Introduction
Primary liver cancer is the seventh deadliest type
of cancer, with a 5-year survival rate of 18%. The annual increase
in the incidence of primary liver cancer indicates that this is
among the most rapidly increasing cancer incidences (3.7% in men
and 3.0% in women) (1). Over 90% of
primary liver cancer cases are hepatocellular carcinomas (HCCs).
The majority of the patients present with advanced-stage disease,
with only palliative treatment options available, including
sorafenib and transarterial chemoembolization (2). Sorafenib is a multikinase inhibitor
that is used as first-line palliative treatment in patients with
advanced HCC; it improves the overall survival (mean, 2.8 months)
and is reasonably well-tolerated, with the main side effects being
diarrhoea, weight loss and hand-foot skin reaction (3).
Several cases of spontaneous tumour regression in
HCC have been reported. The estimated incidence of spontaneous
regression is 0.4% in HCC patients (4). Different hypotheses have been
suggested, including tumour ischemia (5), systemic inflammatory reactions,
discontinuation of immunosuppressive therapy (6), abstinence from alcohol consumption or
the use of herbal preparations.
We herein report a case of regression of untreated
metastasized HCC that not associated with any of the abovementioned
mechanisms.
Case report
A 74-year old Caucasian male patient was admitted to
our hospital with a 6-week history of malaise, loss of appetite,
increased abdominal circumference, epigastric tenderness and a
20-kg weight loss. The liver was non-tender and palpable 5 cm below
the costal margin. A firm, non-tender mass, 2 cm in diameter, was
detected in the epigastric angle. There was no lymphadenopathy or a
