Introduction
Soft tissue sarcomas (STS) are a rare group of
mesenchymal origin tumors which represent 1% of all malignancies in
adults (1). Angiosarcoma is an
uncommon subtype of sarcoma of vascular or lymphatic origin which
represents 2% of STS (2). Risk
factors include prior radiation therapy to the affected site,
chronic lymphedema, and exposures such as vinyl chloride and
arsenic (2). Patients are often
older, with a median age of 60 years (2), and a significant number (20-45%)
present with locally advanced or metastatic disease at diagnosis
(3). Angiosarcoma represents an
aggressive subtype of sarcoma, with 12% survival at 5 years for
unresectable or metastatic disease (3).
The rarity of angiosarcoma precludes large
randomized trials. Randomized trials generally group many subtypes
of STS to achieve sufficient power for the primary outcomes,
however heterogeneity within such trials limits the power for
meaningful subgroup analysis of various sarcoma histologies. Thus,
retrospective chart reviews have continued to provide the majority
of current evidence for treatment and outcomes of rare subtypes of
sarcoma (1,2).
Various factors may impact the survival of patients
with angiosarcoma, including type of therapy used. ANGIOTAX was a
single arm phase II trial (n=30) which introduced taxanes as first
line systemic therapy for unresectable or metastatic angiosarcoma,
with response rates of 18-19% at 6 months (3). This result has been confirmed in a
number of small retrospective studies (4-8).
Beyond taxanes, the majority of other published work includes
retrospective reviews of small numbers of patients which suggest
equipoise between taxanes and anthracyclines (5,7).
Furthermore, previous single institution retrospective reviews have
suggested that individuals with metastasis at presentation,
non-cutaneous primary disease, and unresectable disease have a
worse prognosis.
In terms of local therapy, complete oncologic
resection has been shown to improve overall survival (OS) (6,9). The
effect of radiation therapy is less clear (5-7).
Retrospective studies have focused on individual sites and
endpoints used in analysis have not been consistent (10-12).
In retrospective cohort studies, adjuvant radiation for breast
angiosarcoma, or for unselected patients with localized disease did
not impact recurrence free survival, but the impact on OS was not
explored (11-13).
For scalp primaries, radiation has been demonstrated to prolong
time to local recurrence, and improved OS on univariate analysis
(10).
Here we identify a large retrospective series of
patients treated within a single institution to understand real
world outcomes of patients with angiosarcoma and to establish
potential modifiable predictors of outcomes.
Patients and methods
Patients with angiosarcoma from January 1, 1969 to
September 19, 2017 were identified using the provincial Sarcoma
Outcomes Unit (SARCOU) Database from the institution British
Columbia (BC) Cancer in Canada. Central pathology review at the
provincial academic centre specializing in sarcoma occurred for all
cases at the time of diagnosis. Age at diagnosis, sex, histology,
grade, tumor size, tumor location, chemotherapy [type of
chemotherapy, no of lines, response as per Response Evaluation
Criteria in Solid Tumors (RECIST), duration of therapy],
radiotherapy (prior radiation, treatment dose), surgery (extent of
resection, R0, R1 or R2), date of death/last encounter was
collected for each patient by retrospective chart review. When
possible, charts were reviewed for specific radiation planning
information to determine if the angiosarcoma arose within a prior
radiation field.
Statistical analysis
Descriptive statistical analysis were used and
frequency of occurrence and percentage was calculated for each of
the independent variables. Progression-free survival (PFS) and OS
was calculated for each patient. PFS was measured from the time of
diagnosis until disease progression or death from any cause. OS was
measured from the time of diagnosis until death from any cause.
Kaplan-Meier curves were constructed for PFS and OS to compare
taxanes versus any other chemotherapy. Cox proportional hazard
models were used to calculate hazard ratios (HR) and 95% confidence
intervals (CIs) for OS and PFS. Patients were censored if an event
of interest did not occur prior to September 19, 2017 (the end of
follow-up). All analyses were performed using SAS software, version
9.4 (SAS Institute Inc.). Statistical significance was defined
using a two-tailed P-value of <0.05.
