymph nodes. Additionally, a brain CT scan revealed
a lesion in the left temporal lobe, surrounded by significant
edema. The patient was referred for brain radiation therapy and his
neurological signs improved. Following radiotherapy, the patient
received 6 cycles of paclitaxel/gemcitabine (from May to July,
2005), followed by radiotherapy to the lung and mediastinum. The
patient was then placed on a surveillance program. After 3 months,
follow-up imaging revealed a newly enlarged ipsilateral
supraclavicular lymph node. Although second-line chemotherapy
treatment with 6 cycles of cisplatin/pemetrexed was administered to
the patient, there was disease progression to the right lung. Thus,
the patient received third-line chemotherapy with 6 cycles of
docetaxel (from April to August, 2006). Restaging showed that the
patient achieved partial remission, while the cervical and
supraclavicular lymph nodes were no longer palpable on physical
examination (Fig. 1A). A chest CT
scan, performed in January, 2009, revealed disease progression and
the patient was initiated on fourth-line treatment with erlotinib
(Tarceva; Roche, Basel, Switzerland), 150 mg per os, once
daily. There were no signs of further progression based on
follow-up imaging, indicating stable disease. In December, 2015,
almost 7 years after the initiation of therapy with erlotinib, the
patient remained in a good overall condition, without clinical or
radiological signs of progression (Fig.
1B). The cytological material was retrospectively analyzed and
the tumor was found to be EGFR wild-type, as reverse transcription
polymerase chain reaction analysis revealed no mutations in exons
18, 19, 20 or 21 of the EGFR gene.
Case 2
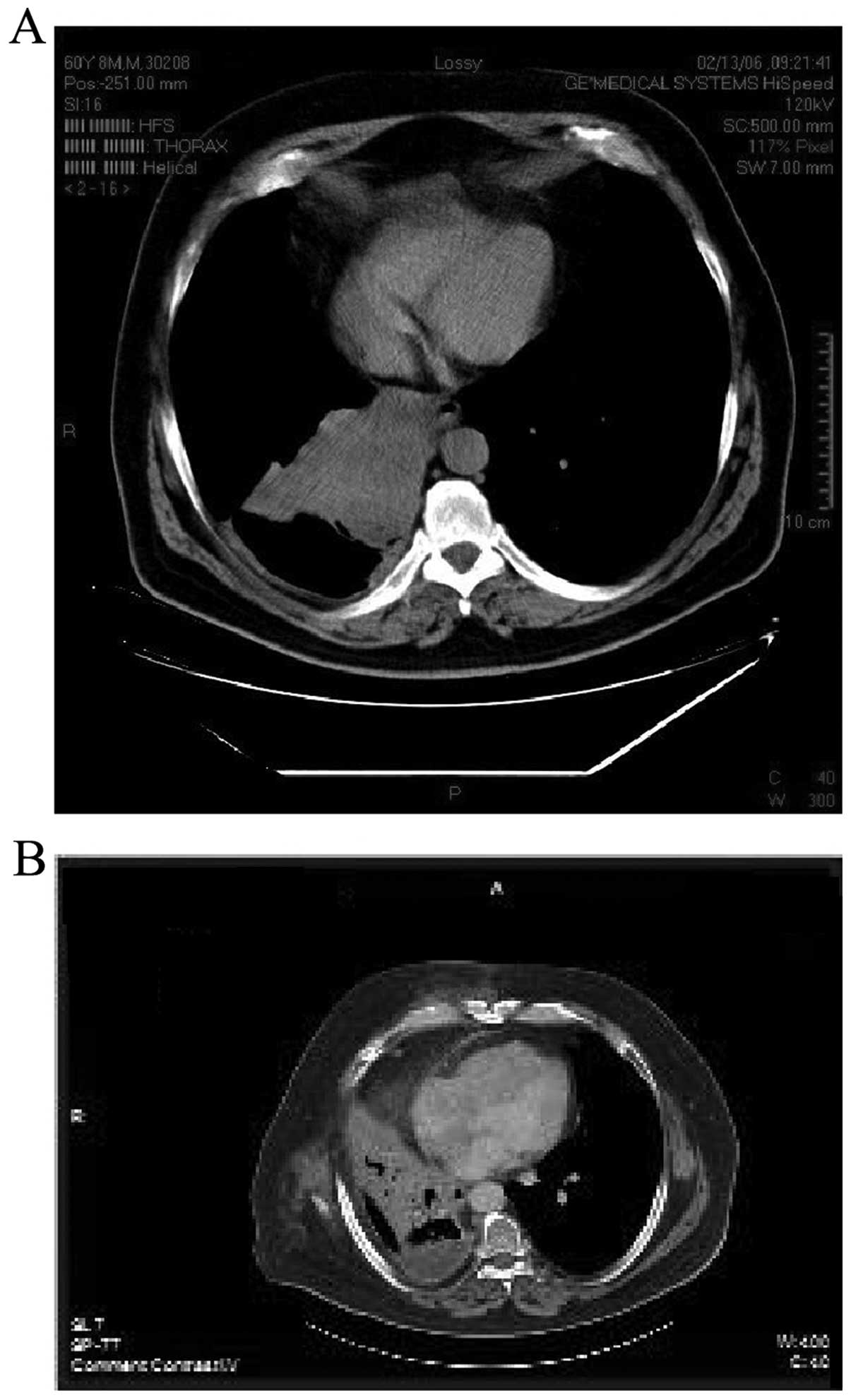
A 61-year-old male patient, who was a smoker, was
diagnosed with undifferentiated NSCLC, according to the
histological report, in March, 2006. As shown in Fig. 2A, the tumor, sized 12×9.8×8.2 cm, was
located in the middle lobe of the right lung and it was
infiltrating the lower pulmonary vein (T4 based on the TNM staging
system) (5). The specimen was tested
