Introduction
Autoimmune diseases including rheumatoid arthritis
are associated with a higher risk of non-Hodgkin lymphoma (1) and the frequency of autoimmune disease
in lymphoma patients was 8.2% (2).
Among autoimmune diseases, combination of immune thrombocytopenia
and autoimmune hemolytic anemia, which is known as Evans syndrome,
may precede lymphoma (3,4). Treatment of these cytopenias is the
same for primary cases although coincident presence of lymphoma is
a clinical problem. Conventional chemotherapy of lymphoma may be
avoided in the presence of severe cytopenia because of the
increased risk of hematological toxicity, however, treatment of
lymphoma may be needed for the few patients with
lymphoma-associated cytopenia.
In the present study, we report a complex case of
thrombocytopenia and hemolytic anemia secondary to CD5-positive
B-cell lymphoma in a patient with massive splenomegaly and
rheumatoid arthritis, which responded to chemotherapy with
bendamustine.
Case report
The present study focused on a 67-year-old Japanese
woman who developed splenomegaly and mild neutropenia after a
20-year course of rheumatoid arthritis which had been in remission
with tofacitinib treatment. In addition, she developed
thrombocytopenia and anemia and tofacitinib was terminated.
Laboratory examination revealed the followings: Reticulocyte
248×109/l, total bilirubin 1.9 mg/dl, lactic
dehydrogenase (LDH) 438 U/l (upper normal limit 223 U/l), direct
anti-globulin test (DAT) negative and platelet-associated
immunoglobulin G 123 ng/107 cells (upper normal limit
46). Peripheral blood smear rarely showed fragmented red cells and
there was no coagulopathy. Bone marrow aspirate and needle biopsy
showed erythroid hyperplasia and no definite lymphoma infiltrates
but several reactive lymphocyte aggregates. Tentative diagnosis of
immune thrombocytopenia (ITP) and DAT-negative hemolytic anemia,
thus DAT-negative Evans syndrome, was made in spite of massive
splenomegaly. Prednisolone 30 mg/day was administered to treat
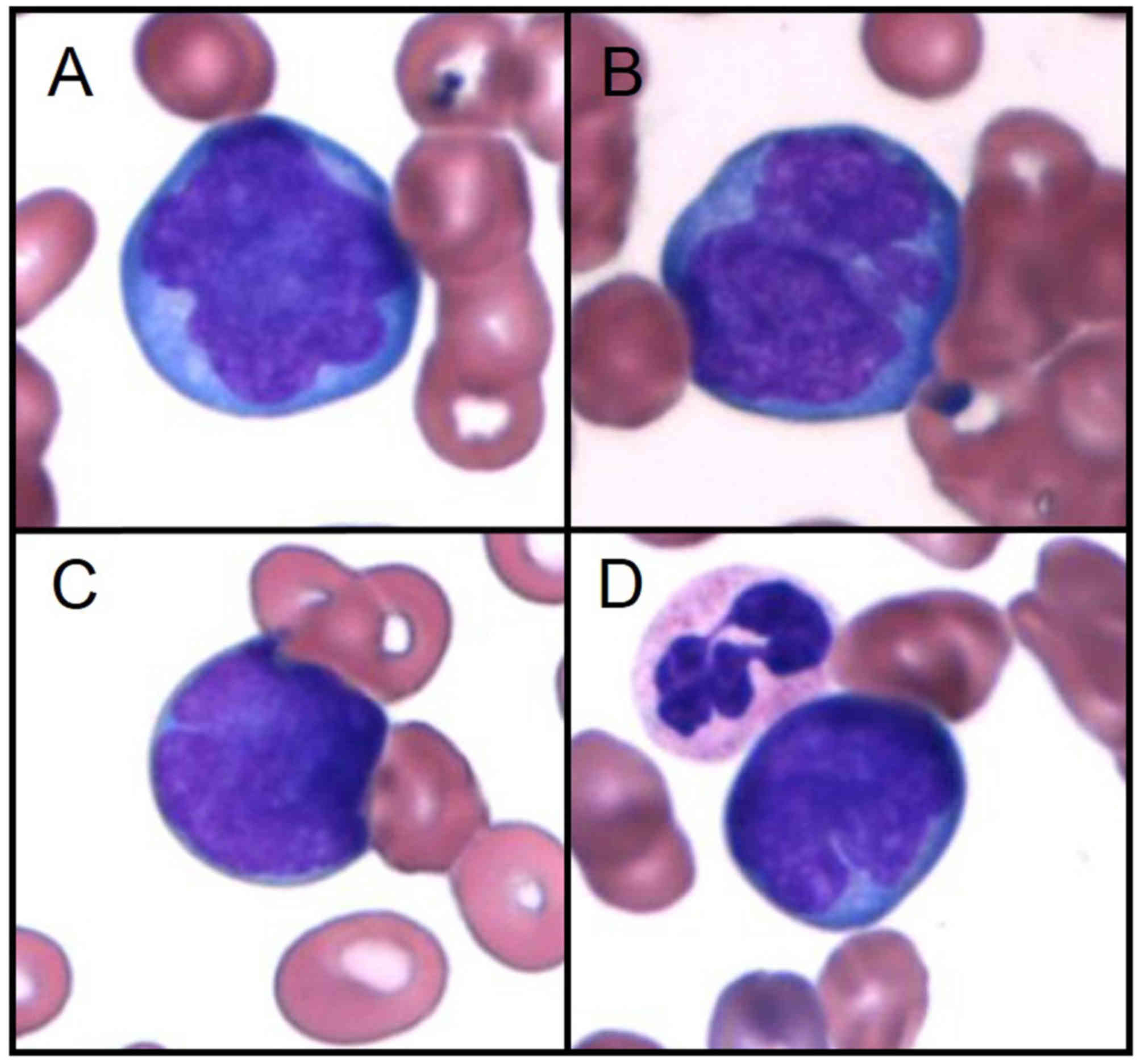
bicytopenia while abnormal lymphocytes appeared in peripheral blood
(Fig. 1). Flow cytometric analysis
showed the presence of monoclonal B-cells expressing CD5, CD19,
CD20, HLA-DR, and surface IgM-λ and partially positive for CD10
without CD23 expression. In addition, fluorescence in situ
hybridization analysis of peripheral blood revealed an increased
number of MYC and IGH signals without any fusion in
