Introduction
Pleural involvement in patients with non-Hodgkin
lymphoma (NHL) is well documented, and ~20% of the cases present
with pleural effusion (1–3). However, primary pleural lymphomas
without any other site of involvement are extremely rare,
accounting for ~0.3% of all NHLs. Malignant lymphoma of the pleura
has been mostly associated with chronic pleural inflammation
(4). Therefore, the treating
physicians must include primary pleural NHL in the differential
diagnosis when a patient presents with pleural inflammation or
effusion, particularly in China, where tuberculosis (TB) and severe
lung infections remain a major public health concern. The case
reported herein is of particular interest, as the patient had no
history of pleuro-pulmonary disease or evidence of lymphoma at any
other site.
Case report
A 49-year-old man presented to the outpatient care
of the First Hospital of Jiaxing (Jiaxing, China) on May 12, 2014
with a lump on the left chest wall accompanied by pain. A chest
computed tomography (CT) scan suggested possible tuberculous
pleurisy along with left pulmonary TB. In addition, bone
destruction was observed in some ribs on the left side, along with
the formation of a cold abscess. Single-photon emission computed
tomography revealed particularly high radioactive 99mTc
uptake in the left anterior thoracic wall. The ratio of target
(area of highest uptake) to non-target (normal tissue) was 117.72.
The fiberoptic bronchoscopic and hydrothorax exfoliative
cytological examinations were negative for malignant cells.
Biochemical analysis of the pleural fluid revealed a markedly high
adenosine deaminase (ADA) level (401.2 IU/L). The differential
white blood cell count revealed 98% lymphocytes and 2% neutrophils.
The fluid was brown in color and cloudy. The fluid protein test was