for EGFR mutations in exons 18, 19, 20 and 21, and the results
revealed that the tumor was wild-type. The patient was not eligible
for lung resection due to his physical and medical condition.
In May, 2006, a combination of cisplatin and
etoposide was administered to the patient, with the addition of
radiation therapy, until July, 2006. A follow-up performed in
November, 2006 revealed that the disease had progressed, as a new
mediastinal mass was found, sized 4.5×3.5 cm, infiltrating the
esophageal wall. One month later, while on chemotherapy with
docetaxel, the patient was diagnosed with disease progression in
the thorax and was placed on a new chemotherapy scheme with
pemetrexed. Subsequently, the patient received 9 cycles prior to
being diagnosed with a new pleural effusion of neoplastic origin in
October, 2007.
The patient therefore received oral erlotinib (150
mg once per day) and achieved stable disease for >5.5 years
(from October, 2007 to May, 2013) (Fig.
2B). However, in May 2013, the patient noticed an enlarged left
cervical lymph node. A biopsy of the lesion revealed the
histological characteristics of squamous cell lung carcinoma (EGFR
wild-type).
Subsequently, the patient received further treatment
with different chemotherapeutic schemes, including
carboplatin/gemcitabine, carboplatin/paclitaxel and vinorelbine. In
April, 2014, the condition of the patient deteriorated
significantly and he developed disease progression, eventually
leading to death after a brief period of time.
Discussion
Tyrosine kinases (TKs) control critical pathways
that regulate important cellular activities (6). Once overexpressed or mutated, TKs play
a significant role in the pathogenesis and development of
malignancies. When a tumor is dependent on such a mechanism,
specific molecules targeting these pathways may be considerably
effective (6).
However, erlotinib does not have long-lasting
effects, since all tumors inevitably develop resistance after a
median of 6–12 months (1). Half of
the cases will carry a number of second-site mutations, which are
able to alter the binding of the drug to the EGFR-specific domain.
