Introduction
Lung cancer is the most common cause of cancer death
worldwide (1). Localized stage of
lung cancer represents approximately 15% of lung cancer (2). Estimated new case of non-small cell
lung cancer (NSCLC) in the United states is approximately 22,800,
with an estimated 13,500 death each year by NSCLC (2). After resection for early-stage NSCLC,
20% of patients developed recurrences (3). NSCLC patients with postoperative
recurrence had poor prognosis. Survivals after recurrence were 13%
at 5 years in patients who underwent resection for NSCLC (4). The most common sites of lung cancer
metastases are the brain, bone, liver, and adrenal glands (5). Previous study showed that the first
recurrent site was distant in 78% of patients and patients with
distant recurrence had a shorter postrecurrent survival than those
with local recurrence (6). There
are only few reports that have demonstrated breast metastases of
primary lung neuroendocrine tumors (7-10).
Here, we report a case of a female patient who developed
metachronous bilateral breast metastases of a lung neuroendocrine
tumor.
Case report
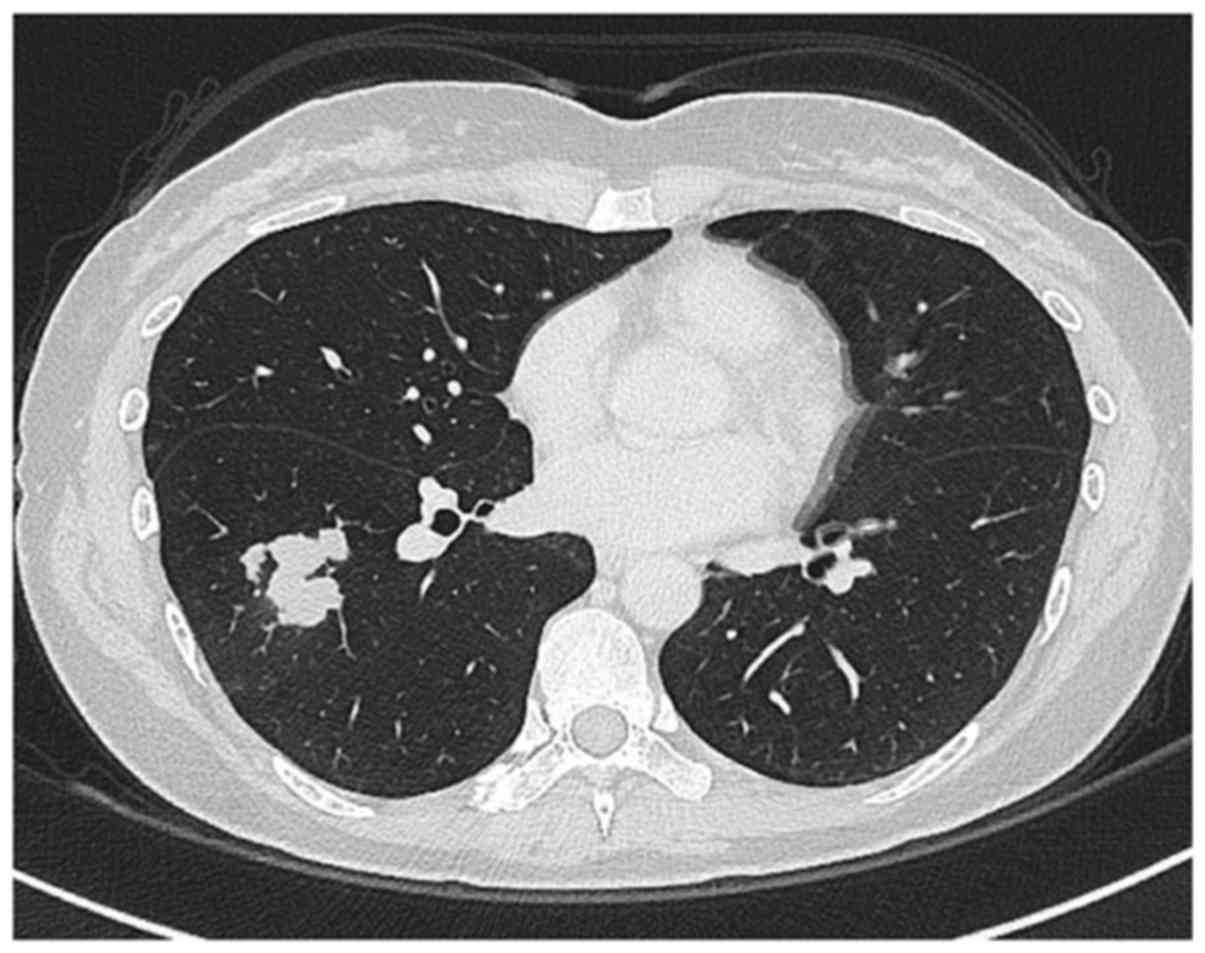
A 41-year-old woman with no history of smoking
underwent surgery for a breast fibroadenoma. An abnormal shadow was
observed on a chest X-ray, and subsequent chest computed tomography
(CT) revealed nodules on the right lung (Fig. 1). 18F-Fluorodeoxyglucose
(FDG) positron emission tomography (PET)/CT revealed increased
