Introduction
Primary lung cancer is common and often malignant,
and is accompanied with a high mortality rate (1). Distant metastases caused by primary
lung cancer are frequently identified in the brain, liver, adrenal
glands and bones, while the gastrointestinal tract is a relatively
unusual site for metastases to occur (2). The incidence of gastrointestinal
metastases of lung cancer was <2% a previous clinical study,
which was much lower compared with its prevalence identified during
autopsies (3). The low clinical
incidence of gastrointestinal metastasis may be due to the fact the
metastasis is usually asymptomatic (4). The clinical incidence and associated
mortality rate of lung cancer are low and the lack of symptoms may
cause studies to be difficult to organize (4). However, in recent years, an increased
number of cases of primary lung cancer have been reported to
metastasize to the gastrointestinal tract, which indicated that the
prevalence of gastrointestinal metastasis may be more frequent
(3). In addition, numerous
retrospective studies have reported that the gastrointestinal
metastasis of lung cancer was an indicator of poor prognosis,
demonstrating a median survival time of 69-130.3 days (3-7).
The present case study reported a patient with upper
gastrointestinal bleeding caused by the duodenal metastasis of a
primary lung adenocarcinoma, which is an extremely rare
complication in the history of the occurrence and development of
lung cancer.
Case report
A 62-year-old male, who had experienced a cough and
hoarseness for 1 month, was admitted to our hospital in June 2017.
He had a history of duodenal ulcers and bleeding, diabetes mellitus
and hypertension. He was also an active ex-smoker and had a family
history of different types of cancer; his father had lung cancer,
