Introduction
Anterior mediastinal tumors, including various types
of neoplasms, are relatively rare (1,2).
Although percutaneous needle biopsy is being used more frequently
to obtain a pathological diagnosis, more invasive procedures need
to be performed to obtain adequate tissue due to their size,
location and heterogeneity and patient characteristics (3-5).
Therefore, the preoperative diagnosis of anterior mediastinal
tumors is comprehensively determined by their clinical presentation
and several imaging modalities, including computed tomography (CT),
magnetic resonance imaging (MRI) or positron emission tomography
(PET). Although essential for the detection of anterior mediastinal
tumors, CT alone cannot differentiate between benign and malignant
tumors in some cases (5). To
improve the accuracy of preoperative diagnosis, MRI and/or PET is
added to CT, depending upon the surgeon's discretion following
guidelines (5). Aside from tumor
detection, MRI is useful in the qualitative assessment of tumors
such hemorrhagic or inflammatory thymic cysts that mimic solid
tumors (6,7). The utility of PET for the clinical
diagnosis of malignant tumors, including thymoma and thymic cancer,
has been reported in numerous publications (8-19).
Fluorodeoxyglucose (FDG) accumulation in high-risk thymoma,
particularly thymic carcinoma, is evidently greater compared with
in low-risk thymoma (10-18,20).
The role of fluorodeoxyglucose-positron emission tomography
(FDG-PET) in differentiating benign and malignant thymic masses has
been previously evaluated by several small-scale studies (21). Therefore, the clinical significance
of PET in distinguishing malignant from benign anterior mediastinal
tumors is still unclear. Furthermore, the diagnostic accuracy of CT
for malignant anterior mediastinal tumors may further improve by
addition of PET or MRI, but it remains unclear whether either
adding PET or MRI is useful. Accurate diagnosis of benign tumors by
imaging modalities is important to avoid unnecessary open
thoracotomy. The present study aimed to elucidate the functionality
of adding a PET or MRI to CT in the diagnosis of the anterior
mediastinal tumors, compared with CT alone. The present study
retrospectively analyzed the sensitivity, specificity, positive
predictive value (PPV) and negative predictive value (NPV) for
these modalities.
Patients and methods
Population
The study was a retrospective analysis of the
medical records of 104 consecutive patients (52 males and 52
females; age range, 1-84 years, mean age 54.0 years) who had
undergone surgery for anterior mediastinal tumor at the Department
of General Surgical Science at Gunma University (Gunma, Japan)
between April 2003 and March 2015. Patients who had undergone
percutaneous biopsy during the same period for a preoperative
diagnosis were excluded from the present study. All patients had
undergone clinical examination, chest X-rays and CT of the chest;
additional PET and/or MRI were determined by each surgeon during
the preoperative diagnosis. In the subgroup analysis, 31 patients
with both additional PET and MRI to CT were excluded to directly
compare with the advantages of additional PET vs. MRI to CT in the
clinical diagnosis of anterior mediastinal tumors. It is difficult
to determine the effect of adding either PET or MRI on accurate
diagnosis in anterior mediastinal tumors in patients with
additional PET and MRI. The study was approved by the ethics
committee of the Gunma University Hospital.
FDG-PET imaging
Patients fasted for at least 4 h before
18F-FDG PET examination. Patients received intravenous
FDG at a dose of 200-250 million Becquerels (MBq) ~1 h before
imaging. Image acquisition was performed using the Advance NXi PET
scanner (GE Healthcare) and the Discovery (LS) PET scanner (GE
Healthcare). Three-dimensional emission scanning was performed from
the groin area up to the top of the skull. The PET images were
reviewed independently by two experienced physicians. The data
obtained were reconstructed by iterative ordered subset expectation
maximization. To evaluate 18F-FDG accumulation, each
tumor was examined visually and the maximum standardized uptake
value (SUV) of the entire tumor was determined.
