Introduction
Preoperative chemoradiotherapy (CRT) has been widely
accepted as a standard therapy for advanced lower rectal cancer and
previous studies have shown that it contributed to tumor
down-staging and decreased postoperative locoregional recurrence
(1-3).
Notably, each patient showed significantly different responses to
CRT, with some cases showing little or no response (4,5).
Therefore, identification of predictive factors for CRT response
would be beneficial for selecting measures of treatment to avoid
adverse events, such as radiation dermatitis, hematologic toxicity,
and enteritis, which may be associated with CRT (1-3).
Previous studies have suggested that the host immune
system might play an important role in the eradication of the tumor
using preoperative CRT and that some immunological markers might
predict the tumor response to CRT (6,7).
Shinto et al (8) reported
positive and negative associations between CRT response and the
density of intraepithelial infiltration of CD8+ T cells
and forkhead box P3 (FoxP3)+ regulatory T cells,
respectively. Some studies have also reported the association
between FoxP3+, CD4+, and CD8+
tumor-infiltrating lymphocytes (TILs) and CRT response in rectal
cancer (9-12).
Lactadherin (MFG-E8) is a secreted glycoprotein with
pleiotropic functions, including enhancement of phagocytosis of
apoptotic cells by macrophages, anti-inflammatory effects, and
VEGF-dependent angiogenesis (13-15).
MFG-E8-knockout mice were reported to develop autoimmune and
inflammatory diseases, due to the accumulation of dead cells
(16). Furthermore, it plays an
important role in the regulation of cancer immunity of the host and
enhances tumorigenicity (16).
Jinushi et al (17) reported
that MFG-E8 promoted phagocytosis of apoptotic cells by macrophages
and induced immune tolerance by the secretion of regulatory T
cells, inducing cytokines. This phenomenon has been observed in
some human tumors, such as cancer of the ovary, bladder, and
prostate; malignant melanoma; and colorectal cancer (18-22).
Notably, MFG-E8 expression has been reported to be a poor
prognostic factor in malignant melanoma (21). Kusunoki et al (23) reported that MFG-E8 promoted tumor
growth in a mouse model of colon cancer, and that MFG-E8 expression
in advanced colorectal cancer was higher compared with that in
adenoma or early colorectal cancer. Furthermore, Zhao et al
(22) revealed that MFG-E8
expression in patients with colorectal cancer who were not treated
with preoperative therapy was associated with lymph node
metastasis, distant metastasis, and poor cancer-specific survival.
However, the significance of MFG-E8 expression in patients with
rectal cancer treated with preoperative CRT has not been clarified
so far. Therefore, CD8+, FoxP3+ TILs, and
MFG-E8 expression level in patients with rectal cancer and treated
with preoperative CRT was investigated, and the association between
their expression levels and clinicopathological features, response
to CRT, and patient prognosis was also analyzed.
Materials and methods
Patients and specimens
A total of 61 patients, who underwent curative
resection following CRT for T3-T4 lower rectal cancer at the
Department of Surgical Oncology, University of Tokyo (Tokyo, Japan)
between March 2001 and October 2009 were retrospectively analyzed.
Written informed consent was obtained from all the patients. Tumor
depth, nodal status, and presence of distant metastases were
determined using colonoscopy, computed tomography, and magnetic
resonance imaging.
The patients received a total radiation dose of 50.4
Gy (1.8 Gy in 28 fractions) and concomitant chemotherapy (oral
administration of tegafur-uracil, 300 mg/m2/day and
leucovorin, 75 mg/day for 28 days from the beginning to the end of
irradiation). Total mesorectal excision, with lymph node
dissection, was performed following an interval of 6-8 weeks
post-CRT. All patients underwent regular follow-up examinations
following surgery. Tumor markers were examined every 3 months, and
abdominal and chest computed tomography was performed every 6
months. Total colonoscopy was performed annually.
All specimens were fixed in 10% formalin at room
temperature for 24 h and embedded in paraffin. The
histopathological findings were confirmed by several pathologists
affiliated to the Department of Pathology, University of Tokyo
(Tokyo, Japan), who were blinded to the samples. Data was collected
from the patients' medical records, which were prospectively
generated. The TNM classification was determined according to the
Union for International Cancer Control, 9th edition (24). The post-CRT histological tumor
regression grade was evaluated according to the Japanese
Classification of Colorectal Carcinoma, 9th edition (Grade 0, no
necrosis or regressive change; 1, >33.3% vital residual tumor
cells; 2, <33.3% vital residual tumor cells; and 3, no vital
residual tumor cells) (25). In the
analysis of CD8 and FoxP3, specimens were evaluated before CRT. For
MFG-E8 expression level, specimens were evaluated after CRT.
Furthermore, in the analysis of MFG-E8, 5 cases with no residual
cancer cells after preoperative CRT (Grade 3) were excluded.
The present study was approved by the Ethics
Committee of the University of Tokyo on July 29, 2014 [approval no.
10476-(1)] and written informed
consent was obtained from all the patients.
CD8, FoxP3, and MFG-E8
immunohistochemical staining
The tumor specimens were cut into 4-µm thick
sections and immunohistochemically stained, as previously described
(9). Primary anti-CD8 (cat. no.
4B11; dilution 1:50; Leica Biosystems) and anti-FoxP3 (cat. no.
236/E7; dilution 1:100; Abcam) mouse monoclonal antibodies, and the
anti-MFG-E8 antibody [cat. no. 14A-11B; dilution 1:120; supplied by
The Institute of Medical Science, University of Tokyo, (Tokyo,
Japan)] were utilized (26). Normal
tonsil tissue was used as the positive control for CD8, FoxP3, and
normal breast tissue was used as the positive control for MFG-E8,
and obtained from autopsy specimens, which were donated to the
Division of Surgical Oncology, University of Tokyo for research
purposes, and written informed consent was provided.
Evaluation of CD8, FoxP3, and MFG-E8
immunostaining
The number of immunoreactive lymphocytes was counted
under a light microscope in three randomly selected fields, at x400
magnification, as previously described (9). Immunoreactive TIL densities and the
median values of all samples were set as thresholds. Each sample
was classified as ‘high’ if it was above the median and ‘low’ if it
was below.
MFG-E8 expression was assigned scores according to
the highest staining intensity, as described previously (26). The criteria for the scoring were as
follows: 0, Negative staining or trace; 1, moderate; and 2, strong.
Based on the scores, all sections were divided into two groups:
High expression (a score of 2) or low expression (a score of 0 and
1). Analysis was performed by 2 observers independently, in a
blinded manner, and interobserver agreement was confirmed using
κ-statistics. Any discrepancies were resolved by discussion. The
association of their expression level with CRT response,
clinicopathological features and patient prognosis was subsequently
analyzed.
Statistical analysis
The association between the density of TILs and CRT
response was evaluated using a Wilcoxon signed rank test, while the
association between MFG-E8 expression level and clinicopathological
features was evaluated using a χ2, Fisher's exact, or
unpaired t-tests, as appropriate. Overall survival (OS; defined as
the time from surgery to death from any cause) and disease-free
survival (DFS; defined as the time from surgery to cancer
recurrence, secondary cancer, or death from any cause), were
analyzed using the Kaplan-Meier method and log-rank test.