rectal mass.
The patient's medical history included hepatic
steatosis, hypertension, diabetes mellitus type 2 and percutaneous
transluminal coronary angioplasties after a myocardial infarction.
He had been prescribed insulin, metformin, pantoprazole, isosorbide
mononitrate, enalapril, clopidogrel, felodipine, simvastatin,
temazepam and metoprolol. The patient was a non-smoker and consumed
2 units of alcohol daily.
Hepatitis B and C and human immunodeficiency virus
serology were assessed with the enzyme immunoassay method and were
negative.
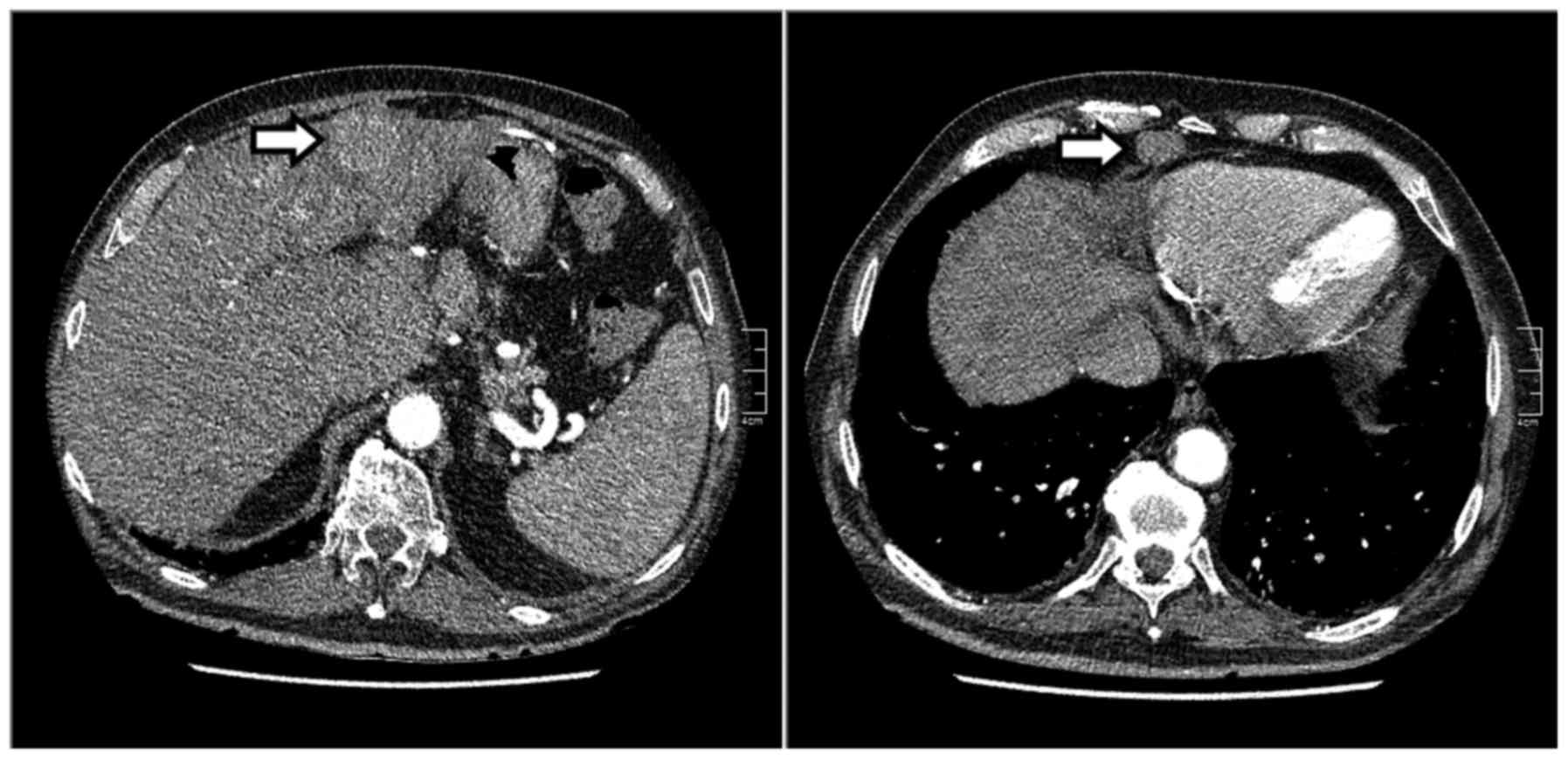
A computed tomography (CT) scan revealed multiple
liver and lung lesions suspicious for metastases, peritoneal
depositions, but no primary tumour (Fig.
1). An ultrasound-guided liver biopsy was performed. The biopsy
revealed malignant cells positive for pancytokeratin, slightly
positive for cytokeratin (CK) 7, α-fetoprotein (AFP), carbohydrate
antigen-125 and CD-10, and negative for CK20, CDX-2, thyroid
transcription factor-1, prostate-specific antigen, CK7 and
monoclonal carcinoembryonic antigen (CEA), findings consistent with
an undifferentiated carcinoma. Additional immunostaining was
positive for hepatocyte paraffin 1 monoclonal antibody, and
polyclonal CEA canalicular immunostaining was also present.
Combined with a serum AFP level of >16,600 kU/l, the diagnosis
of advanced HCC was established. Other laboratory tests are
summarised in Table I. The patient
had a poor performance status (WHO performance status 3) and
declined any form of treatment. Therefore, he was referred to the
general practitioner for supportive palliative care.
 | Table I.Overview of laboratory tests. |
Table I.
Overview of laboratory tests.
