Introduction
Renal cell carcinoma (RCC) is a common malignancy,
of which there were ~12,600 cases in 2015 in Italy (1). It represents 3% of all adult
malignancies in this region, and is the third most frequent
urologic malignancy after prostate and bladder cancer (2). RCC accounts for 90% of kidney cancer
cases, and ~80% of these are clear cell carcinomas (3,4). The
majority of cases of renal cancer are asymptomatic and are
diagnosed incidentally, due to more extensive use of diagnostic
imaging, whereas the classic triad of haematuria, flank pain and
palpable abdominal mass are rarely the first symptoms of
presentation, occurring in 4–17% of cases (5,6).
On occasion, the symptoms occurring due to the
presence of intestinal metastasis may be the first presentation of
renal cancer (7,8). These symptoms usually include nausea,
abdominal pain, intussusception, weight loss, melena, bowel
perforation, and primarily, gastrointestinal bleeding caused by the
infiltration of intestinal vessels (9).
The current study presents the case of a 75-year old
male in which severe anaemia due to bowel bleeding and abdominal
pain from recurrent bowel intussusceptions were the first
presentations of metastatic renal cell carcinoma. A review of the
cases of bowel metastasis from renal cell carcinoma described in
the literature from 2006 to the present was also conducted
(Table I). Written informed consent
was obtained from the patient for the publication of this case
report and accompanying images.
 | Table I.A review of the cases of bowel
metastasis from renal cell carcinoma. |
Table I.
A review of the cases of bowel
metastasis from renal cell carcinoma.
| First author,
year | Sex Age | Presenting
symptoms | Diagnosis | Anatomic site | Number of polypoid
lesions | Dimensions of the
largest polyp, cm | Interval between
diagnosis of primary tumour and metastasis | Histology | Other involved
organs | Renal vein
invasion |
Intussusception | Treatment | Overall
survival | (Refs.) |
|---|
| Sasaki, 2006 | M 64 | Abdominal pain | CT | Small bowel | 2 | 3.5×3.5 | 11 years | Clear cell | Lung | NA | Yes (ileum) | Surgical resection
of ileum and jejunum | Few months | (42) |
| Roviello, 2006 | M 48 | Melena, anaemia,
bowel obstruction | CT | Jejunum | 2 | 4.5×4.5 | 2 years | Clear cell | Lung Brain | NA | Yes (jejunum) | Surgical resection
of small bowel | Alive after 24
months | (13) |
| Rampersad,
2006 | F 69 | Bowel
obstruction | Laparotomy | Ileum | 1 | 2×3 | 3 months | NA | NA | NA | Yes (ileum) | Surgery | NA | (49) |
| Bathia, 2006 | M 55 | Jaundice Abdominal
mass | Endoscopy | Duodenum | 1 | 4×4 | 1 years | Clear cell | Liver | Renal vein | No | Polypectomy | NA | (15) |
| Bahli, 2007 | F 65 | Bowel
obstruction | CT | Jejunum | 1 | NA | 1 years | NA | No | No | No | Surgery | NA | (50) |
| Sridhar, 2008 | M 71 | Vomit Bowel
obstruction | CT | Ileum | 1 | 3.9×3.4 | 7 years | Clear cell | Liver Lung Hilar
lymph nodes | Renal vein,
inferior vena cava | No | Surgical resection
of small bowel | 21 months | (18) |
| Eo, 2008 | M 47 | Abdominal pain | CT | Jejunum | 8 | 4.3×3.5 | 9 months | Clear cell | Lung | NA | Yes (jejunum) | Surgical resection
of jejunum | Alive after 10
