Introduction
Extramedullary nasal plasmacytoma (ENP) is a rare
disease characterized by localized monoclonal plasma cells
proliferation without apparent systemic involvement (1). This tumor represents 5-10% of all
plasma cell neoplasms (2) and,
despite it can be identified in different areas of the head and
neck, nasal cavity and nasopharynx are generally the structures
more affected from this type of cancer (3) maybe because nose is frequently exposed
to inflammation related to pollution and viral infection (4).
ENP represents 1% of all head cancers (5) and involves unspecific symptoms, such as
nasal obstruction due to inflammation of the nasal mucosa over the
tumor in the 80% of cases; sometimes this main symptom is
associated with epistaxis (35%), pain (20%), rhinorrhea (10%),
regional lymphadenopathy (10%), and more rarely with a paralysis of
the sixth cranial nerve (5%) (6).
The endoscopy appearance of ENP looks like as a
benign mass, especially in the early stages of the tumor (7), so it can be misdiagnosed as a polyp and
treated by corticosteroids. The steroid treatment, by reducing the
inflammation, improves part of the symptoms but it does not solve
the problem.
Still today, the etiopathology of ENP is not
completely understood, anyway researchers identified that smog and
viruses [commonly present in the upper airways tract (UA)] are
inflammatory agents able to induce carcinogenesis; this phenome
explains the presence of the tumors observed in this upper
respiratory tract (8,9). However, a correlation between the nasal
inflammation and ENP has not been identified yet.
In this case report, we described a rare case of ENP
that arose, 5 months after surgical removal of a nasal polyp, in
the same area from which the polyp has been resected. This clinical
evidence might support the association between inflammation and ENP
especially in patients over 70 years old that have been exposed to
the carcinogens for several years.
Case report
This case study was conducted in accordance with the
Declaration of Helsinki and all procedures followed the
Institutional Regulations Board (IRB) of Silvestrini Hospital
(Perugia, Italy). The study was approved by the IRB of Silvestrini
Hospital in January 2018, but no approval number was assigned in
accordance with the national laws. The patient signed a written
informed consent for the treatment of his data (publication of his
data and images).
