Introduction
Esophageal cancer is the sixth common cause of
cancer associated deaths worldwide (1). It is often difficult to notice
esophageal cancer using conventional esophagogastroduodenoscopy
(EGD) with white-light imaging (WLI). Many clinical studies have
reported on the diagnostic performance by image-enhanced endoscopy
with narrow-band imaging (NBI) (2,3).
Moreover, endoscopic surveillance of Barrett's esophagus has become
a foundation of the management of esophageal adenocarcinoma, and
this trend has accelerated with recent developments in advanced
endoscopic imaging and treatment technologies (4).
Endoscopic submucosal dissection is a lower invasive
therapy for superficial esophageal cancers. However, esophageal
treatment requires more skill than gastric resection because of the
technical difficulties related with the narrow location and thin
wall in esophagus usually. It is more difficult to distinguish
between ectopic gastric mucosa and early cancer, it rarely reported
that the case for patient to undergo magnifying endoscopy with NBI
and endoscopic submucosal dissection (ESD) for an esophageal
adenocarcinoma in the upper thoracic esophagus (5). Therefore, we have reported a first case
of squamous cell carcinoma coexisting with ectopic gastric mucosa
treated by endoscopic submucosal dissection. I confirmed that the
patient provided informed consent for the use of this data with a
consent form.
Case report
A 69-year-old Japanese man underwent an ESD for
early gastric cancer 2 years prior to his admission. A follow-up
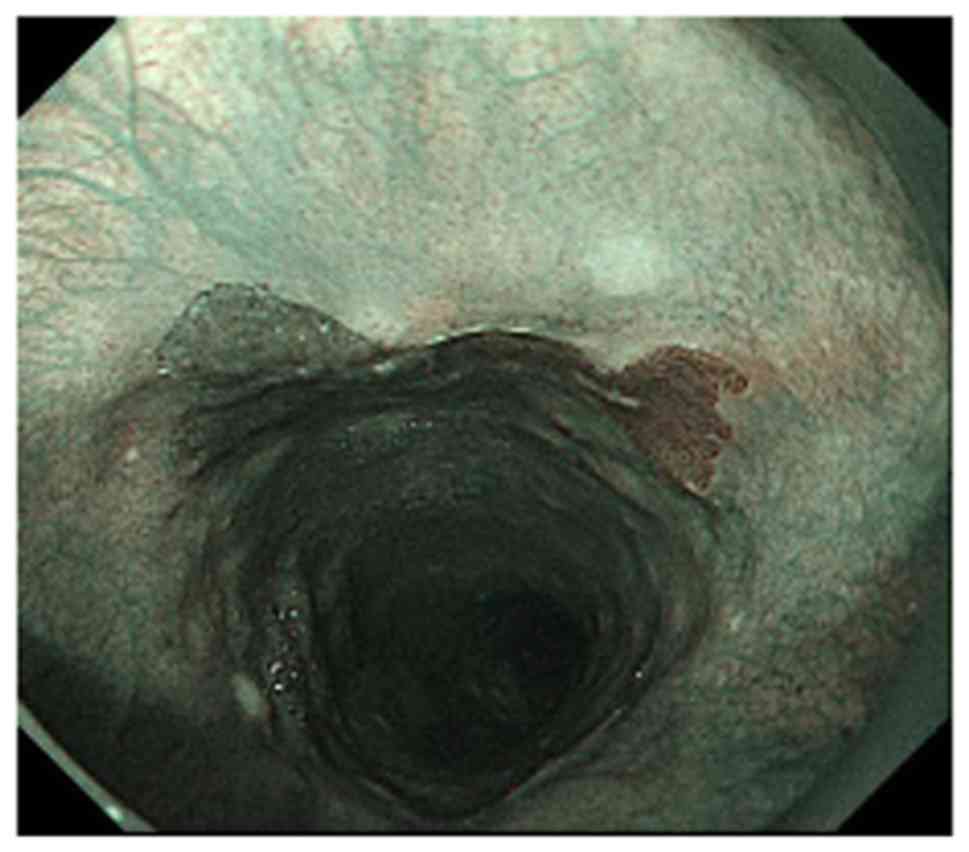
EGD with NBI system showed a butterfly-shaped brownish area
(Fig. 1) in the cervical esophagus.
The patient's history included hypertension and chronic kidney
disease, and his family history included a brother with gastric and
colonic cancer. The patient had smoked for 20 years beginning when
he was 20 years old.