40% of mononuclear cells examined, corroborating the result of bone
marrow cytogenetics which revealed later that 2 out of 20 cells
were near-tetraploid cells with complex cytogenetics. Diagnosis of
CD5-positive B-cell lymphoma was made.
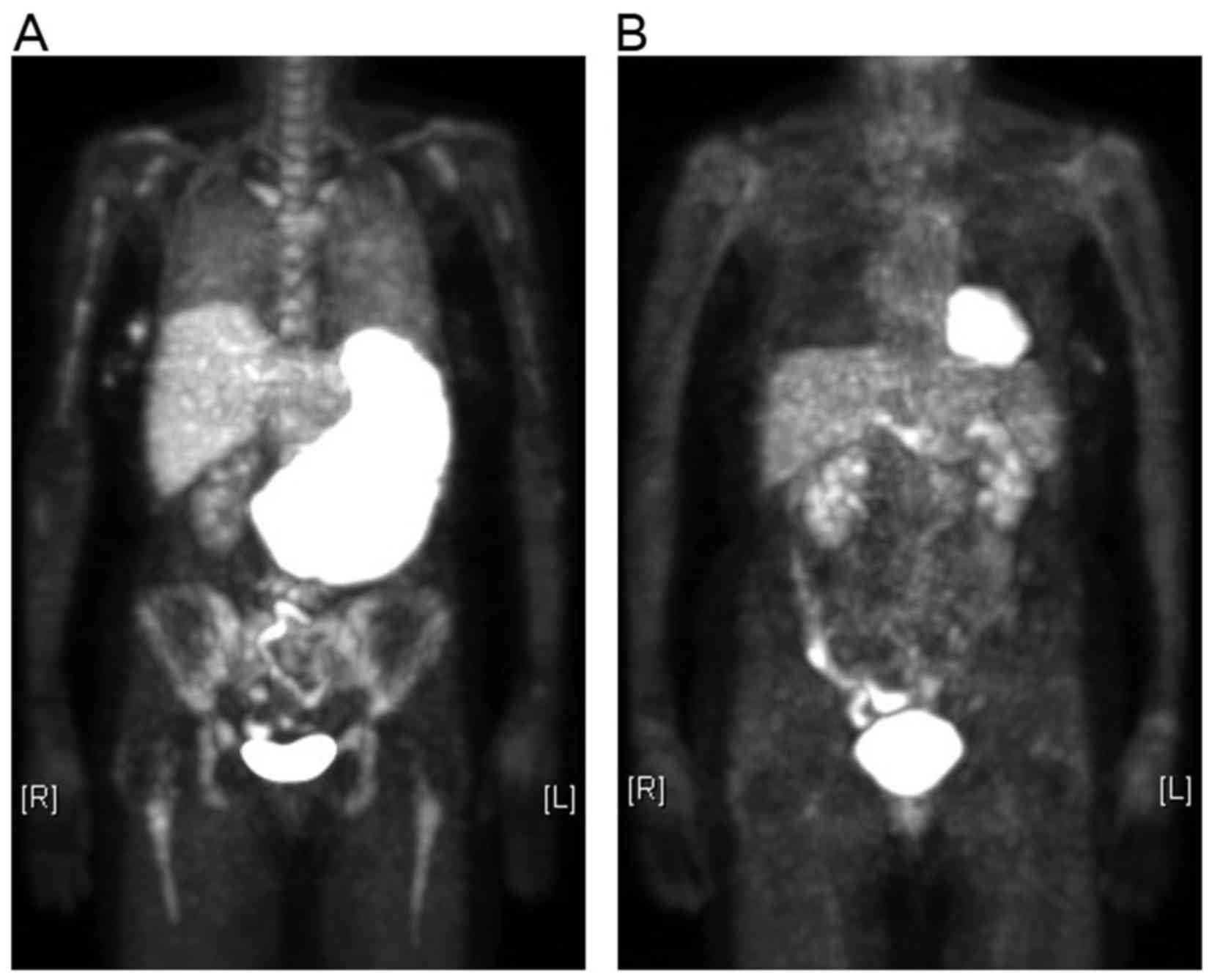
18F-fluorodeoxyglucose (FDG) positron emission
tomography (PET)-computed tomography (CT) showed massive
splenomegaly with high uptake of FDG as well as diffuse FDG uptake
in both lungs and the bone marrow without any abnormal lung shadow
in CT (Fig. 2A), suggesting
intravascular large B-cell lymphoma; hypoxemia developed with
peripheral oxygen saturation 88% (room air). Severe
thrombocytopenia (platelet count <10×109/l)
refractory to platelet transfusion developed and hindered
diagnostic splenectomy or splenic biopsy for histological
determination of lymphoma. We administered high-dose dexamethasone,
high-dose γ-globulin and rituximab along with daily platelet
transfusions and semi-weekly red blood cell transfusions to treat
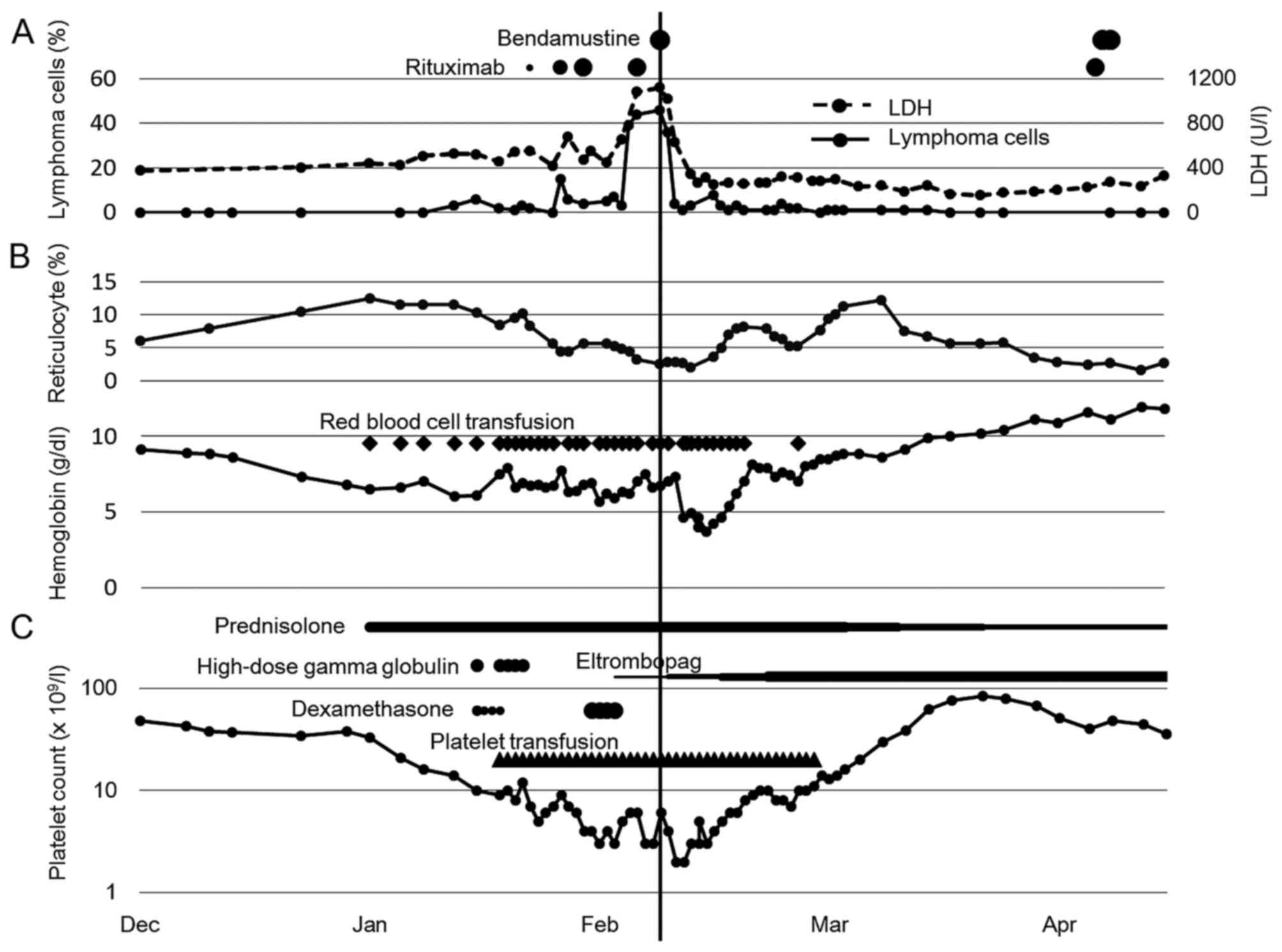
both severe bicytopenia and lymphoma. A transient decrease in
number of lymphoma cells in the peripheral blood was observed after
each dose of rituximab, however, no improvement of bicytopenia
occurred. We administered second high-dose dexamethasone followed
by prednisolone maintenance and start of eltrombopag 12.5 mg/day,
which was planned to be escalated weekly by 12.5 mg per day up to
50 mg per day. Even after 3 doses of rituximab, the number of
peripheral blood lymphoma cells increased as well as serum levels
of LDH as shown in Fig. 3A. Then, we
administered bendamustine 90 mg/m2 once. Due to high
serum levels of total bilirubin (8.8 mg/dl), second dose of
bendamustine was omitted. Severe pancytopenia developed; leukocytes
1.9×109/l, hemoglobin 3.7 g/dl, and platelets
3×109/l at nadir of bone marrow suppression (Fig. 3B and C). Three weeks later,
transfusion-independence for both of erythrocytes and platelets was
obtained while cytomegalovirus antigenemia had become positive and
severe pneumonia had developed. Antiviral, antibiotic and
antifungal treatments were administered successfully to overcome
these complications. Spleen decreased in size and pancytopenia
ultimately disappeared as well as lymphoma cells in the peripheral
blood. She received additional 5 courses of bendamustine plus
rituximab therapy in full doses (5)
and PET-CT scans revealed complete disappearance of FDG uptakes and
splenomegaly (Fig. 2B).
