Introduction
Intravascular large B-cell lymphoma (IVLBCL) is a
rare entity characterized by exclusive or predominant growth of
neoplastic cells within the lumen of blood vessels. This disease
was recently recognized as a subtype of diffuse large B-cell
lymphoma by the World Health Organization (WHO) (1). The clinical presentation of IVLBCL
varies widely due to occlusion of small vessels or capillaries in
different organs. The most common clinical symptoms include fever,
general fatigue, neurological manifestations and non-specific skin
eruptions (2,3). Although autopsy findings have revealed
that pulmonary involvement is also common in this disease, a
primary presentation in the lung is uncommon and has rarely been
described. In non-Hodgkin lymphoma (NHL), extranodal disease
accounts for 24–50% of all cases, whereas only 34% of the cases
include pulmonary lesions, with primary pulmonary lesions
presenting in <1% of the patients (4). As early pulmonary IVLBCL diagnosis is
difficult and treatment for pulmonary IVLBCL is less effective, the
prognosis for the majority of the patients is poor (4). We herein report the case of a patient
with pulmonary IVLBCL who was successfully treated with R-CHOP and
has survived for >1 year.
Case report
A 73-year-old man visited a local clinic complaining
of general malaise, dry cough, hoarseness, a 6-kg weight loss and
fever. The patient was referred to our hospital, as no improvement
was observed after 3 months. The patient's medical history was