Results
Baseline characteristics
A total of 145 patients with angiosarcoma, 48.2% of
which were female, were identified from January 1, 1969 to
September 19, 2017 inclusive. Patient and treatment characteristics
are summarized in Table I. Median
age at diagnosis was 72 years. The majority of patients had
resectable disease at presentation (77 patients, 53.1%), the
remaining 68 patients had metastatic or unresectable disease.
Common sites of primary disease presentation were head and neck
(43/145), breast (35/145), and lower extremity (18/145). Rare sites
of presentation (1 case/location) included: Cervical spine, colon,
thyroid, adrenal gland and spleen.
 | Table IPatient and treatment
characteristics. |
Table I
Patient and treatment
characteristics.
| Variables | n=145, n (%) |
|---|
| Median age
(years) | 72 (19-96) |
| Sex |
|
Female | 70 (48.2) |
|
Male | 75 (51.7) |
| Site |
|
Cutaneous
(head and neck) | 43 (27.7) |
|
Extra
cutaneous | 102 (70.3) |
| Stage at
presentation |
|
Resectable | 77 (53.1) |
|
Unresectable | 42 (29.0) |
|
Metastatic | 26 (18.0) |
| Etiology |
|
Primary | 103 (71.0) |
|
Radiation
associated | 38 (26.2) |
|
Chronic
lymphedema | 4 (2.8) |
| Initial
treatment |
|
Surgery | 71 (48.9) |
|
Chemotherapy | 11 (7.6) |
|
Radiation | 38 (26.2) |
|
Best
supportive care | 18 (12.4) |
|
Othera | 7 (4.8) |
Prior radiation exposure
A total of 38 patients with angiosarcoma had
previous radiation, of which 36 had available data on prior
radiotherapy plans. Angiosarcoma arose within a prior curative
intent radiation therapy field in 28/36 patients: 23/28 adjuvant
breast cancer, 3/28 head and neck/skin cancer, 1/28 for prostate
cancer. The mean radiation dose prescribed was 48.5 Gy (range
42.5-70 Gy). The median time from curative radiation to development
of angiosarcoma was 8 years (range 2-22 years).
Outcomes based on cancer therapy
received