A 72-year-old male patient was initially admitted to
the Department of Otolaryngology of Silvestrini University Hospital
in January 2018 due to a progressive, predominantly left-sided
nasal obstruction without other additional associated symptoms,
such as nasal discharge, epistaxis, or pain.
The patient never experienced any nasal issues until
7 months ago, when he started to perceive a prevalently unilateral
nasal obstruction. The man treated the symptomatology, as suggested
by his general doctor, by cortisone inhalation (two puffs three
times per day for 20 days). The patient, due to the persistence of
the symptoms even after the end of the inhalatory treatment,
arranged a consultation with an otolaryngologist.
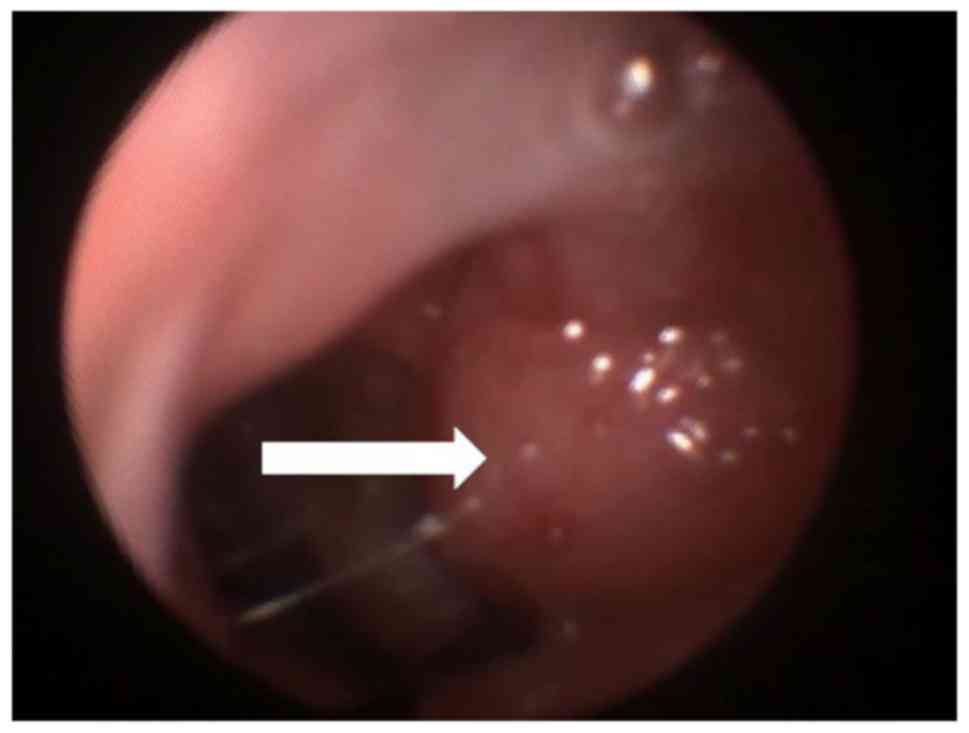
During the first clinical consultation, we did not
observe any evident craniofacial dysmorphism. An endoscopic
examination of the nose was performed to further investigate the
origin of the nasal obstruction. The exam revealed the presence of
a round mass located anteriorly in the left choana, which did not
present any connection with the nasal ostium. The lesion was
covered by normal mucosa. The finding occupied 30% of the nostril
(Fig. 1). No other pathological
findings were identified during the nasal endoscopy both in the
left and in the right choana. The rhinopharynx was disease free as
the mouth and the throat.
The mass, clinically diagnosed as unilateral left
nasal polyp, was surgically removed. Magnetic resonance imaging
(MRI) was not performed because of the clinical findings (symptoms
and signs) were supportive of a benign lesion. The tissue, was
sent, immediately after removal, to the pathologist to determine
its histologic nature. The conclusive report of the pathologist
described an inflammatory picture without signs of atypical mucosa,
typical aspect of a benign nasal polyp. The man completely solved
the nasal obstruction one week after the surgery.
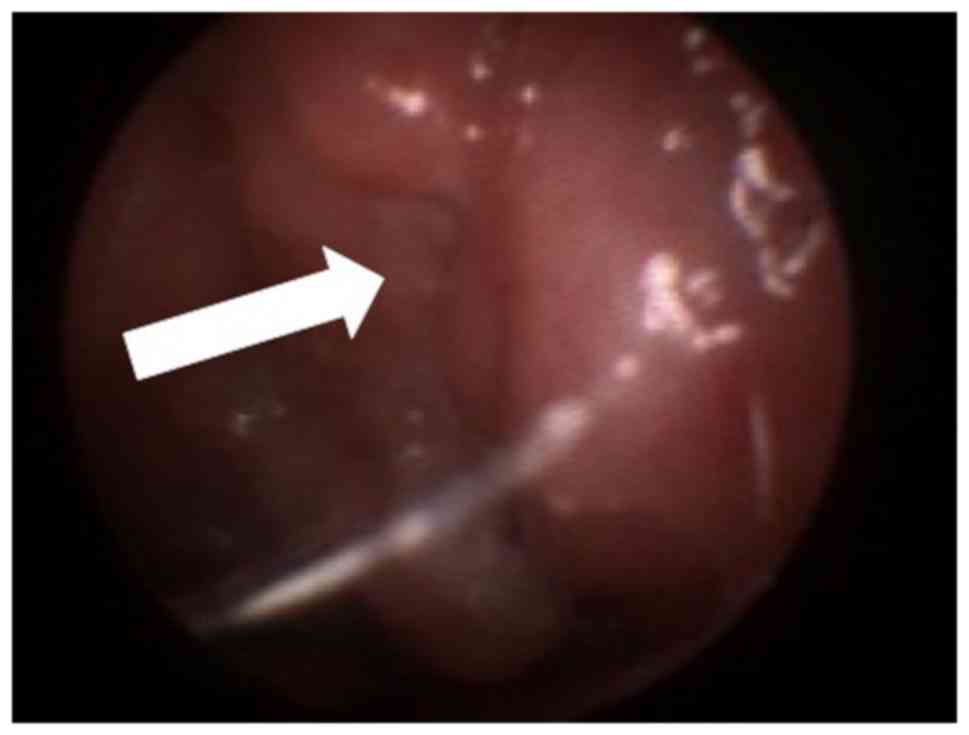
In the end of May, five months later the surgery,
the patient presented to our clinic due to the recurrence of the
left nasal obstruction. Also in this occasion, he did not present
any associated symptoms as nasal discharge, epistaxis, or pain. The
nasal-endoscopic investigation identified a pale-reddish round mass
into the left choana very close to the nostril. The mass, occupying
about 80% of the left nasal cavity (Fig.