Preoperative diagnosis and data
analysis
The radiological findings on CT, MRI or PET were
examined by two radiologists from the Gunma University Graduate
School of Medicine who specialized in diagnosing mediastinal
lesions. Final preoperative diagnosis was comprehensively
determined by clinical presentation and several imaging modalities
that were discussed in a conference that involved chest
radiologists, physicians and thoracic surgeons. Pathological
diagnosis was confirmed on surgically resected specimens. Clinical
preoperative diagnosis and surgical pathological diagnosis, as well
as sensitivity, specificity, PPV, NPV and accuracy were compared
among the patient groups. Specifically, patients were divided into
two groups: Additional PET to another modality and no additional
PET to another modality. The patients were further subdivided into
three groups to compare with the advantages of additional PET vs.
MRI to CT in the clinical diagnosis of anterior mediastinal tumors:
i) CT alone; ii) additional MRI to CT and iii) additional PET to
CT.
Statistical analysis
McNemar's test was used to compare the
sensitivities, specificities and overall accuracies of additional
PET or MRI to CT. Student's t-test and χ2 test were used
to compare continuous and categorical variables, respectively.
Calculations and statistical tests were performed using JMP 5.0
(SAS Institute Inc.). P<0.05 was considered to indicate a
statistically significant difference.
Results
Pathological diagnosis of anterior
mediastinal tumors
Among the 104 patients included in the present
study, 69 (66.3%) had malignant tumors, including thymoma (n=51),
thymic cancer (n=8), thymic carcinoid (n=4), and germinoma (n=2)
(Table I). Two malignant lesions,
from the stomach and the thyroid, were of metastatic origin. The
remaining 35 patients (33.7%) had benign lesions, including thymic
cysts (n=18), mature teratoma (n=6), bronchogenic cysts (n=3),
pericardial cysts (n=3), and others (n=5), such as neurogenic
tumors, lymphangioma, fibroinflammatory lesions, cavernous
hemangioma and chondroma.
