Introduction
Until recently, nodular fasciitis has been
considered to be a reactive process of uncertain cause (1). The recent identification of genomic
rearrangements indicates that nodular fasciitis is a self-limiting
clonal neoplastic process (2).
Nodular fasciitis is most commonly found in adults of 20 to 50
years of age and is rarely seen on the hands (3). Differentiating between nodular
fasciitis and sarcomas is often clinically and pathologically
challenging as nodular fasciitis exhibits rapid growth, high
cellularity, and mitotic activity (3). In addition, a recent report suggested
that nodular fasciitis displays malignant behavior such as multiple
recurrent lesions and metastasis (4).
We report a case in which a locally aggressive
nodular fasciitis lesion grew rapidly on the patient's palm, and
discuss the surgical management of the lesion. Our case suggests
that fusion gene analysis was useful for differentiating nodular
fasciitis from sarcomas. In addition, marginal excision was
sufficient even though the tumor was extremely aggressive and grew
fast, since our patient did not develop local recurrence or
metastasis in two years.
Case report
A 53-year-old female presented with a four-month
history of a painful mass on her left palm. Her medical history
included hyperthyroidism and uterine myomas, but she did not recall
any trauma involving her left hand. On physical examination, a 2-cm
mass was found around the hypothenar eminence. It was elastic,
slightly mobile, and tender. The associated pain and numbness
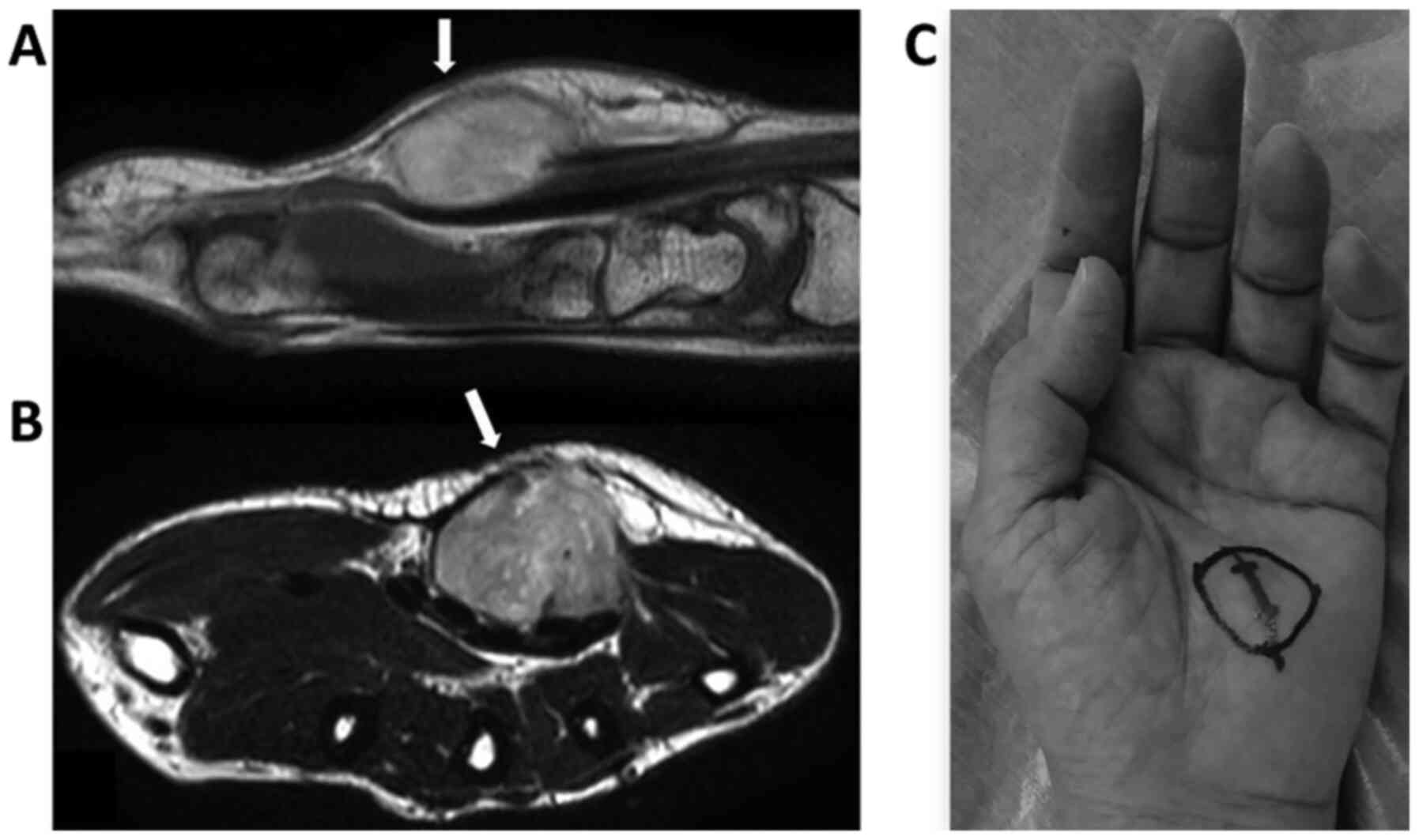
radiated towards the patient's ring and little fingers. On magnetic