2), presented a smooth surface covered by normal mucosa. The
remaining structures as nasopharynx, mouth, pharynx, larynx, neck,
ears appeared to be free of any disease.
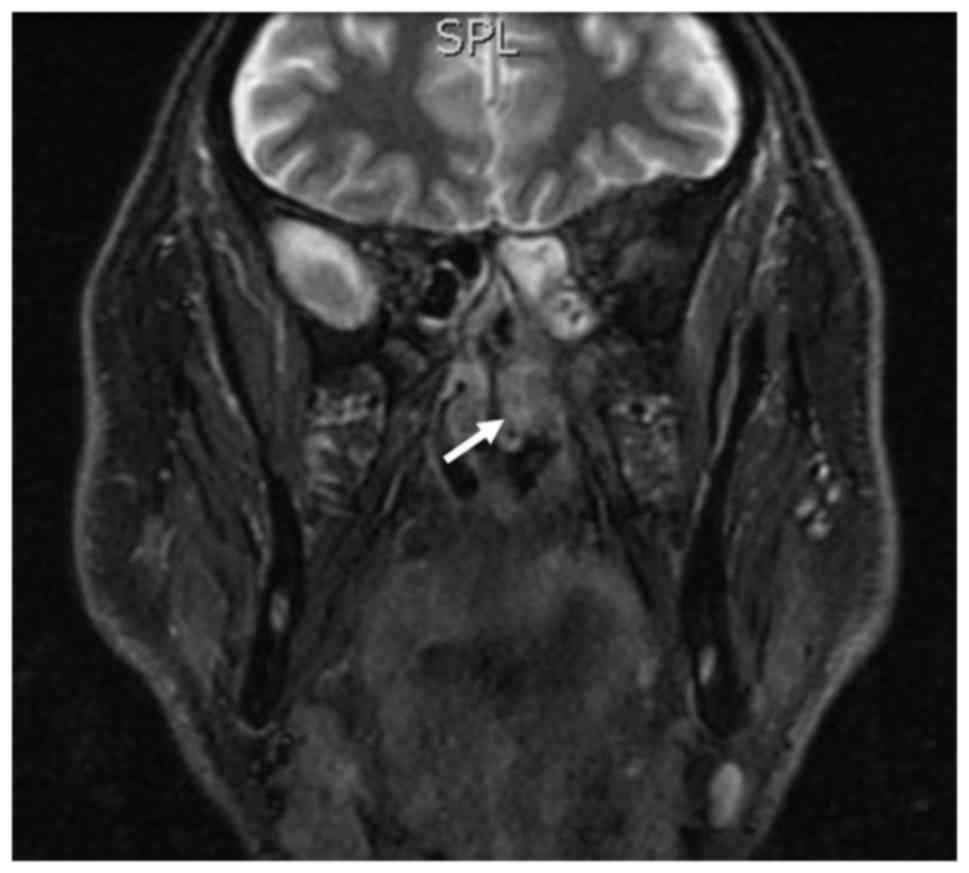
In this occasion, due to the recurrence of the
pathology, we decided, although the lesion seemed to be a benign
finding, to further investigated the patient by MRI. The exam
identified a mass in the left middle nasal cavity that extended to
the homolateral ethmoid bone with no bony erosion (Fig. 3).