months | (51) |
| Tutar, 2008 | M 59 | Abdominal pain
Vomit | CT | Jejunum | Multiple | 3 | 8 years | Clear cell | Lung Brain | NA | Yes (jejunum) | Surgery | NA | (33) |
| Cherian, 2011 | M 80 | Syncope, Melena
Anaemia | CT | Duodenum | 1 | NA | 11 years | Clear cell | Lung Bone | Renal vein | No | Therapy
(sorafenib) | 10 months | (28) |
| Rustagi, 2011 | M 66 | Bleeding, anaemia,
melena | Endoscopy | Duodenum | 1 | 7×4 | 13 years | Clear cell | No | No | No | Surgery | 2 weeks | (52) |
| Vazquez, 2011 | M 68 | Melena | Endoscopy | Jejunum | 1 | NA | 1 year | Clear cell | NA | NA | No | NA | NA | (53) |
| Takeda, 2011 | M 75 | Bleeding | Endoscopy | Jejunum | 1 | 0.12×0.17 | 6 years | Clear cell | Gluteus bone | NA | No | Surgery | Alive after 6
months | (16) |
| Vashi, 2011 | M 53 | Melena,
anaemia | Endoscopy | Small bowel | 70 | 2 | 2 weeks | Clear cell | – | Renal vein | No | laparotomy
polypectomy | NA | (17) |
| Yang, 2012 | F 72 | Melena,
hematemesis, fatigue | CT | Duodenum | 1 | 3×5 | 10 years | Clear cell | Lung Pancreas | NA | No | Surgery | NA | (54) |
| Zhao, 2012 | M 56 | Melena, vomit
fatigue | Endoscopy | Duodenum | 1 | 4.3 | 5 years | Clear cell | Pancreas | NA | No | Surgery | Alive after 18
months | (55) |
| Kerkeni, 2012 | M 32 | Bowel
obstruction | CT | Ileum | 1 | 2 | 17 months | Clear cell | No | NA | Yes
(ileo-colic) | Surgery | 1 month | (56) |
| Aissa, 2012 | M 64 | Bowel
obstruction | CT | Small bowel | Multiple | NA | 1 year |
Tubulo-papillary | NA | NA | Yes | Surgery | NA | (57) |
| Longo, 2013 | F 52 | Anaemia | CT | Ileum | 2 | 7 | 4 years | Clear cell | Lung big toe | NA | Yes | Surgery | >36 months | (58) |
| Hegde, 2014 | M 52 | Vomit Bowel
obstruction | CT | Ileum | 1 | 2.3×2.0 | – | Clear cell | No | Intrarenal
venous | Yes
(ileo-ileum) | Surgery | NA | (8) |
| Staderini,
2015 | M 70 | Subcutaneous
nodules | CT | Sigmoid colon | Multiple | 4 | – | Clear cell | Peritoneum, Lung
subcutaneous | NA | No | Surgery Pazopanib
and sunitinib | Alive after 36
months | (7) |
| Ismail, 2015 | M 66 | Vomit, Abdominal
pain | CT | Jejunum | 1 | 4 | 19 years | Clear cell | No | NA | No | Surgery | Alive after 18
years | (59) |
| Gorsky, 2015 | M 82 | Syncope,
bleeding | Endoscopy | Jejunum/ileum | 3 | NA | 6 years | NA | Lymph nodes | Renal vein | No | NA | NA | (60) |
| Budmiger, 2015 | M 61 | Vomit, abdominal
pain, melena | CT | Jejunum | 5 | 4.5 | 3 years | Clear cell | Lung Lymph
nodes | NA | Yes
(jejuno-jejunal) | Surgery | NA | (61) |
| Geramizadeh,
2015 | M
61 | Melena | Endoscopy | Duodenum | 1 | 7X5 cm | 16 years | Clear cell | No | NA | no | Surgery | Alive | (62) |
| Trojaniello,
2016 | M 77 | Anaemia | CT | Jejunum/ileum | 23 | 8×5 cm | No | Clear cell | No | No | Yes
(jejunum-jejunal) | Surgery | 12 months | Present case |
Case presentation
In February 2014, a 75-year old male presented to
San Paolo Hospital (Naples Italy) emergency department with
symptoms and signs of severe anaemia: Tachycardia, pallor, fatigue
and hypotension. The patient's medical history was relevant for
chronic gastritis, prostate cancer, diabetes mellitus and
Parkinson's disease, recurrent abdominal pain and constipation.