 | Table IPathological diagnosis of anterior
mediastinal tumors after surgical resection. |
Table I
Pathological diagnosis of anterior
mediastinal tumors after surgical resection.
| Pathological
diagnosis | No. (%) |
|---|
| Benign | |
|
Thymic
cysts | 18 (17.3) |
|
Mature
teratoma | 6 (5.8) |
|
Bronchogenic
cysts | 3 (2.9) |
|
Pericardial
cysts | 3 (2.9) |
|
Other | 5 (4.8) |
|
Total
(Benign) | 35 (33.7) |
| Malignant | |
|
Thymoma | 51 (49.0) |
|
Thymic
carcinoma | 8 (7.7) |
|
Thymic
carcinoid | 4 (3.8) |
|
Germinoma | 2 (1.9) |
|
Other | 4 (3.8) |
|
Total
(Malignant) | 69 (66.3) |
Comparison of clinical factors with or
without additional PET to another modality for the detection of
anterior mediastinal tumors
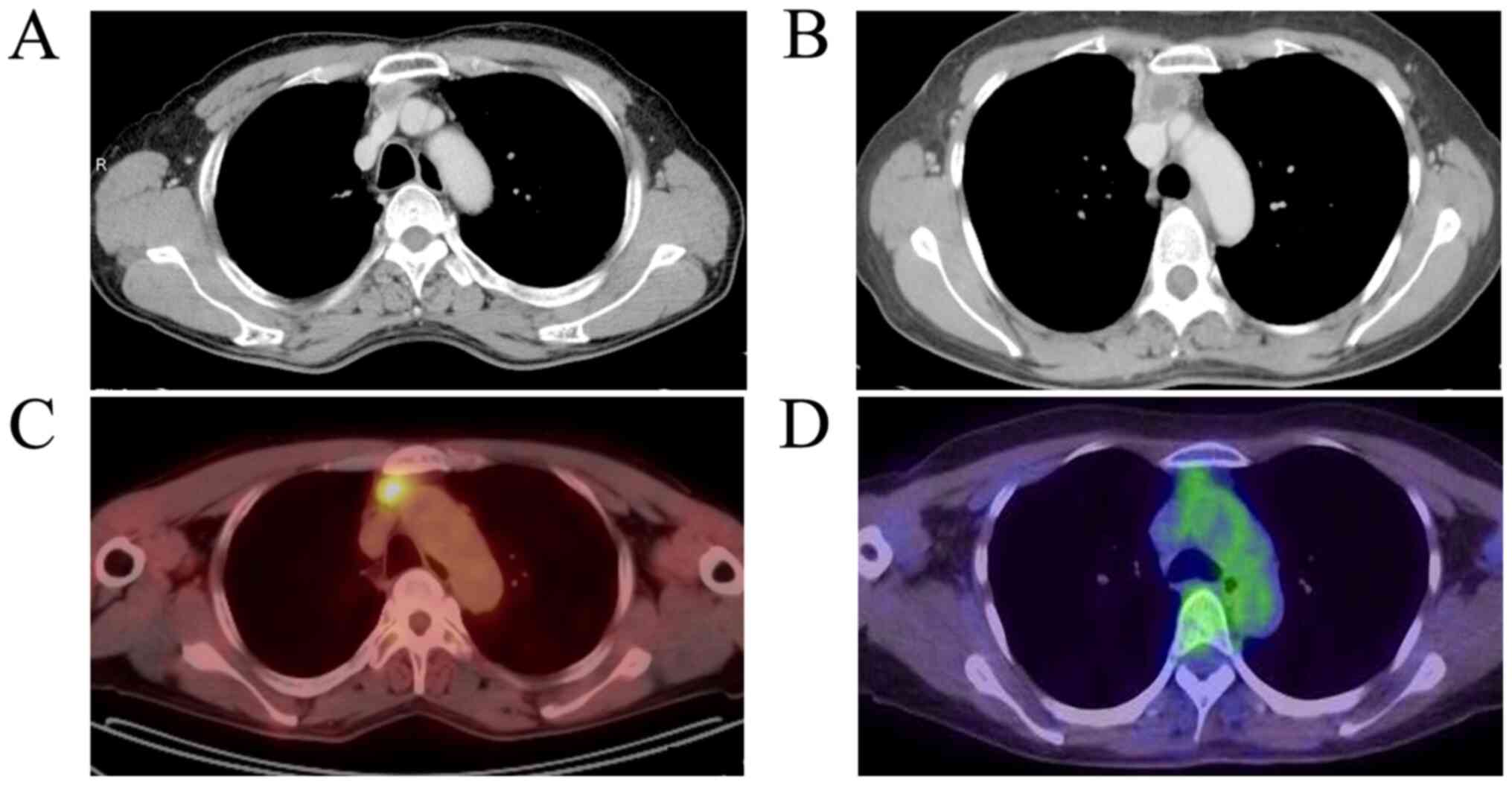
Due to increased glucose metabolism, malignant
tumors typically demonstrate higher FDG uptake compared with benign
tumors (Figs. 1 and 2). The proportion of the patients who
underwent imaging modalities with additional PET and those without
additional PET for preoperative diagnosis were 62.5% (n=65) and
37.5% (n=39), respectively. There was no significant difference in
the age, sex, tumor size, preoperative diagnosis and surgical
approach in the two subgroups (Table
II). The ratio of CT enhancement and presence of MRI images
were comparable between the two subgroups. In cases that did not
undergo PET, the sensitivity and specificity of the clinical
diagnosis of malignancy was 95.2 and 31.6%, respectively (Table III). The sensitivity, specificity,
PPV, NPV and accuracy of the additional PET in detecting malignancy
were 98.0, 75.0, 92.2, 92.3 and 92.2%, respectively. There were
significant differences in specificity and accuracy for detecting
malignancy between the additional PET and the no additional PET
group.
 | Table IIComparison of clinical factors with or
without additional PET to another modality for the detection of
anterior mediastinal tumors. |
Table II
Comparison of clinical factors with or
without additional PET to another modality for the detection of
anterior mediastinal tumors.