| Parameters | Units | Admission 1–2015 | Six months
7–2015 |
|---|
| Hb | mmol/l | 8.4b | 9.4 |
| MCV | fl | 82 | 88 |
| Thrombocytes |
x109/l | 242 | 194 |
| Leukocytes |
x109/l | 7.7 | 9.7 |
| APTT | sec | 28 | – |
| PT | sec | 12.6 | – |
| Sodium | mmol/l | 137 | 139 |
| Potassium | mmol/l | 5.0 | 4.2 |
| Creatinin | µmol/l | 74 | 75 |
| MDRD clearance | ml/min/1.73
m2 | 90 | 89 |
| Total bilirubin | µmol/l | 15 | 13 |
| AP | U/l | 258a | 118 |
| G-GT | U/l | 469a | 294a |
| AST | U/l | 37a | 23 |
| ALT | U/l | 24 | 33 |
| LDH | U/l | 325a | 254a |
| Albumin | g/l | 36.8 | 37.1 |
| Total protein | g/l | 65.2 | 68.5 |
| Calcium | mmol/l | 2.32 | 2.34 |
| AFP | kU/l |
>16600.0a | 1794.7a |
| CEA | ug/l | 1.2 | 1.1 |
| CA-15.3 | kU/l | 14.6 | – |
| CA-19.9 | kU/l | 11 | 18 |
| PSA | ug/l | 1.1 | 0.90 |
| hCG | U/l | <2.0 | <2.0 |
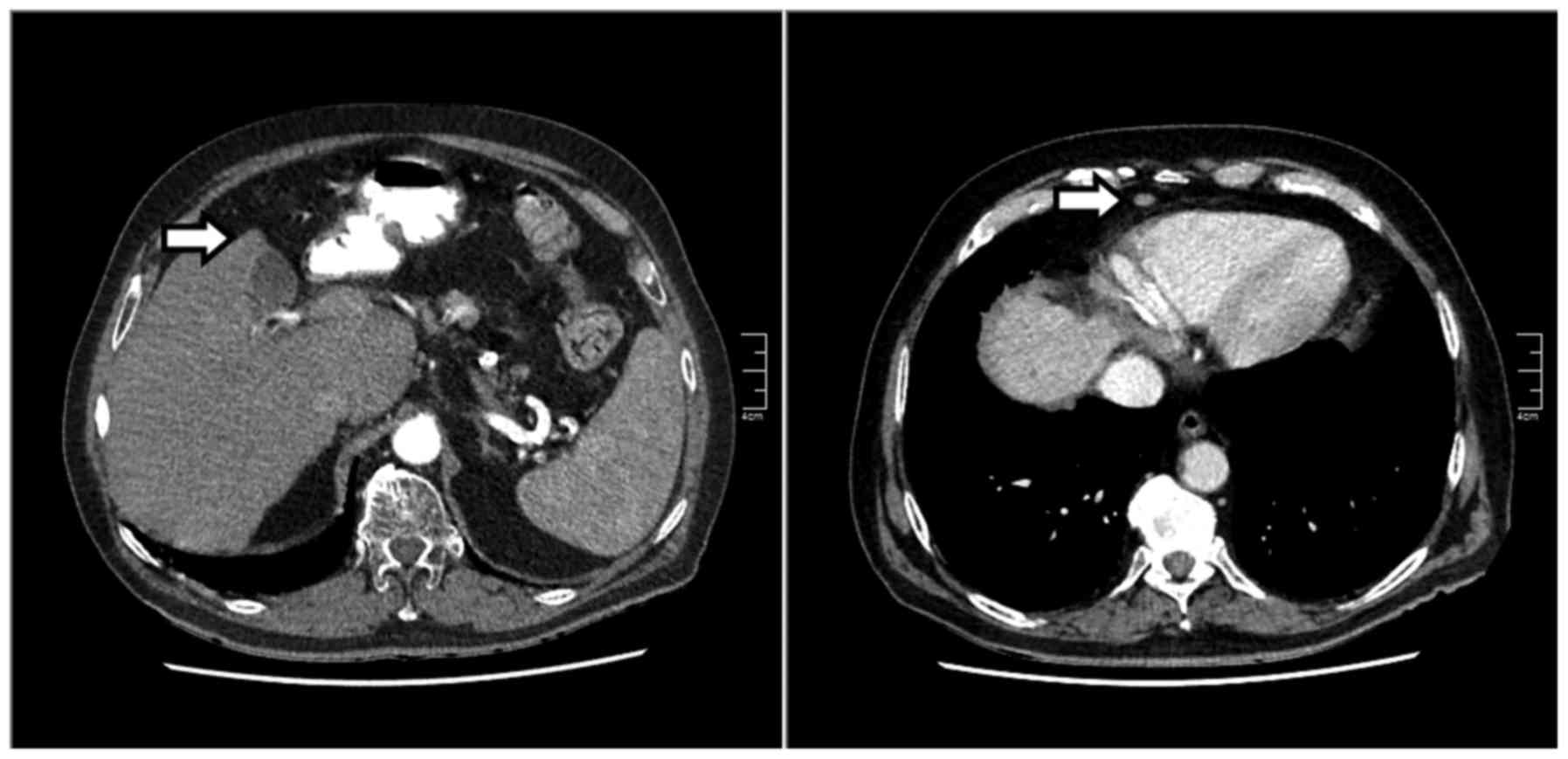
Six months later, the patient attended the
outpatient clinic for re-evaluation of his disease. Over that time
he had suffered a cerebrovascular accident (CVA) with ensuing
