Introduction
Prostate sarcoma is a rare type of carcinoma, which
originated from the interstitial tissue of the prostate. The
predominant symptom is frequent urination, dysuria and hematuria.
Its etiology remains unknown. The common pathological
classification involved rhabdomyosarcoma, leiomyosarcoma, and
fibrosarcoma. This disease normally occurs in middle-aged patients.
Prostate sarcoma always has a poor prognosis and it accounts for
~0.1% of all prostate cancer cases (1). It is reported that a quarter of patients
already exhibit a metastatic mass at the time of diagnosis.
Markowski et al (2) reported
that the median overall survival time of prostate sarcoma is 9
months in patients with bladder invasion and 7.1 months in patients
with metastatic disease. The present study reported a successful
case of surgical management for prostate leiomyosarcoma during 1995
until 2015, with post-operative follow-up for 20 years. The present
study also aimed to perform a literature review, in order to
correctly diagnose patients, and thus establish an effective
treatment plan both individually and collectively.
Case report
A 58-year-old male presented with frequent
micturition and dysuria since 1995, which went without any
treatment until the persistent hematuria appearance for 4 days
prior to hospitalization. The symptoms were becoming progressively
worse the past few days. The patient was a smoker and drank alcohol
socially. No genitourinary cancer history existed in his family.
Rectal examination revealed a significant nodule around the area of
the prostate, ~4–5 cm in diameter. The laboratory examination
revealed that at presentation, the acid phosphatase (ACP) was 1.6
U/l and prostate specific antigen (PSA) was 4.6 µg/l. The
