Introduction
Thyroid papillary carcinoma is a type of malignant
cancer that has a low malignancy tendency and a long survival time.
Although the rate of metastasis of the cervical lymph node is high,
40–70% (1), the therapeutic effect is
good. Currently, the general treatment for cervical lymph node
metastasis of the papillary thyroid cancer is neck lymph node
dissection (2,3). Although there is significant controversy
regarding the application of the technique, it still has a crucial
role in the surgical therapy of thyroid cancer and the main type is
the ‘L’ incision (4). For good
exposure and convenience of surgery, ‘L’ incision is used in the
majority of surgeons' cases. However, a scar is evident on vertical
incision. Such scar tissue following surgery affects the appearance
of the patients. As removing a section of the supraclavicular
cutaneous nerve would cause postoperative sensory loss to the neck
and ear lobe area (5), and
consequentially reduce the patients' quality of life, the low neck
incision and ‘eight reserved’ neck dissection (vena jugularis
interna, vena jugularis externa, sternocleidomastoid, accessory
nerve, superclavicular nerve, transverse cervical artery, musculus
omohyoideus and auricular nerve were reserved) were performed to
reduce the side effects of the neck dissection to an optimal
level.
Materials and methods
General materials
The surgical and pathological prospective protocols
of a series of patients with a histological diagnosis of papillary
thyroid cancer between July 2004 and September 2006 were reviewed.
Patients were excluded from the study if they: i) Had a history of
previous thyroid surgery or ii) were referred for completion
thyroidectomy or for recurrent cancer (local or nodal metastases).
This third criterion was operated in order to avoid attributing to
the thyroid procedure, the sequelae of the parathyroid surgery.
Based on these criteria, the study population comprised 87
patients. These 87 papillary thyroid cancer patients were treated
in Zhejiang Cancer Hospital (Zhejiang, China). The patients include
21 males and 66 females. The male to female ratio was 1:3.14. The
age range of the patients was from 12 to 67 years old, and the
median was 35 years old. The patients had been confirmed to exhibit
papillary thyroid cancer by intra-operative frozen pathology or
were diagnosed postoperatively as papillary cancer.
Incision
While performing cervical low incision
(supracervical arc incision), eight functional tissues were
conserved for the patients. These were the vena jugularis interna,
vena jugularis externa, sternocleidomastoid, accessory nerve,
superclavicular nerve, transverse cervical artery, musculus
omohyoideus and auricular nerve. However, the classic ‘L’ incision