The median OS for best supportive care was 2.2
months. Median OS for localized, unresectable non-metastatic and
metastatic patients was 47, 5 and 3.0 months, respectively. The
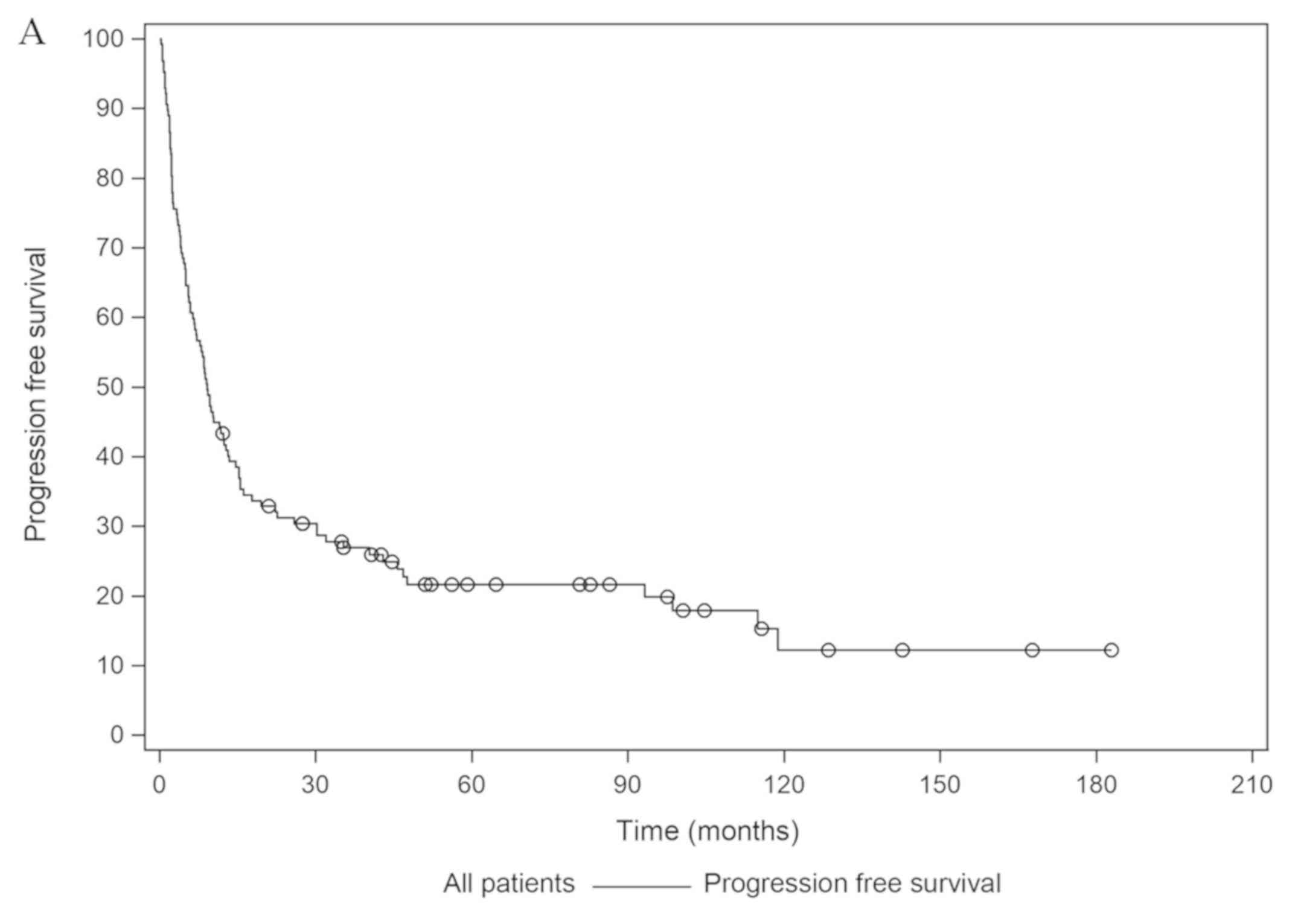
median PFS and OS of the entire cohort is illustrated in Fig. 1. In terms of any treatment received,
of the 145 patients in the cohort, 55.1% patients underwent
surgery, 48.2% received radiation, and 26.2% received chemotherapy
(Table I).
Radiation (n=70)
Radiation intent was curative in 19 patients
(6-neoadjuvant, 13-adjuvant). In addition, 60 patients received
palliative radiation. Median OS for patients whose first treatment
was radiation was 9 months.
Surgery (n=71)
A total of 71 of 77 resectable patients at diagnosis
underwent surgery. The majority of patients underwent an R0
resection (42/71). A total of 18/71 patients underwent an R1, 5/71
R2 and 6/71 were unknown. Median OS by extent of resection was
93.3, 16 and 3.4 months for R0, R1, R2 resections respectively.
Chemotherapy (N=38)
Median OS of patients treated with first line
chemotherapy was 13.2 months. Of the 38 patients who received
chemotherapy, the intent was palliative in the majority of patients
(32 patients, 84.2%). One patient received neoadjuvant chemotherapy
(2.6%), 3/38 patients received adjuvant chemotherapy, of which two
had concurrent radiation for scalp angiosarcoma (Table II). Most patients receiving
chemotherapy received only one line of treatment 21 patients
(≥55.3%), 14 patients (36.8%) patients received two lines and three
(7.9%) patients received three lines of therapy. More patients were
treated with doxorubicin or liposomal doxorubicin (27 patients,
71%) than taxanes (15 patients, 39.5%).
 | Table IIChemotherapy Information for 38
patients treated with systemic therapy. |
Table II
Chemotherapy Information for 38
patients treated with systemic therapy.
