Introduction
The mainstay of treatment for nasopharyngeal
carcinoma (NPC) is radiotherapy (RT). Following the completion of
RT, a post-radiation nasopharyngeal ulcer (PRNU) is an important
consequential adverse effect in patients with NPC (1,2). However,
the diagnosis of PRNU has not been widely discussed, predominantly
due to the lack of understanding and effective diagnosis for this
complication. Traditionally, nasopharyngeal ulcers for patients who
underwent RT are commonly divided into mucosal ulcers induced by
radiation (RIMUs) and tumour necrosis-induced ulcers (TNIUs)
(3,4).
The former belongs to a severe grade of radiation mucositis, which
occurs in normal mucosa tissue; the latter is induced by the
necrosis of tumour tissue, which usually accompanies tumour
tissue.
In the present study, the intention was to elaborate
on a third type of ulcer. This ulcer occurs following the collapse
of radiation-induced tumour necrosis in areas of the primary tumour
bed, which is the major characteristic differing from the two
ulcers described above. This third type of ulcer has been termed
‘ulcer of post-radiation nasopharyngeal necrosis’ (UPRNN), which
has been rarely reported to the best of our knowledge, although
several authors have previously reported on certain NPC patients
with post-radiation nasopharyngeal necrosis (PRNN) (3,5). Only the
simple phenomenon of PRNN was described in these studies, and the
analysis of UPRNN with a full set of clinical characteristics,
including occurrence, evolution, incentive factors, diagnosis,
prognosis and grade of ulceration, has rarely been reported.
The present study aimed to illustrate the clinical
characteristics and risk factors of UPRNN to better understand this
complication.
Patients and methods
Patients
Between June 2010 and December 2015, 53 patients (13
women and 40 men) with pathologically diagnosed NPC were treated at
the Department of Radiation Oncology, Zhejiang Provincial Cancer
Hospital (Hangzhou, China). All these patients underwent
intensity-modulated radiotherapy (IMRT), were diagnosed with a
nasopharyngeal ulcer, and met the diagnosis criteria of a UPRNN.
All the patients underwent a single round of IMRT, and all of them
received chemotherapy, including induction chemotherapy for 34
patients, concurrent chemotherapy for 18 patients and adjuvant
chemotherapy for 12 patients (Table
I).
 | Table I.Characteristics of 53 patients with
nasopharyngeal carcinoma who had post-radiation nasopharyngeal
necrosis. |
Table I.
Characteristics of 53 patients with
nasopharyngeal carcinoma who had post-radiation nasopharyngeal
necrosis.
| Characteristic | UPRNN |
|---|
| Age (years) |
|
| Mean ±
SD | 46.75±6.82 |
| Gender |
|
| Male | 32 |
|
Female | 21 |
| BMI |
|
| Mean ±
SD | 23.47±2.67 |
| Prescriptive dose of
ulcer zone (Gy) |
|
| Mean ±
SD | 70.59±2.36 |
| T stage |
|
| T1 | 0 |
| T2 | 2 |
| T3 | 36 |
| T4 | 15 |
| Sites of
involvementb |
|
| 1–3 | 24 |
|
>3 | 29 |
| Grades of ulcer |
|
| Mild | 4 |
|
Moderate | 27 |
|
Severe | 22 |
| Chemotherapy |
|
|
Neo-CT | 34 |
|
Concurrent | 18 |
|
Adjuvant | 12 |
| Response of
neo-CT |
|
| SD | 22 |
| PR | 12 |
| CR | 0 |
| Intervala (months) |
|
| Mean ±
SD | 2.92±1.26 |
| Outcome of UPRNN |
|
|
Alive | 48 |
| Succumbed
to mortality | 5 |
All the patients were followed up with MRI and
endoscopic examinations every 3 months during the 2 years following
RT, and subsequently 6 months after the 2 years. Once a
nasopharyngeal ulcer had been diagnosed, pathological and MRI
examinations were combined to identify the UPRNN. The follow-up
period was defined from the completion of the RT to the last
follow-up day.
MRI examination
All of the MRI examinations were performed with a
1.5-T MAGNETOM System (Siemens AG, Munich, Germany). The area from
the suprasellar cistern to the inferior margin of the sternal end
of the clavicle was scanned with a head-and-neck combined coil. The
scanning sequence included transverse (T) 1-weighted images on the
axial, coronal and sagittal planes, and the T2-weighted images on
the axial plane were obtained prior to the injection of a contrast
reagent. Following an intravenous gadolinium-diethylenetriamine
pentaacetic acid (Gd-DTPA) injection at a dose of 0.1 mmol/kg of
body weight, T1-weighted axial and sagittal sequences were
performed sequentially. The MRI examinations were interpreted by a
radiologist and a radiation oncologist experienced in NPC diagnoses
and treatment for 10 years, respectively.