only reserves the sternocleidomastoid, vena jugularis interna and
accessory nerve.
Surgical procedures
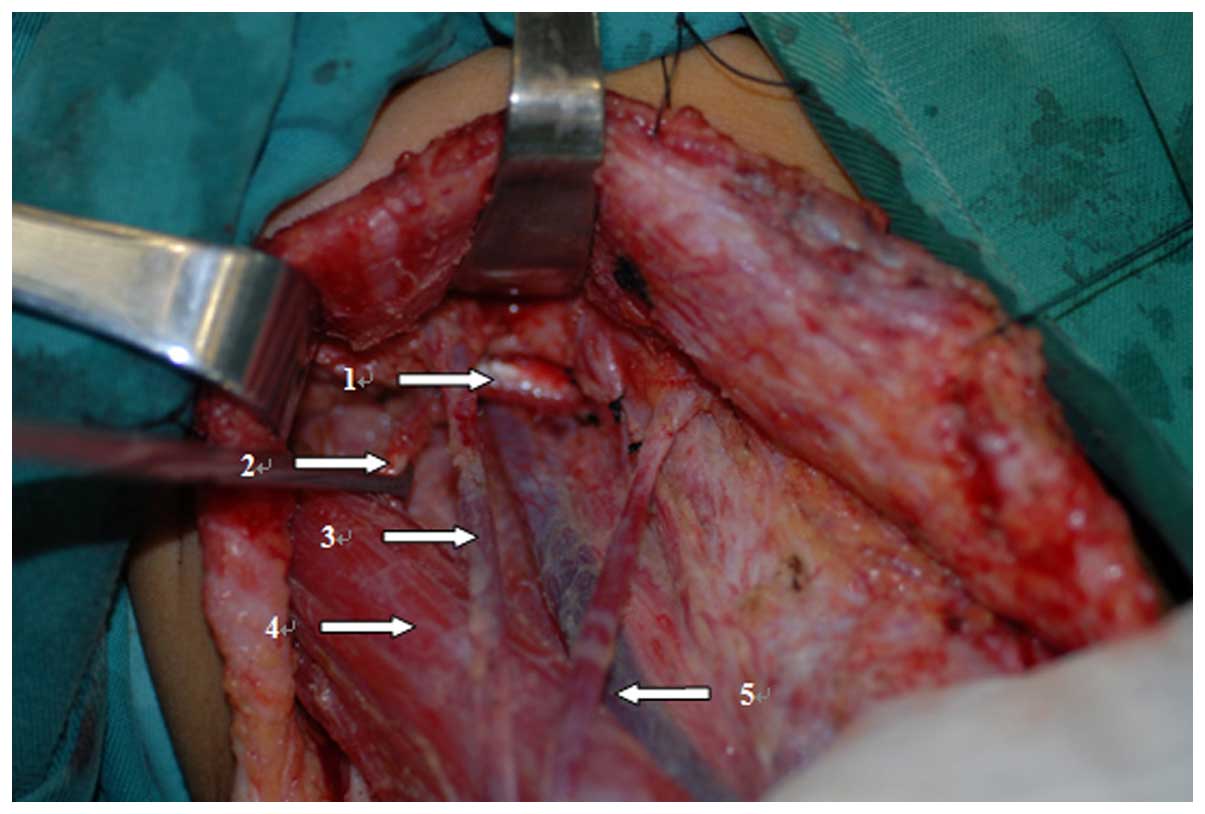
While performing cervical low incision, a
supracervical arc incision on the lesion side was first executed
(usually 2 cm above the collarbone) (Fig.
1). The posterior edge of this incision reached the anterior
edge of the trapezius muscle so that the incision could extend to
provide a good exposure subsequent to the creation of the flap. For
the patients with a long neck, sometimes the incision is lengthened
a little backwards. Subsequently, the sternocleidomastoid, vena
jugularis interna and vena jugularis externa were dissociated to
protect the auricular nerve, and the lymph nodes along the vena
jugularis interna were dissected (Fig.
2). Following this, the neck dissection was performed and the
nerve at cervical levels II and III was dissociated. Finally, all
branches of the cutaneous nerve were dissociated and preserved from
the top to bottom. The range of neck dissection was levels II–VI.
The commonly employed classic ‘L’ incision for thyroid cancer is a
continuation of a Kocher incision along the posterior border of the
sternocleidomastoid muscle superiorly to approximately 1 inch below
the ipsilateral ear lobe (4). These
procedures were performed as described previously (4). The range of conventional neck dissection
was II–VI level lymph nodes and provided good exposure.
Follow-up
All the patients were followed up to 31–60 months,
with an average of 41 months. The tumor extent was defined
according to the 7th edition of the American Joint Committee on
cancer (AJCC) tumor-node-metastasis (TNM) classification of
malignant tumors in 2010. Quantitative data are expressed as the
mean ± standard deviation; qualitative data are expressed as
percentages. P<0.05 was considered to indicate a statistically
significant difference.
Results
Patient demographics and types of
surgery
Patient demographics are shown in Table I. Table
II lists the types of surgical procedures. Among the 87
patients, 3 had partial thyroidectomy in local hospitals; however,
postoperation pathology confirmed these cases as papillary thyroid
cancer. The other 84 patients received their initial treatment at
Zhejiang Cancer Hospital. Intraoperative frozen pathology confirmed
those cases as thyroid papillary carcinoma. More specifically, 5 of
the 84 initial treatment patients were found to have enlarged
cervical lymph node or metastatic lymph node by preoperative fine
needle aspiration. A total of 47 cases of patients, including 11
males (23.4%) and 36 females (76.6%), were treated by the cervical
low incision and 40 cases, including 10 males (25.0%) and 30
females (75.0%), were treated by the classic ‘L’ incision.
