|
1
|
Smith I and Chua S: Medical treatment of
early breast cancer. IV: Neoadjuvant treatment. BMJ. 332:223–224.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Bria E, Nistico C, Cuppone F, Carlini P,
Ciccarese M, Milella M, Natoli G, Terzoli E, Cognetti F and
Giannarelli D: Benefit of taxanes as adjuvant chemotherapy for
early breast cancer: Pooled analysis of 15,500 patients. Cancer.
106:2337–2344. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Buzdar AU, Singletary SE, Valero V, Booser
DJ, Ibrahim NK, Rahman Z, Theriault RL, Walters R, Rivera E, Smith
TL, et al: Evaluation of paclitaxel in adjuvant chemotherapy for
patients with operable breast cancer: Preliminary data of a
prospective randomized trial. Clin Cancer Res. 8:1073–1079.
2002.PubMed/NCBI
|
|
4
|
O'Shaughnessy J, Miles D, Vukelja S,
Moiseyenko V, Ayoub JP, Cervantes G, Fumoleau P, Jones S, Lui WY,
Mauriac L, et al: Superior survival with capecitabine plus
docetaxel combination therapy in anthracycline-pretreated patients
with advanced breast cancer: Phase III trial results. J Clin Oncol.
20:2812–2823. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Albain KS, Nag SM, Calderillo-Ruiz G,
Jordaan JP, Llombart AC, Pluzanska A, Rolski J, Melemed AS,
Reyes-Vidal JM, Sekhon JS, et al: Gemcitabine plus paclitaxel
versus paclitaxel monotherapy in patients with metastatic breast
cancer and prior anthracycline treatment. J Clin Oncol.
26:3950–3957. 2009. View Article : Google Scholar
|
|
6
|
Nielsen DL, Bjerre KC, Jakobsen EH, Cold
S, Stenbygaard L, Sørensen PG, Kamby C, Møller S, Jørgensen CLT and
Andersson M: Gemcitabine plus docetaxel versus docetaxel in
patients with predominantly human epidermal growth factor receptor
2-negative locally advanced or metastatic breast cancer: A
randomized, phase III study by the Danish Breast Cancer Cooperative
Group. J Clin Oncol. 29:4748–4754. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Miller K, Wang M, Gralow J, Dickler M,
Cobleigh M, Perez EA, Shenkier T, Cella D and Davidson NE:
Paclitaxel plus bevacizumab versus paclitaxel alone for metastatic
breast cancer. N Engl J Med. 357:2666–2676. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Brufsky AM, Hurvitz S, Perez E, Swamy R,
Valero V, O'Neill V and Rugo HS: RIBBON-2: A randomized,
double-blind, placebo-controlled, phase III trial evaluating the
efficacy and safety of bevacizumab in combination with chemotherapy
for second-line treatment of human epidermal growth factor receptor
2-negative metastatic breast cancer. J Clin Oncol. 29:4286–4293.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Robert NJ, Diéras V, Glaspy J, Brufsky AM,
Bondarenko I, Lipatov ON, Perez EA, Yardley DA, Chan SY, Zhou X, et
al: RIBBON-1: Randomized, double-blind, placebo-controlled, phase
III trial of chemotherapy with or without bevacizumab for
first-line treatment of human epidermal growth factor receptor
2-negative, locally recurrent or metastatic breast cancer. J Clin
Oncol. 29:1252–1260. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Cortes J, O'Shaughnessy J, Loesch D, Blum
JL, Vahdat LT, Petrakova K, Chollet P, Manikas A, Diéras V,
Delozier T, et al: Eribulin monotherapy versus treatment of
physician's choice in patients with metastatic breast cancer
(EMBRACE): A phase 3 open-label randomised study. Lancet.