| Characteristic | PET- (n=39) | PET+ (n=65) | P-value |
|---|
| Age, mean (range)
(years) | 50.6 (1-84) | 56.5 (28-79) | 0.0776 |
| M/F [n (%)] | 18/21
(46.2/53.9) | 34/31
(52.3/47.7) | 0.5433 |
| Tumor size, mean
(range) (cm) | 4.3 (1.4-9.5) | 4.6 (1.0-11.5) | 0.6530 |
| CT enhancement -/+ [n
(%)] | 9/30 (23.1/76.9) | 6/59 (9.2/90.8) | 0.0558 |
| Additional MRI -/+ [n
(%)] | 19/20
(48.7/51.3) | 33/32
(50.8/49.2) | 0.8395 |
| Preoperative
diagnosis, benign/malignant [n (%)] | 7/32 (18.0/82.0) | 13/52
(20.0/80.0) | 0.7972 |
| Approach, VATS/open
[n (%)] | 16/23
(41.1/58.9) | 29/36
(44.6/55.4) | 0.7206 |
 | Table IIIEfficacy comparison of adding PET for
the detection of malignant tumors. |
Table III
Efficacy comparison of adding PET for
the detection of malignant tumors.
| Subgroup | Sensitivity | Specificity | PPV | NPV | Accuracy |
|---|
| PET- | 95.2 (19/20) | 31.6 (6/19) | 60.6 (19/32) | 85.7 (6/7) | 65.0 (25/39) |
| PET+ | 98.0 (48/49) | 75.0a (4/16) | 92.2 (48/52) | 92.3 (12/13) | 92.2a (60/65) |
Comparison of efficacy of adding PET
or MRI to CT for the detection of malignant tumors
To directly compare the advantages of additional PET
or MRI to CT in the clinical diagnosis of anterior mediastinal
tumors, a subgroup analysis was performed on 73 patients (31
patients were excluded) with additional PET and MRI to CT. The
proportion of the patients who underwent preoperative diagnosis by
CT alone, additional MRI to CT and additional PET to CT were 28.7%
(n=21), 26.0% (n=19) and 45.2% (n=33), respectively (Table SI). To directly compare the
efficacy between adding PET and MRI, three subgroups were selected:
CT alone, adding MRI to CT and adding PET to CT. As shown in
Table IV, CT alone had sufficient
diagnostic sensitivity for malignant tumors and there was no
additional improvement in sensitivity after adding PET or MRI.
However, all seven benign lesions were diagnosed as malignant by CT
alone (Table IV). None of the
patients with benign tumors were classified correctly
(specificity=0%); in these cases, the specificity and NPV of adding
MRI to CT to detect malignant lesions increased up to 50 and 100%,
respectively; the accuracy was comparable with CT alone. Adding PET
to CT showed a significant improvement in specificity and accuracy
for detecting malignant tumors, compared with either additional MRI
to CT or CT alone.
 | Table IVEfficacy comparison of adding PET
and/or MRI to CT for the detection of malignant tumors. |
Table IV
Efficacy comparison of adding PET
and/or MRI to CT for the detection of malignant tumors.
| Subgroup | Sensitivity | Specificity | PPV | NPV | Accuracy |
|---|
| CT alone | 92.9 (13/14) | 0 (0/7) | 69.0 (13/20) | 0 (0/1) | 61.9 (13/21) |
| CT + MRI | 100 (6/6) | 50.0a (6/12) | 50.0 (6/12) | 100 (6/6) | 63.1 (12/19) |
| CT + PET | 100 (28/28) | 80.0a,b (4/5) | 96.6 (28/29) | 100 (4/4) | 97.0a,b (32/33) |
However, the results of the present study are
subject to bias due to its retrospective design. Although almost
all the clinicopathological factors were comparable among the
groups, the mean age of the additional MRI to CT group was lower
and had a higher frequency of benign lesions compared with other
groups (Table SI).
Discussion
Preoperative diagnosis of anterior mediastinal
tumors is comprehensively determined by clinical presentation and
several imaging modalities as needle biopsy is usually anatomically
difficult to perform. Because there has been no consensus on the
optimal preoperative diagnosis of anterior mediastinal tumors, the
choice of imaging modality to add to CT is determined by the
surgeon (1-5).
The present study found the utility of adding PET, but not MRI, to
CT for detecting benign from malignant anterior mediastinal
tumors.