ultrasound guided transrectal prostatic biopsy confirmed the
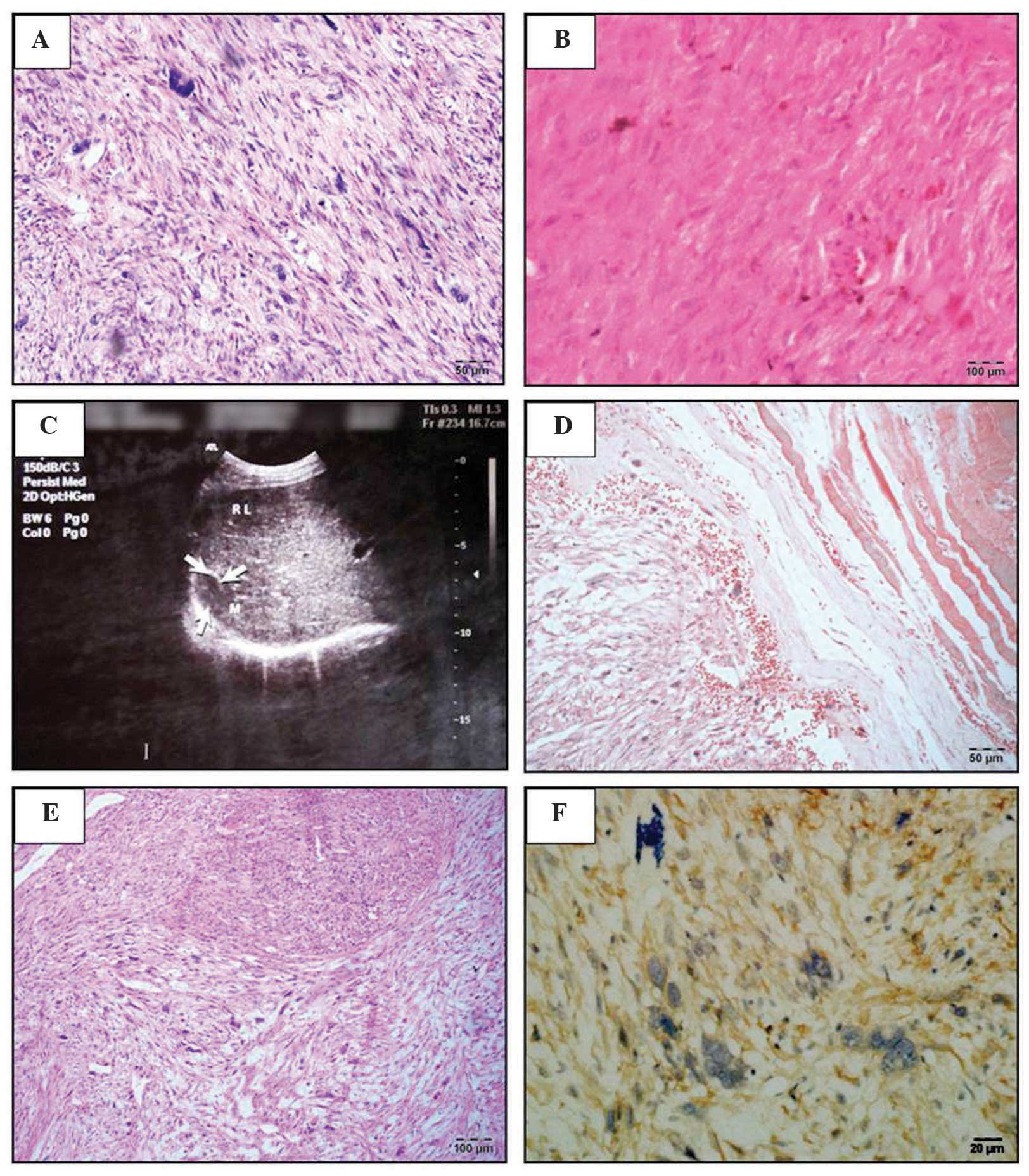
histological type was prostate sarcoma (Fig. 1A). As a result, the patient received
the radical prostatectomy in April 1995. Following the surgery, the
hematuria and dysuria disappeared. The post-operative pathological
diagnosis was prostate leiomyosarcoma (Fig. 1B). At the 2 year follow-up, the
hematuria was observed again, and increased pain was exhibited at
the hypogastrium. A B-ultrasound examination of the abdomen
revealed a slight nodule (~1.8 cm in diameter) in the centre of the
prostate (Fig. 1C). A chest x-ray and
emission computed tomography (ECT) examination revealed no
metastatic masses. The present study considered this as recurrent
prostate sarcoma, and as a result, radical prostatectomy, radical
cystectomy and reconstruction of the bladder with ileum were
performed. After 1 year, the patient found a hard mass (~3.3 cm in
diameter) on the right side of the back, without any clinical
symptoms. A chest x-ray and B-ultrasound revealed that the mass as
a metastatic carcinoma from the prostate. An ECT whole-body bone
scan revealed a striking concentration of radioactivity in the
right ninth rib. The patient received partial rib resection of the
right ninth rib. The post-operative pathological diagnosis was
leiomyosarcoma of the right chest wall (Fig. 1D and E). At the 10 month follow-up, a
new mass was revealed at the operative site. The patient had to
receive a secondary operation of the right ninth rib.
Immunohistochemical results revealed the following: αAT (−), Actin
(+), Vimentin (±), CK (−) and S100 (++) (Fig. 1F). To date, with 17 years of
follow-ups, the patient has exhibited no recurrence.