The most common event is an acquired T790M missence mutation
(referred to as gatekeeper mutation) that accounts for 50–60% of
the acquired resistance (1).
Amplification of MET tyrosine kinase is another mechanism that
accounts for ~22% of the cases and occurs with or without a
concurrent T790M mutation (1).
Another known mechanism includes transformation to small-cell lung
cancer phenotypes (14%) (1).
The response rates are particularly high in patients
with EGFR mutations who are administered EGFR inhibitors as
first-line therapy (6). In selected
patients with mutation positivity, the response rates with
first-line treatment with EGFR inhibitors may be as high as 75%
(1). However, when administered as
second- or third-line treatment, the levels of EGFR mutation and
tumor sensitivity were not found to be strongly correlated,
indicating a possible non-EGFR-related effect in this subgroup of
patients (6,7).
Apart from the EGFR status, other factors have been
suggested to be predictive biomarkers of a positive outcome after
receiving an EGFR inhibitor, including smoking history, female
gender, Japanese ethnicity, adenocarcinoma with bronchoalveolar
characteristics and the development of a skin rash (7,8). Both
patients described herein were Caucasian. Moreover, we were unable
to define the presence of bronchoalveolar characteristics in the
first patient, whereas the tumor of our second patient appeared to
be of squamous cell histology. Furthermore, our patients were male
and smokers, suggesting that the effect of erlotinib was
independent of the classical risk factors. Of note, during the
entire course of his treatment, the first patient did not complain
of a severe skin rash; however, the second patient developed a
grade 2 acne-like rash. Both patients achieved long-term disease
stabilization and survival, despite the fact that they did not
achieve complete or partial response. Determining the EGFR status
in patients with squamous cell lung carcinoma remains
controversial. However, our second case underscores that a subset
of patients may benefit from EGFR inhibitors, with some patients
achieving durable disease stabilization.
A retrospective long-term survival study of patients
receiving therapy with erlotinib performed in Germany, evaluated
the characteristics of patients (irrespective of the EGFR status)
who survived over 12 months, and they matched those of the present
cases (9). However, in the German
study, only 25% of long-term survivors reached 24 months while on
treatment (9).
What caused our patients to exceed the 60–70-month
time frame with progression-free survival remains unknown, and
every effort to explain why certain patients achieve significant
benefits remains highly speculative. Erlotinib is a molecule that
specifically targets EGFR TKs, as it binds reversibly to the
adenosine triphosphate binding site of the receptor. Thus,
signaling cascades are not initiated and EGFR-dependent tumors are
inhibited. However, our patients had no detectable mutations, which
means that there are alternative mechanisms underlying the action
of erlotinib. A possible explanation is that our patients possibly
had an amplification in the gene responsible for EGFR activation,
thus having an overactive TK, without harboring any mutations.
From a clinical perspective, our patients, as well
as one other case previously reported in the literature that
exceeded 5 years of disease stabilization, exhibited no spread of
the disease to the liver, bones, or adrenal glands, despite the
long course of their disease (10).
By contrast, they were mainly characterized by bulky nodal disease,
pointing towards tumors with a predisposition to lymphatic spread,
and a relative inability for hematogenous spread. Lymphatic spread
is unique, as neovascularization is not an essential prerequisite
(11). It was recently demonstrated
that, compared with hematogenous spread, lymphatic spread is
independent of epithelial-to-mesenchymal transition (EMT) in the
primary tumor (12). This is
particularly important, as it indicates that, in our patients, the
tumors may have had an intrinsic defect in the EMT pathway,
predisposing to lymphatic rather than hematogenous spread.
Moreover, the activity of erlotinib has been shown to be correlated
with EMT status via interfering with the ILK-PINCH-Parvin complex
(13). Therefore, we may hypothesize
that erlotinib may have affected the EMT pathway in our
patients.
In conclusion, TKI inhibitors may occasionally be
associated with impressive long-term disease stabilization,
irrespectively of the EGFR status. Unfortunately, these patients
constitute a substantial minority. Further research is required to
identify the subset of patients that will benefit the most from
this treatment.
