Introduction
The glandular tissue of the prostate includes
secretory cells on the side facing the glandular cavity and basal
cells on the basal side. The proliferation of basal cells in the
prostate varies from hyperplasia to carcinoma, but carcinoma
arising from the basal cells of the prostate is extremely rare
(1). Basal cell carcinoma (BCC) of
the prostate has been considered as a tumor with low malignant
potential in a limited number of clinical studies; however, it has
been reported that this tumor has an aggressive potential that
causes metastasis and recurrence (2). We herein report a case of BCC of the
prostate that was diagnosed at an early stage and was treated by
radical surgical resection.
Case report
A 68 year-old-man visited the Department of Urology,
Nankai Medical Center (Saiki, Japan) in August 2017 for a periodic
follow-up examination for bladder cancer. The patient had been
diagnosed with bladder cancer and had undergone transurethral
resection of the bladder tumor in March 2016. Pathological
examination revealed a high-grade urothelial carcinoma in
situ (CIS). Intravesical Bacillus Calmette-Guérin therapy was
administered for CIS of the bladder, after which time no recurrence
of the bladder cancer was observed. Although the
prostate-specific-antigen (PSA) level was normal prior to August
2017, the PSA level measured in August 2017 had increased to 5.61
ng/ml (PSA normal range, ≤4.0 ng/ml). Prostate biopsy was performed
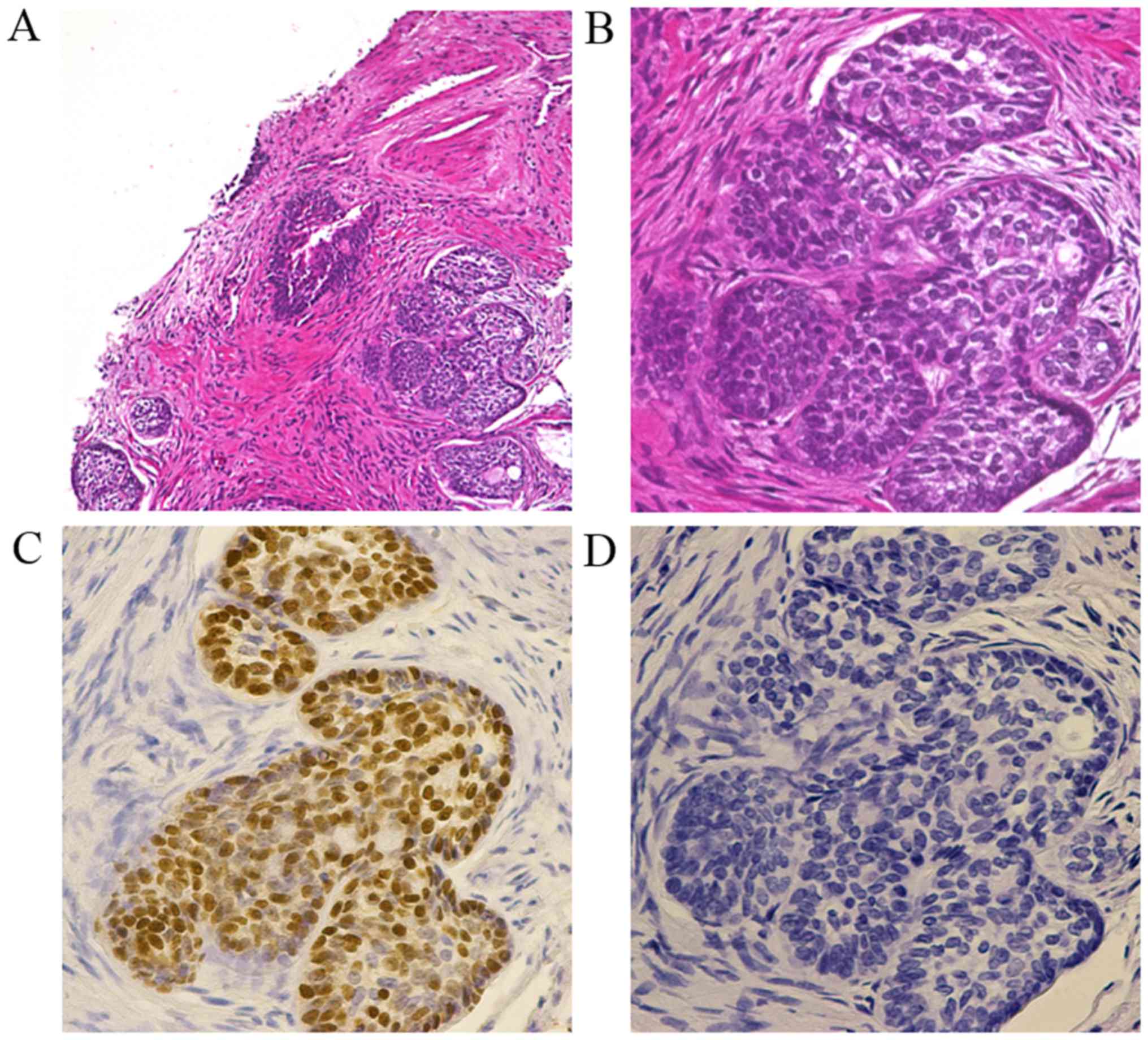
and histological examination revealed tumor cells with a high
nucleus-to-cytoplasm ratio forming a small nest-like basaloid cell
carcinoma in a small part of the biopsy specimen (Fig. 1A). A peripheral palisading pattern
was also observed (Fig. 1B). The
results of immunostaining examination revealed that the tumor cells
tested positive for p63 (Fig. 1C),
but negative for PSA (Fig. 1D).