Laboratory tests revealed severe anaemia (haemoglobin level, 5.6
g/dl, normal range 14–18 g/dl) that required a transfusion of
packed red blood cells. At rectal examination, tarry stools
compatible with melena were evident and an
esophagogastroduodenoscopy was performed, but was negative for
bleeding lesions. Abdominal ultrasound revealed the presence of a
lesion of 35 mm in the lower pole of the left kidney suspicious for
a neoplastic lesion and thickening of the bowel loops into the
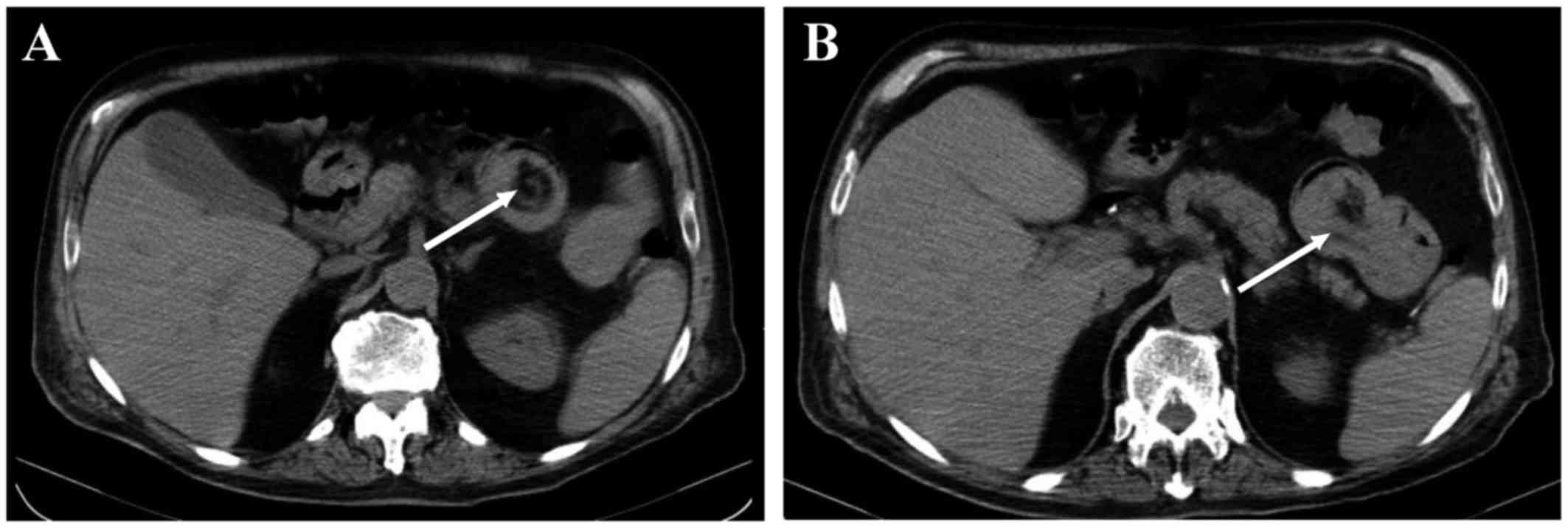
abdomen centre. These findings were further detailed with a total
body computerized tomography (CT) scan that confirmed the
neoplastic lesion of the left kidney and revealed thickening of the
wall of the jejunal loops with target lesions.
The CT scan revealed the requirement for a
colonoscopy, which was negative. During hospitalization, numerous
red blood transfusions were required for the persistence and
worsening of anaemia. Technetium-labelled erythrocyte scintigraphy
was performed to localize the site of acute gastrointestinal
bleeding. It exhibited accumulation in proximity to the lower pole
of the right kidney extending to the right iliac fossa for
peristaltic transportation; these findings identified the jejunal
loops as the source of bleeding (Fig.
1).
Therefore, the patient underwent an exploratory
laparotomy, which determined multiple jejuno-jejunal
intussusceptions with a number of pedunculated polypoid formations
that occupied all the jejunum, with dimensions ranging between 1
and 8 cm. There was also a pedunculated polypoid formation in the
distal ileum. A small neoplastic lesion of the lower pole of the
left kidney was identified using palpation. Resection of the
jejunum with side- to-side anastomosis was performed. The
postoperative course was uneventful without complications.
Macroscopic examination of the jejunal segment
revealed 23 polyps, covered with eroded mucosa (the largest
measuring 8×5 cm), with a yellow-grey colour when dissected
(Fig. 2). Histopathology tests
revealed cellular elements with abundant eosinophilic cytoplasm,
atypical nuclei with aspects of signet ring cell, atypical mitotic
figures and angioinvasion, which were positive for cytokeratin,
vimentin and Wilms cancer protein. The definitive diagnosis was
metastases from high-grade renal cell carcinoma. Metastases were
also identified in 5/40 removed lymph nodes. The patient was
discharged 10 days after surgery without any complications. The
multidisciplinary team decided to begin only best supportive care,
due to the patient's comorbidity, old age and poor performance
status. The patient succumbed to mortality in December 2014, nine
months following surgery.
Discussion
Between 25 and 30% of patients are found to have
metastases at diagnosis, and a further 30–50% of patients with
local disease will develop metastases during the course of their
illness (10). Approximately 60% of
kidney cancer cases are diagnosed incidentally, as a direct result
of the more extensive use of diagnostic imaging in patients not
suspected for renal cancer (11,12).
