Introduction
Lung cancer is the leading cause of cancer-related
mortality worldwide (1). The
incidence of heavy smoking is higher in those with psychiatric
disorders than that in the general population (2,3), and the
incidence of lung cancer in patients with schizophrenia is
significantly higher than that in the general population (4). In addition, the mortality rate in
patients with lung cancer with schizophrenia is higher than that in
the general population (5). However,
the cause for the increased lung cancer mortality rate in patients
with schizophrenia is poorly understood.
In general, it is challenging to determine the
appropriate diagnostic and treatment modality for patients with
lung cancer with psychiatric disorders due to difficulties in
obtaining their cooperation and consent for treatment. It is also
estimated that many patients with psychiatric conditions are not
properly diagnosed or treated due to their deteriorated mental
status during examination and treatment. Patients with lung cancer
who have schizophrenia have acceptable postoperative outcomes
(6), but studies on the outcome of
patients with lung cancer with severe psychiatric disorders who
need to be hospitalized are limited.
Our hospital in Japan has a Medical Psychiatric Unit
(MPU) where patients with psychiatric conditions who require
admission to a psychiatric facility are admitted for examination
and treatment of physical conditions (7). In the MPU, patients are co-managed by
both psychiatrists and physicians. This study aimed to evaluate the
clinical profiles and treatment results of patients with lung
cancer with severe psychiatric disorders who were admitted to the
MPU.
Patients and methods
We retrospectively reviewed the clinical profiles,
diagnostic methods, and treatment courses for patients who were
admitted to the MPU from January 2010 to December 2016 and
diagnosed with primary lung cancer. All patients had been
previously admitted to a psychiatric hospital to receive treatment
for severe psychiatric disorders diagnosed by the ICD-10
classification. The patients were referred to our hospital for
chest radiograph abnormalities, fever, difficulty of breathing, and
other reasons. All included patients were histologically diagnosed
with primary lung cancer. Staging was according to the 8th edition
of the Union for International Cancer Control TNM classification.
Kaplan-Meier curves were used to assess overall survival.
The patients' mental status was assessed daily by
their psychiatrists during hospitalization, and treatments for
their psychiatric disorders were adjusted as necessary. Written
informed consent was obtained from patients and/or their legal
guardian or key family member.
This study was conducted in accordance with the 1964
Declaration of Helsinki, as revised in 2013, and was approved by
the Ethical review board of Tachikawa Hospital (Tokyo, Japan).
Results
A total of 24 patients were included in the
analysis. The median patient age was 64 years (range, 53-75 years).
The patients were referred to our hospital for chest radiograph
abnormalities (n=17), fever (n=3), difficulty of breathing (n=2),
and other reasons (n=2). In total, 20 and 4 were diagnosed with
schizophrenia and mood disorders, respectively. All patients had
severe psychiatric symptoms requiring hospitalization in a
psychiatric facility for a long period of time even though their
psychotropic medications were adjusted. In patients with
schizophrenia, 5 patients took first-generation antipsychotics, 14
patients took second- generation antipsychotics, and one patient
took no medications. The histological type of cancer was
adenocarcinoma in 11 patients, squamous cell carcinoma in 8
patients, non-small cell lung carcinoma-not otherwise specified in
1 patient, and small cell lung cancer in 4 patients. The baseline
patient characteristics are shown in Table I. Fifteen patients were diagnosed via
bronchoscopy, while 6, 2, and 1 patient was diagnosed via CT-guided
percutaneous lung biopsy, surgical biopsy, and sputum cytology,
respectively. All patients had no family history on lung cancer. In
addition, there were 10, 2, 6, 3, and 3 patients who had clinical
stage I, II, IIIA, IIIB, and IV disease, respectively. Regarding
comorbidities, 3 patients had interstitial pneumonia or chronic
obstructive pulmonary disease, and 5 patients had diabetes
mellitus. The oxygenation level of all patients as assessed
according to arterial blood gas was normal. Echocardiography showed
that all patients were eligible for surgery.