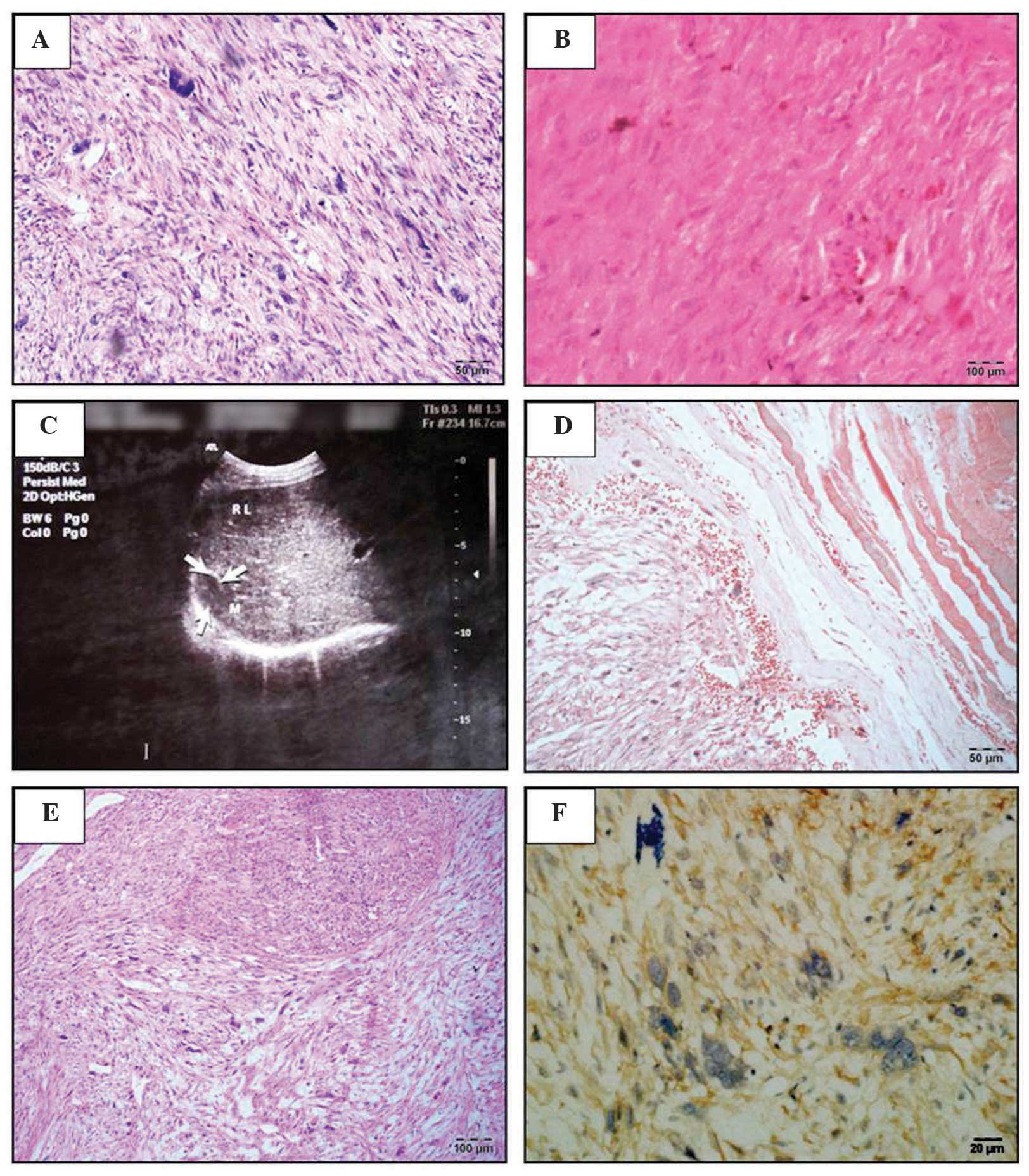 | Figure 1.Assessment of the biopsy samples at
various stages. (A) The first prostate biopsy slice, stained with
H&E, revealed tumor cells were predominantly spindle-shaped,
the cytoplasm was dyed in red, nuclei were rod-shaped and rounded
at each end. The majority of the tumor cells were with mild to
moderate atypia and occasionally giant tumor cells were visible
(magnification, ×20). (B) A biopsy slice of the first recurrence
tumor, stained with H&E, revealed that tumor cells were in long
spindle-shaped or oval and arranged in a palisade. Significant
cellular atypia was observed and the cytoplasm was dyed in bright
red. Mitotic cells were easily detected and a section of the tumor
cell exhibited large nuclei, and interstitial was more loose
(magnification, ×20). (C) The right bib metastatic cancer observed
by the abdominal B-ultrasound results (a solid mass ~2.2×1.7 cm) in
the capsule between diaphragm and liver. (D) A biopsy slice of the
first resection of the rib metastases, stained with Masson-Goldnen
trichrome, revealed red tumor cells were red (magnification, ×20).