positive (4+). Taking into consideration the patient's history,
tuberculous abscess was considered, and tuberculous pleurisy was
diagnosed as the cause of abnormal radioactive uptake in the left
pleura. As the patient and his family did not consent to an open
biopsy, treatment was initiated based on the diagnosis of pulmonary
and thoracic TB of the left chest wall, with tuberculous pleurisy.
The patient received 0.3 g isoniazid i.v.gtt qd, 0.45 g rifampincin
i.v.gtt qd, 0.4 g amikacin i.v.gtt qd, 8.0 g aminosalicylic acid
i.v.gtt qd, 0.4 g galtixacin p.o. qd, 0.75 g ethambutol
hydrochloride p.o. qd, and 0.5 g pyrazinamide p.o. tid. Following
anti-tuberculous treatment for 1 month, no significant change was
observed in the lesion of the left chest wall. Thoracoscopic
resection of the lump was performed on June 18, 2014, followed by
histopathological examination and consultation with the Fudan
University Shanghai Cancer Center. At that time, the suspicion of
diffuse large B-cell lymphoma (DLBCL) in the chest was raised. The
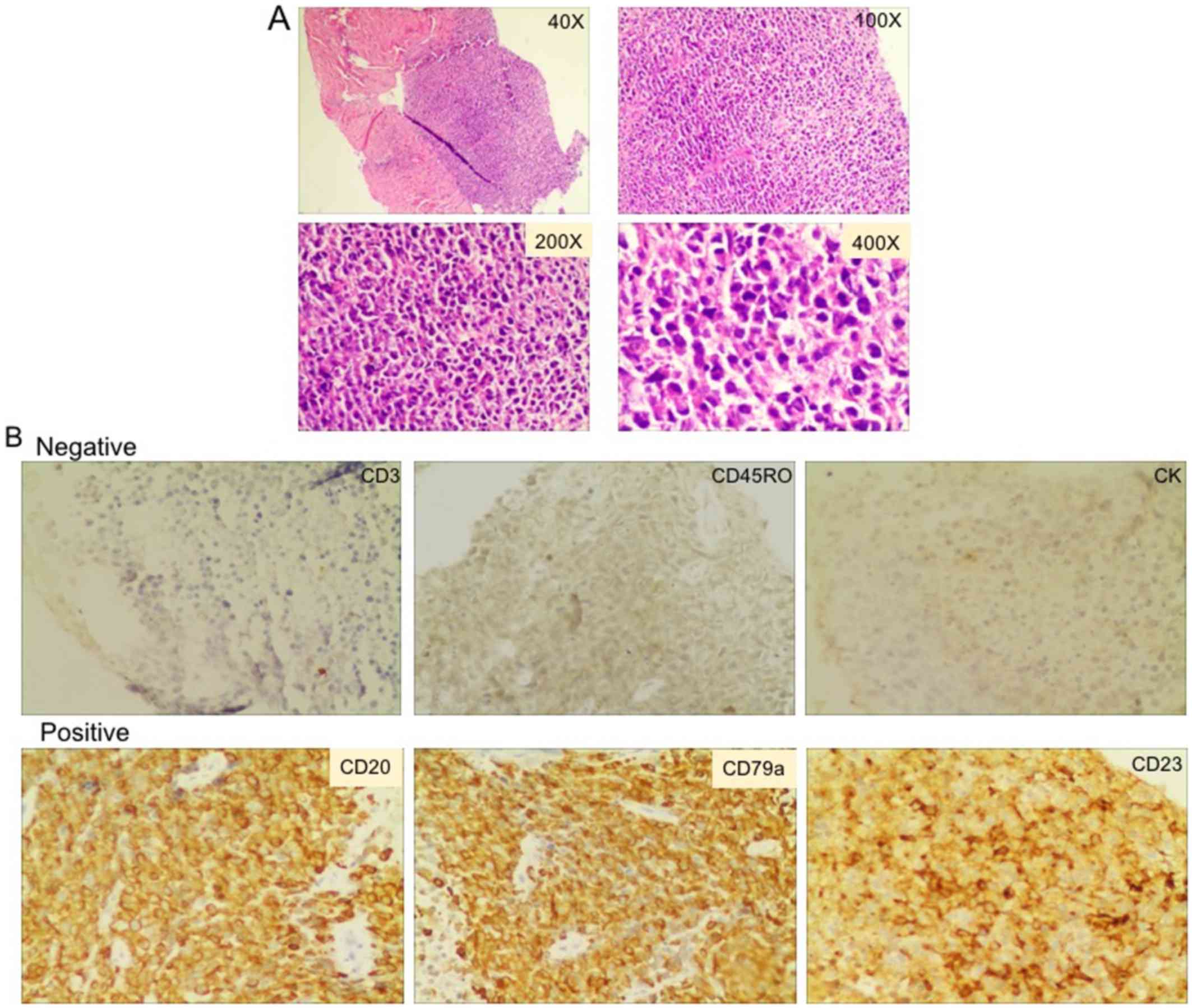
examination of hematoxylin and eosin (H&E)-stained sections
(Fig. 1A) revealed a diffuse
lymphoid infiltrate in the thoracic lump. Examination under
high-power magnification revealed numerous large atypical lymphoid
cells with irregular nuclei, which were double in size compared to
a typical lymphocyte, with uneven chromatin distribution. The
results of immunohistochemistry were as follows: CD20+,
CD10−, B-cell lymphoma (Bcl)-6−,
Bcl-2+, MUM1+, CD30+ (diffuse and
weak positivity), Epstein-Barr virus latent membrane protein
1+/− (spotty positivity with nuclear localization),
CD3−, AE1/AE3− and Ki-67+ (~95%).
Representative results of H&E staining and immunohistochemistry
are shown in Fig. 1.