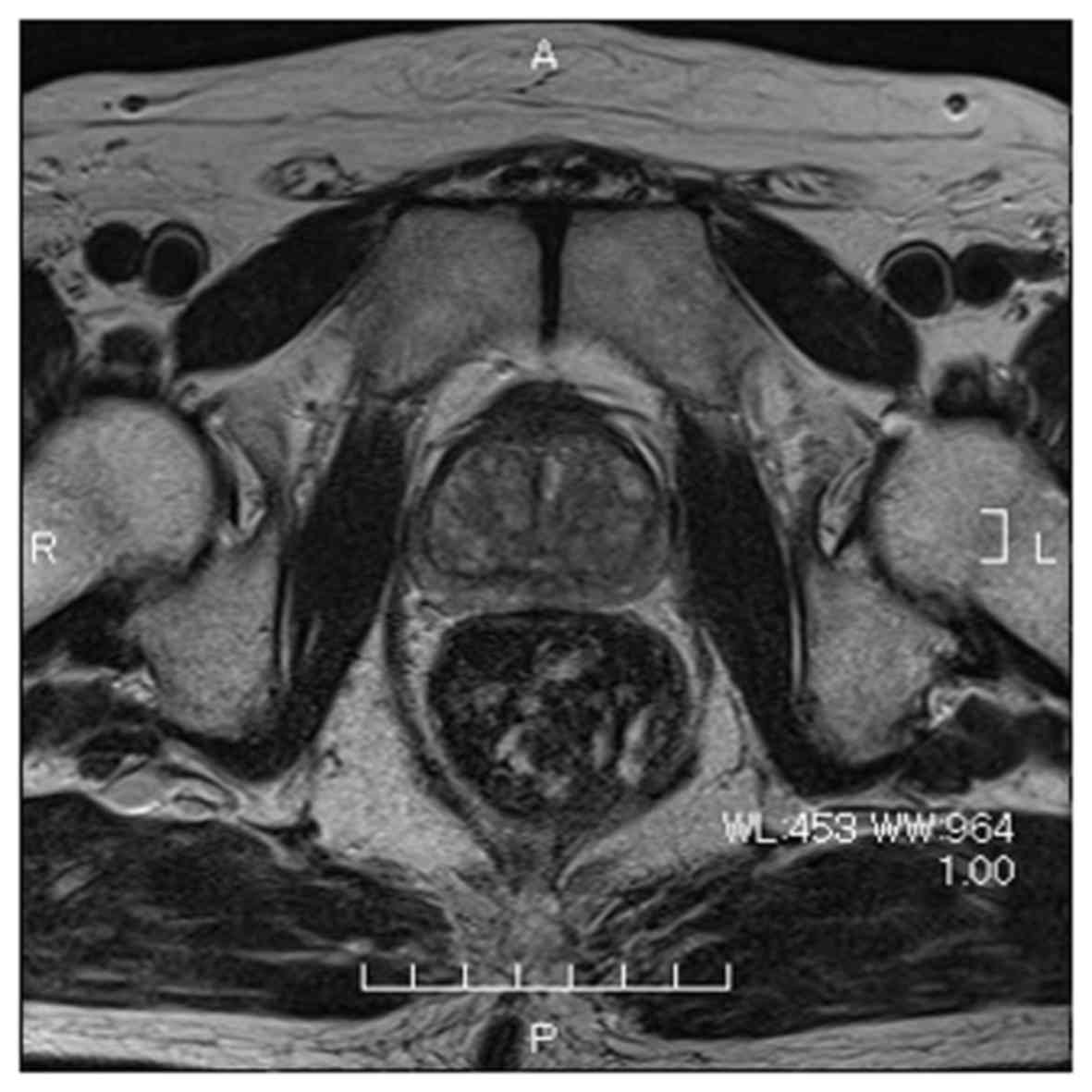
Based on the abovementioned results, the patients was diagnosed
with BCC of the prostate. Magnetic resonance imaging did not reveal
any obvious abnormal lesion in the prostate (Fig. 2). Computed tomography and bone
scintigraphy showed no metastatic lesions. After confirming that
there was no recurrence of the bladder cancer by random biopsy,
retropubic radical prostatectomy with extended lymph node
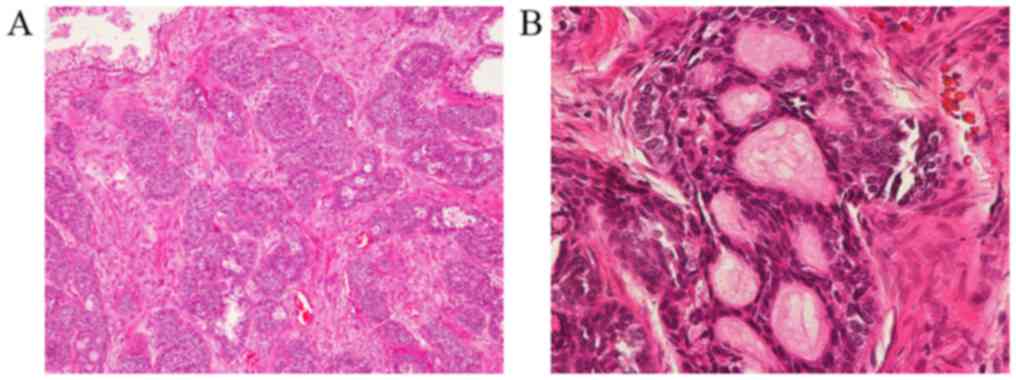
dissection was performed. Pathological examination of the surgical
specimen revealed a predominant basaloid component admixed with an
adenoid cystic-like tumor with cribriform appearance (Fig. 3A and B). The resection margin was
negative and there were no lymph node metastases. The patient was
examined via CT scan every 3 months until the last follow up on
August 15th 2018. The individual remained alive and recurrence-free
1 year after surgery.