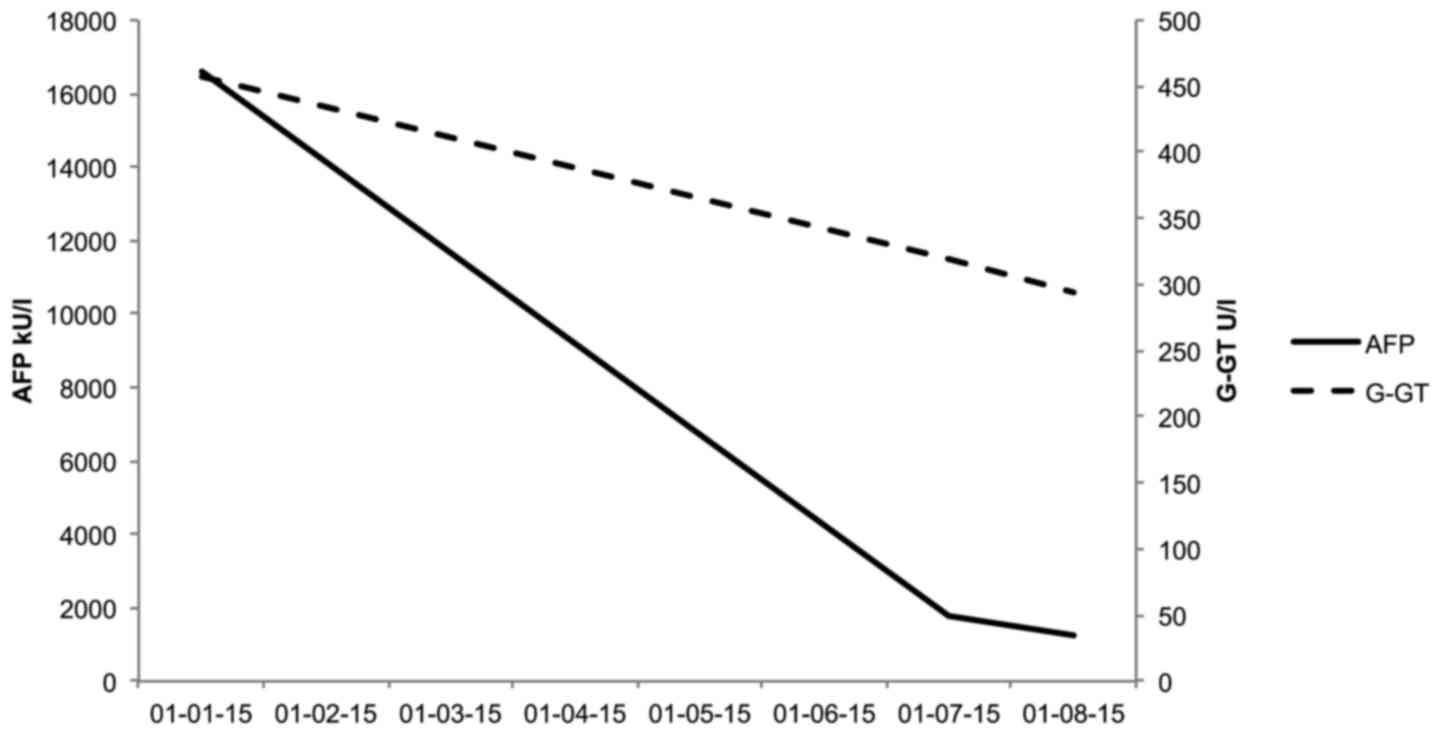
partial hemiparesis. The AFP level had decreased to 1,795 kU/l. The
CT scan revealed that the pulmonary lesion had disappeared, whereas
the suspicious hepatic lesion and the lesion anterior to the
pericardium had significantly decreased in size (Fig. 2). An ultrasound-guided biopsy was
repeated and the pathological examination indicated the previously
diagnosed HCC. An independent academic pathology department
confirmed the results. The patient had gained 4 kg in weight over 6
months and maintained the consumption of 2 units of alcohol per
day; he also reported improvement of his overall condition on a
weekly basis. Two months after the CVA, he had been initiated on
enalapril, furosemide and cucurmin, whereas he discontinued the use
of simvastatin due to the side effects. The patient had not used
androgens or herbal preparations and did not suffer from any type
of inflammatory disease. One month later, the AFP level further
decreased to 1,252 kU/l (Fig.