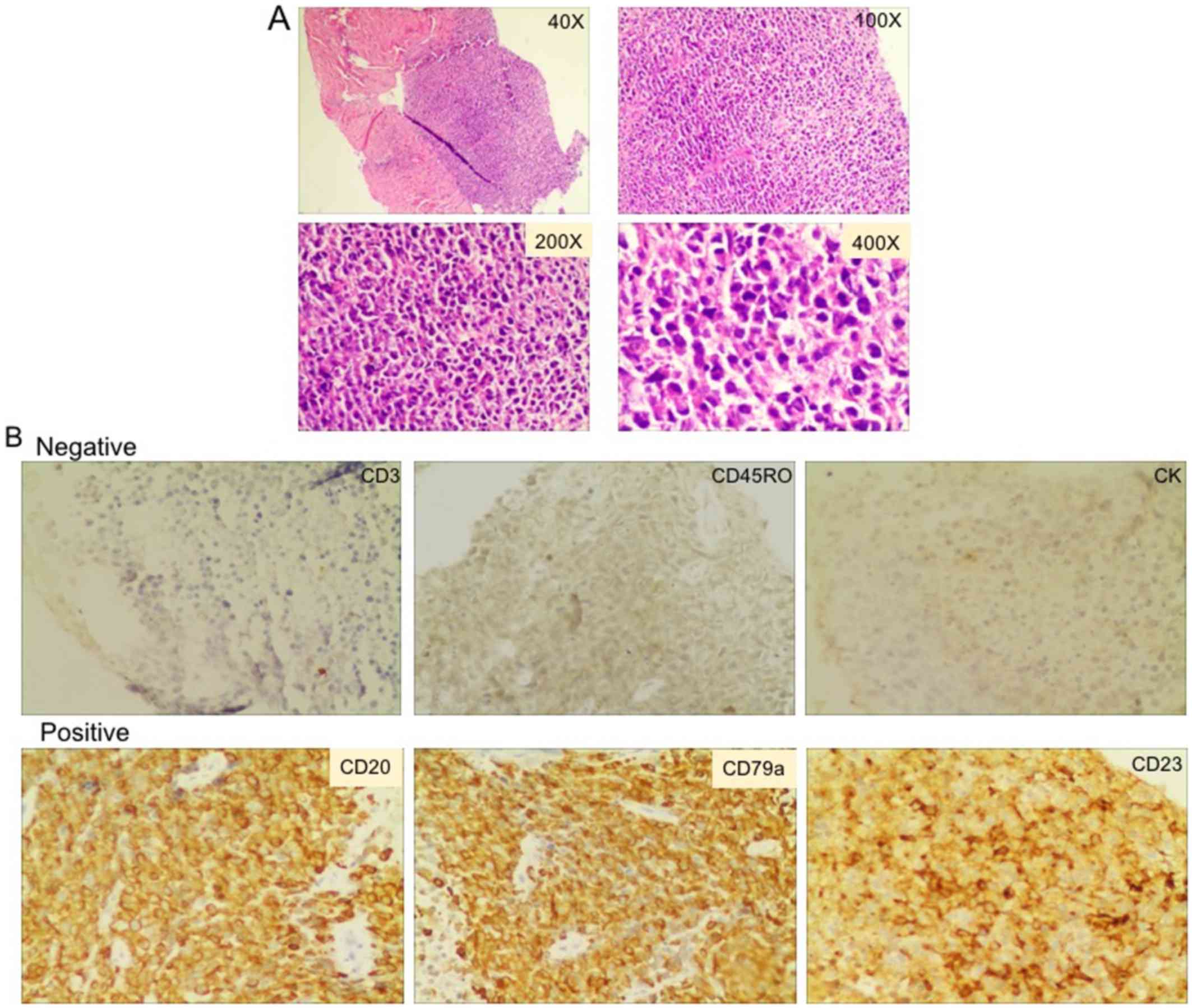 | Figure 1.(A) Histopathology of the
thoracoscopic biopsy specimen revealed confluent aggregates of
numerous lymphocytes, exhibiting lack of germinal centers
(hematoxylin and eosin staining; magnification, ×40, ×100, ×200 and
×400). Briefly, following deparaffinization and rehydration, the
slides were stained with hematoxylin for 1.5 min at room
temperature, rinsed with deionized water and dipped in tap water
for 5 min to allow the stain to develop, then dipped in acid
ethanol to destain. After rinsing with deionized water 3 times, the
slides were stained with eosin for 3–4 sec at room temperature,
followed by graded rehydration in 75, 90 and 100% ethanol. The
slides were covered by coverslips with mounting medium and
subjected to microscopic observation. (B) Immunohistochemistry of
the thoracoscopic biopsy specimen revealed positive CD20 (cat. no.