unremarkable, he had never smoked and had no history of
occupational dust exposure. On admission, there were no enlarged
superficial lymph nodes, skin lesions, or neurological
abnormalities There were no abnormal findings on chest
auscultation. Laboratory tests revealed the following results:
Total leukocyte count, 5,400 cells/mm3 (69% neutrophils,
11% lymphocytes, 20% monocytes, 0% basophils and eosinophils);
hemoglobin concentration, 11.6 g/dl; mean corpuscular volume, 82.5
fl; reticulocyte percentage, 8%; platelet count, 117,000/µl;
C-reactive protein, 17.9 mg/dl; ferritin, 5,720 ng/ml; serum
lactate dehydrogenase, 562 U/l; and soluble interleukin-2 receptor,
8,313 U/ml. Hypoxemia was also present, with an arterial oxygen
tension of 53.2 Torr (room air). The pulmonary function test
results were within normal limits, except for a reduction in the
diffusion capacity of carbon monoxide (64.3% of the predicted
value). There were no laboratory data suggestive of infection or
autoimmune disease.
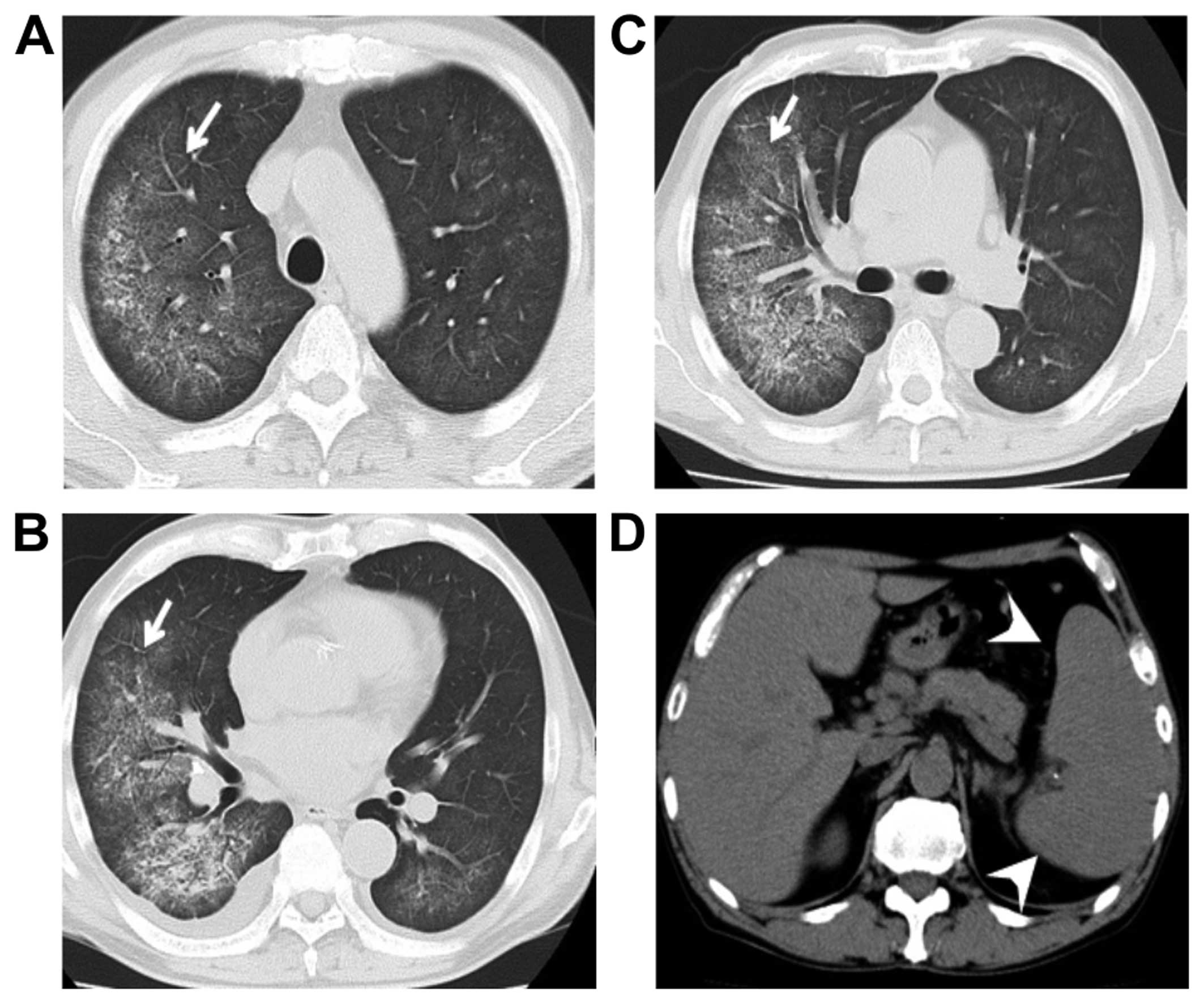
Chest radiography revealed diffusely spreading
ground-glass opacities (GGOs) in both lungs, predominantly in the
inferior lobes, but there were no signs of cardiac enlargement,
pleural effusion, or enlarged mediastinal lymph nodes. Bilateral
diffuse GGOs were also evident on computed tomography (CT) scans,
but there were no signs of interlobular septal thickening or
decreased volume. The spleen was also enlarged on CT (Fig. 1). Gallium scintigraphy also revealed
