Introduction
Infections caused by carbapenem-resistant
Klebsiella pneumoniae (CRKP) represent a significant public
health concern worldwide. Infections caused by CRKP isolates are
associated with high morbidity and mortality rates, particularly in
patients with haematological malignancies. Infection and
colonization by these multiresistant bacteria may represent a
challenge in SCT recipients for the management of
post-transplantation complications, as well as for the eligibility
to receive a transplant in patients who acquire the pathogen prior
to the procedure (1,2).
We herein report the case of a blast-phase chronic
myeloid leukemia (BP-CML) patient with a highly resistant,
CRKP-associated tricuspid valve endocarditis, who was treated with
a combination of systemic antimicrobial therapy and surgical valve
repair, and subsequently underwent successful allogeneic stem cell
transplantation (allo-SCT). To the best of our knowledge, this is
the first reported CRKP tricuspid valve endocarditis in the medical
literature.
Case report
A 50-year-old female patient with BP-CML was
referred to the Istanbul Medipol University in January 2015. The
patient had been diagnosed with CML in Libya (July, 2014). The
disease was in chronic phase, so treatment with imatinib was
started by her physicians. After treatment with imatinib for 3
months, the patient developed progressive disease with myeloid
blastic transformation and 7+3 induction chemotherapy was
initiated. During this treatment, the patient was intubated for
severe pneumonia with sepsis and had to stay in the intensive care
unit (ICU) for ~2 months in a Libyan hospital. The bone marrow
biopsy that was performed after the infection had resolved was
consistent with complete remission of the leukaemia; thus, the
patient was referred to our hospital for an allo-SCT.