The patient has provided her consent regarding the
publication of the case details. The present study was undertaken
according to a project of clinical surveillance in Tottori
University Hospital, which was approved by the Ethics Committee at
Tottori University Faculty of Medicine (approval no. 2489).
Discussion
Massive splenomegaly may constitute the initial
presentation of lymphoma. In the subset of patients in which
splenomegaly remains unexplained, lymphomas account for the leading
cause and splenectomy is required for a definitive diagnosis
although primary effort must be taken to achieve diagnosis by
integrating presenting clinical and laboratory data with imaging,
peripheral blood, bone marrow assessment, thus trying to avoid
splenectomy for diagnostic purposes (6). In the current case, bone marrow
examination gave no definitive diagnosis and severe
thrombocytopenia hindered diagnostic splenectomy while CD5-positive
monoclonal B cells with bizarre morphology and complex cytogenetics
appeared in the peripheral blood. Taken splenomegaly and diffuse
pulmonary involvement as suggested by the PET-CT scan into
consideration, pulmonary intravascular large B-cell lymphoma is
probable diagnosis (7,8).
Evans syndrome is a rare disease characterized by
the simultaneous and sequential development of autoimmune hemolytic
anemia and ITP and/or immune neutropenia. Michel et al
analyzed the data from 68 patients with Evans syndrome including 3
DAT-negative cases (4). Half of the
patients were associated with an underlying disorder including
lymphoproliferative disorders and two patients with B-cell
non-Hodgkin lymphoma was included (4). The presence of massive splenomegaly
suggested against autoimmune mechanisms underlying bicytopenia in
the current case although the severity of bicytopenia refractory to
multiple transfusions could not negate the presence of immune
dysregulation like Evans syndrome especially because the patient
suffered from rheumatoid arthritis. Whether it was via
immunological mechanisms or not, severe bicytopenia was a clinical
problem confronting lymphoma progression. Park et al
reported a case of DAT-negative Evans syndrome associated with
diffuse large B-cell lymphoma, in which cytopenia preceded lymphoma
and R-CHOP chemotherapy was effective (3). Multirefractory ITP is a serious and
potentially life-threatening condition although chemotherapy may be
needed for the few patients with ITP secondary to lymphoma
(9). In the current case,
prednisolone, high-dose γ-globulin, high-dose dexamethasone,
rituximab and eltrombopag failed to increase platelet counts and
hemoglobin levels. In addition, peripheral lymphoma cells increased
in number and serum levels of LDH elevated despite repeated
rituximab doses. Then, administration of bendamustine successfully
eradicated lymphoma cells from the peripheral blood and increased
platelet counts. Furthermore, anemia, although transiently
aggravated, ultimately disappeared. Bendamustine is effective for
indolent and mantle cell lymphoma (5) and even aggressive lymphoma (10,11).
Bendamustine plus rituximab was better tolerated than R-CHOP with
lower rates of myelotoxicity while higher frequency of grade 3–4
lymphocytopenia was seen in the bendamustine plus rituximab group
(5). Bendamustine may be favored for
patients with lymphoma associated with severe cytopenia because of
less myelotoxicity. Furthermore, lymphotoxicity of bendamustine may
affect autoimmune cytopenia favorably.
In conclusion, we here report a complex case of
severe bicytopenia and B-cell lymphoma in a patient with rheumatoid
arthritis. Bendamustine was successful for both diseases and may be
preferred in case of lymphoma complicated with cytopenia.