 | Table IPatient characteristics. |
Table I
Patient characteristics.
| Patient
characteristics | No. of patients |
|---|
| Total enrolled | 24 |
| Age (years) | |
|
Median
(range) | 64 (53-75) |
| Sex | |
|
Male | 14 |
|
Female | 10 |
| Type of psychiatric
disorder | |
|
Schizophrenia | 20 |
|
Mood
disorder | 4 |
| ECOG performance
status (pre-treatment) | |
|
0 | 17 |
|
1 | 3 |
|
2 | 2 |
|
3 | 2 |
|
4 | 0 |
| Histology | |
|
Adenocarcinoma | 11 |
|
Squamous
cell carcinoma | 8 |
|
NSCLC-NOS | 1 |
|
Small-cell
lung cancer | 4 |
| Clinical stage (TNM
classification, 8th edition) | |
|
I | 10 |
|
II | 2 |
|
IIIA/IIIB | 6/3 |
|
IV | 3 |
| Comorbidity | |
|
Diabetes
mellitus | 5 |
|
Interstitial
pneumonia | 3 |
|
Chronic
obstructive pulmonary disease | 3 |
| Diagnostic
method | |
|
Bronchoscopy | 15 |
|
CT-guided
percutaneous lung biopsy | 6 |
|
Surgical
biopsy | 2 |
|
Cytology | 1 |
Regarding the type of treatment, 13, 4, 2, 1, and 4
patients underwent surgery, chemoradiotherapy, radiotherapy,
chemotherapy and received best supportive care (BSC), respectively
(Table II). Two patients with good
performance status (case 10 and 21) did not undergo treatment and
instead chose BSC based on an individual or family decision. Among
the 13 patients who underwent surgery, lobectomy was performed in
11, while segmentectomy of the left upper division and wedge
resection was performed in 1 patient each. Of the 4 patients with
small-cell lung cancer, 1 underwent chemoradiotherapy, 1 patient
underwent chemotherapy, and 2 patients received BSC.
 | Table IIPatient treatment course. |
Table II
Patient treatment course.
| Case | Age | Sex | Histology | Stage | Psyhiatric
disorder | PS | Length of hospital
stay (day) | Treatment | Survival | Survival time
(months) |
|---|
| 1 | 65 | F | Ad | IA1 | Schizophrenia | 0 | 29 | Surgery | Survival | 61.1 |
| 2 | 61 | F | Ad | IA1 | Schizophrenia | 0 | 24 | Surgery | Survival | 38.7 |
| 3 | 58 | M | Ad | IA2 | Schizophrenia | 0 | 24 | Surgery | Survival | 12.8 |
| 4 | 68 | F | Ad | IA2 | Schizophrenia | 0 | 34 | Surgery | Survival | 85.6 |
| 5 | 74 | F | Ad | IA3 | Mood disorder | 0 | 36 | Surgery | Death | 74.7 |
| 6 | 60 | M | Ad | IA3 | Schizophrenia | 0 | 26 | Surgery | Death | 22.5 |
| 7 | 62 | M | Ad | IA3 | Schizophrenia | 1 | 58 | Surgery | Survival | 13.1 |
| 8 | 55 | M | Ad | IIIA | Schizophrenia | 0 | 57 | Surgery | Survival | 7.3 |
| 9 | 62 | M | Ad | IIIA | Schizophrenia | 0 | 189 | Surgery | Survival | 4.4 |
| 10 | 75 | M | Ad | IIIA | Schizophrenia | 1 | 33 | Best supportive
care | Death | 3.9 |
| 11 | 69 | F | Ad | IVc | Schizophrenia | 3 | 20 | Best supportive