diffuse and increased uptake in the lung field, as well as
increased uptake in the spleen and splenomegaly.
At that point, the differential diagnosis included
atypical pneumonia, eosinophilic pneumonia, hypersensitivity
pneumonitis, pulmonary alveolar hemorrhage, pulmonary alveolar
proteinosis and intravascular large B-cell lymphoma. However, a
transbronchial lung biopsy (TBLB) could not be performed due to the
patient's coughing. Antibiotic and steroid treatment was initiated,
but the patient's general condition continued to deteriorate. A
lung biopsy was then performed using video-assisted thoracoscopic
surgery (VATS).
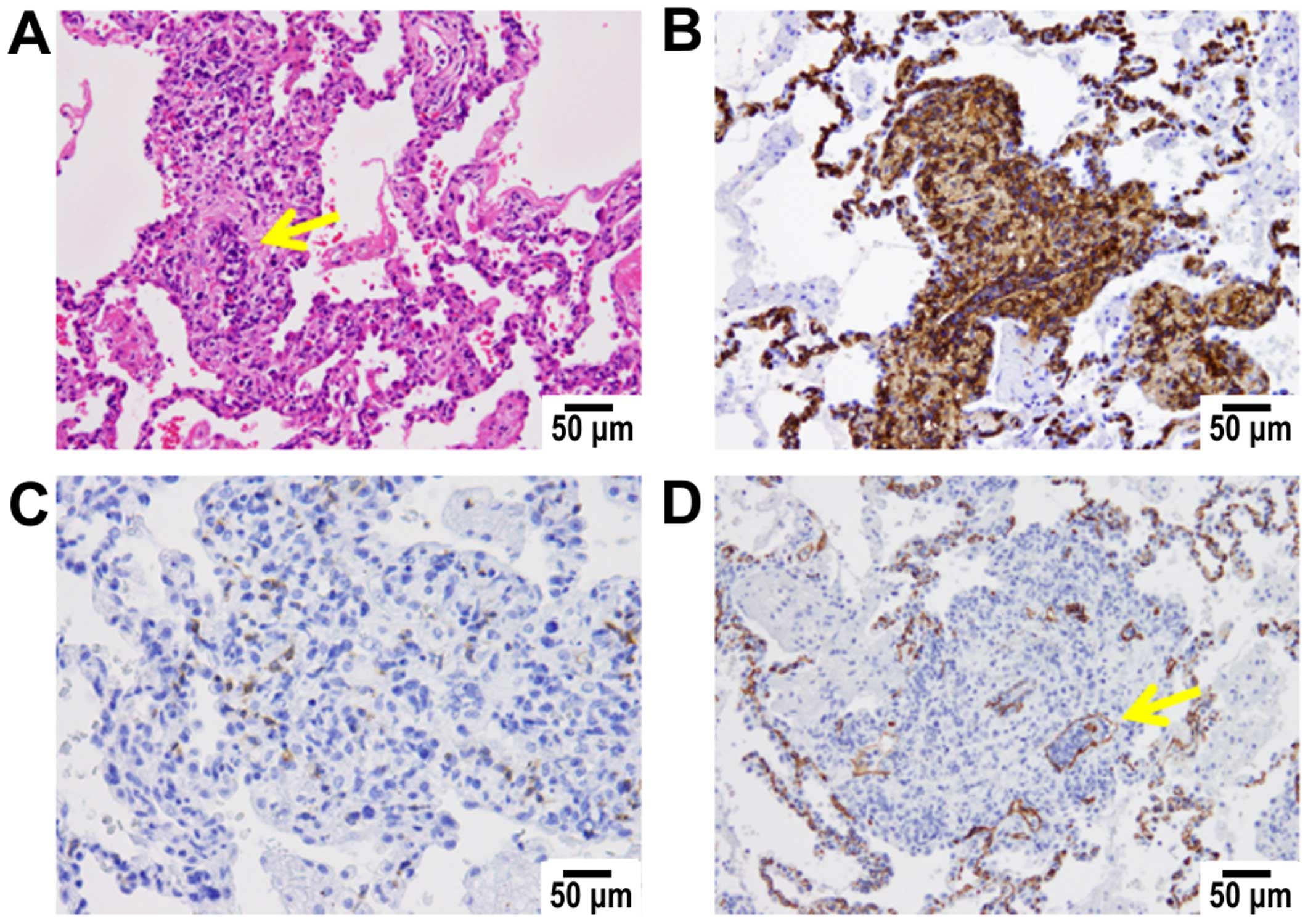
Histological examination of the bioptic specimen
revealed several large atypical cells, mainly located within the
small vessels and alveolar wall capillaries (Fig. 2A and D). These atypical cells also
infiltrated an extravascular area of the stroma, with a patchy
distribution in the enlarged interstitium throughout the lesion.
Imunohistochemically, the atypical cells were positive for CD20
(Fig. 2B) but were negative for CD5
(Fig. 2C). Epstein-Barr virus
(EBV)-encoded RNA in situ hybridization was also performed,
but only a few positive cells were detected, ruling out involvement
of EBV in this case. Bone marrow infiltration was not observed,
although phagocytosis of neutrophils by macrophages was present at
a very low frequency. The findings of the skin biopsy were
unremarkable. Based on these findings, the patient was diagnosed
with IVLBCL.