Multivariate analysis was performed using Cox proportional hazards
regression analysis. Interobserver agreement was confirmed using
κ-statistics. P<0.05 was considered to indicate a statistically
significant difference. All analyses were performed using JMP v11.0
software (SAS Institute Inc.).
Results
Clinicopathological analysis
The clinicopathological features of the patients are
shown in Table I. The median age
was 61.4 years (range, 33-78 years) and 39 patients (63.9%) were
male. After preoperative CRT, 35 (57.4%) patients had T3-4 tumors.
A total of 44 patients (72.1%) showed papillary carcinoma or
well-differentiated adenocarcinoma histology, while 9 (14.8%) and 7
(11.5%) patients had lymph node and distant metastases (3 to the
liver, 2 to the lung, 1 to the brain, and 1 paraaortic lymph node
metastases), respectively. Based on the response to CRT
classification, 35 (57.4%), 21 (34.4%), and 5 (8.2%) patients were
categorized as Grades 1, 2 and 3. The median follow-up period was
5.8 years (range, 0.8-10.9 years).
 | Table ICharacteristics of the patients with
rectal cancer. |
Table I
Characteristics of the patients with
rectal cancer.
|
Characteristics | Value |
|---|
| Sex, n (%) | |
|
Male | 39 (63.9) |
|
Female | 22 (36.1) |
| Mean age ± SD,
years | 61.4±9.6 |
| pT
stagea, n (%) | |
|
T0-2 | 26 (42.6) |
|
T3-4 | 35 (57.4) |
| Histological type,
n (%) | |
|
Well | 44 (72.1) |
|
Mod | 16 (26.2) |