his elder brother had colon cancer and his two younger sisters had
uterine and breast cancer, respectively. A CT scan revealed the
presence of a mass in the left upper lobe of the chest. Therefore,
a thoracoscopic lobectomy was performed on the left upper lobe and
the posterior segment of the left lower lobe. In addition, the
patient was discovered to have both hilar and mediastinal
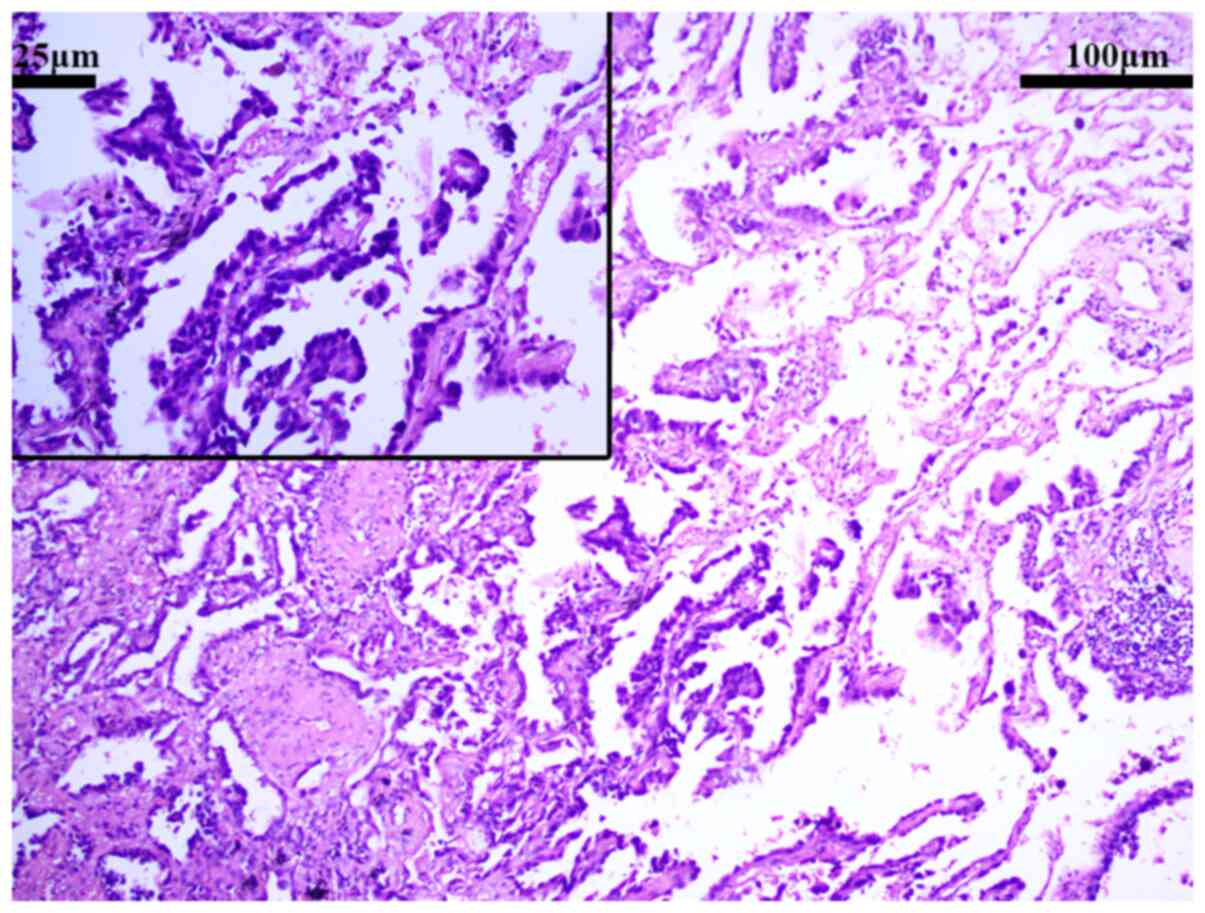
lymphadenopathy and biopsies were taken. The histopathological
examination revealed a well-differentiated adenocarcinoma with
lymph node metastasis and partial infiltration into the pulmonary
membrane (T4N2M1) (Figs. 1 and
2). The patient received six cycles
of chemotherapy with liposomal paclitaxel and cisplatin, six cycles
of chemotherapy with pemetrexed, and five cycles of chemotherapy
with pemetrexed and carboplatin.
After complaining of abdominal pain for 3 days, the