CT is essential for the diagnosis of anterior
mediastinal tumors (5). It was
reported that morphological changes, including intralesional fat,
midline location and triangular thymic shapes on the CT may help
characterize thymic masses as benign (22,23).
In the present study, all seven benign lesions were diagnosed as
malignant by CT alone, based on the lobulated contour,
heterogeneous enhancement and increased diameter. The specificity
of CT examination alone was more accurate in all cases, including
follow-up cases without surgical indication because our series
included only consecutive patients who had undergone surgical
resection for highly suspicious malignant lesions. However, in the
present study, CT alone had higher sensitivity, but lower
specificity in detecting malignancy, indicating that it was not
sufficient for the diagnosis of benign anterior mediastinal
tumors.
Numerous studies reported the utility of PET for the
diagnosis of malignant anterior mediastinal tumors (8-20).
Due to increased glucose metabolism, malignant tissues typically
demonstrate higher FDG uptake compared with benign and normal
tissue. The role of FDG PET in differentiating benign and malignant
thymic masses was previously evaluated in a study, albeit a small
sample size (21). Therefore, the
clinical significance of PET in differentiating benign and
malignant anterior mediastinal tumors is still unclear. The present
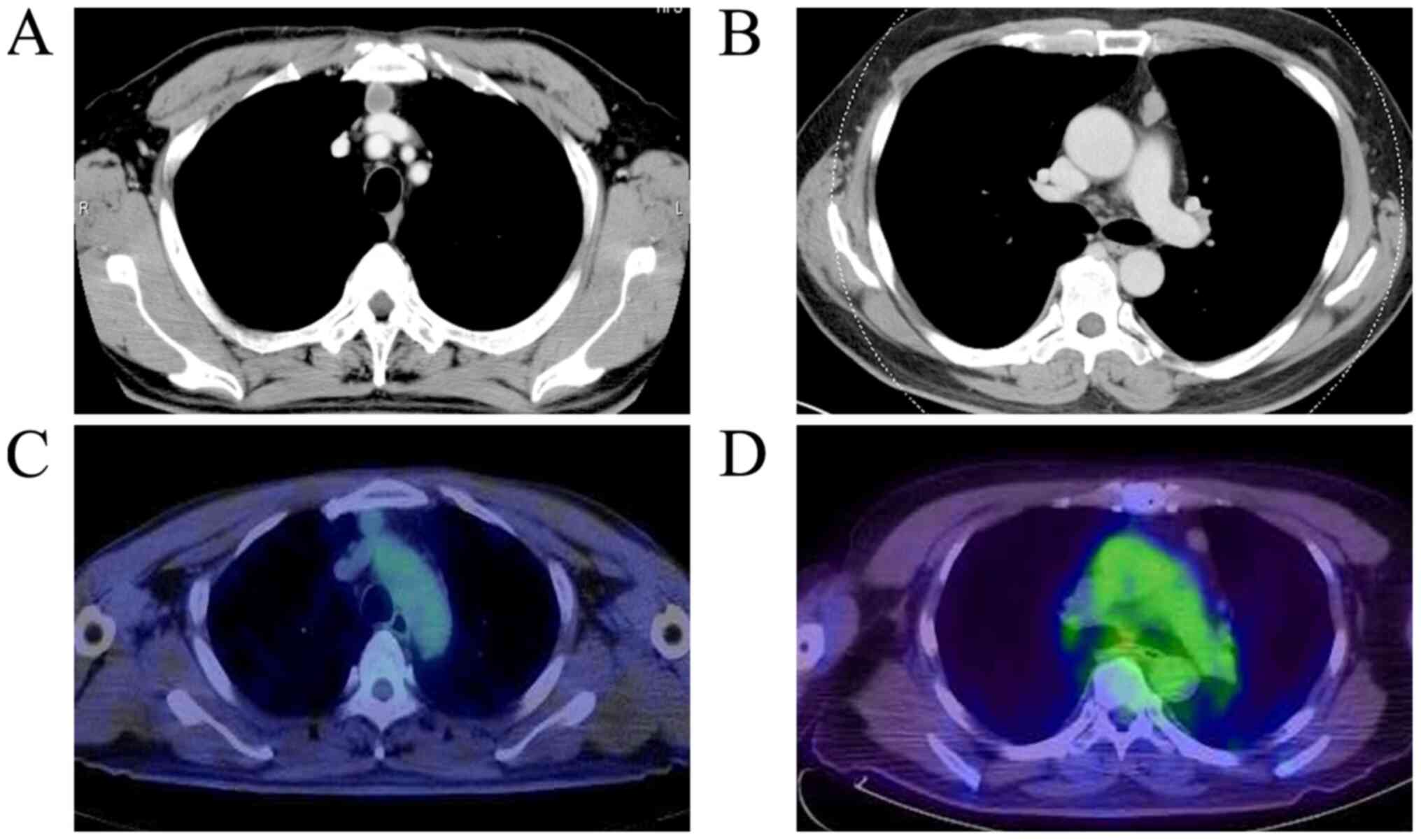
study found that adding PET to CT showed high sensitivity and
specificity for detecting these tumors. In particular, the
specificity and PPV improved after adding PET, as almost all the
benign anterior mediastinal lesions did not have an FDG uptake,
resulting in true diagnosis as a benign lesion (Fig. 2). The high accuracy of additional
PET to CT was not affected by irrespective of MRI presence.
Therefore, preoperative diagnosis of anterior mediastinal tumors by
CT requires additional PET, but not MRI. A number of patients may
undergo invasive procedures for benign disease; in fact, in the
present study, 28 patients underwent resection and 13 patients
underwent sternotomy. Additional PET to CT may be valuable in
deciding the need for the surgical resection of anterior
mediastinal tumors and could be considered as standard procedure in
the preoperative assessment of patients with these tumors in the
future.
MRI is useful for the qualitative assessment of
tumors, especially cystic lesions, including benign thymic cysts
(5). Therefore, adding MRI to CT
may improve the specificity and false-positive rate of detecting