Written informed consent was obtained from the
patients for the publication of the case reports and any
accompanying images.
References
|
1
|
Nelson V, Ziehr J, Agulnik M and Johnson
M: Afatinib: Emerging next-generation tyrosine kinase inhibitor for
NSCLC. Onco Targets Ther. 6:135–143. 2013.PubMed/NCBI
|
|
2
|
Köhler J and Schuler M: Afatinib,
erlotinib and gefitinib in the first-line therapy of egfr
mutation-positive lung adenocarcinoma: A review. Onkologie.
36:510–518. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Health Quality Ontario, . Epidermal Growth
Factor Receptor Mutation (EGFR) testing for prediction of response
to EGFR-Targeting Tyrosine Kinase Inhibitor (TKI) drugs in patients
with advanced non-small-cell lung cancer: An evidence-based
analysis. Ont Health Technol Assess Ser. 10:1–48. 2010.
|
|
4
|
Shepherd FA, Pereira J Rodrigues, Ciuleanu
T, Tan EH, Hirsh V, Thongprasert S, Campos D, Maoleekoonpiroj S,
Smylie M, Martins R, et al: Erlotinib in previously treated
non-small-cell lung cancer. N Engl J Med. 353:123–132. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Goldstraw P: Staging Manual in Thoracic
Oncology. Editorial Rx Press; Orange Park, FL: 2009, View Article : Google Scholar
|
|
6
|
Pao W, Miller V, Zakowski M, Doherty J,
Politi K, Sarkaria I, Singh B, Heelan R, Rusch V, Fulton L, et al:
EGF receptor gene mutations are common in lung cancers from ‘never
smokers’ and are associated with sensitivity of tumors to gefitinib
and erlotinib. Proc Natl Acad Sci USA. 101:13306–13311. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Karam I and Melosky B: Response to
second-line erlotinib in an EGFR mutation-negative patient with
non-small-cell lung cancer: Make no assumptions. Curr Oncol.
19:42–46. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Dudek AZ, Kmak KL, Koopmeiners J and
Keshtgarpour M: Skin rash and bronchoalveolar histology correlates
with clinical benefit in patients treated with gefitinib as a
therapy for previously treated advanced or metastatic non-small
cell lung cancer. Lung Cancer. 51:89–96. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Schumann C, Heigener D, Dittrich I,
Abenhardt W, Dederke B, Duell T, et al: Long term benefit from
erlotinib treatment is independent of prognostic factors and
therapeutic response (abstract 9146). Eur J Cancer. 7:12009.
|
|
10
|
Polychronidou G and Papakotoulas P:
Long-term treatment with erlotinib for EGFR wild-type non-small
cell lung cancer: A case report. Case Rep Oncol. 6:189–196. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Jeong HS, Jones D, Liao S, Wattson DA, Cui
CH, Duda DG, Willett CG, Jain RK and Padera TP: Investigation of
the lack of angiogenesis in the formation of lymph node metastases.
J Natl Cancer Inst. 107(pii): djv1552015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Markiewicz A, Książkiewicz M, Seroczyńska
B, Skokowski J, Szade J, Welnicka-Jaskiewicz M, Wełnicka-Jaśkiewicz
M and Zaczek AJ: Heterogeneity of mesenchymal markers
expression-molecular profiles of cancer cells disseminated by
lymphatic and hematogenous routes in breast cancer. Cancers.
5:1485–1503. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Augustin A, Lamerz J, Meistermann H,
Colling S, Scheiblich S, Hermann JC, Duchateau-Nguyen G, Tzouros M,
Avila DW, Langen H, et al: Quantitative chemical proteomics
profiling differentiates erlotinib from gefitinib in EGFR wild-type
non-small cell lung carcinoma cell lines. Mol Cancer Ther.
12:520–529. 2013. View Article : Google Scholar : PubMed/NCBI
|