Diagnosis and grading of UPRNN
The diagnosis criteria of a UPRNN were established
in order to conform with the following points: i) The pathological
confirmation included typical features of an ulcer without evidence
of tumour recurrence or any residual tumour; ii) the MRI
examination revealed an ulcer site at the primary tumour bed; and
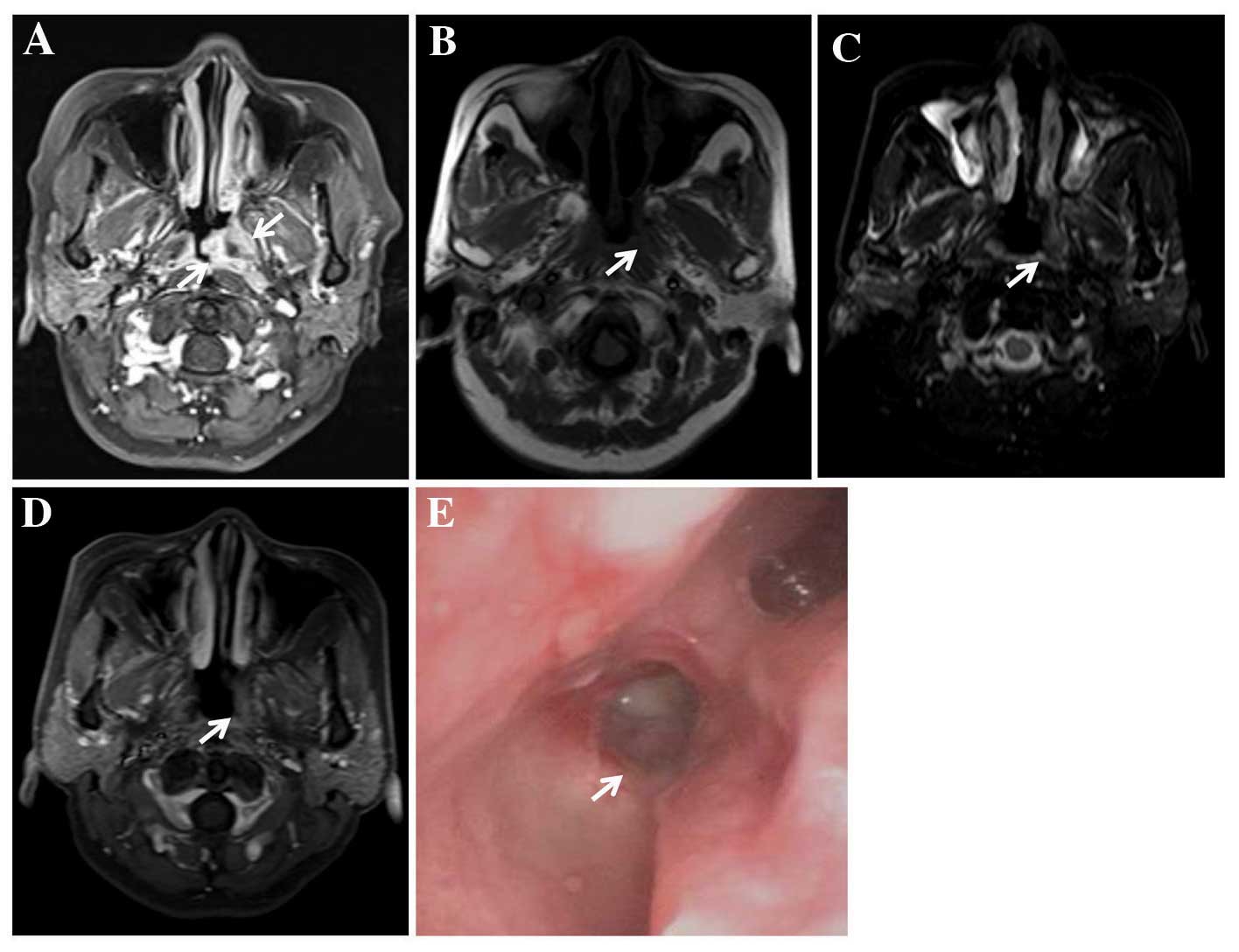
iii) the patients had previously undergone RT. The grading of the
UPRNN was divided into three degrees according to the depth of the
ulcer on MRI examination: A mild-grade UPRNN was classified as an
ulcer confined to the mucosa (Fig.
1); a moderate-grade UPRNN was an ulcer invading, but not
exceeding, the muscle tissue (Fig.
2); and a severe-grade UPRNN was an ulcer exceeding the muscle
tissue (Fig. 3).
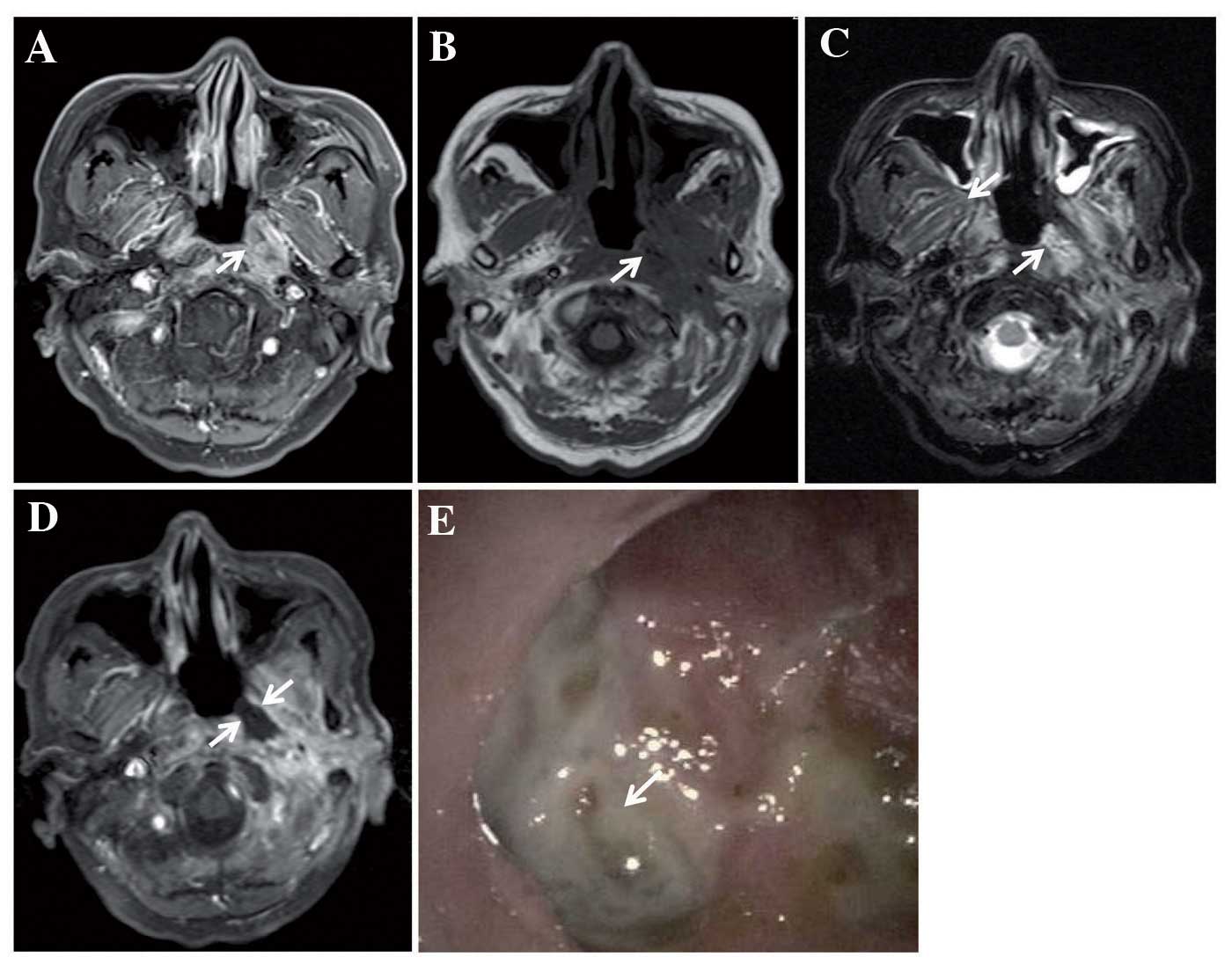
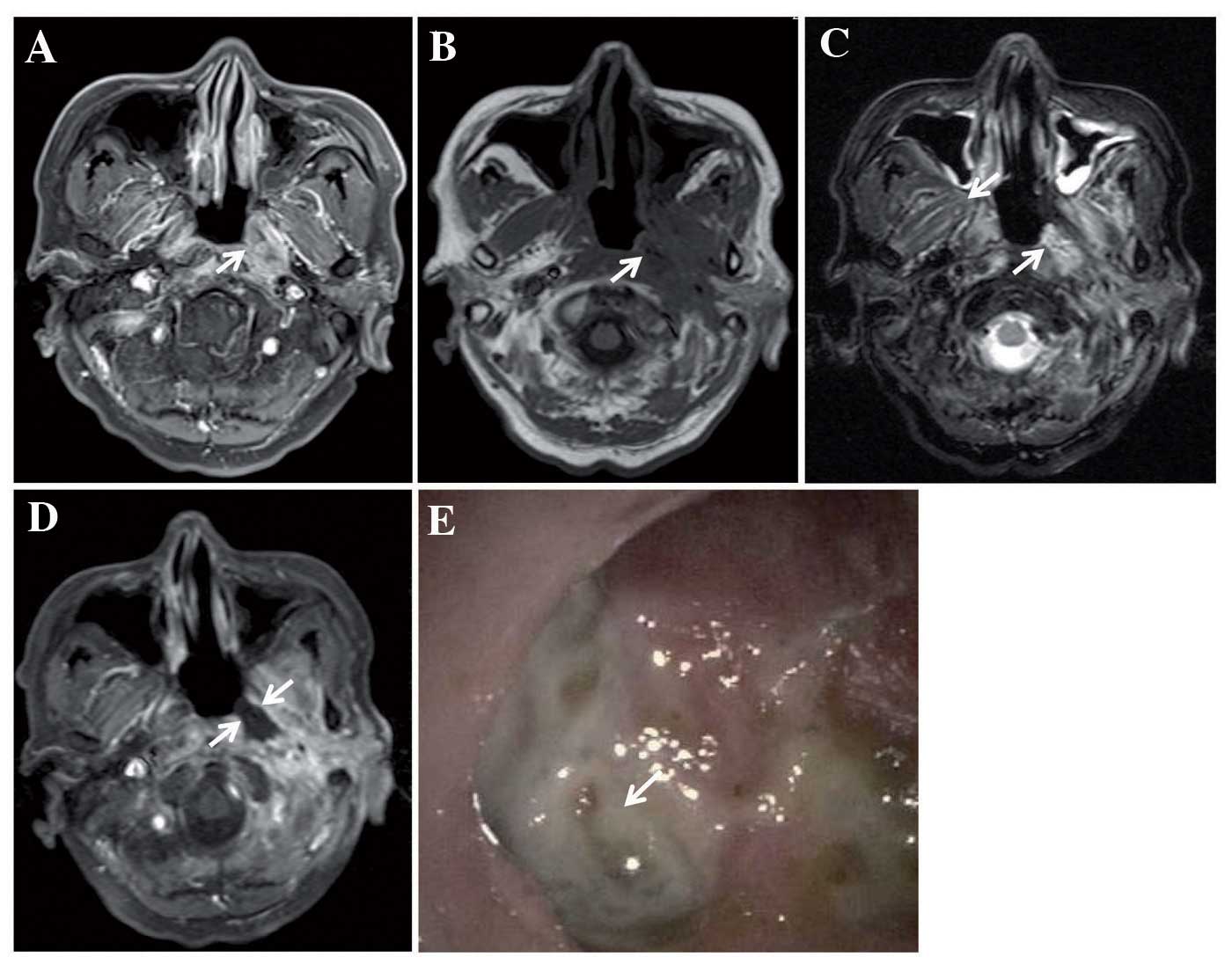 | Figure 1.MRI examination performed on a
63-year-old man diagnosed with NPC with T3N2M0, who underwent IMRT
without neo-adjuvant chemotherapy. (A) Transverse
contrast-enhanced, T1-weighted MRI revealed enhanced tumour tissue
invading the musculus longus capitis and medial pterygoid muscle on
the left side of the nasopharyngeal cavity. (B) Transverse