tracer uptake that was highly suggestive of lung cancer, with no
evidence of metastasis. The patient underwent right lower and
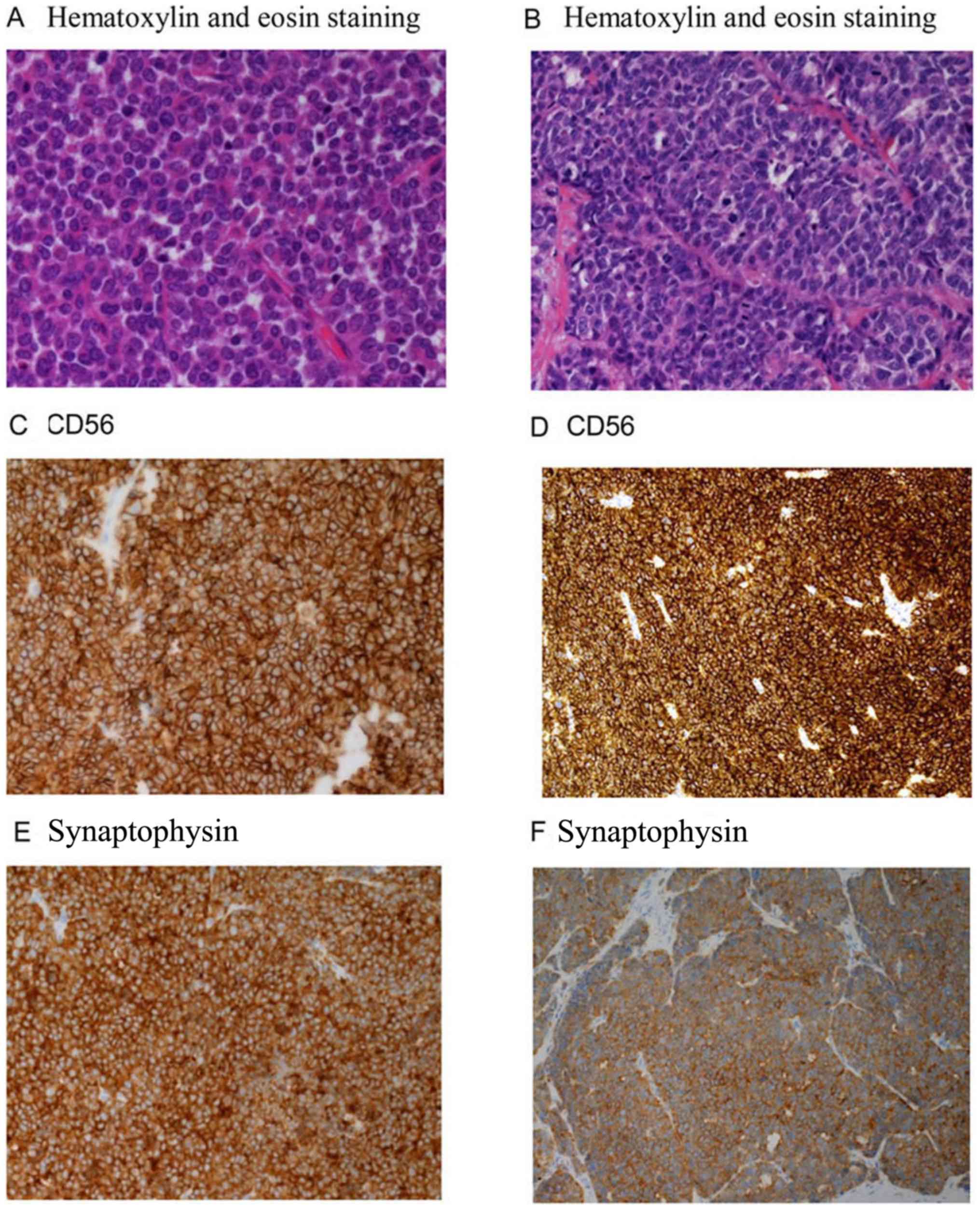
middle lobectomy, and immunohistochemistry revealed that the tumor
cells were positive for transcription termination factor-1 (TTF-1),
CD56, chromogranin A, and synaptophysin (Fig. 2). Additionally, 25.7% of the tumor
cells expressed the proliferation marker Ki67. A pathological
analysis led to a diagnosis of neuroendocrine tumor.
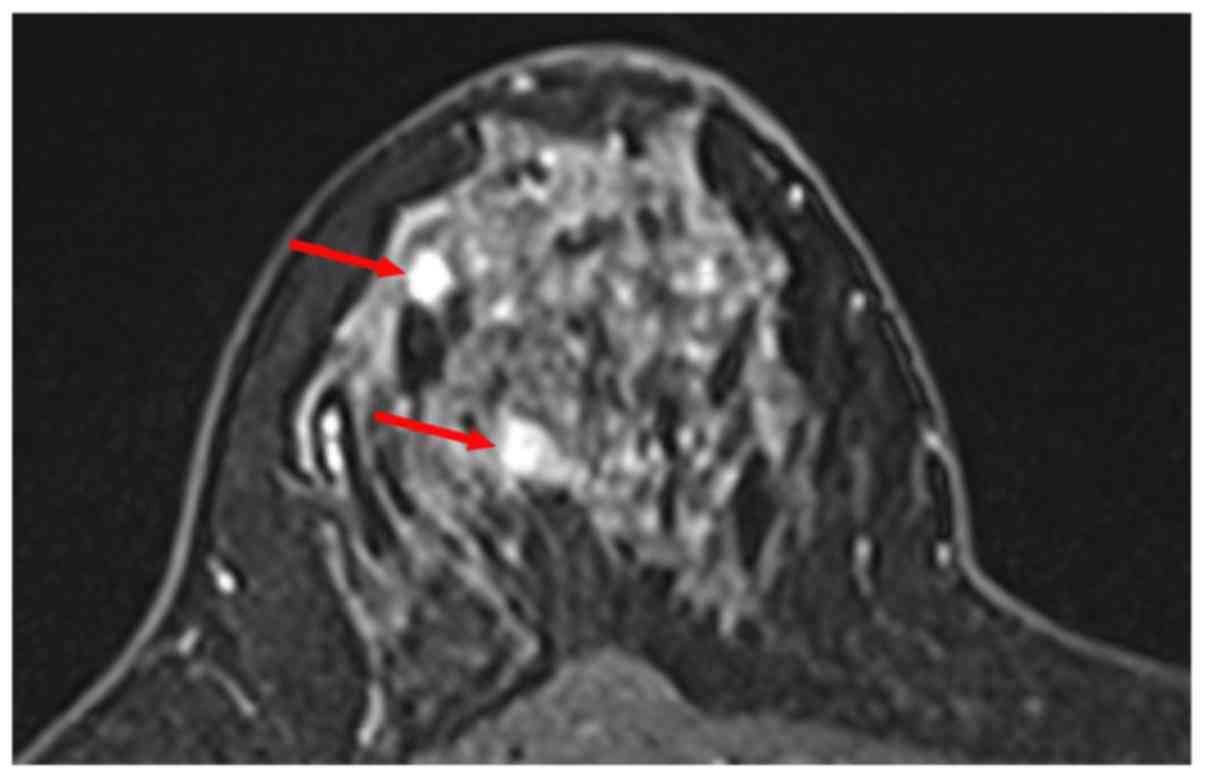
A regular medical follow-up of the surgical outcomes
for breast fibroadenoma revealed nodules in the right breast 3
months after adjuvant chemotherapy (Fig. 3), which were subsequently biopsied.