|
Muc | 1 (1.6) |
| Lymphatic invasion,
n (%) | |
|
Present | 5 (8.2) |
|
Abscent | 56 (91.8) |
| Vascular
invasion | |
|
Present | 31 (50.8) |
|
Abscent | 30 (49.1) |
| Lymph node
metastasis, n (%) | |
|
Present | 9 (14.8) |
|
Abscnet | 52 (85.2) |
| Distant metastasis,
n (%) | |
|
Present | 7 (11.5) |
|
Abscent | 54 (88.5) |
| TNM
stagea, n (%) | |
|
0-II | 49 (80.3) |
|
III-IV | 12 (19.7) |
| Tumor regression
gradeb, (%) | |
|
1 | 35 (57.4) |
|
2 | 21 (34.4) |
|
3 | 5 (8.2) |
CD8, FoxP3 and MFG-E8 expression
level
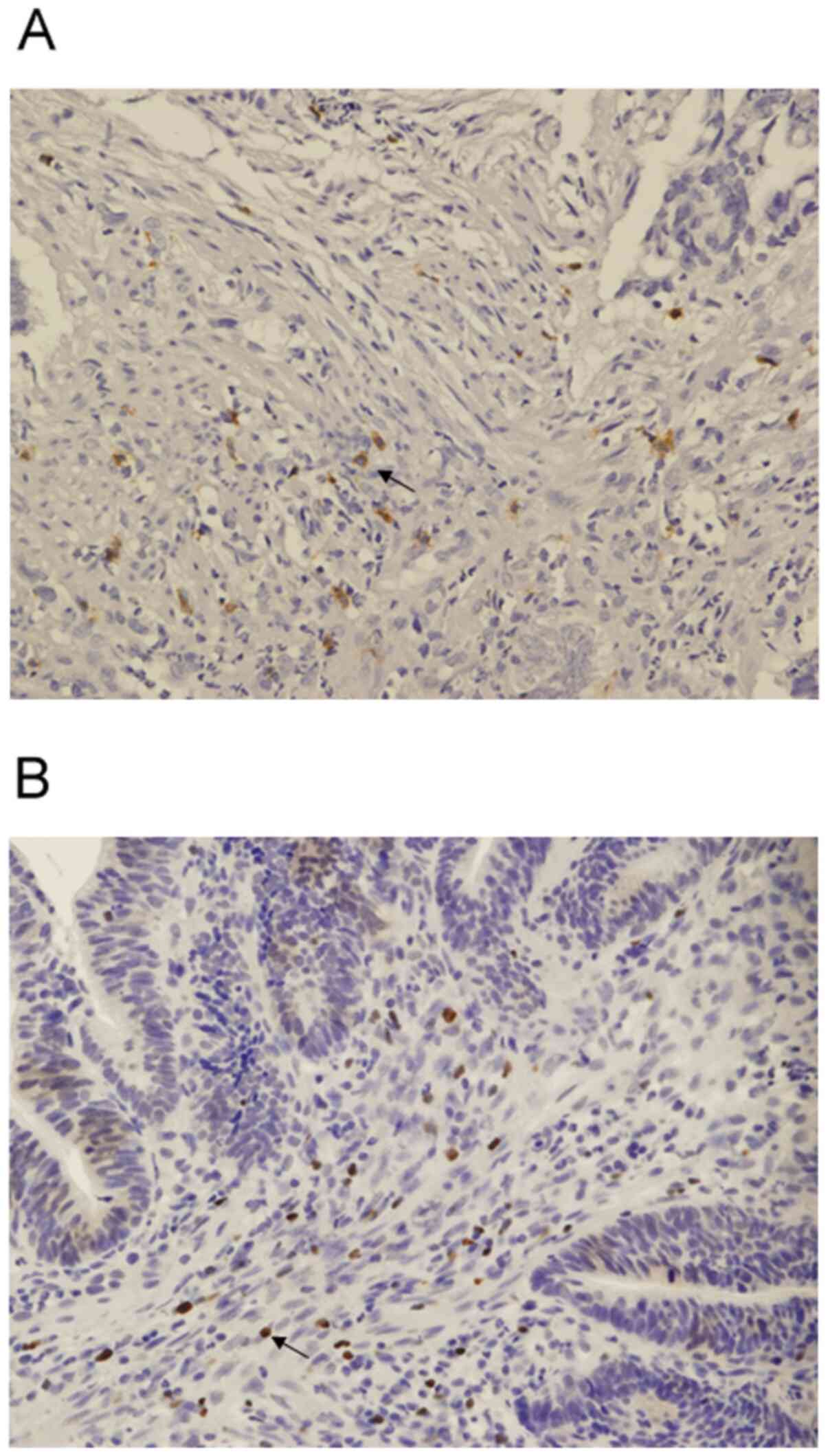
CD8 expression was detected in the cell membrane,
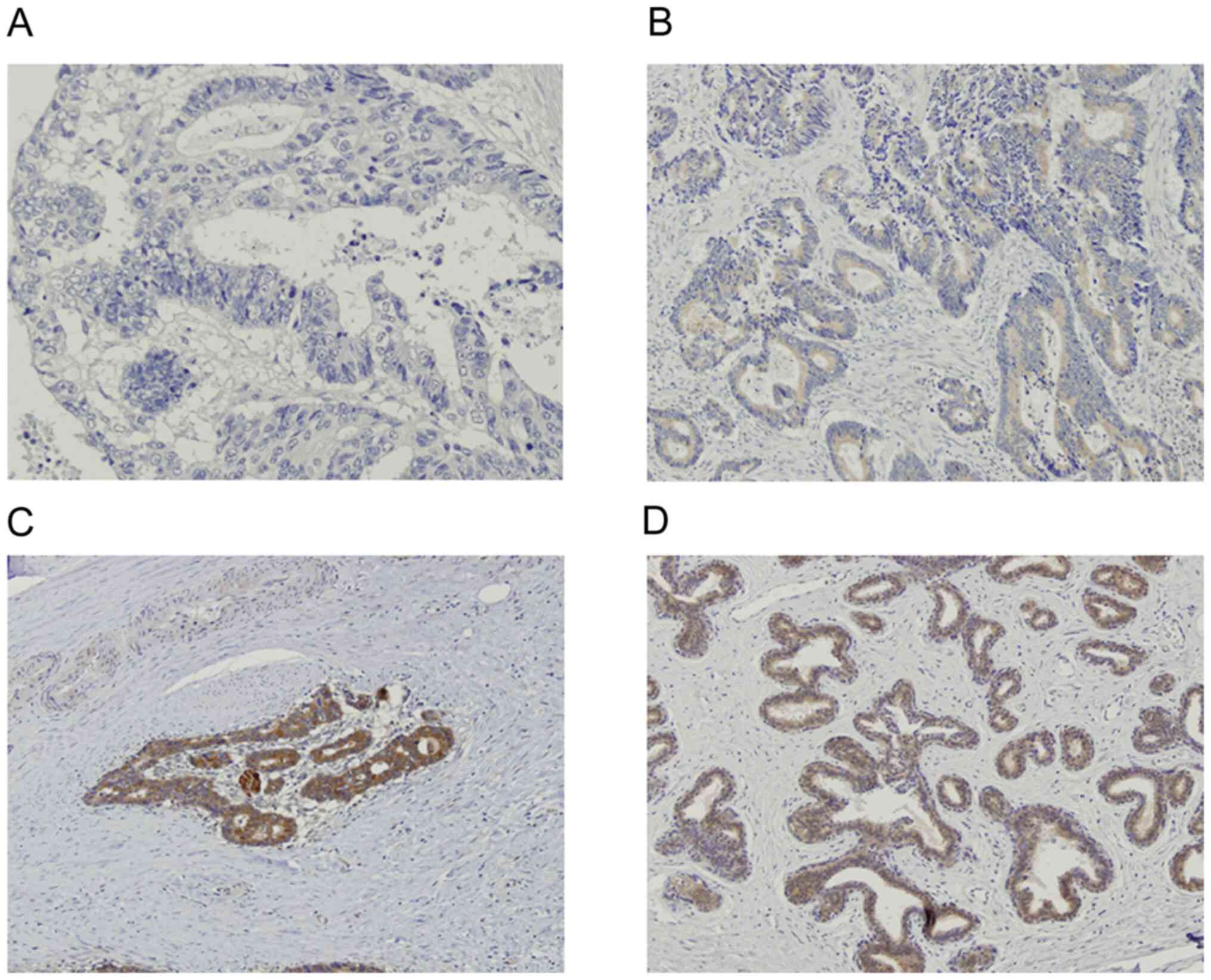
while FoxP3 was detected in the nucleus (Fig. 1A and B, respectively). MFG-E8 expression level
was detected in the cytoplasm of normal breast tissue, which was
used as the positive control (Fig.
2A). MFG-E8 expression was also detected in the cytoplasm of
rectal cancer tissue (Fig. 2B-D).
Based on the immunohistochemistry scoring, 23 (41.1%) patients were
categorized as MFG-E8 high.
Association between CD8+
and FoxP3+ TILs, and CRT response
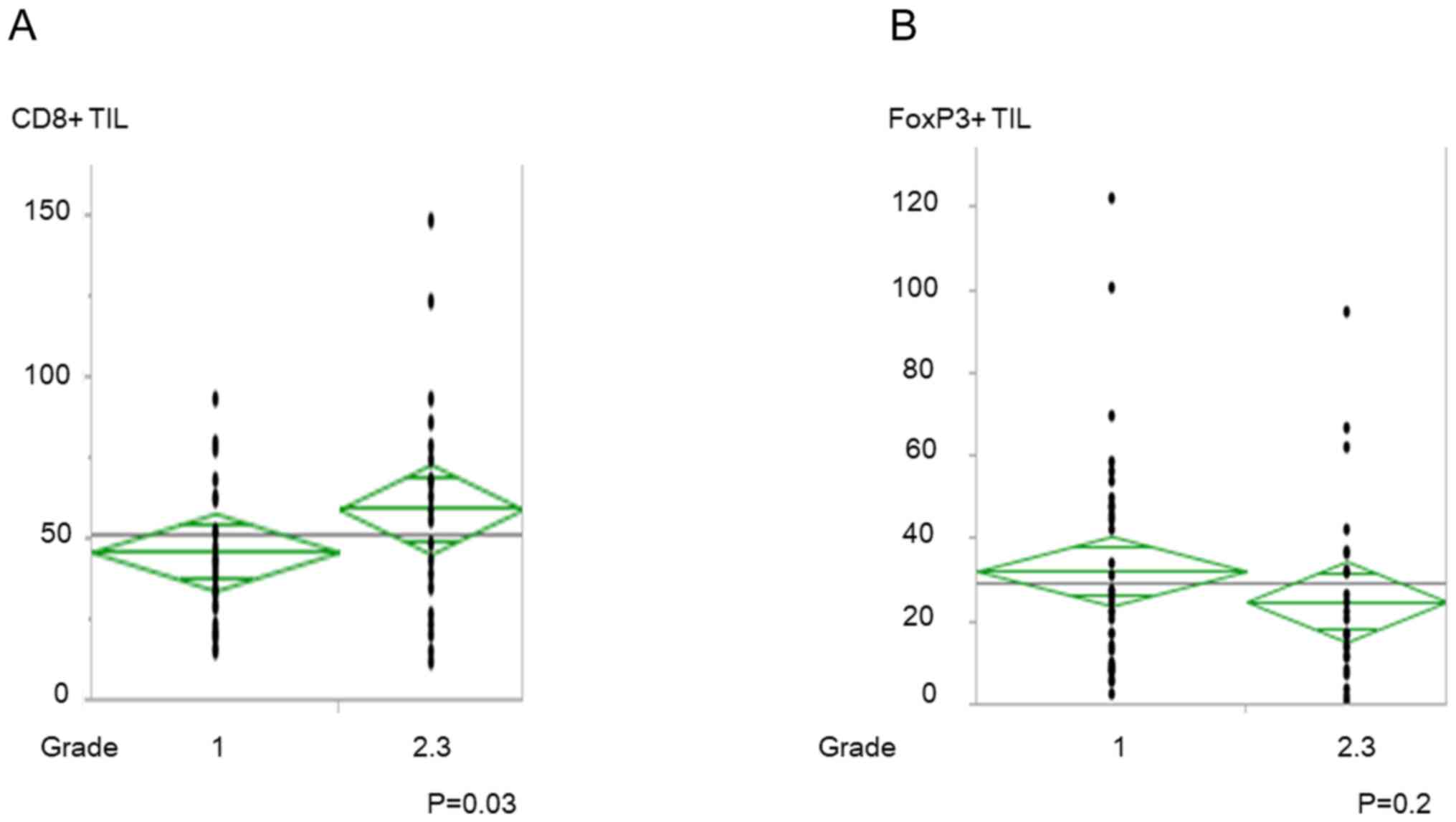
The increased number of CD8+ TILs before
CRT was significantly associated with good CRT response (P=0.03;
Fig. 3A); however, there was no
significant association with FoxP3+ TILs (Fig. 3B). CD8/FoxP3+ TIL ratio
was also associated with good CRT response (P=0.04; data not
shown).