ab78237, 1:200), CD79a (cat. no. ab79414, 1:100) and CD23 (cat. no.
ab92495, 1:100) expression, and negative CD3 (cat. no. ab52959,
1:200), CD45RO (cat. no. ab23, 1:100) and CK (cat. no. ab82254,
1:100) expression on the surface of the cancer cells. All
antibodies were obtained from Abcam, Cambridge, UK. CK,
cytokeratin. |
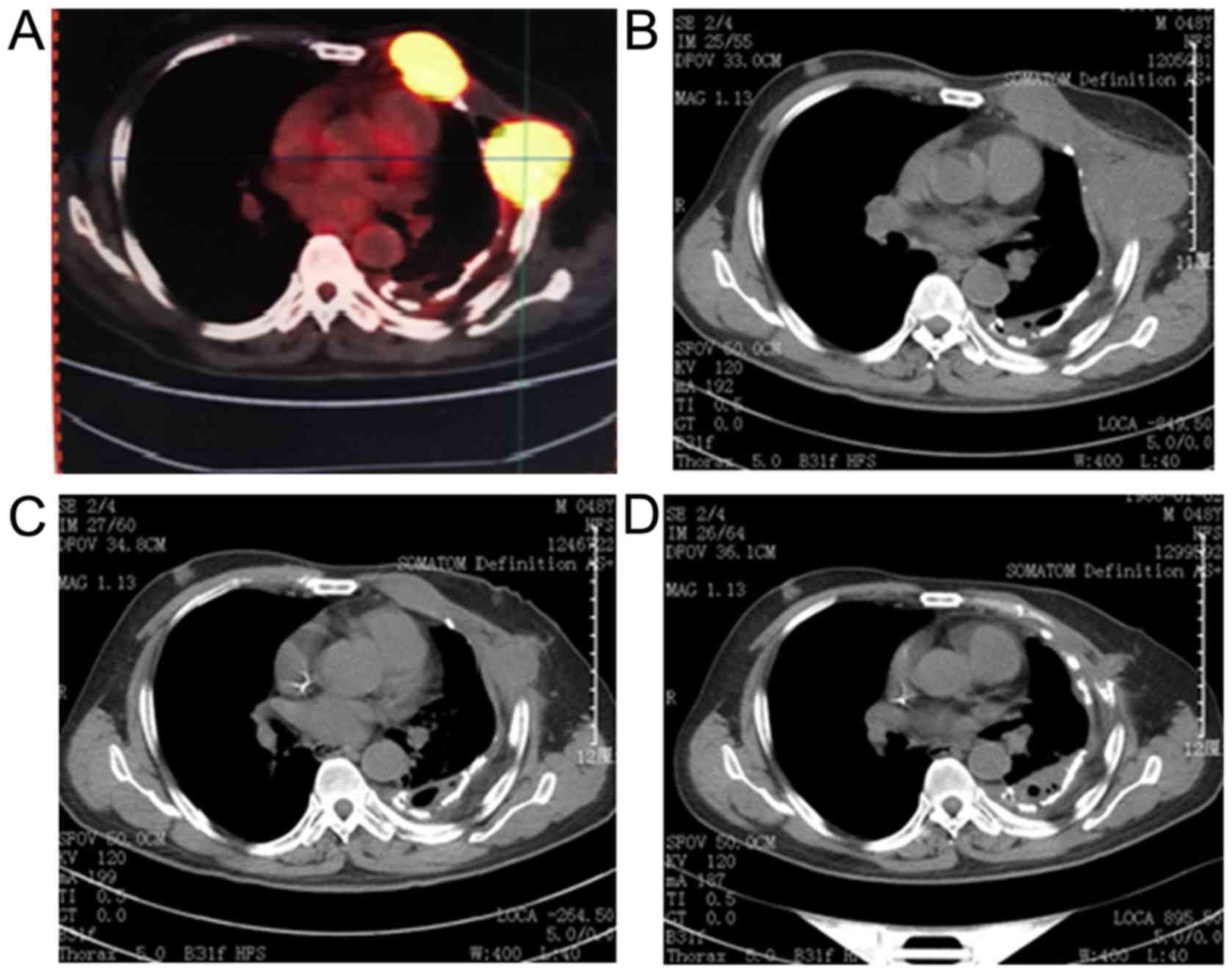
On July 25, 2014, a positron emission tomography/CT
scan (Fig. 2A), performed at Fudan
University Shanghai Cancer Center revealed the following: i) A
space-occupying lesion was identified on the left chest wall that
invaded the neighboring ribs. An extremely high intensity of
fluorine-18-fluorodeoxyglucose uptake was considered to indicate a
possible lymphoma. Multiple lymphatic invasions were demonstrated
in the left axillary, internal mammary and intercostal lymph nodes
and pleural effusion was observed in the left pleural space. ii)
Left-sided pulmonary infection and hydropneumothorax were
demonstrated. Old pathological changes were also observed in the
left pleura. A subsequent bone marrow biopsy was negative for
lymphoma. On August 9, 2014, a repeat thoracic CT (Fig. 2B), revealed that the lesion in the
chest wall had significantly increased in size, causing destruction
of the ribs. Furthermore, the left axillary nodes were found to be
enlarged. On August 20, 2014, the patient was initiated on CHOP
chemotherapy (cyclophosphamide 0.8 mg/dl, doxorubicin hydrochloride
60 mg/dl, with the addition of vincristine sulfate 2 mg/dl, and
prednisone 100 mg/dl) for 8 cycles. Rituximab was not included in