The sizes of primary tumours are not associated with
the risk of metastasis. The major sites of kidney cancer metastasis
are lung (75%), bone (20%), lymph nodes (11%), liver (18%), and
brain (8%) but virtually all organs may be affected (7). However, intestinal metastasis is rare
and usually occurs when there is widespread dissemination of the
primary cancer. In the current case, bowel metastases were the only
site of metastases from RCC. The present study examined the
literature for cases of bowel metastasis from RCC published from
2006 to present, and identified 24 case reports (Table I).
Symptoms of bowel metastases from RCC usually
include nausea, abdominal pain, intussusception, weight loss,
melena, bowel perforation (9)
gastrointestinal bleeding (due to the invasion of the intestinal
vessels by the disease), which in the reported cases represented
~55.6% of the onset of manifestations of intestinal metastasis from
RCC, and symptoms of intestinal obstruction due to the presence of
a mass within the intestinal wall (12), which in the current review was found
to be present in 50% of patients.
However, there is a delay in diagnosis in the
identification of metastases to the small intestine. Certain
patients with gastrointestinal bleeding remain undiagnosed even
following upper endoscopy and colonoscopy in, as these regions are
challenging to access for diagnosis (13) and traditional methods of
investigating the small intestine such as barium follow-through and
CT have a low yield for cancer detection. Abdominal CT is only able
to reveal a thickening of the intestinal wall and a fold in the
intestine (14), and is frequently
unable to determine the cause, as in the present review, in which
the diagnosis of metastases to the small intestine is performed in
65% of cases.
Diagnosis of small bowel metastasis in RCC is most
frequently performed by upper enteroscopy with tissue sampling,
where the lesion can be detected as an ulcer, submucosal mass with
ulceration or multiple nodules or small polyps of varying sizes
(15). Capsule endoscopy (CE) is a
simple, safe, and comfortable diagnostic technique, but does not
allow biopsies and it is not performed when intussusception is
suspected. On the other hand, double balloon enteroscopy (DBE) is a
useful method for histological confirmation of small bowel lesions.
Using the combination of CE and DBE, it is possible to obtain clear
endoscopic images of the lesions and histological diagnosis prior
to the patient undergoing surgery. CE is a reliable approach to
such screening, and DBE is an effective approach to the
histological diagnosis of small intestinal neoplasms (16,17).
The duration of the interval between initial
nephrectomy and presentation of intestinal metacronous metastases
ranges from 3 months to 20 years, and correlates with overall
survival (12,18–20). The
mean time from nephrectomy to metastatic recurrence is 8 years, and
~11% of metastases occur after ≥10 years (21). Few cases of renal cancer present with
synchronous bowel metastasis, including the current case.
Small bowel intraluminal metastases from renal cell
cancer are unusual (2–4%) (22) and
autopsy cases revealed an incidence of 0.7–14.6% (23,24).
Several mechanisms may be hypothesized including: Peritoneal
dissemination, direct spread from an intra-abdominal malignancy,
haematogenous and lymphatic spread (25). Haematogenous dissemination from the
pulmonary circulation appears to have an important role in the
metastatic spread of RCC to the intestine (26) and the majority of patients with
intestinal metastases have lung involvement (9).
Males are more commonly affected (male:
female=1.5:1) and the incidence of metastasis from RCC increases
with age (12). In the current
review, males were more commonly affected (22 M vs. 4F; ratio 5:1).
The mean age at diagnosis of metastasis was 61 years (median age,
61; range, 32–86 years). The possible aetiology of extensive small
bowel metastasis presenting as polyposis, may be transient
showering of multiple tumour emboli in the celiac and mesenteric
arteries (17). The cases of
isolated intestinal metastases were rare, and generally the
metastases are also present in other organs (27). In the case of right-sided RCC, the
probability of duodenal metastasis is always higher due to the
greater risk of loco-regional invasion (28). Intestinal metastases occur equally in
the jejunum and the ileum (usually present with intestinal bleeding
due to tumoral invasion of intestinal vessels) (18); however, certain studies, including
38% of those reviewed in the current study, indicate the jejunum as
the most frequent area of intestinal metastases (13). In the present review, only one case
of metastasis to the colon sigmoid was identified. The average
number of metastatic intestinal polyps usually present as a result
of RCC is 2 (as is evidenced in our review); the only 2 cases that
have been reported in the literature for 10 years to date are the
case report of Vashi et al (17) with 70 polyps and the current case
with 23 polyps, of which the largest was 8×5 cm in size, the
largest detected in any of the reviewed cases.