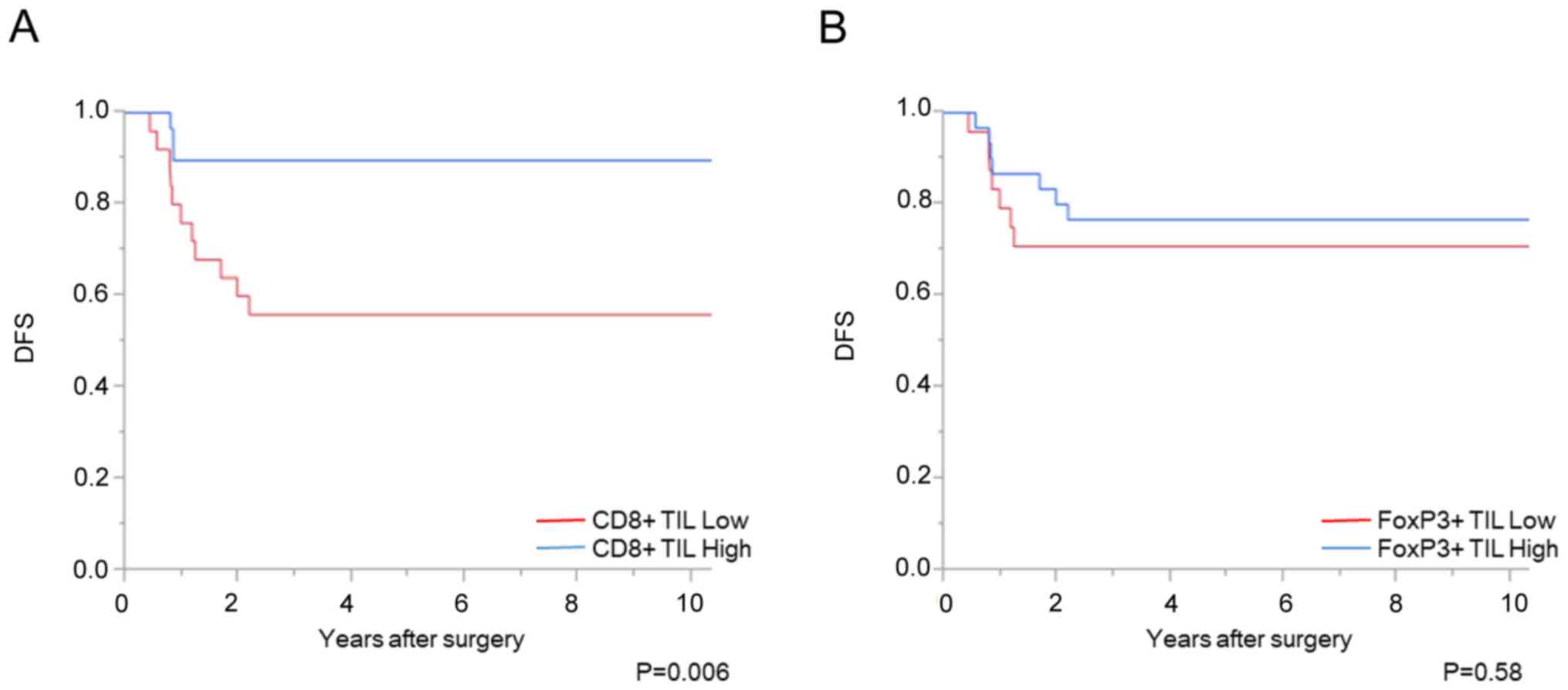
Association between CD8+
and FoxP3+ TILs, and patient prognosis
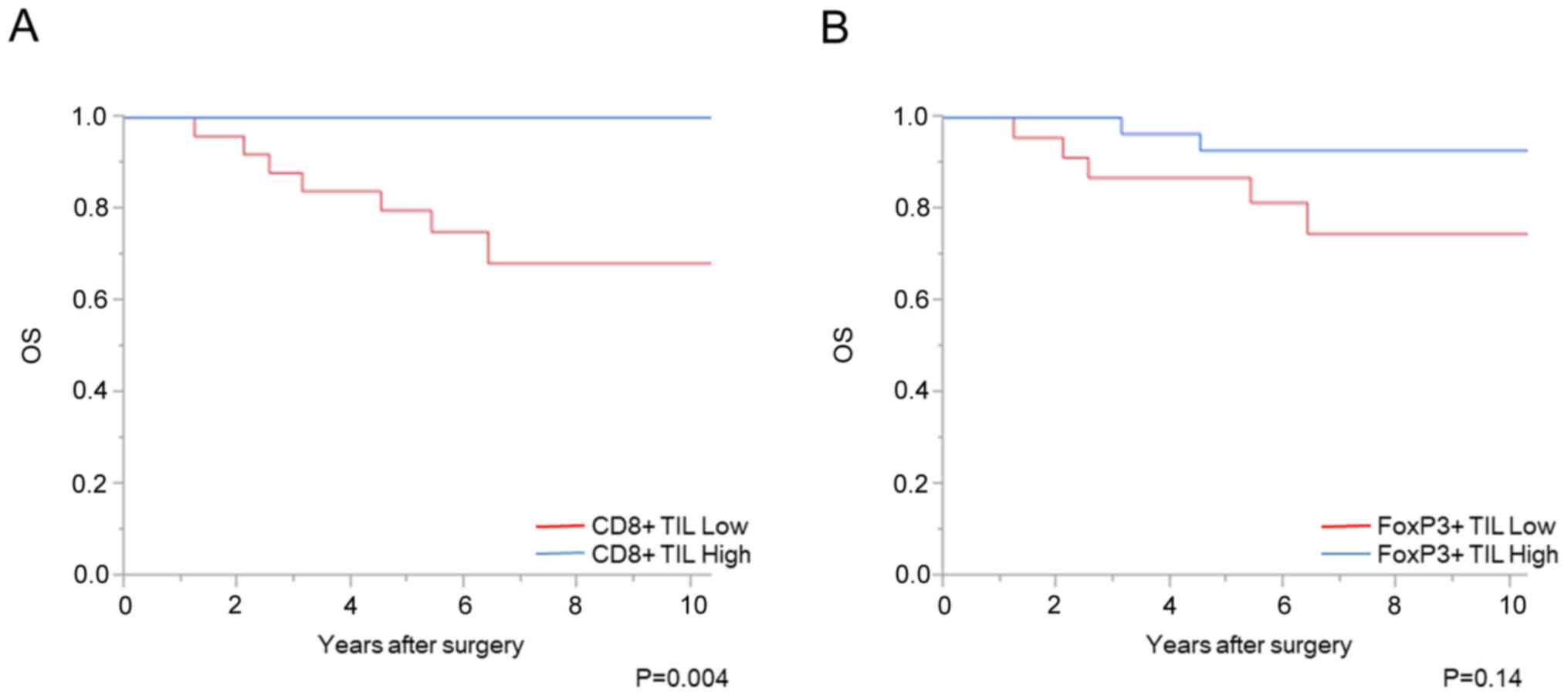
A total of 7 cases with distant metastasis were
excluded from the prognostic analysis. The increased number of
CD8+ TILs before CRT was significantly associated with
favorable OS and DFS times (P<0.01 and P<0.01, respectively);
however, there was no significant association with the number of
FoxP3+ TILs (Figs. 4 and
5). Univariate analysis showed that
the density of CD8+ TIL before CRT, vascular invasion
and pathological T stage was associated with DFS time (P<0.01,
P=0.04, and P<0.01, respectively). Using a multivariate
analysis, the density of CD8+ TIL before CRT, in
addition to pathological T stage, was independently associated with
DFS time (Table II). With respect
to OS time, univariate analysis showed that the density of
CD8+ TIL before CRT and pathological T stage was
associated with OS time (P<0.01 and P<0.01, respectively). In
addition, multivariate analysis showed that the density of
CD8+ TIL before CRT was independently associated with OS
time (P=0.01), although 7 patients died.