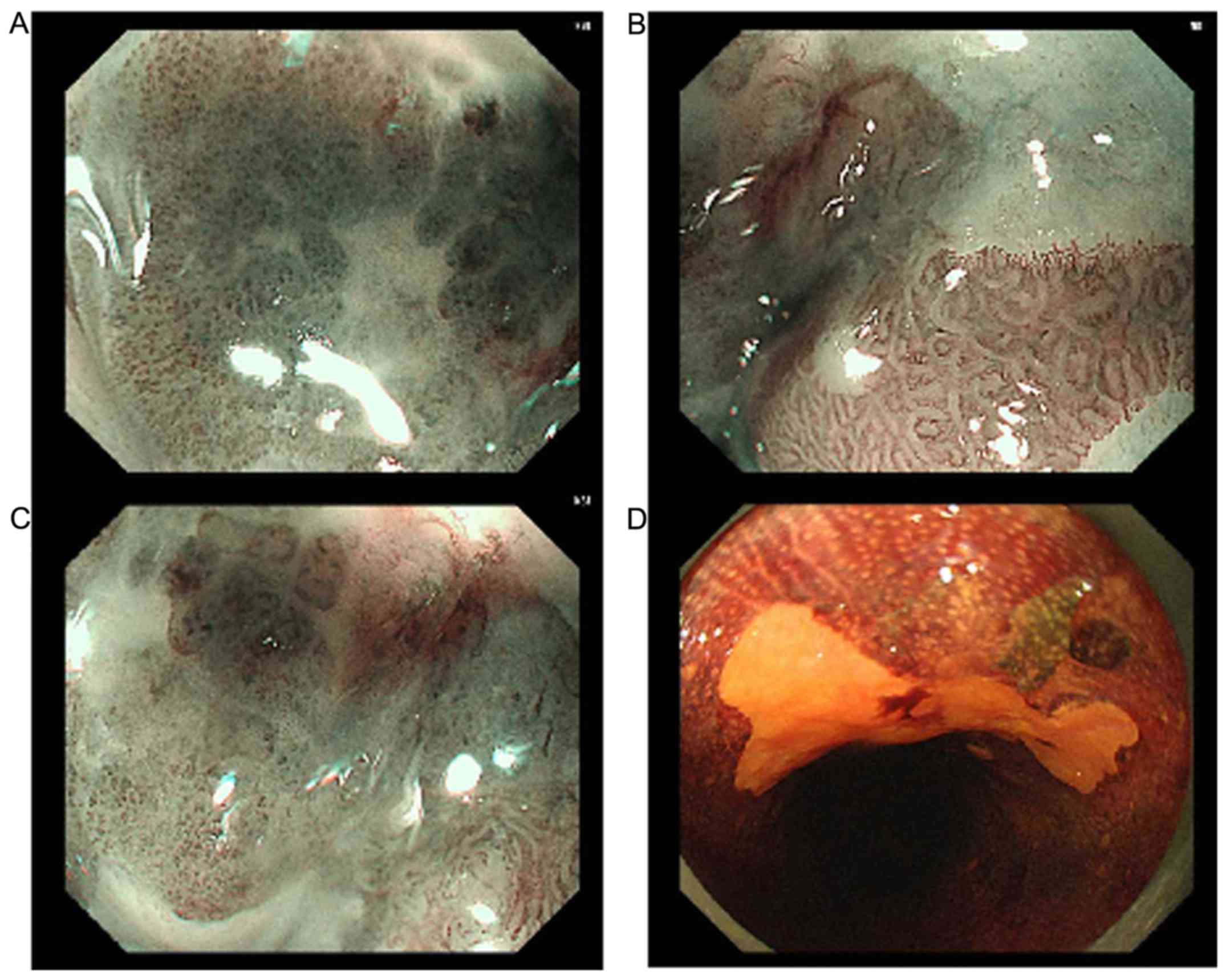
NBI magnifying endoscopy, revealed that the
patient's butterfly-shaped brownish area had type B2 vessels (per
the Japanese esophageal Society expansion endoscopic classification
(6) in 2/3 of its area (Fig. 2A and B). In addition, 1/3 of this area showed a
gastric mucosal pattern (Fig.
2C).
The endoscopic image of the same lesion after
spraying with Lugol's solution showed that the lesion remained
unstained (Fig. 2D). A squamous cell
carcinoma was diagnosed based on the biopsy from the lesion, which
revealed type B1-2 vessels.
