Introduction
Fine-needle aspiration (FNA) cytology is a
well-established, safe and useful diagnostic procedure for salivary
gland lesions. Cytological features of pleomorphic adenoma (PA) are
well recognized, and its diagnosis using FNA specimens is usually
straightforward (1). However, some
diagnostic pitfalls and difficulties have been reported for PA,
such as prominent squamous metaplasia, predominant cellular
component without chondromyxoid stroma, and the presence of nuclear
atypia (1). Infarction following
the FNA procedure is well-recognized phenomenon in case of some
organs including thyroid (2). This
phenomenon has also been reported in the salivary gland (3-5),
and previous FNA procedure may induce histological alterations
including squamous metaplasia, infarction, necrosis, and
haemorrhage, resulting in potential overdiagnosis (5). Although extremely rare, it has been
documented that spontaneous infarction without previous FNA
procedure can occur in salivary gland tumours. To our knowledge,
there are very few reports (6-8)
and so this is only fourth cytological case report of spontaneous
infarction of PA of the parotid gland using immunocytochemical
analysis for the first time.
Case report
A 57-year-old Japanese female presented with
persistent swelling of the right neck region. Physical examination
revealed a relatively well-circumscribed tumour in the right
parotid gland. FNA examination of the right parotid gland tumour
was performed.
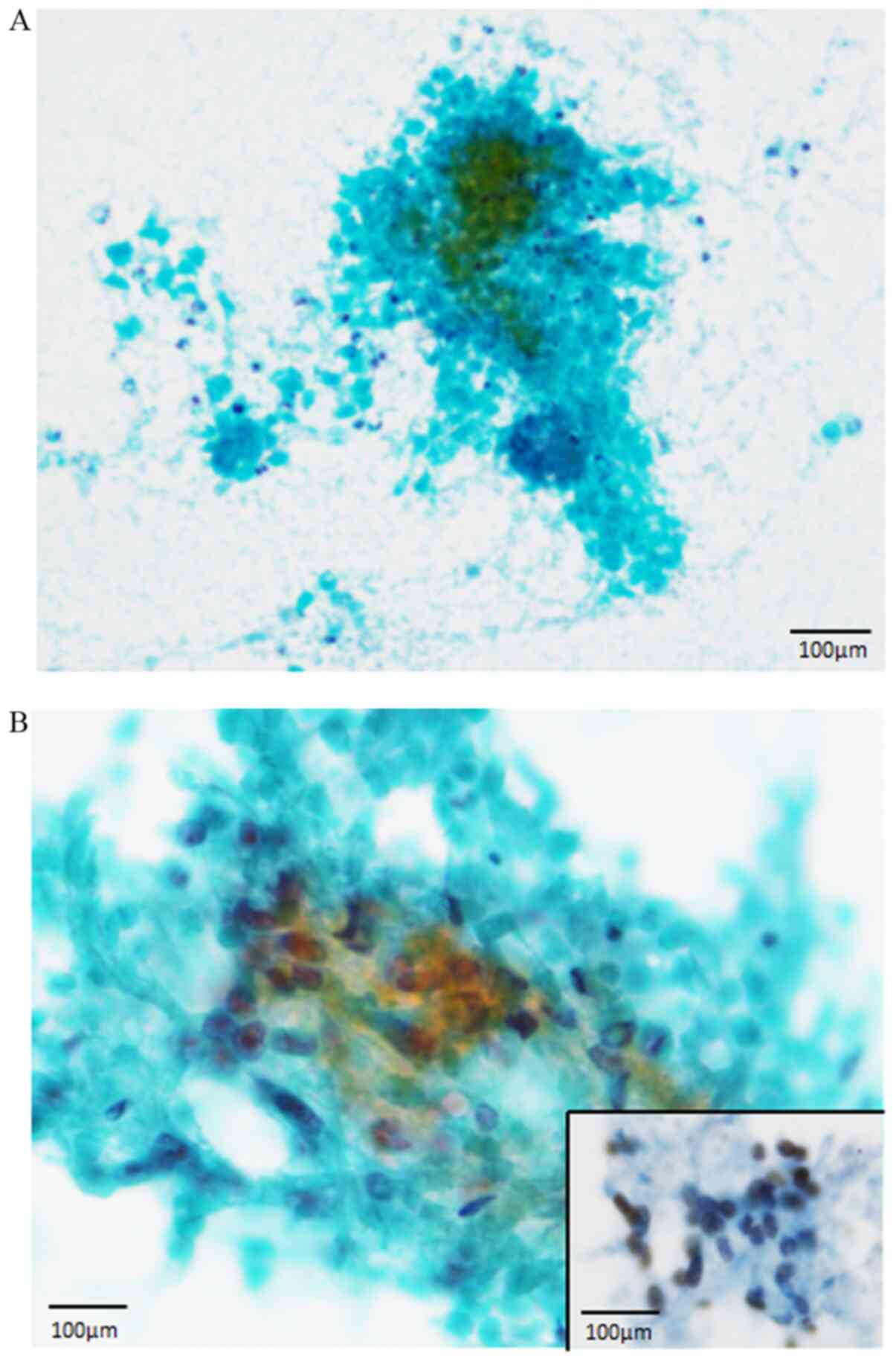
The Papanicolaou smear of the FNA specimens revealed
the presence of variable-sized completely necrotic cell clusters in
a necrotic background accompanying neutrophils (Fig. 1A). Only a few viable cell clusters
were observed, along with a few non-neoplastic acinar cells
(Fig. 1B). These cells were
polygonal to spindle-shaped and had large round to oval nuclei with
conspicuous nucleoli (Fig. 1B).
Although nuclear pleomorphism was noted, the nuclear chromatin was
fine and evenly distributed (Fig.
1B). No non-nucleated squamous cells were observed. Moreover,
typical neoplastic myoepithelial cells were not observed, and the