resonance imaging, a lesion measuring 20x15x30 mm was located
between the palmar aponeurosis and flexor tendons (Fig. 1). It was well delineated and
exhibited low intensity on T1-weighted imaging, whereas it was
isointense on T2-weighted imaging and displayed inhomogeneous
contrast enhancement. An open biopsy showed a lesion composed of
spindle-shaped cells, which was consistent with nodular fasciitis.
After the biopsy, the patient's pain and numbness were unchanged,
and a marginal excision was planned.
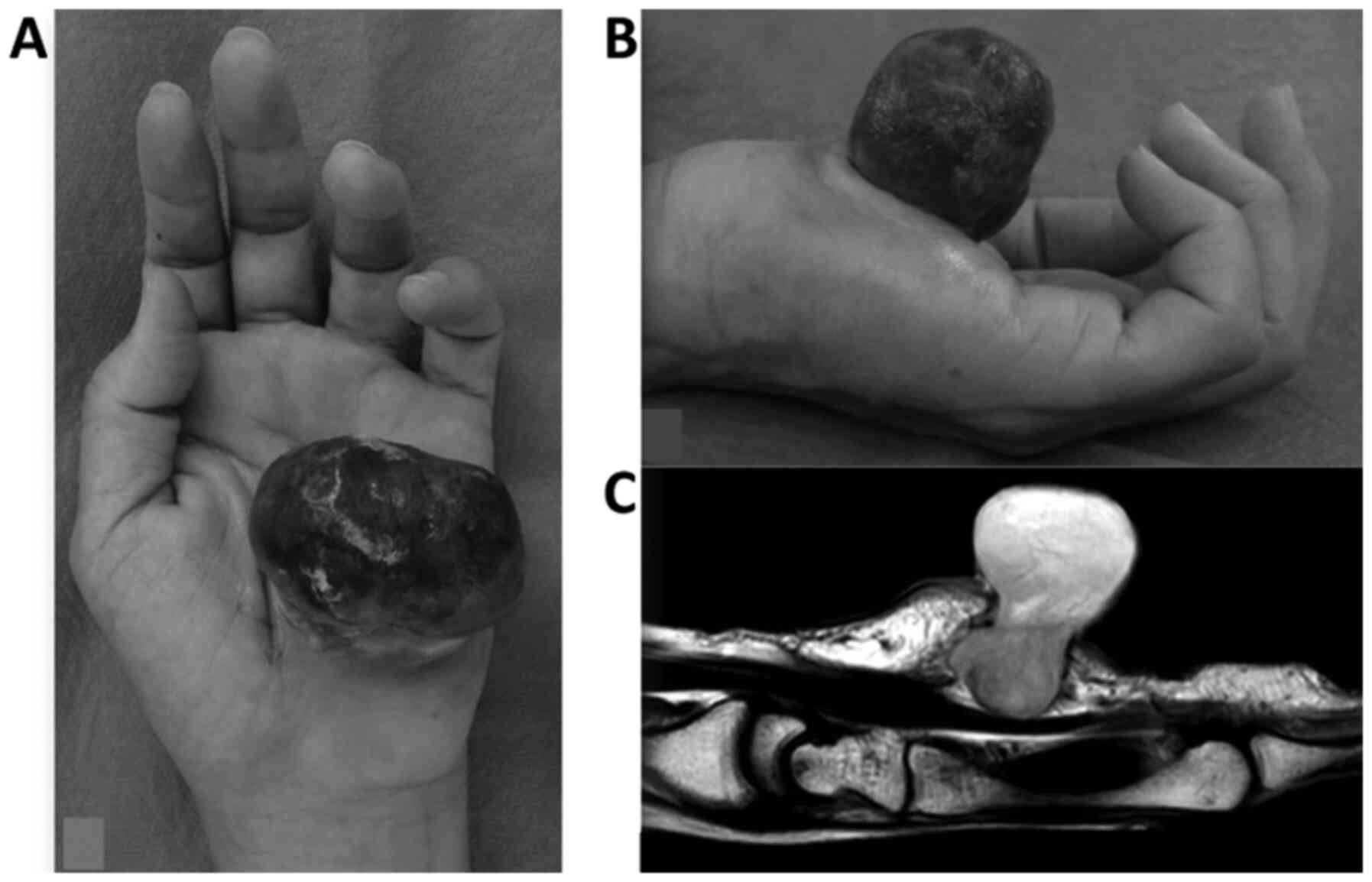
Two weeks after the initial biopsy, the wound
opened, and the tumor protruding from the palm had reached the size
of a golf ball (Fig. 2). The
numbness affecting the patient's left ring and little fingers
disappeared after the wound dehiscence, possibly because the