 | Table IIUnivariate and multivariate analysis
between disease free survival and clinicopathological
characteristics. |
Table II
Univariate and multivariate analysis
between disease free survival and clinicopathological
characteristics.
| | Univariate | Multivariate |
|---|
|
Charactertistic | HR | 95% CI | P-value | HR | 95% CI | P-value |
|---|
| pT stage (T3-4 vs.
T0-2) | 6.5 | 1.8-41.8 | <0.01 | 4.2 | 1.02-28.68 | 0.046 |
| Lymphatic invasion
(present vs. absent) | 4.3 | 0.23-22.1 | 0.25 | | | |
| Vascular invasion
(present vs. absent) | 3.2 | 1.08-11.84 | 0.04 | 1.6 | 0.50-6.27 | 0.45 |
| Lymph node
metastasis (present vs. absent) | 2 | 0.45-6.31 | 0.33 | | | |
| CD8+ TIL
(high vs. low) | 0.2 | 0.04-0.64 | <0.01 | 0.3 | 0.06-0.94 | 0.038 |
| FoxP3+
TIL (high vs. low) | 0.74 | 0.25-2.17 | 0.58 | | | |
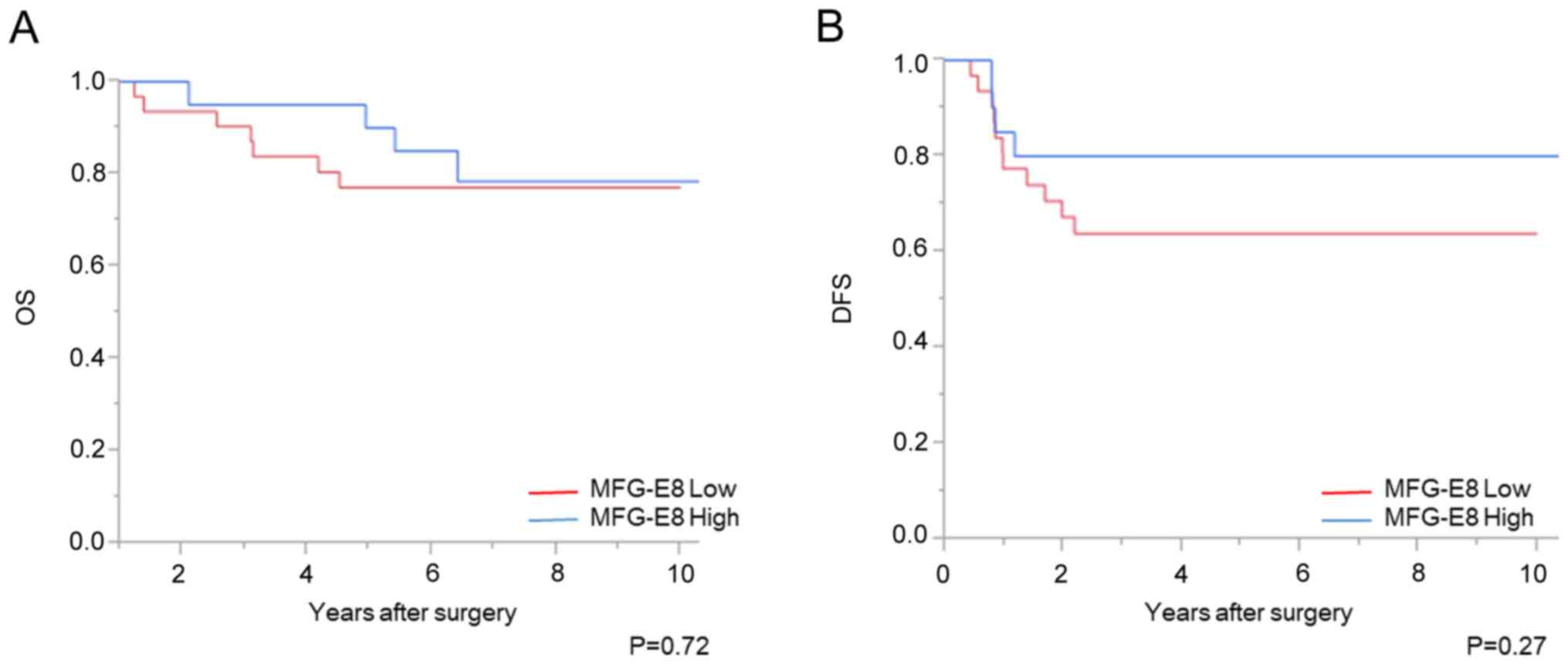
Association between MFG-E8 expression
level and clinicopathological features
High MFG-E8 expression after CRT was significantly
associated with high tumor regression grade (P<0.01; Table III). However, no significant
difference with OS or DFS time was found between the patient groups
with high and low MFG-E8 expression level (Fig. 6).
 | Table IIIAssociation between MFG-E8 expression
level and clinicopathological characteristics. |
Table III
Association between MFG-E8 expression
level and clinicopathological characteristics.
| | MFG-E8+
(n=23) | MFG-E8- (n=33) | |
|---|
| Characteristic | Number | Percentage | Number | Percentage | P-value |
|---|
| Sex | | | | | |
|
Male | 13 | 56.5 | 25 | 75.8 | 0.21 |
|
Female | 10 | 43.5 | 8 | 24.2 | |
| Mean age ± SD,
years | 59.6±10.4 | 63.4±8.7 | 0.16 |
| pT
stagea | | | | | |
|
T0-2 | 8 | 34.8 | 13 | 39.4 | 0.73 |
|
T3-4 | 15 | 65.2 | 20 | 60.6 | |
| Histological
type | | | | | |
|
Well | 18 | 78.3 | 21 | 63.6 | 0.24 |
|
Mod | 5 | 21.7 | 11 | 33.3 | |
|
Muc | 0 | 0 | 1 | 3.1 | |
| Lymphatic
invasion | | | | | |
|
Present | 1 | 4.3 | 4 | 12.1 | 0.30 |
|
Abscent | 22 | 95.7 | 29 | 87.9 | |
| Vascular
invasion | | | | | |
|
Present | 11 | 47.8 | 20 | 60.6 | 0.34 |
|
Abscent | 12 | 52.2 | 13 | 39.4 | |
| Lymph node
metastasis | | | | | |
|
Present | 3 | 13.0 | 6 | 18.2 | 0.60 |
|
Abscent | 20 | 87.0 | 27 | 81.8 | |
| Distant
metastasis | | | | | |
|
Present | 3 | 13.0 | 3 | 9.1 | 0.37 |
|
Abscent | 20 | 87.0 | 30 | 90.9 | |
| TNM
stagea | | | | | |
|
I-II | 18 | 78.3 | 26 | 78.8 | 0.96 |
|
III-IV | 5 | 21.7 | 7 | 21.2 | |
| Tumor regression
gradeb | | | | | |
|
1 | 9 | 39.1 | 26 | 78.8 | <0.01 |
|
2 | 14 | 60.9 | 7 | 21.2 | |
Discussion
Preoperative CRT for advanced lower rectal cancer
decreased post-operative locoregional recurrence and contributed to
tumor down-staging, which lead to an increased
sphincter-preservation rate (27).