T1-weighted MRI revealed a low-signal area in the initial tumour
bed at 2 months following the completion of RT (as indicated by the
arrow). (C) Transverse T2-weighted MRI revealed a high-signal area
in the initial tumour bed (indicated by the arrow). (D) Transverse
contrast-enhanced, T1-weighted MRI revealed a non-enhanced area,
which showed the ulcer exceeding the muscle tissue (arrow), and
this was categorised as a severe-grade UPRNN. (E) The ulcer was
located on the left side of the nasopharyngeal cavity (demonstrated
by the arrow). RT, radiotherapy; MRI, magnetic resonance imaging;
NPC, nasopharyngeal carcinoma; IMRT, intensity-modulated RT; UPRNN,
ulcer of post-radiation nasopharyngeal necrosis. |
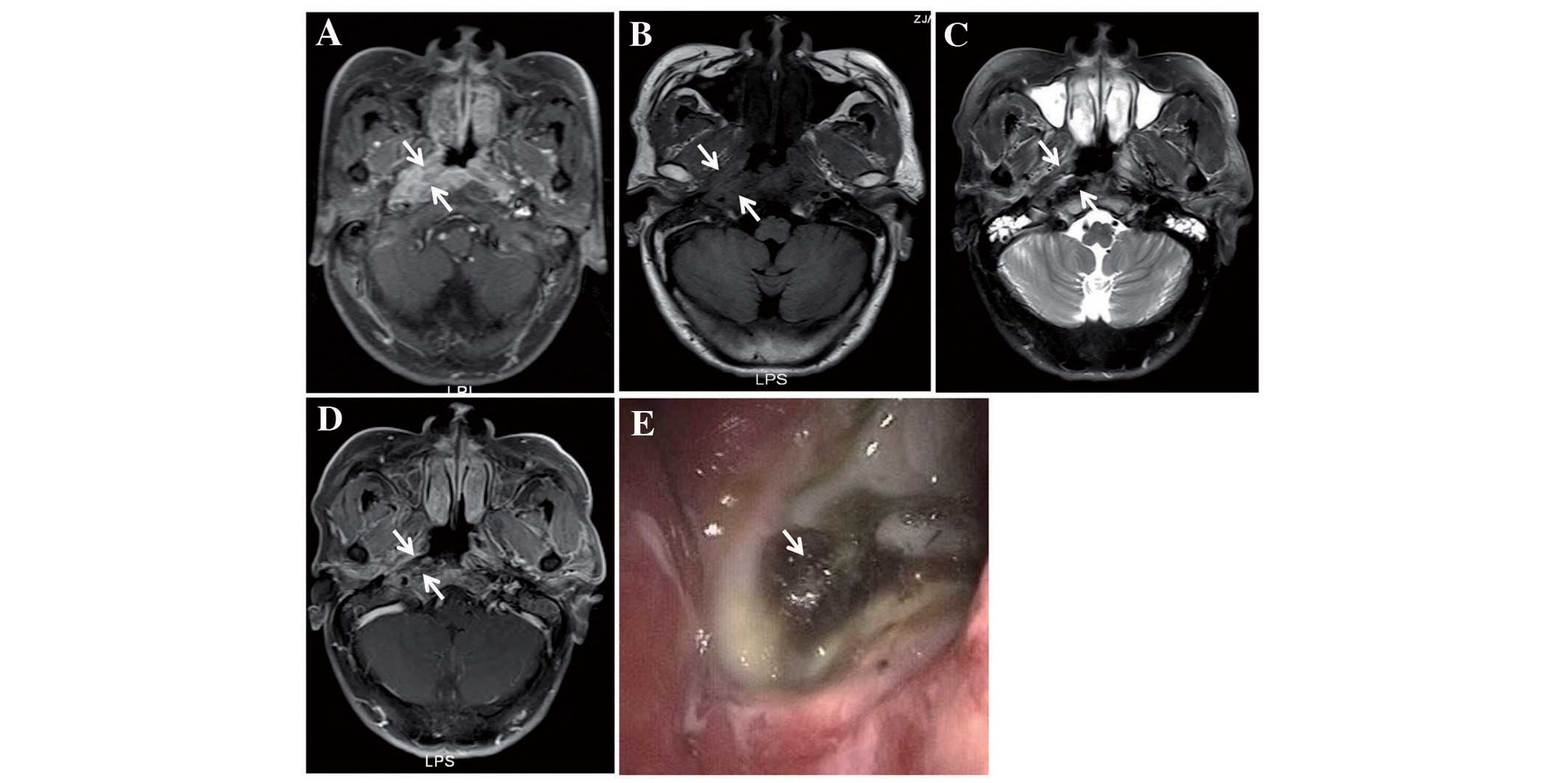
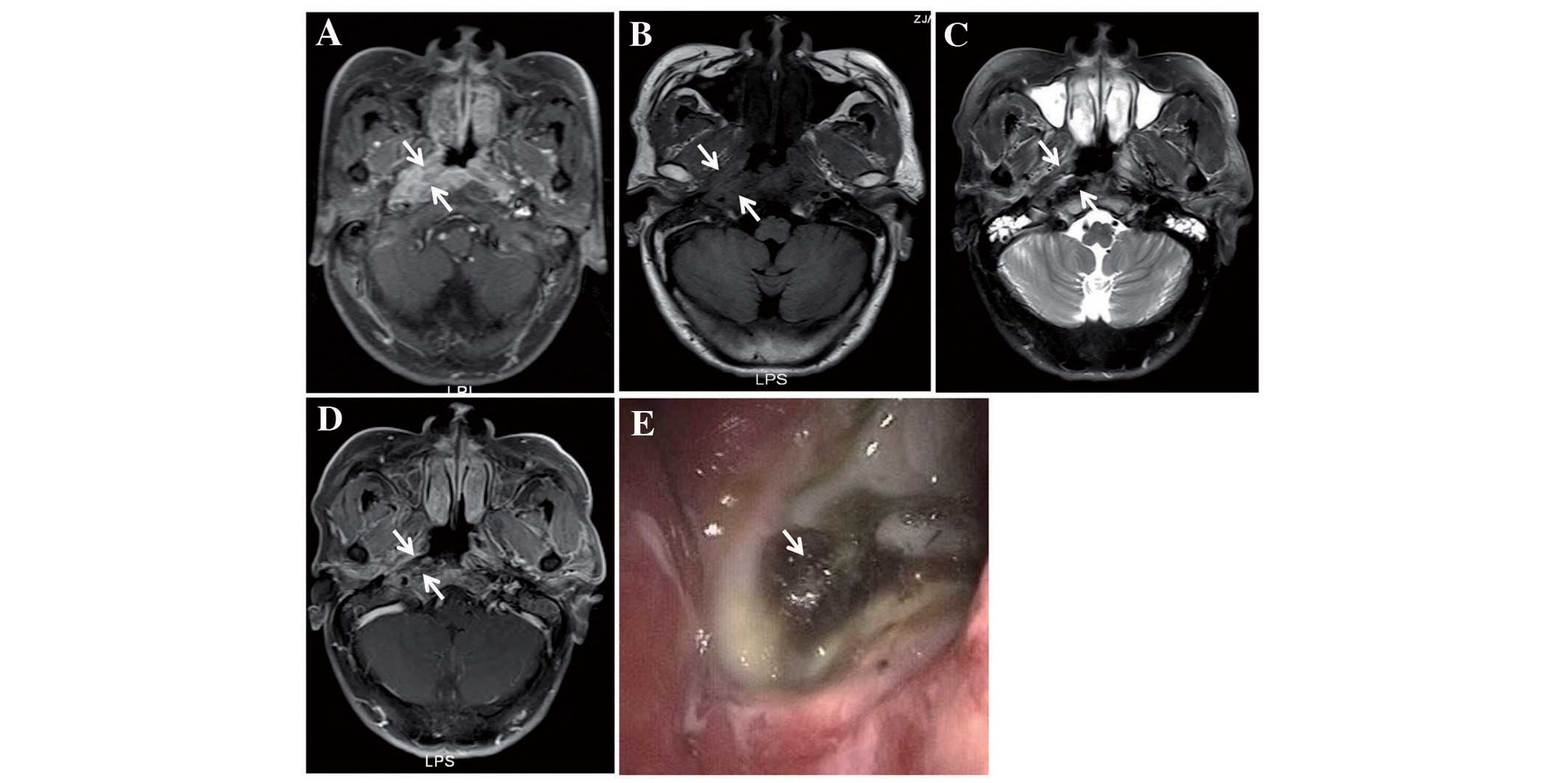 | Figure 2.MRI examination performed on a
64-year-old man diagnosed with NPC with T3N3M0, who underwent IMRT
with two courses of neo-adjuvant chemotherapy and received a
partial response of short-term therapeutic effects of chemotherapy.
(A) Transverse contrast-enhanced T1-weighted MRI revealed enhanced
tumour tissue invading the musculus longus capitis, parapharyngeal
space and medial pterygoid muscle on the right side of the