pressure on the ulnar nerve had been reduced. Another incisional
biopsy was carried out to exclude malignancies, as the tumor had
grown extremely fast, and we suspected that it was a sarcoma. The
lesion outside the skin, which measured 47x35x40 mm, was excised
for histological examination. The cut surface of the lesion was
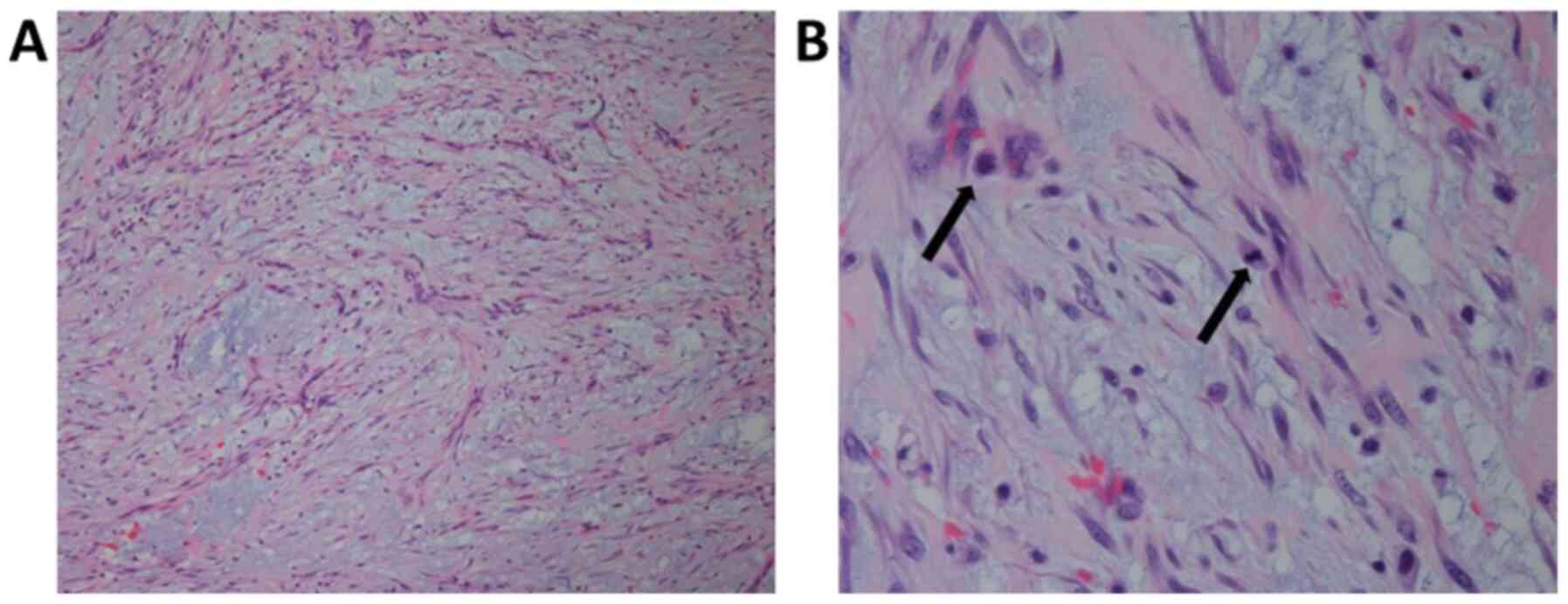
gelatinous and hemorrhagic. Histologically, it consisted of
spindle-shaped cells proliferating in a myxoid stroma (Fig. 3). The lesion demonstrated low
cellularity. There were some mitotic figures without atypical
mitoses, and slight pleomorphism was seen among the proliferating
spindle-shaped cells. Some of the cells exhibited slightly
hyperchromatic nuclei, but no bizarre nuclei were seen. These are
typical histological findings of nodular fasciitis. On
immunohistochemistry, the tumor was found to be positive for smooth