care | Death | 1.0 |
| 12 | 64 | M | Sq | IA2 | Schizophrenia | 0 | 92 | Surgery | Survival | 29.9 |
| 13 | 66 | M | Sq | IA2 | Schizophrenia | 0 | 46 | Surgery | Survival | 92.4 |
| 14 | 69 | M | Sq | IA3 | Schizophrenia | 0 | 102 | Surgery | Death | 19.5 |
| 15 | 59 | M | Sq | IIB | Schizophrenia | 0 | 40 | Surgery | Death | 76.7 |
| 16 | 64 | F | Sq | IIIA | Schizophrenia | 0 | 182 |
Chemoradiotherapy | Death | 14.2 |
| 17 | 73 | M | Sq | IIIA | Mood disorder | 2 | 227 |
Chemoradiotherapy | Death | 27.5 |
| 18 | 62 | F | Sq | IIIB | Schizophrenia | 0 | 73 | Radiotherapy | Death | 27.7 |
| 19 | 76 | F | Sq | IIIB | Schizophrenia | 2 | 86 | Radiotherapy | Survival | 6.0 |
| 20 | 74 | M | NSCLC-NOS | IIIB | Mood disorder | 0 | 53 |
Chemoradiotherapy | Death | 13.0 |
| 21 | 53 | M | SCLC | IIA | Schizophrenia | 0 | 43 | Best supportive
care | Death | 2.3 |
| 22 | 61 | F | SCLC | IIIA | Mood disorder | 0 | 153 |
Chemoradiotherapy | Survival | 64.1 |
| 23 | 73 | F | SCLC | IVa | Schizophrenia | 3 | 13 | Best supportive
care | Death | 0.8 |
| 24 | 63 | M | SCLC | IVa | Schizophrenia | 1 | 142 |
Chemoradiotherapy | Death | 6.6 |
Among those who underwent surgery, 5 cases of
postoperative complications were recorded: Aspiration pneumonia
(n=1), fistulous empyema (n=1), and psychosis (n=3) (Table III). In addition, grade 3/4 adverse
events (Common Terminology Criteria for Adverse Events, version 4)
occurred in 4 cases of chemoradiotherapy: Pneumonitis, 2 cases
(Grade 3); neutropenia, 3 cases (Grade 3, 1 case; Grade 4, 2
cases); and thrombocytopenia, 1 case (Grade 4). Complications
occurred in 2 cases of radiotherapy: Pneumonitis (n=1) and
psychosis (n=1).
 | Table IIITreatment complications. |
Table III
Treatment complications.
| Treatment
modality | Complication | No. of
patients |
|---|
| Surgery | Aspiration
pneumonia | 1 |
| | Fistulous
empyema | 1 |
| | Psychosis | 3 |
|
Chemoradiotherapy | Pneumonitis | 2 |
| | Neutropenia | 3 |
| |
Thrombocytopenia | 1 |
| Radiation | Aspiration
pneumonia | 1 |
| | Psychosis | 1 |
| Chemotherapy | Aspiration
pneumonia | 1 |
The median length of hospitalization was 40 days
(range, 24-170 days), 80 days (range, 73-86 days), 153 days (53-227
days), and 142 days among those who underwent surgery, radiation
therapy, chemoradiotherapy, and chemotherapy alone, respectively
(Table II). The prolonged
hospitalization was because it was difficult for the patients to
admit to our hospital regularly for chemotherapy or radiotherapy
due to the lack of caregiver manpower; thus, patients stayed in the
hospital until the entire treatment course was completed.