nasopharyngeal cavity (as indicated by the arrows). (B) Transverse
T1-weighted MRI revealed a low-signal area in the initial tumour
bed at 1 month following the completion of RT (demonstrated by the
arrows). (C) Transverse T2-weighted MRI revealed a mixed signal
area in the initial tumour bed (shown by the arrows). (D)
Transverse contrast-enhanced, T1-weighted MRI revealed a
non-enhanced area, which showed the ulcer invading, but not
exceeding, the muscle tissue (demonstrated by the arrows). The
ulcer was categorised as a moderate-grade UPRNN. (E) The ulcer was
located on the right side of the nasopharyngeal cavity (indicated
by the arrow). RT, radiotherapy; MRI, magnetic resonance imaging;
NPC, nasopharyngeal carcinoma; IMRT, intensity-modulated RT; UPRNN,
ulcer of post-radiation nasopharyngeal necrosis. |
Laboratory examination
All the patients accepted a routine laboratory
examination every week during the course of RT, including routine
blood and biochemical testing. All the above examinations were
reviewed from the medical record.
Treatment of UPRNN
According to the severity of the UPRNN, the patients
with a mild or moderate grade UPRNN were administered a
conservative treatment, including anti-inflammation treatment and
flushing with 0.9% saline. The patients with a severe UPRNN were
treated with endoscopic debridement and anti-inflammation
treatment.
Statistical analyses
All statistical analyses were performed using SPSS
16.0 software (SPSS, Inc., Chicago, IL, USA). Descriptive
statistics were produced for continuous variables. The results are
presented as the mean ± SD for continuous variables.
Results
General clinical feature of UPRNN
The general clinical data of the 53 patients
included in the present study are summarised in Table I. All the 53 patients complained of
headache and experienced a foul odour. The average age was
46.75±6.82 years. The body mass index was 23.47±2.67
kg/m2, and the prescriptive dose of the ulcer zone was
70.59±2.36 Gy. As for the tumour (T) stage, the UPRNN was
predominantly distributed at the T3/4 stage. All the patients
underwent chemotherapy, including neo-adjuvant chemotherapy for 34
patients, concurrent chemotherapy for 18 patients and adjuvant
chemotherapy for 12 patients. In the analysis of the neo-adjuvant
chemotherapy response, 22 patients were categorised as having
stable disease (SD), and 12 patients received a partial response.
