Introduction
Castleman's disease is a rare benign disorder of
unknown etiology characterized by proliferation of lymphoid tissues
(1). Although Castleman's disease
has been found in lymphatic tissues of the chest, neck, abdomen,
and pelvis, its retroperitoneal localization is rare; further, its
localization in the pelvic retroperitoneum is extremely rare
(2,3). To date, only 14 cases of
retroperitoneal localization of Castleman's disease occurring in
female pelvis have been documented in the English literature
(Table I) (4-17).
The pre-operative diagnosis of pelvic retroperitoneal Castleman's
disease is difficult, and most cases have been diagnosed based on
post-operative pathological examination. Furthermore, due to the
limited number of cases described, the appropriate clinical
management strategy for this disease is not yet established.
Herein, we report a rare case of Castleman's disease localized in
the female pelvic retroperitoneum, which was completely resected by
laparoscopic surgery.
 | Table IPreviously reported cases of
Castleman's disease in the female pelvic retroperitoneum since 1962
in English literature. |
Table I
Previously reported cases of
Castleman's disease in the female pelvic retroperitoneum since 1962
in English literature.
| Author, year | Age, years | Disease site | Tumor size | Treatment | (Refs.) |
|---|
| Latters and Pachter,
1962 | 29 | Pre-sacral | 5.0x2.5x2.0 cm | Abdominal
resection | (4) |
| Giaretta et
al, 1971 | 37 | Para-iliac
vessel | 9.0 cm | Abdominal
resection | (5) |
| Emson, 1973 | 14 | Para-iliac
vessel | not specified | Abdominal biopsy | (6) |
| Bainbridge 1976 | 21 | Para-iliac
vessel | 8.0x5.0x4.0 cm | Abdominal
resection | (7) |
| Tanaka et al,
1976 | 36 | Para-iliac
vessel | 9.0x8.0x5.0 cm | Abdominal
resection | (8) |
| Kumar and
Shah, 1979 | 19 | Adherent to
ovary | 10.0x9.0x3.0 cm | Abdominal
resection | (9) |
| Goodman et al,
1983 | 17 | Pre-sacral | 8.0x5.0x4.0 cm | Abdominal
resection | (10) |
| Ylinen et al,
1995 | 26 | Retro pubic | 5.0x4.0x4.0 cm | Abdominal
resection | (11) |
| MacDonald et
al, 1996 | 58 | Sigmoid colon
mesentery | 8.0x4.0 cm | Abdominal
resection | (12) |
| Gaunt et al,
2002 | Not specified | Pre-sacral | 6.0 cm | Abdominal
resection | (13) |
| Nakamura et
al, 2004 | 30 | Para-iliac
vessel | 6.5x5.0x4.0 cm | Abdominal
resection | (14) |
| Sato, 2013 | 22 | Para-sacral
vessel | 9.5x7.0x7.0 cm | Abdominal
resection | (15) |
| Lee et al,
2015 | 27 | Para-iliac
vessel | 7.0 cm | Laparoscopic
resection | (16) |
| Schelble and
Merritt, 2019 | 13 | Pelvic side
wall | 5.5x3.5x2.0 cm | Abdominal
resection | (17) |
| Present study | 47 | Para-iliac
vessel | 5.2 cm | Laparoscopic
resection | - |
Case report
A 47-year-old gravida 5, para 3 female was referred
to our hospital because of a pelvic mass accidentally found by
radiological examination at a health checkup. She had no systemic
symptoms such as pelvic pain, fatigue, fever, or weight loss.