Histological analyses of hematoxylin and eosin (H&E)-stained,
paraffin-embedded biopsy sections indicated carcinoma, and positive
immunohistochemical staining for CD56, chromogranin A, and
synaptophysin confirmed a neuroendocrine origin (Fig. 2). Accordingly, a diagnosis of breast
metastasis of primary lung neuroendocrine tumor was made based on
cytological and immunohistochemical similarities between the
primary and metastatic lesions. The patient underwent mastectomy of
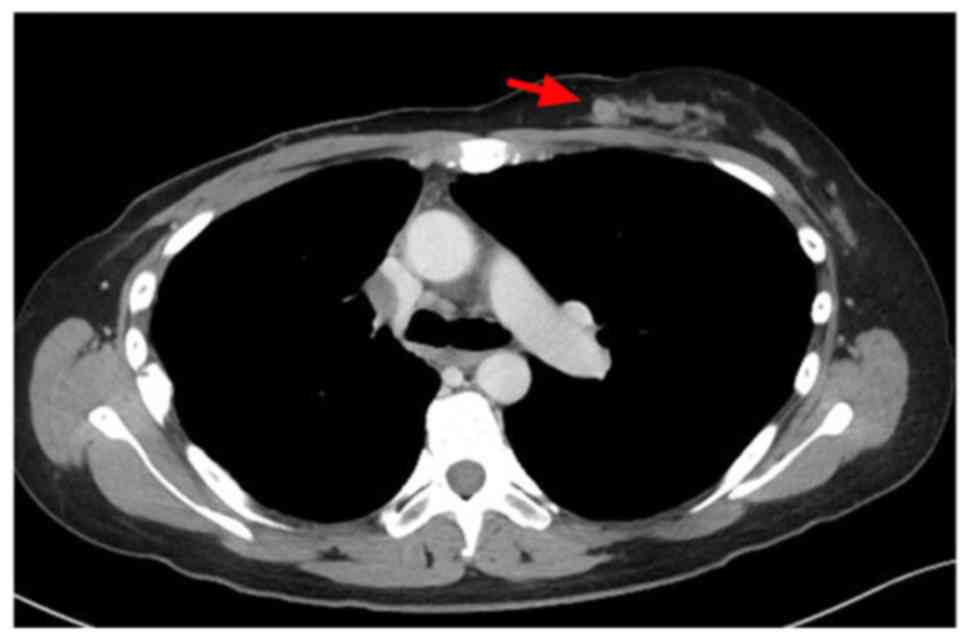
the right breast after 18F-FDG-PET/CT revealed no areas
of increased tracer uptake. Subsequently, she developed metastases
in the left breast, lung, lymph node, and peritoneum at 2 months
post-mastectomy (Fig. 4). Systemic
chemotherapy and local radiotherapy to the left breast were
administered. The patient remained alive 6 months later, with no
evidence of a bilateral breast recurrence.
Discussion
Breast metastasis of lung cancer is rarely reported.
Particularly, a few reports have described breast metastasis from
lung neuroendocrine tumors, which account for approximately 3% of
lung cancers in surgical series (7-11).
Overall, breast metastases of all extramammary malignancies are
very rare, accounting for 0.4-1.3% of all mammary malignancies
(12,13). These generally arise from primary
hematological malignancies, melanoma, rhabdomyosarcoma, lung
tumors, renal cell carcinoma, thyroid and cervical carcinomas,
intestinal carcinoid, epidermoid carcinoma of the head and neck,
and leiomyosarcoma (12,13).
Previous reports have demonstrated the benefits of
local therapy for a subset of patients with stage IV non-small cell
lung cancer and a small number of metastases (14,15).