Giemsa staining did not reveal any chondromyxoid material. Presence
of these cytological features led to suspicion of malignancy
(carcinoma, not specified). Atypical polygonal to spindle-shaped
cells showed positive nuclear reactivity for p40 (BC28, Roche) by
immunocytochemical analysis (using archival slides and an
autostainer (XT System Benchmark, Roche, Basel, Switzerland)
(Fig. 1B, inset).
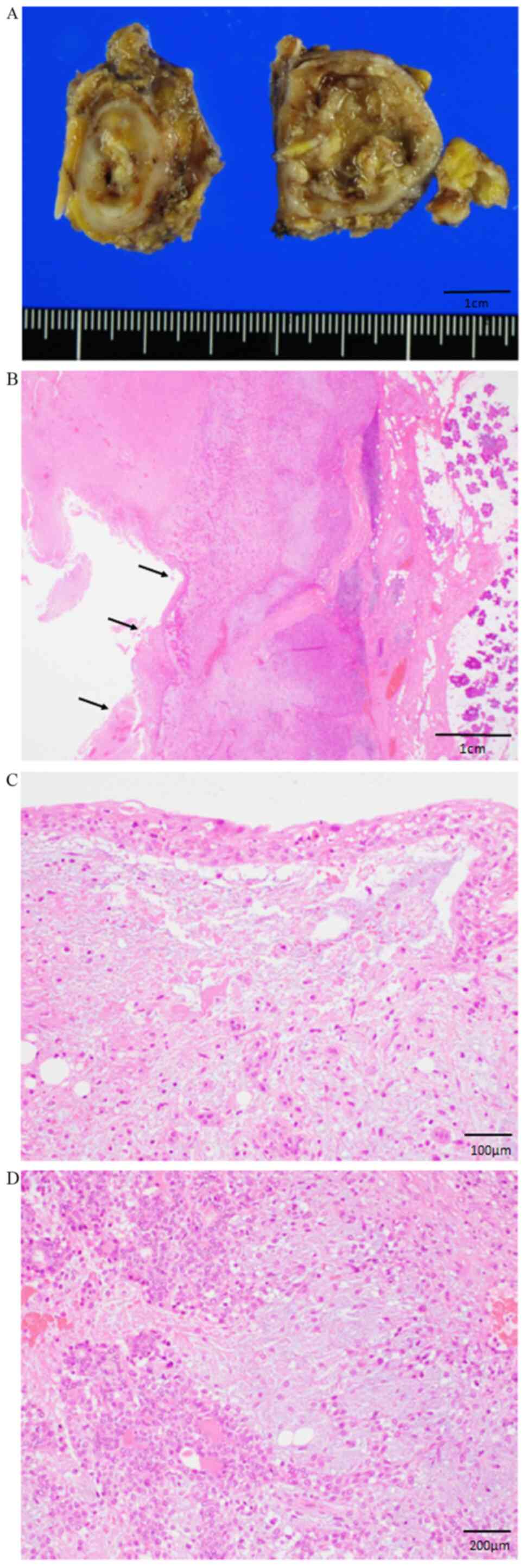
The surgical resection of the right parotid gland
tumour was performed. Histopathological examination of the resected
parotid gland tumour revealed a well-circumscribed tumour,
measuring 2.5x2.5 cm in diameter, and a cystic cavity filled with
necrotic tissue (Fig. 2A). Atypical
squamous metaplastic cells were present around this cavity
(Fig. 2B). These cells were
polygonal to spindle-shaped, and they exhibited large round to oval
nuclei containing a conspicuous nucleoli (Fig. 2C). Although nuclear pleomorphism was
noted, no mitotic features were observed in these metaplastic
cells. Conventional PA component, composed of proliferating
neoplastic myoepithelial cells with bland, round nuclei within a
myxochondromatous material and occasional ductal formation was
observed around the cavity (Fig.
2D). Accordingly, a diagnosis of PA with spontaneous infarction
was made. Post-operative course was uneventful, and no tumor
recurrence has been observed during 4 months of medical
follow-up.
Discussion
Here, we describe the first cytological report of
infarcted PA with immunocytochemical analysis of p40. Infarction
following FNA procedure in PA is a well-known phenomenon; however,
it might be associated with potential diagnostic challenges
(5). According to a study that
evaluated the histological alterations of parotid gland lesions
associated with pre-operative FNA, the resected specimens exhibited
acute and chronic haemorrhage and inflammation (100%); squamous
metaplasia (80%), which is considered as a reparative process
secondary to infarction; infarction and necrosis (40%); and stromal
hyalinization (30%) (5). Among
these characteristics, the presence of squamous metaplasia and