On admittance to the hospital, the patient was
febrile. Peripheral and central venous port blood cultures were
collected, which grew KP that was susceptible only to tigecycline.
As venous port infection was suspected, the patient's venous port
was removed and she was treated with tigecycline and meropenem
(Table I, 1st bacteraemia). Treatment
was discontinued after 14 days. The patient was in good condition
and preparations for allo-SCT were initiated. During her work-up,
the patient developed new onset fever 5 days after the cessasion of
antibiotics. The blood cultures again revealed KP, with the same
resistance pattern (Table I, 2nd
bacteraemia). Tigecycline and imipenem were administered. The fever
resolved and the acute-phase parameters returned to normal levels
within 5 days. Treatment was again discontinued after 2 weeks, but
the patient developed fever shortly after. Repeated blood cultures
again grew pan-resistant KP (Table I,
3rd bacteraemia). Rectal swabs that were collected during the
hospitalisation period were all negative for the carrier state of
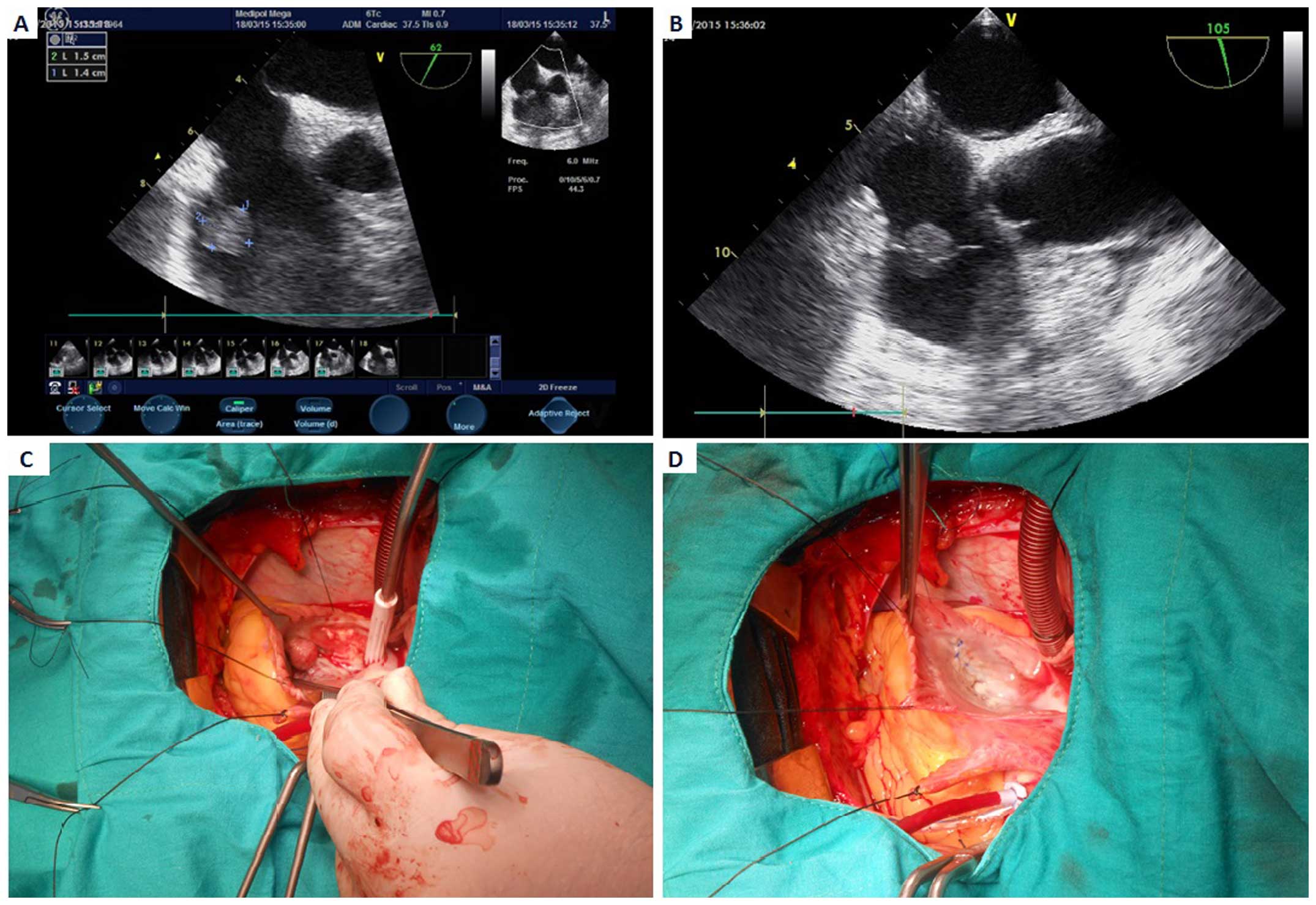
CRKP. Transthoracic echocardiogram was performed for repeated
bacteraemia, and revealed enlarged right cardiac chambers, moderate
tricuspid valve insufficiency and a mass sized 1.5×1.4 cm on the
tricuspid valve, compatible with a septic vegetation. With the
diagnosis of tricuspid valve endocarditis due to a multiresistant
pathogen, the patient was operated for excision of the vegetation
and tricuspid valve repair (Fig. 1).
The patient was treated with imipenem-cilastatin 1 g intravenously
every 6 h, plus gentamicin 80 mg intravenously every 8 h, plus
sulbactam 1 g intravenously every 6 h for 4 weeks.
 | Table I.Antibiotic resistance pattern of
bacteraemia and endocarditis. |
Table I.
Antibiotic resistance pattern of
bacteraemia and endocarditis.