3).
Discussion
The present case differs from other case reports on
spontaneous regression of HCC, as neither invasive diagnostic
procedures (e.g., hepatic arteriography) nor any form of treatment
was performed, and no apparent inflammatory reaction occurred.
During follow-up, the patient suffered a CVA and started using
enalapril, furosemide and curcumin, which require further
evaluation.
Curcumin is a substance found in turmeric roots and
is a ginger-like herb. Curcumin has shown antitumour properties in
cell lines by blocking nuclear factor-κB, thereby inducing cell
death in curcumin-sensitive cells (7). Moreover, curcumin may act as an iron
chelator and as a hepcidin suppressor. Iron overload in
hemochromatosis is associated with an increased risk of HCC
(8). However, there are insufficient
data to propose iron depletion for the treatment of HCC. The
patient had used curcumin for only 2 months. Given the extent of
the tumour regression, it is unlikely that this may be attributed
to the use of curcumin for 2 months. Moreover, the optimal dosing
for the use of curcumin in oncology is unknown. More research is
required to assess a potential role for curcumin in cancer
treatment.
The only new medications the patient received were
furosemide and enalapril. To the best of our knowledge, furosemide
has no therapeutic properties in cancer, although the combined use
of angiotensin-converting enzyme inhibitors and curcumin has been
associated with inhibition of angiogenesis and diminished tumour
growth in HCC in mice (9).
Some of the other medications used by the patient
have been associated with a decreased risk of HCC. However, these
are unlikely causes of tumour regression, as the tumour developed
while the patient was receiving these preparations. Aspirin, but
not non-aspirin non-steroidal anti-inflammatory drugs (NSAIDs), has
been associated with a reduced risk of HCC (risk ratio=0.59) in a
large prospective observational study (10). The non-randomized allocation of
treatment increases the risk of confounding of results. Our patient
used clopidogrel, which is a non-aspirin NSAID. Metoprolol has been
associated with an inhibition of low-density lipoprotein
cholesterol synthesis in a study on human cell lines, thereby
reducing the risk of HCC (11).
Metformin has been associated with a decreased risk of HCC in a
meta-analysis of 8 observational studies (odds ratio=0.50), whereas
insulin usage increased the risk on HCC (odds ratio=1.62) (12). Metformin decreases insulin resistance
and inhibits the mammalian target of rapamycin pathway, thereby
inhibiting cell proliferation and inducing apoptosis (13). Simvastatin was associated with a
decreased risk of HCC in a large epidemiological study (14); thus, its discontinuation would
increase rather than reduce the risk of HCC. To the best of our
knowledge, pantoprazole, felodipine and temazepam have no
therapeutic properties in cancer.
Ischemia may have contributed to tumour regression,
given the patient's history of cardiovascular and cerebrovascular
disease. However, although the CT scan revealed calcifications of
the superior mesenteric artery, there was no thrombosis of the
hepatic artery or the portal vein. Moreover, the extrahepatic
lesions decreased in size. Thus, there appears to be no possible
route through which CVA exerted any effect on the regression of the
HCC and its metastases. Thus, ischemia appears to be an unlikely
cause of tumour regression in this patient.