necrosis could lead to a histological misdiagnosis of carcinoma,
such as squamous cell carcinoma and mucoepidermoid carcinoma
(5).
Albeit extremely rare, infarction can occur in PA
without previous FNA procedure. Layfield et al described the
first cytological case of spontaneous infarcted PA (8). Since then, only three additional
cytological cases, including the present one, have been reported in
the English-language literature (6,7). The
cytological features of the infarcted PA are follows: i) Presence
of atypical squamous metaplastic cells in a necrotic background
(4/4 cases), ii) presence of anucleated squamous cells (3/4 cases),
and iii) presence of sheets of oncocytic cells without atypia (1/4
case) (6-8).
In all of these cases, an initial cytological diagnosis of probable
malignancy was made (6-8).
Atypical squamous metaplastic cells in a necrotic background is a
common cytological feature of infarcted PA; these cells could show
extremely atypical features, including ovoid to elongated large
nuclei, conspicuous nucleoli with irregular shapes and sizes, and
marked pleomorphism (6). These
atypical cells were considered as metaplastic squamous cells, as
per the histopathological features of the resected tumour. However,
immunocytochemical confirmation has not been performed. Our
immunocytochemical analysis clearly showed nuclear p40 expression
in the atypical cells with large nuclei containing conspicuous
nucleoli and nuclear pleomorphism. Accordingly, these atypical
cells in the cytological specimens of the infarcted PA were
confirmed as metaplastic squamous cells.
Cytological differential diagnostic considerations
in cases where atypical squamous cells are present in a necrotic
background include Warthin's tumour and mucoepidermoid carcinoma.
Presence of necrotic material is a common feature of Warthin's
tumour, and squamous cells are occasionally noted (9,10). The
cytological specimens of Warthin's tumour usually contain
characteristic oncocytic cells, along with squamous cells (10) which is a useful in diagnosis of
Warthin's tumour. Mucoepidermoid carcinoma has at least some mucous
and/or intermediate cells (10).
