Introduction
Excision with adequate margins for malignant soft
tissue tumors arising from the chest wall is often challenging.
Moreover, treatment after recurrence or inadequate excision is more
difficult because of unexpected margins. The prognosis of malignant
soft tissue tumors arising from the chest wall is poor compared
with tumors arising from the extremities. Radiotherapy is
additionally required in such difficult cases and chemotherapy is
performed to prevent local recurrence or metastases.
When these adjuvant therapies are performed for
tumors arising from the chest wall, interstitial pneumonitis must
be considered as a complication. In particular, radiation recall
pneumonitis, a rare inflammatory reaction in the previously
irradiated lung field caused by administration of antitumor agents,
should be kept in mind (1).
Here, we present a case of interstitial pneumonitis
induced by ifosfamide following radiotherapy after excision of a
recurrent malignant soft tissue tumor arising from the chest wall.
To our knowledge, this is the first report of radiation recall
pneumonitis attributable to ifosfamide used as a single antitumor
agent. Written informed consent was obtained from the patient.
Case report
A 74-year-old man visited his doctor with a 2-month
history of a painless mass in his right upper chest wall after
contusion. He was diagnosed with hematoma and underwent curettage.
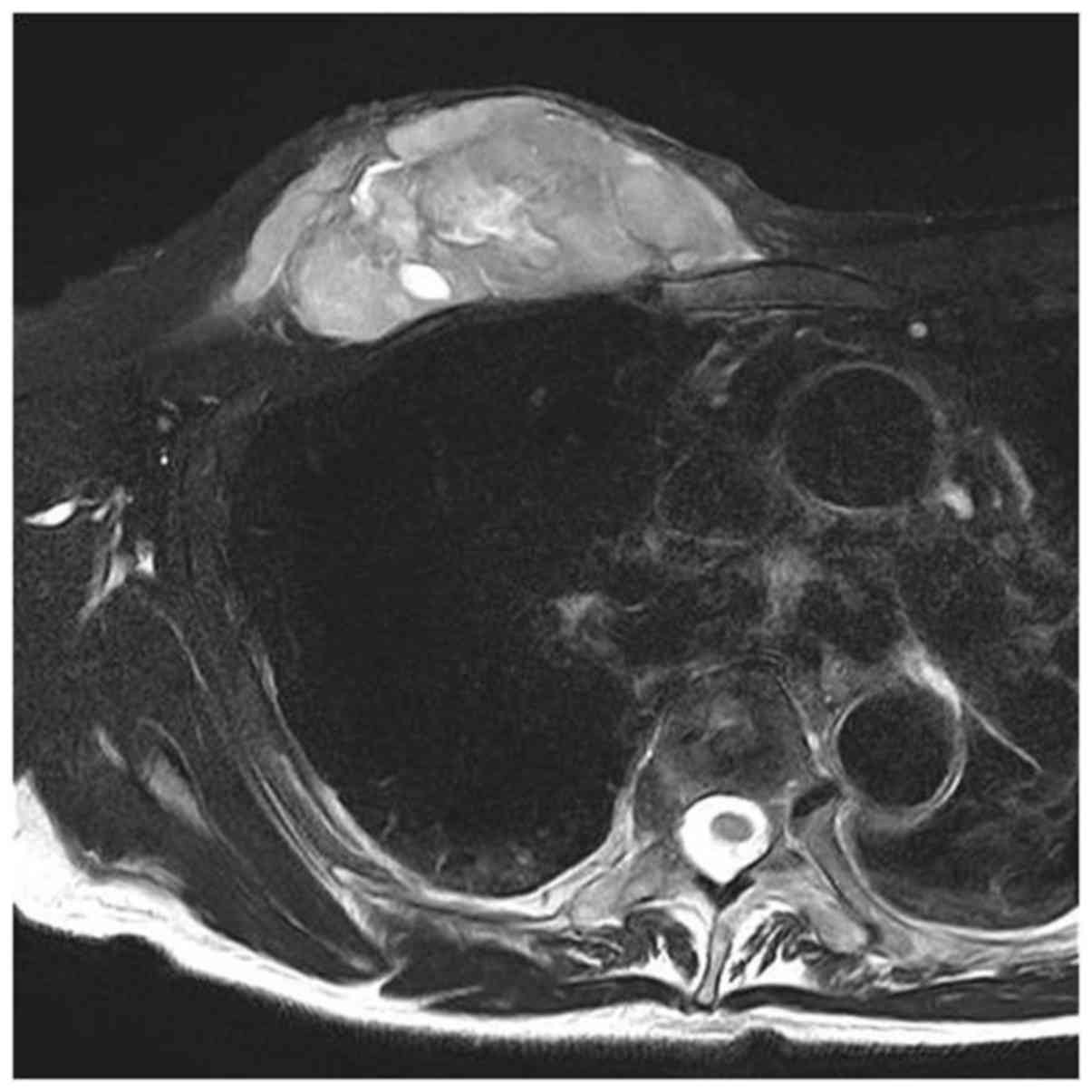
The mass rapidly increased in size 2 months after the previous
surgery (Fig. 1), and surgical
excision was performed under the diagnosis of chronic expanding
hematoma. He was then referred to our hospital 1 month after the
last surgery because the mass was histologically diagnosed as
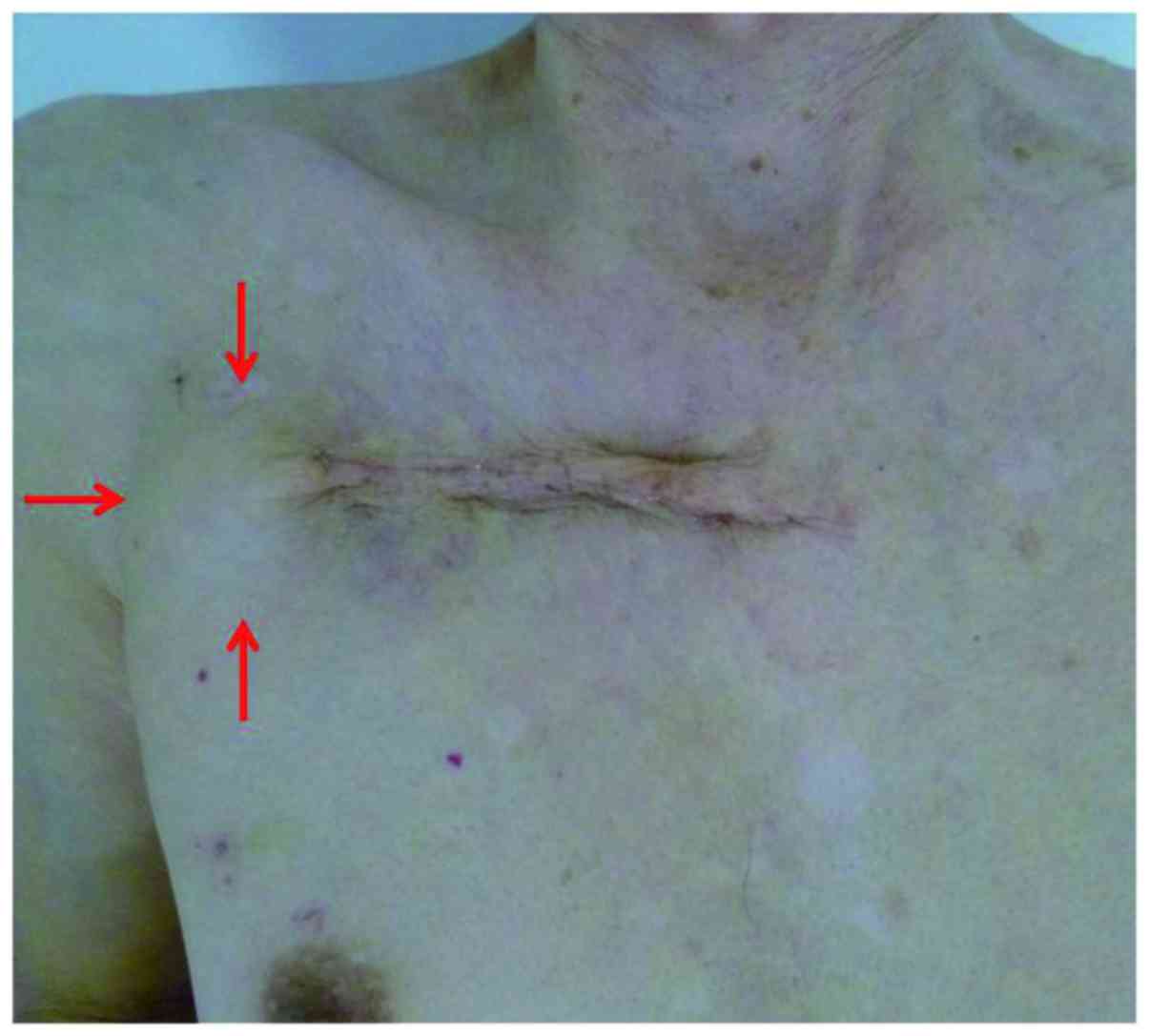
undifferentiated high grade sarcoma. He had a new growing mass on
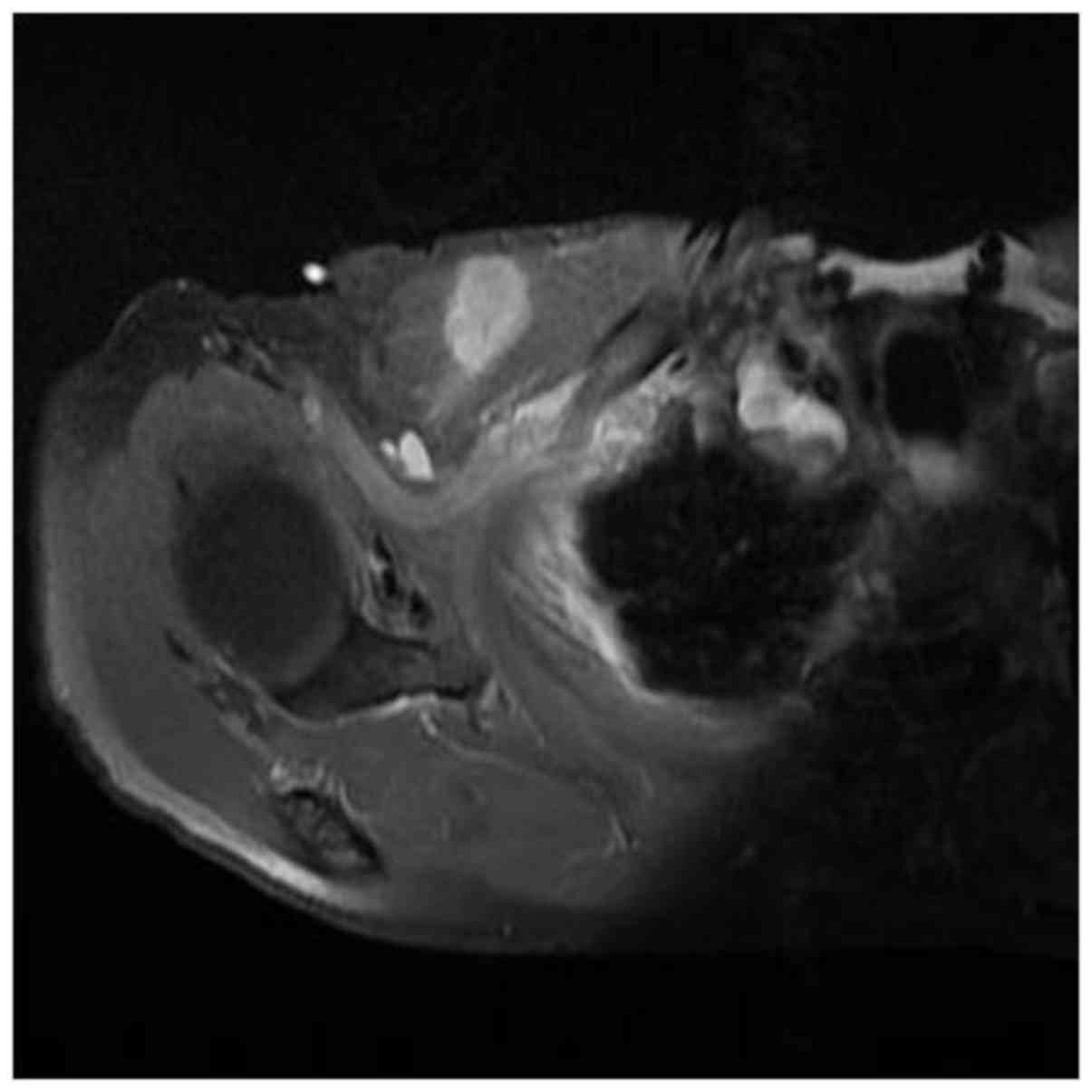