Transvaginal ultrasound examination revealed a 7.8 cm-sized simple
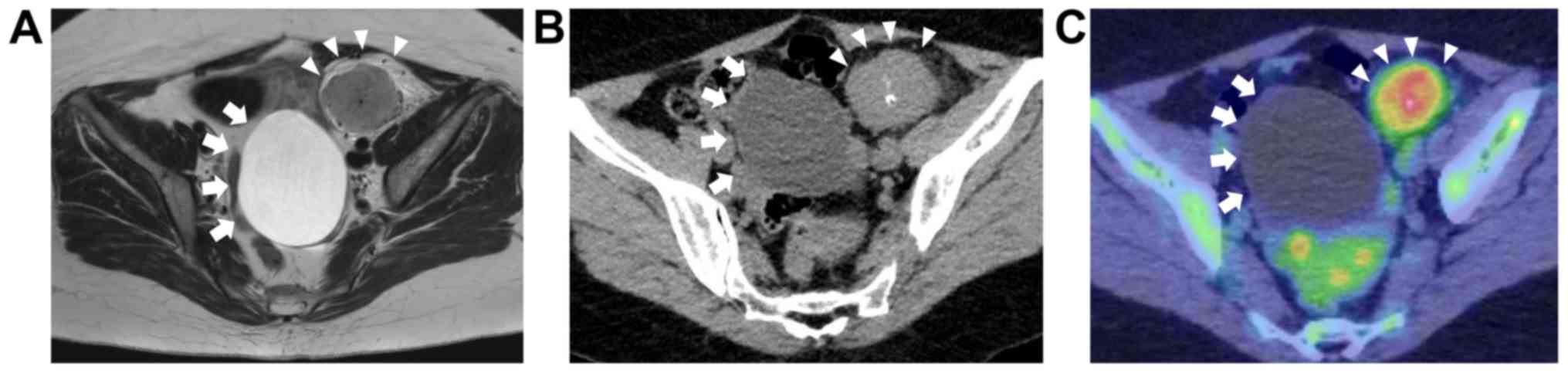
cystic tumor on the left ovary. Magnetic resonance imaging (MRI)
revealed an 8.2 cm-sized ovarian cyst and a 5.2 cm-sized
heterogeneously hyper-enhanced solid tumor in the retroperitoneal
space of the left pelvis on T2-weighted (T2W) images (Fig. 1A). On T1-weighted (T1W) images, the
pelvic retroperitoneal tumor was homogeneous and nearly isointense
to uterus in signal intensity. Computed tomography (CT) revealed
partial calcification of both the cystic and solid pelvic
retroperitoneal tumors, with no pelvic lymph node swelling
(Fig. 1B).
18F-fluoro-2-deoxy-D-glucose positron emission
tomography combined with computed tomography (FDG-PET/CT) detected
high radiotracer uptake by the retroperitoneal tumor [maximum
standardized uptake value (SUVmax): 4.14], with no distant
metastases (Fig. 1C). Serum levels
of carcinoembryonic antigen (CEA), cancer antigen (CA) 19-9, CA125,
and interleukin 6 (IL-6) were within the normal range. Except for
the above-mentioned findings, serum biochemical and clotting
studies were within the normal limits.
A laparoscopic surgery was performed for both pelvic
retroperitoneal tumor and left ovarian cyst. Intraoperative
examination evidenced that the pelvic retroperitoneal tumor was
most likely to represent a lymph node enlargement at the left
external iliac area and was associated with mobile and smooth left
ovarian tumor (Fig. 2A). A
laparoscopic monopolar device was applied to excise the pelvic
peritoneum and expose the pelvic mass, and a bipolar device was
subsequently applied to ensure coagulation around the tumor.
Although it was closely located to the external iliac vessels, no
direct vascular invasion was noted in the tumor and its surface was
well circumscribed (Fig. 2B). This
way, tissues around the tumor could be dissected and the feeding
vessel desiccated from the external iliac artery with limited
bleeding. No enlarged lymph nodes were found at the retroperitoneal
region. These tumors were placed in a plastic bag and removed
through the umbilical trocar site.
Macroscopically, the pelvic retroperitoneal tumor
was rubbery firm, with the cut surface appearing soft, finely
granular, and pale yellow in color (Fig.