the regimen due to financial difficulties. Between the treatment
cycles the status of the tumor was monitored by periodic thoracic
CT scans [September 28 (Fig. 2C),
October 21 and November 28 (Fig.
2D)], which revealed that the lesion had slightly shrunk. The
therapeutic efficacy of CHOP chemotherapy was classified as stable
disease. Overall, the treatment prolonged the patient's
progression-free survival to ~2 months, and the overall survival to
~1 year. The patient ultimately succumbed to severe thoracic
infection and pleural effusion.
Discussion
Lymphoma is a type of hematological malignancy that
usually originates from lymph nodes or the lymphatic system. The
two main types of lymphoma are NHL (~90% of cases) and Hodgkin's
lymphoma (~10% of cases). NHL may be further subdivided into T-cell
and B-cell lymphoma, with relatively rare cases of natural
killer-cell lymphoma. DLBCL is the most common type of NHL
(1,5,6). In the
majority of the cases, early-stage lymphoma is not associated with
any specific clinical characteristics. Approximately 30–40% of the
patients exhibit only general symptoms, such as fever, weight loss
and night sweats. Physical signs of lymphoma include painless
enlarged lymph nodes, enlarged spleen and local lumps (5). It has been reported that ~25% of
patients with NHL develop pleural effusion during disease
progression (7,8). Pathological changes in the lung have
been demonstrated in ~50% of lymphoma patients on autopsy, the
majority of which were metastases from mediastinal or pulmonary
hilar lymph nodes (7,9).