Furthermore, previous reports described the usefulness of the
‘watch and wait’ strategy or local excision after CRT (28,29).
Therefore, the identification of predictive factors for CRT
response is important to determine whether preoperative CRT should
be performed.
Firstly, using biopsy samples before CRT, the
association between TIL infiltration density, MFG-E8 expression
level, and CRT response was investigated. Teng et al
(11) and Anitei et al
(12) demonstrated that patients
with high CD8+ TIL density showed favorable CRT
responses. FoxP3+ TILs suppressed the host immune
system, contrary to cytotoxic CD8+ TILs. Therefore, we
hypothesized that both CD8+ and FoxP3+ TIL
densities could be valuable indicators. Shinto et al
(8) reported the effectiveness of
intraepithelial CD8/FoxP3 TILs ratio in patients with short-term
preoperative CRT regimen (20 Gy administered in 5 daily doses of 4
Gy, with the administration of tegafur/uracil at 400 mg/day and
surgery was performed ~30 days after CRT). However, their results
may not be applicable to long-term preoperative CRT, with a higher
radiation dose and a longer period before surgery [50.4 Gy (1.8 Gy
in 28 fractions) with concomitant chemotherapy and surgery was
performed 6-8 weeks after CRT]. Therefore, the association between
TIL density and CRT response using long-term preoperative CRT
samples was determined in the present study. CD8+ TIL
density, but not FoxP3+ TIL density, was associated with
CRT response. The association between the CD8/FoxP3 TIL ratio and
CRT response was determined; however, it was not a more effective
indicator than CD8+ TIL density alone. Thus, we
hypothesized that FoxP3+ TILs may not play an important
role in long-term preoperative CRT. Furthermore, McCoy et al
(30) recently reported that there
was no association between TIL density before CRT, including
CD8+ and FoxP3+ TIL densities, and CRT
response. A further study, with a larger sample size, would,
therefore, be required to validate the results from the present
study. It was difficult to determine the grade of MFG-E8 expression
level using small biopsy samples obtained before CRT and surgery,
which showed heterogenous expression patterns. Therefore, further
study using other methodology, such as PCR will also be
required.
Secondly, using surgically resected specimens after
CRT, immunology-related responses on the tumor microenvironment
were analyzed. With respect to TlLs, a considerable number of TILs
were detected in normal tissue in post-CRT specimens, and the
distribution of TILs varied as a result of prominent fibrosis
caused by CRT. Therefore, accurate TIL density after CRT was
difficult to evaluate. Shinto et al (8) evaluated TILs in specimens after
short-term CRT; however, we hypothesized that the different total
radiation dose and time between CRT and surgery resulted in
different results in the present study. High MFG-E8 expression
level in post-CRT specimens was significantly associated with a
favorable CRT response; however, no significant difference in
patient prognosis was observed. In previous trials (1-3),
preoperative CRT decreased postoperative locoregional recurrence,
although CRT did not improve the survival time in the patients. In
the present study, MFG-E8 expression level was associated with high
tumor regression grade, although no significant difference with OS
was found, which was consistent with previous reports (1-3).
With respect to DFS, we hypothesized that MFG-E8 expression might
be associated with high tumor regression grade and DFS, however no
significance differences were observed, which may be due to small
sample size. Jinushi et al (31) reported MFG-E8 induced resistance to
chemotherapy and irradiation in melanoma cells from the secretion
of regulatory T cells, inducing cytokines, and MFG-E8 induced
resistance to chemotherapy in melanoma cells through Akt.
Therefore, we hypothesized that MFG-E8 could be associated with
resistance to CRT in rectal cancer. Surprisingly, high MFG-E8
expression level in post-CRT specimens was significantly associated
with favorable CRT response. This type of association was not found
in the recent study on esophageal cancer (26). In the present study, it could not be
determined whether MFG-E8 expression level after CRT reflected the
MFG-E8 expression in samples before CRT or it was induced by CRT.
The association between MFG-E8 expression level and TIL density was
also not evaluated; however, high MFG-E8 expression level in
esophageal squamous cell carcinoma was associated with a low
CD8+/FoxP3+ TILs ratio (26). We hypothesized that this may be due
to the local microenvironment of the type of cancer. In esophageal
cancer, lipopolysaccharide, a component of gram-negative bacterial
cell walls, participates in the oncogenic process.
Lipopolysaccharide has been reported to activate the nuclear
factor-κ B signaling pathway, and to promote the release of
inflammation-associated mediators, including interleukin (IL) 1β,
IL6, IL8 and tumor necrosis factor-α (32,33).
However, the gut microbiome in the colon is a complex community in
the human body, and microbiota metabolites have either tumorigenic
or anti-tumorigenic effects. Lipopolysaccharide has also been
reported to be associated with tumorigenesis in colorectal cancer
(34), and Ladoire et al
(35) previously described that
numerous bacterial species produce proinflammatory cytokines, which
led to carcinogenesis. They also demonstrated that by suppressing
inflammation, FoxP3+ TILs could be anti-tumorigenic in
colorectal cancer. Furthermore, microbes in colorectal cancer have
been reported to induce epithelial-to-mesenchymal transition though
various signaling pathways, such as TGFβ, Wnt and Notch (34). On the other hand, butyric acid and
urolithins, which are also generated from colonic bacteria have
been reported to be anti-tumorigenic by inhibiting the Wnt
signaling pathway (36,37). The association between MFG-E8
expression level and TILs density could not be investigated;
however, Jinushi et al (17,38)
reported that MFG-E8 enhanced regulatory T cell activity. Thus, it
may be possible that MFG-E8 expression level in patients with
rectal cancer affects regulatory T cell activity and CRT
response.
With respect to the prognosis of patients, several
meta-analyses investigating patients with colorectal cancer and who
did not receive preoperative therapy revealed that the density of
CD8+ and FoxP3+ TILs was associated with
favorable patient prognosis (39).
Whereas, in patients with rectal cancer who received CRT, the
impact of TILs on patient prognosis has not been fully elucidated.
Teng et al (11) reported
that pre-CRT CD8+ TIL density was associated with
favorable patient prognosis, which is similar to the result in the
present study. Shinto et al (8) reported that high post-CRT
CD8+ TIL density, and not pre-CRT CD8+ TIL
density, was associated with favorable patient prognosis. However,
in the study by Shinto et al (8), the patients received a short course of
CRT, and immunological response on tumor microenvironment could be
different between their study and the present study. McCoy et
al (10,30) evaluated FoxP3+ TIL
density in pre- and post-CRT samples and reported that post-CRT
FoxP3+ TIL density, but not pre-CRT FoxP3+
TIL density, was associated with worsening prognosis. However, TILs
in the post-CRT samples were not investigated in the present study
as aforementioned. Therefore, further studies investigating TIL
density after CRT are warranted. With respect to MFG-E8, Zhao et
al (22) recently reported that
MFG-E8 expression level in colorectal cancer was associated with
advanced tumor depth, lymph node metastasis, and poor patient
survival. However, there was no significant association between
MFG-E8 expression level, clinicopathological features, and patient
prognosis. To the best of our knowledge, this is the first report
evaluating MFG-E8 expression level in patients with lower rectal
cancer treated with preoperative CRT, and MFG-E8 expression level
could be affected by CRT. Therefore, the results from the study by
Zhao et al (22) may not be
applicable to rectal cancer cases with CRT, and further study is
required.