| Variables | n=38, n (%) |
|---|
| Chemotherapy
lines |
|
1 | 21 (14.5) |
|
2 | 14 (9.7) |
|
3 | 3 (2.1) |
| Regimen exposure (any
line) |
|
Taxane | 15 (39.5) |
|
Doxorubicin
or liposomal doxorubicin | 27 (71.0) |
|
Gemcitabine,
Sunitinib, Cisplatin/ | 1 each (2.6) |
|
Doxorubicin,
Dacarbazine, Vinorelbine, Pembrolizumab,
Doxorubicin/Ifosfamide | |
| Intent |
|
Neoadjuvent | 1 (2.6) |
|
Concurrent
with radiation | 2 (5.3) |
|
Adjuvant | 3 (7.9) |
|
Palliative | 32 (84.2) |
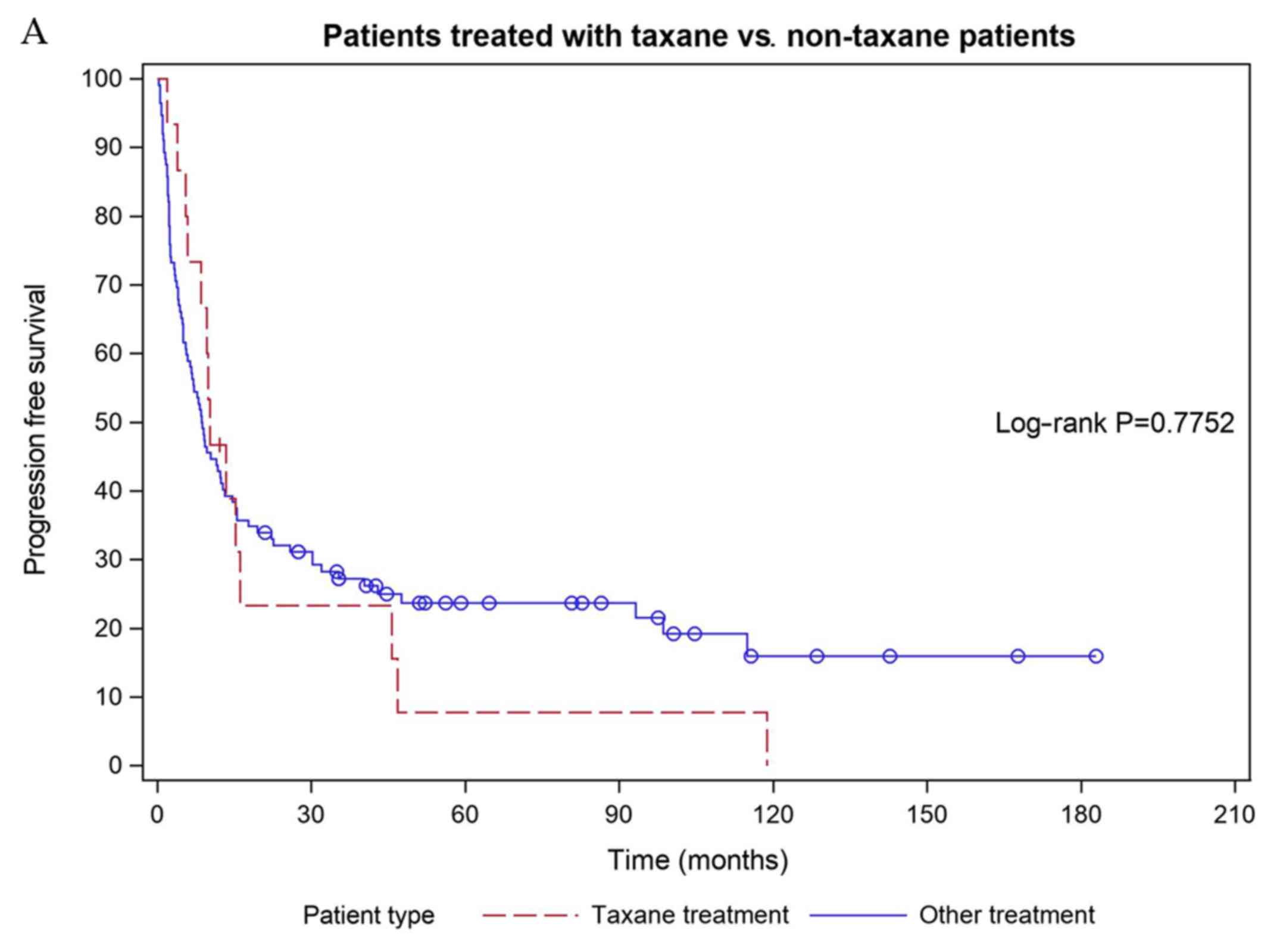
There was no difference in PFS and OS for patients
treated with a taxane versus non-taxane (Fig. 2), PFS for taxane treated patients
10.2, vs. 8.7 months for non-taxane treated patients (P=0.78). OS
for taxane treated patients was 28 months, compared to 13.2 months
for non-taxane treated patients (P=0.35). A total of 13 patients
who received an anthracycline in the first line went on to have
second line chemotherapy, while 3 patients who received a taxane
went onto second line treatment.