According to the 2002 AJCC staging of thyroid papillary carcinoma,
22 cases were T1N0M0. A total of
60 cases were T1N1M0 and 5 were
T1N2M0. In the cervical low
incision group, 9 patients (19.1%) were at
T1N0M0 stage, 35 (74.5%) were
T1N1M0 and 3 (6.4%) were
T1N2M0. In the classic ‘L’
incision group, 13 patients (32.5%) were at
T1N0M0 stage, 25 (62.5%) were
T1N1M0 and 2 (5.0%) were
T1N2M0 (Table I). Among the 87 patients, 4 exhibited
bilateral papillary thyroid carcinoma (implemented bilateral neck
dissection) and 83 had unilateral papillary thyroid cancer.
Bilateral dissection was performed in 2 cases (4.3%) of the
cervical low incision group and in 2 cases (5%) of the classic ‘L’
incision group. Additionally, unilateral dissection was performed
in 45 cases (95.7%) of the cervical low incision group and in 38
cases (95.0%) of the classic ‘L’ incision group (Table II).
 | Table I.Patient demographics. |
Table I.
Patient demographics.
| Demographics | Total no. of cases
(n=87) | Cervical low incision
(n=47) | Classic ‘L’ incision
(n=40) |
|---|
| Male, n (%) | 21 (24.1) | 11 (23.4) | 10 (25.0) |
| Female, n (%) | 66 (75.9) | 36 (76.6) | 30 (75.0) |
| Mean age, years
(range) | 35
(12–67) | 36
(12–67) | 33
(12–65) |
|
T1N0M0, n
(%) | 22 (25.3) | 9
(19.1) | 13 (32.5) |
|
T1N1M0, n
(%) | 60 (69.0) | 35 (74.5) | 25 (62.5) |
|
T1N2M0, n
(%) | 5 (5.7) | 3 (6.4) | 2 (5.0) |
 | Table II.Types of surgery. |
Table II.
Types of surgery.
| Surgery | Total no. of cases
(%) | Cervical low
incision | Classic ‘L’
incision |
|---|
| Total
thyroidectomy | 87 | 47 | 40 |
| Unilateral
dissection | 83 (95.4) | 45 (95.7) | 38 (95.0) |
| Bilateral
dissection | 4 (4.6) | 2 (4.3) | 2 (5.0) |
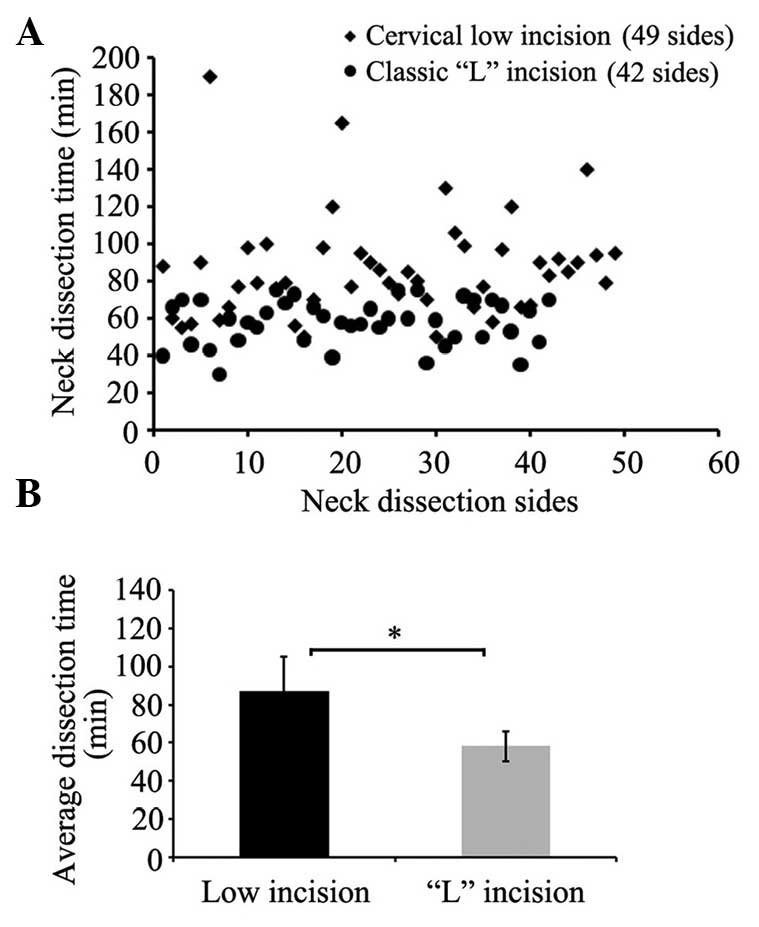
Lateral neck dissection time
The surgical time ranged from 50–190 min in the
cervical low incision group and 30–75 min in the classic ‘L’
incision group, with an average of 87 and 58 min, respectively.