Discussion
BCC of the prostate is morphologically diverse and
may be considered as an adenoid cystic carcinoma, which is
histologically similar to a salivary gland tumor; it may also be
classified as a basaloid cell carcinoma, which is histologically
similar to a basal cell carcinoma of the skin (3,4). Some
cases have been reported to comprise a single tissue type, namely
basaloid cell carcinoma or adenoid cystic carcinoma; however, cases
have been reported where these two types coexist within the same
tumor. In a clinicopathological study of 29 cases of BCC of the
prostate, Ali and Epstein reported that small, solid, nest-like
tumors with peripheral palisading and adenoid cystic-like tumors
were the most common pattern (5). In
the present case, small basaloid nests and adenoid cystic-like
tumor were also observed, which is considered to be similar to the
tissue pattern previously reported (5).
BCC of the prostate is a rare tumor; upon searching
the PubMed electronic database, only 98 reported cases of BCC of
the prostate were retrieved. When summarizing the 75 cases that
were available (6–13), the mean patient age was 65.3±13.6
years, and the mean observation period was 41.8±44.8 months. This
type of cancer was most common among elderly men (age range, 65–84
years) and the chief complaint of several patients was urinary
obstruction. Radical prostatectomy was performed in 26 of the 75
patients; among those, 16 patients were alive without cancer
recurrence at the time of reporting these cases. In the remaining
10 patients, radical prostatectomy was not curative. Some patients
only underwent transurethral resection of prostate, which is not a
curative option for prostate cancer, and achieved long-term
survival without recurrence. Of the 75 patients, 28 (37%) developed
disease progression, such as metastasis and recurrence, and
eventually succumbed to the disease. BCC of the prostate may
present as an indolent tumor that allows long-term survival with
non-curative treatment, such as transurethral resection of the
prostate alone; however, it may also present as an aggressive tumor
prone to metastasis or recurrence. It is impossible to determine
whether BCC of the prostate is of the indolent or aggressive type
at the time of early-stage diagnosis; however, some reports suggest
that a predominant basaloid component may be associated with a poor
prognosis (6,14).
According to the previous literature, radiation
therapy, chemotherapy and hormone therapy have been included in the
treatment in addition to surgery. Tuan et al reported the
only case of BCC of the prostate where complete remission was
achieved by a combination of chemotherapy and radiotherapy
(9), but the efficacy of these
treatment options has not yet been established. Therefore, due to
the possibility of an aggressive tumor and the lack of effective
treatment options, radical surgery should be considered if BCC of
the prostate is diagnosed at an early stage and a basaloid
component is detected. In the present case, the possibility of an
aggressive potential could not be excluded, as a basaloid component
was detected in the biopsy specimen and imaging examination
revealed that the BCC was confined to the prostate; therefore,
retropubic radical prostatectomy was selected as the treatment. An
adenoid cystic-like tumor component was also identified in the
surgical specimen, but the basaloid component was predominant.
These pathological findings suggested the possibility of a poor
prognosis if curative treatment was not selected.
Invasion of the bladder cancer cells into the
prostate was included in the differential diagnosis of BCC of the
prostate (15). Since this patient
had a history of CIS of the bladder, immunostaining of the biopsy
specimen was performed. The results of immunostaining demonstrated
that the tumor cells tested negative for cytokeratin (CK)7 and
CK20, which are usually expressed in urothelial carcinoma cells
(16). Furthermore, random biopsy
was performed, and it was confirmed that CIS of the bladder had not
recurred. The absence of immunoreactivity with antibodies against
CK7 and CK20 and the results of the random biopsy of the bladder
confirmed that the CIS of the bladder had not invaded the
prostate.
BCC of the prostate is a rare tumor and an optimal
treatment has not yet been established. The present case report and
a review of the relevant literature suggest that radical surgery
must be considered if BCC of the prostate is diagnosed at an early
stage due to its aggressive potential, particularly if it includes
a predominant basaloid component.
Acknowledgements
Not applicable.
Funding
No funding was received.
Authors' contributions
GT and TK were part of the treatment team for the
patient. TS was the attending physician and surgeon of the patient
and was the first author of the manuscript.
Ethics approval and consent to
participate
Not applicable.
Availability of data and materials
Not applicable.