malignant tumors. The present study found that compared with CT
alone, adding MRI to CT substantially increased the specificity,
but the false-positive rate was higher (CT: 7/7, MRI: 6/12). The
proportion of benign lesions detected by additional MRI to CT was
significantly higher (63.2%) compared with the other groups
(37.1%); differences in patient characteristics may have
contributed to the lower specificity of additional MRI to CT. A
study reported that diffusion-weighted (DW) MRI had much higher
specificity and accuracy for differentiating between malignant and
benign anterior mediastinal lesions than conventional MRI protocols
(24). Further analysis is needed
to confirm the utility of MRI in the diagnosis of anterior
mediastinal tumors.
In addition, it was reported that DW MRI could add a
‘histologic’ parameter for malignant invasion by measuring cell
density and apparent diffusion coefficient (ADC) values (24). Therefore, combining the SUV of PET
and the ADC of DW MRI may be more useful in diagnosing malignancy.
Further studies are needed to confirm this possibility.
The present study did not assess the utility of each
modality for detecting malignant tumors because, in our opinion, a
comprehensive diagnosis using several imaging modalities may be
more clinically realistic. Clinical presentation, including tumor
markers and signs of myasthenia gravis (MG), also play an important
role in the preoperative diagnosis of anterior mediastinal tumors
(1-5).
In the present study, the number of patients diagnosed with thymoma
with MG by CT alone was higher than that by adding PET to CT (data
not shown). These data showed that additional PET did not improve
the specificity and accuracy of CT alone. Several detailed
examinations on clinical presentation are needed to establish the
utility of PET.
The present study had several limitations. First is
the retrospective design with the relatively small number of
samples; although >100 patients were included, we plan to extend
the study to a larger patient population. Since anterior
mediastinal tumors are relatively rare, a large scale, prospective
multicenter study is needed. Second, the selection bias is
inevitable as only patients who underwent surgical resection were
included. Therefore, more cases, including follow-up cases treated
by chemotherapy or radiotherapy without surgical indication, should
be included to determine the true accuracy of additional PET to CT.
Third, the selection is based on surgeon's decision, which may
cause selection bias.