(P<0.05) (Fig. 3A and B). The
dissection time of the cervical low incision group was longer than
that of the classic ‘L’ incision group.
Lymph node number during neck
dissection
For the cervical low incision group there were 16 to
49 lymph nodes on each side and 18 to 50 lymph nodes for the
classic ‘L’ incision group. For the former, the average total
amount and the region II lymph nodes of the unilateral neck
dissection were 33 and 10, and for the latter they were 35 and 11,
respectively (P>0.05) (Fig. 4A and
B). In total, cervical lymph node metastasis was pathologically
confirmed in 35 patients (37 sides) of the cervical low incision
group and 30 (32 sides) in the classic ‘L’ incision group. On
average, 4.8 and 4.2 metastasis nodes were identified on each side
for the two groups, respectively (Table
III).
 | Table III.Cervical lymph node metastasis. |
Table III.
Cervical lymph node metastasis.
| Variables | Total | Cervical low
incision | Classic ‘L’
incision |
|---|
| Cases, n | 87 | 47 | 40 |
| Dissection sides,
n | 91 | 49 | 42 |
| Cases with lymph node
metastasis, n (%) | 65 (74.7) | 35 (74.5) | 30 (75.0) |
| Dissection sides with
lymph node metastasis, n (%) | 69 (75.8) | 37 (75.5) | 32 (76.2) |
| Metastasis node on
each side, n | 4.8 | 4.2 | 0.6 |
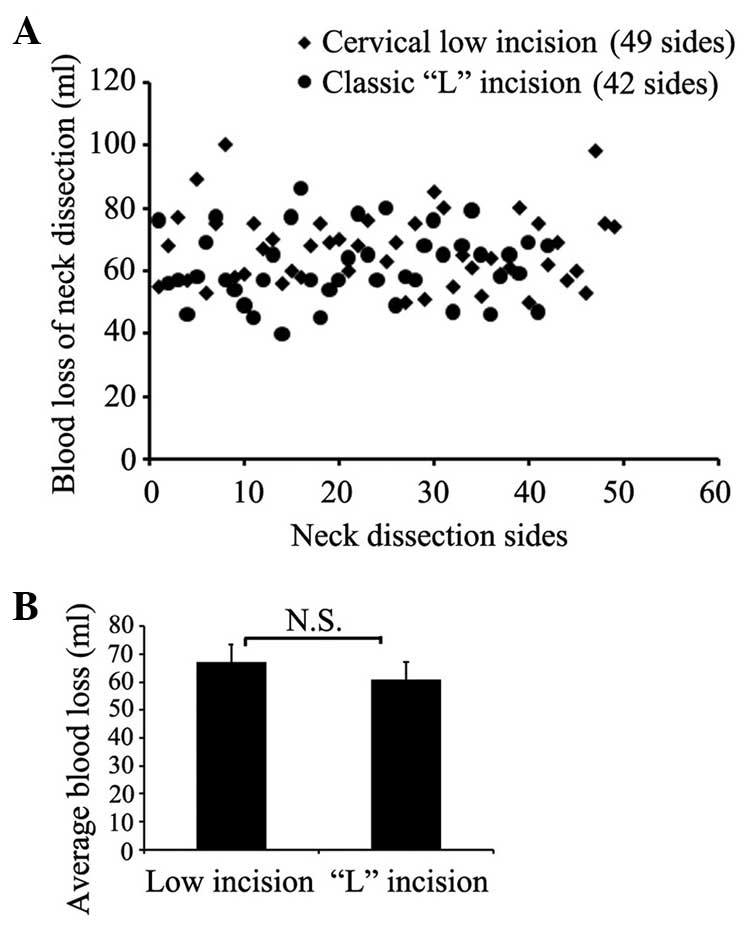
Blood loss during neck dissection
Blood loss in the cervical low incision group was
50–100 ml on each side with an average of 67 ml, while for the
classic ‘L’ incision group it was 40–80 ml with an average of 61 ml
(P>0.05) (Fig. 5A and B).