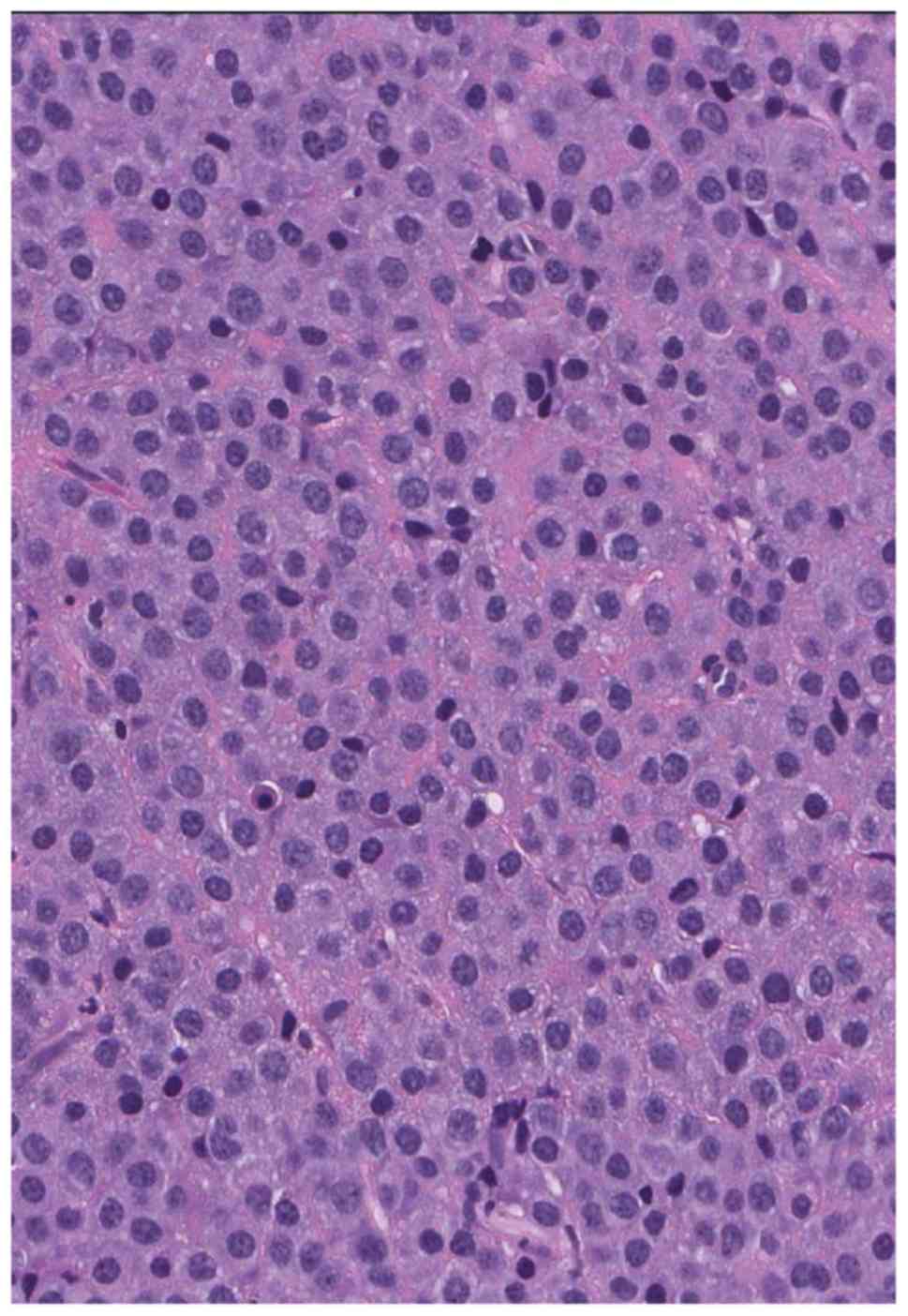
The tumor was completely removed by surgery through
endonasal endoscopy and, the operatory piece was sent to the
pathologist for cellular and biochemical analyses. The pathology
report described the following: i) Macroscopically, the neoplasm
consisted of multiple greyish fragments up to 0.8 cm that were
submitted in their entirety for histological review and ii)
microscopically, the mass consisted of a pure population of plasma
cells with basophilic cytoplasm and small, eccentric nuclei
(Fig. 4).