Regression of HCC has been associated with systemic
inflammatory responses (e.g., regression following cholangitis or
capsular rupture) (5). It is
unlikely that any inflammatory reaction occurred, given the absence
of fever, leukocytosis, or elevation of the C-reactive protein
levels. It is therefore unlikely that inflammation contributed to
tumour regression. More research is required to elucidate the
mechanisms underlying the spontaneous regression of HCC in the
present case.
In conclusion, we herein report a case of
spontaneous regression of advanced HCC in a Caucasian male patient
that may not be attributed to ischemia or inflammation.
Acknowledgements
We would like to thank Professor JPH Drenth for his
comments during the preparation of the manuscript.
References
|
1
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2016. CA Cancer J Clin. 66:7–30. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Bruix J and Sherman M: American
Association for the Study of Liver Diseases: Management of
hepatocellular carcinoma: An update. Hepatology. 53:1020–1022.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Llovet JM, Ricci S, Mazzaferro V, Hilgard
P, Gane E, Blanc JF, de Oliveira AC, Santoro A, Raoul JL, Forner A,
et al: Sorafenib in advanced hepatocellular carcinoma. N Engl J
Med. 359:378–390. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Oquiñena S, GuillenGrima F, Iñarrairaegui
M, Zozaya JM and Sangro B: Spontaneous regression of hepatocellular
carcinoma: A systematic review. Eur J Gastroenterol Hepatol.
21:254–257. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Huz JI, Melis M and Sarpel U: Spontaneous
regression of hepatocellular carcinoma is most often associated
with tumour hypoxia or a systemic inflammatory response. HPB
(Oxford). 14:500–505. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kumar A and Le DT: Hepatocellular
carcinoma regression after cessation of immunosuppressive therapy.
J Clin Oncol. 34:e90–e92. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Marquardt JU, GomezQuiroz L, Camacho LO
Arreguin, Pinna F, Lee YH, Kitade M, Domínguez MP, Castven D,
Breuhahn K, Conner EA, et al: Curcumin effectively inhibits
oncogenic NF-κB signaling and restrains stemness features in liver
cancer. J Hepatol. 63:661–669. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kowdley KV: Iron, hemochromatosis, and
hepatocellular carcinoma. Gastroenterology. 127:(5 Suppl 1).
S79–S86. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Nasr M, Selima E, Hamed O and Kazem A:
Targeting different angiogenic pathways with combination of
curcumin, leflunomide and perindopril inhibits
diethylnitrosamine-induced hepatocellular carcinoma in mice. Eur J
Pharmacol. 723:267–275. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Sahasrabuddhe VV, Gunja MZ, Graubard BI,
Trabert B, Schwartz LM, Park Y, Hollenbeck AR, Freedman ND and
McGlynn KA: Nonsteroidal anti-inflammatory drug use, chronic liver
disease, and hepatocellular carcinoma. J Natl Cancer Inst.
104:1808–1814. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Naegele H, Behnke B, Gebhardt A and
Strohbeck M: Effects of antihypertensive drugs on cholesterol
metabolism of human mononuclear leukocytes and hepatoma cells. Clin
Biochem. 31:37–45. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Singh S, Singh PP, Singh AG, Murad MH and
Sanchez W: Anti-diabetic medications and the risk of hepatocellular
cancer: A systematic review and meta-analysis. Am J Gastroenterol.
108:881–891; quiz 892. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Jalving M, Gietema JA, Lefrandt JD, de
Jong S, Reyners AK, Gans RO and de Vries EG: Metformin: Taking away
the candy for cancer? Eur J Cancer. 46:2369–2380. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lai SW, Liao KF, Lai HC, Muo CH, Sung FC
and Chen PC: Statin use and risk of hepatocellular carcinoma. Eur J
Epidemiol. 28:485–492. 2013. View Article : Google Scholar : PubMed/NCBI
|