the lateral edge of the previous skin incision (Fig. 2). The extension of the tumor after
surgery was aggressive and was unclear on MR imaging (Fig. 3). It was difficult to set sufficient
tumor margins. He had good general condition for his age. Past and
family histories were unremarkable. He had no metastasis. Due to
the extent of the disease, he was not considered to be a candidate
for additional curative surgical excision including the previous
lesion. Therefore, we planned wide excision for the new tumor, and
adjuvant radiotherapy and chemotherapy after surgery because of the
high risk of local recurrence and metastasis. After wide excision
was performed with adequate margins for the new tumor, concurrent
chemoradiotherapy with ifosfamide and local radiotherapy up to 60
Gy in 30 fractions of 2 Gy over 6 weeks was started 1 month after
the final surgery to control the growth of any residual tumors. The
irradiated region around the right subclavicular area was set to
not include lung as much as possible. Although our protocol for
this tumor was ordinary combination therapy with ifosfamide and
doxorubicin, he was treated with only ifosfamide because he had
minor arrhythmia and mild cardiac dysfunction. Ifosfamide (3.5 g ×
4 days) was administered intravenously twice every 4 weeks.
Platelet transfusion was given because thrombopenia occurred during
the second cycle. There were no other complications. Third cycle
chemotherapy with ifosfamide (3 g × 4 days) was started 80 days
after final surgery and at 15 days after termination of
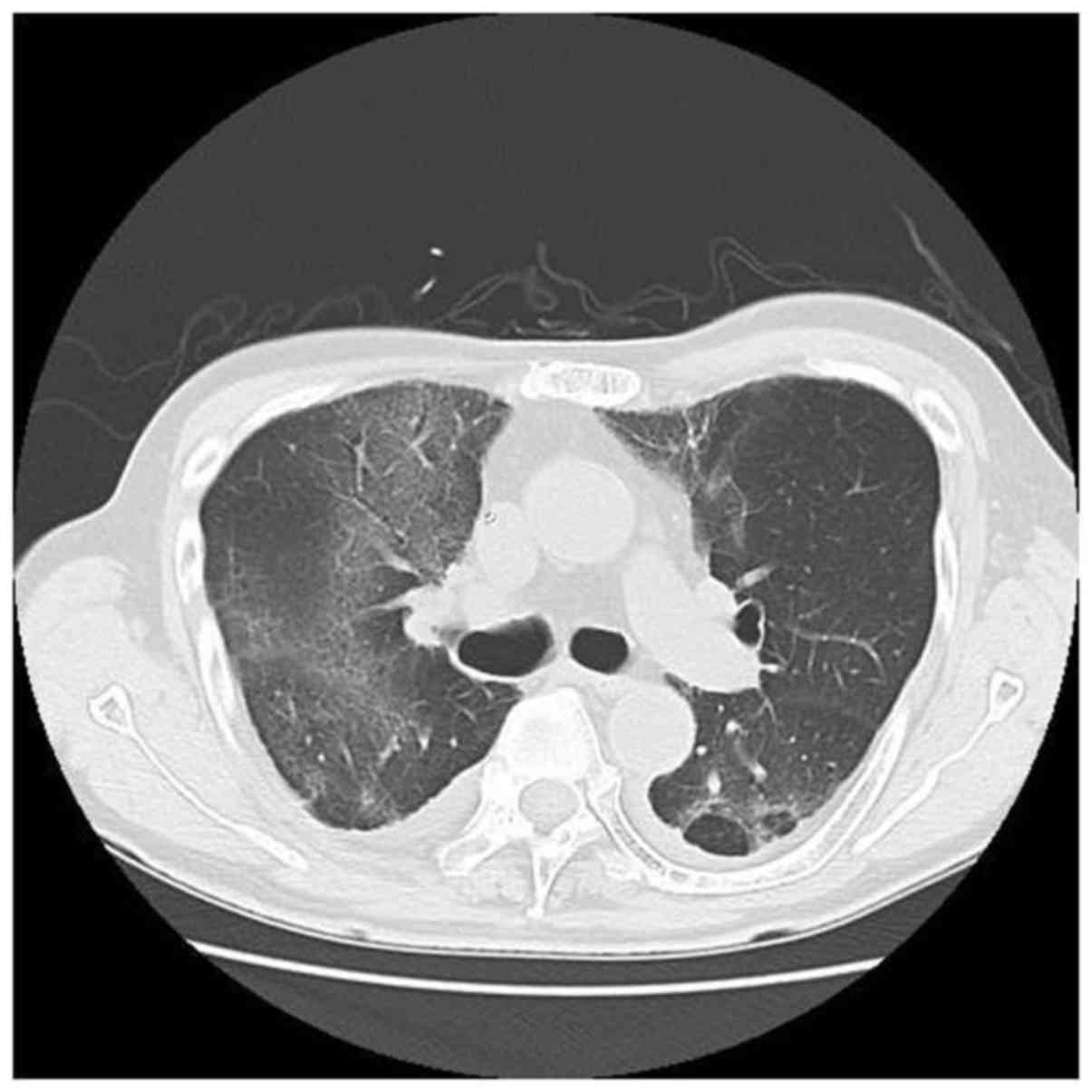
radiotherapy. He felt shortness of breath since following
administration. Dyspnea gradually increased, and chest X-ray and CT
revealed ground-glass infiltrations in the right pulmonary lobe
(Fig. 4). No evidence of infection
was found. This condition was diagnosed as interstitial pneumonitis
induced by ifosfamide and radiotherapy. Corticosteroid pulse
therapy was started immediately. However, his oxygen concentration
did not improve and the infiltrative lesion spread. He died due to
respiratory failure despite ventilator support 110 days after the
final surgery. No autopsy was performed.
Discussion
Malignant soft tissue tumors arising from the chest
wall are rare. Excision with an adequate margin is usually
performed and radiotherapy is not needed. However, it is often
impossible to excise with a wide margin, such as in our case, after
recurrence in the chest wall or inadequate excision because
planning of the excision range is often difficult. The prognosis of
malignant soft tissue tumors arising from the chest wall is poor
compared with tumors arising from the extremities. Moreover,
treatment of recurrent tumors is more difficult. Radiotherapy is
additionally required in such difficult cases, and chemotherapy is
performed to prevent local recurrence or metastases.