In conclusion, additional PET has advantages over CT
alone in clinically distinguishing benign from malignant tumors of
the mediastinum, regardless of additional MRI. Furthermore, adding
PET may help guiding the decision-making process for performing
surgical resection for anterior mediastinal tumors.
Supplementary Material
Comparison of clinical factors in
patients with adding PET or MRI to CT for the detection of anterior
mediastinal tumors.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author upon reasonable
request.
Authors' contributions
TY and AM were involved in the study design. TY
contributed to the preparation of the manuscript and data analysis.
EY, RO, TK, KS and HK contributed to the data analysis and prepared
the tables. All authors read and approved the final manuscript and
agree to be accountable for all aspects of the work.
Ethics approval and consent to
participate
The present study was approved by the ethics
committee of Gunma University Hospital. The requirement for
informed consent was waived by the ethics committee because of the
study's retrospective nature; however, patients could opt out of
sharing their information.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Duwe BV, Sterman DH and Musani AI: Tumors
of the mediastinum. Chest. 128:2893–2909. 2005.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Yoneda KY, Louie S and Shelton DK:
Mediastinal tumors. Curr Opin Pulm Med. 7:226–233. 2001.
|
|
3
|
Kern JA, Deniel TN, Trible CG, Silen ML
and Rodgers BM: Thoracoscopic diagnosis and treatment of
mediastinal masses. Ann Thorac Surg. 56:92–96. 1993.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Rendina EA, Venuta F, De Giacomo T,
Ciriaco PP, Pescarmona EO, Francioni F, Pulsoni A, Malagnino F and
Ricci C: Comparative merits of thoracoscopy, mediastinoscopy, and
mediastinotomy for mediastinal biopsy. Ann Thorac Surg. 57:992–995.
1994.PubMed/NCBI View Article : Google Scholar
|
|
5
|
David SE, Gregory JR and Wallace A: NCCN
Clinical Practice Guidelines in Oncology (NCCN Guidelines®)
Thymomas and Thymic Carcinomas. J Natl Compr Cancer Netw.
11:562–576. 2013.
|
|
6
|
Tomiyama N, Honda O, Tsubamoto M, Inoue A,
Sumikawa H, Kuriyama K, Kusumoto M, Johkoh T and Nakamura H:
Anterior mediastinal tumors: Diagnostic accuracy of CT and MRI. Eur
J Radiol. 69:280–288. 2009.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Sakai S, Murayama S, Soeda H, Matsuo Y,
Ono M and Masuda K: Differential diagnosis between thymoma and
non-thymoma by dynamic MR imaging. Acta Radiol. 43:262–268.
2002.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Endo M, Nakagawa K, Ohde Y, Okumura T,
Kondo H, Igawa S, Nakamura Y, Tsuya A, Murakami H, Takahashi T, et
al: Utility of 18FDG-PET for differentiating the grade
of malignancy in thymic epithelial tumors. Lung Cancer. 61:350–355.
2008.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Terzi A, Bertolaccini L, Rizzardi G, Luzzi
L, Bianchi A, Campione A, Comino A and Biggi A: Usefulness of 18-F
FDG PET/CT in the pre-treatment evaluation of thymic epithelial
neoplasms. Lung Cancer. 74:239–243. 2011.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Lococo F, Cesario A, Okami J, Cardillo G,
Cavuto S, Tokunaga T, Apolone G, Margaritora S and Granone P: Role
of combined18F-FDG-PET/CT for predicting the WHO
malignancy grade of thymic epithelial tumors: A multicenter
analysis. Lung Cancer. 82:245–251. 2013.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Igai H, Matsuura N, Tarumi S, Chang SS,
Misaki N, Go T, Ishikawa S and Yokomise H: Usefulness of
[18F]fluoro-2-deoxy-D-glucose positron emission
tomography for predicting the world health organization malignancy
grade of thymic epithelial tumors. Eur J Cardiothorac Surg.
40:143–145. 2011.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Otsuka H: The utility of FDG-PET in the
diagnosis of thymic epithelial tumors. J Med Invest. 59:225–234.