patient was readmitted to our hospital in July 2019. While
conducting physical examinations, the doctors noted that the
patient was mildly pale and that there was mild tenderness in the
epigastrium, but recorded no signs of rigidity or rebound
tenderness. Laboratory investigations revealed that the patient had
anemia, with hemoglobin levels of 104 g/l and a carcin embryonic
antigen (CEA) level of 113.2 µg/l. The stool test for the presence
of occult blood returned positive. CT-positron emission tomography
(CT-PET) and an abdominal CT scan revealed that the patient had
brain, bone and hepatic metastases. The patient underwent
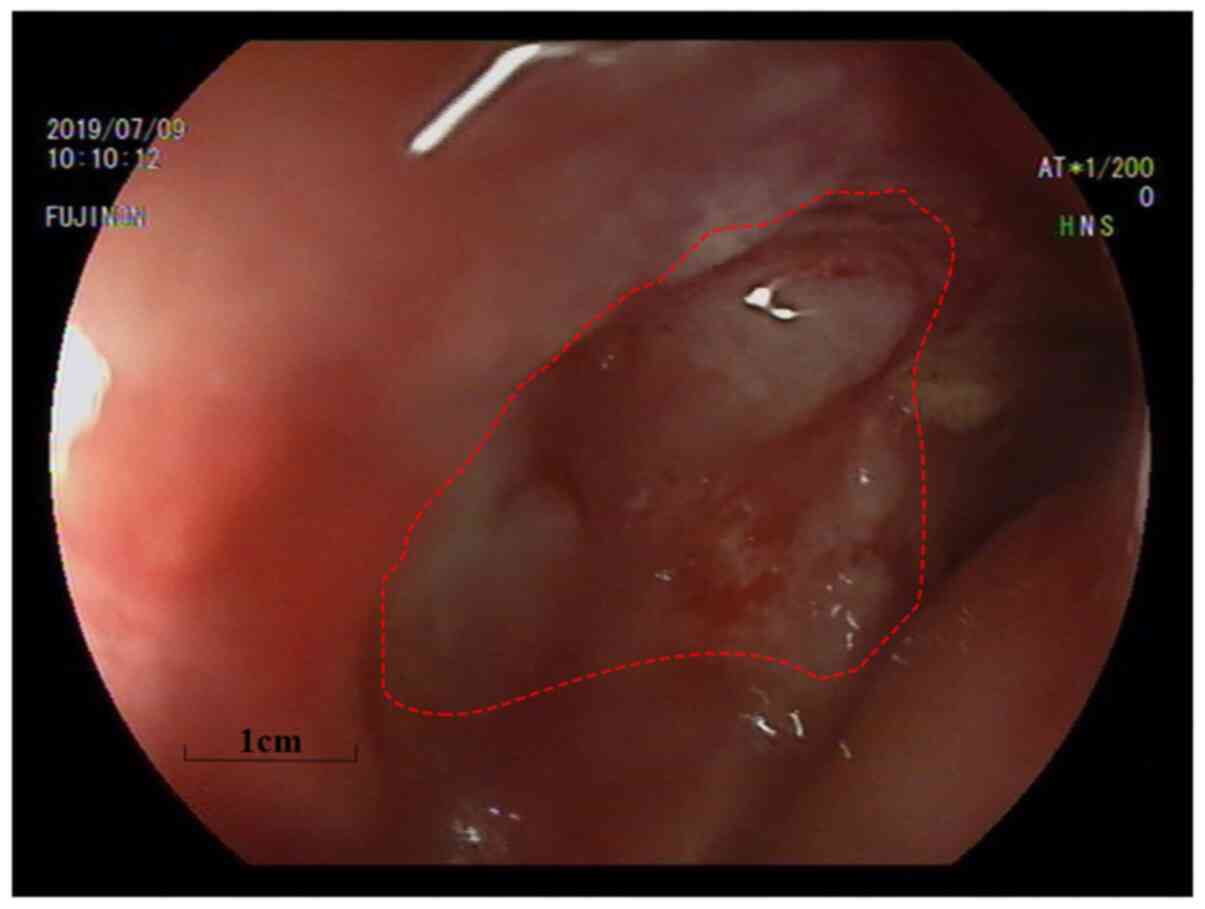
esophagogastroduodenoscopy, which confirmed the presence of a
2.5x3.5 cm malignant ulcer accompanied by the whitish center due to
the thick layers of skin cells and bloody discharge in the junction