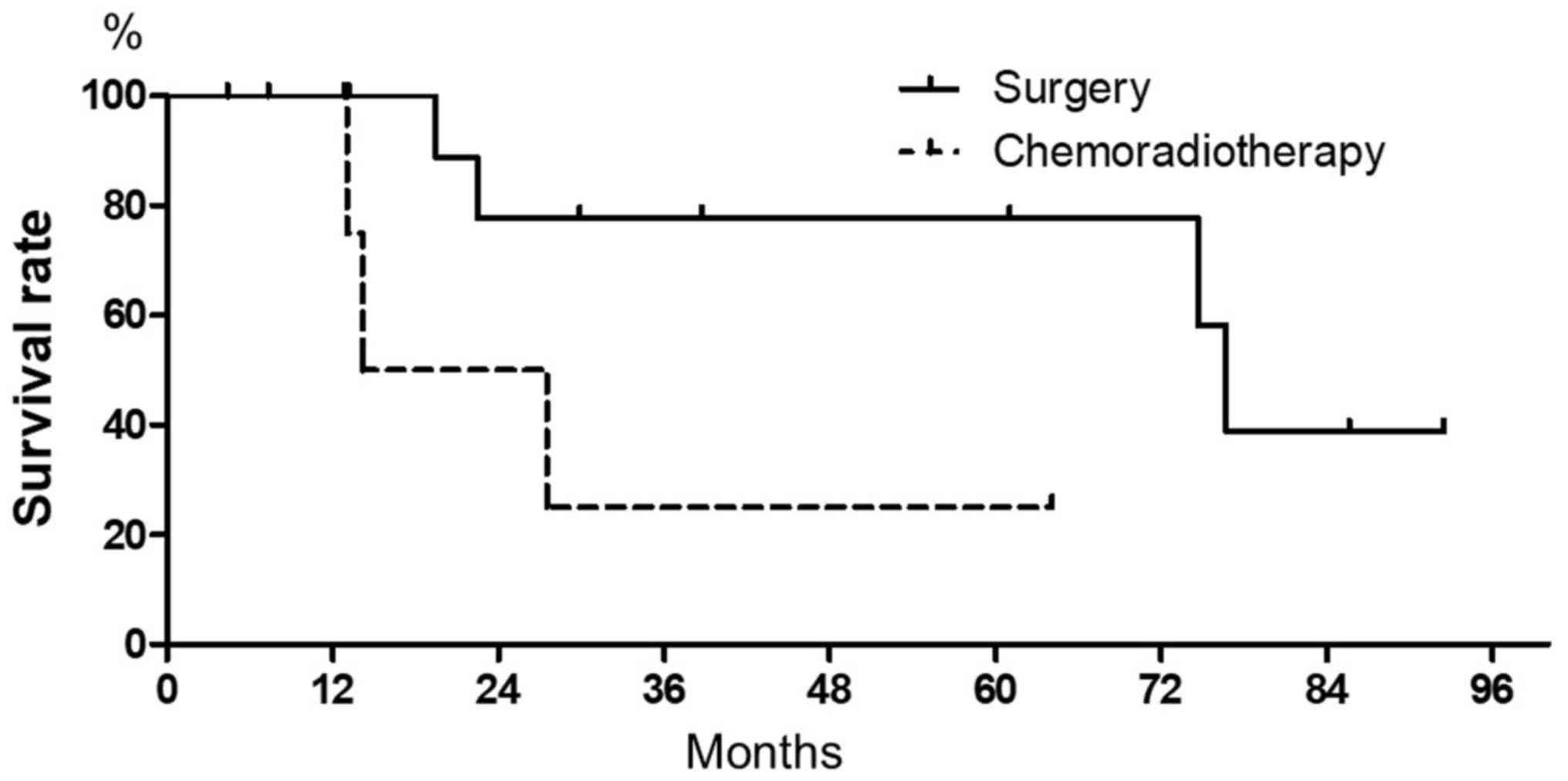
The median survival time was 76.7 months among those
who underwent surgery and 14.4 months among those who underwent
chemoradiotherapy (Fig. 1). All
patients and their families refused adjuvant chemotherapy and
further treatment for recurrent lung cancer; thus, the median
disease-free survival and progression-free survival could not be
evaluated.
Discussion
The prognosis of patients with lung cancer with
schizophrenia is considerably poor (5) because they generally do not receive
standard treatment modalities due to various reasons, including the
patient wishes, medical comorbidities, psychiatric symptoms, and
deficiency of subjective symptoms (8). Patients with psychiatric disorders are
difficult to diagnose and treated because they sometimes have poor
cooperation making it challenging to obtain consent for diagnosis
and treatment. The most important obstacle is psychomotor
excitement, which often includes impulsive or poorly controlled
activities. For example, positive symptoms including psychomotor
excitement are often displayed by patients with acute-phase
schizophrenia (9). Our MPU was
established for patients who have both physical and severe
psychiatric disorders (10). In the
MPU, the patients' mental status is assessed daily by
psychiatrists, and psychotropic drugs are prescribed to prevent
psychomotor excitement.