The present study has several limitations. Firstly,
TIL density was evaluated using pre-CRT samples, whereas MFG-E8
expression level was evaluated using post-CRT samples. Therefore,
the association between MFG-E8 expression level and T cell immunity
was not clarified. Secondly, this was a retrospective study with a
relatively small number of patients. Therefore, prospective
studies, with a larger number of patients are required.
In conclusion, the results from the present study
suggest that the number of CD8+ TILs before CRT could be
a valuable predictor for CRT response, and high CD8+ TIL
density before CRT was associated with favorable prognosis in
patients with lower rectal cancer who were treated with CRT. High
MFG-E8 expression level after CRT was found to be associated with a
favorable CRT response.
Acknowledgements
Not applicable.
Funding
This research was supported by Grants-in-Aid for Scientific
Research (A: Grant no. 16H02672, C: Grant nos. 16K07143, 16K07161,
17K10620, 10621 and 17K10623) from the Japan Society for the
Promotion of Science and by the Project for Cancer Research and
Therapeutic Evolution (grant no. 16cm0106502h0001) from the Japan
Agency for Medical Research and Development.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author upon reasonable
request.
Authors' contributions
YH performed the experiment and wrote the
manuscript. SK evaluated IHC scoring and offered advice for IHC
analyses. TM evaluated IHC scoring. HS, HI, SE, KM, MK, KS, YS, TN,
TT, KK, KH and HN involved in acquiring clinicopathological
features of patients. TU offered advice for the evaluation of IHC
scoring. HT and SI were responsible for the study design and the
revised manuscript. All authors revised the manuscript and approved
the final version. YH and SI confirm the authenticity of all the
raw data.
Ethics approval and consent to
participate
This study was approved by the Ethics Committee of
the University of Tokyo on July 29, 2014 [approval no.
10476-(1)] and written informed
consent was provided by all the patients.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Folkesson J, Birgisson H, Pahlman L,
Cedermark B, Glimelius B and Gunnarsson U: Swedish rectal cancer
trial: Long lasting benefits from radiotherapy on survival and
local recurrence rate. J Clin Oncol. 23:5644–5650. 2005.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Peeters KC, Marijnen CA, Nagtegaal ID,
Kranenbarg EK, Putter H, Wiggers T, Rutten H, Pahlman L, Glimelius
B, Leer JW, et al: The TME trial after a median follow-up of 6
years: Increased local control but no survival benefit in
irradiated patients with resectable rectal carcinoma. Ann Surg.
246:693–701. 2007.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Bosset JF, Collette L, Calais G, Mineur L,
Maingon P, Radosevic-Jelic L, Daban A, Bardet E, Beny A and Ollier
JC: EORTC Radiotherapy Group Trial 22921. Chemotherapy with
preoperative radiotherapy in rectal cancer. N Engl J Med.
355:1114–1123. 2006.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Topova L, Hellmich G, Puffer E, Schubert
C, Christen N, Boldt T, Wiedemann B, Witzigmann H and Stelzner S:
Prognostic value of tumor response to neoadjuvant therapy in rectal
carcinoma. Dis Colon Rectum. 54:401–411. 2011.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Tomono A, Yamashita K, Kanemitsu K, Sumi
Y, Yamamoto M, Kanaji S, Imanishi T, Nakamura T, Suzuki S, Tanaka K
and Kakeji Y: Prognostic significance of pathological response to
preoperative chemoradiotherapy in patients with locally advanced
rectal cancer. Int J Clin Oncol. 21:344–349. 2016.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Tada N, Kawai K, Tsuno NH, Ishihara S,
Yamaguchi H, Sunami E, Kitayama J, Oba K and Watanabe T: Prediction
of the preoperative chemoradiotherapy response for rectal cancer by
peripheral blood lymphocyte subsets. World J Surg Oncol.
13(30)2015.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Ishihara S, Iinuma H, Fukushima Y, Akahane
T, Horiuchi A, Shimada R, Shibuya H, Hayama T, Yamada H, Nozawa K,
et al: Radiation-induced apoptosis of peripheral blood lymphocytes
is correlated with histological regression of rectal cancer in
response to preoperative chemoradiotherapy. Ann Surg Oncol.
19:1192–1198. 2012.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Shinto E, Hase K, Hashiguchi Y, Sekizawa
A, Ueno H, Shikina A, Kajiwara Y, Kobayashi H, Ishiguro M and
Yamamoto J: CD8+ and FOXP3+ tumor-infiltrating T cells before and
after chemoradiotherapy for rectal cancer. Ann Surg Oncol. 21
(Suppl 3):S414–S421. 2014.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Yasuda K, Nirei T, Sunami E, Nagawa H and
Kitayama J: Density of CD4(+) and CD8(+) T lymphocytes in biopsy
samples can be a predictor of pathological response to
chemoradiotherapy (CRT) for rectal cancer. Radiat Oncol.
6(49)2011.PubMed/NCBI View Article : Google Scholar
|
|
10
|
McCoy MJ, Hemmings C, Miller TJ, Austin
SJ, Bulsara MK, Zeps N, Nowak AK, Lake RA and Platell CF: Low
stromal Foxp3+ regulatory T-cell density is associated with
complete response to neoadjuvant chemoradiotherapy in rectal
cancer. Br J Cancer. 113:1677–1686. 2015.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Teng F, Meng X, Kong L, Mu D, Zhu H, Liu
S, Zhang J and Yu J: Tumor-infiltrating lymphocytes, forkhead box
P3, programmed death ligand-1, and cytotoxic T
lymphocyte-associated antigen-4 expressions before and after
neoadjuvant chemoradiation in rectal cancer. Transl Res.
166:721–732.e1. 2015.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Anitei MG, Zeitoun G, Mlecnik B, Marliot
F, Haicheur N, Todosi AM, Kirilovsky A, Lagorce C, Bindea G,
Ferariu D, et al: Prognostic and predictive values of the
immunoscore in patients with rectal cancer. Clin Cancer Res.