According to the depth of invasion, the UPRNN was divided into
three grades, including four mild-grade UPRNNs, 27 moderate-grade
UPRNNs and 22 severe-grade UPRNNs. The average interval from the
completion of RT to the initiation of UPRNN was 2.92±1.26
months.
In the laboratory examinations, the results revealed
that 47 patients also had anaemia during the course of RT, which
included 27 patients with mild anaemia, 20 with moderate anaemia
and none with severe anaemia. However, as for an infectious marker,
the majority of the patients were diagnosed with a normal value of
C-response protein during the course of RT (Table II). During the follow-up period, 48
patients were alive, whereas five patients succumbed to mortality
due to a massive nasopharyngeal haemorrhage. In the analysis of the
sites that contained an ulcer, the parts especially for
medial/lateral pterygoid muscle, and musculus longus capitis
involved by tumour, was easier to complicate with UPRNN (Table III).
 | Table II.Laboratory examination of 53 patients
with UPRNN. |
Table II.
Laboratory examination of 53 patients
with UPRNN.
| Item | No. of patients |
|---|
| Blood routine |
|
|
Normal | 6 |
| Mild
anaemiaa | 27 |
| Moderate
anaemia | 20 |
| Severe
anaemia | 0 |
| C-response
protein |
|
|
Normalb | 31 |
| 2 folds
of normal | 18 |
| 10 folds
of normal | 4 |
 | Table III.Involvement of parts of the tumour in
53 patients with UPRNN. |
Table III.
Involvement of parts of the tumour in
53 patients with UPRNN.
| Part | No. of patients |
|---|
| Medial pterygoid
muscle | 36 |
| Lateral pterygoid
muscle | 15 |
| Parapharyngeal
space | 53 |
| Musculus longus
capitis | 43 |
| Skull base | 12 |
MRI and endoscopic features of
patients with UPRNN
The results of the MRI examinations, combined with
the endoscopic examinations, were revealed to be well consistent
with UPRNN. It is a good modality for an MRI examination to
estimate the invasion scope of a moderate- or severe-grade UPRNN,
whereas it is difficult to detect a mild-grade UPRNN from an MRI
examination alone. From an MRI examination, UPRNNs are revealed to
commonly present with different sizes of defects located in the
primary tumour bed, unless there is an adhesion of necrosis or
secreta. However, it may be advantageous for a diagnosis of UPRNN
to be made using contrast-enhanced MRI, which highlights
non-enhanced zones in the UPRNN.
Treatment and prognosis of UPRNN
Of the four patients with a mild-grade UPRNN, three
of them were stable and ultimately recovered following an
anti-inflammation and flushing treatment, although the condition of
one patient deteriorated into moderate-grade UPRNN, and this
patient underwent conservative treatment. None of the patients
succumbed to mortality. Of the 27 patients with a moderate-grade
UPRNN, 14 were stable and finally recovered, although 13 patients
were progressive and underwent debridement. One of them succumbed
to mortality. Of the 22 patients with a severe-grade UPRNN, none of
them were stable and all the patients underwent endoscopic
debridement. Four of the patients succumbed to mortality due to a
massive haemorrhage (Table IV).
 | Table IV.Distribution and prognosis of the 53
patients with UPRNN. |
Table IV.
Distribution and prognosis of the 53
patients with UPRNN.
| Grade of UPRNN | Stable | Debridement | Progressive | Dead |
|---|
| Mild | 3 | 0 | 1 | 0 |
| Moderate | 14 | 13 | 13 | 1 |
| Severe | 0 | 22 | 22 | 4 |
Discussion
RT, as the most effective treatment modality, exerts
a vital role in NPC treatment, while it is a kopis for the
treatment as increasing numbers of patients are experiencing
various post-radiation complications, corresponding to the
increasing number of survivors of irradiated NPC. An RIMU in NPC,
as a severe grade of post-radiation nasopharyngeal mucositis for
patients with NPC, was considered to be the only type of ulcer
other than the tumorigenic ulcer (6).
However, the present hypothesis is that a third type of ulcer that
is different from an RIMU may exist when a patient undergoes RT,
which in the present study has been termed a ‘UPRNN’.
In the present study, 53 patients were included who
met our diagnosis criteria for a UPRNN, and the clinical
characteristics of a UPRNN were analysed. Based on the results
obtained, three clinical factors were identified that may be
associated with the occurrence of a UPRNN. First, the occurrence of
nasopharyngeal necrosis is associated with the response to
neoadjuvant chemotherapy for NPC in the study. The results
demonstrated that 22 of the 34 patients who underwent
neo-chemotherapy were of SD and suffered from a UPRNN, which
revealed that those patients that respond poorly to treatment may
be more prone to suffering from a UPRNN. Secondly, the present
results revealed that the majority of the patients with UPRNN also
had anaemia, which demonstrated that malnutrition may exert an
important role in the development of a UPRNN. Thirdly, it remained
the case that the lesion area and T stage were more closely
associated with the occurrence of UPRNN. The invasion of muscle
(particularly for the musculus longus capitis and medial/lateral
pterygoid muscle) and T3/4 stage have a tendency to complicate a
UPRNN. On the other hand, inflammatory factors did not appear to be
associated with the occurrence of a UPRNN.
The exact mechanism underlying the formation of a
UPRNN has yet to be fully elucidated. It has been reported that
hypoxia, hypovascularity and hypocellularity may be caused by RT in
areas occupied by a tumour. Consequently, normal collagen synthesis
and cell production may be impaired due to malnutrition and a
deficiency of oxygen, which may subsequently lead to tissue
breakdown and a chronic, non-healing wound (7). In the present study, factors, including
poor response of chemotherapy, anaemia and large bulk of a tumour,
seem to be in accordance with the above hypothesis. A large tumour,
and poor response of a tumour, are predictive of a deficiency of
the blood supply and oxygen in the parenchyma of a tumour.