Vaughan et al described three cases of breast metastases of
neuroendocrine tumors of the lung, of which two were treated with
surgery. One patient developed a breast metastasis 38 months after
her original diagnosis, for which she underwent a lumpectomy and
remained free of a breast recurrence 7 months later. The second
patient presented with a breast metastasis 8 months after her
original diagnosis and underwent an excisional biopsy. She
subsequently developed another breast metastasis 4 months after the
first excision and underwent radiation treatment (10). The patient in our case achieved good
local control with a right mastectomy, but subsequently developed
metastases in the left breast. However, she maintained good local
control of the left-sided breast nodules after radiation
therapy.
A search of the PubMed database between 2007 and
2017 identified 13 cases of breast metastases from neuroendocrine
tumors of the lung (Table I).
Despite the rarity of this condition, the possibility of metastasis
to the breast from a lung neuroendocrine tumor should be considered
in the differential diagnosis of a primary mammary carcinoma in
patients postoperatively discovered to have a breast lesion. One of
13 patients had bilateral breast metastases during the initial
diagnostic evaluation (Table I).
This finding and our observation of metachronous bilateral breast
metastases in the present case leads us to suggest that the
contralateral breast should be considered in an investigation of
metastasis.
 | Table ICharacteristics of previously reported
cases of breast metastases from lung neuroendocrine tumors. |
Table I
Characteristics of previously reported
cases of breast metastases from lung neuroendocrine tumors.
| Patient no. | Age, years/sex | Interval, from NET
diagnosis to breast tumor (months) | Vital status | Secondary survival
(months)a | Breast
laterality | Breast
surgery/radiotherapy | Chemotherapy |
|---|
| 1(9) | 44/F | 0 | NR | NR | NR | Mastectomy | NR |
| 2(9) | 60/F | 22 | NR | NR | NR | Lumpectomy | NR |
| 3(9) | 44/F | 37 | NR | NR | NR | Lumpectomy | NR |
| 4(9) | 28/F | 87 | NR | NR | NR | Lumpectomy | NR |
| 5(9) | 42/F | 69 | NR | NR | NR | Lumpectomy | NR |
| 6(9) | 62/F | 20 | NR | NR | NR | Lumpectomy | NR |
| 7(9) | 45/F | 36 | NR | NR | NR | Not performed | NR |
| 8(9) | 72/F | 20 | NR | NR | NR | Not performed | NR |
| 9(10) | 30/F | 38 | Alive | 7 | Left | Lumpectomy | NR |
| 10(10) | 35/F | 0 | Alive | 9 | Bilateral | Not performed | NR |
| 11(10) | 28/F | 8 | Dead | 17 | Right | Lumpectomy,
radiotherapy | NR |
| 12(8) | 49/F | 6 | Dead | 7 | Left | Radiotherapy | Not performed |
| 13(7) | 59/F | 0 | Dead | NR | Right | Not performed | Cisplatin +
etoposide, topotecan |
| The current case | 41/F | 12 | Alive | 18 | Bilateral | Mastectomy,
radiotherapy | Performed |
In summary, we report herein a rare case of a
patient with metachronous bilateral breast metastases of a primary
lung neuroendocrine tumor. The present case suggests that local
therapy provides good control of these metastatic lesions.
Acknowledgements
The authors would like to thank Dr Takeshi Kawakami
and Dr Hiroyuki Horikoshi (Division of Diagnostic Radiology of
Gunma Prefectural Cancer Center) for helping with figure
preparation. The authors would also like to thank Dr Sakae Fujimoto
(Division of Respiratory Medicine of Gunma Prefectural Cancer
Center) for his assistance in preparing this manuscript.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during the present
study are included in this published article.
Authors' contributions
MK, HI and KM designed the current study. MK, HI,
RO, AF, TF, YY, YN, MI and KM acquired and analyzed the data. YN
and MI performed histological examinations of the tumor specimens.