Predictors of OS
OS was significantly improved for female patients,
who had resectable disease (HR=0.22, P<0.01) and surgery with no
residual disease (R0 vs. R1, HR=0.26, P<0.01, R0 vs. R2 HR=0.07,
P<0.01). Patients who received any of chemotherapy, radiation or
surgery versus best supportive care had significantly improved OS
(chemotherapy HR=0.21, radiation HR=0.19, surgery HR 0.08,
P<0.01). Surgery (HR=0.10, P=0.02) significantly improved PFS,
but chemotherapy and radiation did not (chemotherapy HR 0.21,
P=0.13, radiation HR=0.19, P=0.12) (Table III).
 | Table IIIHRs for PFS and OS variable. |
Table III
HRs for PFS and OS variable.
| | HR for PFS | P-value | HR for OS | P-value |
|---|
| Sex (F vs. M) | 0.70 | <0.01a | 0.715 | <0.01a |
| Non cutaneous vs.
cutaneous | 0.71 | 0.07 | 0.76 | 0.16 |
| Tumor size (per
cm) | 1.05 |
<0.01a | 1.01 | 0.27 |
| Age at diagnosis
(per year) | 1.00 | 0.26 | 1.01 | 0.11 |
| Resectable
disease | 0.10 | 0.15 | 0.22 |
<0.01a |
| Extent of Surgery
(R0 vs. R1) | 0.30 |
<0.01a | 0.26 |
<0.01a |
| Extent of Surgery
(R0 vs. R2) | 0.14 |
<0.01a | 0.07 |
<0.01a |
| Extent of Surgery
(R1 vs. R2) | 0.47 | 0.14 | 0.29 | 0.03a |
| First treatment
surgery vs. chemotherapy | 0.23 |
<0.01a | 0.37 |
<0.01a |
| First treatment
surgery vs. radiation | 0.49 |
<0.01a | 0.416 |
<0.01a |
| First treatment
surgery vs. best supportive care | 0.10 | 0.02a | 0.08 |
<0.01a |
| First treatment
radiation vs. chemotherapy | 0.83 | 0.85 | 0.88 | 0.72 |
| First treatment
radiation vs. best supportive care | 0.19 | 0.12 | 0.19 |
<0.01a |
| First treatment
chemotherapy vs. best supportive care | 0.21 | 0.13 | 0.21 |
<0.01a |
OS and PFS was significantly improved if the first
treatment was surgery compared to radiation (PFS HR 0.49,
P<0.01, OS HR=0.41, P<0.01) or chemotherapy (PFS HR 0.23,
P<0.01, OS HR=0.37, P<0.01). There was no difference in PFS
or OS if chemotherapy or radiation was given first.
Discussion
Unresectable and metastatic angiosarcoma remains a
subtype of soft tissue sarcoma with poor prognosis. Data from our
provincial institution over 48 years demonstrated that adequate
upfront surgical resection remains the most significant predictor
of survival. For those with incurable disease, systemic therapy or
radiation therapy offer a meaningful improvement in survival
compared to best supportive care. No difference in survival was
identified with respect to which modality is used first (radiation
or chemotherapy) and type of systemic therapy used (taxane vs.
non-taxane).
The median age of our cohort, 72 years, was slightly
older than previously published studies (57.4-67 years) (3-8)
and similar to a recent large Dutch cohort (14). Incidence was similar between males
and females, although prior studies demonstrated slightly increased
incidence in females (55-65%) (3,6,7,14). The
most common site was cutaneous (head and neck) at 27.7% which is a
similar proportion to other large cohorts (5,9). The
majority were primary angiosarcomas, however, 28 patients (19.3%)
had angiosarcoma arise in a previous curative intent radiation
field. Our proportion of radiation associated angiosarcomas is
similar to previously reported incidence which ranges from 17-34%
(3-7,14),
and similar time to development as reported previously for a cohort
of radiation induced breast angiosarcomas (12,14).