Our patient developed interstitial pneumonitis
during chemotherapy after surgery and radiotherapy. Although
chemotherapy is effective for tumor cells present throughout the
body, antitumor drugs used in oncology may cause many adverse
effects. One is interstitial pneumonitis. There are many reports of
interstitial pneumonitis associated with chemoradiotherapy. The
most common agents are methotrexate, cyclophosphamide, and
bleomycin (2–4). Ifosfamide is one of the standard drugs
for soft tissue sarcomas (5,6). However, interstitial pneumonitis that
is clearly associated with only ifosfamide, as in our case, has not
been reported, although there have been some studies on
interstitial pneumonitis after administration of combined
chemotherapy including ifosfamide, which is used for bone and soft
tissue sarcoma, and lymphoma (3,7–9).
Radiotherapy was considered as another cause of
interstitial pneumonitis. Respiratory symptoms of this disease
attributed to radiotherapy usually occur in the first 1–6 months
following lung radiotherapy (2,10). In
our case, the onset of symptoms developed in three weeks, even
though the irradiation field around the right subclavicular area
was set not to include the lung as much as possible. Consequently,
it unlikely that only radiotherapy caused interstitial pneumonitis.
We think that combined chemotherapy and radiotherapy to the lung
field may have caused this pneumonia. There are previous reports of
radiation recall pneumonitis induced by chemotherapy after thoracic
irradiation of malignant tumors such as lung cancer, lymphoma,
rhabdomyosarcoma, and Ewing's sarcoma (11–13).
Although there have been no previous reports, it was concluded that
the pneumonitis was radiation recall pneumonitis which is a rare
inflammatory reaction in the previously irradiated lung field due
to administration of ifosfamide.
Some antitumor drugs are associated with a recall
effect of pneumonitis after radiotherapy, especially doxorubicin
(11,14), taxanes (14–16),
gemcitabine (16), and
molecular-target drugs such as vemurafenib (4) and erlotinib (10). The etiology and mechanism of
radiation recall pneumonitis is unknown. The time interval from the
end of radiation to interstitial pneumonia may not be very long
(15,16). The period to onset following
radiotherapy was reported to be short in lung cancer and pediatric
malignant disease, which are treated by combined chemotherapy and
radiotherapy to the lung field (4,8). The
median time interval from beginning chemotherapy to radiation
recall pneumonitis for lung cancer was 12 h for anthracyclines, 30
days for combination gemcitabine and docetaxel, and 59 days for
taxanes (16). The time to
pneumonitis was short in our case. To our knowledge, there have
been no previous reports of interstitial pneumonitis associated
with ifosfamide used as a single agent. Ifosfamide is a popular
antitumor agent. It may be toxic and occasionally induce radiation
recall, including pneumonitis.
Radiotherapy is usually given for residual tumors
after incomplete excision or recurrent tumors for malignant bone
and soft tissue tumors. Moreover, chemotherapy is performed to
avoid local recurrence or to treat distant metastases. In this
case, radiotherapy and chemotherapy were performed to avoid
progression of residual tumors and to prevent distant metastases
because this tumor was histologically highly malignant. Ifosfamide
is a standard agents for malignant bone and soft tissue sarcomas,
and may be used in such situations. We report a rare case of
radiation recall pneumonia with rapid progress induced by only
ifosfamide despite a small irradiated region. Ifosfamide following
chest irradiation may cause enhanced toxicity. Interstitial
pneumonitis, which is likely to become fatal, must be considered
for sarcoma, especially that arising from the chest wall.