The most suitable treatment for metastases of the
small intestine from RCC remains controversial, and is dependent on
several factors, including clinical conditions, comorbidities, free
interval between nephrectomy and metastasis, the number, location
and resectability of metastases (29). Surgery must be considered not only to
palliate symptoms, but also as it may lead to improved overall
survival (30). In fact, the
complete removal of secondary lesions aids the improvement of the
prognosis of patients with metastatic RCC (30). A recent retrospective case series has
revealed a benefit in terms of cancer specific survival (CSS) in
favour of the complete resection of metastases (CSS, 4.8 vs. 1.3
years) regardless of the sites of disease and time of onset
(30). The patient in the current
case report did not undergo radical surgery of metastatic lesions
due to distant locations; however, surgery was performed to control
the complication of bowel bleeding.
On occasion, symptoms of metastases from RCC
presentations are secondary to the phenomena of
sub-occlusion/occlusion due to the phenomenon of intussusception,
which is rare in adults and accounts for 1% of all bowel
obstruction cases (31).
Intussusceptions are more frequent in the jejunum and ileum, and
detection of an intestinal intussusception in patients with RCC
must always raise suspicion of a secondary metastasis in the small
intestine (32,33). The management of adult
intussusception remains controversial; however, metastasectomy may
extend patient survival (34).
Therefore, surgical resection of the involved intestinal segment
has been recommended as the treatment of choice (35,36). The
diagnosis of intussusception is complex, but in the majority of
cases CT allows the diagnosis of the presence of an intraluminal
soft-tissue density within the lumen of the bowel, the
intussuscepted hernia, referred to as the ‘target’ sign, which is
associated with the presence of eccentric mesenteric fat and
vessels and is considered a pathognomonic sign of intussusception
on CT images (37).
Other authors instead identify other equally valid
diagnostic methods, including barium enema, abdominal ultrasound,
plain film X-rays and radionucleotide studies (38–40) and
colour Doppler ultrasound may be used to evaluate the vascularity
of the intussusception and to predict bowel viability (41). However, the diagnosis can be too
challenging to determine preoperatively, and is performed only
during the surgical examination. Colonoscopy and sigmoidoscopy are
usually nondiagnostic (19).
At present, there have been few case reports
detailing intussusceptions of the small intestine secondary to RCC
(19,42–46),
with only one another case (in addition to the present case) of
multiple intussusception of the small intestine (19). Unlike in children, intussusceptions
in adults are more often associated with underlying diseases
(47). Intussusceptions may develop
either from the small or the large intestine, but the aetiology is
variable. Intussusception of the small intestine is usually
secondary to benign lesions, whereas those of the large intestine
are more frequently associated with malignant lesions (47,48).
Patients who are not candidates for radical
resection of metastatic lesions must be treated with targeted
therapy. The standard first line treatment for metastatic renal
cell carcinoma is bevacizumab (combined with interferon-α),
sunitinib or pazopanib for patients with good or intermediate
prognosis and temsirolimus or sunitinib for patients with poor
prognosis. The choice of treatment must account for the
characteristics of the disease (tumour burden and histotype), of
patients (performance status, age, comorbidities) and drug safety.
In the current case, the patient was not candidate for first line
treatment due to comorbidity, age and poor performance status.
In conclusion, the present case report highlights
the importance of vigilance and a high index of suspicion in
patients with renal cancer history upon presentation of new
clinical symptoms. Appropriate awareness, recognition and
aggressive work-up of gastrointestinal symptoms in these patients
are of paramount importance. This case report focuses on two
aspects that must be considered. Firstly, an accurate diagnosis
must be obtained upon presentation of a particular sign/symptom, in
this case anaemia. The present study recommends investigating the
possibility of small intestinal metastases in cases of intestinal
bleeding or anaemia with iron deficiency in patients with a history
of malignant tumour, using endoscopy or CT. Secondly, based on
clinical conditions and comorbidities and following an accurate
tumour staging, it is important to identify the potential for a
radical resection of intestinal metastases that may lead to symptom
control and to a prolonged survival, particularly if an active
therapy is possible.
References
|
1
|
I numeri del cancro in Italia.
2014.https://www.registri-tumori.it
|
|
2
|
Maldazys JD and deKernion JB: Prognostic
factors in metastatic renal carcinoma. J Urol. 136:376–379. 1986.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Moch H, Gasser T, Amin MB, Torhorst J,
Sauter G and Mihatsch MJ: Prognostic utility of the recently
recommended histologic classification and revised TNM staging
system of renal cell carcinoma: A Swiss experience with 588 tumors.