2012.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Luzzi L, Campione A, Gorla A, Vassallo G,
Bianchi A, Biggi A and Terzi A: Role of fluorine-flurodeoxyglucose
positron emission tomography/computed tomography in preoperative
assessment of anterior mediastinal masses. Eur J Cardiothorac Surg.
36:475–479. 2009.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Shibata H, Nomori H, Uno K, Sakaguchi K,
Nakashima R, Iyama K, Tomiyoshi K, Kaji M, Goya T, Suzuki T and
Horio H: 18F-fluorodeoxyglucose and
11C-acetate positron emission tomography are useful
modalities for diagnosing the histologic type of thymoma. Cancer.
115:2531–2538. 2009.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Kaira K, Sunaga N, Ishizuka T, Shimizu K
and Yamamoto N: The role of [18F]fluorodeoxyglucose
positron emission tomography in thymic epithelial tumors. Cancer
Imaging. 11:195–201. 2011.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Toba H, Kondo K, Sadohara Y, Otsuka H,
Morimoto M, Kajiura K, Nakagawa Y, Yoshida M, Kawakami Y, Takizawa
H, et al: 18F-fluorodeoxyglucose positron emission
tomography/computed tomography and the relationship between
fluorodeoxyglucose uptake and the expression of hypoxia-inducible
factor-1α, glucose transporter-1 and vascular endothelial growth
factor in thymic epithelial tumours. Eur J Cardiothorac Surg.
44:e105–e112. 2013.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Fukumoto K, Taniguchi T, Ishikawa Y,
Kawaguchi K, Fukui T, Kato K, Matsuo K and Yokoi K: The utility of
[18F]-fluorodeoxyglucose positron emission
tomography-computed tomography in thymic epithelial tumours. Eur J
Cardiothorac Surg. 42:e152–e156. 2012.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Sung YM, Lee KS, Kim BT, Choi JY, Shim YM
and Yi CA: 18F-FDG PET/CT of thymic epithelial tumors:
Usefulness for distinguishing and staging tumor subgroups. J Nucl
Med. 47:1628–1634. 2006.PubMed/NCBI
|
|
19
|
Seki N, Sakamoto S, Karube Y, Oyaizu T,
Ishihama H and Chida M: 18F-fluorodeoxyglucose positron
emission tomography for evaluation of thymic epithelial tumors:
Utility for world health organization classification and predicting
recurrence-free survival. Ann Nucl Med. 28:257–262. 2014.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Yajima T, Mogi A, Shimizu K, Kosaka T,
Ohtaki Y, Obayashi K, Nakazawa S, Nakajima T, Tsushima Y and
Shirabe K: Quantitative analysis of metabolic parameters at
18F-fluorodeoxyglucose positron emission tomography in
predicting malignant potential of anterior mediastinal tumors.
Oncol Lett. 19:1865–1871. 2020.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Kitami A, Sano F, Ohashi S, Suzuki K,
Uematsu S, Suzuki T and Kadokura M: The usefulness of
positron-emission tomography findings in the management of anterior
mediastinal tumors. Ann Thorac Cardiovasc Surg. 23:26–30.
2017.PubMed/NCBI View Article : Google Scholar
|
|
22
|
McErlean A, Huang J, Zabor EC, Moskowitz
CS and Ginsberg MS: Distinguishing benign thymic lesions from
early-stage thymic malignancies on computed tomography. J Thorac
Oncol. 8:967–973. 2013.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Priola SM, Priola AM, Cardinale L, Perotto
F and Fava C: The anterior mediastinum: Anatomy and imaging
procedures. Radiol Med. 111:295–311. 2006.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Priola AM, Priola SM, Giraudo MT, Gned D,
Fornari A, Ferrero B, Ducco L and Veltri A: Diffusion-weighted
magnetic resonance imaging of thymoma: Ability of the apparent
diffusion coefficient in predicting the world health organization
(WHO) classification and the Masaoka-Koga staging system and its
prognostic significance on disease-free survival. Eur Radiol.
26:2126–2138. 2016.PubMed/NCBI View Article : Google Scholar
|