muscle actin, vimentin, and p16, but negative for epithelial
membrane antigen, bcl-2, CD34, CD56, cytokeratin AE1/AE3, desmin,
mic2 (CD99), anaplastic lymphoma kinase, S-100, mucin 4, and signal
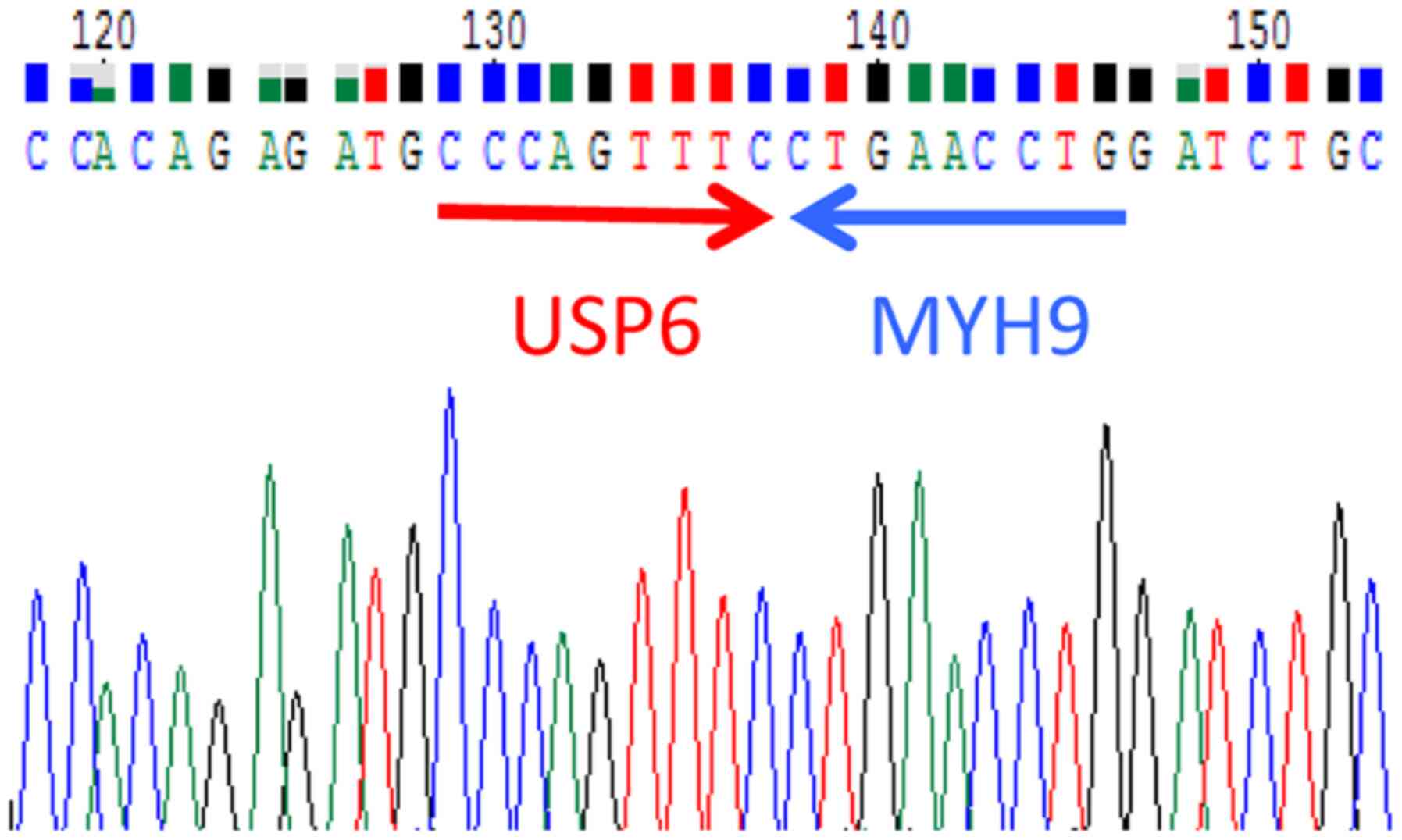
transducer and activator of transcription 6. RNA was extracted from
the frozen specimen and subjected to reverse transcription
polymerase chain reaction (RT-PCR) using the primers myosin-9
(MYH9) 75F: 5'-AGGGCACGGAAGGCTAAGC-3' and ubiquitin
carboxyl-terminal hydrolase 6 (USP6) 1630R:
5'-TGTGGATGTGAACTGCGGTC-3'. This revealed the presence of the
MYH9-USP6 fusion gene, which supported a diagnosis of nodular
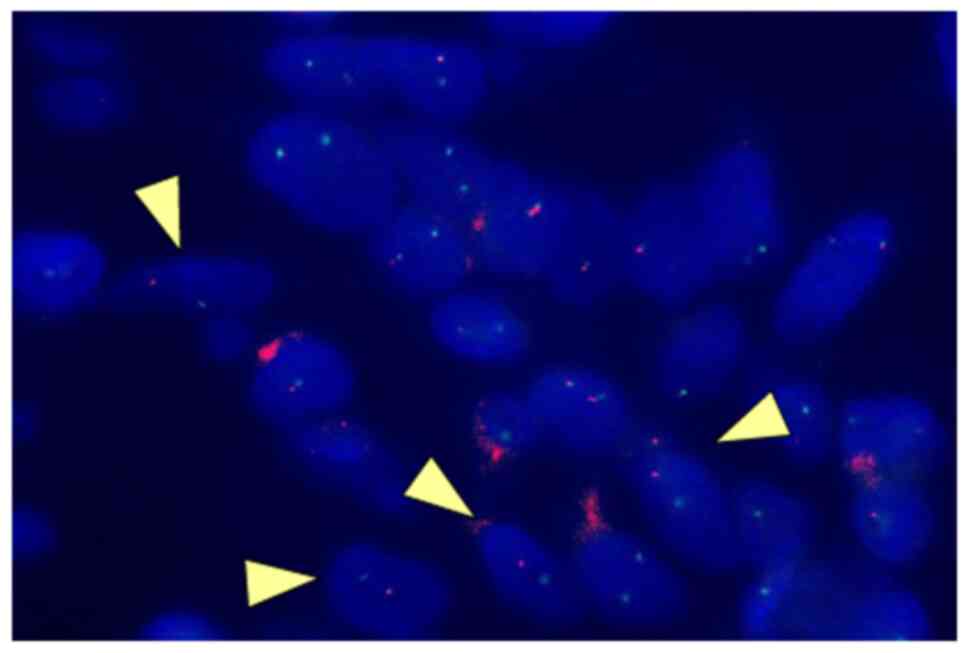
fasciitis (Fig. 4). Fluorescence
in situ hybridization (FISH) also confirmed the chromosomal
translocation (Fig. 5).