between the bulb and descending portions of the duodenum (Fig. 3). The results of the
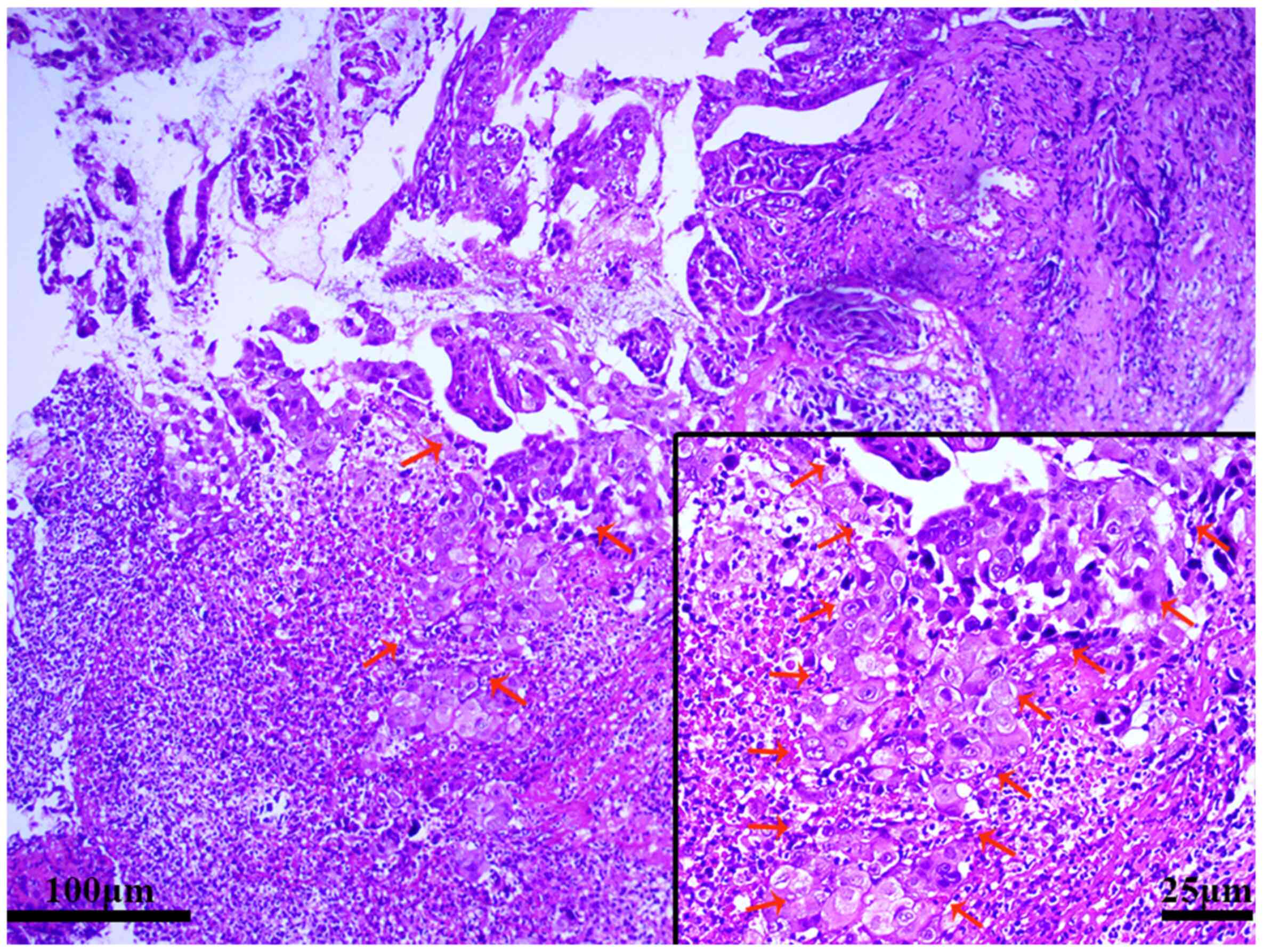
histopathological examination of the duodenal mucosal biopsy
specimen demonstrated that the mucosa was denatured and necrotic,
with a heteromorphic epithelioid cell infiltration consisting of
solitary cells, or cells arranged in sheets, microglandular duct
and/or papillary formations (Fig.
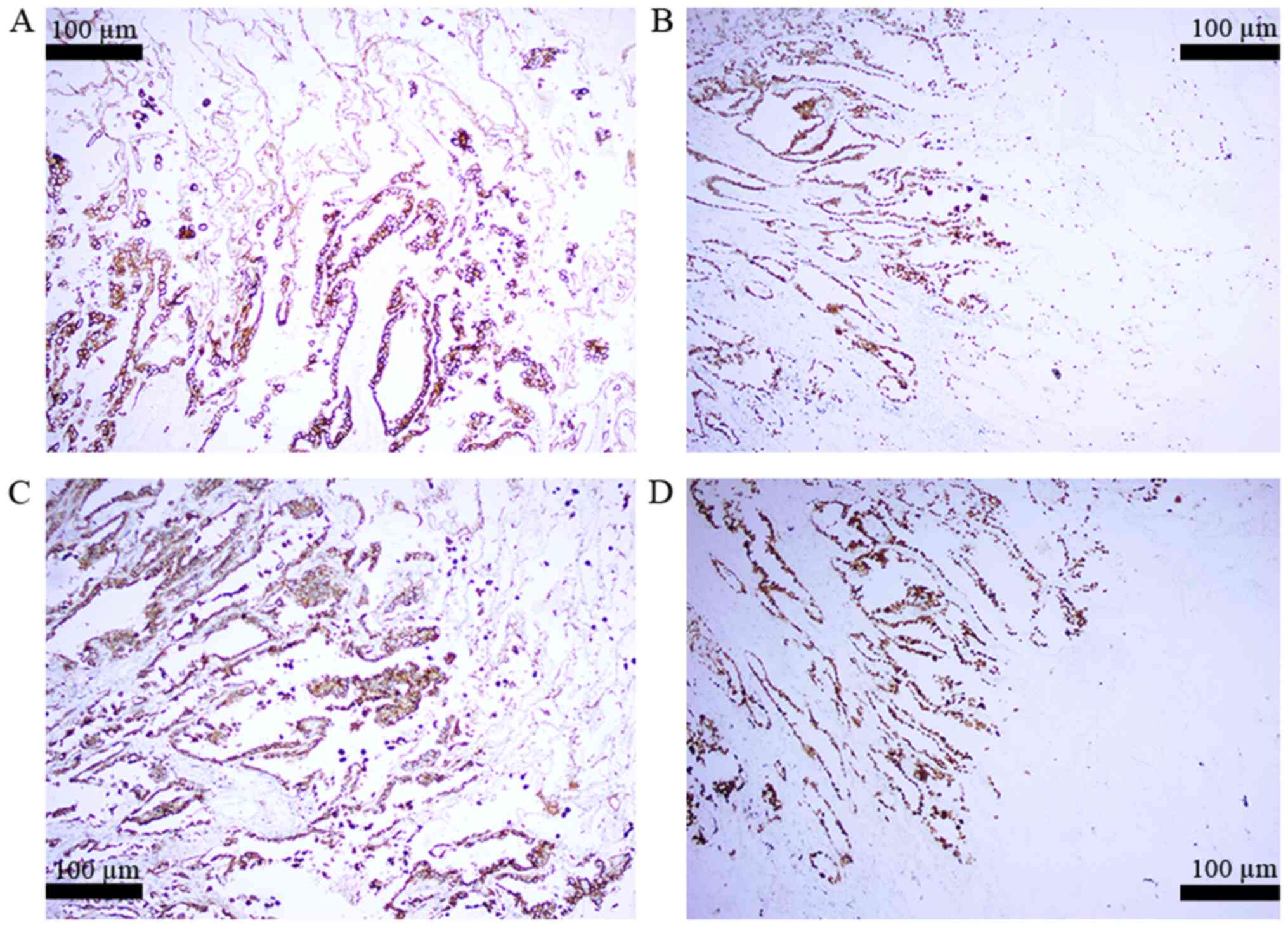
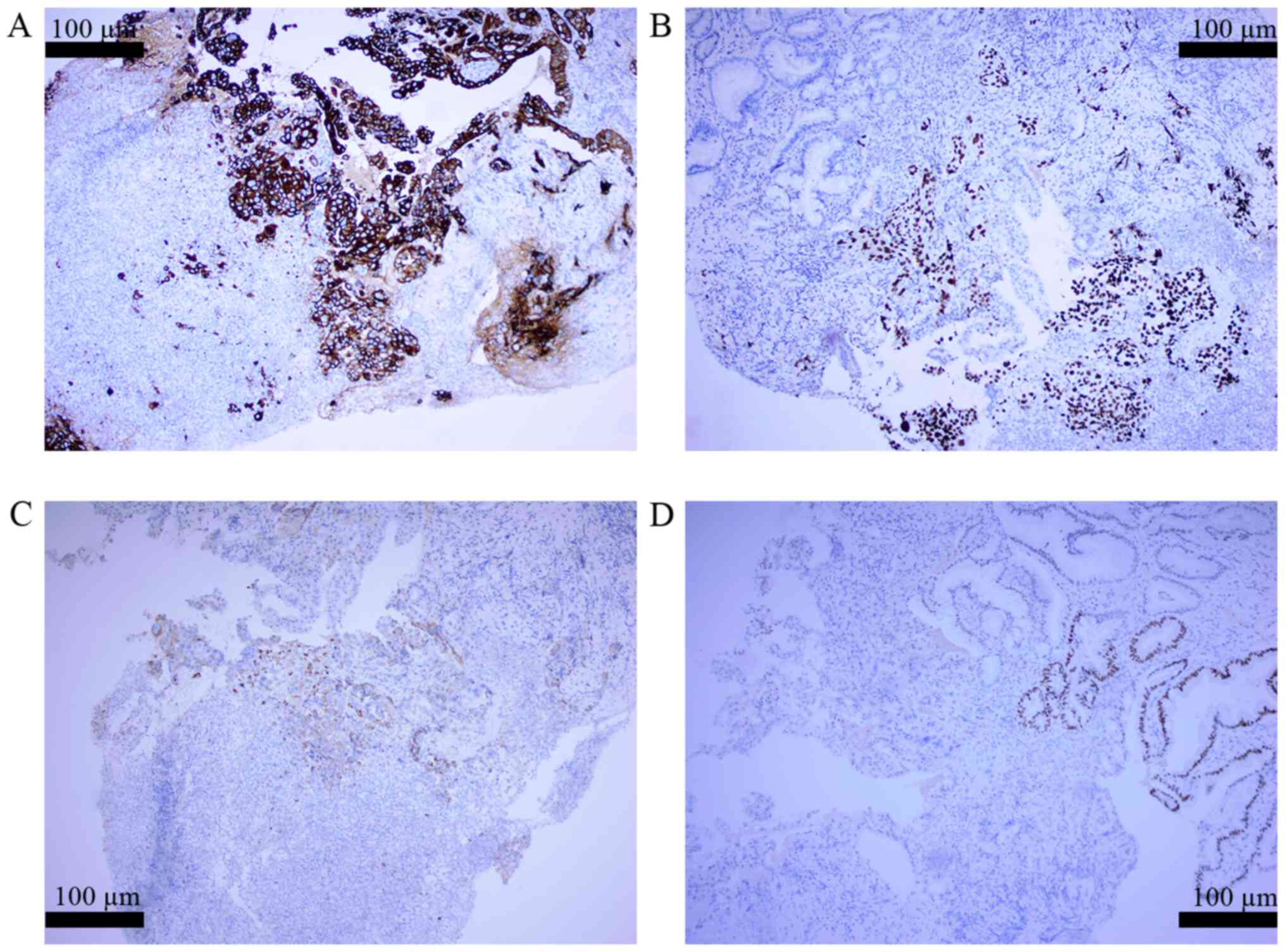
4). The results of the immunohistochemical staining of the
lesion illustrated that the tumor cells were positive for
cytokeratin-7, thyroid transcription factor-1 and napsin-A
expression, but negative for caudal-related homeobox 2 expression
(Fig. 5), which confirmed the
diagnosis of duodenal metastasis from a primary lung
adenocarcinoma. Therefore, the patient received targeted treatment
with anlotinib.