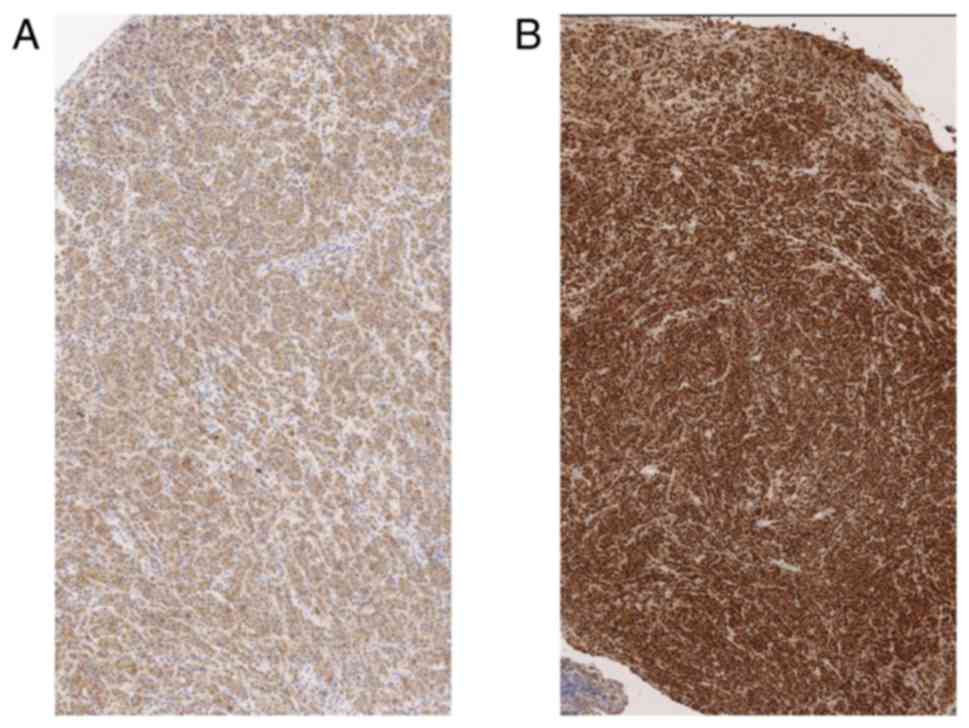
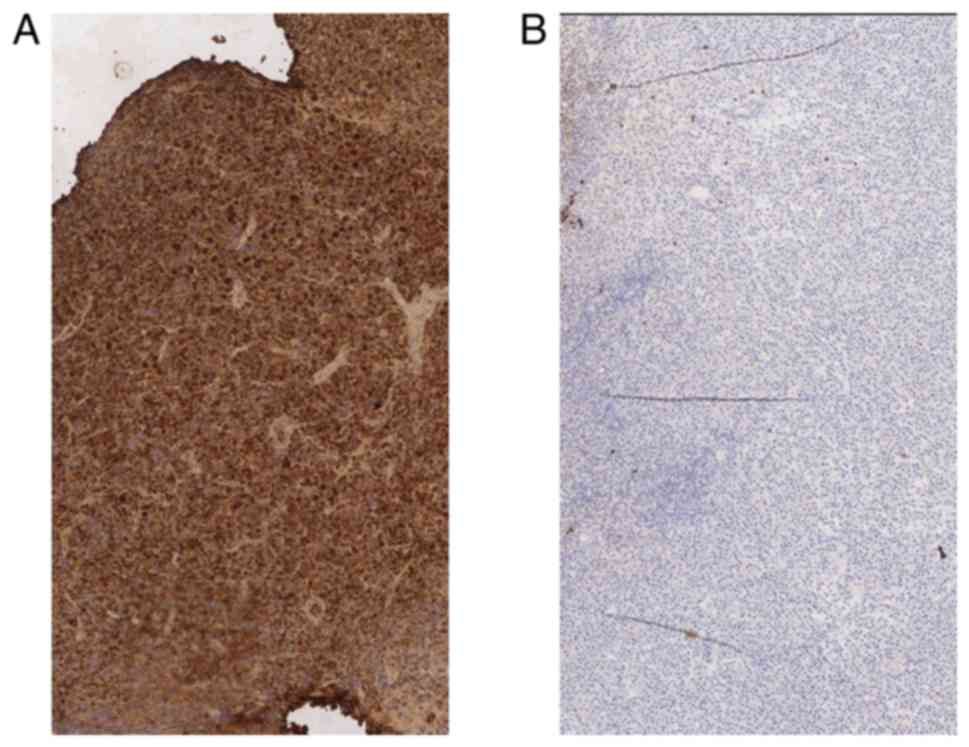
The immunohistochemistry, conducted on the tissue
surgically removed, confirmed the plasmatic nature of the cells,
including CD38 and MUM1 (Fig. 5A and
B) reactivity. The presence of the
monotypic immunoglobulin light chains κ and the absence of λ chain
(Fig. 6A and B) indicated a monoclonal process. Due to
these two findings the pathologist concluded that the removed mass
was an ENP (10).