To our knowledge, this is the first study to
describe the profile of patients with lung cancer who have severe
psychiatric disorders and who are treated in the MPU. Our study
demonstrated the safety profile and tolerable outcome of patients
with these concomitant conditions. Invasive examinations and
treatment for lung cancer were performed in spite of the patients'
psychiatric disorders through cooperation with psychiatrists. There
were no complications during or after bronchoscopy and CT-guided
biopsy. The frequency and severity of all treatment complications
were found to be equivalent to those of lung cancer patients
without severe psychiatric disorders (11).
The American College of Chest Physicians and the
British Thoracic Society (BTS) recommends that forced expiratory
volume in one second (FEV1) and the diffusing capacity for carbon
monoxide (DLCO) be measured preoperatively in all patients with
lung cancer who are scheduled for surgical resection (12,13). The
risk of complications after lung resection has been shown to be
inversely related to both FEV1 and DLCO (14). The lung function could not be tested
in the patients because they were not able to follow instructions.
Tests for arterial blood gas have also been used to evaluate
pulmonary function before thoracic surgery to prevent subsequent
respiratory complications (15).
Therefore, the patients' lung function was assessed according to
their arterial blood gas levels in the MPU.
The mental status of 4 patients worsened during
treatment. Symptoms of psychosis included delirium and
restlessness. Psychosis of three patients appeared after the
reduction of psychotropic medications. However, these symptoms were
controlled by restorations to original medications and additions of
sedatives.
One past study reported that curative surgery can be
safely performed in lung cancer patients with schizophrenia, and a
high 5-year survival rate can be expected (6). In the current study, we also confirmed
that surgery can lead to long-term survival in patients with lung
cancer with severe psychiatric disorders. This indicates that
surgery should be considered as the primary treatment modality for
these patients.
In addition, the median survival time among patients
who underwent chemoradiotherapy was as short as that of lung cancer
patients without psychiatric disorder (16). The duration of other treatment
modalities was longer than that of surgery because of the
possibility of posttreatment complications and the necessity of
admission until the whole treatment is completed.
There are other issues that need to be considered in
the management of patients with lung cancer with psychiatric
disorders such as obtaining informed consent and the appropriate
follow-up strategy. In the current study, informed consent was
obtained from all patients and/or their legal guardian or key
family member because it is difficult to evaluate patients'
awareness of the disease mortality. Therefore, the legality of a
consent form obtained from patients with psychiatric conditions is
difficult to determine.
There are some limitations to this study. First,
this study was restricted to patients with histologically or
cytologically diagnosed lung cancer. The patients' abilities to
cooperate for an invasive biopsy showed that they may be more
likely to be candidates for cancer treatment. Second, the number of
patients in this study was small. Therefore, there were not any
statistical analyses. Especially, the number of patients who
underwent non-surgical treatment was limited. The effectiveness of
radiotherapy and chemotherapy for psychiatric patients is
inconclusive. Third, most of the patients were referred to our
hospital due to chest radiograph abnormalities, and chest
radiograph examinations were performed a few times yearly in the
previous hospital. The examinations may improve the outcome of lung
cancer patients with severe psychiatric disorder.
In summary, patients with early-stage lung cancer
with severe psychiatric disorders who are admitted to the MPU can
safely achieve long-term survival. Thus, we concluded that patients
with early-stage lung cancer should be treated as ordinary ones.
The specific psychiatric disorder should not limit the opportunity
of patients for receiving standard treatments for lung cancer.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
TTak and TTan conceived and designed the study.