Complication ratings
No fatalities were recorded. Two patients with
cervical low incision had postoperative lymphatic fistula. However,
following pressure dressing, fasting and other treatments, this
complication was healed. However, incision separations were
identified in 3 patients with the classic ‘L’ incision (Fig. 6).
One week after the surgery, all the patients were
tested for their dermal sensations of the surgical region by
acupuncture. Their dermal sensation function was staged. Among the
49 sides (47 cases in the cervical low incision group), 46 sides
exhibited good dermal sensation, and the other 3 sides had no
sensation at all. Among all the patients with cervical low
incision, the surgical sides of 45 patients who received unilateral
neck dissection were tested for dermal sensation with respect to
their contralateral normal skin. Among these 45 cases, 21 patients
reported that the bilateral symmetry of cervical dermal sensations
was similar, while the postoperative sides of 22 patients were
slightly lower compared to the normal side, however, pains and
tactual sensation were reported. The remaining 2 patients had no
feeling on the postoperative sides. One patient in these 2 cases
who underwent the bilateral neck dissection had no pain and tactual
sensation on 1 side (Table IV).
However, among the 42 sides (40 cases in the classic ‘L’ group),
all the sides nearly lost the feeling below the ear lobe and had
persistent numbness of the ear lobe.
 | Table IV.Complication ratings. |
Table IV.
Complication ratings.
|
| Cervical low
incision | Classic ‘L’
incision |
|---|
|
|
|
|
|---|
| Variables | Total no. (%) | Unilateral | Bilateral | Total no. (%) | Unilateral | Bilateral |
|---|
| Neck dissection
cases, n | 47 | 45 | 2 | 40 | 38 | 2 |
| Good dermal
sensation, n (%) | 22 (46.8) | 21 (44.7) | 1 (2.1) | 0 | 0 | 0 |
| Slightly weak
sensation, n (%) | 22 (46.8) | 22 (46.8) | 0 | 0 | 0 | 0 |
| No dermal sensation,
n (%) | 3 (6.4) | 2 (4.3) | 1 (2.1) | 40
(100.0) | 38 (95.5) | 2 (5.0) |
| Persistent neck pain,
n (%) | 4 (8.5) | 4 (8.5) | 0 | 11 (27.5) | 10 (25.0) | 1 (2.5) |
| Postoperative
recurrence, n (%) | 2 (4.3) | 1 (2.1) | 1 (2.1) | 1 (2.5) | 1 (2.5) | 0 |
In addition, 4 of the 47 patients in the cervical
low incision group had a persistent neck pain. However, this pain
was tolerated and disappeared within 2 to 3 months after the
surgery. There were 2 cases of cervical lymph node postoperative
recurrence, 1 in the middle neck region (III area), and the other
in the lower neck region (IV area). In the 2 cases, the cervical
lymph nodes were excised. In total, 11 of the 40 patients in the
classic ‘L’ incision group underwent a long and persistent neck
pain, for almost 3 months (Table
IV), resulting from the destruction of the fiber connection of
the skin surface at the longitudinal incision and the large tension
in the late healing process, which caused delayed healing (Fig. 6). There was 1 case of cervical lymph
node postoperative recurrence in the IV area.