Cancer. 89:604–614. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Leibovich BC, Lohse CM, Crispen PL,
Boorjian SA, Thompson RH, Blute ML and Cheville JC: Histological
subtype is an independent predictor of outcome for patients with
renal cell carcinoma. J Urol. 183:1309–1315. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Waters WB and Richie JP: Aggressive
surgical approach to renal cell carcinoma: Review of 130 cases. J
Urol. 122:306–309. 1979. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Griffiths LH and Thackray AC: Parenchymal
carcinoma of the kidney. Br J Urol. 21:128–151. 1949. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Staderini F, Cianchi F, Badii B, Skalamera
I, Fiorenza G, Foppa C, Qirici E and Perigli G: A unique
presentation of a renal clear cell carcinoma with atypical
metastases. Int J Surg Case Rep. 11:29–32. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hegde RG, Gowda HK, Agrawal RD, Yadav VK
and Khadse GJ: Renal cell carcinoma presenting as small bowel
obstruction secondary to a metastatic ileal intussusception. J
Radiol Case Rep. 8:25–31. 2014.PubMed/NCBI
|
|
9
|
Nozawa H, Tsuchiya M, Kobayashi T, Morita
H, Kobayashi I, Sakaguchi M, Mizutani T, Tajima A, Kishida Y,
Yakumaru K, et al: Small intestinal metastasis from renal cell
carcinoma exhibiting rare findings. Int J Clin Pract. 57:329–331.
2003.PubMed/NCBI
|
|
10
|
Pavlakis GM, Sakorafas GH and
Anagnostopoulos GK: Intestinal metastases from renal cell
carcinoma: A rare cause of intestinal obstruction and bleeding. Mt
Sinai J Med. 71:127–130. 2004.PubMed/NCBI
|
|
11
|
Klatte T, Patard JJ, de Martino M,
Bensalah K, Verhoest G, de la Taille A, Abbou CC, Allhoff EP,
Carrieri G, Riggs SB, et al: Tumor size does not predict risk of
metastatic disease or prognosis of smal renal cell carcinomas. J
Urol. 179:1719–1726. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Decastro GJ and McKiernan JM:
Epidemiology, clinical staging, and presentation of renal cell
carcinoma. Urol Clin North Am. 35:581–592, vi. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Roviello F, Caruso S, Moscovita Falzarano
S, Marrelli D, Neri A, Rampone B, De Marco G, Perrotta ME and
Mariani F: Small bowel metastases from renal cell carcinoma: A rare
cause of intestinal intussusception. J Nephrol. 19:234–238.
2006.PubMed/NCBI
|
|
14
|
Honda W, Ohmiya N, Hirooka Y, Nakamura M,
Miyahara R, Ohno E, Kawashima H, Itoh A, Watanabe O, Ando T and
Goto H: Enteroscopic and radiologic diagnoses, treatment, and
prognoses of small-bowel tumors. Gastrointest Endosc. 76:344–354.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Bhatia A, Das A, Kumar Y and Kochhar R:
Renal cell carcinoma metastasizing to duodenum: A rare occurrence.
Diagn Pathol. 1:292006. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Takeda T, Shibuya T, Osada T, Izumi H,
Mitomi H, Nomura O, Suzuki S, Mori H, Matsumoto K, Kon K, et al:
Metastatic renal cell carcinoma diagnosed by capsule endoscopy and
double balloon endoscopy. Med Sci Monit. 17:CS15–CS17. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Vashi PG, Abboud E and Gupta D: Renal cell
carcinoma with unusual metastasis to the small intestine
manifesting as extensive polyposis: Successful management with
intraoperative therapeutic endoscopy. Case Rep Gastroenterol.
5:471–478. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Sridhar SS, Haider MA, Guindi M and Moore
MJ: A case of small bowel obstruction due to intraluminal
metastases from metastatic renal cell cancer. Oncologist. 13:95–97.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Deguchi R, Takagi A, Igarashi M, Shirai T,
Shiba T, Watanabe S, Kurumada T, Miwa T, Sadahiro S and Yasuda M: A
case of ileocolic intussusception from renal cell carcinoma.
Endoscopy. 32:658–660. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Van der Poel HG, Roukema JA, Horenblas S,
van Geel AN and Debruyne FM: Metastasectomy in renal cell
carcinoma: A multicenter retrospective analysis. Eur Urol.