Two months later, the patient reported the
occurrence of hematochezia on three occasions, with 200 ml of blood
lost each time, prior to receiving the second cycle of the targeted
treatment in our hospital. In order to prevent gastrointestinal
bleeding, he underwent superior mesentery artery and coeliac artery
arteriography, and transcatheter gastroduodenal and left gastric
arterial embolization. However, the patient died of acute kidney
injury three days after the operation.
Immunohistochemical analysis was performed on 10%
neutral formalin-fixed with neutral resin mounting medium
specimens. Thickness of sections was 1 µm. Three percent UV
inhibitor (24 h in 37˚C; Roche Diagnostics) were used as the
blocking reagent. Cytokerin-7 (CK7; IR619; 32 min in 37˚C; Dako),
Thyroid transcription factor-1 (TTF-1; 790-4756; 32 min in 37˚C;
Roche Diagnostics), Napsin-A (CNM-0012; 32 min in 37˚C; Celnovte),
p53 (IR616; 32 min in 37˚C; Dako), and caudal-related homeobox 2
(CDX-2; IR080; 32 min in 37˚C; Dako) antibodies were used as the
primary antibodies. Ready-to-use antibodies (760-500; 4-12 min in
37˚C; Roche Diagnostics) were used as the secondary antibodies. For
staining, we used an automated stainer (Dako) according to the
manufacturer's protocol. ChemMate EnVision (Dako) methods were used
for detection and Olympus BX51 biological microscope
(magnification, x100 or x200) was used for observation.
Discussion
The gastrointestinal tract is considered a rare site
for the metastasis of primary lung cancer. According to clinical
statistics, the odds of metastasis is <2% (3). Although the small intestine was
described as the most common gastrointestinal metastatic site in
previous studies (4,8,9), the
proportion of the cases of primary lung cancer metastasizing to the
duodenum only accounts for 15.8% of small bowel metastases
(6). Usually, the gastrointestinal
metastasis of primary lung cancer is asymptomatic. Numerous
previous studies have reported that perforation is the most common
symptom of small bowel metastasis (5,6,9). In
reports where patients presented with symptoms, the most commonly
experienced symptoms were abdominal pain, melena and anemia, while
other symptoms included weight loss, jaundice and pyrosis, amongst
others (4,5,8,10,11).
Therefore, the symptoms that we discussed above have been suggested
to be associated with different organs and incubation times
(3,10).
In a retrospective study by Hu et al
(3), >3/4 of the incidences of
gastrointestinal metastases of lung cancer cases analyzed were
squamous cell carcinomas, adenocarcinomas and large cell
carcinomas. In a published series of 423 autopsies, in which 58
patients presented with gastrointestinal tract secondary lesions
from lung cancer, the most frequently encountered histological
types were squamous cell (33%), large cell (29%) and oat cell (19%)
(12). As squamous cell carcinoma
and adenocarcinoma are common types of primary lung cancer, the
conclusions drawn may have selection bias. Further studies are
required to estimate whether a strong association between the
histopathology and gastrointestinal tract metastases exists.