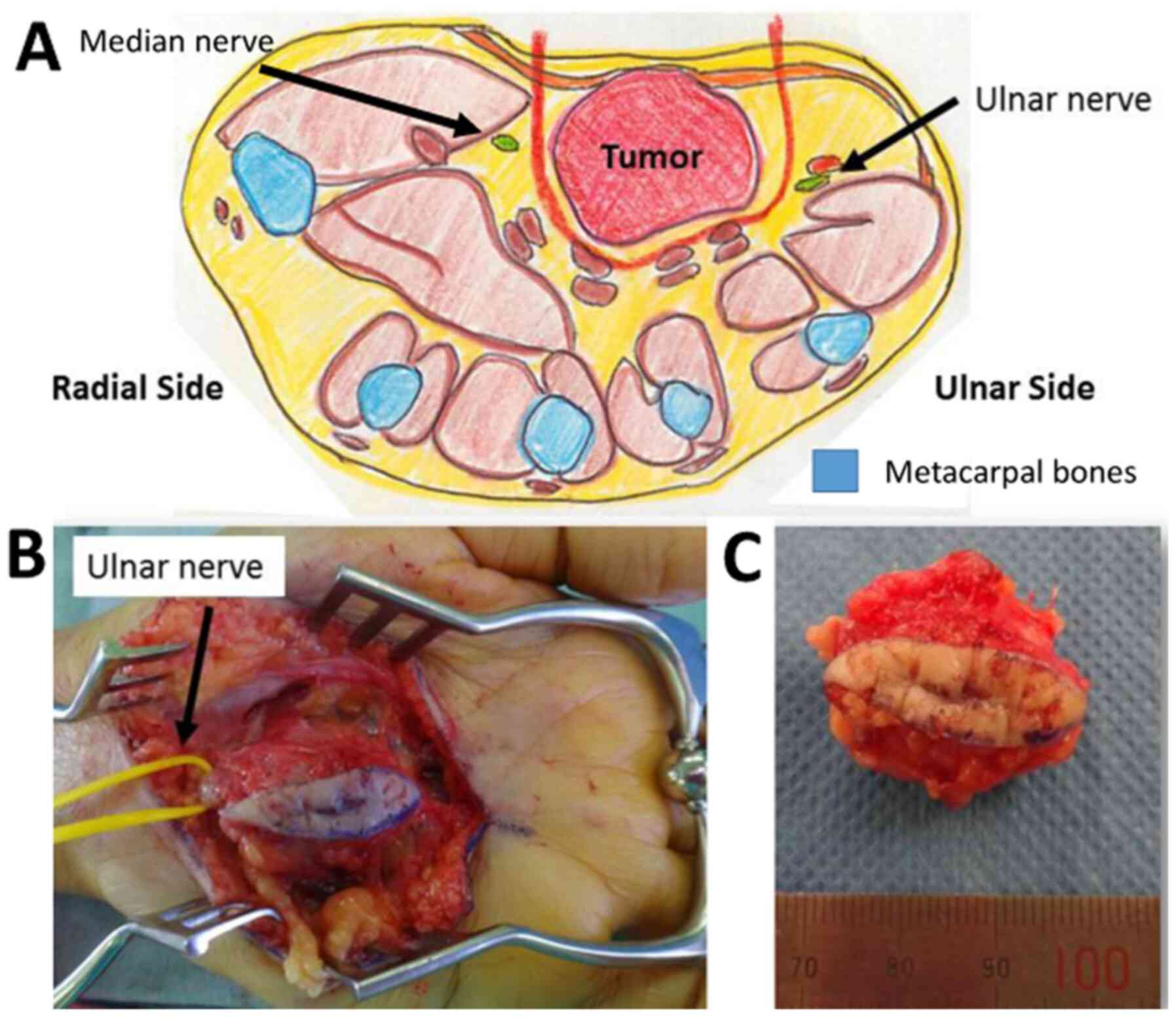
Since the histological examination did not suggest
that the lesion was a sarcoma or other type of malignancy, the
tumor was marginally excised. A spindle-shaped incision was
employed, and the palmar aponeurosis was excised en bloc (Fig. 6). The palmaris brevis was partially
resected together with the tumor, as it was very close to the
lesion. The ulnar nerve, which was located under the tumor, was
released and kept intact. The median nerve was not exposed, as it
was sufficiently far away from the tumor. The superficial palmar
artery and venous arches had adhered to the tumor; therefore, they
were ligated and sacrificed. After the excision of the tumor, the
skin was closed directly without flaps or skin grafts. The patient
had not suffered any local recurrence or metastasis at 24 months
post-operation.
Discussion
We reported a rare case of aggressive nodular
fasciitis of the hand. A strong point of this study is the
confirmation of the MYH9-USP6 fusion gene by both RT-PCR and FISH.
In addition, the tumor was biopsied twice to confirm the diagnosis.
The patient was already followed up for two years without local
recurrence of metastasis. A limitation of the study is that this is
a case report and we do not have similar cases to compare the
outcomes. Some nodular fasciitis may behave differently and require
different treatment strategies. Although we believe that our case
is sufficiently informative because the size and speed of tumor
growth were aggressive, the tumor was locally controlled by
surgical excision only.
Nodular fasciitis of the palm is rare and may
exhibit very rapid growth, mimicking that of sarcomas. Such
aggressive growth can cause nerve palsy, especially when the tumor
is located in the hand, as it is rich in nerves. Kanaya et
al reported a case in which intraneural nodular fasciitis