As respiratory failure was progressing rapidly,
steroid pulse therapy and oral cyclophosphamide (100 mg per day for
6 days) were administered until the histological results became
available. After diagnosis was confirmed, six courses of R-CHOP
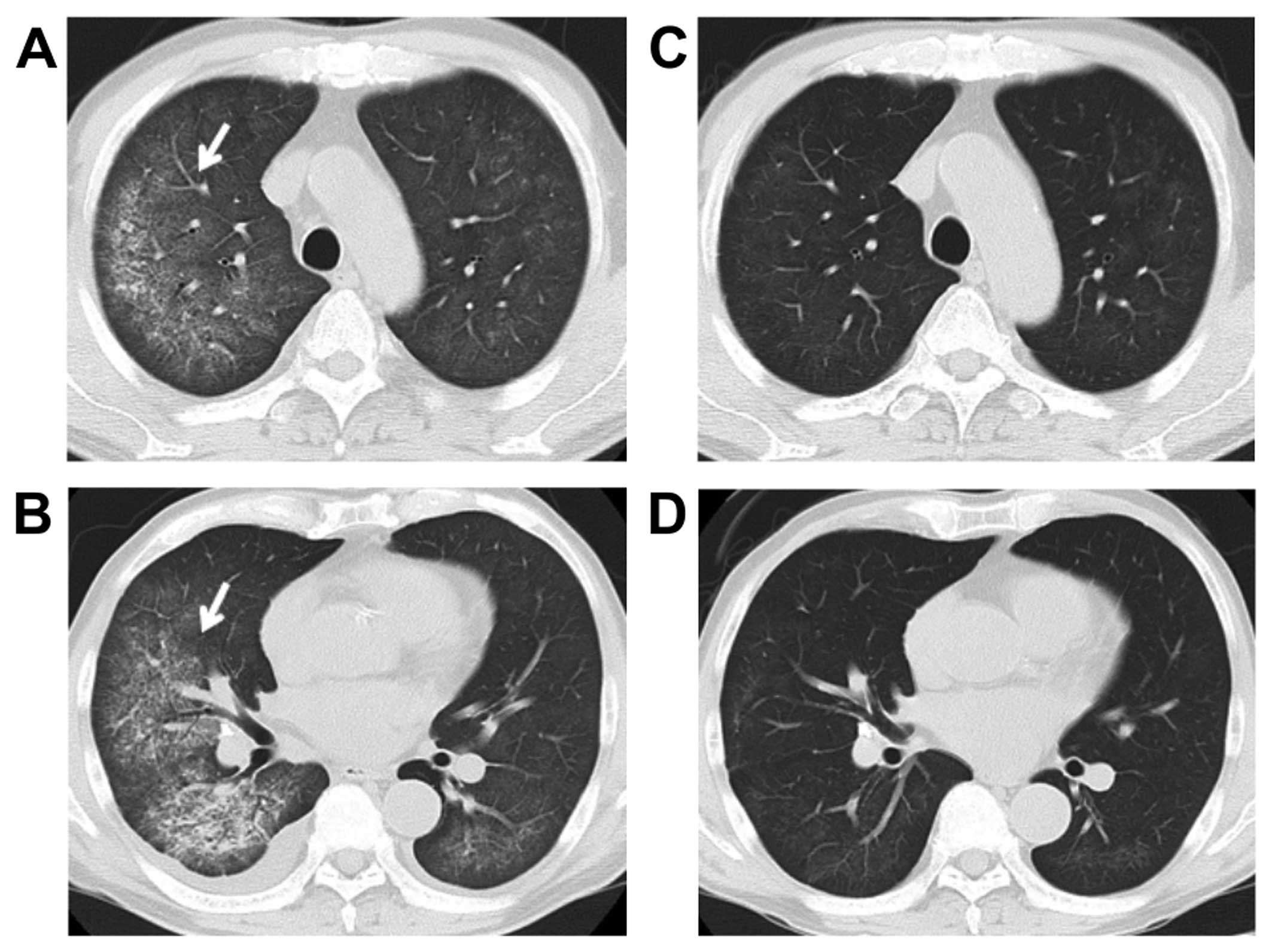
immunochemotherapy were administered. The GGOs in the lung field
rapidly disappeared and the respiratory status improved (Fig. 3). A positron emission tomography
(PET)/CT scan after the completion of the sixth course revealed no
uptake in the lung or spleen and the patient remains alive and
symptom-free for >1 year.
The patient has provided his consent regarding the
publication of the case details.
Discussion
IVLBCL is characterized by proliferation of atypical
lymphoid cells within the lumen of capillaries. IVLBCL is a rare
variant of diffuse large B-cell lymphoma that has been included in
the WHO classification (5). The
central nervous system (CNS) and skin are usually involved. By
contrast, IVLBCL patients in Asian countries often exhibit
hepatosplenomegaly, thrombocytopenia and fever, but CNS and skin
involvement are rare (6,7). In the present case, the patient
exhibited findings typical of an Asian patient. In addition,
several pulmonary IVLBCL cases were recently reported in Asia
(2–4).
Recently, fluorodeoxyglucose (FDG)-PET/CT was shown
to be useful for staging NHL (8),
and several authors reported that FDG-PET/CT is a powerful tool for
early diagnosis of IVLBCL (9);
however, biopsy is essential. Due to its low invasiveness, TBLB is
one of the most useful biopsy techniques for pulmonary lesions
(4). In the present case,
VATS-guided surgical biopsy was crucial, as TBLB could not be
performed. If diffuse GGOs are present, IVLBCL should be included
in the differential diagnosis, and a biopsy should be proactively
performed.