Because of a localization in cervical esophagus, the
surgical operation method will be Pharyngolaryngoesophagectomy.
Considering that endoscopic treatment will be more beneficial for
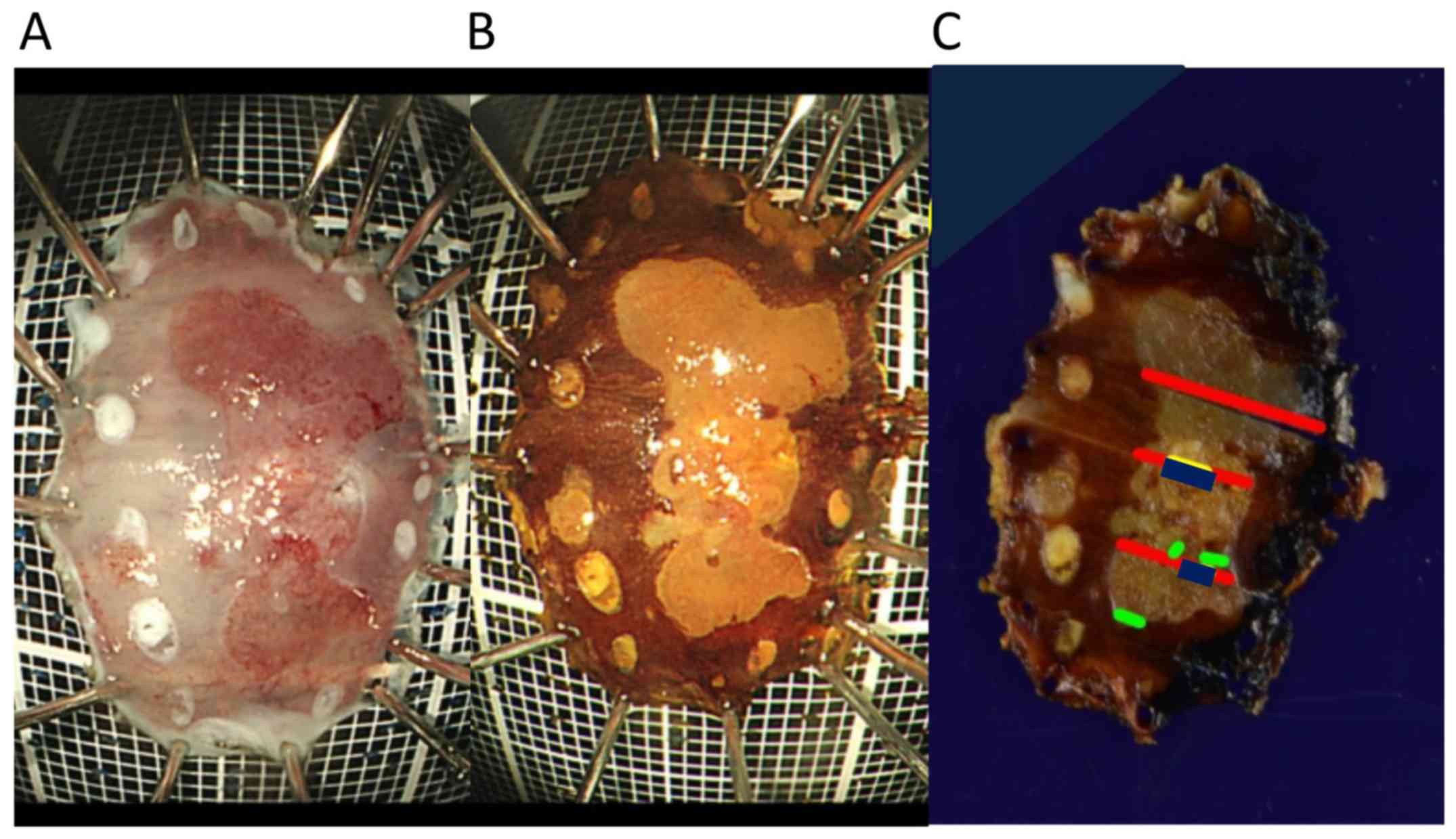
patient, we performed an endoscopic submucosal dissection (ESD) of
the esophageal lesion for the purpose of doing a total biopsy. We
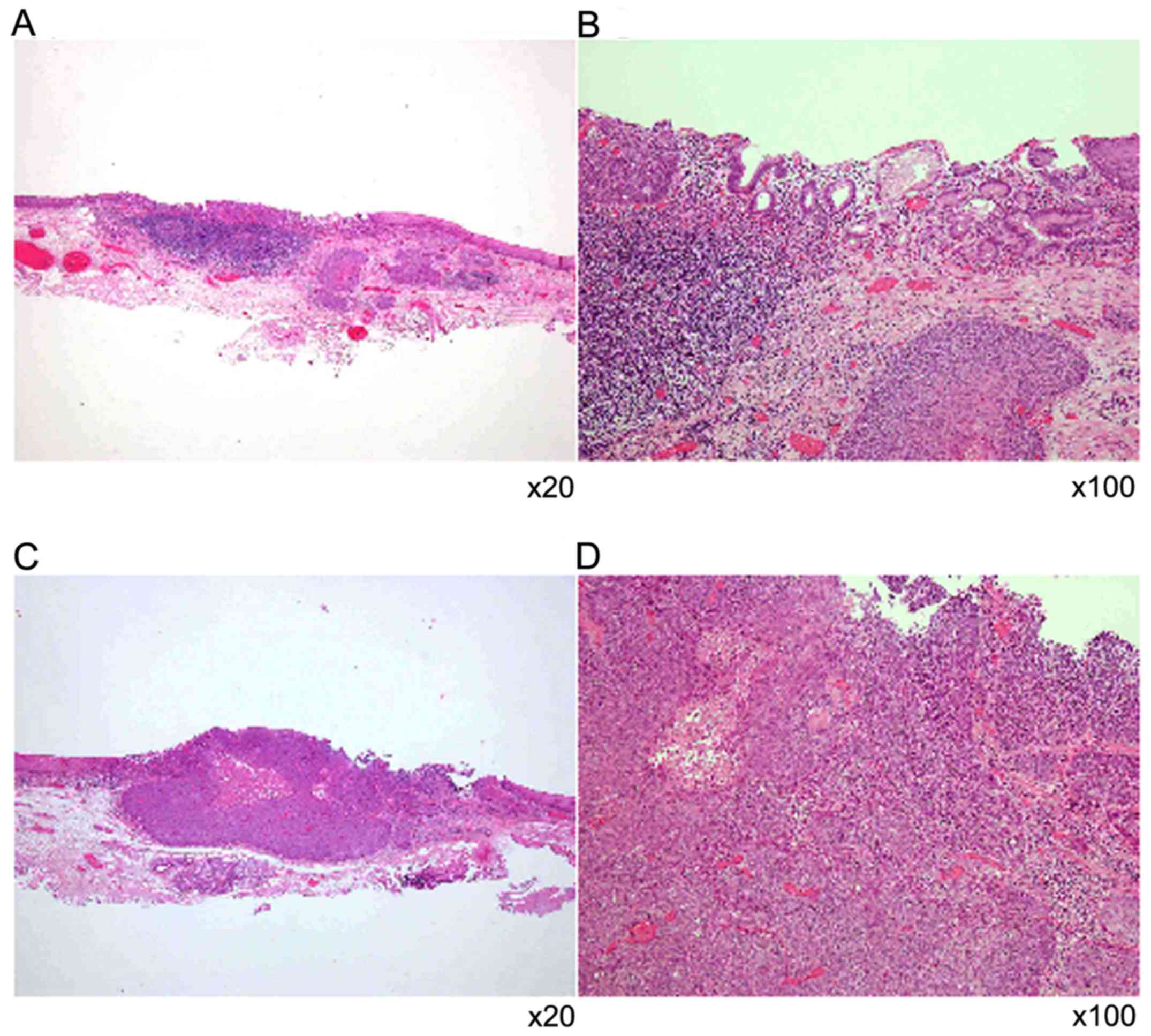
completed that endoscopic surgery as planned (Fig. 3A-C). The histopathological analysis
of the resected specimen revealed squamous cell carcinoma
(moderately differentiated) of the esophagus, Ce, 0- IIb, 14x8 mm,
pT1b(SM1), INFα, ly0(D2-40), v0(EVG), pHM0, pVM0 (Fig. 4A-D). The squamous cell carcinoma
invaded into the submucosal layer under the ectopic gastric
mucosa.