377:914–923. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
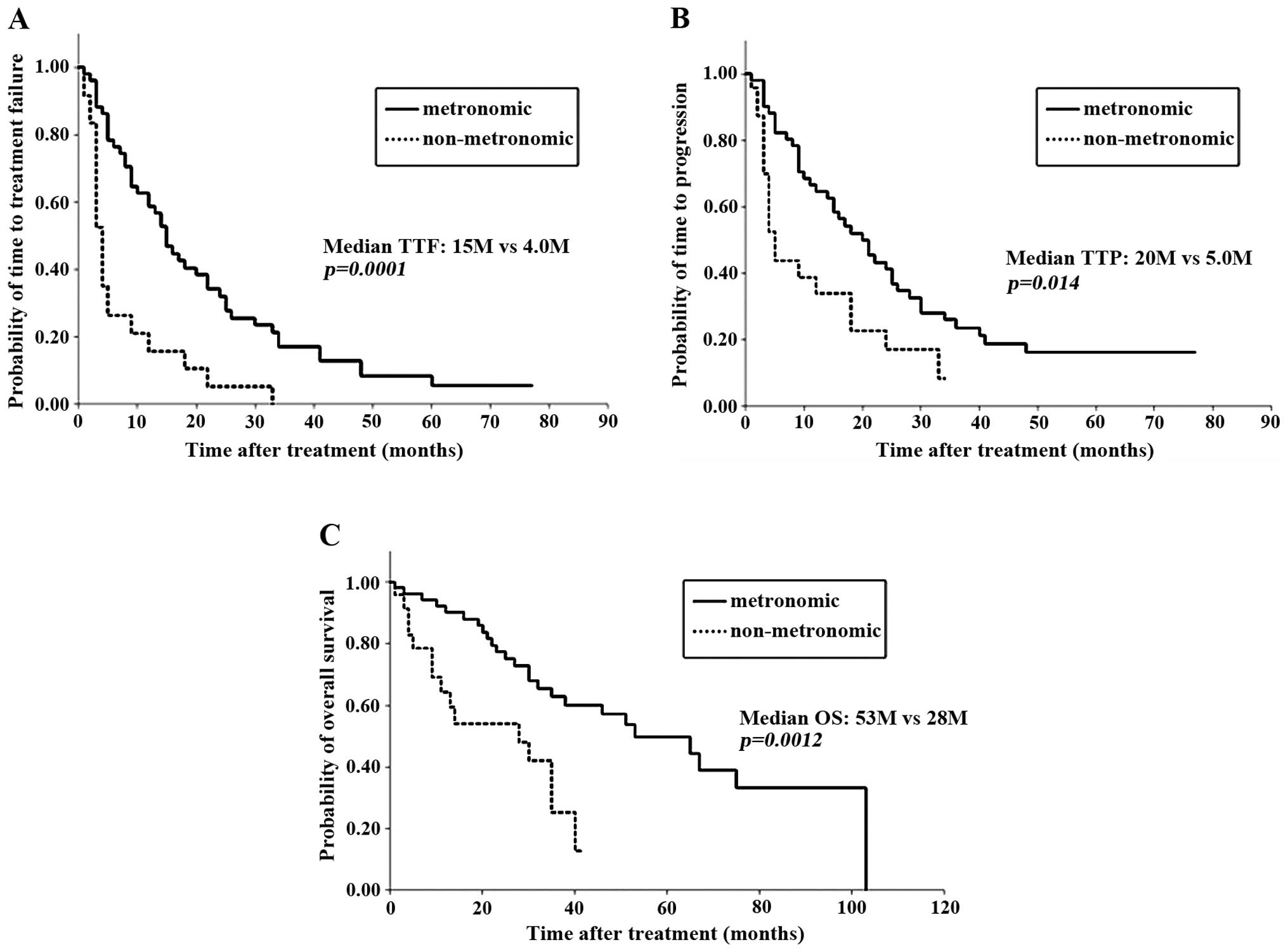
Kontani K, Hashimoto SI, Murazawa C,
Norimura S, Tanaka H, Ohtani M, Fujiwara-Honjo N, Date M, Houchi H
and Yokomise H: Metronomic chemotherapy for metastatic breast
cancer to prolong time to treatment failure to 12 months or more.
Mol Clin Oncol. 1:225–230. 2013.PubMed/NCBI
|
|
12
|
Kontani K, Hashimoto S, Murazawa C,
Norimura S, Tanaka H, Ohtani M, Fujiwara-Honjo N, Date M, Teramoto
K, Houchi H and Yokomise H: Factors responsible for long-term
survival in metastatic breast cancer. World J Surg Oncol.