In previous studies, results from autopsies have
revealed that the rate of gastrointestinal metastases from lung
cancer was 4.7-14.0% (13-15),
which is notably higher compared with clinical statistics. The
reasons for these differences are as follows: Firstly, the majority
of patients who presented with gastrointestinal metastasis
following lung cancer had no specific signs and symptoms; secondly,
the gastrointestinal tract is not a typical metastatic site for
primary lung cancer, thus it is rarely considered as a priority
when the clinicians are making a differential diagnosis; thirdly,
even if patients present with gastrointestinal symptoms, it is very
likely that the symptoms will be mistaken to be due to the common
gastrointestinal disturbances experienced following chemotherapy
and other benign lesions, such as peptic ulcer and intestinal
polyposis; and finally, although laboratory examinations, CT and
MRI scans, and CT-PET can help to diagnose gastrointestinal
metastasis, there still remains the risk that these techniques will
miss the presence of the lesions. Histopathology and
immunohistochemistry are vital methods required for the diagnosis
(3,8).
The route by which lung cancer metastasizes to the
gastrointestinal tract is currently unknown, but both hematogenous
and lymphatic routes are considered to be involved (4,5,12). The
patient in the present case report had diabetes, which could block
the immunological surveillance of cancer cells and may cause
unusual metastases (16). However,
there are several limitations to this report. For example, when the
patient first complained of the abdominal pain, the endoscopy was
not immediately scheduled because his previous
esophagogastroduodenoscopy indicated that he had Barrett's
esophagus and duodenal ulcers with bleeding. In addition, there was
no evidence of gastrointestinal metastasis on the CT or PET/CT
scan. In fact, the initial diagnosis was a peptic ulcer. However,
the symptoms of the patient had not improved following the
treatment with omeprazole. Therefore, an endoscopy was performed
and specimens were obtained to perform pathological and
immunohistochemical examinations. The results confirmed the
diagnosis of duodenal metastasis from a primary lung
adenocarcinoma. It is worth mentioning that the laboratory findings
of anemia with hemoglobin levels of 103 g/l in April 2019 may be
crucial indicators. However, at the time, it was thought that these
results were due to a reduction in iron intake that caused iron
deficiency anemia, and the possibility of occult gastrointestinal
bleeding was ignored at the time. Therefore, upon encountering
patients who have primary lung cancer with gastrointestinal
symptoms or anemia, it is vital that doctors consider whether
gastrointestinal metastases may have occurred and perform further
examinations to confirm.
For the majority of patients who have
gastrointestinal metastasis with no particular symptoms, one must
determine the presence of metastatic lesions in other organs. In a
study by McNeill et al (14), it was reported that 46 patients with
small bowel metastases had ≥1 other metastatic site, with an
average of 4.8 sites. Yoshimoto et al (15) suggested that gastrointestinal
metastasis should be considered when patients had adrenal gland,
kidney and abdominal lymph node metastases. Therefore, further
investigations into the occurrence of gastrointestinal metastasis
following lung cancer must be appropriately investigated if distant
metastasis has occurred at other sites. It is of vital importance
to perform these appropriate examinations as soon as possible.
According to the research by Kim et al (17), 93% of patients with gastrointestinal
metastases from lung cancer had positive findings on the CT scan,
which included wall thickening, an intraluminal mass and a
protruding lump. PET/CT may also be helpful in diagnosing the
gastrointestinal metastasis of lung cancer (3). However, due to the high cost and
shortage of clinical cases, the necessity of using PET-CT for the
diagnosis of the gastrointestinal metastasis of lung cancer remains
controversial (5,6,11). For
example, certain patients who had confirmed gastrointestinal
metastases exhibited no signs on either the PET scan or through
endoscopy, and presented with possible mucosal edema, hyperemia,
multiple nodules with or without mucosal ulcerations, or even as a
single ‘volcano-like’ lesion imitating a primary gastrointestinal
tumor (8). Therefore,
histopathological and immunohistochemical examinations are
considered the only method to confirm whether the lung carcinoma
has metastasized to the gastrointestinal tract (3,8,10).
In conclusion, although the gastrointestinal tract
is a rare site of metastasis for primary lung cancer, on account of
the increasing incidence of primary lung cancer and the development
of medical technology for the diagnosis and treatment of the
disease, an increasing number of cases of gastrointestinal
metastases from lung cancer have been reported. Therefore,
clinicians should pay more attention to the infrequent metastatic
sites of primary lung cancer and consider the possibility of
gastrointestinal metastasis if digestive symptoms are experienced
or if other distant metastasis sites are present in patients who
have been diagnosed with lung cancer, so that the lesions can be
located to obtain a biopsy for histopathological and
immunohistochemical examinations in a timely manner.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during the current
study are included in this published article.