Consent for publication
The patient provided written informed consent to the
publication of the case details and any associated images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
McKenney JK, Amin MB, Srigley JR, Jimenez
RE, Ro JY, Grignon DJ and Young RH: Basal cell proliferations of
the prostate other than usual basal cell hyperplasia: A
clinicopathologic study of 23 cases, including four carcinomas,
with a proposed classification. Am J Surg Pathol. 28:1289–1298.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Iczkowski KA, Ferguson KL, Grier DD,
Hossain D, Banerjee SS, McNeal JE and Bostwick DG: Adenoid
cystic/basal cell carcinoma of the prostate: Clinicopathologic
findings in 19 cases. Am J Surg Pathol. 27:1523–1529. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ayyathurai R, Civantos F, Soloway MS and
Manoharan M: Basal cell carcinoma of the prostate: Current
concepts. BJU Int. 99:1345–1349. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Begnami MD, Quezado M, Pinto P, Linehan WM
and Merino M: Adenoid cystic/basal cell carcinoma of the prostate:
Review and update. Arch Pathol Lab Med. 131:637–640.
2007.PubMed/NCBI
|
|
5
|
Ali TZ and Epstein JI: Basal cell
carcinoma of the prostate: A clinicopathologic study of 29 cases.
Am J Surg Pathol. 31:697–705. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Komura K, Inamoto T, Tsuji M, Ibuki N,
Koyama K, Ubai T, Azuma H and Katsuoka Y: Basal cell carcinoma of
the prostate: Unusual subtype of prostatic carcinoma. Int J Clin
Oncol. 15:594–600. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Bohn OL, Rios-Luna NP, Navarro L,
Duran-Peña A and Sanchez-Sosa S: Basal cell carcinoma of the
prostate gland: A case report and brief review of the basal cell
proliferations of the prostate gland. Ann Diagn Pathol. 14:365–368.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ahuja A, Das P, Kumar N, Saini AK, Seth A
and Ray R: Adenoid cystic carcinoma of the prostate: Case report on
a rare entity and review of the literature. Pathol Res Pract.
207:391–394. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Tuan J, Pandha H, Corbishley C and Khoo V:
Basaloid carcinoma of the prostate: A literature review with case
report. Indian J Urol. 28:322–324. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Stearns G, Cheng JS, Shapiro O and Nsouli
I: Basal cell carcinoma of the prostate: A case report. Urology.
79:e79–e80. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Chang K, Dai B, Kong Y, Qu Y, Wu J, Ye D,
Yao X, Zhang S, Zhang H, Zhu Y, et al: Basal cell carcinoma of the
prostate: Clinicopathologic analysis of three cases and a review of
the literature. World J Surg Oncol. 11:1932013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Tsuruta K, Funahashi Y and Kato M: Basal
cell carcinoma arising in the prostate. Int J Urol. 21:1072–1073.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Simper NB, Jones CL, MacLennan GT,
Montironi R, Williamson SR, Osunkoya AO, Wang M, Zhang S, Grignon
DJ, Eble JN, et al: Basal cell carcinoma of the prostate is an
aggressive tumor with frequent loss of PTEN expression and
overexpression of EGFR. Hum Pathol. 46:805–812. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Hudson E, Rashid M, Carter AC and Lester
JF: Basaloid carcinoma of the prostate: A case report and review of
the literature. Eur J Cancer Care (Engl). 17:509–511. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Segawa N, Tsuji M, Nishida T, Takahara K,
Azuma H and Katsuoka Y: Basal cell carcinoma of the prostate:
Report of a case and review of the published reports. Int J Urol.
15:557–559. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Bassily NH, Vallorosi CJ, Akdas G, Montie
JE and Rubin MA: Coordinate expression of cytokeratins 7 and 20 in
prostate adenocarcinoma and bladder urothelial carcinoma. Am J Clin
Pathol. 113:383–388. 2000. View Article : Google Scholar : PubMed/NCBI
|