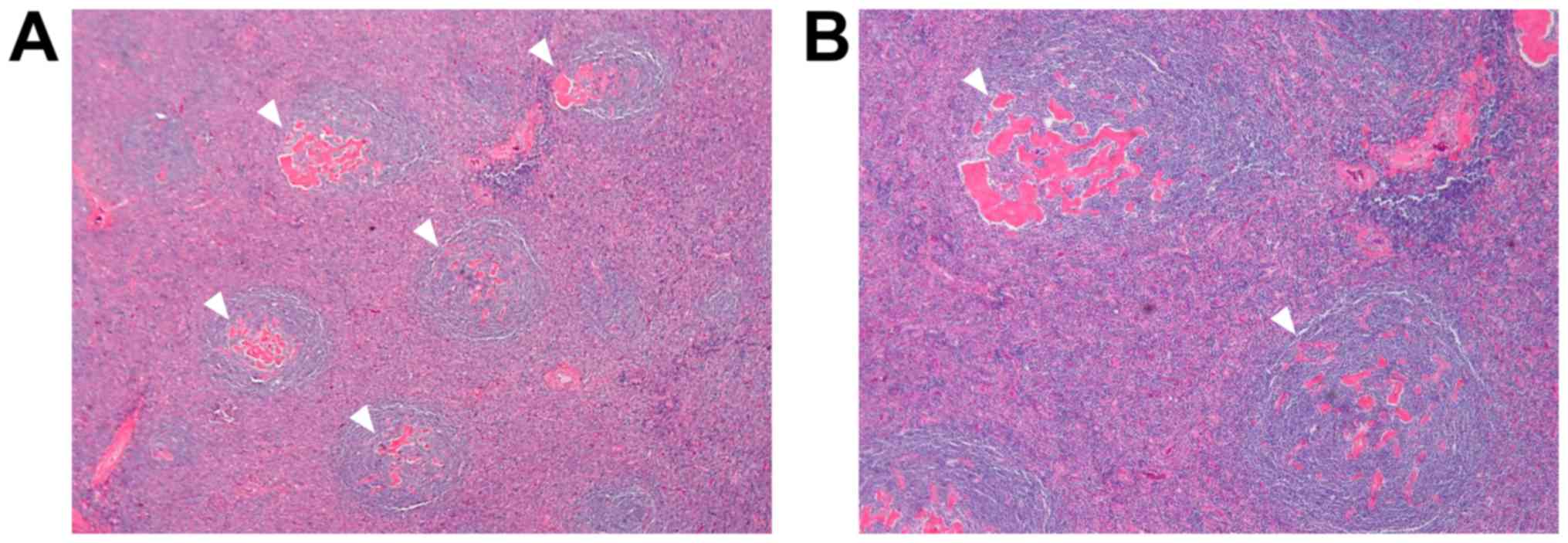
2C). Microscopic examination revealed marked follicular
hyperplasia with concentric layering of mantle-zone lymphocytes
(Fig. 3). Most follicles were
hyalinized and atrophic, with an expanded follicular dendritic cell
network. Paraffin section immunostain showed mixed populations of
CD20-immunoreactive B cells and CD3-immunoreactive T cells and
negative staining for immunoglobulin G4 (IgG4) (data not shown).
The pathological diagnosis was unicentric and hyaline vascular type
of Castleman's disease localized in the pelvic retroperitoneum. The
cystic tumor in the left ovary was diagnosed as a benign simple
cyst. The postoperative course was uneventful, and the patient was
discharged from the hospital on postoperative day 5. Six months
after diagnosis, there was no evidence of local recurrence or
systemic disease.
Discussion
The present case refers to an incidentally found
unicentric and hyaline vascular type of Castleman's disease
localized in the pelvic retroperitoneum, with no symptoms.
Castleman's disease is a rare, benign lymphoproliferative disorder
originally described by Castleman and Towne in 1954(18). Castleman's disease includes
unicentric and multicentric forms, which are thought to represent
distinct clinical entities with different risk factors,
presentation, treatment response, and long-term survival (19). The most common-unicentric-form, is
often found in both males and females aged 20-30 years and presents
asymptomatically or with compressive symptoms related to the mass
(20). Unicentric Castleman's
disease affects a single group of lymph nodes, often in the chest
or abdomen, and is generally cured with surgical resection of the
involved group of lymph nodes (19).
Multicentric Castleman's disease is more often found in adults aged
50-60 years and is likely to present with systemic symptoms,
including fever, malaise, night sweats, weakness, weight loss, and
peripheral lymphadenopathy (20).
Multicentric Castleman's disease may also be found in
immunosuppressed patients infected with HIV and human herpesvirus
8(21). Multicentric Castleman's
disease tends to behave aggressively, similarly to a lymphoma, and
is less likely to be cured by surgical resection (19). Castleman's disease can also be
grouped into hyaline vascular and plasma cell types according to
histopathological subsets (22). The
hyaline vascular type accounts for 90% of cases. Recently, a mixed
type of hyaline vascular and plasma cell types has also been
reported (23).