MK and HI drafted the manuscript and constructed the figures. TH
advised the study and analyzed the data. All the authors read and
approved the final version of the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the
patient for publication.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Ferlay J, Soerjomataran I, Dikshit R, Eser
S, Mathers C, Rebelo M, Parkin DM, Forman D and Bray F: Cancer
incidence and mortality worldwide, sources, methods and major
patterns in GLOBOCAN 2012. Int J Cancer. 136:E359–E386.
2015.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2020. CA Cancer J Clin. 70:7–30. 2020.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Lou F, Huang J, Sima CS, Dycoco J, Rusch V
and Bach PB: Patterns of recurrence and second primary lung cancer
in early-stage lung cancer survivors followed with routine computed
tomography surveillance. J Thorac Cardiovasc Surg. 145:75–81.
2013.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Sekihara K, Hishida T, Yoshida J, Oki T,
Omori T, Katsumata S, Ueda T, Miyoshi T, Goto M, Nakasone S,
Ichikawa T, et al: Long-term survival outcome after postoperative
recurrence of non-small-cell lung cancer: who is ‘cured’ from
postoperative recurrence? Eur J Cardiothorac Surg. 52:522–528.
2017.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Quint LE, Tummala S, Brisson LJ, Francis
IR, Krupnick AS, Kazerooni EA, Iannettoni MD, Whyte RI and Orringer
MB: Distribution of distant metastasis from newly diagnosed
non-small cell lung cancer. Ann Thorac Surg. 62:246–250.
1996.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Ichinose Y, Yano T, Yokoyama H, Inoue T,
Asoh H, Tayama K and Takanashi N: Postrecurrent survival of
patients with non-small-cell lung cancer undergoing a complete
resection. J Thorac Cardiovasc Surg. 108:158–61. 1994.PubMed/NCBI
|
|
7
|
Papa A, Rossi L, Verrico M, Di Cristofano
C, Moretti V, Strudel M, Zoratto F, Minozzi M and Tomao S: Breast
metastasis and lung large-cell neuroendocrine carcinoma: First
clinical observation. Clin Respir J. 11:574–578. 2017.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Rimner A and Rosenzweig KE: Palliative
radiation for lung cancer metastasis to the breast: Two case
reports. J Thorac Oncol. 2:1133–1135. 2007.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Crona J, Granberg D, Norlén O, Wärnberg F,
Stålberg P, Hellman P and Björklund P: Metastases from
neuroendocrine tumors to the breast are more common than previously
thought A diagnostic pitfall? World J Surg. 37:1701–1706.
2013.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Vaughan A, Dietz JR, Moley JF, Debenedetti
MK, Aft RL, Gillanders WE, Eberlein TJ, Ritter J and Margenthaler
JA: Metastatic disease to the breast: The Washington university
experience. World J Surg Oncol. 5(74)2007.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Travis WD: Pathology and diagnosis of
neuroendocrine tumors: Lung neuroendocrine. Thorac Surg Clin.
24:257–266. 2014.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Vizcaíno I, Torregrosa A, Higueras V,
Morote V, Cremades A, Torres V, Olmos S and Molins C: Metastasis to
the breast from extramammary malignancies: A report of four cases
and a review of literature. Eur Radiol. 11:1659–1665.
2001.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Toombs BD and Kalisher L: Metastatic
disease to the breast: Clinical, pathologic, and radiographic
features. AJR Am J Roentgenol. 129:673–676. 1977.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Gomez DR, Blumenschein GR Jr, Lee JJ,
Hernandez M, Ye R, Camidge DR, Doebele RC, Skoulidis F, Gaspar LE,
Gibbons DL, et al: Local consolidative therapy versus maintenance
therapy or observation for patients with oligometastatic
non-small-cell lung cancer without progression after first-line
systemic therapy: A multicentre, randomised, controlled, phase 2
study. Lancet Oncol. 17:1672–1682. 2016.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Matsuguma H, Nakahara R, Wakamatsu I,
Kishikawa T, Sugiyama T, Nakamura Y, Kasai T, Kamiyama Y, Hoshi N,
Inoue K, et al: Definitive local therapy for oligo-recurrence in
patients with completely resected non-small cell lung cancer. Am J
Clin Oncol. 43:210–217. 2020.PubMed/NCBI View Article : Google Scholar
|