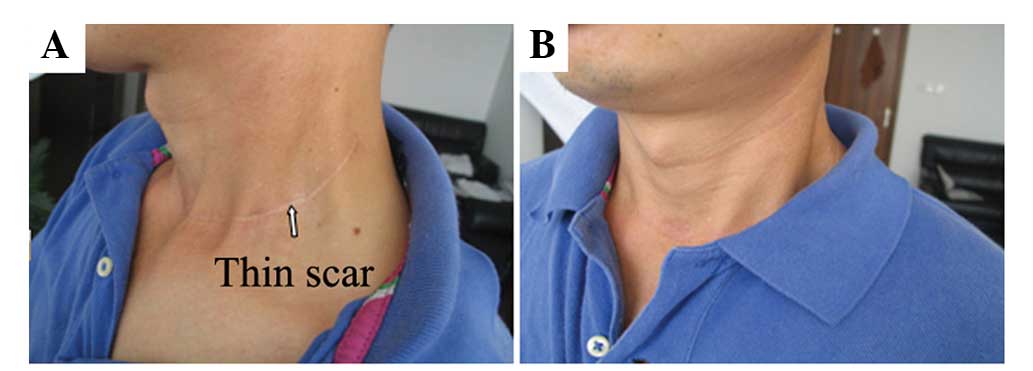
Postoperative satisfaction
ratings
The neck scars of 43 patients (out of 47) in the
cervical low incision group were not evident, as there was only a
thin line on the lower neck (Fig.
7A). The other 4 patients had visible red scars, which were
significant granulation tissues. However, the scars were located in
the lower regions so that they could be covered (Fig. 7B). As the scars were lower than usual
and could be covered by a collar, 25 patients reported satisfaction
with this surgery. A total of 19 patients were primarily satisfied
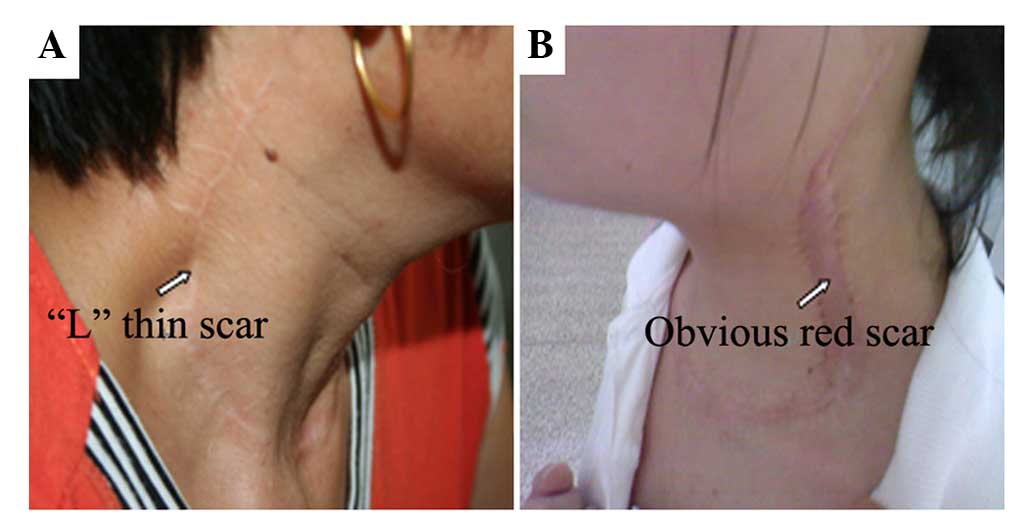
and only 3 patients were dissatisfied (Table V). However, the neck scars of almost
all the patients in the classic ‘L’ incision group were evident.
The neck scars of 21 patients were an ‘L’ thin line extending from
the lower neck to the ear (Fig. 8A),
while the other 19 patients had clear red scars or granulations
(Fig. 8B). However, as the scars were
located in the exposed regions and could not be covered by a
collar, 27 patients expressed dissatisfaction with this surgery. A
total of 9 patients were primarily satisfied and only 4 were
satisfied (Table V).
 | Table V.Postoperative satisfaction
ratings. |
Table V.
Postoperative satisfaction
ratings.
| Variables | Cervical low
incision, n (%) (n=47) | Classic ‘L’ incision,
n (%) (n=40) |
|---|
| Evident neck
scars | 4 (8.5) | 40
(100.0) |
| No evident neck
scars | 43 (91.5) | 0 (0.0) |
| Satisfied | 25 (53.2) | 4
(10.0) |
| Basically
satisfied | 19 (40.4) | 9
(22.5) |
| Dissatisfied | 3 (6.4) | 27 (67.5) |
Discussion
The techniques of neck dissections have evolved from
the radical neck dissection to present modified neck dissection,
which reserves the sternocleidomastoid, vena jugularis interna and
accessory nerve. The conventional ‘L’-shaped incision has clear
scars, particularly for the vertical section, which caused patient
dissatisfaction regarding their appearance. The focus is currently
on improving the patient quality of life. The modified neck
dissection also has disadvantages. It requires the removal of the
superclavicular and auricular nerves, and causes an inevitable
result of loss of feeling below the ear lobe, including numbness,
causing issues with patients, particularly for certain young
patients. As thyroid papillary carcinoma has a favorable prognosis,
maximizing the life quality of patients is important. Therefore,
the low neck incision was applied to complete the neck dissection.