References
|
1
|
Burris HA III and Hurtig J: Radiation
recall with anticancer agents. Oncologist. 15:1227–1237. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Shanholtz C: Acute life-threatening
toxicity of cancer treatment. Crit Care Clin. 17:483–502. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Doi M, Okamoto Y, Yamauchi M, Naitou H and
Shinozaki K: Bleomycin-induced pulmonary fibrosis after tumor lysis
syndrome in a case of advanced yolk sac tumor treated with
bleomycin, etoposide and cisplatin (BEP) chemotherapy. Int J Clin
Oncol. 17:528–531. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Forschner A, Zips D, Schraml C, Röcken M,
Iordanou E, Leiter U, Weide B, Garbe C and Meier F: Radiation
recall dermatitis and radiation pneumonitis during treatment with
vemurafenib. Melanoma Res. 24:512–516. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Brunello A, Rizzato MD, Rastrelli M, Roma
A, Maruzzo M, Basso U, Fiduccia P, Buzzaccarini MS, Scarzello G,
Rossi CR, et al: Adjuvant chemotherapy for soft tissue sarcomas: A
10-year mono-institutional experience. J Cancer Res Clin Oncol.
142:679–685. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Tanaka K, Mizusawa J, Fukuda H, Araki N,
Chuman H, Takahashi M, Ozaki T, Hiruma T, Tsuchiya H, Morioka H, et
al: Perioperative chemotherapy with ifosfamide and doxorubicin for
high-grade soft tissue sarcomas in the extremities (JCOG0304). Jpn
J Clin Oncol. 45:551–561. 2015.
|
|
7
|
Baker WJ, Fistel SJ, Jones RV and Weiss
RB: Interstitial pneumonitis associated with ifosfamide therapy.
Cancer. 65:2217–2221. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Prestwich RJ, Picton SV, Glaser A and
Taylor RE: Fatal pneumonitis in children with metastatic
rhabdomyosarcoma following whole lung radiotherapy and sequential
epirubicin. Pediatr Blood Cancer. 48:586–590. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Dincol D, Buyukcelik A, Dogan M, Akbulut
H, Samur M, Demirkazik A, Senler FC, Onur H and Icli F: Long-term
outcome of mesna, ifosfamide, mitoxantrone, etoposide (MINE)
regimen as a consolidation in patients with aggressive non-Hodgkin
lymphoma responding to CHOP. Med Oncol. 27:942–945. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Arakawa H, Johkoh T, Sakai F, Kusumoto M,
Hataji O and Taguchi O: Exacerbation of radiation fibrosis with
erlotinib: Another pattern of radiation recall phenomenon. Jpn J
Radiol. 29:587–589. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ma LD, Taylor GA, Wharam MD and Wiley JM:
‘Recall’ pneumonitis: Adriamycin potentiation of radiation
pneumonitis in two children. Radiology. 187:465–467. 1993.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Minami-Shimmyo Y, Ohe Y, Yamamoto S, Sumi
M, Nokihara H, Horinouchi H, Yamamoto N, Sekine I, Kubota K and
Tamura T: Risk factors for treatment-related death associated with
chemotherapy and thoracic radiotherapy for lung cancer. J Thorac
Oncol. 7:177–182. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Fox AM, Dosoretz AP, Mauch PM, Chen YH,
Fisher DC, LaCasce AS, Freedman AS, Silver B and Ng AK: Predictive
factors for radiation pneumonitis in Hodgkin lymphoma patients
receiving combined-modality therapy. Int J Radiat Oncol Biol Phys.
83:277–283. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Azria D, Magné N, Zouhair A, Castadot P,
Culine S, Ychou M, Stupp R, Van Houtte P, Dubois JB and Ozsahin M:
Radiation recall: A well recognized but neglected phenomenon.
Cancer Treat Rev. 31:550–570. 2005. View Article : Google Scholar
|
|
15
|
Schweitzer VG, Juillard GJ, Bajada CL and
Parker RG: Radiation recall dermatitis and pneumonitis in a patient
treated with paclitaxel. Cancer. 76:1069–1072. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ding X, Ji W, Li J, Zhang X and Wang L:
Radiation recall pneumonitis induced by chemotherapy after thoracic
radiotherapy for lung cancer. Radiat Oncol. 6:242011. View Article : Google Scholar : PubMed/NCBI
|