Authors' contributions
MZ, JS and XL collected the patient's data. LL and
QW analyzed the data and performed reference search. MZ, JS and XL
drafted the manuscript and revised it critically for important
intellectual content. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the
patient for publication of this case report and any accompanying
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Mao Y, Yang D, He J and Krasna MJ:
Epidemiology of lung cancer. Surg Oncol Clin N Am. 25:439–445.
2016.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Hoffman PC, Mauer AM and Vokes EE: Lung
cancer. Lancet. 355:479–485. 2000.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Hu Y, Feit N, Huang Y, Xu W, Zheng S and
Li X: Gastrointestinal metastasis of primary lung cancer: An
analysis of 366 cases. Oncol Lett. 15:9766–9776. 2018.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Taira N, Kawabata T, Gabe A, Furugen T,
Ichi T, Kushi K, Yohena T, Kawasaki H, Higuchi D, Chibana K, et al:
Analysis of gastrointestinal metastasis of primary lung cancer:
Clinical characteristics and prognosis. Oncol Lett. 14:2399–2404.
2017.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Yang CJ, Hwang JJ, Kang WY, Chong IW, Wang
TH, Sheu CC, Tsai JR and Huang MS: Gastro-intestinal metastasis of
primary lung carcinoma: Clinical presentations and outcome. Lung
Cancer. 54:319–323. 2006.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Liu W, Zhou W, Qi WL, Ma YD and Xu YY:
Gastrointestinal hemorrhage due to ileal metastasis from primary
lung cancer. World J Gastroenterol. 21:3435–3440. 2015.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Di JZ, Peng JY and Wang ZG: Prevalence,
clinicopathological characteristics, treatment, and prognosis of
intestinal metastasis of primary lung cancer: A comprehensive
review. Surg Oncol. 23:72–80. 2014.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Rossi G, Marchioni A, Romagnani E,
Bertolini F, Longo L, Cavazza A and Barbieri F: Primary lung cancer
presenting with gastrointestinal tract involvement:
Clinicopathologic and immunohistochemical features in a series of
18 consecutive cases. J Thorac Oncol. 2:115–120. 2007.PubMed/NCBI
|
|
9
|
Garwood RA, Sawyer MD, Ledesma EJ, Foley E
and Claridge JA: A case and review of bowel perforation secondary
to metastatic lung cancer. Am Surg. 71:110–116. 2005.PubMed/NCBI
|
|
10
|
AlSaeed EF, Tunio MA, AlSayari K, AlDandan
S and Riaz K: Duodenal metastasis from lung adenocarcinoma: A rare
cause of melena. Int J Surg Case Rep. 13:91–94. 2015.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Lo CK, Kao SS, Tai KC, Ma CC, Ho KK, Ko KM
and Cheung MT: Gastrointestinal metastasis from primary lung
cancer. Surgical Practice. 13:73–76. 2010.
|
|
12
|
Misiakos EP, Gouloumi AR, Schizas D,
Damaskou V, Tsapralis D, Farrugia FA, Machairas N, Papaconstantinou
D, Tzaneti A and Machairas A: Small bowel perforation with multiple
intestinal metastases from lung carcinoma: A case report. Oncol
Lett. 17:3862–3866. 2019.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Antler AS, Ough Y, Pitchumoni CS, Davidian
M and Thelmo W: Gastrointestinal metastases from malignant tumors
of the lung. Cancer. 49:170–172. 1982.PubMed/NCBI View Article : Google Scholar
|
|
14
|
McNeill PM, Wagman LD and Neifeld JP:
Small bowel metastases from primary carcinoma of the lung. Cancer.
59:1486–1489. 1987.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Yoshimoto A, Kasahara K and Kawashima A:
Gastrointestinal metastases from primary lung cancer. Eur J Cancer.
42:3157–3160. 2006.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Jeba J, Backianathan S, Ishitha G and
Singh A: Oral and gastrointestinal symptomatic metastases as
initial presentation of lung cancer. BMJ Case Rep.
2016(bcr2016217539)2016.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Kim SY, Ha HK, Park SW, Kang J, Kim KW,
Lee SS, Park SH and Kim AY: Gastrointestinal metastasis from
primary lung cancer: CT findings and clinicopathologic features.
AJR Am J Roentgenol. 193:W197–W201. 2009.PubMed/NCBI View Article : Google Scholar
|