Furthermore, the supracervical epithelial nerve, jugular vein and
auricular nerve were conserved to reduce the impact of surgery on
patients. This technique received satisfactory feedback.
Due to its good exposure, the conventional
‘L’-shaped incision is accepted by the majority of surgeons.
However, in the postoperative follow-up, due to the evident
vertical section of the scar tissue, numerous patients expressed
dissatisfaction. Therefore, the incision was first modified to be
parallel to the neck dermatoglyph and ≥2 cm above the clavicle,
making it a transverse incision that can cause a satisfactory
appearance (Fig. 9A and B). In the
follow-up of the 47 patients in the cervical low incision group,
only 4 had an incision of granulation tissue hyperplasia with
evident scars. The scars of the remaining 43 cases were
inconspicuous. All these patients could cover their neck scars by
their clothes (Fig. 7B). According to
the relevant literature, Uchino et al (6) termed this an extended collar incision,
Shah (7) defined it as the single
transverse incision, Xi et al (8) termed it the long low collar incision and
Zhang et al (9) termed it
extending collar incision. These studies all agree that the
incision scars are not evident and have less impact on the
appearance.
With regards to the cleaning range, the range of
conventional neck dissection was level II–VI lymph nodes and
provided good exposure. At the beginning of the study, cervical low
incision was not thought to provide as good an exposure to levels
II and III as the conventional dissection. Therefore, it may
obscure a thorough lymph dissection. However, in the present
surgery, levels III and IV were well exposed. The exposure of level
II was slightly worse compared to the conventional incision.
However, once a full free flap was separated, an extremely good
exposure to level II, as well as to level IIb, lymph nodes was
obtained (Fig. 10). Therefore, the
scope of the neck dissection was the same as the conventional neck
dissection. When a patient required level I dissection, the surgery
was more difficult due to the cervical low incision only.
Therefore, in these types of cases, an auxiliary transverse neck
incision (or MACFEE incision) is required to provide enough
exposure. However, in the majority of papillary thyroid cancer
cases, no exposure of level I is required, and the low incision can
well replace the conventional neck dissection. Those patients, who
have large cervical lymph nodes and dense adhesions following
radiotherapy, may require conventional incision.
The patients who received routine lymph dissection
always reported neck numbness or loss of the ability to feel pain
around the ear lobe. Certain patients cannot sense when the skin of
their neck is burned in that area. The loss of sensory function is
due to the removal of the supracervical epithelial nerve and
auricular nerve. For this reason, the neck dissection was modified
by reserving the supracervical epithelial nerve and auricular nerve
in addition to the conventional methods, which only reserves the
sternocleidomastoid, vena jugularis interna and accessory nerve.
This modification was successful (Fig.
2). Among the 49 sides (47 patients), 46 sides of the neck felt
tactile pain. The preservation of sensory function was good.
Postoperative sensory function of the neck was satisfactory. In
theory, if the supracervical epithelial nerve and auricular nerve
are retained, the patient should have a sensory function on the
neck. However, there remain three sides of that neck that do not
feel tactile pain, and 4 patients had severe neck pain. This may be
due to nerve degeneration caused by the electric knife during skin
flap separation. Therefore, how to preserve the nerve as well as
its function requires further research. As for the surgery, based
on the present experience, the neck has only to be exposed to two
to three nerve roots to dissect level II and III lymph nodes from
top to bottom and from the nerve cord to supracervical epithelial
nerve branches. This feature makes the surgery less time consuming
and more convenient.
Certain doctors are concerned that reserving so many
normal structures may affect the outcome of neck dissection.