Due to results observed on the second specimen, the
first one was re-analyzed for confirming the primary diagnosis of
polyp. The pathologist observed a mixed inflammatory infiltrate
consisting of neutrophil granulocytes, eosinophils and lymphocytes
on the background of an edematous stroma that confirmed the first
diagnosis and he did not retain necessary to perform
immunohistochemistry on the tissue due to the clarity of the
finding.
The patient, to complete the diagnostic process,
underwent a hematologic screening, protein electrophoresis, Bence
Jones proteinuria, and bone marrow analysis. Total body MRI and
PET/CT scans were performed to exclude a systemic condition. The
definitive diagnosis, based on the results of all overmentioned
investigations, was extramedullary plasmacytoma class 1(11).
After an oncologist consulting, we decided to avoid
additional treatments such as radio and chemotherapy, due to the
early stage of tumor and the absence of systemic disease, but to
monitor the patient with short follow ups. The patient was seen at
1 week, 2 weeks, and 6 months after surgery and consecutively every
6 months until May 2019 (date of last follow up). The nasal
endoscopy performed during the last control was negative for
disease recurrence, as well as the MRI results.
Discussion
We presented a patient suffering from nasal
obstruction as single isolated symptom-without additional
complaints, which in the first occasion was due to polyp in the
left choana as clearly identified by the endoscopic exam, while on
the second observation five months after polyp removal, was due to
a malign mass. The mass responsible of the nasal obstruction
appeared like a benign lesion at the endoscopic investigation and
the apparent benignity was confirmed by the absence of an
infiltrative process (typical of malignant lesion) in the MRI but,
the immunohistochemistry performed on the tissue removed by surgery
evidenced the typical findings of an ENP.
The bilateral nasal obstruction is a common symptom
both of the inflammation associated with a nasal polyp and, to the
one due to a neoplasia. In our patient, this symptom was correlated
with a benign lesion in the first observation and secondly, it was
symptomatic of an ENP in early stage. In both observations, the
patient never presented any other symptoms associated with the
nasal obstruction such as epistaxis (12,13),
rhinorrhea (12), anosmia (13), nasal discharge (12,13) or
sudden episode of obstructive sleep apnea syndrome (14). These symptoms have been widely
described in patients affected from nasal cancer (12-14).
In addition to this poor symptomatology, the
endoscopy, that we performed in both consultations, showed similar
benign aspects. The mass had a regular smooth shape, and it was
covered by normal mucosa during the first check-up (nasal polyp) or
slightly inflamed mucosa during the second one (ENP). Slight mucosa
inflammation is rarely observed in case of neoplasia, in fact,
usually, a malign lesion presents a mucosa with color alterations
(extreme redness) (11) a mass with
irregular shape (12-14),
and diffused ulcerations with or without active bleeding (13). A benign mass instead, appears with a
pink or grey in natural mucosa (15)
and the neoformation presents a regular round/ovular shape
(15).
Our patient performed MRI (an investigation
generally performed after nasal endoscopy to evaluate the
invasiveness and aggressiveness of the mass) that did not evidence
typical signs of cancer, such as bone erosion (16) or infiltration of close structures
(12).
Despite the two neoformations showed clinically
similar aspects, the results of pathologic analysis on their
histology were completely opposite. The tissue removed during the
first surgery presented an inflammatory aspect without signs of
cellular atypia, while the one that was taken off during the second
surgery presented κ chains characteristic of ENP (6,17).
The mass in the left choana recurred within five
months after the first surgery for polyp's asportation. The mass
arose exactly in the same point from which the polyp was previously
removed, looking like as the inflammation from the previous surgery
had stimulated an aberrant lymphocyte response.
The relationship between inflammation and cancer has
been previously described by other authors in particular related to
nose and paranasal sinus (4). The
researchers affirmed that episodes of recurrent inflammation could
be a precursor of nasopharyngeal carcinoma (4). However, the connection/correlation
between inflammation and ENP has not been investigated yet.