Chronic lymphedema was an identified risk factor in 2.8% of
patients, which is less than reported rates of 4-13% (3,6,14).
Our study offers a large cohort of 145 patients
treated for angiosarcoma, comparable to other published series
(5,7,8,14). However, the OS for metastatic
patients in our cohort is lower than previously reported studies (3
vs. 7.3-16 months) (6,7,11,14).
This anomaly may be explained by the comparatively lower use of
chemotherapy in our cohort and the poor OS of patients who received
best supportive care alone. The OS for any chemotherapy was 13.2
months, comparable to the survival rates that have been reported in
other cohorts (3,14). The OS with best supportive care (BSC)
was also similar to previously published data (3,7) at 2.2
months. Interestingly, patients who were female had improved PFS
and OS, which is discordant with previous cohorts (14).
Local therapies such as surgery and radiation
continue to impact survival. Appropriate upfront resection remains
the most significant predictor of OS in our study and others
(6,9,14). The
OS benefit for complete resection is consistent across multiple
studies that highlight the importance of complete resection in soft
tissue sarcoma management (15-17).
This further highlights the importance of multi-disciplinary review
with experienced surgeons for even a borderline resectable
case.
Radiation therapy use in this cohort is higher than
previously published reports (19.8-41%) (6,14). In
our cohort, radiation use led to an improved PFS and OS for those
treated versus best supportive care in the non-curative setting.
Previous large single institution data of localized and metastatic
cohorts have seen reduction in local recurrence (11,13) or
only seen a trend towards OS benefit with radiation (47 vs. 10
months) (6). Our results are
congruent with a recently published large cohort which found
radiation treatment correlated with improved OS (14). Importantly, in our cohort, the impact
of radiation on OS met significance (9 vs. 2.2 months) for patients
whose first treatment for metastatic disease was radiation. This
difference may have been due to local control of the primary to
improve symptoms enabling systemic treatment to be delivered, or
simply good local control for a prolonged period delaying reduction
in performance status.
Our study identified lower rates of chemotherapy
usage (26%) in the incurable setting compared to most other
published cohorts. Apart from a large Dutch cohort reporting a 13%
chemotherapy usage rate (14),
previous retrospective cohorts demonstrate higher rates of
chemotherapy use, ranging from 40-89.8% (7,9,14,18).
Notably, previous published cohorts were either from a single
academic centre (9) or from a group
of Specialized Sarcoma Centres (7),
while in BC, patient care can be geographically disparate, and not
all patients were treated in an academic center with sarcoma
expertise. This coupled with slightly older baseline age of our
cohort may have led to less chemotherapy being prescribed.
Importantly, in our cohort, OS was significantly improved if any
chemotherapy was used versus best supportive care (13.2 vs. 2.2
months) consistent with reports that angiosarcoma is chemosensitive
(7). However, this overall
difference may be driven by the poor survival of patients treated
with best supportive care and must be interpreted carefully. The
specific reason for chemotherapy not being prescribed is unknown,
however could be related to baseline comorbidities or performance
status of patients in our cohort. Thus, ongoing advocacy and
education may be required to increase systemic therapy uptake and
its tolerability in patients.
Although not statistically significant, OS was
higher among patients treated with first line taxane versus first
line doxorubicin by 18 months. However, this difference must be
interpreted with caution given the small number of patients treated
with chemotherapy in this cohort. Additionally, more than half of
taxane treated patients (8/15) had cutaneous angiosarcoma, for
which higher response rates to paclitaxel have been reported
(5,19). The equipoise between taxanes and
anthracyclines seen in our cohort is reflected in previously
published retrospective series (5,7,9). Due to smaller than expected number of
patients treated with chemotherapy, we were unable to confidently
determine the impact of sequencing systemic therapy on outcome
(i.e. PFS2). Future studies of large cohorts of patients treated
with chemotherapy across multiple institutions could evaluate the
impact of first line treatment on subsequent chemotherapy
responsiveness (PFS2). Such studies would be helpful to determine
if there is an optimal first line treatment for angiosarcoma.