However, the present results show that only 2 patients had cervical
lymph node recurrence, which was only 4% of the sample. Those
recurrences of lymph nodes were located in the lower neck, but not
the poor exposure region (level II lymph nodes) of low incision.
Therefore, we believe that good skill and full free skin flap can
provide a good exposure, as well as the ‘L’-shaped incision.
Therefore, the effect of the cervical low incision neck dissection
for ‘eight reserved’ (vena jugularis interna, vena jugularis
externa, sternocleidomastoid, accessory nerve, superclavicular
nerve, transverse cervical artery, musculus omohyoideus and
auricular nerve) is not an issue. However, the long-term effect
requires further follow-ups.
The reservation of vena jugularis externa can
significantly reduce facial edema, while the omohyoid muscle is
believed to have limited function. We believe that at the initial
stage of treatment, these two can be sacrificed.
Due to poor exposure and fine dissection to retain a
variety of normal tissues, ‘eight reserved’ cervical low incision
neck dissection requires more surgical time compared to the
conventional modified neck dissection.
Among the 47 cases in the cervical low incision
group analyzed, only 2 had postoperative lymphatic fistula. No
other complications were reported, indicating that the low incision
neck dissection and ‘eight reserved’ did not increase the
complications and were safe for patients. However, as low incision
requires an upward pull flap to expose the surgical field, the
surgery may cause tissue edema. However, it can be recovered
quickly.
In conclusion, as living standards are improving,
patients expect doctors to guarantee their qualities of life
following surgery. The cervical low incision neck dissection for
‘eight reserved’ has only a hidden incision compared to the
conventional method. Additionally, the scar tissue is not evident
and the neck preserves sensation. These advantages meet the
expectations of the patient. By contrast, it does not increase the
suffering of patients and postoperative complications, since it
conforms to eliminate the cervical lymph node and spare normal
tissue requirements. Therefore, in the treatment of thyroid
papillary carcinoma, low incision neck dissection for ‘eight
reserved’ may replace the conventional modified neck
dissection.
Acknowledgements
The present study was supported by the National 863
Fundamental Research Project (grant no. 2014AA02240), the National
Natural Science Foundation of China (grant nos. 81550033 and
81202127), the Zhejiang Provincial Program for the Cultivation of
High-Level Innovative Health Talents (grant no. 2008-134), and the
Zhejiang Medical and Health Science and Technology Plan (grant nos.
2012KYA031, 2013KYB033, 2013KYB042 and 2014KYB038).
References
|
1
|
Shaha AR, Shah JP and Lorre TR: Patterns
of nodal and distant metastasis based on histologic varities in
differentiated carcinoma of thyroid. Am J Surg. 172:692–694. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Pisello F, Geraci G, Lo Nigro C, Li Volsi
F, Modica G and Sciumè C: Neck node dissection in thyroid cancer. A
review. G Chir. 31:112–118. 2010.PubMed/NCBI
|
|
3
|
Palestini N, Borasi A, Cestino L, Freddi
M, Odasso C and Robecchi A: Is central neck dissection a safe
procedure in the treatment of papillary thyroid cancer? Our
experience. Langenbecks Arch Surg. 393:693–698. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Daniel O and Robert U: Surgery of the
thyroid and parathyroid glands. Berlin: Springer-Verlag. 101–106.
2007.
|
|
5
|
Xue S, Wang P and Chen G: Neck dissection
with cervical sensory preservation in thyroid cancer. Gland
Surgery. 2:212–218. 2013.PubMed/NCBI
|
|
6
|
Uchino S, Noguchi S, Yamashita H and
Watanabe S: Modified radical neck dissection for differentiated
thyroid cancer: Operative technique. World J Surg. 28:1199–2203.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Shah JP, Patel SG and Singh B: Head and
neck surgery and oncology. Han DM, Yu ZK, translation
(Philadelphia). Elsevier Mosby. 4952005.
|
|
8
|
Xi ZH, Wang QZ, Lu XB, et al: Long low
collar incision in differentiated thyroid cancer radical surgery.
Journal of Henan Medical University. 37:426–427. 2002.
|
|
9
|
Zhang B, Yan DG, An CM, et al: Application
of an extended collar incision in neck dissection for
differentiated thyroid cancer. Chin J Oncol. 31:223–225. 2009.
|