ENP is a B-cell neoplasm that generally occurs in
the UA. The nose, paranasal sinus, and oropharynx are commonly
exposed to smog that contains small carcinogenic particles
(8) and also to recurrent virus
infection (e.g., Epstein-Barr), whose role in cancer development
has been confirmed (9). Virus and
carcinogenic substance hyperstimulate B-cells to react for fighting
the host aggression in case of viral infection, or to fight the
inflammation in case of smog (18,19). The
rapid growth of B-lymphocyte due to recurrent inflammations induces
genetic mutations in these hematopoietic cells that can cause tumor
formation (20,21).
The aging process impacts the immune system by
reducing the number of hematopoietic cells (22) and by increasing the risk of DNA
mutation during an active immune response that, furthermore, may
contribute to the development of hematopoietic cancer (23). Smog and pesticides as
Hexachlorobenzene that are normally present in the air can
affect the efficiency of the immune-response and increasing the
risk of DNA damage (24).
We speculate that in our patient ENP was due to an
aberrant B-cells response in an aging patient (72 years old)
exposed to pollution and pesticides for years. Recurrent
inflammation and the direct effect of the carcinoid on the DNA
integrity, other than their effect on the immunity answer (reduced)
allowed the growth of an ENP, by activating an aberrant immune
response after the polyp excision.
As support of ‘the inflammatory theory’ as cause of
ENP, we had the 1 year follow-up of our patient without disease
recurrence, despite he did not receive radio-chemotherapy as usual
in cases of ENP (24-26).
We speculate that the absence of tumor recurrence was due to the
absence of additional inflammatory process that could potentially
stimulate a new aberrant immune response.
This case report presents a limitation related to
the absence of Epstein-Barr test that was not performed during the
patient's screening.
Additional studies on large sample are necessary to
conclusively elucidate which factors contribute to development of
nasal plasmacytoma.
Plasmacytoma might present all aspects of a typical
benign lesion, both clinically and upon MRI, especially in the
early stages of the disease. The resection of a benign nasal lesion
in an elderly patient should be carefully monitored over time,
because of the inflammation induced by the surgery could initiate
the growth of a malignant lesion due to a pathological immune
response.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
ADS contributed to study design, analysis of data,
analysis of results, definition of conclusion and writing. VG
contributed to data collection, supported writing the manuscript.
SDC and AS collected and analyzed the data. MCC contributed to data
collection and the literature review. ADG collected the data and
contributed to the literature review. MM collected the data and
contributed criticism to the paper. GR analyzed the results,
critically revised the manuscript and supervised the study.
Ethics approval and consent to
participate
The present study was approved by the International
Revisional Board (IRB) of Silvestrini University Hospital and the
patient signed a written consent before being included in the
study.
Patient consent for publication
The patient authorized publication of his data in an
anonymized form.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Dores GM, Landgren O, McGlynn KA, Curtis
RE, Linet MS and Devesa SS: Plasmacytoma of bone, extramedullary
plasmacytoma, and multiple myeloma: Incidence and survival in the
United States, 1992-2004. Br J Haematol. 144:86–94. 2009.PubMed/NCBI View Article : Google Scholar
|
|
2
|
International Myeloma Working Group:
Criteria for the classification of monoclonal gammopathies,
multiple myeloma and related disorders: A report of the
international myeloma working group. Br J Haematol 121: 749-757,
2003.
|
|
3
|
Chang YL, Chen PY and Hung SH:
Extramedullary plasmacytoma of the nasopharynx: A case report and
review of the literature. Oncol Lett. 7:458–460. 2014.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Wu EL, Riley CA, Hsieh MC, Marino MJ, Wu
XC and McCoul ED: Chronic sinonasal tract inflammation as a
precursor to nasopharyngeal carcinoma and sinonasal malignancy in
the United States. Int Forum Allergy Rhinol. 7:786–793.
2017.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Moyano MD, Mella TA, Eduardo PO and Bermeo
SJ: Extramedullary plasmacytoma nasal septum: Case report and
literature review. Rev Otorrinolaringol Cir Cabeza Cuello.
76:301–307. 2016.
|
|
6
|
Susnerwala SS, Shanks JH, Banerjee SS,
Scarffe JH, Farrington WT and Slevin NJ: Extramedullary
plasmacytoma of the head and neck region: Clinicopathological
correlation in 25 cases. Br J Cancer. 75:921–927. 1997.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Corvo MA, Granato L, Ikeda F and de
Próspero JD: Extramedullary nasal plasmacytoma: Literature review
and a rare case report. Int Arch Otorhinolaryngol. 17:213–217.