caused median nerve palsy and eventually required the resection of
the median nerve (5). Sevilla et
al reported a case in which a large nodular fasciitis lesion on
the palm grew to 9 cm in five months (6). According to the latter report, the
patient stated that the lesion had grown faster in the few weeks
before their initial visit. The location and size of the tumor were
similar to those of our case; thus, nodular fasciitis of the palm
may have the potential to grow rapidly and to be of considerable
size.
The relationship between the malignant potential of
nodular fasciitis and its oncogenic mechanism is currently being
intensively investigated (4). In
contrast, some nodular fasciitis lesions are self-limiting and
spontaneously regress (7,8). Guo et al reported a case of
‘malignant nodular fasciitis’, which recurred several times and
even metastasized to soft tissues (4). In the latter case, molecular analyses
revealed the presence and amplification of the
serine/threonine-protein phosphatase 6 catalytic subunit
(PPP6)-USP6 fusion gene, which resulted in upregulated
transcription of USP6 mRNA. In addition, Guo et al suggested
that USP6 amplification may underlie the biology of many
unclassifiable low-grade spindle-shaped cell/myofibroblastic
sarcomas.
Nodular fasciitis often poses a diagnostic challenge
to pathologists, as it does not express any specific
immunohistochemical markers, and until recently, the diagnosis of
such lesions was based on histological features alone. In 2011,
rearrangement of the USP6 gene was reported as a recurrent and
specific finding of nodular fasciitis (2). USP6 gene rearrangement was found in
92% of cases of nodular fasciitis, and the sensitivity and
specificity of FISH for detecting USP6 were reported to be 86 and
100%, respectively (2,9). The detection of USP6 fusion genes may
be useful for diagnosing nodular fasciitis lesions.