(E) A biopsy slice of the first resection of the rib metastases,
stained with H&E (magnification, ×10). (F) A biopsy slice of
the second resection of rib metastases, stained with actin antibody
(magnification, ×40). |
Discussion and literature review
Sarcoma of the prostate is a rare malignant
carcinoma of genitourinary cancer. According to different
histological types, it can be divided into prostate leiomyosarcoma,
rhabdomyosarcoma, fibrosarcoma and spindle cell sarcoma (3). The anatomic structure of prostate
leiomyosarcoma was the mesenchymal tissue in the prostate smooth
muscle. The development is rapid and as early as the time to reveal
a metastatic mass. This disease accounts for ~0.1% of all prostate
cancer cases and it normally occurs in patients aged between 40 and
78-year-old (1). Clinical symptoms
are not normally significant. The majority of the symptoms revealed
only mild to moderate urinary tract obstructive symptoms, including
frequent urination, urine urgency, voiding difficulty, hematuria
and perineal pain. No significant abnormal changes were observed in
the prostatic physical examination, and the prostate volume and
serum PSA levels remain in the normal range (4), whereas the imaging examination,
including B-type ultrasound can often be reveal the early stage
carcinoma as it always develops with an invasive growth.
The differential diagnosis of prostate
leiomyosarcoma includes leiomyosarcoma, which originated in the
bladder or adjacent to the predominant blood vessels, as well as
other rare benign or malignant primary prostate spindle cell
tumors. Imaging or radiology examination, including computed
tomography, may be important in the identification. The most common
confirmed diagnostic method was the B-ultrasound guided transrectal
prostate biopsy or transurethral resection of the prostate.
Additionally, Barwad et al (5)
reported that fine needle aspiration cytology can also be adopted
for the initial diagnosis of prostate leiomyosarcoma. Prostate
leiomyosarcoma tissue exhibited moderate to severe abnormal spindle
cells cross-enriched under the microscope. The degree of cell
atypia, the lesion site, the degree of mitosis and the rate of
infiltration can be used to distinguish the low-grade malignant
smooth muscle sarcoma and leiomyoma on the pathological section. A
closer association was observed between the degree of
atypia/mitosis and the characteristics of the disease. Even though
it was reported that leiomyosarcoma cells with more atypia or
mitosis tend to have higher degree of malignancy (6), certain low-grade prostate leiomyosarcoma
were reported (7). To differentiate
from stromal sarcoma, leiomyosarcoma lacks normal glands, in
addition to the coated glands.
Radical prostate resection was the major measurement
on the treatment of prostate leiomyosarcoma. The extent of surgical
resection markedly affected the prognosis. An improved prognosis
occurs in the microscopic negative margin compared with the
positive ones. To date, no optimal treatment of this disease
exists. Scholars have suggested that pre-operative adjuvant
therapy, followed by radical surgery or post-operative adjuvant
therapy, may provide an improved prognosis (8). Radical surgery can often be defined as
both radical prostate and bladder resection, and it always involves
pelvic lymph node dissection. Current treatment opinions for
locally advanced prostate leiomyosarcoma are neoadjuvant
chemotherapy or neoadjuvant radiochemotherapy, where chemotherapy
may involve ifosfamide, cyclophosphamide or dacarbazine (9). Other literature also reported that
chemotheraphy with methotrexate + etoposide + cisplatin may benefit
a similar outcome (10). However, no
consensus on the radiation dose exists. Sakano et al
(11) suggested that local control
can be achieved when the radiation dose was controlled between ~60
and 66 Gy. Since the disease is more prone to local and distant
recurrence, physical and other auxiliary examination, including
chest and abdomen x-ray and whole-body bone scan for patients
readmitted is highly important. Another important factor, to make a
comprehensive examination, was the regular follow-up of a patient,
which is difficult under the current constrained clinical situation
caused by various factors.