Acknowledgements
The present study was supported in part by grants
from Teijin Pharma Ltd., Chugai pharmaceutical Co., Ltd. and Taiho
Pharmaceutical Co., Ltd.
Glossary
Abbreviations
Abbreviations:
|
ITP
|
immune thrombocytopenia
|
|
DAT
|
direct antiglobulin test
|
|
LDH
|
lactic dehydrogenase
|
|
FDG
|
18F-fluorodeoxyglucose
|
|
PET
|
positron emission tomography
|
|
CT
|
computed tomography
|
References
|
1
|
Fallah M, Liu X, Ji J, Försti A, Sundquist
K and Hemminki K: Autoimmune diseases associated with non-Hodgkin
lymphoma: A nationwide cohort study. Ann Oncol. 25:2025–2030. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Váróczy L, Gergely L, Zeher M, Szegedi G
and Illés A: Malignant lymphoma-associated autoimmune diseases-a
descriptive epidemiological study. Rheumatol Int. 22:233–237. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Park SY, Kim S, Kim ES, Choi SU, Hyun HJ,
Ahn JY, Lee JH, Ryu SH, Park JH, Lee GI and Lee HJ: A case of
Non-Hodgkin's lymphoma in patient with coombs' negative hemolytic
anemia and idiopathic thrombocytopenic purpura. Cancer Res Treat.
44:69–72. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Michel M, Chanet V, Dechartres A, Morin
AS, Piette JC, Cirasino L, Emilia G, Zaja F, Ruggeri M, Andrès E,
et al: The spectrum of Evans syndrome in adults: New insight into
the disease based on the analysis of 68 cases. Blood.
114:3167–3172. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Rummel MJ, Niederle N, Maschmeyer G, Banat
GA, von Grünhagen U, Losem C, Kofahl-Krause D, Heil G, Welslau M,
Balser C, et al: Bendamustine plus rituximab versus CHOP plus
rituximab as first-line treatment for patients with indolent and
mantle-cell lymphomas: An open-label, multicentre, randomised,
phase 3 non-inferiority trial. Lancet. 381:1203–1210. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Iannitto E and Tripodo C: How I diagnose
and treat splenic lymphomas. Blood. 117:2585–2595. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Nishii-Ito S, Izumi H, Touge H, Takeda K,
Hosoda Y, Yamasaki A, Kuwamoto S, Shimizu E and Motokura T:
Pulmonary intravascular large B-cell lymphoma successfully treated
with rituximab, cyclophosphamide, vincristine, doxorubicin and
prednisolone immunochemotherapy: Report of a patient surviving for
over 1 year. Mol Clin Oncol. 5:689–692. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yousem SA and Colby TV: Intravascular
lymphomatosis presenting in the lung. Cancer. 65:349–353. 1990.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Mahevas M, Gerfaud-Valentin M, Moulis G,
Terriou L, Audia S, Guenin S, Le Guenno G, Salles G, Lambotte O,
Limal N, et al: Characteristics, outcome, and response to therapy
of multirefractory chronic immune thrombocytopenia. Blood.
128:1625–1630. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Hitz F, Zucca E, Pabst T, Fischer N,
Cairoli A, Samaras P, Caspar CB, Mach N, Krasniqi F, Schmidt A, et
al: Rituximab, bendamustine and lenalidomide in patients with
aggressive B-cell lymphoma not eligible for anthracycline-based
therapy or intensive salvage chemotherapy-SAKK 38/08. Br J
Haematol. 174:255–263. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ohmachi K, Niitsu N, Uchida T, Kim SJ,
Ando K, Takahashi N, Takahashi N, Uike N, Eom HS, Chae YS, et al:
Multicenter phase II study of bendamustine plus rituximab in
patients with relapsed or refractory diffuse large B-cell lymphoma.
J Clin Oncol. 31:2103–2109. 2013. View Article : Google Scholar : PubMed/NCBI
|