As for the treatment of nodular fasciitis lesions,
surgical excision is usually curative. Some clinicians recommend
that nodular fasciitis lesions should initially be observed because
of the self-limiting nature of the disease (8). We recommend excising such lesions,
especially when they are symptomatic, and marginal resection seems
to be sufficient for achieving local control. Intralesional or
piecemeal resection may be employed when the lesion is located
adjacent to nerves, although it may increase the risk of tumor
growth (5).
In conclusion, we reported a rare case of aggressive
nodular fasciitis of the hand. The lesion increased rapidly in
size, and obtainment of a histological diagnosis was challenging,
as the lesion exhibited non-specific immunohistochemical findings.
The detection of the MYH9-USP6 fusion gene supported a diagnosis of
nodular fasciitis. In spite of its aggressive characteristics, the
tumor was locally controlled via marginal excision, and no
metastasis was detected postoperatively.
Acknowledgements
The authors would like to thank Ms. Kimie Nomura
(Department of Pathology, Saitama Cancer Center) for her help with
the molecular diagnosis.
Funding
No funding was received.
Availability of data and materials
Data sharing is not applicable to this article, as
no datasets were generated or analyzed during the present
study.
Authors' contributions
CS drafted the manuscript. AI and HK performed the
histological examination. JM and HK supervised and reviewed the
contents of the manuscript and the data and image analysis. CS, TG,
AI, JM, and HK contributed to acquisition, analysis, and
interpretation of data, and writing and revision of the manuscript
critically for important intellectual content. All authors read and
approved the final version of the manuscript.
Ethics approval and consent to
participate
This study was approved by the ethics committee of
Saitama Cancer Center (approval no. 1119).
Patient consent for publication
The consent for publication of the manuscript and
the related images was obtained from the patient.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Oliveira AM and Chou MM: USP6-induced
neoplasms: The biologic spectrum of aneurysmal bone cyst and
nodular fasciitis. Hum Pathol. 45:1–11. 2014.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Erickson-Johnson MR, Chou MM, Evers BR,
Roth CW, Seys AR, Jin L, Ye Y, Lau AW, Wang X and Oliveira AM:
Nodular fasciitis: A novel model of transient neoplasia induced by
MYH9-USP6 gene fusion. Lab Invest. 91:1427–1433. 2011.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Goldblum JR, Weiss SW and Folpe AL (eds):
Benign fibroblastic/myofibroblastic proliferations, including
superficial fibromatoses. In: Enzinger and Weiss's Soft Tissue
Tumors. 6th edition. Elsevier Health Sciences, Philadelphia,
pp188-255, 2013.
|
|
4
|
Guo R, Wang X, Chou MM, Asmann Y, Wenger
DE, Al-Ibraheemi A, Molavi DW, Aboulafia A, Jin L, Fritchie K, et
al: PPP6R3-USP6 amplification: Novel oncogenic mechanism in
malignant nodular fasciitis. Genes Chromosomes Cancer. 55:640–649.
2016.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Kanaya K, Iba K, Yamashita T, Wada T and
Hasegawa T: Intraneural nodular fasciitis in a child: A case report
and review of the literature. J Hand Surg Am. 41:e299–e302.
2016.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Sevilla JJ, Ares-Rodriguez O, Seijas R and
Perez-Dominguez M: Unusual presentation of nodular fasciitis of the
hand. A case report. Acta Orthop Belg. 75:141–144. 2009.PubMed/NCBI
|
|
7
|
Al-Qattan MM and Arafah MM: Nodular
fasciitis of the hand: Excision preserving ‘vital’ structures. J
Hand Surg Eur Vol. 39:881–884. 2014.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Nishida Y, Tsukushi S, Wasa J, Iwata Y,
Kozawa E and Ishiguro N: Nodular fasciitis of the finger and hand:
Case report. J Hand Surg Am. 35:1184–1186. 2010.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Shin C, Low I, Ng D, Oei P, Miles C and
Symmans P: USP6 gene rearrangement in nodular fasciitis and
histological mimics. Histopathology. 69:784–791. 2016.PubMed/NCBI View Article : Google Scholar
|