12:3442014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Oostendorp LJ, Stalmeier PF, Donders AR,
van der Graaf WT and Ottevanger PB: Efficacy and safety of
palliative chemotherapy for patients with advanced breast cancer
pretreated with anthracyclines and taxanes: A systematic review.
Lancet Oncol. 12:1053–1061. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kerbel RS and Kamen BA: The
anti-angiogenic basis of metronomic chemotherapy. Nat Rev Cancer.
4:423–436. 2004. View
Article : Google Scholar : PubMed/NCBI
|
|
15
|
Colleoni M, Rocca A, Sandri MT, Zorzino L,
Masci G, Nolè F, Peruzzotti G, Robertson C, Orlando L, Cinieri S,
et al: Low-dose oral methotrexate and cyclophosphamide in
metastatic breast cancer: Antitumor activity and correlation with
vascular endothelial growth factor levels. Ann Oncol. 13:73–80.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Colleoni M, Orlando L, Sanna G, Rocca A,
Maisonneuve P, Peruzzotti G, Ghisini R, Sandri MT, Zorzino L, Nolè
F, et al: Metronomic low-dose oral cyclophosphamide and
methotrexate plus or minus thalidomide in metastatic breast cancer:
Antitumor activity and biological effects. Ann Oncol. 17:232–238.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Wong NS, Buckman RA, Clemons M, Verma S,
Dent S, Trudeau ME, Roche K, Ebos J, Kerbel R, Deboer GE, et al:
Phase I/II trial of metronomic chemotherapy with daily dalteparin
and cyclophosphamide, twice-weekly methotrexate, and daily
prednisone as therapy for metastatic breast cancer using vascular
endothelial growth factor and soluble vascular endothelial growth
factor receptor levels as markers of response. J Clin Oncol.
28:723–730. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Eisenhauer EA, Therasse P, Bogaerts J,
Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S,
Mooney M, et al: New response evaluation criteria in solid tumors:
revised RECIST guideline (version 1.1). Eur J Cancer. 45:228–247.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
US Department of Health and Human
Services. Common Terminology Criteria for Adverse Events (CTCAE).
version 4.0. http://evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03_2010-06-14_QuickReference_8.5x11.pdfAccessed.
January 14–2014
|
|
20
|
Jassem J, Pieńkowski T, Płuzańska A, Jelic
S, Gorbunova V, Mrsic-Krmpotic Z, Berzins J, Nagykalnai T, Wigler
N, Renard J, et al: Doxorubicin and paclitaxel versus fluorouracil,
doxorubicin, and cyclophosphamide as first-line therapy for women
with metastatic breast cancer: Final results of a randomized phase
III multicenter trial. J Clin Oncol. 19:1707–1715. 2001.PubMed/NCBI
|
|
21
|
Bonneterre J, Dieras V, Tubiana-Hulin M,
Bougnoux P, Bonneterre ME, Delozier T, Mayer F, Culine S, Dohoulou
N and Bendahmane B: Phase II multicentre randomised study of
docetaxel plus epirubicin vs 5-fluorouracil plus epirubicin and
cyclophosphamide in metastatic breast cancer. Br J Cancer.
91:1466–1471. 2004.PubMed/NCBI
|
|
22
|
Sledge GW, Neuberg D, Bernardo P, Ingle
JN, Martino S, Rowinsky EK and Wood WC: Phase III trial of
doxorubicin, paclitaxel and the combination of doxorubicin and
paclitaxel as front-line chemotherapy for metastatic breast cancer:
An intergroup trial (E1193). J Clin Oncol. 21:588–592. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Paridaens R, Biganzoli L, Bruning P, Klijn
JG, Gamucci T, Houston S, Coleman R, Schachter J, Van Vreckem A,
Sylvester R, et al: Paclitaxel versus doxorubicin as first-line
single-agent chemotherapy for metastatic breast cancer: A European
Organization for Research and Treatment of Cancer Randomized Study
with cross-over. J Clin Oncol. 18:724–733. 2000.PubMed/NCBI
|