35:197–203. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Adamo R, Greaney PJ Jr, Witkiewicz A,
Kennedy EP and Yeo CJ: Renal cell carcinoma metastatic to the
duodenum: Treatment by classic pancreaticoduodenectomy and review
of the literature. J Gastrointest Surg. 12:1465–1468. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Farthouat P, Faucompret S, Louis C,
Debourdeau P, Pero C and Breda Y: Gastrointestinal hemorrhage due
to jejunal metastases from kidney cancer. Ann Chir. 125:797–798.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
DeCastro CA, Dockerty MB and Mayo CW:
Metastatic tumors of the small intestines. Surg Gynecol Obstet.
105:159–165. 1957.PubMed/NCBI
|
|
24
|
Saitoh H, Nakayama M, Nakamura K and Satoh
T: Distant metastasis of renal adenocarcinoma in nephrectomized
cases. J Urol. 127:1092–1095. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Loualidi A, Spooren PF, Grubben MJ,
Blomjous CE and Goey SH: Duodenal metastasis: An uncommon cause of
occult small intestinal bleeding. Neth J Med. 62:201–205.
2004.PubMed/NCBI
|
|
26
|
Saitoh H: Distant metastasis of renal
adenocarcinoma. Cancer. 48:1487–1491. 1981. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Smith SJ, Carlson HC and Gisvold JJ:
Secondary neoplasms of the small bowel. Radiology. 125:29–33. 1977.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Cherian SV, Das S, Garcha AS, Gopaluni S,
Wright J and Landas SK: Recurrent renal cell cancer presenting as
gastrointestinal bleed. World J Gastrointest Oncol. 3:99–102. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Herrans AF, Diez CJ and Garcìa BJ:
“Factores pronósticos en el ade-nocarcinoma de riñón”. Tumores de
riñón. Ediciones Doyma. Madrid. 2001.
|
|
30
|
Alt AL, Boorjian SA, Lohse CM, Costello
BA, Leibovich BC and Blute ML: Survival after complete surgical
resection of multiple metastases from renal cell carcinoma. Cancer.
117:2873–2882. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Coleman MJ, Hugh TB, May RE and Jensen MJ:
Intussusception in the adult. Aust N Z J Surg. 51:179–181. 1981.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Karahan N, Bozkurt KK, Cırış IM, Songür Y,
Akin M, Cetın M and Koşar A: Duodenojejunal invagination caused by
small bowel metastasis of renal cell carcinoma. Turk J
Gastroenterol. 22:355–357. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Tutar NU, Töre HG, Aydin HM, Geyik E,
Coskun M and Niron EA: Case report: Jejuno-jejunal nvagination from
metastatic renal cell carcinoma. Br J Radiol. 81:e115–e117. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Venugopal A, Mahesh S, Lekha V, Jacob G,
Gandhi MD, Bedi MM, Sharma M, Jacob M and Ramesh H: Intussusception
due to ileal metastases from renal cell carcinoma. Trop
Gastroenterol. 28:35–36. 2007.PubMed/NCBI
|
|
35
|
Tolia BM and Whitmore WF Jr: Solitary
metastasis from renal cell carcinoma. J Urol. 114:836–838. 1975.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Eo WK, Kim GY and Choi SI: A case of
multiple intussusceptions in the small intestine caused by
metastatic renal cell carcinoma. Cancer Res Treat. 40:97–99. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Gayer G, Zissin R, Apter S, Papa M and
Hertz M: Pictorial review: Adult intussusception-a CT diagnosis. Br
J Radiol. 75:185–190. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Bar-Ziv J and Solomon A: Computed
tomography in adult intussusception. Gastrointest Radiol.
16:264–266. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Iko B, Teal J, Siram SM, Chinwuba CE, Roux
VJ and Scott VF: Computed tomography of adult colonic
intussusception: Clinical and experimental studies. AJR Am J
Roentgenol. 143:769–772. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Montali G, Croce F, De Pra L and Solibiati
L: Intussusception of the bowel: A new sonographic pattern. Br J
Radiol. 56:621–623. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Verschelden P, Filiatrault D, Garel L,
Grignon A, Perreault G, Boisvert J and Dubois J: Intussusception in
children: Reliability of US in diagnosis-a prospective study.
Radiology. 184:741–744. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Sasaki M, Murakami Y, Takesue Y, Yokoyama
Y, Morifuji M, Hayashidani Y, Koyama M and Sueda T: Double
intussusceptions in the small intestine caused by metastatic renal
cell carcinoma: Report of a case. Surg Today. 36:85–88. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Johnson WA and Straus FH: Intussusception
of the small intestine produced by metastatic renal carcinoma.