| Antibiotics | 1st bacteraemia | 2nd bacteraemia | 3rd bacteraemia | Culture of
vegetation |
|---|
|
Ampicillin-sulbactam | >32 | R | >32 | R | >32 | R | >32 | R |
| Piperacillin | >128 | R | >128 | R | >128 | R | >128 | R |
|
Piperacillin-tazobactam | >128 | R | >128 | R | >128 | R | >128 | R |
| Ceftazidime | 16 | R | 4 | I | 16 | R | 4 | R |
|
Cefoperazone-sulbactam | >64 | R | >64 | R | >64 | R | >64 | R |
| Cefepime | >64 | R | >64 | R | >64 | R | >64 | R |
| Imipenem | >16 | R | 2 | I | 8 | R | >16 | R |
| Meropenem | >16 | R | >16 | R | >16 | R | >16 | R |
| Amikacin | >64 | R | >64 | R | >64 | R | >64 | R |
| Gentamicin | >16 | R | >16 | R | >16 | R | >16 | R |
| Netilmicin | 8 | I | 8 | I | 8 | I | 8 | I |
| Ciprofloxacin | >4 | R | >4 | R | >4 | R | >4 | R |
| Levofloxacin | >8 | R | >8 | R | >8 | R | >8 | R |
| Tetracycline | 4 | I | 4 | I | 8 | I | 8 | I |
| Tigecycline | 2 | S | 1 | S | 4 | I | 4 | I |
| Colistin | >16 | R | R | R | >16 | R | >16 | R |
|
Trimetoprim-sulfamethoxazole | >320 | R | >320 | R | >320 | R | >320 | R |
During the treatment period of endocarditis, the
patient was also treated for CML with nilotinib. However,
polymerase chain reaction (PCR) for Bcr/Abl remained positive,
indicating residual disease. After the infection had resolved,
unmanipulated peripheral blood allo-SCT from a full-matched sibling
donor was performed in November, 2015. The reduced intensity
conditioning (RIC) regimen included fludarabine at 30
mg/m2/day for 5 days and busulfan at 3.2 mg/kg/day for 2
days. Cyclosporin A, short-course methotrexate and antithymocyte
globulin were used for acute graft-vs.-host disease (GVHD)
prophylaxis. Allo-SCT was performed without complications;
neutrophil engraftment was achieved on day +15 and thrombocyte
engraftment was achieved on day +14 post-transplantation. The
patient is currently in complete remission with complete chimerism,
without evidence of any GVHD, for >3 months after allo-SCT. The
PCR of Bcr/Abl is also negative, showing no signs of residual
disease.
Written informed consent was obtained from the
patient for the publication of the case details.
Discussion
KP is one of the most important causes of health
care- and ICU-acquired infections (3)
and has been reported as the second overall cause of Gram-negative
bloodstream infections (BSI) after Escherichia coli.
However, Klebsiella species are a particularly rare cause (1.5%) of
Gram-negative bacterial endocarditis. Klebsiella species cause 1.2%
of the cases of native valve endocarditis and 4.1% of the cases of
prosthetic valve endocarditis. It has been reported that the most
commonly affected valve is the aortic valve, followed by the mitral
and tricuspid valves. The most common source of bacteraemia is
defined as urinary tract infection and infection of a pacemaker
(4,5).
In our patient, the source was an infected port catheter, which led
to tricuspid valve endocarditis. To the best of our knowledge, this
is the first reported case of tricuspid valve endocarditis due to
CRKP.
KP is a rare but extremely dangerous cause of
bacterial endocarditis. Large vegetations, valve perforation and
root abscesses are frequent complications. Combined medical and
surgical treatment is usually required. The reported mortality rate
of Klebsiella endocarditis is 49% (6). The main predictors of CRKP infection are
poor functional status, high severity of underlying conditions, ICU
stay and prior exposure to antimicrobial agents. Patients with
haematological malignancies and haematopoietic stem cell transplant
recipients are particularly vulnerable to CRKP infections due to
chemotherapy-induced gastrointestinal mucositis, prolonged
hospitalizations and neutropenia, as well as the frequent use of
broad-spectrum antibacterial agents (7). Our patient combined several risk
factors, namely poor functional status, serious haematological
malignancy, history of active chemotherapy, prolonged
hospitalization with ICU stay and the use of broad-spectrum
antibiotics, making her treatment more challenging.
There is currently no consensus regarding the
optimal regimen for treating CRKP. Treatment selection is generally
based on the results of retrospective and/or single-center studies
of CRKP BSIs. It is currently widely accepted that the combination
of a first-line antibiotic, mainly carbapenems, at higher doses to
overcome resistance, and a second-line antibiotic with
Gram-negative activity for which resistance has hopefully not yet
developed (for example, colistin, tigecycline, gentamicin,
fosfomycin) is the most suitable treatment option for CRKP BSIs
(4,8).