Additionally, the complication of anaemia during the course of RT
demonstrated that malnutrition may exert an important role in the
development of UPRNN.
An RIMU in NPC, a major severe late adverse effect,
was reported with an incidence as high as 31.5–40.6%. It is one of
the complications attributed to RT-induced mucositis (1,5), and
should be distinguished from a UPRNN. To the best of our knowledge,
the location of an RIMU usually originates from normal mucosa
tissue, and the onset time of an RIMU is 1 year following the
completion of RT (Fig. 4). However,
the site of a UPRNN is closely associated with the site of the
primary tumour, and the onset time of a UPRNN is usually within 6
months following the completion of RT. A UPRNN may be cured in that
early period (Figs. 1–3). It may be helpful to differentiate both
types of ulcer via MRI and endoscopic examinations. In the present
study, the UPRNNs were ranked into three grades according to the
depth of invasion, and it was revealed that a severe-grade UPRNN
should be treated with debridement. Otherwise, the UPRNN may worsen
and endanger the life of the patient.
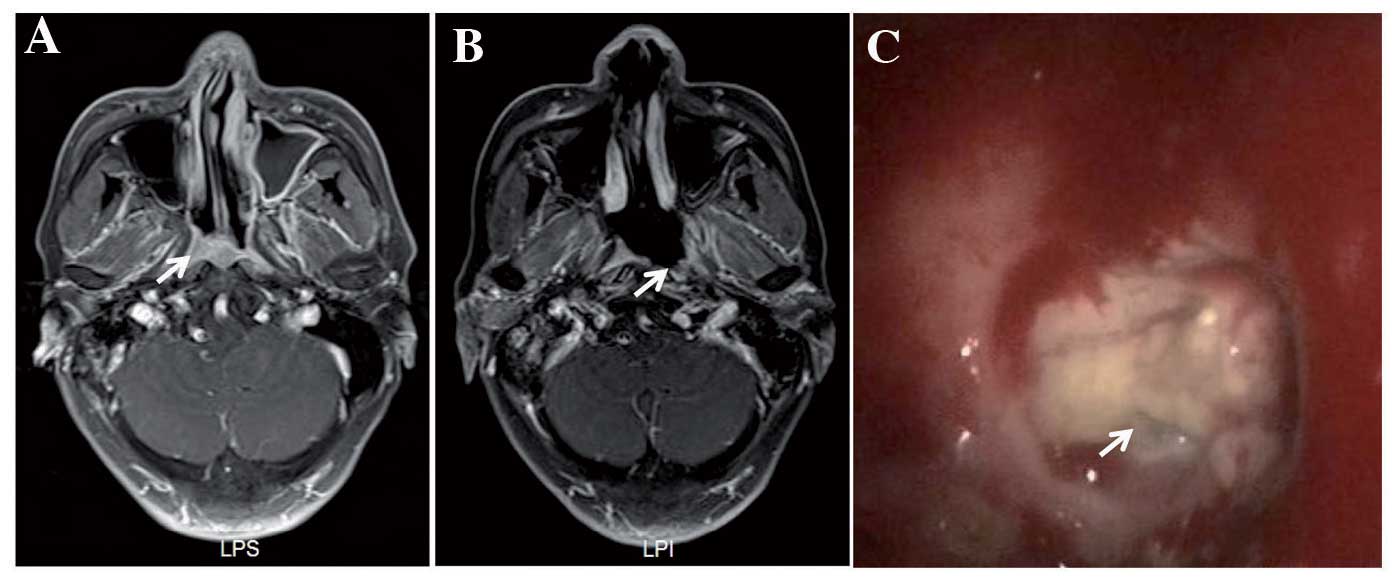
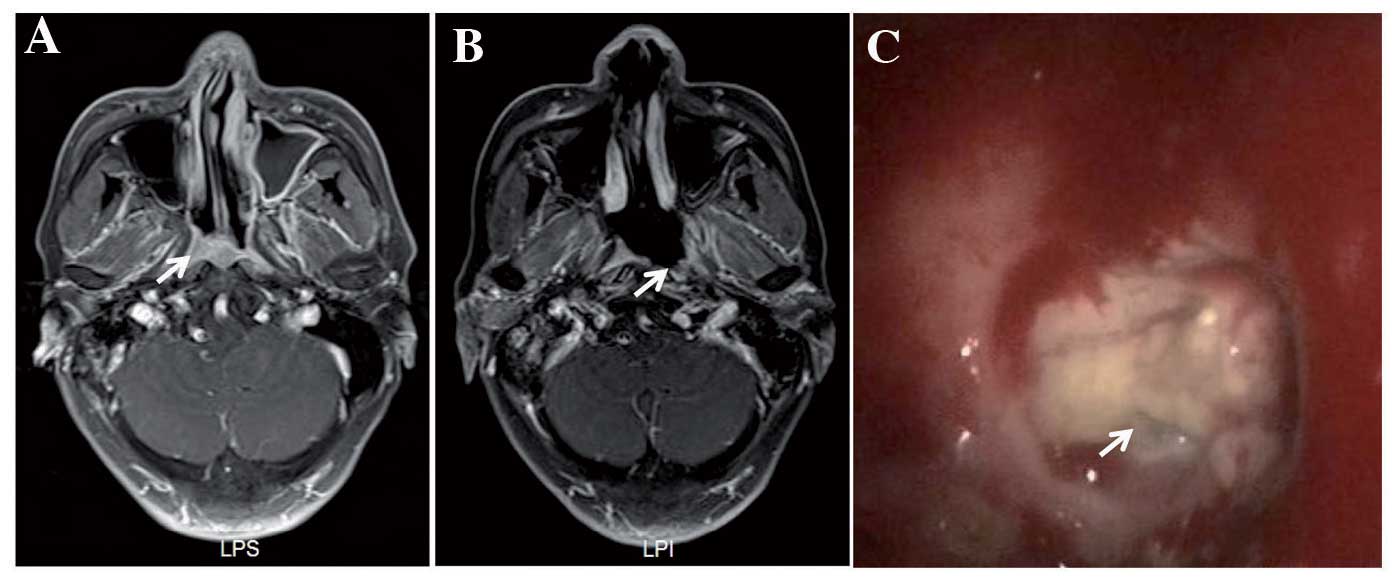 | Figure 4.MRI examination performed on a
69-year-old man diagnosed with NPC with T3N2M0/rT3N0M0, who
underwent RT twice. The second RT was IMRT with two courses of
neo-adjuvant chemotherapy. The ulcer occurred at 4 months following
the completion of IMRT. The patient was diagnosed with RIMU, not
UPRNN. (A) Transverse contrast-enhanced, T1-weighted MRI revealed
enhanced tumour tissue invading the parapharyngeal space and medial
pterygoid muscle on the left side of the nasopharyngeal cavity
(shown by the arrow). (B) Transverse contrast-enhanced, T1-weighted
MRI revealed a large ulcer with non-enhancement on the right side
of the nasopharyngeal cavity at 4 months following the completion
of RT, which was not previously occupied by clear tumour tissue
(shown by the arrow). (C) The ulcer was located on the left side of
the nasopharyngeal cavity (indicated by the arrow). RT,
radiotherapy; MRI, magnetic resonance imaging; NPC, nasopharyngeal
carcinoma; IMRT, intensity-modulated RT; RIMU, mucosal ulcer
induced by radiation; UPRNN, ulcer of post-radiation nasopharyngeal
necrosis. |
The MRI characteristics of a UPRNN usually reveal
defects in the region of the primary tumour bed, unless there is an
adhesion of the pseudomembrane or necrosis, and a non-enhanced
region is observed in areas of UPRNN. A mild-grade UPRNN exhibits
discontinuous enhanced mucosa, which can be easily overlooked due
to the small size of the ulcer. An endoscopic examination is
helpful in diagnosing a mild-grade UPRNN. An MRI examination allows
for the assessment of the scope of the UPRNN; therefore, the UPRNNs
were divided into three grades according to the invasion depth.
The treatment of a UPRNN is diverse, according to
the severity of the UPRNN. A mild-grade UPRNN may call for a
conservative treatment or a follow-up examination, and a
moderate-grade UPRNN should be treated medically, with a subsequent
follow-up examination. If the disease is progressive, debridement
may be necessary for the patient. A patient with a severe-grade
UPRNN should be given endoscopic debridement and irrigation of the