Discussion
We performed an endoscopic submucosal dissection of
the cervical esophageal lesion for a total biopsy as planned. The
reason why I determined that ESD would be more benefical is a
location of esophageal cancer. Because of a localization of
cervical esophagus, the operation will be
pharyngolaryngoesophagectomy. Needless to say, blood cancer
biomarker of squamous cell cancer was normal. Metastatic lesion was
not detected in all body CT scan.
The reported frequency of ectopic gastric mucosa of
the upper esophagus is 11% (7).
Approximately 30 case reports of adenocarcinoma occurring from
ectopic gastric mucosa of the esophagus have been reported since
1950(8), but our search of the
literature revealed no reported case of squamous cell carcinoma
neighboring and invading ectopic gastric mucosa. As another rare
case, there are a report to undergo ESD for esophageal
adenocarcinoma with enteroblastic differentiation arising from
ectopic gastric mucosa in the esophagus (9). In our case, the squamous cell carcinoma
invaded into the submucosal layer under the ectopic gastric mucosa.
From now, it is necessary for us to consider how to be invaded into
submucosal layer pathologically. We have thus apparently reported
the first case of a patient with squamous cell carcinoma coexisting
with ectopic gastric mucosa treated by endoscopic submucosal
dissection.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
TT and KI performed the ESD of the esophageal
lesion. KOm and NI aided the endoscopic surgery. KOk and YI, TasH
performed white-light and narrow band imaging magnifying endoscopy.
TaiH and TO performed an ESD for early gastric cancer. AN performed
histological examinations of esophageal cancer tissue. TK and KK
supervised treatment. KK wrote the manuscript. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
The present study was approved by the Fukuchiyama
City Hospital (Kyoto, Japan). Informed consent was obtained from
the patient.
Patient consent for publication
Informed consent was obtained for publication of
patient data.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Bray F, Ferlay J, Soerjomataram I, Siegel
RL, Torre LA and Jemal A: Global cancer statistics 2018: GLOBOCAN
estimates of incidence and mortality worldwide for 36 cancers in
185 countries: CA Cancer J. Clin. 68:394–424. 2018.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Gai W, Jin XF, Du R, Li L and Chai TH:
Efficacy of narrow-band imaging in detecting early esophageal
cancer and risk factors for its occurrence. Indian J Gastroenterol.
37:79–85. 2018.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Chiu PWY, Uedo N, Singh R, Gotoda T, Ng
EKW, Yao K, Ang TL, Ho SH, Kikuchi D, Yao F, et al: An Asian
consensus on standards of diagnostic upper endoscopy for neoplasia.
Gut. 68:186–197. 2019.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Ishihara R, Goda K and Oyama T: Endoscopic
diagnosis and treatment of esophageal adenocarcinoma: Introduction
of Japan Esophageal Society classification of Barrett's esophagus.
J Gastroenterol. 54:1–9. 2019.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Nonaka K, Watanabe M, Yuruki H, Okuda A,
Sakurai K, Iyama K and Sasaki Y: Narrow band imaging of
adenocarcinoma arising from ectopic gastric mucosa in the upper
esophagus. Endoscopy. 45 (Suppl 2) UCTN:E112–E113. 2013.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Oyama T, Inoue H, Arima M, Momma K, Omori
T, Ishihara R, Hirasawa D, Takeuchi M, Tomori A and Goda K:
Prediction of the invasion depth of superficial squamous cell
carcinoma based on microvessel morphology: Magnifying endoscopic
classification of the Japan Esophageal Society. Esophagus.
14:105–112. 2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Weickert U, Wolf A, Schröder C, Autschbach
F and Vollmer H: Frequency, histopathological findings, and clinical
significance of cervical heterotopic gastric mucosa (gastric inlet
patch): A prospective study in 300 patients. Dis Esophagus.
24:63–68. 2011.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Paulides E, de Boer NK and Grasman ME:
Proximal esophageal cancer missed during
esophagogastroduodenoscopy: Should the detection of an inlet patch
be added to the quality criteria for upper gastrointestinal
endoscopy? Endoscopy. 48 (Suppl 1)(E273)2016.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Gushima R, Narita R, Shono T, Naoe H, Yao
T and Sasaki Y: Esophageal adenocarcinoma with enteroblastic
differentiation arising in ectopic gastric mucosa in the cervical
esophagus: A case report and literature review. J Gastrointestin
Liver Dis. 26:193–197. 2017.PubMed/NCBI View Article : Google Scholar
|