Our patient was successfully treated with a combination of
high-dose imipenem-cilastatin, gentamicin and sulbactam.
In tricuspid valve endocarditis, surgery is
indicated for persistent right-sided heart failure despite medical
therapy, recurrent pulmonary septic emboli, septic shock, abscess
formation or failure of antimicrobial therapy to control the
infection (7). In our patient,
recurrent bacteraemia with a multiresistant pathogen was the main
indication for valve surgery. The surgical options comprise
tricuspid valve reconstruction and tricuspid valve replacement. In
tricuspid valve endocarditis, both options are applicable. However,
the main limitation of tricuspid valve replacement was the need for
long-term anticoagulation, which would be a major problem for
performing heart surgery, as well as for performing allo-SCT in our
patient. In case of the latter condition, data are limited, as
there is only one reported case of allo-SCT being performed in a
patient with a prosthetic valve (9).
Another problem is the increased risk of bleeding, infectious
complications and reoperation rates of patients with haematological
malignancies undergoing cardiac surgery (10). In our case, no cardiac complications
occurred, without the need for additional measures during
allo-SCT.
In CML, the incidence of BP is a rare condition.
Optimal outcomes are achieved with allo-SCT after obtaining
complete remission with induction chemotherapy (11). In our patient, complete remission
after induction chemotherapy was an absolute indication for
allo-SCT. However, recent CRKP endocarditis was a challenge when
deciding to perform allo-HSCT. Satlin et al published a
retrospective analysis of 18 malignant haematological patients with
carbapenem-resistant Enterobacteriaceae BSI. In that study, initial
empirical antimicrobial therapy was active in only 11% of the
patients and the mortality rate was 56% (12). In another multicenter retrospective
study, Girmenia et al assessed the epidemiology and
prognostic factors of CRKP infections in an SCT setting. CRKP
infections were reported in 53.4% of the centers and were
documented in 0.4% of autologous and 2% of allogeneic SCTs. CRKP
colonization was followed by an infection in ~30% of the cases. The
infection-related mortality rate was 16% in autologous and 64.4% in
allogeneic SCT. A pre-transplant CRKP infection and an inadequate
first-line treatment were associated with an increased mortality in
allo-SCT patients who developed a CRKP infection. Indeed, despite
the administration of first-line CRKP-targeted antibiotic therapy
(CTAT), 55% of the patients who received CTAT succumbed to the
disease (13). Zuckerman et al
evaluated the eradication of CRKP carrier state in 15 patients
undergoing intensive chemotherapy or SCT. In that study, the
eradication rate was 66% and all the patients in whom eradication
failed succumbed to the disease, usually due to active CRKP
infection (14). According to the
results of Kuruvilla et al, recurrence of endocarditis
during allo-SCT was the worst outcome, exhibiting a very high
mortality rate (15). For these
reasons, we decided to reduce the transplantation-associated risks
with complete eradication of the endocarditis and the CRKP
infection prior to the transplantation, and opted for performing a
less invasive surgery rather than a mechanical tricuspid valve,
which would require a higher level of anticoagulation. We also
planned to use an RIC regimen instead of myeloablative conditioning
during the transplantation.
In conclusion, we herein report a case of a BP-CML
patient with a highly resistant, CRKP-associated tricuspid valve
endocarditis, who was treated with a combination of systemic
antimicrobial therapy and surgical valve repair, and subsequently
underwent successful allo-SCT. To the best of our knowledge, this
is the first reported CRKP tricuspid valve endocarditis and the
first reported case of CRKP endocarditis that proceeded to undergo
a successful allo-SCT in the medical literature. This report
demonstrated that extensively resistant CRKP endocarditis may be
treated with combination therapy without mechanical heart valve
replacement in patients with haematological malignancies. Our case
also emphasises the significance of a collaborative
multidisciplinary approach in such patients.