The risk of misdiagnosis is relatively high when
lymphoma is complicated by pleural effusion, and it is often
misdiagnosed as tuberculous pleurisy due to the high ADA level in
the patient's pleural fluid, together with the clinical signs. ADA
is considered as one of the key enzymes involved in purine
metabolism; its primary function is associated with the development
and maintenance of the immune system, as it plays an important role
in T-cell differentiation and proliferation (10,11). T
cells mediating anti-TB immunity may cause ADA elevation in
tuberculous pleural effusion (11).
However, the invasion of the pleura by lymphoma also leads to a
higher number of lymphocytes in the pleural effusion, increasing
ADA concentration (10). Therefore,
it may not be appropriate to set a high ADA level as the index for
tuberculous pleurisy. It was reported recently by several studies
that increased ADA level in pleural effusion may be an indication
of lymphoma (10–12). According to Porcel et al, an
extremely high ADA activity (>250 U/L) in the pleural fluid
should raise the suspicion of empyema or lymphoma rather than TB
(12).
In previous case reports on misdiagnosis of
lymphoma, the majority of the cases were misdiagnosed as TB
(9). The major causes of
misdiagnosis are as follows. i) Lymphoma and TB share a number of
common clinical characteristics, such as fever, night sweats,
feeling of satiety after ingestion of only a small amount of food,
fatigue and unexplained weight loss. ii) Particularly in China, the
incidence of TB is significantly higher compared with that of
lymphoma, and TB is usually preferentially considered, as
clinicians are prone to suspect the most common and frequent
disease. iii) Both lymphoma and TB originate at sites where a
biopsy is generally difficult to perform. The patients and their
families usually decline invasive examinations. iv) Clinicians may
rely excessively on the results of biochemical and imaging
examination for diagnosis, whereas they must improve their ability
to perform a comprehensive analysis of the symptoms, clinical
signs, bacteriology, histopathology and therapeutic efficacy.
In the present case, the causes of misdiagnosis may
be summarized as follows. i) The patient was a middle-aged man who
presented with a lump in the left chest wall, raising the suspicion
of TB. ii) The radiographic changes observed on the thoracic CT
scan matched left pulmonary TB and tuberculous pleurisy. iii) The
biochemical analysis of the patient's pleural fluid revealed
markedly elevated ADA levels (401.20 IU/L), which is characteristic
of tuberculous pleurisy. iv) As the patient and his family did not
consent to an open biopsy at first, pathological examination was
delayed, as were diagnosis and treatment.
There are several clinically important prognostic
factors in NHL, including age, serum lactate dehydrogenase level,
performance status, Ann Arbor stage and number of extranodal sites.
When detected early, there is a better chance for quick diagnosis,
timely treatment and improved overall survival. The standard
treatment for DLBCL is chemotherapy in combination with
immunotherapy (13,14). The most common chemotherapy regimen
is CHOP (cyclophosphamide, doxorubicin, vincristine and prednisone)
plus rituximab for CD20+ patients. Additionally,
autologous hematopoietic stem cell transplantation remains a
treatment of choice for DLBCL patients with chemotherapy-sensitive
disease relapse (15,16).
Acknowledgements
Not applicable.
Funding
The present study was supported by Key Discipline
(Oncology) in Medical Sciences of Jiaxing City (grant no. 04-F-14),
and the Science and Technology Project of Jiaxing City (grant no.
2016AY23041).
Availability of data and materials
Not applicable.
Authors' contributions
XY and XX analyzed and interpreted the patient data
regarding the lymphoma and the infectious condition. BS, QZ and XY
conducted the final diagnosis of lymphoma based on the
immunohistochemical and PET-CT results. BS made substantial
contributions to the acquisition of the complete medical charts of
the patient for this case report. QZ conducted the literature
search and summarization during the whole process. YZ was a major
contributor in drafting the manuscript. The final version of the
manuscript has been read and approved by all authors.
Ethics approval and consent to
participate
The present study meets all applicable standards
with regard to the ethics of experimentation and research
integrity, and has been approved by the Ethics Committee of the
First Hospital of Jiaxing.