These features may aid differential diagnosis from infarcted
PA.
In conclusion, the present report describes the
cytological features of infarcted PA through immunocytochemical
analysis of p40 expression. Presence of atypical metaplastic
squamous cells positive for p40 in a necrotic background was
characteristic cytological feature of infarcted PA. Although a
necrotic background is an important indication of malignancy in the
cytological diagnosis of salivary gland tumours (11), the presence of atypical metaplastic
squamous cells in a necrotic background does not directly indicate
malignant diagnosis. Though cytological diagnosis of infarcted PA
is extremely difficult, pathologists and cytopathologists must
consider that atypical metaplastic squamous cells may be present in
benign salivary gland tumours, including infarcted PA.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
HI and MI conceived of and designed the study. HI,
MI, KO, KS, YE, SY, TF, HI and KT collected and analyzed the data.
HI and MI drafted the manuscript and figures. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
This study was conducted in accordance with the
Declaration of Helsinki and the study protocol was approved by the
Institutional Review Board of Kansai Medical University Hospital
(Approval no. 160954). Informed consent was obtained.
Patient consent for publication
Opt-out consent was obtained from participant of the
current study.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Klijanienko J and Vielh P: Fine-needle
sampling of salivary gland lesions I. Cytology and histology
correlation of 412 cases of pleomorphic adenoma. Diagn Cytopathol.
14:195–200. 1996.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Kini SR: Post-fine-needle biopsy
infarction of thyroid neoplasms: A review of 28 cases. Diagn
Cytopathol. 15:211–220. 1996.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Pabuççuoglu HU, Lebe B, Sarioglu S and
Lebe E: Infarction of pleomorphic adenoma: A rare complication of
fine-needle aspiration obscuring definitive diagnosis. Diagn
Cytopathol. 24:301–303. 2001.PubMed/NCBI View
Article : Google Scholar
|
|
4
|
Pinto RG, Couto F and Mandreker S:
Infarction after fine needle aspiration. A report of four cases.
Acta Cytol. 40:739–741. 1996.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Li S, Baloch ZW, Tomaszewski JE and
LiVolsi VA: Worrisome histologic alterations following fine-needle
aspiration of benign parotid lesions. Arch Pathol Lab Med.
124:87–91. 2000.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Fulciniti F, Losito NS, Botti G, Manola M
and Ionna F: Spontaneous infarction of pleomorphic adenoma: Report
of a case simulating malignancy on fine-needle cytology sample.
Diagn Cytopathol. 38:430–434. 2010.PubMed/NCBI View
Article : Google Scholar
|
|
7
|
Behzatoglu K, Bahadir B, Huq GE and Kaplan
HH: Spontaneous infarction of a pleomorphic adenoma in parotid
gland: Diagnostic problems and review. Diagn Cytopathol.
32:367–369. 2005.PubMed/NCBI View
Article : Google Scholar
|
|
8
|
Layfield LJ, Reznicek M, Lowe M and
Bottles K: Spontaneous infarction of a parotid gland pleomorphic
adenoma. Report of a case with cytologic and radiographic overlap
with a primary salivary gland malignancy. Acta Cytol. 36:381–386.
1992.PubMed/NCBI
|
|
9
|
Cobb CJ, Greaves TS and Raza AS: Fine
needle aspiration cytology and diagnostic pitfalls in Warthin's
tumor with necrotizing granulomatous inflammation and facial nerve
paralysis: A case report. Acta Cytol. 53:431–434. 2009.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Klijanienko J and Vielh P: Fine-needle
sampling of salivary gland lesions II. Cytology and histology
correlation of 71 cases of Warthin's tumor (adenolymphoma). Diagn
Cytopathol. 16:221–225. 1997.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Okano K, Ishida M, Sandoh K, Fujisawa T,
Iwai H and Tsuta K: Cytological features of carcinoma ex
pleomorphic adenoma of the salivary glands: A diagnostic challenge.
Diagn Cytopathol. 48:149–153. 2020.PubMed/NCBI View
Article : Google Scholar
|