According to the literature, the prognosis of
patients with prostate leiomyosarcoma is poor. It is reported that
~25% of patients already exhibit a metastatic mass at the time of
diagnosis, and the predictive survival interval was 2–5 years
following diagnosis in 50–75% of patients. The lung metastases can
be found on the other patients in a short period of time (12). Vandoros et al (13) performed a comprehensive analysis based
on 54 prostate leiomyosarcoma cases in the published literature
prior to 2008. In this previous study, ~23.5% of patients exhibited
metastatic disease at the time of diagnosis. The proportion of lung
metastasis was ~17.6%, followed by ~11.7% of liver metastases, 5.8%
of bone metastases and only 3.6% of brain metastases.
The present case was without obvious metastases at
the time of diagnosis, with early post-operative recurrence and
distant metastasis. Therefore, although prostate leiomyosarcoma has
a poor prognosis, early treatment of post-operative recurrence and
metastases via a whole-body examination and closer follow-up was
realistic. These measurements may significantly prolong the
survival time and improve the quality of life for patients.
Acknowledgements
The present study was funded by grants from The Key
Project of Science and Technology of Zigong (no. 2015SF03) and the
Scientific research project of Health Department of Sichuan
Province (no. 110590).
References
|
1
|
Hansel DE, Herawi M, Montgomery E and
Epstein JI: Spindle cell lesions of the adult prostate. Mod Pathol.
20:148–158. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Markowski MC, Eisenberger MA, Zahurak M,
Epstein JI and Paller CJ: Sarcomatoid carcinoma of the prostate:
retrospective review of a case series from the Johns Hopkins
Hospital. Urology. 86:539–543. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Janet NL, May AW and Akins RS: Sarcoma of
the prostate: A single institutional review. Am J Clin Oncol.
32:27–29. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Talapatra K, Nemade B, Bhutani R, Kane S,
Bakshi A, Muckaden MA and Laskar S: Recurrent episodes of
hematuria: A rare presentation of leiomyosarcoma of prostate. J
Cancer Res Ther. 2:212–214. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Barwad A, Khandelwal N, Vyas S, Gogoi D
and Dey P: Primary leiomyosarcoma of the prostate with lung
metastasis: Report of a case diagnosed by fine-needle aspiration
cytology. Diagn Cytopathol. 39:700–702. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Tavora F, Kryvenko ON and Epstein JI:
Mesenchymal tumours of the bladder and prostate: An update.
Pathology. 45:104–115. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Dominguez A, Piulats JM, Suárez JF, Condom
E, Castells M, Camps N, Del García Muro FX and Franco E: Prostatic
sarcoma after conservative treatment with brachytherapy for
low-risk prostate cancer. Acta Oncol. 52:1215–1216. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hayashi T, Nakai Y, Kakuta Y, Takayama H,
Nakayama M, Nonomura N, Okumi M and Nakao A: A case of
leiomyosarcoma of prostate: Multimodality therapy suppressed
disease progression for long term. Hinyokika Kiyo. 56:527–530.
2010.PubMed/NCBI
|
|
9
|
Herawi M and Epstein JI: Specialized
stromal tumors of the prostate: A clinicopathologic study of 50
cases. Am J Surg Pathol. 30:694–704. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Suppiah R, Wood L, Elson P and Budd G:
Phase I/II study of docetaxel, ifosfamide, and doxorubicin in
advanced, recurrent, or metastatic soft tissue sarcoma (STS).
Invest New Drugs. 24:509–514. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Sakano Y, Yonese J, Okubo Y, Yoshimura K,
Maeda H, Yamauchi T, Fukui I, Kawai T and Ishikawa Y:
Leiomyosarcoma of the prostate: A case report of remission for 9
years by radiotherapy. Hinyokika Kiyo. 41:629–632. 1995.(In
Japanese). PubMed/NCBI
|
|
12
|
Martini N and McCormack PM: Evolution of
the surgical management of pulmonary metastases. Chest Surg Clin N
Am. 8:13–27. 1998.PubMed/NCBI
|
|
13
|
Vandoros GP, Manolidis T, Karamouzis MV,
Gkermpesi M, Lambropoulou M, Papatsoris AG, Zachos I and
Konstantinopoulos PA: Leiomyosarcoma of the prostate: Case report
and review of 54 previously published cases. Sarcoma.
2008:4587092008. View Article : Google Scholar : PubMed/NCBI
|