Preoperative diagnosis of Castleman's
disease-especially when located in the pelvis-is difficult due to
its very low frequency and nonspecific radiographic signs. Benign
retroperitoneal tumors are relatively uncommon, comprising only
approximately 20% of all primary retroperitoneal neoplasms
(24). The differential diagnosis of
a retroperitoneal mass includes lymphoma, sarcoma, metastasis,
neural tumor, and granulomatous disease (2). Among these entities, lymphoma is the
most difficult to distinguish from Castleman's disease because of
its similar homogeneity on radiographic findings. CT generally
demonstrates a homogeneous soft tissue mass, and both histological
types of Castleman's disease show contrast enhancement (25). Variable patterns of calcification can
be seen in CT in up to 31% of cases, including the present one
(25). On MRI, unicentric
Castleman's disease exhibits mild hyperintensity in T1W and T2W
imaging compared with skeletal muscle (26). MRI is particularly suitable to
evaluate the extent of the lesion and its relationship to adjacent
structures, but it is less sensitive to calcifications (2). In FDG-PET/CT, Castleman's disease
demonstrates only moderate radiotracer uptake with reported SUVmax
between 4.7 and 5.8 (27,28). Most active lymphomas express much
higher average SUVs than FDG-avid lymph nodes in Castleman's
disease (29,30); however, some degree of overlap with
low- and intermediate-grade lymphoma is possible. Murphy et
al (30) emphasized that, in
several cases of low- and intermediate-grade lymphomas, SUVs are
higher than those found in Castleman's disease. Retroperitoneal
sarcoma and lymphoma are more likely to demonstrate higher apparent
diffusion coefficient values (ADC) on MRI (31) and higher 18F-FDG avidity
(SUVmax, 4.2-23.6) on PET/CT (32).
In the present case, MRI allowed us to conclude that the mass was
located on the retroperitoneal space and not in the ovary, and
FDG-PET/CT helped to narrow down the differential diagnosis,
particularly considering lymphoma and sarcoma.
In the English literature, a small number of
Castleman's disease cases have been reported in the female pelvis
(4-17),
with clinical characteristics resembling a tubo-ovarian abscess,
endometriotic cyst, or dermoid cyst of ovarian origin. The mean age
and tumor size of Castleman's disease cases were 26.5 (13-58) and
7.5 cm (5.0-10.0 cm), respectively (Table I). Due to the low incidence of
Castleman's disease in the female pelvis and the clinical
resemblances with other pelvic masses, it may be difficult to
diagnose Castleman's disease in initial evaluation and the case may
be included in the differential diagnosis of pelvic mass. In most
cases, pelvic Castleman's disease presents as a pelvic mass with
clinical suspicion of adnexal tumor. Fortunately, this case of
pelvic retroperitoneal Castleman's disease was associated with an
ipsilateral benign ovarian cyst, which also helped to diagnose the
mass as retroperitoneal-and not ovarian-in origin. Castleman's
disease is an important consideration in the differential diagnosis
of pelvic masses in women.
The appropriate clinical management strategy for
pelvic retroperitoneal Castleman's disease has not been
established, as clinical experience with such cases is limited.
While only limited successful management with steroids and
cytotoxic agents has been reported (33), surgical excision has been considered
as standard therapy. A wide, complete excisional margin is
preferred due to the lesion's infiltrative pattern and potential
for recurrence. Incomplete resection may be associated with poorer
outcome (34). Although Castleman's
disease has a benign histology, surgical excision is not always
easy. As observed in the present case, hypervascularity is
frequently associated with massive hemorrhage at excision. Pelvic
retroperitoneal Castleman's disease is often accompanied by
remarkable fibrous adhesion to the surrounding tissues (35). To avoid massive hemorrhage, it is
essential to fully dissect tissues around the tumor and have enough
space to desiccate the feeding vessel originated from large vessel.
A thorough pre-operative discussion about radiological examination
could be useful for assisting the preparation for surgical
resection. Although several cases of unicentric Castleman's disease
in the abdominal cavity treated laparoscopically have been reported
(36,37), to the best of our knowledge, only one
report on female pelvic retroperitoneal Castleman's disease treated
by laparoscopy is available in literature (Table I) (16). As some masses are well vascularized
and adjacent to the great vessels, laparoscopy can provide
magnified images that facilitate and secure dissection.
In summary, a rare case of female pelvic
retroperitoneal Castleman's disease was found, for which a
laparoscopic surgery was performed. Gynecologists should be aware
of the possible event of such rare cases, and available surgical
interventions should be fully discussed. Laparoscopic surgery may
be a possible treatment option for such a rare condition.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets uesd and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Author's contributions
KN, NI and KI conceived and designed this case
report. KN, NI and KI wrote the initial draft of the report. HM, TN
and TY acquired the data in the surgical field. NO and YM acquired
the data in the diagnostic imaging and pathological examination.