References
|
1
|
Doi Y and Paterson DL:
Carbapenemase-producing Enterobacteriaceae. Semin Respir Crit Care
Med. 36:74–84. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Girmenia C, Viscoli C, Piciocchi A,
Cudillo L, Botti S, Errico A, Sarmati L, Ciceri F, Locatelli F,
Giannella M, et al: Management of carbapenem resistant Klebsiella
pneumoniae infections in stem cell transplant recipients: An
Italian multidisciplinary consensus statement. Haematologica.
100:e373–e376. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Vardakas KZ, Matthaiou DK, Falagas ME,
Antypa E, Koteli A and Antoniadou E: Characteristics, risk factors
and outcomes of carbapenem-resistant Klebsiella pneumoniae
infections in the intensive care unit. J Infect. 70:592–599. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Girometti N, Lewis RE, Giannella M,
Ambretti S, Bartoletti M, Tedeschi S, Tumietto F, Cristini F,
Trapani F, Gaibani P and Viale P: Klebsiella pneumoniae bloodstream
infection: Epidemiology and impact of inappropriate empirical
therapy. Medicine (Baltimore). 93:298–309. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Anderson MJ and Janoff EN: Klebsiella
endocarditis: Report of two cases and review. Clin Infect Dis.
26:468–474. 1998. View
Article : Google Scholar : PubMed/NCBI
|
|
6
|
Srinivas KH, Sharma R, Agrawal N and
Manjunath CN: Silent destruction of aortic and mitral valve by
Klebsiella pneumoniae endocarditis. BMJ Case Rep.
2013.pii:bcr2013200704, 2013.
|
|
7
|
Yong MS, Coffey S, Prendergast BD, Marasco
SF, Zimmet AD, McGiffin DC and Saxena P: Surgical management of
tricuspid valve endocarditis in the current era: A review. Int J
Cardiol. 202:44–48. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Satlin MJ, Jenkins SG and Walsh TJ: The
global challenge of carbapenem-resistant Enterobacteriaceae in
transplant recipients and patients with hematologic malignancies.
Clin Infect Dis. 58:1274–1283. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Prébet T, Devillier R, Fürst S, Vey N and
Blaise D: Allogeneic hematopoietic SCT and mechanical heart valve:
Feasibility of reduced toxicity myeloablative conditioning. Bone
Marrow Transplant. 45:1574–1575. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Fecher AM, Birdas TJ, Haybron D, Papasavas
PK, Evers D and Caushaj PF: Cardiac operations in patients with
hematologic malignancies. Eur J Cardiothorac Surg. 25:537–540.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Saußele S and Silver RT: Management of
chronic myeloid leukemia in blast crisis. Ann Hematol. 94(Suppl 2):
S159–S165. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Satlin MJ, Calfee DP, Chen L, Fauntleroy
KA, Wilson SJ, Jenkins SG, Feldman EJ, Roboz GJ, Shore TB, Helfgott
DC, et al: Emergence of carbapenem-resistant Enterobacteriaceae as
causes of bloodstream infections in patients with hematologic
malignancies. Leuk Lymphoma. 54:799–806. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Girmenia C, Rossolini GM, Piciocchi A,
Bertaina A, Pisapia G, Pastore D, Sica S, Severino A, Cudillo L,
Ciceri F, et al: Infections by carbapenem-resistant Klebsiella
pneumoniae in SCT recipients: A nationwide retrospective survey
from Italy. Bone Marrow Transplant. 50:282–288. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zuckerman T, Benyamini N, Sprecher H,
Fineman R, Finkelstein R, Rowe JM and Oren I: SCT in patients with
carbapenem resistant Klebsiella pneumoniae: A single center
experience with oral gentamicin for the eradication of carrier
state. Bone Marrow Transplant. 46:1226–1230. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kuruvilla J, Forrest DL, Lavoie JC, Nantel
SH, Shepherd JD, Song KW, Sutherland HJ, Toze CL, Hogge DE and
Nevill TJ: Characteristics and outcome of patients developing
endocarditis following hematopoietic stem cell transplantation.
Bone Marrow Transplant. 34:969–973. 2004. View Article : Google Scholar : PubMed/NCBI
|