nasal cavity. The prognosis of a UPRNN also differs from the
severity of the UPRNN. For example, a patient with a
mild/moderate-grade UPRNN may recover from the disease after
medical treatment has been administered; however, a severe-grade
UPRNN may be fatal unless debridement is given.
As for the pathological development of a UPRNN, this
may be described as a process of three stages through dynamic
observation. In the early stage, necrosis occurs in the region of
the tumour bed. In the second stage, granulation tissue may be
observed around the area of necrosis, and in the last stage, scar
tissue may be formed in the region of the granulation tissue.
However, the above three stages are not observed in all the
patients, since the majority of the patients are not followed up at
regular intervals or do not visit the hospital in time.
In conclusion, in the present study UPRNNs have been
demonstrated to possess characteristic clinical features and a
characteristic appearance following MRI, and the occurrence of a
UPRNN may be associated with several clinical factors. Therefore,
the recognition of UPRNNs may be useful as a prerequisite in terms
of their treatment and avoidance.
Acknowledgements
The present study was supported by grants from
Zhejiang Provincial Medical Science and Technology Program (grant
no. 2015RCB005), the Provincial Natural Science Funds of the
Zhejiang Province of China (grant no. Q15H160012), and the General
Project of the Zhejiang Provincial Health Bureau (grant nos.
2015KYB063, 2015KYB048 and 2016KYA051).
References
|
1
|
Qiu S, Lin S, Tham IW, Pan J, Lu J and Lu
JJ: Intensity-modulated radiation therapy in the salvage of locally
recurrent nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys.
83:676–683. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Wu X, Huang PY, Peng PJ, Lu LX, Han F, Wu
SX, Hou X, Zhao HY, Huang Y, Fang WF, et al: Long-term follow-up of
a phase III study comparing radiotherapy with or without weekly
oxaliplatin for locoregionally advanced nasopharyngeal carcinoma.
Ann Oncol. 24:2131–2136. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Chen MY, Mai HQ, Sun R, Guo X, Zhao C,
Hong MH and Hua YJ: Clinical findings and imaging features of 67
nasopharyngeal carcinoma patients with postradiation nasopharyngeal
necrosis. Chin J Cancer. 32:533–538. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hua YJ, Chen MY, Qian CN, Hong MH, Zhao C,
Guo L, Guo X and Cao KJ: Postradiation nasopharyngeal necrosis in
the patients with nasopharyngeal carcinoma. Head Neck. 31:807–812.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Chen HY, Ma XM, Ye M, Hou YL, Xie HY and
Bai YR: Effectiveness and toxicities of intensity-modulated
radiotherapy for patients with locally recurrent nasopharyngeal
carcinoma. PLoS One. 8:e739182013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kwong DL, Nicholls J, Wei WI, Chua DT,
Sham JS, Yuen PW, Cheng AC, Yau CC, Kwong PW and Choy DT:
Correlation of endoscopic and histologic findings before and after
treatment for nasopharyngeal carcinoma. Head Neck. 23:34–41. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Marx RE: Osteoradionecrosis: A new concept
of its pathophysiology. J Oral Maxillofac Surg. 41:283–288. 1983.
View Article : Google Scholar : PubMed/NCBI
|