Surgery. 32:991–996. 1952.PubMed/NCBI
|
|
44
|
Haynes IG, Wolverson RL and O'Brien JM:
Small bowel intussusception due to metastatic renal carcinoma. Br J
Urol. 58:4601986. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Khan AB: Ileocaecal intussusception due to
metastatic renal carcinoma. Br J Urol. 67:657–658. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Savoye-Collet C, Thoumas D, Dunet F,
Lemercier E, Benozio M and Dacher JN: CT diagnosed jejunal
intussusception revealing metastatic renal cell carcinoma. JBR-BTR.
84:153–154. 2001.PubMed/NCBI
|
|
47
|
Gayer G, Zissin R, Apter S, Papa M and
Hertz M: Pictorial review: Adult intussusception-a CT diagnosis. Br
J Radiol. 75:185–190. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Begos DG, Sandor A and Modlin IM: The
diagnosis and management of adult intussusception. Am J Surg.
173:88–94. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Rampersad RD, Ramcharan R and Maharaj D:
Small bowel intussusception: A rare complication of renal cell
carcinoma. West Indian Med J. 55:68–69. 2006.PubMed/NCBI
|
|
50
|
Bahli ZM and Panesar KJ: Solitary jejunal
metastasis from renal cell carcinoma. J Ayub Med Coll Abbottabad.
19:62–63. 2007.PubMed/NCBI
|
|
51
|
Eo WK, Kim GY and Choi SI: A case of
multiple intussusceptions in the small intestine caused by
metastatic renal cell carcinoma. Cancer Res Treat. 40:97–99. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Rustagi T, Rangasamy P and Versland M:
Duodenal Bleeding from metastatic renal cell carcinoma. Case Rep
Gastroenterol. 5:249–257. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Vazquez C, Berrueta J, De Simone F,
Tcheckmedyian A, Gonzalez N, Bernachin J, Perrota A, Curi J, Mariño
A and Olano C: Small-intestinal bleeding due to metastatic renal
cell cancer. Endoscopy. 43 Suppl 2:UCTN:E132011. View Article : Google Scholar
|
|
54
|
Yang J, Zhang YB, Liu ZJ, Zhu YF and Shen
LG: Surgical treatment of renal cell carcinoma metastasized to the
duodenum. Chin Med J. 125:3198–3200. 2012.PubMed/NCBI
|
|
55
|
Zhao H, Han K, Li J, Liang P, Zuo G, Zhang
Y and Li H: A case of wedge resection of duodenum for massive
gastrointestinal bleeding due to duodenal metastasis by renal cell
carcinoma. World J Surg Oncol. 10:1992012. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Kerkeni W, Bouzouita A, Jarraya H, Selmi
MS, Cherif M, Derouich A, Kourda N, Dziri C, Zermani R, Ben Slama
MR and Chebil M: Ileocolic intussusception from metastatic renal
cell carcinoma. Prog Urol. 23:73–75. 2013.(In French). View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Aissa A, Kherifech M, Alouini R, Hajji H
and Stita W: Multiple intussusceptions revealing metastases from
renal carcinoma to the small intestine. J Visc Surg. 149:e223–e224.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Longo R, Gattuso D, Luchetti R, Giannetti
C, Mero A, Bernardi C and Gasparini G: Atypical multiple ileum
metastases of renal cell carcinoma. J Gastrointest Cancer.
44:477–480. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Ismail I, Neuen BL and Mantha M: Solitary
jejunal metastasis from renal cell carcinoma presenting as small
bowel obstruction 19 years after nephrectomy. BMJ Case Rep. pii:
bcr2015210857. 2015. View Article : Google Scholar
|
|
60
|
Gorski RL, Jalil SA, Razick M and Jalil
AA: An obscure cause of gastrointestinal bleeding: Renal cell
carcinoma metastasis to the small bowel. Int J Surg Case Rep.
15:130–132. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Budmiger MA, Nagy V, Hürlimann S and
Metzger J: Triple jejuno-jejunal intussusception due to metastatic
renal cell carcinoma. J Surg Case Rep. 2015:pii: rjv047. 2015.
|
|
62
|
Geramizadeh B, Mostaghni A, Ranjbar Z,
Moradian F, Heidari M and Khosravi MB: An unusual case of
metastatatic renal cell carcinoma presenting as melena and duodenal
ulcer, 16 years after nephrectomy; a case report and review of the
literature. Iran J Med Sci. 40:175–180. 2015.PubMed/NCBI
|