2013.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Nettesheim P, Creasia DA and Mitchell TJ:
Carcinogenic and cocarcinogenic effects of inhaled synthetic smog
and ferric oxide particles. J Natl Cancer Inst. 55:159–169.
1975.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Sinha S and Gajra A: Cancer, Nasopharynx.
In: StatPearls (Internet). StatPearls Publishing, Treasure Island,
FL, 2019.
|
|
10
|
El-Naggar AK, Chan JKC, Grandis JR, Takata
T and Slootweg PJ (eds): WHO classification of head and neck
tumours. Vol 9. 4th edition. IARC Press, Lyon, 2017.
|
|
11
|
Bataskis JG: Pathology consultation.
Plasma cell tumors of the head and neck. Ann Otol Rhinol Laryngol.
92:311–313. 1983.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Ashraf MJ, Azarpira N, Khademi B, Abedi E,
Hakimzadeh A and Valibeigi B: Extramedullary plasmacytoma of the
nasal cavity report of three cases with review of the literature.
Iran Red Cresceny Med J. 15:363–366. 2013.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Fernandes AM, Podovani JA and Maniglia JP:
Extramedullary plasmocytoma of nasopharynx: A case report and
revision of literature. BJORL. 64:296–298. 1998.
|
|
14
|
Asai N, Ohkuni Y, Kawamura Y and Kaneko N:
A case of obstructive sleep apnea syndrome caused by malignant
melanoma in the nasal cavity and paranasal sinus. J Cancer Res
Ther. 9:276–277. 2013.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Stevens WW, Schleimer RP and Kern RC:
Chronic rhinosinusitis with nasal polyps. J Allergy Clin Immunol
Pract. 4:565–572. 2016.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Agarwal A: Neuroimaging of plasmacytoma. A
pictorial review. Neuroradiol J. 27:431–437. 2014.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Strojan P, Soba E, Lamovec J and Munda A:
Extramedullary plasmacytoma: Clinical and histopathologic study.
Int J Radiat Oncol Biol Phys. 1:692–701. 2002.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Yi B, Rykova M, Jäger G, Feuerecker M,
Hörl M, Matzel S, Ponomarev S, Vassilieva G, Nichiporuk I and
Choukèr A: Influences of large sets of environmental exposures on
immune responses in healthy adult men. Sci Rep.
5(13367)2015.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Hatton OL, Harris-Arnold A, Schaffert S,
Krams SM and Martinez OM: The interplay between epstein-Barr virus
and B lymphocytes: Implications for infection, immunity, and
disease. Immunol Res. 58:268–276. 2014.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Jeon JP, Kim JW, Park B, Nam HY, Shim SM,
Lee MH and Han BG: Identification of tumor necrosis factor
signaling-related proteins during epstein-barr virus-induced B cell
transformation. Acta Virol. 52:151–159. 2008.PubMed/NCBI
|
|
21
|
Hansen KD, Sabunciyan S, Langmead B, Nagy
N, Curley R, Klein G, Klein E, Salamon D and Feinberg AP:
Large-scale hypomethylated blocks associated with epstein-barr
virus-induced B-cell immortalization. Genome Res. 24:177–184.
2014.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Geiger H and Rudolph KL: Aging in the
lympho-hematopoietic stem cell compartment. Trends Immunol.
30:360–365. 2009.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Moehrle BM and Geiger H: Aging of
hematopoietic stem cells: DNA damage and mutations? Exp Hematol.
44:895–901. 2016.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Starek-Świechowicz B, Budziszewska B and
Starek A: Hexachlorobenzene as a persistent organic
pollutant: Toxicity and molecular mechanism of action. Pharmacol
Rep. 69:1232–1239. 2017.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Creach KM, Foote RL, Neben-Wittich MA and
Kyle RA: Radiotherapy for extramedullary plasmacytoma of the head
and neck. Int J Radiat Oncol Biol Phys. 73:789–794. 2009.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Attanasio G, Viccaro M, Barbaro M, De Seta
E and Filipo R: Extramedullary plasmacytoma of paranasal sinuses. A
combined therapeutic strategy. Acta Otorhinolaryngol Ital.
26:118–120. 2006.PubMed/NCBI
|