The recommended treatment is systemic chemotherapy
with an anthracycline-based regimen. However, the majority of
IVLBCL cases are associated with poor prognosis. Recently, R-CHOP
immunochemotherapy was shown to yield better results compared with
CHOP (4,10,11). Our
patient was treated with R-CHOP, and 1 year later there has been no
recurrence. Pulmonary IVLBCL presenting with GGOs is exceedingly
rare, but it should be considered in the differential diagnosis of
respiratory disease presenting with GGOs.
Acknowledgements
The authors are deeply grateful to Hiroshige
Nakamura and Tomohiro Haruki who performed the biopsy using VATS.
We are also indebted to Shu Nakamoto for their invaluable
comments.
References
|
1
|
Swerdllow S, Campo E and Harris NL: WHO
classification of tumours of haematopoietic and lymphoid tissues.
IARC press; France: 2008
|
|
2
|
Xiao D, Fu C, Long X, Liu W, Chen C, Zhou
J and Fan S: Lung intravascular large B-cell lymphoma with ground
glass opacities on chest computed tomography: A case report. Int J
Clin Exp Pathol. 7:5285–5290. 2014.PubMed/NCBI
|
|
3
|
Liu C, Lai N, Zhou Y, Li S, Chen R and
Zhang N: Intravascular large B-cell lymphoma confirmed by lung
biopsy. Int J Clin Exp Pathol. 7:6301–6306. 2014.PubMed/NCBI
|
|
4
|
Chen Y, Ding C, Lin Q, Yang K, Li Y and
Chen S: Primary intravascular large B-cell lymphoma of the lung: A
review and case report. J Thorac Dis. 6:E242–E245. 2014.PubMed/NCBI
|
|
5
|
Kotake T, Kosugi S, Takimoto T, Nakata S,
Shiga J, Nagate Y, Nakagawa T, Take H and Katagiri S: Intravascular
large B-cell lymphoma presenting pulmonary arterial hypertension as
an initial manifestation. Intern Med. 49:51–54. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kawamura T, Sando Y, Tajima S, Hosono T,
Sato M, Maeno Y, Maeno T, Suga T, Kurabayashi M and Nagai R:
Pulmonary intravascular lymphoma complicated with Pneumocystis
carinii pneumonia: A case report. Jpn J Clin Oncol. 31:333–336.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Takamura K, Nasuhara Y, Mishina T, Matsuda
T, Nishimura M, Kawakami Y, Fujita M, Mikuni C and Yamashiro K:
Intravascular lymphomatosis diagnosed by transbronchial lung
biopsy. Eur Respir J. 10:955–957. 1997.PubMed/NCBI
|
|
8
|
Juweid ME, Stroobants S, Hoekstra OS,
Mottaghy FM, Dietlein M, Guermazi A, Wiseman GA, Kostakoglu L,
Scheidhauer K, Buck A, et al: Use of positron emission tomography
for response assessment of lymphoma: Consensus of the imaging
subcommittee of international harmonization project in lymphoma. J
Clin Oncol. 25:571–578. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yamashita H, Suzuki A, Takahashi Y, Kubota
K, Kano T and Mimori A: Intravascular large B-cell lymphoma with
diffuse FDG uptake in the lung by 18FDG-PET/CT without chest CT
findings. Ann Nucl Med. 26:515–521. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zinzani PL, Martelli M, Poletti V, Vitolo
U, Gobbi PG, Chisesi T, Barosi G, Ferreri AJ, Marchetti M,
Pimpinelli N, et al: Practice guidelines for the management of
extranodal non-Hodgkin's lymphomas of adult non-immunodeficient
patients. Part I: Primary lung and mediastinal lymphomas. A project
of the Italian society of hematology, the Italian society of
experimental hematology and the Italian group for bone marrow
transplantation. Haematologica. 93:1364–1371. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Murase T, Yamaguchi M, Suzuki R, Okamoto
M, Sato Y, Tamaru J, Kojima M, Miura I, Mori N, Yoshino T and
Nakamura S: Intravascular large B-cell lymphoma (IVLBCL): A
clinicopathologic study of 96 cases with special reference to the
immunophenotypic heterogeneity of CD5. Blood. 109:478–485. 2007.
View Article : Google Scholar : PubMed/NCBI
|