TTak, TTan, AI, TY and HK developed the methodology. TTak, TTan, HT
and RT acquired the data. TTak, TTan, RT, AI, TY and HK analysed
and interpreted the data. TTak, TTan and HK wrote, revised and
reviewed the manuscript. TTan and HK supervised the study. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
The Ethical review board committee of Tachikawa
Hospital (Tokyo, Japan) approved the present study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Siegel R, Miller KD and Jemal A: Cancer
statistics, 2018. CA Cancer J Clin. 68:7–30. 2018.PubMed/NCBI View Article : Google Scholar
|
|
2
|
de Leon J and Diaz FJ: A meta-analysis of
worldwide studies demonstrates an association between schizophrenia
and tobacco smoking behaviors. Schizophr Res. 76:135–157.
2005.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Landow L, Szetela B and Know MA: Reducing
smoking among psychiatric inpatients: A survey of psychiatrists. Am
J Public Health. 85(1169)1995.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Catts VS, Catts SV, O'Toole BI and Frost
AD: Cancer incidence in patients with schizophrenia and their
first-degree relatives-A meta-analysis. Acta Psychiatr Scand.
117:323–336. 2008.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Tran E, Rouillon F, Loze JY, Casadebaig F,
Philippe A, Vitry F and Limosin F: Cancer mortality in patients
with schizophrenia: An 11-year prospective cohort study. Cancer.
115:3555–3562. 2009.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Obuchi T, Okabayashi K, Imakiire T, Yoneda
S and Iwasaki A: Outcomes of surgery in lung cancer patients with
schizophrenia. Surg Today. 44:855–858. 2014.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Miyagawa S, Inoue Y and Higa K: Medical
and psychiatric treatment in liaison psychiatric ward of a general
hospital. Jap J General Hospital Psychiatry. 24:245–252. 2012.(In
Japanese).
|
|
8
|
Mateen FJ, Jatoi A, Lineberry TW,
Aranguren D, Creagan ET, Croghan GA, Jett JR, Marks RS, Molina JR
and Richardson RL: Do patients with schizophrenia receive
state-of-the-art lung cancer therapy? A brief report.
Psychooncology. 17:721–725. 2008.PubMed/NCBI View
Article : Google Scholar
|
|
9
|
Carpenter WT Jr, Strauss JS and Bartko JJ:
The diagnosis and understanding of schizophrenia. Part I. Use of
signs and symptoms for the identification of schizophrenic
patients. Schizophr Bull. 37–49. 1974.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Fava GA, Wise TN, Molnar G and Zielezny M:
The medical-psychiatric unit: A novel psychosomatic approach.
Psychother Psychosom. 43:194–201. 1985.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Myrdal G, Gustafsson G, Lambe M, Horte LG
and Stahle E: Outcome after lung cancer surgery. Factors predicting
early mortality and major morbidity. Eur J Cardiothorac Surg.
20:694–699. 2001.PubMed/NCBI View Article : Google Scholar
|
|
12
|
British Thoracic Society; Society of
Cardiothoracic Surgeons of Great Britain and Ireland Working Party:
BTS guidelines: Guidelines on the selection of patients with lung
cancer for surgery. Thorax 56: 89-108, 2001.
|
|
13
|
Brunelli A, Kim AW, Berger KI and
Addrizzo-Harris DJ: Physiologic evaluation of the patient with lung
cancer being considered for resectional surgery: Diagnosis and
management of lung cancer, 3rd ed: American College of Chest
Physicians evidence-based clinical practice guidelines. Chest. 143
(Suppl 5):e166S–e190S. 2013.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Ferguson MK and Vigneswaran WT: Diffusing
capacity predicts morbidity after lung resection in patients
without obstructive lung disease. Ann Thorac Surg. 85:1158–1164;
discussion 1164-1165. 2008.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Tisi GM: Preoperative evaluation of
pulmonary function. Validity, indications, and benefits. Am Rev
Respir Dis. 119:293–310. 1979.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Yoon SM, Shaikh T and Hallman M:
Therapeutic management options for stage III non-small cell lung
cancer. World J Clin Oncol. 8:1–20. 2017.PubMed/NCBI View Article : Google Scholar
|