Consent for publication
Written informed consent has been obtained from the
patient and his family for the publication of the case details and
associated images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Armitage JO and Weisenburger DD: New
approach to classifying non-Hodgkin's lymphomas: Clinical features
of the major histologic subtypes. Non-Hodgkin's Lymphoma
Classification Project. J Clin Oncol. 16:2780–2795. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Usuda D, Arahata M, Takeshima K, Sangen R,
Takamura A, Kawai Y, Kasamaki Y, Iinuma Y and Kanda T: A case of
diffuse large B-cell lymphoma mimicking primary effusion
lymphoma-like lymphoma. Case Rep Oncol. 10:1013–1022.
2017.PubMed/NCBI
|
|
3
|
Iwasa Y, Okada A, Takenaka H, Takahashi T,
Koguchi N, Katayama K, Murakami S, Choh S, Tomoda K and Kimura H:
Primary malignant lymphoma originating from the chest wall without
preceding pleural disease. Intern Med. 56:681–686. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Krol EM, Ogrodnik A, Sieber S, Chronakos J
and Mahfoozi AP: Unusual case of isolated pleural B-cell lymphoma.
Conn Med. 79:347–349. 2015.PubMed/NCBI
|
|
5
|
Abramson JS and Shipp MA: Advances in the
biology and therapy of diffuse large B-cell lymphoma: Moving toward
a molecularly targeted approach. Blood. 106:1164–1174. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Nogai H, Dörken B and Lenz G: Pathogenesis
of non-Hodgkin's lymphoma. J Clin Oncol. 29:1803–1811. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Mian M, Wasle I, Gritsch S, Willenbacher W
and Fiegl M: B cell lymphoma with lung involvement: What is it
about? Acta Haematol. 133:221–225. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Vega F, Padula A, Valbuena JR, Stancu M,
Jones D and Medeiros LJ: Lymphomas involving the pleura: A
clinicopathologic study of 34 cases diagnosed by pleural biopsy.
Arch Pathol Lab Med. 130:1497–1502. 2006.PubMed/NCBI
|
|
9
|
Sun J, Li G, Zhang N, Li S and Chen R:
Analysis of lymphoma presenting with pulmonary symptoms: Report of
79 cases. Zhonghua Jie He He Hu Xi Za Zhi. 37:597–600. 2014.(In
Chinese). PubMed/NCBI
|
|
10
|
Yao CW, Wu BR, Huang KY and Chen HJ:
Adenosine deaminase activity in pleural effusions of lymphoma
patients. QJM. 107:887–893. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Krenke R and Korczyński P: Use of pleural
fluid levels of adenosine deaminase and interferon gamma in the
diagnosis of tuberculous pleuritis. Curr Opin Pulm Med. 16:367–375.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Porcel JM, Esquerda A and Bielsa S:
Diagnostic performance of adenosine deaminase activity in pleural
fluid: A single-center experience with over 2100 consecutive
patients. Eur J Intern Med. 21:419–423. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Vose JM: Molecular pathogenesis in
non-Hodgkin lymphoma: Implications for therapy. Transfus Apheresis
Sci. 49:155–156. 2013. View Article : Google Scholar
|
|
14
|
Fang C, Xu W and Li JY: A systematic
review and meta-analysis of rituximab-based immunochemotherapy for
subtypes of diffuse large B cell lymphoma. Ann Hematol.
89:1107–1113. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Gisselbrecht C: Is there any role for
transplantation in the rituximab era for diffuse large B-cell
lymphoma? Hematology Am Soc Hematol Educ Program. 2012:410–416.
2012.PubMed/NCBI
|
|
16
|
Stiff PJ, Unger JM, Cook JR, Constine LS,
Couban S, Stewart DA, Shea TC, Porcu P, Winter JN, Kahl BS, et al:
Autologous transplantation as consolidation for aggressive
non-Hodgkin's lymphoma. N Engl J Med. 369:1681–1690. 2013.
View Article : Google Scholar : PubMed/NCBI
|