All authors have read and approved the final version of the
manuscript.
Ethics approval and consent to
participate
Written informed consent for surgery was obtained
from the patient.
Patient consent for publication
Written informed consent for publication of the
present report was obtained from the patient.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Castleman B, Iverson L and Menendez VP:
Localized mediastinal lymph node hyperplasia resembling thymoma.
Cancer. 9:822–830. 1956.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Bonekamp D, Horton KM, Hruban RH and
Fishman EK: Castleman disease: The great mimic. Radiographics.
31:1793–1807. 2011.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Aygun C, Tekin MI, Demirhan B,
Peskircioglu CL, Agildere M and Ozkardes H: A case of incidentally
detected Castleman's disease with retroperitoneal paravertebral
localization. Int J Urol. 7:22–25. 2000.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Latters R and Pachter MR: Benign lymphoid
masses of probable hamartomatous nature. Analysis of 12 cases.
Cancer. 15:197–214. 1962.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Giaretta MI, Hyun J and Gibbons JM Jr:
Angiomatous lymphoid hamartoma as a pelvic mass. A case report.
Obstet Gynecol. 38:391–394. 1971.PubMed/NCBI
|
|
6
|
Emson HE: Extrathoracic angiofollicular
lymphoid hyperplasia with coincidental myasthenia gravis. Cancer.
31:241–245. 1973.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Bainbridge ET: Angiomatous lymphoid
hamartoma of the pelvis. Br J Obstet Gynaecol. 83:823–826.
1976.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Tanaka T, Kobayashi K, Sho T and Hamazaki
M: Castleman's lymphoma among Japanese population. Acta Pathol Jpn.
26:547–559. 1976.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Kumar D and Shah S: Angiomatous lymphoid
hamartoma or pseudolymphoma of pelvic retroperitoneum: Clinical
significance and evaluation of pelvic ureter. Urology. 13:677–681.
1979.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Goodman K, Baim RS, Clair MR and Perkes
EA: Angiomatous lymphoid hamartoma of the pelvis. Characteristic
calcification and computed tomographic appearance. Radiology.
146(728)1983.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Ylinen K, Sarlomo-Rikala M and Laatikainen
T: Pelvic Castleman disease mimicking an adnexal tumor. Obstet
Gynecol. 85:894–897. 1995.PubMed/NCBI View Article : Google Scholar
|
|
12
|
MacDonald SR, Lurain JR, Hoff F,
Variakojis D and Fishman DA: Castleman disease presenting as a
pelvic mass. Obstet Gynecol. 87:875–877. 1996.
|
|
13
|
Gaunt GA, Gostout BS, Remstein E and Cliby
WA: Pelvic Castleman disease presenting as vaginal occlusion.
Obstet Gynecol. 100:1082–1085. 2002.
|
|
14
|
Nakamura Y, Tokuyama O, Muso A, Kawamura
N, Yasui T and Ishiko O: Asymptomatic pelvic Castleman disease in
an infertile woman: Case report. Arch Gynecol Obstet. 269:156–158.
2004.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Sato A: Castleman's disease in the pelvic
retroperitoneum: A case report and review of the Japanese
literature. Int J Surg Case Rep. 4:19–22. 2013.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Lee J, Paek J, Lee YH, Kong TW, Chang SJ
and Ryu HS: Pelvic Castleman's disease presenting as an adnexal
tumor in a young woman. Obstet Gynecol Sci. 58:323–326.
2015.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Schelble AP and Merritt DF: Pelvic
Castleman's disease presenting as an adnexal mass in an adolescent.
J Pediatr Adolesc Gynecol. 32:86–89. 2019.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Castleman B and Towne VW: Case records of
the Massachusetts General Hospital: Case No. 40231. N Engl J Med.
250:1001–1005. 1954.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Talat N, Belgaumkar AP and Schulte KM:
Surgery in Castleman's disease: A systematic review of 404
published cases. Ann Surg. 255:677–684. 2012.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Roca B: Castleman's disease. A review.
AIDS Rev. 11:3–7. 2009.PubMed/NCBI
|
|
21
|
Shah D, Darji P, Lodha S and Bolla S:
Unicentric Castleman's disease of abdomen. J Radiol Case Rep.