In total, using the strength of a large provincial
database over several decades, our study supports that
multi-disciplinary care is key to improved survival of patients
with angiosarcoma. In our cohort, surgery, chemotherapy, and
importantly, radiation therapy all improve OS. This data
encompasses multiple treating centers (academic and community)
within a province providing universal health care and access to
evidence-based therapies.
This study has limitations. As a retrospective
cohort over several decades, pathological expertise and diagnosis
of angiosarcoma improved over time, as such there is potential for
under-reporting of angiosarcoma from earlier decades. Fortunately,
BC conducts a central pathology review and all of our cases were
reviewed at the time of diagnosis. The presence of a central
pathology review report on the electronic medical record confirms a
sarcoma expert reviewed each case. Additionally, usage of
chemotherapy and radiation therapy was first noted in 1992 for our
cohort, thus our results remain valid for the impact of systemic
and radiotherapy. As a passive cancer registry, the registry may
not identify all cancer cases, as non-registry personnel may not be
familiar with all reporting criteria. Lastly, we were unable to
capture all individuals treated with agents funded by mechanisms
other than BC Cancer, such as private drug insurance and self-pay
options. A manual chart review of all cases was undertaken to
identify systemic therapy accessed through non-public mechanisms to
address this limitation. Finally, given the limited sample size and
the number of variables of interest, a multivariate analysis was
not performed as it was unlikely that we would be able to control
for confounding factors without over fitting the model. Despite
these limitations, the impact on our final results are minimal and
we anticipate no changes in our outcomes.
In conclusion, this study identified that upfront
surgical resection remains the most important predictor of OS in
patients affected by angiosarcoma. Unlike other published cohorts,
both radiotherapy and chemotherapy statistically improved OS
compared to best supportive care. There was equipoise between
outcomes of patients treated taxanes versus non taxane chemotherapy
within our cohort. Though challenging, more research is needed with
large cohorts of patients to better understand the sequencing of
taxanes and anthracyclines in this population.
Acknowledgements
Not applicable.
Funding
The present study was supported by institutional
funds provided by the BC Cancer, for maintenance of the Sarcoma
Outcomes Unit.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
ASm, and ASr conceived the present study. ASm
collected the data. AK collected the data and reviewed cases of
radiation-induced angiosarcoma to determine if they arose with a
previously irradiated field. ASm, ASr and JH designed the
statistical analysis. ASm, ASr wrote the manuscript. JH performed
statistical analysis. ASm, AK, CS, ASr interpreted the data and
revised the manuscript for intellectual content. All authors read
and approved the manuscript.
Ethics approval and consent to
participate
The British Columbia Cancer Agency Ethics Board and
Privacy Office approved the present study prior to commencement
(University of British Columbia, BC Cancer Research Ethics Board;
approval no. H17-02826). Consent was not obtained from individual
patients; however, all patient information was anonymized and
de-identified by the investigators for analysis.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Linch M, Miah AB, Thway K, Judson IR and
Benson C: Systemic treatment of soft-tissue sarcoma-gold standard
and novel therapies. Nat Rev Clin Oncol. 11:187–202.
2014.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Young RJ, Brown NJ, Reed MW, Hughes D and
Woll PJ: Angiosarcoma. Lancet Oncol. 11:983–991. 2010.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Penel N, Bui BN, Bay J-O, Cupissol D,
Ray-Coquard I, Piperno-Neumann S, Kerbrat P, Fournier C, Taieb S,
Jimenez M, et al: Phase II trial of weekly paclitaxel for
unresectable angiosarcoma: The ANGIOTAX Study. J Clin Oncol.
26:5269–5274. 2008.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Schlemmer M, Reichardt P, Verweij J,
Hartmann J, Judson I, Thyss A, Hogendoorn PC, Marreaud S, Van
Glabbeke M and Blay JY: Paclitaxel in patients with advanced
angiosarcomas of soft tissue: A retrospective study of the EORTC
soft tissue and bone sarcoma group. Eur J Cancer. 44:2433–2436.