20:1891–1899. 2014.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Taylor MR, Couto JR, Scallan CD, Ceriani
RL and Peterson JA: Lactadherin (formerly BA46), a
membrane-associated glycoprotein expressed in human milk and breast
carcinomas, promotes Arg-Gly-Asp (RGD)-dependent cell adhesion. DNA
Cell Biol. 16:861–869. 1997.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Hanayama R, Tanaka M, Miwa K, Shinohara A,
Iwamatsu A and Nagata S: Identification of a factor that links
apoptotic cells to phagocytes. Nature. 417:182–187. 2002.PubMed/NCBI View
Article : Google Scholar
|
|
15
|
Miyasaka K, Hanayama R, Tanaka M and
Nagata S: Expression of milk fat globule epidermal growth factor 8
in immature dendritic cells for engulfment of apoptotic cells. Eur
J Immunol. 34:1414–1422. 2004.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Li BZ, Zhang HY, Pan HF and Ye DQ:
Identification of MFG-E8 as a novel therapeutic target for
diseases. Expert Opin Ther Targets. 17:1275–1285. 2013.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Jinushi M, Nakazaki Y, Dougan M, Carrasco
DR, Mihm M and Dranoff G: MFG-E8-mediated uptake of apoptotic cells
by APCs links the pro- and antiinflammatory activities of GM-CSF. J
Clin Invest. 117:1902–1913. 2007.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Tibaldi L, Leyman S, Nicolas A, Notebaert
S, Dewulf M, Ngo TH, Zuany-Amorim C, Amzallag N, Bernard-Pierrot I,
Sastre-Garau X and Théry C: New blocking antibodies impede
adhesion, migration and survival of ovarian cancer cells,
highlighting MFGE8 as a potential therapeutic target of human
ovarian carcinoma. PLoS One. 8(e72708)2013.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Sugano G, Bernard-Pierrot I, Laé M,
Battail C, Allory Y, Stransky N, Krumeich S, Lepage ML, Maille P,
Donnadieu MH, et al: Milk fat globule-epidermal growth
factor-factor VIII (MFGE8)/lactadherin promotes bladder tumor
development. Oncogene. 30:642–653. 2011.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Soki FN, Koh AJ, Jones JD, Kim YW, Dai J,
Keller ET, Pienta KJ, Atabai K, Roca H and McCauley LK:
Polarization of prostate cancer-associated macrophages is induced
by milk fat globule-EGF factor 8 (MFG-E8)-mediated efferocytosis. J
Biol Chem. 289:24560–24572. 2014.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Oba J, Moroi Y, Nakahara T, Abe T,
Hagihara A and Furue M: Expression of milk fat globule epidermal
growth factor-VIII may be an indicator of poor prognosis in
malignant melanoma. Br J Dermatol. 165:506–512. 2011.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Zhao Q, Xu L, Sun X, Zhang K, Shen H, Tian
Y, Sun F and Li Y: MFG-E8 overexpression promotes colorectal cancer
progression via AKT/MMPs signalling. Tumour Biol.
39(1010428317707881)2017.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Kusunoki R, Ishihara S, Tada Y, Oka A,
Sonoyama H, Fukuba N, Oshima N, Moriyama I, Yuki T, Kawashima K, et
al: Role of milk fat globule-epidermal growth factor 8 in colonic
inflammation and carcinogenesis. J Gastroenterol. 50:862–875.
2015.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Brierley JD, Gospodarowicz MK and
Wittekind C (eds): The TNM classification of malignant tumours, 8th
edition. Wiley Blackwell, Oxford, 2017.
|
|
25
|
Japanese classification of colorectal
carcinoma. Kanehara & Co., Ltd., Tokyo, 2018.
|
|
26
|
Kanemura T, Miyata H, Makino T, Tanaka K,
Sugimura K, Hamada-Uematsu M, Mizote Y, Uchida H, Miyazaki Y,
Takahashi T, et al: Immunoregulatory influence of abundant MFG-E8
expression by esophageal cancer treated with chemotherapy. Cancer
Sci. 109:3393–3402. 2018.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Crane CH, Skibber JM, Feig BW, Vauthey JN,
Thames HD, Curley SA, Rodriguez-Bigas MA, Wolff RA, Ellis LM,
Delclos ME, et al: Response to preoperative chemoradiation
increases the use of sphincter-preserving surgery in patients with
locally advanced low rectal carcinoma. Cancer. 97:517–524.
2003.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Habr-Gama A, Perez RO, Proscurshim I,
Campos FG, Nadalin W, Kiss D and Gama-Rodrigues J: Patterns of
failure and survival for nonoperative treatment of stage c0 distal
rectal cancer following neoadjuvant chemoradiation therapy. J
Gastrointest Surg. 10:1319–1329. 2006.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Yu CS, Yun HR, Shin EJ, Lee KY, Kim NK,
Lim SB, Oh ST, Kang SB, Choi WJ, Lee WY, et al: Local excision
after neoadjuvant chemoradiation therapy in advanced rectal cancer:
A national multicenter analysis. Am J Surg. 206:482–487.
2013.PubMed/NCBI View Article : Google Scholar
|
|
30
|
McCoy MJ, Hemmings C, Anyaegbu CC, Austin
SJ, Lee-Pullen TF, Miller TJ, Bulsara MK, Zeps N, Nowak AK, Lake RA
and Platell CF: Tumour-infiltrating regulatory T cell density
before neoadjuvant chemoradiotherapy for rectal cancer does not
predict treatment response. Oncotarget. 8:19803–19813.
2017.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Jinushi M, Sato M, Kanamoto A, Itoh A,
Nagai S, Koyasu S, Dranoff G and Tahara H: Milk fat globule
epidermal growth factor-8 blockade triggers tumor destruction
through coordinated cell-autonomous and immune-mediated mechanisms.
J Exp Med. 206:1317–1326. 2009.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Cani PD, Amar J, Iglesias MA, Poggi M,
Knauf C, Bastelica D, Neyrinck AM, Fava F, Tuohy KM, Chabo C, et
al: Metabolic endotoxemia initiates obesity and insulin resistance.
Diabetes. 56:1761–1772. 2007.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Yang L, Francois F and Pei Z: Molecular
pathways: Pathogenesis and clinical implications of microbiome
alteration in esophagitis and Barrett esophagus. Clin Cancer Res.
18:2138–2144. 2012.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Meng C, Bai C, Brown TD, Hood LE and Tian
Q: Human gut microbiota and gastrointestinal cancer. Genomics
Proteomics Bioinformatics. 16:33–49. 2018.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Ladoire S, Martin F and Ghiringhelli F:
Prognostic role of FOXP3+ regulatory T cells infiltrating human
carcinomas: The paradox of colorectal cancer. Cancer Immunol
Immunother. 60:909–918. 2011.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Canani RB, Costanzo MD, Leone L, Pedata M,
Meli R and Calignano A: Potential beneficial effects of butyrate in
intestinal and extraintestinal diseases. World J Gastroenterol.
17:1519–1528. 2011.PubMed/NCBI View Article : Google Scholar
|
|
37
|
González-Sarrías A, Giménez-Bastida JA,
Núñez-Sánchez MÁ, Larrosa M, García-Conesa MT, Tomás-Barberán FA
and Espín JC: Phase-II metabolism limits the antiproliferative
activity of urolithins in human colon cancer cells. Eur J Nutr.
53:853–864. 2014.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Jinushi M, Nakazaki Y, Carrasco DR,
Draganov D, Souders N, Johnson M, Mihm MC and Dranoff G: Milk fat
globule EGF-8 promotes melanoma progression through coordinated Akt
and twist signaling in the tumor microenvironment. Cancer Res.
68:8889–8898. 2008.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Kong JC, Guerra GR, Pham T, Mitchell C,
Lynch AC, Warrier SK, Ramsay RG and Heriot AG: Prognostic impact of
tumor-infiltrating lymphocytes in primary and metastatic colorectal
cancer: A Systematic review and meta-analysis. Dis Colon Rectum.
62:498–508. 2019.PubMed/NCBI View Article : Google Scholar
|