7:26–33. 2013.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Keller AR, Hochholzer L and Castleman B:
Hyaline-vascular and plasma-cell types of giant lymph node
hyperplasia of the mediastinum and other locations. Cancer.
29:670–683. 1972.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Seco JL, Velasco F, Manuel JS, Serrano SR,
Tomas L and Velasco A: Retroperitoneal Castleman's disease.
Surgery. 112:850–855. 1992.PubMed/NCBI
|
|
24
|
Takihara H, Yamakawa G, Baba Y, Takahashi
M and Ishihara T: Castleman disease. Unusual retroperitoneal
location indistinguishable from malignant tumor in preoperative
angiographic appearance. Urology. 41:162–164. 1993.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Chung EM, Biko DM, Arzamendi AM, Meldrum
JT and Stocker JT: Solid tumors of the peritoneum, omentum, and
mesentery in children: radiologic-pathologic correlation: From the
radiologic pathology archives. Radiographics. 35:521–546.
2015.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Ko SF, Hsieh MJ, Ng SH, Lin JW, Wan YL,
Lee TY, Chen WJ and Chen MC: Imaging spectrum of Castleman's
disease. AJR Am J Roentgenol. 182:769–775. 2004. View Article : Google Scholar
|
|
27
|
Hill AJ, Tirumani SH, Rosenthal MH,
Shinagare AB, Carrasco RD, Munshi NC, Ramaiya NH and Howard SA:
Multimodality imaging and clinical features in Castleman disease:
Single institute experience in 30 patients. Br J Radiol.
88(20140670)2015.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Lee ES, Paeng JC, Park CM, Chang W, Lee
WW, Kang KW, Chung JK and Lee DS: Metabolic characteristics of
Castleman disease on 18F-FDG PET in relation to clinical
implication. Clin Nucl Med. 38:339–342. 2013.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Oida Y, Shimizu K, Mukai M, Imaizumi T,
Nakamura M and Makuuchi H: FDG-PET and diffusion-weighted MR
imaging appearance in retroperitoneal Castleman's disease: A case
report. Clin Imaging. 32:144–146. 2008.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Murphy SP, Nathan MA and Karwal MW:
FDG-PET appearance of pelvic Castleman's disease. J Nucl Med.
38:1211–1212. 1997.PubMed/NCBI
|
|
31
|
Nakayama T, Yoshimitsu K, Irie H, Aibe H,
Tajima T, Shinozaki K, Nishie A, Asayama Y, Kakihara D, Matsuura S
and Honda H: Usefulness of the calculated apparent diffusion
coefficient value in the differential diagnosis of retroperitoneal
masses. J Magn Reson Imaging. 20:735–742. 2004.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Platzek I, Beuthien-Baumann B, Schramm G,
Maus J, Laniado M, Kotzerke J, van den Hoff J and Schuler M: FDG
PET/MR in initial staging of sarcoma: Initial experience and
comparison with conventional imaging. Clin Imaging. 42:126–132.
2017.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Summerfield GP, Taylor W, Bellingham AJ
and Goldsmith HJ: Hyaline-vascular variant of angiofollicular lymph
node hyperplasia with systemic manifestations and response to
corticosteroids. J Clin Pathol. 36:1005–1011. 1983.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Bowne WB, Lewis JJ, Filippa DA, Niesvizky
R, Brooks AD, Burt ME and Brennan MF: The management of unicentric
and multicentric Castleman's disease: A report of 16 cases and a
review of the literature. Cancer. 85:706–717. 1999.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Kiguchi H, Ishii T, Ishikawa Y, Masuda S,
Asuwa N, Yamafuji K and Takahashi T: Castleman's disease of the
abdomen and pelvis: Report of three cases and a review of the
literature. J Gastroenterol. 30:661–666. 1995.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Corcione F, Caiazzo P, Cuccurullo D,
Settembre A, Miranda L, Pirozzi F and Caracino V: Laparoscopic
treatment of unicentric Castleman's disease with abdominal
localization. J Laparoendosc Adv Surg Tech A. 15:400–404.
2005.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Brusciano L, Rossetti G, Maffettone V,
Napolitano V, Izzo D, Pizza F, Russo G, Russo F, del Genio G and
del Genio A: Laparoscopic treatment of an uncommon abdominal
localization of Castleman disease. Surg Laparosc Endosc Percutan
Tech. 15:241–243. 2005.PubMed/NCBI View Article : Google Scholar
|