2008.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Italiano A, Cioffi A, Penel N, Levra MG,
Delcambre C, Kalbacher E, Chevreau C, Bertucci F, Isambert N, Blay
JY, et al: Comparison of doxorubicin and weekly paclitaxel efficacy
in metastatic angiosarcomas. Cancer. 118:3330–3336. 2012.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Buehler D, Rice SR, Moody JS, Rush P,
Hafez GR, Attia S, Longley BJ and Kozak KR: Angiosarcoma outcomes
and prognostic factors: A 25-year single institution experience. Am
J Clin Oncol. 37(473)2014.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Penel N, Italiano A, Ray-Coquard I,
Chaigneau L, Delcambre C, Robin YM, Bui B, Bertucci F, Isambert N,
Cupissol D, et al: Metastatic angiosarcomas: Doxorubicin-based
regimens, weekly paclitaxel and metastasectomy significantly
improve the outcome. Ann Oncol. 23:517–523. 2011.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Fury MG, Antonescu CR, Van Zee KJ, Brennan
ME and Maki RG: A 14-year retrospective review of angiosarcoma:
Clinical characteristics, prognostic factors, and treatment
outcomes with surgery and chemotherapy. Cancer J. 11:241–247.
2005.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Skubitz KM and Haddad PA: Paclitaxel and
pegylated-liposomal doxorubicin are both active in angiosarcoma.
Cancer. 104:361–366. 2005.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Pawlik TM, Paulino AF, Mcginn CJ, Baker
LH, Cohen DS, Morris JS, Rees R and Sondak VK: Cutaneous
angiosarcoma of the scalp: A multidisciplinary approach. Cancer.
98:1716–1726. 2003.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Abraham JA, Hornicek FJ, Kaufman AM,
Harmon DC, Springfield DS, Raskin KA, Mankin HJ, Kirsch DG,
Rosenberg AE, Nielsen GP, et al: Treatment and outcome of 82
patients with angiosarcoma. Ann Surg Oncol. 14:1953–1967.
2007.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Sher T, Hennessy BT, Valero V, Broglio K,
Woodward WA, Trent J, Hunt KK, Hortobagyi GN and Gonzalez-Angulo
AM: Primary angiosarcomas of the breast. Cancer. 110:173–178.
2007.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Mark RJ, Poen JC, Tran LM, Fu YS and
Juillard GF: Angiosarcoma: A report of 67 patients and a review of
the literature. Cancer. 77:2400–2406. 1996.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Weidema ME, Flucke UE, van der Graaf WTA,
Ho VKY and Hillebrandt-Roeffen MHS: Dutch Nationwide Network and
Registry of Histo- and Cytopathology (PALGA)-Group,
Versleijen-Jonkers YMH, Husson O and Desar IME. Prognostic factors
in a large nationwide cohort of histologically confirmed primary
and secondary angiosarcomas. Cancers (Basel).
11(E1780)2019.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Bonvalot S, Rivoire M, Castaing M,
Stoeckle E, Le Cesne A, Blay JY and Laplanche A: Primary
retroperitoneal sarcomas: A multivariate analysis of surgical
factors associated with local control. J Clin Oncol. 27:31–37.
2009.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Le Cesne A, Ouali M, Leahy MG, Santoro A,
Hoekstra H, Hohenberger P, Van Coevorden F, Rutkowski P, Van Hoesel
R, Verweij J, et al: Doxorubicin-based adjuvant chemotherapy in
soft tissue sarcoma: Pooled analysis of two STBSG-EORTC phase III
clinical trials. Ann Oncol. 25:2425–2432. 2014.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Gronchi A, Vullo SL, Colombo C, Collini P,
Stacchiotti S, Mariani L, Fiore M and Casali PG: Extremity soft
tissue sarcoma in a series of patients treated at a single
institution: Local control directly impacts survival. Ann Surg.
251:506–511. 2010.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Young R, Natukunda A, Litière S, Woll P,
Wardelmann E and Van Der Graaf W: First-line anthracycline-based
chemotherapy for angiosarcoma and other soft tissue sarcoma
subtypes: Pooled analysis of eleven European Organisation for
Research and Treatment of Cancer Soft Tissue and Bone Sarcoma Group
trials. Eur J Cancer. 50:3178–3186. 2014.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Fata F, O'Reilly E, Ilson D, Pfister D,
Leffel D, Kelsen DP, Schwartz GK and Casper ES: Paclitaxel in the
treatment of patients with angiosarcoma of the scalp or face.
Cancer. 86:2034–2037. 1999.PubMed/NCBI
|